Abstract
Objective. The aim was to study symptoms managed as the main problem by the general practitioner (GP) and to describe the frequencies and characteristics of presented symptoms when no specific diagnosis could be made. Design. Cross- sectional study. Setting. General practices in the Central Denmark Region. Subjects. In total, 397 GPs included patients with face-to-face contacts during one randomly assigned day in 2008–2009; 7008 patients were included and 5232 presented with a health problem. Main outcome measures. GPs answered a questionnaire after each patient contact. Symptoms and specific diagnoses were subsequently classified using the International Classification of Primary Care (ICPC). Symptom frequency, comorbidity, consultation length, and GP-assessed final outcome and burden of consultations were analysed. Results. The GPs could not establish a specific diagnosis in 36% of patients with health problems. GPs expected that presented symptoms would not result in a future specific diagnosis for half of these patients. Musculoskeletal (lower limb and back) and respiratory (cough) symptoms were most frequent. More GPs had demanding consultations when no specific diagnosis could be made. Higher burden was associated with age, comorbidity, and GP expectancy of persistent symptoms when no diagnosis could be made. Conclusion. Interpretation and management of symptoms is a key task in primary care. As symptoms are highly frequent in general practice, symptoms without a specific diagnosis constitute a challenge to GPs. Nevertheless, symptoms have been given little priority in research. More attention should be directed to evidence-based management of symptoms as a generic phenomenon to ensure improved outcomes in the future.
Keywords: Cross-sectional, Denmark, diagnosis, general practice, medically unexplained symptoms (non-MESH), primary health care, signs and symptoms
GPs handled symptoms without diagnosis in 36% of patients presenting with health problems; half of the symptoms were expected to resolve or persist as “medically unexplained”.
Consultations were found more demanding when dealing with symptoms without specific diagnosis, in particular when symptoms were expected to be persistent.
The study highlights the need for a professional and scientific approach to symptoms as a phenomenon in its own right.
Introduction
Patients present with symptoms and unselected health problems in primary care, and general practitioners (GPs) generally find symptoms and complaints meaningful to deal with [1]. Nevertheless, symptoms as a generic phenomenon have been devoted little attention in research. The WONCA Europe research agenda states that professional management of as yet unclarified symptoms and signs is a core competency in general practice [2], but the primary focus of this agenda and most research is on assessment of symptoms as early signs of physical disease or psychiatric disorder. However, in primary care, symptoms may take other trajectories, which need further exploration.
The subjective experience of symptoms is common, and symptoms are frequently reported in primary care [3,4]. Nevertheless, consultations focusing on symptoms (as the main problem) that are concluded without a clinical diagnosis have been less explored. Symptom frequency has been reported in primary care surveys, but the estimated magnitude varies considerably, from 20% to 65%, due to differences in research settings and case definitions [5–7].
A few studies have investigated the persistence of symptoms. As much as half of all common symptoms may be classified as persistent on a long-term scale [7,8], and patients with persistent symptoms may risk developing poor health and work disability [3,9–12]. Furthermore, GPs tend to focus on the biomedical aspects of experienced health problems [13], which may increase the risk of iatrogenic harm when symptoms persist [14].
Most primary care studies on symptoms without diagnosis have been dedicated to the subgroup of symptoms that turn out to be persistent or medically unexplained upon thorough examination. Due to a poor definition of the concept of medically unexplained symptoms (MUS), especially regarding milder conditions [15], most literature in this field addresses severe and persistent disorders, but includes only a few encounters dealing with the initial presentation and management of symptoms. In line with this, an exploratory mixed-methods study showed that GPs would label only a minority of their encounters (3–6%) as MUS although a third of all encounters dealt with symptoms without a final diagnosis [16]. Recent research even suggests abandoning the term MUS and instead focusing on symptoms in general [17].
In consideration of the high frequencies of symptoms in primary care and the risk of negative consequences, symptom research that is independent of specific diagnoses deserves more attention in the medical arena. Hence, we set out to explore symptoms as a generic phenomenon (i.e. symptoms for which the GP could not establish a specific diagnosis at the end of the consultation). This concept included not only resolving symptoms and MUS, but also symptoms that later developed into a specific disease or disorder. We aimed to study the frequency and specific characteristics of symptoms without diagnosis managed by the GP and to explore the GP's assessed consultation length and perceived burden of consultation in the cases where no diagnosis was made.
Material and methods
Design and setting
The present cross-sectional study is based on data from a survey of Danish general practice, which was conducted from December 2008 to December 2009 [18]. The Central Denmark Region is a mixed rural and metropolitan area with almost 1.3 million inhabitants served by 871 GPs (covering approximately 20% of the entire Danish population). The Danish health-care system is tax-funded, and 98% of all Danes are listed with a general practice.
Participants
All GPs in the Central Denmark Region were invited to participate. Participating GPs registered all patient contacts during one randomly assigned work-day. The GPs received remuneration for their participation (€32) and for each registered contact (€3).
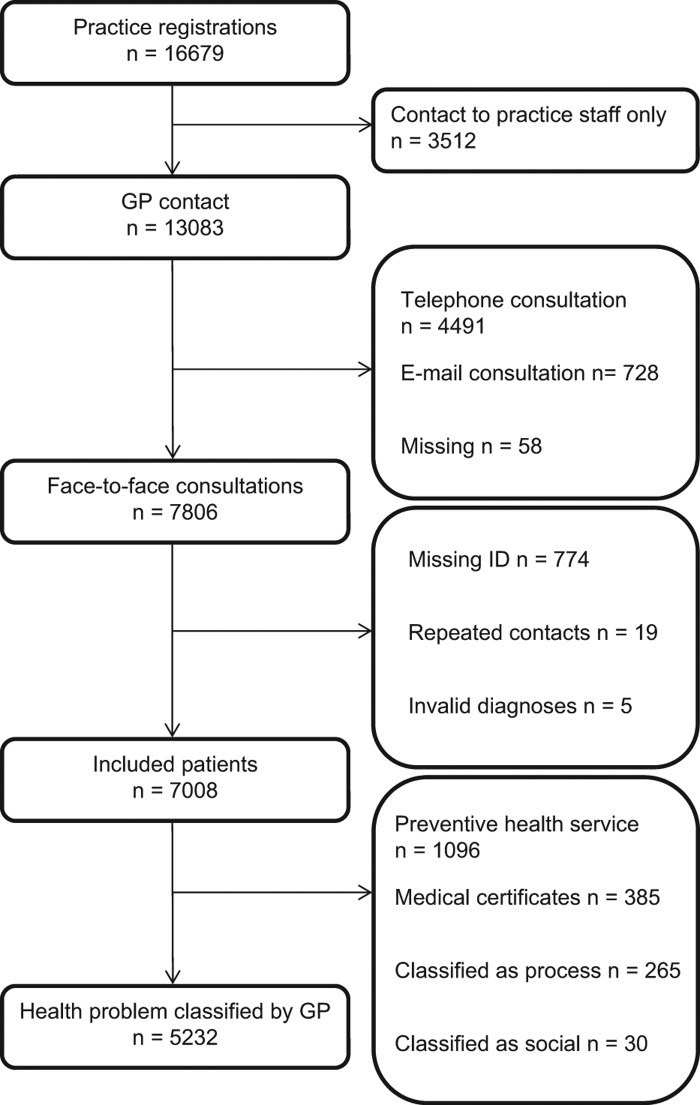
For the purpose of the present paper, we included GP face-to-face contacts (consultations and home visits) with patients identified by their civil registration number (ID). Contacts with missing IDs could not be associated with individuals and were excluded. Half of these (n = 388) were caused by 20 GPs who chose not to state the ID of their patients. If the patients appeared more than once, only their first contact was included in the study (Figure 1).
Figure 1.
Flow of patient inclusion.
Data sources, variables, and outcome measures
Background information on GPs and patients listed with participating practices was obtained from the Danish National Health Service Register.
Each patient contact was registered on a one-page registration form by the GP. The form included questions on the civil registration number, gender, age, type of contact (face-to-face consultation, home visit, telephone, or e-mail contact), and content of contact (health problem, preventive health service, or health certificate). Furthermore, GPs entered the main reason for encounter (RFE), as stated by the patient, and added their own assessment of the main problem at the end of the consultation. GPs could enter this information as free text or by using codes from the International Classification of Primary Care (ICPC). Text entered on the registration forms was translated into ICPC-2-R codes by an ICPC-trained medical student using an electronic standard terminology (http://www.dak-e.dk/icpc). All ICPC codes were reviewed by one of the authors (GM). All ICPC codes were subsequently dichotomized into “symptoms without diagnosis” (component 1, except for specific codes in the skin chapter, addiction, and contraception) and “specific diagnoses” (other codes). The ICPC consists of 17 chapters, which in combination constitute seven main components: symptom codes (component 1), process codes (components 2–6), and specific disease codes (component 7).
If the GP stated more than one diagnosis (207 contacts; 3.7%), the first code entered on the registration form was included in the analysis. In cases where the diagnosis was missing as the GP had chosen only to provide a label or code for the RFE (n = 741, 13.4%), the RFE was extrapolated to replace the missing diagnostic code.
GPs also listed the following information: number of problems presented, chronic conditions, expected final outcome (specific disease, resolving symptom, or persistent/medically unexplained symptom), consultation length (duration in minutes), and GP-perceived burden of consultation (rated between 1 and 10).
Only consultations concerning health problems were included in the main analyses, while consultations categorized on the registration form as “preventive health service” or “health certificates” and consultations involving ICPC codes for processes and social problems were excluded after the initial analyses. Patients with symptoms without a diagnosis were compared with patients with a specific diagnosis.
Statistical methods
The representativeness of the participating GPs with regard to gender, seniority, and type of practice (single-handed or partnership) was examined using chi-square statistics. The association between patient group and patient age and gender was also tested using the same approach. For GP assessments, tests were adjusted for patient age, gender, chronic disorders, and GP clusters using generalized linear models (GLM) with ID link and the Bernoulli family supplemented by Wald tests in combined analyses. Odds ratios for GP-assessed burden of consultation were calculated using an ordered logistic regression model with mutual adjustments for included parameters. The proportional odds assumption was checked using a Brant test. Each contact registration form was optically scanned by TeleForm 8.0™ (Digital Vision, Highland Park, IL, USA), and Stata 13.1™ (StataCorp LP, College Station, TX, USA) was used for the statistical analyses.
Results
Characteristics of GPs and patient contacts
A total of 387 GPs (44.4%) consented to participate in the survey [13]. Patients listed with participating GPs were comparable to those listed with non- participating GPs with regard to age and gender distribution (p = 0.354 and 0.389, respectively). Furthermore, contacts not included due to missing ID were statistically comparable to included patients with regard to age and gender.
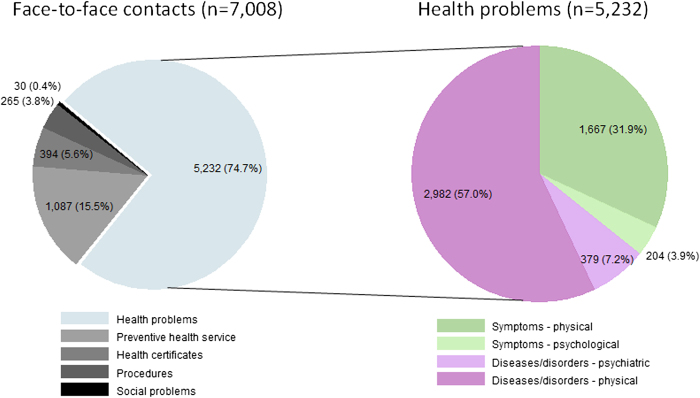
A total of 7008 patients with face-to-face contacts formed the population of the present study. Of these, 5232 (74.7%) consulted for a health problem, with 5059 practice consultations and 173 home visits (see Figures 1 and 2). On average, each GP had 8.3 (standard deviation [SD] 5.5) contacts regarding a health problem during one day (median 7; interquartile range [IQR] 4–12); 61% were consultations with women, 59% were first-contact consultations, and 35% of the patients presented more than one health problem in the consultation.
Figure 2.
Encounters in general practice (type of contact and GP diagnoses of health problems).
Frequency of symptoms without diagnosis
The frequencies of GP diagnoses for health problems are presented in Figure 2. The GP did not make a specific diagnosis for the presented health problem at the end of the consultation in 35.8% of cases, i.e. in 26.7% of all contacts. However, the GP diagnoses of health problems varied; the mean frequency of symptoms without diagnosis was 36.4% (SD 17.4%), and the median was 34.8 (IQR 25.0–47.1%). Subgroup analyses of psychological health problems, i.e. 11.1% of all presented health problems (see Figure 2), showed identical frequencies; 65.0% of patients were given a specific diagnosis, whereas 35.0% were classified as symptoms.
In 64.0% of all contacts, patients consulted the GP due to symptoms alone, i.e. symptoms were stated as their main RFE. In this group, the frequency of symptoms without a diagnosis was 52.3%, a mean for GPs of 56.8% (SD 27.1) and a median of 53.3% (IQR 37.5–80.0%).
The frequency of symptoms without diagnosis was influenced by gender, age, and whether the patient came for a first consultation (40.0% [n = 1162] of first-time consultations [n = 2908)] or for a follow-up consultation (29.2% [n = 582] of follow-up consultations [n = 1992]). Compared with patients with specific diagnoses, a higher proportion of patients with symptoms without diagnosis were women in the age group 18–65 years who presented their health problems for the first time (Table I).
Table I.
Characteristics of symptoms without diagnosis (compared with specific diagnoses).
| Symptom n (%) |
Disease/disorder diagnosed n (%) |
Total n (%) |
||
|---|---|---|---|---|
| 1871 | 3361 | 5232 | ||
| Gender: | ||||
| Female | 1167 (62.4) | 2003 (59.6) | 3170 (60.6) | 0.0491 |
| Male | 704 (37.6) | 1358 (40.4) | 2062 (39.4) | |
| Age: | ||||
| 0–18 years | 293 (15.7) | 529 (15.7) | 822 (15.7) | 0.0011 |
| > 18 and < 65 years | 1179 (63.0) | 1968 (58.6) | 3147 (60.2) | |
| 65 + years | 399 (21.3) | 864 (25.7) | 1263 (24.1) | |
| Consultation type:* | ||||
| First consultation | 1162 (66.6) | 1746 (55.3) | 2908 (59.4) | < 0.0012 |
| Follow-up consultation | 582 (33.4) | 1410 (44.7) | 1992 (40.7) | |
| Reason for encounter according to the GP:* | ||||
| Symptom | 1627 (92.2) | 1484 (48.0) | 3111 (64.0) | < 0.0012 |
| Disease/disorder | 137 (7.8) | 1609 (52.0) | 1746 (36.0) | |
| Concomitant chronic disorder: | ||||
| No | 1146 (61.3) | 1808 (53.8) | 2954 (56.5) | < 0.0012 |
| Yes | 725 (38.7) | 1553 (46.2) | 2278 (43.5) | |
| GP assessment of final outcome:* | ||||
| Specific diagnosis | 925 (50.8) | 2535 (77.8) | 3460 (68.1) | < 0.0012 |
| Resolving symptom | 718 (39.4) | 561 (17.2) | 1279 (25.2) | |
| Persistent (medically unexplained) symptom | 179 (9.8) | 164 (5.0) | 343 (6.7) | |
| Length of consultation:* | ||||
| < = 5 minutes | 188 (10.2) | 491 (14.8) | 679 (13.1) | < 0.0012 |
| 5–15 minutes | 1281 (69.5) | 2251 (67.7) | 3532 (68.4) | |
| 15–30 minutes | 338 (18.4) | 545 (16.4) | 883 (17.1) | |
| > 30 minutes | 35 (1.9) | 37 (1.1) | 72 (1.4) | |
| Burden* | ||||
| 1–2 (0–20 centile) | 510 (27.9) | 1236 (37.3) | 1746 (34.0) | < 0.0012 |
| 3–6 (20–80 centile) | 943 (51.5) | 1574 (47.6) | 2517 (49.0) | |
| 7–10 (80–100 centile) | 377 (20.6) | 501 (15.1) | 878 (17.1) |
Notes: *Missing values in GP questionnaire were: RFE (n = 375), consultation type (n = 332), GP assessment (n = 150), length of consultation (n = 66), burden (n = 91).
Statistical tests: 1 = chi-squared test, 2 = Wald test adjusted for gender, age, chronic disorder, and GP clusters.
Characteristics of symptoms without diagnosis
Ten symptoms accounted for 35.8% of all symptoms without diagnosis. The 10 most frequent symptoms are listed in Table II for various age groups. Not unexpectedly, symptoms varied with age; cough and fever were frequent among children, and cardio- pulmonary symptoms tended to increase with age, whereas psychological problems were common among younger adults.
Table II.
The 10 most frequent symptoms without diagnosis (according to age).
| Symptom | ICPC code | All | 0–18 years | 18–65 years | > = 65 years |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | ||
| Lower limb | L13–L17 | 128 (6.8) | 20 (6.8) | 78 (6.6) | 30 (7.5) |
| Cough | R05 | 107 (5.7) | 39 (13.3) | 50 (4.2) | 18 (4.5) |
| Back symptom | L02–L03 | 93 (5.0) | 9 (3.1) | 68 (5.8) | 16 (4.0) |
| Acute stress reaction | P02 | 68 (3.6) | 58 (4.9) | ||
| Upper limb | L08–L12 | 64 (3.4) | 2 (0.7) | 53 (4.5) | 9 (2.3) |
| Rash localized | S06 | 47 (2.5) | 12 (4.1) | 27 (2.3) | |
| Muscle pain | L18 | 47 (2.5) | 33 (2.8) | 12 (3.0) | |
| Weakness/tiredness | A04 | 42 (2.2) | 6 (2.0) | 25 (2.1) | 11 (2.8) |
| Vertigo/dizziness | N17 | 39 (2.1) | 16 (4.0) | ||
| Headache | N01 | 35 (1.9) | 27 (2.3) | ||
| Fever | A03 | 18 (6.1) | |||
| Abdominal pain | D01 | 9 (3.1) | |||
| Constipation | D12 | 8 (2.7) | |||
| Diarrhoea | D11 | 7 (2.4) | |||
| Bedwetting/enuresis | P12 | 7 (2.4) | |||
| Feeling anxious/nervous/tense | P01 | 25 (2.1) | |||
| Sleep disturbance | P06 | 13 (3.3) | |||
| Swollen ankles/oedema | K07 | 9 (2.3) | |||
| Shortness of breath/dyspnoea | R02 | 9 (2.3) | |||
| Total for all diagnoses (n) | 1871 | 293 | 1179 | 399 |
Note: Top three most common symptoms in each column have been marked in bold.
Musculoskeletal symptoms were frequent in all age groups. The pattern among women was the same as described for all in Table 2, whereas dyspnoea (2.0%) and sleep problems (1.8%) replaced vertigo and headache among the 10 most common symptoms for men.
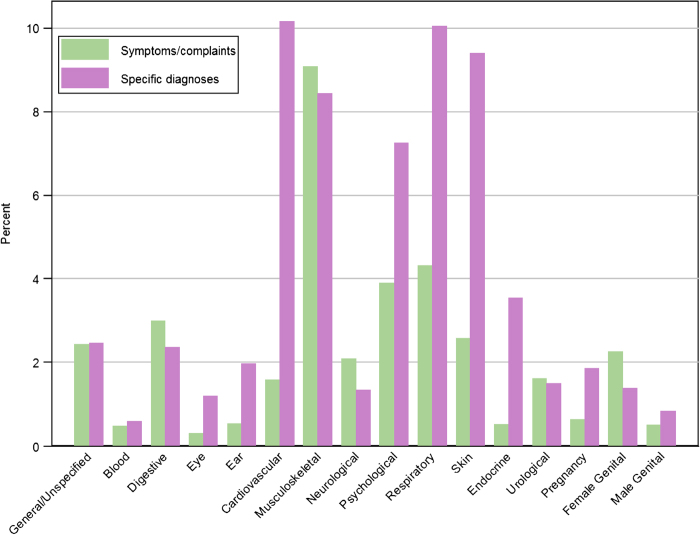
For symptoms without diagnosis overall, the most common localisations were the musculoskeletal system (25.4% of symptoms and 9.1% of all health problems), followed by the respiratory system (12.1% and 4.3%, respectively) and psychological issues (10.9% and 3.9%, respectively). This pattern was the same for men alone, whereas musculoskeletal, psychological, and genital problems were the most frequent localisations among women. Symptoms relating to the respiratory or musculoskeletal systems were also dominant in all age groups, followed by the digestive system for children and the elderly, while psychological issues were prevalent in the group aged 18–65 years (see Figure 3 for details on localisations).
Figure 3.
Distribution of symptoms and specific diagnoses according to localization.
GP-assessed comorbidity and outcome of symptoms without diagnosis
Concomitant chronic disorders were stated in 43.5% (n = 2278) of all included patients. Not unexpectedly, the frequency was lower among patients with symptoms without diagnosis than among patients with a specific diagnosis (see Table I). The three most common disorders in both groups were diabetes (5.1% and 8.6%, respectively), depression (4.6% and 6.9%, respectively), and chronic obstructive pulmonary disease (4.3% and 4.7% respectively).
GPs expected 50.8% of all symptoms without a diagnosis (n = 1822) to develop into a specific disease; 9.8% were expected to become persistent symptoms, while 39.4% were thought likely to resolve.
Consultation length and burden
GPs spent on average 13.2 minutes (SD 6.9) per consultation, and most consultations lasted 5–15 minutes (see Table II). Consultations regarding symptoms for which no specific diagnosis could be established were slightly longer than other types of consultations (13.7 vs. 12.9 minutes, p < 0.001).
Furthermore, the GPs more often found these consultations more burdensome than consultations resulting in a specific diagnosis (see Table I) (median 4, IQR 2–6 vs. median 3, IQR 2–5). An exploratory analysis of burden in consultations regarding symptoms without diagnosis demonstrated a higher probability of having comorbid chronic disorders (adjusted OR 1.98; 95% CI 1.60–2.46), and of being assessed as having persistent symptoms (adjusted OR 3.28; 95% CI 2.33–4.61). Furthermore, burden was associated with age (adjusted OR for age groups 18–65 and 65 + were 1.60; 95% CI 1.23–2.08, and 1.68; 95% CI 1.21–2.33, respectively) but not with gender. Psychological and musculoskeletal problems were identified most frequently among patients causing a high burden.
Discussion
Key results
Symptoms were the predominant reason for encounters in primary care. In one-third of the patients with health problems, or half of the patients presenting symptoms as their primary reason for encounter, the GP could not make a specific diagnosis. This was irrespective of whether the symptoms were physical or mental. When GPs dealt with patients without a specific diagnosis, they found the encounters more burdensome. Although these patients generally had less comorbidity and 39% were expected to have resolving symptoms, high burden was associated with comorbidity and GP expectancy of persistent symptoms. The 10 most common symptoms accounted for 36% of all symptoms without diagnosis; the most common related to the musculoskeletal and respiratory systems.
Strengths and limitations
A major strength of this study was the large number of GPs and patients who agreed to participate; this ensures that data are representative of patients in the primary care setting. However, the setting itself is selected, and we do not know the extent to which the results may apply to other (e.g. non-Western) primary care settings. Most importantly, the study design ensured that the symptoms stated and explored were, in fact, dealt with by the GPs.
The prevalence of symptoms managed may have been underestimated for two reasons. First, GPs were allowed to give only one diagnostic label for each patient, but in about a third of all primary care encounters (including this study) patients present several problems in the same consultation [5]. Second, some GPs tend to place more emphasis on diseases than symptoms and hence may use specific diagnostic codes for particular symptom patterns. In this study, this is reflected in the frequency variations of the symptom diagnoses applied by the GPs. However, despite variation in GP classification, even the 25% percentile presented a significant frequency of symptoms without diagnosis.
The study was strengthened by the GPs’ option to use either ICPC diagnoses or describe their assessment in text, which was subsequently converted systematically to ICPC codes. On the other hand, the GPs’ diagnostic labelling was not validated. Previous studies have demonstrated high GP inter-rater variability, especially at the level of diagnostic codes, whereas variations at the level of chapters and components (symptom vs. disease) are generally smaller [19]. Hence, diagnostic variations would mainly affect the reporting of single-symptom frequencies.
Comparison with existing literature
Evaluations of primary care consultations and GPs’ diagnoses have mainly been published in health services reports, and consultations or health problems (rather than patients) have been applied as denominators. Our results on the frequency of symptoms are in agreement with these reports, but we have put more focus on symptoms as the main problem managed by the GP. The Royal College of General Practitioners in the UK showed that 30% of the health problems in 1958 were provided with only tentative diagnoses [20], and a later study found comparative proportions of 31% of consultations or 43% of health problems [21], while newer studies have found frequencies from 22% to 32% [5,22]. An American study reported a much higher prevalence of 48%, but this study was based on data from questionnaire screening before the consultation [7]. Lower frequencies of 13–19% are reported by GPs in studies of MUS [23,24]; these figures indicate that symptoms without diagnosis include a broader category of patients than MUS does.
The distribution of diagnoses across organ systems in our study is equivalent to previous findings of high frequencies of musculoskeletal problems (12–19%) and respiratory problems (12–13%) [5,22,25], although these studies have reported on symptoms and specific diseases combined.
The GPs expected about half of the symptoms without diagnosis to remain coded as symptoms (resolved or persistent). This proportion is somewhat higher than reported in most literature on MUS. In a five-year follow-up study, 34% of common symptoms remained medically unexplained [7]. This finding corresponds to a 10-year follow-up study, where 37% of all contacts remained coded as symptoms [6]. On the other hand, a study from 1989 found no specific diagnosis for common symptoms in 75% of all cases during three years of follow-up [26]. The different findings may be explained by variations in the included symptoms and denominators, but all studies indicate a high prevalence in primary care of symptoms that do not develop into specific diseases.
Furthermore, our findings that GPs tend to report higher burden for patients expected to have persistent symptoms or mental problems is in agreement with the current literature on MUS [1;27].
Interpretation and implications
Symptoms that are not related to a well-defined disease are common in primary care, and GPs generally find it demanding to deal with symptoms when no specific diagnosis can be made. Although GPs must deal with such symptoms every day in clinical practice, research and medical training still pay little attention to symptoms as a generic phenomenon [28]. The field of medicine tends to focus on symptoms as part of disease, and professional management of symptoms as such is downgraded.
Our results indicate that general medicine should include expertise in symptoms, whether or not symptoms are related to known disease. Research on symptoms as such would allow for future evidence-based education and improved treatment of patients seen in primary care. GPs must treat all patients professionally and respectfully; this includes an obligation to increase the existing knowledge concerning symptom epidemiology and risk indicators, thereby providing better management of symptoms [29]. As stated by Dinant in 2007, “In primary care treatment choices will be better supported by evidence relating signs and symptoms to outcomes, rather than finding better ways of making a precise etiological diagnosis” [30, p. 3].
Acknowledgments
The authors would like to thank participating GPs in the Central Denmark Region, their staff and their patients for their contributions to this study. Furthermore, they would like to acknowledge Peter Vedsted and Frede Olesen for their work on the Contact and Disease Pattern Cohort, which made this study possible.
Ethical approval
The project was approved by the Danish Data Protection Agency (J.no. 2010-41-5671) and by the Danish Health and Medicines Authority (J.no. 7-604-04-2/49/EHE). According to Danish law, approval by the National Committee on Health Research Ethics was not required as no biomedical intervention was performed in this study.
Funding sources
The study was funded by the Research Fund for General Practice of the Central Denmark Region, “Samarbejdsudvalget for Aarhus Amt”, the Danish Research Foundation for General Practice, and the Committee for Quality Improvement and Continuing Medical Education in the Central Denmark Region. The funding sources had no role in the study and no influence on data collection and analyses, interpretation of results, or writing of the publication.
Declaration of interest
All authors declare to have no competing interests. The authors alone are responsible for the content and writing of the paper.
References
- Halvorsen PA, Edwards A, Aaraas IJ, Aasland OG, Kristiansen IS. What professional activities do general practitioners find most meaningful? Cross sectional survey of Norwegian general practitioners. BMC Fam Pract 2013;14:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummers-Pradier E, Beyer M, Chevallier P, Eilat-Tsanani S, Lionis C, Peremans L, et al. The research agenda for general practice/family medicine and primary health care in Europe, Part 1: Background and methodology. Eur J Gen Pract 2009;15:243–50. [DOI] [PubMed] [Google Scholar]
- Kjeldsberg M, Tschudi-Madsen H, Dalen I, Straand J, Bruusgaard D, Natvig B. Symptom reporting in a general population in Norway: Results from the Ullensaker study. Scand J Prim Health Care 2013;31:36–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAteer A, Elliott AM, Hannaford PC. Ascertaining the size of the symptom iceberg in a UK-wide community-based survey. Br J Gen Pract 2011;61:e1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britt H, Miller GC, Henderson J, Bayram C, Valenti L, Harrison C, et al. General practice activity in Australia 2012– 2013. Sydney: Sydney University Press; 2013. [Google Scholar]
- Van Boven K., Lucassen P, van Ravesteijn HJ, Olde HT, Bor H, van Weel-Baumgarten E, et al. Do unexplained symptoms predict anxiety or depression? Ten-year data from a practice-based research network. Br J Gen Pract 2011; 61:e316–e325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JL, Passamonti M. The outcomes among patients presenting in primary care with a physical symptom at 5 years. J Gen Intern Med 2005;20:1032–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch H, van Bokhoven MA, Bindels PJ, van der Weijden T, Dinant GJ, ter RG. The course of newly presented unexplained complaints in general practice patients: A prospective cohort study. Fam Pract 2009;26:455–65. [DOI] [PubMed] [Google Scholar]
- Tomenson B, Essau C, Jacobi F, Ladwig KH, Leiknes KA, Lieb R, et al. Total somatic symptom score as a predictor of health outcome in somatic symptom disorders. Br J Psychiatry 2013;203:373–80. [DOI] [PubMed] [Google Scholar]
- Olde Hartman TC, Borghuis MS, Lucassen PL, van de Laar FA, Speckens AE, van WC. Medically unexplained symptoms, somatisation disorder and hypochondriasis: Course and prognosis. A systematic review. J Psychosom Res 2009;66: 363–77. [DOI] [PubMed] [Google Scholar]
- Aamland A, Malterud K, Werner EL. Phenomena associated with sick leave among primary care patients with medically unexplained physical symptoms: A systematic review. Scand J Prim Health Care 2012;30:147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rask MT, Rosendal M, Fenger-Grøn M, Bro F, Ornbol E, Fink P. Sick leave and work disability in patients with recent-onset multiple medically unexplained symptoms and persistent somatoform disorders: A 10-year follow-up of the FIP study. Gen Hosp Psychiatry 2015;37:53–9. [DOI] [PubMed] [Google Scholar]
- Rosendal M, Vedsted P, Christensen KS, Moth G. Psychological and social problems in primary care patients: General practitioners’ assessment and classification. Scand J Prim Health Care 2013;31:43–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon P. The potentially somatizing effect of clinical consultation. CNS Spectr 2006;11:190–200. [DOI] [PubMed] [Google Scholar]
- Olde HT, Hassink-Franke L, Dowrick C, Fortes S, Lam C, van der Horst H, et al. Medically unexplained symptoms in family medicine: Defining a research agenda. Proceedings from WONCA 2007. Fam Pract 2008;25:266–71. [DOI] [PubMed] [Google Scholar]
- Rask MT, Andersen RS, Bro F, Fink P, Rosendal M. Towards a clinically useful diagnosis for mild-to-moderate conditions of medically unexplained symptoms in general practice: A mixed methods study. BMC Fam Pract 2014;15:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpe M. Somatic symptoms: Beyond “medically unexplained”. Br J Psychiatry 2013;203:320–1. [DOI] [PubMed] [Google Scholar]
- Moth G, Olesen F, Vedsted P. Reasons for encounter and disease patterns in Danish primary care: Changes over 16 years. Scand J Prim Health Care 2012;30:70–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britt H, Angelis M, Harris E. The reliability and validity of doctor-recorded morbidity data in active data collection systems. Scand J Prim Health Care 1998;16:50–5. [DOI] [PubMed] [Google Scholar]
- The continuing observation and recording of morbidity : A study by the Research Committee of the College of General Practitioners. J Coll Gen Pract Res Newsl 1958;1:107–28. [PMC free article] [PubMed] [Google Scholar]
- Thomas KB. Temporarily dependent patient in general practice. BMJ 1974 30;1:625–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nossen JP. Hva foregaar på legekontorene? [What happens in the doctor's office?]. 2007 NAV-rapport 4. https://wwwnavno/Forsiden/_attachment/805368917? = true = &_ts = 116a9ace2a0 (accessed October 22, 2014)
- Peveler R, Kilkenny L, Kinmonth AL. Medically unexplained physical symptoms in primary care: A comparison of self-report screening questionnaires and clinical opinion. J Psychosom Res 1997;42:245–52. [DOI] [PubMed] [Google Scholar]
- Rosendal M, Bro F, Fink P, Christensen KS, Olesen F. Diagnosis of somatisation: Effect of an educational intervention in a cluster randomised controlled trial. Br J Gen Pract 2003;53:917–22. [PMC free article] [PubMed] [Google Scholar]
- Mansson J, Nilsson G, Strender LE, Bjorkelund C. Reasons for encounters, investigations, referrals, diagnoses and treatments in general practice in Sweden: A multicentre pilot study using electronic patient records. Eur J Gen Pract 2011;17:87–94. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: Incidence, evaluation, therapy, and outcome. Am J Med 1989;86:262–6. [DOI] [PubMed] [Google Scholar]
- Hahn SR. Physical symptoms and physician-experienced difficulty in the physician–patient relationship. Ann Intern Med 2001 1;134:897–904. [DOI] [PubMed] [Google Scholar]
- Shattock L, Williamson H, Caldwell K, Anderson K, Peters S. “They've just got symptoms without science”: Medical trainees’ acquisition of negative attitudes towards patients with medically unexplained symptoms. Patient Educ Couns 2013;91:249–54. [DOI] [PubMed] [Google Scholar]
- Love T, Fahey T. Defining diagnosis: Screening and decision making in primary care. Br J Gen Pract 2003;53:914–15. [PMC free article] [PubMed] [Google Scholar]
- Dinant GJ, Buntinx FF, Butler CC. The necessary shift from diagnostic to prognostic research. BMC Fam Pract 2007;8:53. [DOI] [PMC free article] [PubMed] [Google Scholar]