Abstract
Background
Uganda’s rapid population growth (3.2%) since 1948 has placed more demands on health sector and lowered living standard of Ugandans resulting into 49% of people living in acute poverty especially in post conflict Northern Uganda. The population rise was due to low use of contraceptive methods (21% in rural areas and 43% in urban areas) and coupled with high unmet need for family planning (41%). This indicated poor access to reproductive health services. Effective use of family planning could reduce the rapid population growth.
Objective
To determine obstacles to family planning use among rural women in Northern Uganda.
Design
A descriptive cross-sectional analytical study.
Setting
Atiak Health Centre IV, Amuru District, rural Northern Uganda.
Subjects
Four hundred and twenty four females of reproductive ages were selected from both Inpatient and Outpatient Departments of Atiak Health Centre IV.
Results
There was high level of awareness 418 (98.6%), positive attitude 333 (78.6%) and fair level of utilisation 230 (54.2%) of family planning. However, significant obstacles to family planning usage included; long distance to Health facility, unavailability of preferred contraceptive methods, absenteeism of family planning providers, high cost of managing side effects, desire for big family size, children dying less than five years old, husbands forbidding women from using family planning and lack of community leaders’ involvement in family planning programme.
Conclusions
In spites of the high level of awareness, positive attitude, and free family planning services, there were obstacles that hindered family planning usage among these rural women. However, taking services close to people, reducing number of children dying before their fifth birthday, educating men about family planning, making sure family planning providers and methods are available, reducing cost of managing side effects and involving community leaders will improve utilisation of family planning and thus reduce the rapid population growth and poverty.
INTRODUCTION
Uganda’s population was projected at 34.1 million in 2012, the high population has strained the economy of the country has led to Uganda being ranked 156 out of 179 countries on the Human development index. Northern Uganda had a more acute poverty (49%) than the rest of the regions in Uganda (1, 2). In 2012, 1.7 million babies were born reference. If this high population growth rate continues, Uganda’s population will be 54 million in 2025 and 130 million by 2050 (3). The main factors underlying the high population growth rate were the high fertility rate of 6.2 children per woman, the high unmet need for family planning (41%), the low contraceptive prevalence rate (24%) and the high teenage pregnancy rates (24%). This created a big gap in access to contraceptives (2, 3, 4). Contraceptive usages significantly declined in Northern Uganda from 21% in 2001/2 down to only 11% in 2005/6 whereas the unmet need for family planning increased from 26% in 2001/2 to 46% in 2005/6 (2).
Previous studies showed that key obstacles to family planning usage were; low level of education (5, 6), living in Northern Uganda, having three or more children, living in rural areas, husband’s disagreement on contraceptive use, perceived side effects, infant mortality; negative traditional practices, desires such as naming relatives, knowledge gaps on contraceptive methods, fears, rumours and misconceptions about specific methods and unavailability and poor quality of services (7, 8, 9). Likewise, unmet need for family planning increases with increase in ideal number of children women wanted to have (1, 2). However, spousal communication and approval of family planning increased it use. Likewise, respondents who had positive attitude and approved of family planning were two times as likely to be using contraceptives as those who disapproved (10). Unmet need for family planning reduces with age, education level of the women and of their partners and family planning awareness through the media (7).
Failure to control fertility rates and population growth rates points to inability to extend family planning services to the most vulnerable women. This rapid population growth put extra pressure on service delivery, infrastructure and resources needed to ensure the functionality of the existing infrastructure like drugs in the hospitals, scholastic materials in schools and social welfare programme. Addressing the obstacles to family planning use will reduce population growth and relieves pressure on health services (13).This study therefore look in to obstacles to family planning use among rural women in Northern Uganda.
MATERIALS AND METHODS
A descriptive cross-sectional study where both qualitative and quantitative data were collected. 424 participants were selected from both inpatient and outpatient Departments using simple random sampling and systematic random sampling respectively to fill semi-structured questionnaires. Quantitative data were analyzed using SPSS version 16.0. 40 FGD participants were also selected from both Inpatient and Outpatient Departments using simple random sampling and systematic random sampling respectively. They were interviewed in a group of 10 participants each four key informants were selected by convenience among those involved in family planning provision at Atiak Health Centre IV. Qualitative data were manually analysed. We got ethical clearance from St. Mary’s Hospital Lacor Institutional review board and approval from District Health Officer and the In-Charge of Atiak Health Centre IV. All respondents made a written informed consent before being included in the study.
RESULTS
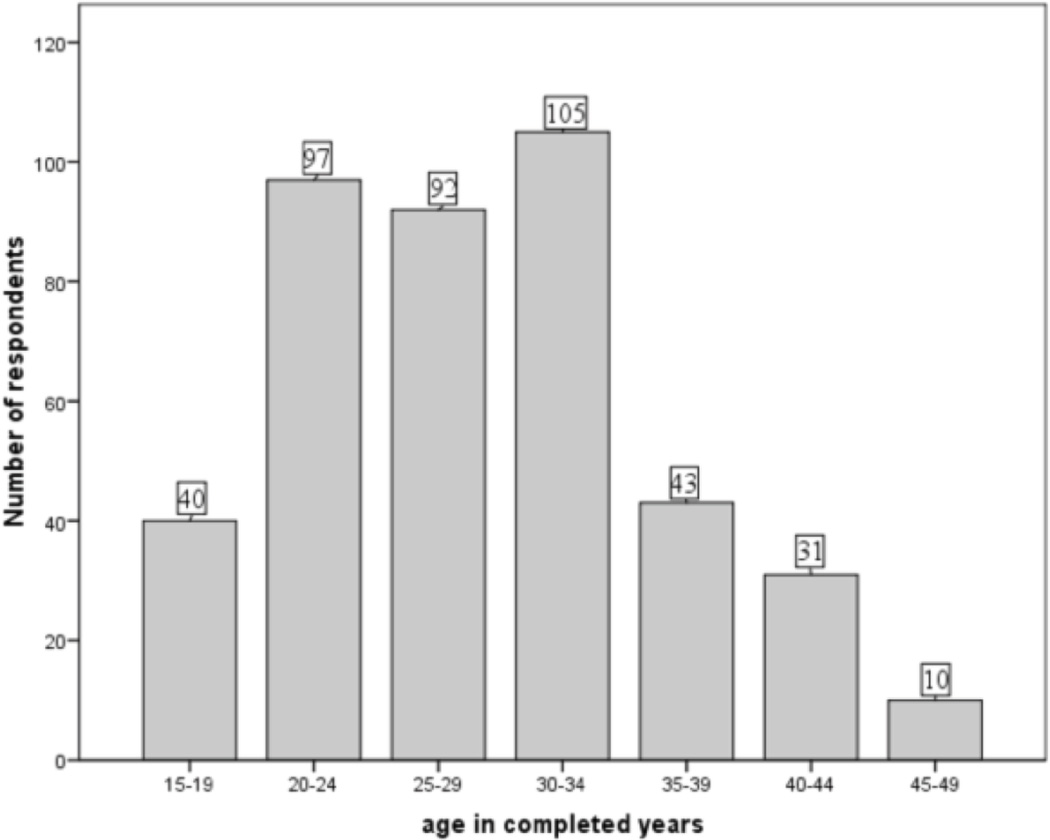
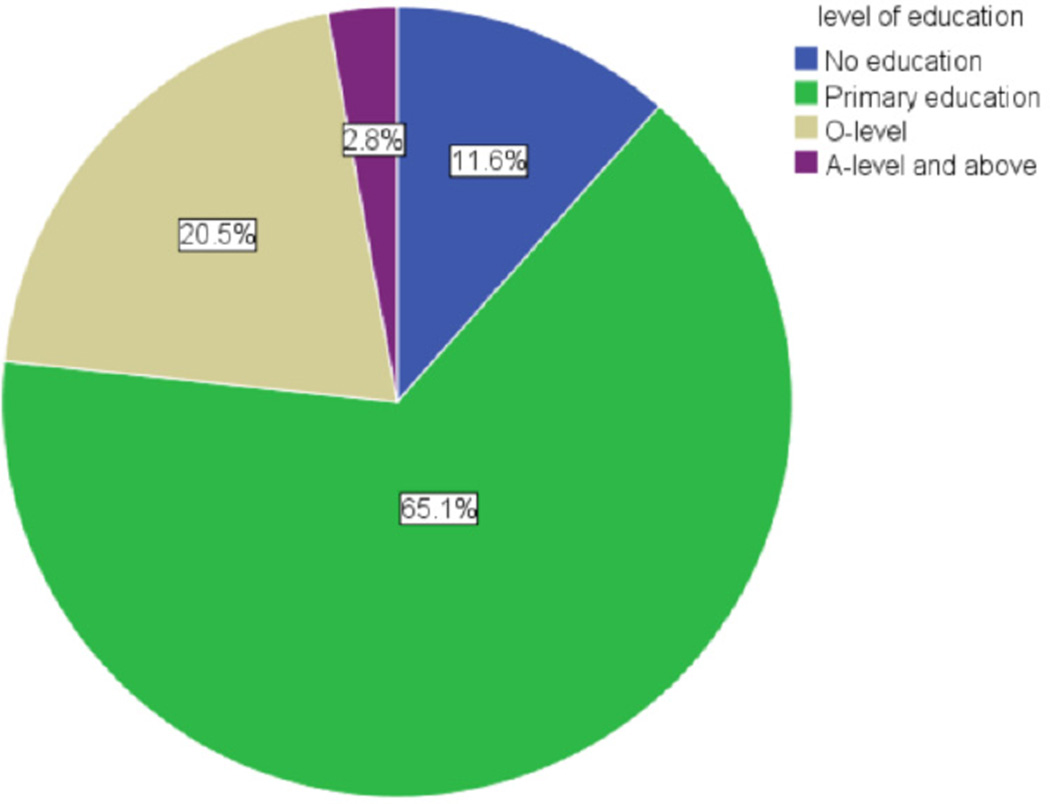
A total of 424 respondents were selected, majority were at their twenties 189 (44.6%) and thirties 148 (34.9%), farmers 332 (78.3%) who had at least some formal education 375 (88.4%) with 276 (65.1%) having primary education. Most women 357 (84.2%) were married and 344 of their spouses (91.7%) had at least primary education. Majority of the married women 309 (86.5%) first got married at teenage (19 years and below). Most married women 321 (85.6%) were dependents on their husbands as main source of household income compared to only 19 (5.1%) who were the main sources of household income. Most women 248 (58.5%) desired a moderate number (3–4) children. However, 148 women (34.9%) desired 5 or more children.
Family planning Awareness
Most women 418 (98.6 %) were aware of family planning. Three hundred and nineteen women (76.3%) last heard about family planning within the last six months prior the study. The main sources of family planning information were Health Centres 249 (58.7%), Village health team 85 (20%) and health educators 59 (14%). However, very few respondents mentioned either radio 6 (1.4%) or community leaders 1 (0.2%) as their sources of family planning information.
More importantly most of the respondents knew at least a source of family planning services 410 (96.7%). Family planning awareness was not affected by partners’ level of education. All the 40 participants in FGDs were aware of family planning and most had a fair knowledge about common family planning methods. There was a significant correlation between family planning awareness and positive attitudes towards and use of family planning (P=0.000) (P=0.000) respectively.
Attitudes towards family planning
Most women 333 (78.5%) had positive attitude towards family planning use. However, 64 women (15.1%) were undecided, and 12 women (2.8%) disapproved use of family planning use. Among the 383 mothers, 305 women of 365 (83.6%) who never had any child dying under age of 5 years had positive attitude towards use of family planning. Also 13 of the 15 women (86.7%) who had only (1–2) children dying under age of 5 years had positive attitude towards use of family planning. However, of the 12 women who had 3 or more than children dying under age of 5 years only 5 (41.6%) had positive attitude towards family planning use. 301 women aged (20–39) years of the 337 (89.3%) had positive attitude towards use of family planning. However, 30 of the 40 teenagers of (78.9%) were undecided about family planning use. Sexual partners’ approval of family planning increases with education level. At extremes only 10 of 20 (50 %) of husbands with No education approved that their spouse use family planning compared to 146 of 213 (68.5%), 32 of 44 (72.7%), 11 of 13 (84.6%) of husbands with Primary, Ordinary-level certificate and at least Advance-level certificate of education respectively.
Women who opposed use of family planning advanced the following reasons; fear of side effects, high cost of managing side effects, desire to have many children to take care of them at old age, uncertainty about the survival of children as such they desired giving birth to many so that at least some may be healthy.
Utilization of family planning
Two hundred and thirty women (54.2%) were using family planning methods. Highest proportion of users, 6 out of 9 (66.7%), were divorced women, followed by married women 217 (60.8%), and lowest among the single women 4 (8.5%). None of the 3 widows were using family planning. 2/3 of the women, 217 of 337 (64.4%) aged (20–39) years were using family planning. However, of the 40 teenagers, only 2 (5%) were using any of the family planning methods. Use of family planning methods increased with women’s education level. Contraceptive usage with respect to education levels were; 58.1%, 58.3% among Ordinary level and Advance level respectively compared to 39.6% among women with No education. However, partner’s level of education did not affect use of family planning; 17 women out of 31 (54.8%), 166 women out of 269 (61.7%), and 31 women out of 57 (54.4%) whose sexual partners had No, Primary, and Ordinary education respectively were using family planning. Family planning use reduced in participants whose children died less than 5 years of age. Majority of women, 218 out 365 (59.7%) who never lost a child less than five years of age were using family planning compared to only 3 out of 13 (23%) of women who ever lost more than 2 children less than 5 years of age. There was strong correlation between; spousal communication and positive attitude and current use of family planning (P=0.000) (P=0.000) respectively. However, 61 women (27.9%) were using family planning in spite of their sexual partners’ disapproval. Injectaplan was the most preferred family planning methods 166 (39.2%), followed by implant 111 (26.2%), and intrauterine device 36 (8.5%). Also among the members of FGDs most preferred family planning methods were; Injectaplan, and implants. Women stated that they faced the following problems in accessing family planning services; services far away from home 137 (32.3%), husbands forbid 73 (17.2%) and family forbid 21 (5%) them from using family planning services, services were not available 62 (14.6%).
Family planning providers at Atiak HC IV were well trained and competent. Modern family planning methods available included; short term methods (Pills, Male and Female condom, and Injectaplan), and the long term methods (Implants, and Coil). Permanent methods were only provided at the Health Centre by outreach teams from Marie Stopes Uganda but also few clients opted for them (KI1, KI2, KI3). Sole use of abstinence was discouraged, because it might not be reliable. Lactational amenorrhea method was also discouraged as women presume menstruation unaware and ended up with unplanned pregnancy. The Health Centre had stock piles of female condoms but women were not willing to use them (KI1). Family planning education was carried out daily in maternity during antenatal care visits but also sometimes during integrated community health outreaches (KI1, KI 4).
Women were willing to utilize modern family planning methods but providers were not there on the ground to offer them the services. FP services were cost free but mostly accessible to the nearby people. The problem was made worst since the Health Centre IIs did not provide family planning services as a result women from long distances who were using methods that needed refill usually came late for the refill. Due to inadequate man power, sometimes, there was no provider at the Health Centre and clients had to wait for a long time for the provider. No home based follow up programme was in place and in case of side effects that required medical attention, clients were managed at the facility. There was also Marie Stopes Uganda hotline for the family planning attaché if there was need for further consultation as far as managing side effects was concern (KI1, KI2, KI3, KI4). Lack of community links to the Centre providing family planning was an obstacles to family planning provision. Some women took decision to use family planning unilaterally and if men discovered, it often resulted in to quarrel. Culturally people thought there was no need for family planning since land was abundant and they needed to multiply and fill the land (KI 2). Preferred methods like the injectable, sometimes run out of stock. There is a National Family Planning policy but people were not aware of such policy because the policy was not communicated but the biggest challenge faced by clients was the long distance to the Health Centre where family planning services were provided (KI 4).
DISCUSSIONS
Family planning Awareness
Most women 418 (98.6 %) were aware of family planning. This is because family planning was cost free in all government and NGO Health Centres (19) and the universal primary and secondary education had improved education status of Ugandans. These findings agree with previous findings showing that almost all married women heard of at least one method of family planning (14). 319 women who were aware of family planning (76.3%) heard about it within the last 6 months prior to our study. The main sources of family planning information were; Health Centres 249 (58.7%), Village Health Team 85 (20%) and Health Educators 59 (14%) and very few respondents heard about family planning message over radio 6 (1.4%) or from the community leaders 1(0.2%). According to government policy family planning is a component of a good ante natal care service therefore health care workers should provide family planning services to any mother attending ante natal care (19). This explained why Health Centres were the main source of family planning education. There was little family planning awareness campaign over the radio stations coupled with the low coverage of radio in the rural households. This finding agree with a previous study showing that most (53.2%) of rural Ugandans get informations by words of mouth (15). The lack of involvement of community leaders in family planning programme is indicated by their low contribution towards family planning awareness.
Attitudes towards family planning: Most of the women, 333 (78.5%), had positive attitude towards family planning use. However, 64 (15.1%) women were undecided, while 12 women (2.8%) disapproved use of family planning. Among the 383 mothers, 305 women of 365 (83.6%) who never had any child dying under age of 5 years had positive attitude towards family planning use. Of the 15 women who lost (1–2) children under age of 5 years, 13 (86.7%) had positive attitude towards family planning use. However, of the 12 participants who had 3 or more than children dying under age of 5 years only 5 (41.6%) had positive attitude towards family planning use. These findings agree with a previous study implicating infant mortality as an obstacle to family planning use (9). Majority, 301 women of 337 (89.3%) aged (20–39) years had positive attitude towards of family planning use. However, of the 40 teenagers, 30 (78.9%) were undecided about family planning use. Sexual partners’ approval of family planning increased with education level: 10 of 20 (50 %) partners with no education approving family planning use compared to 146 of 213 (68.5%), 32 of 44 (72.7%), 11 of 13 (84.6%) of partners with Primary, Ordinary level and at least Advance level education respectively. Some women opposed family planning use for the following reasons; fear of side effects, high cost of managing side effects, desire to have many children for social security in their old ages, uncertainty about their children’s health.
Utilization of family planning
Majority of women 230 (54.2%) were currently using family planning methods. This finding agree with a study that showed that worldwide, contraceptive prevalence rate increased from 54·8% in 1990 to 63·3% in 2010 and that the East African region had one of the largest absolute increase in contraceptive prevalence rate (16). There was higher contraceptive prevalence rates among these rural women compared to the previous national figure 24 % (2). This finding is consonant with a study that showed that Amuru district had lower annual population growth rate of 2.9% (17) than the national figure of 3.2% (2, 3). The contraceptive prevalence rate due to the combine efforts of both the governments and the NGOs in providing family planning services in this post conflict region. This has led to improved availability of free family planning services to this population. Highest proportion of divorced women 6 of 9 (66.7%) were using family planning, followed by married women 217 (60.8%), and lowest among the single women 4 (8.5%). None of the 3 (0.0%) widows were using family planning. 2 out 3 of the widow, (217 of 337) aged (20–39 years) were using family planning. However, of the 40 teenagers (15–19) years, only 2 (5%) were using family planning methods. The low utilization of family planning among teenagers could be due to their undecided attitude towards family planning use. Use of family planning methods, however, increased with women’ education level; 50 (58.1%) of Ordinary level and 7 (58.3%) of Advance level were using family planning compared to 19 (39.6%) of women with NO education. These findings agree with a study that showed that less-educated respondents had the highest level of unmet need (5, 6, 12). However, sexual partner’s level of education did not affect the use of contraception; 17 women out of 31 (54.8%), 166 women out of 269 (61.7%), and 31 women out of 57 (54.4%) whose sexual partners had No, Primary, and Ordinary education respectively were using family planning. This finding is not in agreement with a previous study (12). This could be due to women tendency to use family planning is spite of the partners’ disapproval. Our finding showed that 27.9% of married women use family planning is spite of the partners’ disapproval. Contraceptive prevalence rate reduced with number of children who died in less than 5 years of age. This finding agree with a previous study showing that infant mortality was an obstacle to family planning use (9). There was a strong correlation between spousal communication and positive attitude and current use of family planning (P=0.000) (P=0.000) respectively. These findings were in agreement with a Nigerian study (10). Most preferred the Injectaplan 166 (39.2%), implant 111 (26.2%), intrauterine device 36 (8.5%). The most preferred family planning methods by members of FGDs were Injectaplan and implants.
Obstacles to family planning use
This study showed that women had high level of awareness and knowledge about family planning. Therefore, knowledge barrier was not an important obstacle to family planning use among women of rural Northern Uganda. This finding is not in agreement with an Eritrean study which showed that lack of knowledge was a major factor for non-use of contraception among women (18). The high level of awareness and knowledge of family planning in the post conflict Northern Uganda was mainly because of the government policy that family planning services be provided to all women attending antenatal care (19). According to key informants, the development partners were providing free family planning services which was also responsible for the high level of family planning awareness and knowledge. Women stated that they faced the following problems in accessing family planning services; services far away from home 137 (32.3%), husbands 73 (17.2%) and family 21 (5%) forbid them from using family planning services, and services not available 62 (14.6%). According to a key informant, family planning providers’ absenteeism was also an obstacle to family planning use. These findings agree with previous study showing that health care services were far away from many residents of Amuru district and the district was grappling with staff absenteeism (17). Other obstacles to family planning use were; fear of side effects, fear of cost of managing side effects, fear of children dying less than 5 years of age, lack of men’s and community leaders’ participation in family planning programme, the desire for many children which decreased with education level; 44 women (89.6 %) with No education and 97 (35%) with primary education desired 5 or more children compared to only 6 women (7%) with Ordinary level education who desired 5 or more children. This findings agree with a previous report showing that desired number of children among those with primary education was high (5.9 children) compared to those with post primary education (3.8 children) (15). Moreover, desire to have many children is a known obstacle to family planning use (12).
In conclusion, taking services closer to people, reducing number of children dying less than 5 years of age, educating men about family planning, making sure family planning providers and family planning methods are always available, reducing cost of managing side effects and involving community leaders will improve family planning use and thus reduce the rapid population growth and poverty (2).
Figure 1.
Showing age of respondents
Figure 2.
Showing levels of education of respondents.
Table 1.
Showing occupation of the respondents
| Occupation | Number of respondents (N=424) | Percentage (%) |
|---|---|---|
| housewife | 14 | 3.3 |
| farming | 332 | 78.3 |
| personal business | 16 | 3.8 |
| work in private organization | 10 | 2.4 |
| government employee | 8 | 1.9 |
| student | 40 | 9.4 |
| None | 4 | 0.9 |
| Total | 424 | 100 |
Table 2.
Showing composition of key informants
| Code | Composition of Key Informants |
|---|---|
| K11 | Family planning focal person at Atiak Health Centre IV |
| K12 | The In charge of Atiak Health Centre IV |
| K13 | Training and vetting officer Maries Stopes Uganda - Gulu office |
| K14 | Amuru District Assistant District Health Officer In Charge of Maternal and Child Health |
Acknowledgments
This study was A MESAU-MEPI Supported Undergraduate Mentored Research, Awarded through Award Number 1r24tw008886 (MESAU-MEPI Programmatic Award) from the Fogarty International Center 2014. Our utmost appreciation goes to all respondents, the In-charge and Staffs of Atiak Health Centre IV, office of the Amuru District Health Officer, for their support during data collection, Mr. Luryama-Moi Kenneth and Mr. Onen Yagos of faculty of Medicine, Gulu University, for their guidance during our research.
Contributor Information
S. Ouma, Paediatric and Child Health, Head of Department of Paediatric and Child Health, Faculty of Medicine, Gulu University.
M. Turyasima, Paediatric and Child Health, Head of Department of Paediatric and Child Health, Faculty of Medicine, Gulu University.
H. Acca, Paediatric and Child Health, Head of Department of Paediatric and Child Health, Faculty of Medicine, Gulu University.
F. Nabbale, Paediatric and Child Health, Head of Department of Paediatric and Child Health, Faculty of Medicine, Gulu University.
K. O. Obita, Paediatric and Child Health, Head of Department of Paediatric and Child Health, Faculty of Medicine, Gulu University.
M. Rama, Paediatric and Child Health, Head of Department of Paediatric and Child Health, Faculty of Medicine, Gulu University.
C. C. Adong, Paediatric and Child Health, Head of Department of Paediatric and Child Health, Faculty of Medicine, Gulu University.
A. Openy, Paediatric and Child Health, Head of Department of Paediatric and Child Health, Faculty of Medicine, Gulu University.
M. O. Beatrice, Paediatric and Child Health, Head of Department of Paediatric and Child Health, Faculty of Medicine, Gulu University.
E. I. Odongo-Aginya, Head of Microbiology/Immunology, Faculty of Medicine, Gulu University, P.O. BOX 166, Gulu-Uganda.
S. Awor, Department of Reproductive Health, Faculty of Medicine, Gulu University, P.O. BOX 166, Gulu-Uganda.
REFERENCES
- 1.The Daily Monitor. Rich, Poor gaps widens. Kampala: The Daily Monitor; 2013. [19/11/2013]. [Google Scholar]
- 2.Population Secretariat (POPSEC) Ministry of Finance, Planning and Economic Development: Uganda population Report 2012: Uganda at 50 years, population and service Delivery: Challenges, Opportunities and Prospects” Kampala. 2012 [Google Scholar]
- 3.Uganda Demographic and Health Survey, UDHS 2011. Kampala: 2012. Mar, pp. 8–9. [Google Scholar]
- 4.United Nations Children Fund. Country Programme Action plan 2010–2014. Kampala: UNICEF; 2009. (2009) [Google Scholar]
- 5.Klijzing E. Are There Unmet Family Planning Needs in Europe? Family Planning Perspectives. 2000 Mar-Apr;32(2) (2000) [PubMed] [Google Scholar]
- 6.Abdel AA, Amira O. Factors affecting unmet need of family planning in Eastern Sudan. BMC Public Health. 2013:13–102. doi: 10.1186/1471-2458-13-102. (2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khan Shane, Sarah EK, Joy F, Vinod M. Unmet Need and the Demand for Family Planning in Uganda: Further Analysis of the Uganda Demographic and Health Surveys, 1995–2006. Calverton, Maryland, USA: 2008. [Google Scholar]
- 8.Feyisetan BJ. Spousal Communication and Contraceptive Use among the Yoruba of Nigeria. Population Research and Policy Review. 2000;19:29–45. [Google Scholar]
- 9.Kamau RK, Karanja J, Sekadde KC. Barriers to contraceptive use in Kenya. East Afr Med J. 1996;73:651–659. (1996) [PubMed] [Google Scholar]
- 10.Odimegwu OC. Family Planning Attitudes and Use in Nigeria: A Factor Analysis. International. Family Planning Perspectives. 1999 Jun;25(2) (1999) [Google Scholar]
- 11.Maki S. Unmet need for family planning persist in developing countries. Population reference bureau. 2007 Oct [Google Scholar]
- 12.Mukisa SW, James N, Betty K. Does couple discussion influence unmet need for family planning in Uganda? 2011 (2011) [Google Scholar]
- 13.Government of Uganda. Ministry of health, Health sector strategic plan III 2010/11–2014/2015 [Google Scholar]
- 14.Uganda Bureau of Statistics (UBOS) and Macro International Inc. Uganda Demographic and Health Survey-1995. Calverton Maryland, USA: Statistics Department, [Uganda] and Macro International Inc; 1996. [Google Scholar]
- 15.Population Secretariat (POPSEC) Ministry of Finance, Planning and Economic Development: Uganda population Report 2008. Kampala: 2008. [Google Scholar]
- 16.Alkema L, V K. National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysis. The Lancet. 2013;381:1642–1652. doi: 10.1016/S0140-6736(12)62204-1. (2013) [DOI] [PubMed] [Google Scholar]
- 17.Otile OM, Arthur O, Walter A. Local Government Councils’ Performance and Public Service Delivery in Uganda: Amuru District Council Score-Card Report 2011/12.Series No.4. Kampala: ACODE Public Service Delivery and Accountability Report; 2013. (2013) [Google Scholar]
- 18.Gebremariam W, Roderic B. Currently married women with an unmet need for contraception in Eritrea: Profile and determinants. Canadian Studies in population. 2011;38:78. [Google Scholar]
- 19.Government of Uganda, Ministry of health. Kampala: 2010. Jan, Uganda Clinical Guidelines 2010. (2010) [Google Scholar]