Abstract
Purpose
It is well known that old age is a risk factor for postoperative complications. Therefore, this study aimed to explore the risk factors for poor postoperative surgical outcomes in elderly gastric cancer patients.
Materials and Methods
Between January 2006 and December 2015, 247 elderly gastric cancer patients who underwent curative gastrectomy were reviewed. In this study, an elderly patient was defined as a patient aged ≥65 years. All possible variables were used to explore the risk factors for poor early surgical outcomes in elderly gastric cancer patients.
Results
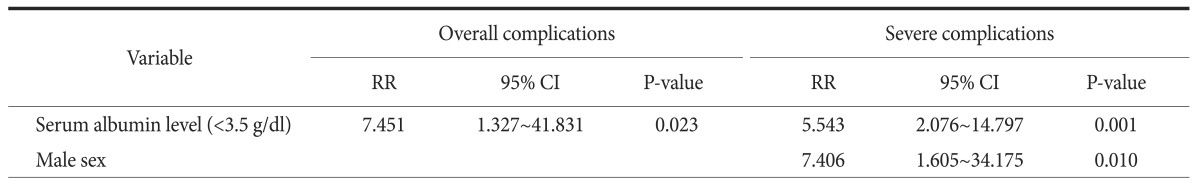
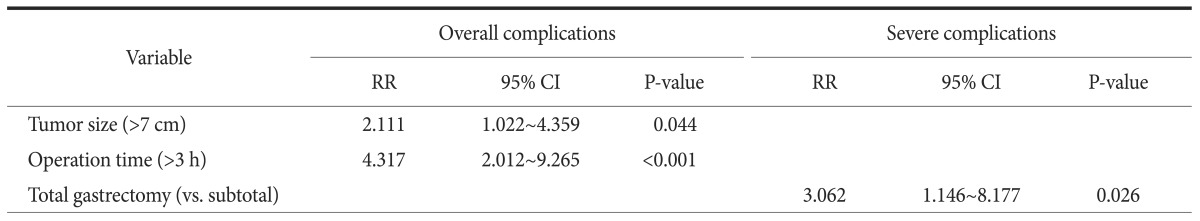
Based on multivariate analyses of preoperative risk factors, preoperative low serum albumin level (<3.5 g/dl) and male sex showed statistical significance in predicting severe postoperative complications. Additionally, in an analysis of surgery-related risk factors, total gastrectomy was a risk factor for severe postoperative complications.
Conclusions
Our study findings suggest that low serum albumin level, male sex, and total gastrectomy could be risk factors of severe postoperative complications in elderly gastric cancer patients. Therefore, surgeons should work carefully in cases of elderly gastric cancer patients with low preoperative serum albumin level and male sex. We believe that efforts should be made to avoid total gastrectomy in elderly gastric cancer patients.
Keywords: Stomach neoplasms, Aged, Risk factors, Postoperative complications
Introduction
As the average life expectancy for elderly persons is increasing dramatically in many parts of the world,1,2 many countries are expected to develop what is known as super-aged societies in the near future. This increase in the elderly population parallels the proportional increase in geriatric patients with cancer.3 Therefore, the average age at cancer diagnosis is also expected to increase in most countries with aging populations. Following this trend, the results of geriatric assessments were introduced to provide information about risk evaluation in the surgical treatment of elderly cancer patients.4,5
The impact of old age on the early surgical outcomes of gastric cancer surgery is controversial. Several studies have suggested that old age is an independent risk factor of postoperative morbidity and mortality due to decreased reserve capacity.6,7 Most elderly patients have multiple morbidities that may lead to severe postoperative complications and mortality. In particular, super-elderly patients (≥75 years of age) have increasing numbers of comorbidities and functional disorders.8,9 Another study documented that having multiple morbidities increases the risk of postoperative complications in patients who undergo elective surgery.10 Therefore, the risk assessment of elderly persons has become an important issue in the field of gastric cancer surgery. Several investigators recently suggested that old age is an important predictive risk factor of gastric cancer surgery.11,12,13
On the other hand, other studies suggested that open gastrectomy can also be safely performed in elderly patients because of improvements in surgical techniques and perioperative management. 14,15 Some recent studies in particular have shown that laparoscopic gastrectomy can be safely performed in elderly patients. 16,17
Therefore, this study planned to explore the risk factors of minimal invasive surgeries such as laparoscopic gastrectomy.
Materials and Methods
1. Patients
We retrospectively reviewed data that were prospectively collected for 247 elderly gastric cancer patients who underwent curative gastrectomy with lymph node dissection between January 2006 and December 2015 at Hanyang University Guri Hospital. In this study, an elderly patient was defined as a patient aged 65 years or older according to World Health Organization guidelines. 18 According to this criterion, some studies showed that elderly patients had poor surgical outcomes including hospital stay length and days of inpatient care.19
2. Surgical techniques
Laparoscopic gastrectomy was performed in elderly gastric cancer patients with serosa-negative and perigastric lymph node metastasis according to preoperative clinical staging results. Clinical staging was determined by preoperative gastrofiberoscopy, computed tomography, and endoscopic ultrasonography. D1 plus beta lymphadenectomy was performed in all gastric cancer patients. In laparoscopic gastrectomy, total omentectomy was performed in patients with advanced gastric cancer. The extent of gastrectomy was dictated based on tumor location.
3. Clinical analysis
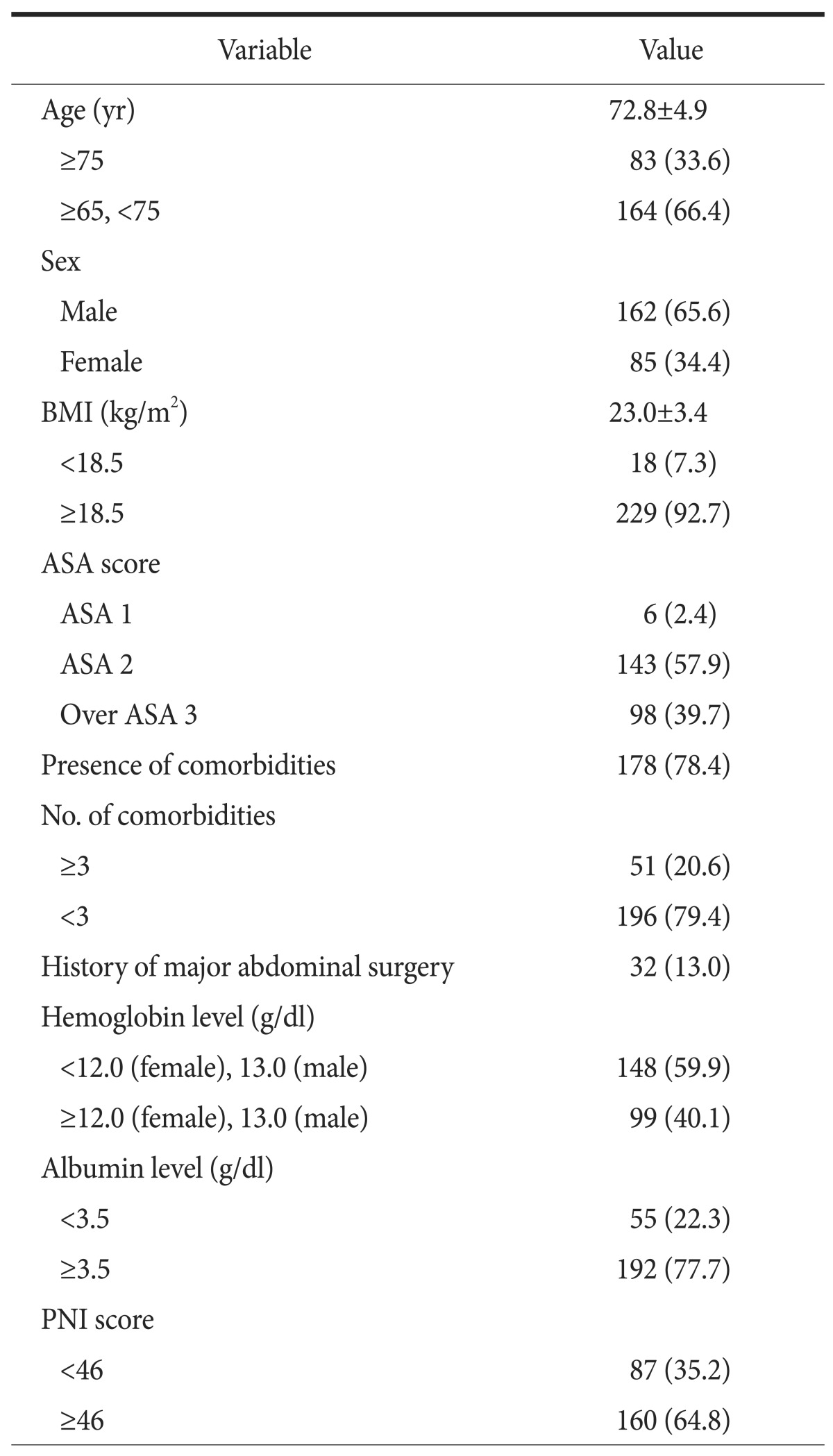
Clinical data obtained from medical records included patient age, sex, body mass index (BMI; kg/m2), American Society of Anesthesiologist (ASA) score, and others (Table 1). The operative characteristics and early surgical outcomes reviewed included operation method (laparoscopic vs. open surgery), extent of gastrectomy (total vs. subtotal gastrectomy), omentectomy (total vs. partial), combined resection of other organs, operation time, postoperative complications, postoperative mortality, and length of postoperative hospital stay. Pathologic results were analyzed for tumor size, number of retrieved lymph nodes, and 7th American Joint Committee on Cancer staging system score.20
Table 1. Clinical characteristics of elderly patients who underwent gastrectomy.
Values are presented as mean±standard deviation or number (%). BMI = body mass index; ASA = American Society of Anesthesiologists; PNI = Prognostic Nutritional Index.
The classification of underweight was defined as a BMI<18.5 kg/m2. The ASA classification was determined by anesthesiologists 1 day before the surgery. The preoperative serum albumin and hemoglobin levels were measured when the patient was admitted to the hospital. Hypoalbuminemia was defined as serum albumin levels below the normal range (<3.5 g/dl). The Prognostic Nutrition Index (PNI) was used as risk factor of postoperative complication.21,22 Anemia was defined as a decreased hemoglobin level (female<12.0; male<13.0 g/dl).
Postoperative complications were defined as any condition requiring conservative or surgical treatment. Severe postoperative complications were defined as those that required management by an endoscopic or interventional procedure or re-operation (expanded classification>level 3).23 Thirty-day mortality was used for postoperative mortality and defined as death within 30 days of surgery.
In this study, a soft diet was started when patients felt comfortable enough to consume a liquid diet twice at consecutive meal times. Patients were discharged if they had no problems eating a soft diet, showed an absence of inflammatory conditions including leukocytosis, unstable vital signs, or abrupt-onset abdominal pain, and if they were generally comfortable. The final decision regarding discharge was left up to each patient.
4. Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics ver. 21 (IBM Co., Armonk, NY, USA). All values are expressed as means±standard deviation. Categorical variables were analyzed using the chi-square test and all continuous variables were analyzed with Student's t-test depending on the data. A multivariate analysis was performed to identify risk factors associated with early surgical outcomes. Factors with relatively small Pvalues (P<0.1) on univariate analysis were selected as variables for multivariate analysis. A multivariate analysis was performed using multiple logistic regression analysis. Hazard ratios with 95% confidence intervals were estimated for each variable in the multivariate analysis. A P-value <0.05 was considered statistically significant.
Results
1. Clinical characteristics
The clinical characteristics of the 247 patients are shown in Table 1. The mean patient age was 72.8 years. Eighty-three patients (33.6%) were 75 years of age or older. Men outnumbered women in this study population. The majority of patients (78.4%) had one or more comorbid conditions, while 51 patients had three or more comorbidities. Anemia was seen in 148 patients (59.9%). A low serum albumin level was measured in 55 patients (22.3%). A low PNI score was seen in 87 patients.
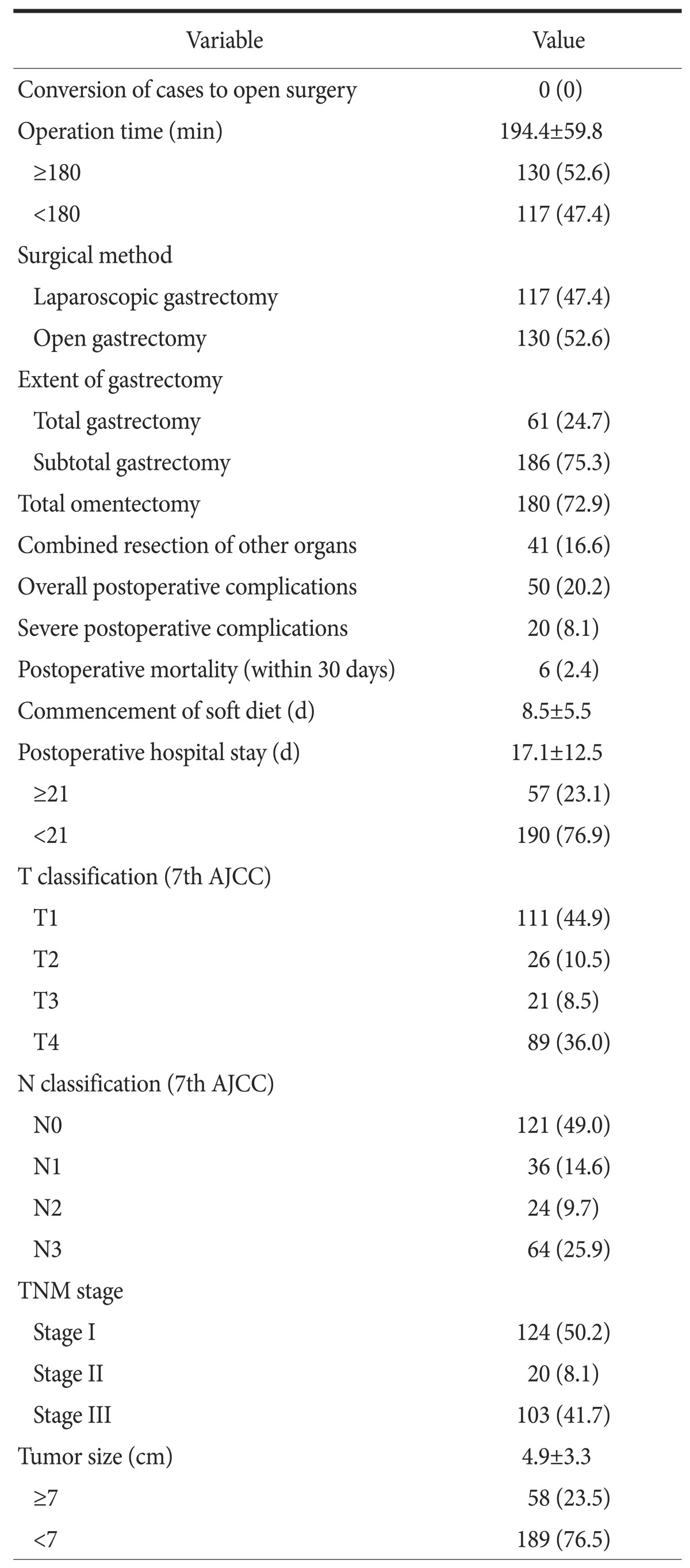
2. Surgery-related characteristics
Table 2 shows the early surgical outcomes and pathologic results of elderly gastric cancer patients. None of these patients required conversion to open surgery. The mean operation time was 194.4 minutes. A little more than half of the operations (52.6%) lasted longer than 3 hours. Laparoscopic gastrectomy was performed in 117 patients (47.4%). The percentage of patients who underwent total gastrectomy was 24.7%. Forty-one patients (16.6%) underwent combined resection of another organ. Postoperative complications occurred in 50 patients (20.2%). A total of 20 patients (8.1%) experienced severe postoperative complications. Postoperative mortality occurred in six patients (2.4%). The mean postoperative hospital stay was 17.1 days. Fifty-seven patients (23.1%) were hospitalized for >3 weeks after their operations. One hundred and eleven patients had early gastric cancer. Negative lymph node metastasis occurred in 121 patients. Fifty-eight patients had large tumors (≥7 cm).
Table 2. Surgery-related characteristics of elderly patients who underwent gastrectomy.
Values are presented as number (%) or mean±standard deviation. AJCC = American Joint Committee on Cancer; TNM = tumor, node, metastasis.
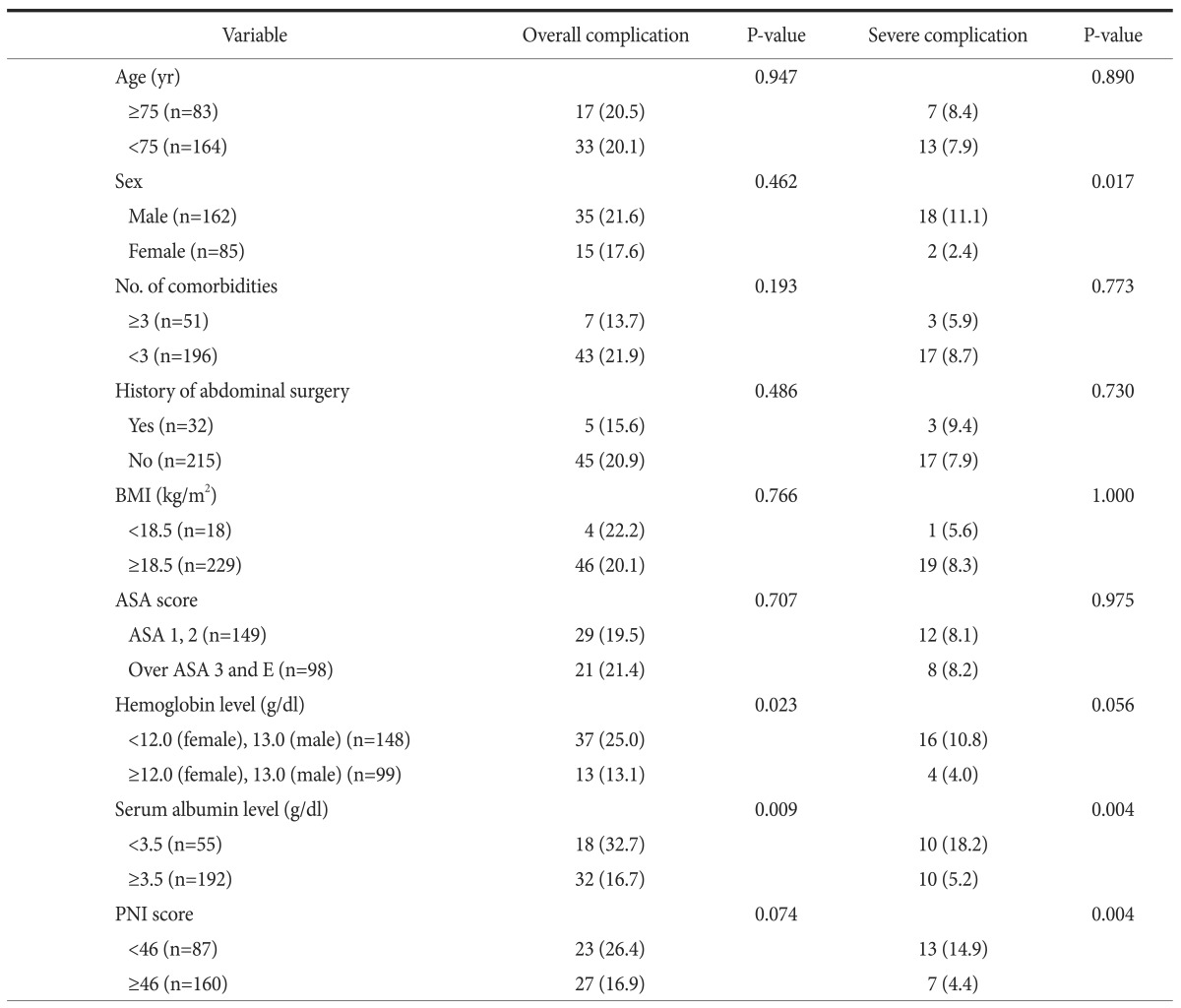
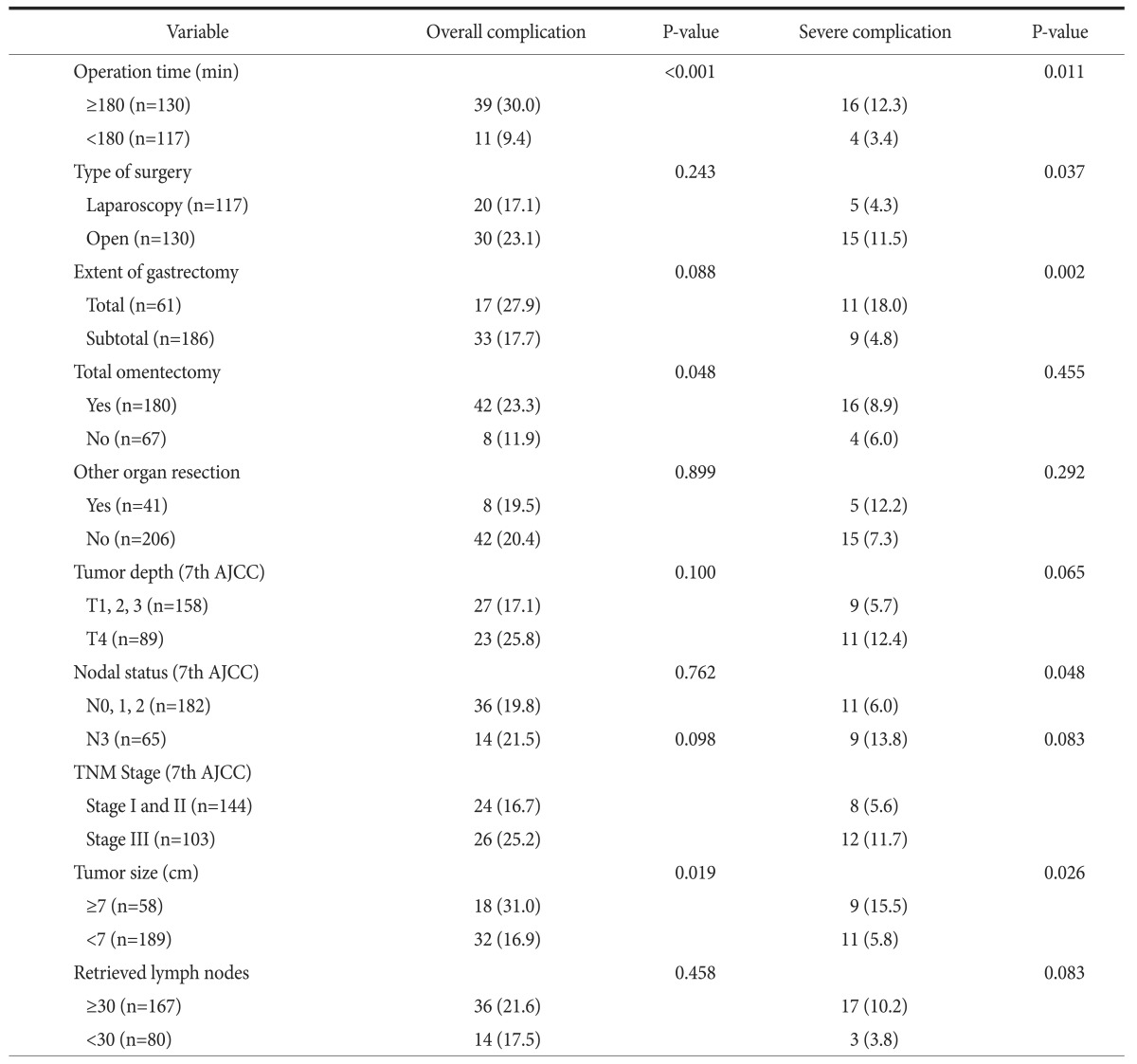
3. Univariate analyses of risk factors for early surgical outcomes
Table 3 and 4 list the risk factors for early surgical outcomes. More patients who developed overall postoperative complications were found in the anemia, low serum albumin level, long operation time, total omentectomy, and large size tumor groups. Severe postoperative complications were significantly different in the male sex, low serum albumin level, low PNI score, long operation time, total gastrectomy, N3 stage, and large size tumor groups.
Table 3. Univariate analysis of preoperative risk factors for early surgical outcomes.
Values are presented as number (%). BMI = body mass index; ASA = American Society of Anesthesiologists; E = emergency; PNI = Prognostic Nutritional Index.
Table 4. Univariate analysis of surgery-related risk factors for early surgical outcomes.
Values are presented as number (%). AJCC = American Joint Committee on Cancer; TNM = tumor, node, metastasis.
4. Multivariate analyses of risk factors for early surgical outcomes
Table 5 shows the preoperative risk factors. Low serum albumin level was an overall risk factor (odds ratio [OR], 7.451; 95% confidence interval [CI], 1.327~41.831; P=0.023) and severe postoperative complications (OR, 5.543; 95% CI, 2.076~14.797; P=0.001) of elderly gastric cancer patients.
Table 5. Multivariate analysis of preoperative risk factors for early surgical outcomes.
RR = relative risk; CI = confidence interval.
In surgery-related risk factors, large tumor size (>7 cm; OR, 2.111; 95% CI, 1.022~4.359; P=0.044) and long operation time (>3 hours; OR, 4.317; 95% CI, 2.012~9.265; P<0.001) were risk factors of overall postoperative complications, while total gastrectomy (OR, 3.062; 95% CI, 1.146~8.177; P=0.026) was a risk factor of severe postoperative complications (Table 6).
Table 6. Multivariate analysis of surgery-related risk factors for early surgical outcomes.
RR = relative risk; CI = confidence interval.
Discussion
Biological age is a key factor in determining surgical success. Consequently, a comprehensive geriatric assessment was recently instituted to assess the components of an elderly person's physical, mental, and social status.4,5 However, determining how this overarching method should be applied in practice for surgical patients remains challenging.24 Furthermore, there has been no consensus with respect to the best tool for predicting postoperative outcomes.25,26
Our multivariate analyses showed that three variables (serum albumin level, sex, and extent of gastrectomy) can be risk factors for poor early surgical outcomes in elderly gastric cancer patients. In particular, our study showed that elderly age (≥75 years) is not a significant risk factor for early surgical outcomes of conventional gastric cancer surgery.
Several authors have reported that postoperative mortality rates are higher in elderly patients because of pre-existing comorbidities.14,27 Meanwhile, recent studies have suggested that elderly gastric cancer patients can be safely operated on using improved surgical techniques and perioperative management.14,15,16,17 Our study also obtained a similar result in that we found no difference in early surgical outcomes between elderly patients aged ≥65 years and those ≥75 years. Despite this, we are not arguing that old age is not a risk factor for early surgical outcomes of gastric cancer. We previously reported that early surgical outcomes of totally laparoscopic distal gastrectomy were also affected by old age.28
It is well known that low preoperative serum albumin is a strong predictor of postoperative morbidity and mortality.29,30 Our study also showed that hypoalbuminemia can be an independent risk factor of postoperative complications. The important thing to note is that initial hypoalbuminemia can affect early surgical outcomes irrespective of the replacement of albumin. It is assumed that initial hypoalbuminemia reflects a state of malnutrition. Therefore, this serum albumin test could be a reasonably simple and cost-effective method for identifying at-risk patients. On the other hand, our study did not show the significance of PNI as a predictive risk factor for early surgical outcomes.
Several recent studies have suggested that male sex is a risk factor of postoperative complication in bowel surgery.31,32,33 In particular, our results showed that male sex is an independent risk factor for severe postoperative complications in multivariate analysis.
Total gastrectomy is a known risk factor of postoperative complications.33,34 One report stated that total gastrectomy should be performed in patients >80 years of age only if absolutely necessary.35 Our multivariate analysis also showed that total gastrectomy is an independent risk factor of severe postoperative complication in elderly gastric cancer patients.
This study had several limitations. First, it was a retrospective study with possible selection bias. Second, only a small number of patients had severe postoperative complications. Therefore, further large randomized controlled trials are needed to evaluate the risk factors.
In clinical practice, most surgeons believe that, based on their experience, they can predict the physiological reserve of an elderly person who plans to undergo cancer surgery. On the other hand, most surgeons are aware that their methods for determining this status are fairly subjective. As a result, some elderly persons miss the opportunity to undergo surgery. In contrast, the overestimation of patient reserve can also lead to postoperative death. Therefore, despite the study limitations, we believe that our identification of poor risk factors will help physicians predict postoperative surgical outcomes in elderly gastric cancer patients.
In summary, we found that the poor risk factors for early surgical outcomes of gastric cancer surgery in elderly patients included low serum albumin level, male sex, and total gastrectomy. In particular, we suggest that surgeons should operate carefully in elderly male patients with gastric cancer as well as in those with low serum albumin levels to decrease severe postoperative complications. We believe that efforts should be made to avoid total gastrectomy in elderly gastric cancer patients.
Footnotes
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.McKenna RJ., Sr Clinical aspects of cancer in the elderly. Treatment decisions, treatment choices, and follow-up. Cancer. 1994;74(7 Suppl):2107–2117. doi: 10.1002/1097-0142(19941001)74:7+<2107::aid-cncr2820741719>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) World health statistics 2014 [Internet] Geneva: WHO; 2014. [cited 2014 May]. Available from: http://www.who.int/gho/publications/world_health_statistics/2014/en/ [Google Scholar]
- 3.Yancik R, Ries LA. Aging and cancer in America. Demographic and epidemiologic perspectives. Hematol Oncol Clin North Am. 2000;14:17–23. doi: 10.1016/s0889-8588(05)70275-6. [DOI] [PubMed] [Google Scholar]
- 4.Balducci L, Extermann M. Management of cancer in the older person: a practical approach. Oncologist. 2000;5:224–237. doi: 10.1634/theoncologist.5-3-224. [DOI] [PubMed] [Google Scholar]
- 5.Feng MA, McMillan DT, Crowell K, Muss H, Nielsen ME, Smith AB. Geriatric assessment in surgical oncology: a systematic review. J Surg Res. 2015;193:265–272. doi: 10.1016/j.jss.2014.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Polanczyk CA, Marcantonio E, Goldman L, Rohde LE, Orav J, Mangione CM, et al. Impact of age on perioperative complications and length of stay in patients undergoing noncardiac surgery. Ann Intern Med. 2001;134:637–643. doi: 10.7326/0003-4819-134-8-200104170-00008. [DOI] [PubMed] [Google Scholar]
- 7.Evers BM, Townsend CM, Jr, Thompson JC. Organ physiology of aging. Surg Clin North Am. 1994;74:23–39. doi: 10.1016/s0039-6109(16)46226-2. [DOI] [PubMed] [Google Scholar]
- 8.Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83. doi: 10.1093/epirev/mxs009. [DOI] [PubMed] [Google Scholar]
- 9.From the centers for disease control and prevention. Public health and aging: trends in aging: United States and worldwide. JAMA. 2003;289:1371–1373. [PubMed] [Google Scholar]
- 10.Kim KI, Park KH, Koo KH, Han HS, Kim CH. Comprehensive geriatric assessment can predict postoperative morbidity and mortality in elderly patients undergoing elective surgery. Arch Gerontol Geriatr. 2013;56:507–512. doi: 10.1016/j.archger.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Seo SH, Hur H, An CW, Yi X, Kim JY, Han SU, et al. Operative risk factors in gastric cancer surgery for elderly patients. J Gastric Cancer. 2011;11:116–121. doi: 10.5230/jgc.2011.11.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Otsuji E, Fujiyama J, Takagi T, Ito T, Kuriu Y, Toma A, et al. Results of total gastrectomy with extended lymphadenectomy for gastric cancer in elderly patients. J Surg Oncol. 2005;91:232–236. doi: 10.1002/jso.20330. [DOI] [PubMed] [Google Scholar]
- 13.Kitamura K, Yamaguchi T, Taniguchi H, Hagiwara A, Yamane T, Sawai K, et al. Clinicopathological characteristics of gastric cancer in the elderly. Br J Cancer. 1996;73:798–802. doi: 10.1038/bjc.1996.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gretschel S, Estevez-Schwarz L, Hunerbein M, Schneider U, Schlag PM. Gastric cancer surgery in elderly patients. World J Surg. 2006;30:1468–1474. doi: 10.1007/s00268-005-0633-5. [DOI] [PubMed] [Google Scholar]
- 15.Kunisaki C, Akiyama H, Nomura M, Matsuda G, Otsuka Y, Ono HA, et al. Comparison of surgical outcomes of gastric cancer in elderly and middle-aged patients. Am J Surg. 2006;191:216–224. doi: 10.1016/j.amjsurg.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Mohri Y, Yasuda H, Ohi M, Tanaka K, Saigusa S, Okigami M. Short- and long-term outcomes of laparoscopic gastrectomy in elderly patients with gastric cancer. Surg Endosc. 2015;29:1627–1635. doi: 10.1007/s00464-014-3856-4. [DOI] [PubMed] [Google Scholar]
- 17.Kunisaki C, Makino H, Takagawa R, Oshima T, Nagano Y, Ono HA, et al. Efficacy of laparoscopy-assisted distal gastrectomy for gastric cancer in the elderly. Surg Endosc. 2009;23:377–383. doi: 10.1007/s00464-008-9949-1. [DOI] [PubMed] [Google Scholar]
- 18.Statistics Korea. Korean Statistical Information Service [Internet] Daejeon: Statistics Korea; [cited 2011 May 1]. Available from: http://kosis.kr/ [Google Scholar]
- 19.Popovic JR. 1999 National hospital discharge survey: annual summary with detailed diagnosis and procedure data. Vital Health Stat 13. 2001:1–206. doi: 10.1037/e309042005-001. [DOI] [PubMed] [Google Scholar]
- 20.Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol. 2010;17:3077–3079. doi: 10.1245/s10434-010-1362-z. [DOI] [PubMed] [Google Scholar]
- 21.Jiang N, Deng JY, Ding XW, Ke B, Liu N, Zhang RP, et al. Prognostic nutritional index predicts postoperative complications and long-term outcomes of gastric cancer. World J Gastroenterol. 2014;20:10537–10544. doi: 10.3748/wjg.v20.i30.10537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984;85:1001–1005. [PubMed] [Google Scholar]
- 23.Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009;250:177–186. doi: 10.1097/SLA.0b013e3181afde41. [DOI] [PubMed] [Google Scholar]
- 24.Kothari A, Phillips S, Bretl T, Block K, Weigel T. Components of geriatric assessments predict thoracic surgery outcomes. J Surg Res. 2011;166:5–13. doi: 10.1016/j.jss.2010.05.050. [DOI] [PubMed] [Google Scholar]
- 25.Puts MT, Hardt J, Monette J, Girre V, Springall E, Alibhai SM. Use of geriatric assessment for older adults in the oncology setting: a systematic review. J Natl Cancer Inst. 2012;104:1133–1163. doi: 10.1093/jnci/djs285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamaker ME, Jonker JM, de Rooij SE, Vos AG, Smorenburg CH, van Munster BC. Frailty screening methods for predicting outcome of a comprehensive geriatric assessment in elderly patients with cancer: a systematic review. Lancet Oncol. 2012;13:e437–e444. doi: 10.1016/S1470-2045(12)70259-0. [DOI] [PubMed] [Google Scholar]
- 27.Wu CW, Lo SS, Shen KH, Hsieh MC, Lui WY, P'Eng FK. Surgical mortality, survival, and quality of life after resection for gastric cancer in the elderly. World J Surg. 2000;24:465–472. doi: 10.1007/s002689910074. [DOI] [PubMed] [Google Scholar]
- 28.Kim MG, Kim HS, Kim BS, Kwon SJ. The impact of old age on surgical outcomes of totally laparoscopic gastrectomy for gastric cancer. Surg Endosc. 2013;27:3990–3997. doi: 10.1007/s00464-013-3073-6. [DOI] [PubMed] [Google Scholar]
- 29.Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF. Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg. 1999;134:36–42. doi: 10.1001/archsurg.134.1.36. [DOI] [PubMed] [Google Scholar]
- 30.Moghadamyeghaneh Z, Hwang G, Hanna MH, Phelan MJ, Carmichael JC, Mills SD, et al. Even modest hypoalbuminemia affects outcomes of colorectal surgery patients. Am J Surg. 2015;210:276–284. doi: 10.1016/j.amjsurg.2014.12.038. [DOI] [PubMed] [Google Scholar]
- 31.Kirchhoff P, Dincler S, Buchmann P. A multivariate analysis of potential risk factors for intra- and postoperative complications in 1316 elective laparoscopic colorectal procedures. Ann Surg. 2008;248:259–265. doi: 10.1097/SLA.0b013e31817bbe3a. [DOI] [PubMed] [Google Scholar]
- 32.Lipska MA, Bissett IP, Parry BR, Merrie AE. Anastomotic leakage after lower gastrointestinal anastomosis: men are at a higher risk. ANZ J Surg. 2006;76:579–585. doi: 10.1111/j.1445-2197.2006.03780.x. [DOI] [PubMed] [Google Scholar]
- 33.Sasako M. Risk factors for surgical treatment in the Dutch Gastric Cancer Trial. Br J Surg. 1997;84:1567–1571. doi: 10.1111/j.1365-2168.1997.02842.x. [DOI] [PubMed] [Google Scholar]
- 34.Launois B, Cardin JL, Bardaxoglou E, Bourdonnec P, de Chateaubriant P, Buard JL, et al. Management of cancer of the stomach: total gastrectomy versus sub-total gastrectomy. Hepatogastroenterology. 1991;38:45–52. [PubMed] [Google Scholar]
- 35.Korenaga D, Moriguchi S, Baba H, Kakeji Y, Orita H, Haraguchi M, et al. Surgery for gastric carcinoma is feasible for patients over 80 years of age. World J Surg. 1991;15:642–647. doi: 10.1007/BF01789215. [DOI] [PubMed] [Google Scholar]