Abstract
Objective
Vigorous physical activity (PA) has been promoted for improving cardiorespiratory fitness (CRF). However, therapeutic techniques designed to engage participants in vigorous PA have fallen short; one reason for this may be the unpleasant physical sensations associated with vigorous exercise (e.g., temporary shortness of breath and mild muscle soreness). Mindfulness and acceptance-based therapies such as Acceptance and Commitment Therapy (ACT) may be helpful at improving adherence to vigorous PA levels. In this open clinical trial, we sought to demonstrate the feasibility and acceptability of a mindfulness- and acceptance-based intervention for increasing CRF in sedentary adults and to generate initial outcomes data.
Design
Participants (N=24) engaged in a 10-week fitness walking program while attending regular group sessions based on ACT.
Main outcome measures and results
The feasibility and acceptability of the intervention were demonstrated through high levels of walking adherence (89.30%) and group session attendance (85.50%). A large significant decrease in total 1-mile walk test time [t(18)=4.61, p=.0002, d=.64] and a moderate significant increase in estimated VO2max [t(18)=−4.05, p=.0007, d=−.43] were observed. Analyses indicated a large significant increase in exercise-related experiential acceptance [t(18)=−9.19, p <.0001, d=−2.09].
Conclusion
This study demonstrates the feasibility and acceptability of an ACT-based intervention for supporting participation in vigorous PA in sedentary individuals.
Keywords: Cardiorespiratory fitness, Mindfulness, Acceptance and commitment therapy, Physical activity, Sedentary
1. Introduction
Increasing physical activity (PA) has long been supported as an important behavior change for health improvement. Vigorous PA, in particular, has been promoted for improving cardiorespiratory fitness (CRF), which has a strong inverse relationship with premature morbidity and mortality in adults (Lee et al., 2011; Williams & Thompson, 2013). Further epidemiological research has shown that vigorous PA has greater health benefits, in terms of blood pressure and glucose control, than moderate-intensity PA (Swain & Franklin, 2006). In addition, it has been found that vigorous PA produces greater cardioprotective benefits, including decreased risk for coronary heart disease, while lower intensity PA is associated with minimal risk reduction (Lee et al., 2011; Lee, Sesso, Oguma, & Paffenbarger, 2003; Sesso, Paffenbarger, & Lee, 2000; Tanasescu et al., 2002). However, the dose–response curve between CRF levels and risk reduction has not shown an evenly graded relationship. The largest risk reduction occurs in individuals moving from the lowest to the second-lowest fitness category, suggesting that public health efforts should focus on the most sedentary individuals (Blair et al., 1989; Blair, & Church, 2003; Kodama et al., 2009; Lee et al., 2011; Myers et al., 2002, 2004).
1.1. CRF and PA
Although the greatest health gains are made through vigorous PA, many fitness and PA trials prescribe moderate-intensity exercise programs, perhaps because they expect to observe difficulties in adherence to high-intensity regimens (Duncan et al., 2005; Swain & Franklin, 2006). The affective response to varying exercise intensity levels has been investigated to elucidate these differences in adherence rates. Ekkekakis (2003) purported, in his Dual Mode Model, that affective responses to exercise are impacted by both cognitive factors (e.g., self-efficacy) and interoceptive cues (e.g., muscular or respiratory). Furthermore, while intensity may not influence affective response from pre- to post-exercise, affective responses during exercise are likely to become more negative as the intensity increases, possibly impacting adherence (Ekkekakis, Hall, & Petruzello, 2008).
Cognitive-behavioral therapies (CBTs) widely used in fitness and PA trials (e.g., Duncan et al., 2005; Dunn et al., 1999) often seek to modify cognitions and affective responses to internal sensations during PA by controlling, restructuring, or eliminating negative thoughts, with the goal of promoting behavioral engagement. For example, restructuring a negative self-statement such as “I am a failure at exercising” into a positive self-statement like “I am proud of myself for trying to exercise” can impact an individual’s motivation as well as their self-efficacy to engage in PA behaviors. However, these trials have yielded only modest improvements of about 1/2 metabolic equivalent (MET)3 or less (a disease risk reduction goal is 1–2 METs) (Blair et al., 1989; Lee et al., 2011) and highlight the difficulty of having individuals maintain even moderate-intensity PA (Church, Earnest, Skinner, & Blair, 2007; Duncan et al., 2005; Dunn et al., 1999).
1.2. Contextual CBTs
Acceptance and Commitment Therapy (ACT) (Hayes, Strosahl, & Wilson, 1999) is part of a larger class of therapeutic approaches known as “contextual CBTs” (Hayes, Luoma, Bond, Masuda, and Lillis, 2006; Hayes et al., 2011). This label is derived from their focus on the context or function of a problematic cognition or emotion rather than its content, form, or frequency. The overarching goal of ACT is to produce greater psychological flexibility, decreasing experiential avoidance of negative internal events (Hayes et al., 2006). Psychological flexibility can be thought of as the ability to accept the presence of unwanted sensations, thoughts, or feelings in the present moment and to act in a values-based fashion (Hayes, 2004; Lillis, Hayes, Bunting, & Masuda, 2009). Experiential avoidance, in the ACT paradigm, refers to the tendency of humans to avoid or escape negative internal experiences (Hayes, Stroshal, & Wilson, 1999; Hayes, 2004); attempts to fix, alter, or restructure these unwanted private experiences can distract individuals from a values-based behavioral path.
There are six core processes that facilitate psychological flexibility in the ACT model: values, committed action, acceptance, cognitive defusion, present-moment contact, and self-as-context. The process of acceptance is defined as a willingness to experience uncomfortable or even painful internal events (e.g., thoughts, feelings, sensations, and memories) without engaging in avoidance or change strategies for the sake of valued living (Hayes et al., 1999; Hayes, 2004). Cognitive defusion refers to the process through which one creates a distance or “space” between themselves and their thoughts, so that one may hold thoughts lightly and increase their behavioral repertoire (Hayes et al., 1999; Hayes, 2004). Self-as-context refers to “the self being a perspective from which thoughts, feelings, and experiences are observed, without judgment, as they pass through the context of the self (Hayes et al., 2006). The primary goal of ACT is to help an individual engage in mindful, values-based living. Values are persistent, may be enacted on an ongoing basis, and have a global quality, uniting various patterns of action (Hayes et al., 1999). Once values have been clarified, committed actions designed to achieve values-based goals are carried out as mindful, purposeful behaviors (Hayes et al., 1999; Hayes, 2004).
1.3. Contextual CBTs as applied to PA
A considerable amount of research exists regarding the efficacy of contextual CBTs in the area of mental health (Hayes, Villatte, Levin, & Hildebrandt, 2011; Ruiz, 2012), and empirical support is growing for their application to behavioral medicine, including issues such as chronic pain (McCracken, MacKichan, & Eccleston, 2007; Vowles & McCracken, 2008), type 2 diabetes management (Gregg, Callaghan, Hayes, & Glenn-Lawson, 2007), smoking cessation (Bricker, Wyszynski, Comstock, & Heffner, 2013; Gifford et al., 2004), epilepsy (Lundgren, Dahl, Melin, & Kies, 2006), obesity (Lillis et al., 2009), weight management (Forman, Butryn, Hoffman, & Herbert, 2009; Tapper et al., 2009), and PA (Butryn, Forman, Hoffman, Shaw, & Juarascio, 2011). These ACT-based promotions of health-related behavior change suggest that this mindfulness and acceptance-based approach may be uniquely suited for interventions in behavioral medicine (Gregg et al., 2007; Lillis et al., 2009; Tapper et al., 2009).
Promising findings from recent randomized controlled trials of ACT-based interventions for weight loss and PA-directed behaviors include a significant effect of a mindfulness-based weight loss intervention on PA (Tapper et al., 2009) and a significant impact of a brief ACT-based intervention on increasing gym visits among college students (Butryn et al., 2011). Recently, Moffitt and Mohr (2015) trial of a self-managed ACT-based intervention DVD for PA showed significant increases in post-intervention PA levels. However, one limitation of these trials was the use of self-reported measures for PA or proxy behaviors (e.g., entering the university gym), which are often inaccurate and do not allow for the interpretation of objective changes in participants’ health status (Dhurandhar et al., 2014; Helmerhorst, Brage, Warren, Besson, & Ekelund, 2012; Prince et al., 2008; Sloane, Snyder, Demark-Wahnefried, Lobach, & Kraus, 2009). The use of objective measures for PA and disease risk is an important next step in moving physical health research forward (Dhurandhar et al., 2014).
1.4. Current study
One reason that other therapeutic techniques have fallen short in engaging participants in vigorous PA may be the unpleasant physical sensations associated with vigorous exercise (e.g., temporary shortness of breath and mild muscle soreness). Mindfulness and acceptance-based therapies such as ACT may be particularly helpful in this regard, as these techniques have proven effective in fostering psychological flexibility towards negative internal events and health-related behavior change (Ruiz, 2010).
In this open trial, we determined the feasibility and acceptability of a manualized group intervention to promote adherence to an assigned fitness walking intervention for CRF in sedentary individuals. While the use of psychotherapeutic approaches for PA is not new, previous studies have often used techniques of cognitive change and control. This study is novel in that it used mindfulness- and acceptance-based techniques to address the potentially aversive aspects of PA. The findings of this study will support the feasibility and acceptability of this type of therapeutic intervention for PA and provide initial data for future studies to build on regarding the efficacy of this approach.
2. Methods
2.1. Study design and participants
This study was approved by the institutional review board at the participating institution. Participants were recruited through local advertising (print and electronic) and completed a telephone screening for initial eligibility. Eligible participants were adults who were classified as sedentary, as defined by the American College of Sports Medicine (ACSM) (i.e., <30 min of moderate PA 5 days per week or <20 min of vigorous PA 3 days per week; American College of Sports Medicine (2013)), for the preceding year on the basis of self-report and a fitness assessment (the Rockport 1-mile walk test). To ensure participant safety, the exclusion criteria included (a) a body mass index (BMI) below 18.5 or above 39; (b) current smoker; (c) a diagnosis of a cardiovascular, pulmonary, or metabolic disease; and (d) a physical condition that restricted the individual’s ability to engage in vigorous walking or a “high-risk” status, as defined by the ACSM guidelines (2013).
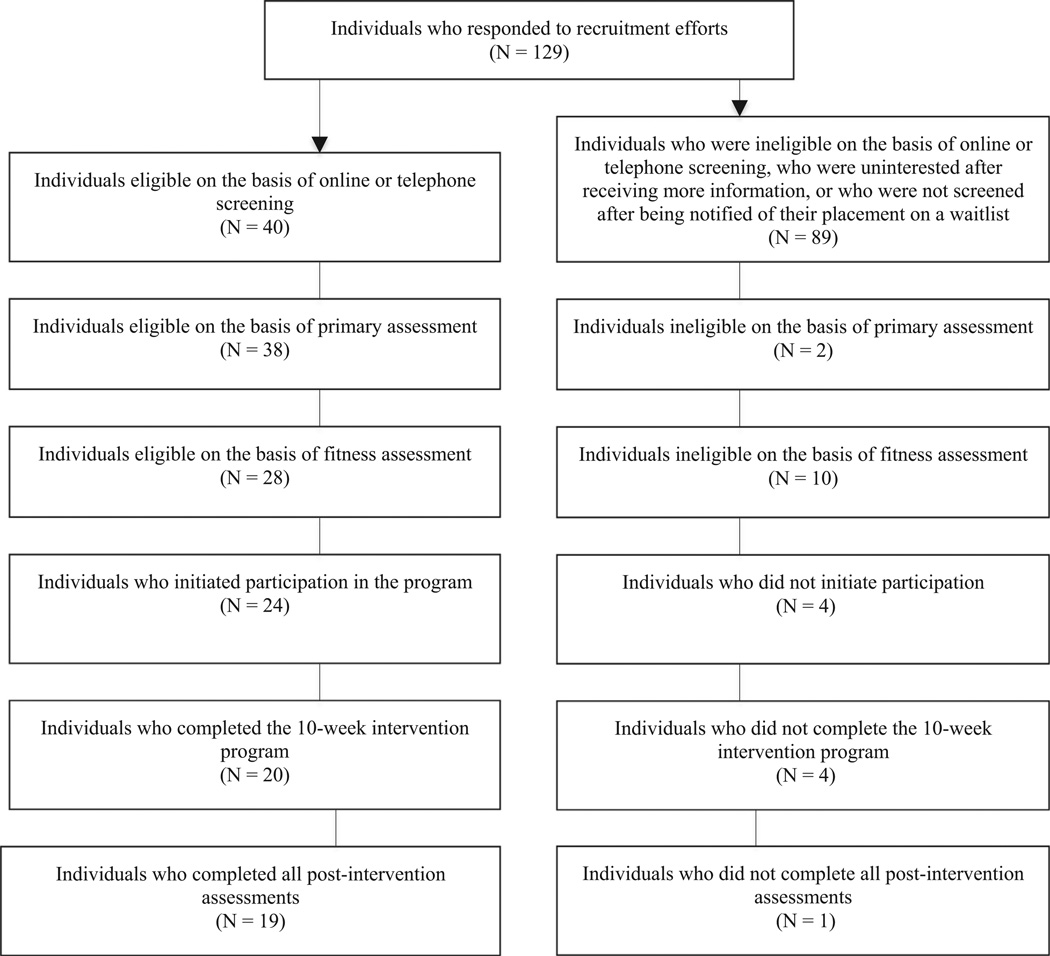
As shown in the Consort diagram (see Fig. 1), 129 individuals responded to the recruitment efforts. Thirty-eight of those individuals chose not to undergo telephone screening after receiving more information regarding the study, 46 underwent telephone screening, and 45 were placed on a waitlist after the recruitment capacity had been reached. After an initial telephone screening, 40 individuals were identified as eligible. These participants attended an in-person assessment, during which paper-and-pencil measures were administered and weight and height were measured. Thirty-eight individuals were deemed eligible on the basis of the in-person assessment and underwent a final fitness assessment (the Rockport 1-mile walk test, described below) to ensure that their fitness levels met the inclusion criteria. Twenty-eight individuals were eligible following the baseline fitness assessment and were randomly assigned to one of four group sessions times, all of which occurred on different weeknights and included five to eight participants. Twenty-four participants initiated the 10-week intervention program, and 19 completed it. The final completers sample had a mean age of 50.47 years; they were mostly female (79%) and white (90%). Their mean weight was 81.45 kg, with a mean BMI of 29.02. Additional data regarding participant demographics can be found in Table 1.
Fig. 1.
Consort diagram.
Table 1.
Demographics of patients who completed the intervention.
| Characteristic | Data (N = 19) |
|---|---|
| Age, years | 50.47 (SD = 10.92) |
| Sex, n | |
| Female | 15 |
| Male | 4 |
| Weight (kg) | 81.45 (SD = 19.14) |
| BMI (kg/m2) | 29.02 (SD = 4.28) |
| Marital status, n | |
| Married | 17 |
| Single | 1 |
| Divorced | 1 |
| Ethnicity, n | |
| Caucasian | 17 |
| Asian-American or Pacific Islander | 1 |
| Latino | 1 |
| Education, n | |
| High school | 2 |
| Some college | 4 |
| 4-year college | 6 |
| Masters degree | 6 |
| Post-masters | 1 |
| Income ($), n | |
| 10,001–20,000 | 1 |
| 20,001–30,000 | 0 |
| 30,001–40,000 | 0 |
| 40,001–50,000 | 1 |
| 50,001–60,000 | 2 |
| 60,001–70,000 | 1 |
| 70,001–80,000 | 2 |
| 80,001–90,000 | 10 |
| N/A | 2 |
2.1.1. Group therapy intervention
The mindfulness- and acceptance-based group intervention included eight 90-min sessions over 10 weeks. Sessions were held at a community-based, university-affiliated mental health clinic. The intervention was delivered according to a manual developed by the first two authors and underwent expert review. This manual employed key concepts, metaphors, and exercises commonly used in ACT that had been adapted to promote the adoption, adherence, and maintenance of a fitness walking program (see Table 2). Specifically related to the core processes of ACT, participants in the current study were instructed on skills that could facilitate the acceptance of negative feelings about exercise as well as the unpleasant physical sensations experienced while performing PA. In addition, participants were given several strategies to assist them in defusing from judgments about the state of their health or their perceived ability to participate in PA. Present-moment contact was discussed as an alternative to the experiential avoidance often associated with PA among individuals with low fitness levels. Related to self-as-context, participants in the study were encouraged to practice mindful, ongoing awareness of transient internal experiences, especially physical discomfort or unpleasant thoughts, and to notice that they were able to observe these transient experiences from the perspective of the self without being defined by them. Values were discussed regularly in several sessions, including the values that led participants to join the group and to persist in participation. Participants were encouraged to consider whether fitness was a value in and of itself or in the service of another value (e.g., longevity for the sake of family). The relationship among goals, values, and committed actions was discussed; participants were encouraged to identify and perform committed actions in support of values in addition to walking for fitness.
Table 2.
Manual protocol.
| Session (week) |
Topic or targeted component |
Sample suggested exercisesa | Aims or application to fitness intervention |
|---|---|---|---|
| 1 (1) | Introduction | Magic wand activity | Familiarize participants with the concept of CRF and the fitness walking program protocol (i.e., RPE and heart rate monitor) |
| 2 (2) | Values | The compass metaphor Skiing metaphor Values identification |
Identify and clarify personal values Identify how increasing fitness supports such values Enhance motivation to increase fitness |
| 3 (3) | Values, committed action, and barriers |
Skiing metaphor | Identify goals consistent with the individual’s values Help participants increase their awareness of and achieve fitness goals, despite internal and external barriers |
| Two kids in the car metaphor | Encourage adherence to interval training and exercise stra- tegies over the long term |
||
| Demons on a boat metaphor | Bring awareness to day-to-day choices and the connection to one’s goals |
||
| 4 (4) | Mindfulness | Extended mindfulness practice: sweet spot exercise Sunset vs. math problem metaphor Monitoring of bodily reactions and feelings before, during, and after physical exercise to explore responses to acute bouts of activity |
Enable negative internal events (i.e., thoughts) to flow without attachment Engaging in non-judgmental contact with psychological and physical events that occur Increase awareness during PA |
| 5 (5) | Acceptance (willingness) | Backpack metaphor | Distress tolerance Acknowledgment vs. avoidance internal discomfort (i.e., ne- gative emotions, cognitions, or bodily sensations) |
| Path up the mountain metaphor Passengers on a bus metaphor |
Recognize that modifying aversive or negative states often results in the delay or cessation of a goal-directed behavior |
||
| 6 (6) | Acceptance through cog- nitive defusion |
Leaves on a stream activity milk, milk, milk exercise Thought-distancing techniques – pushing against a clip- board exercise |
Break the link between thoughts and behavior (fitness related) Be more aware of thoughts sabotaging exercise plans |
| 7 (8) | Review | Review of selected exercises from above | Review key concepts Answer questions from participants |
| 8 (10) | Maintenance | Identification of negative internal experiences related to lapses in fitness-directed activity |
Continue to clarify values Renew commitment |
Complete list of suggested exercises available from the first author
2.1.2. Fitness walking program
All participants were provided specific guidelines for engaging in a walking program, which consisted solely of brisk, fitness-directed walking, outside of the group setting, during the participant’s free time. This mode of exercise requires minimal skill, equipment, or physical fitness (American College of Sports Medicine, 2013). Following the ACSM guidelines (2013), participants were instructed to engage in high-intensity interval walking at least 3 days a week, for a minimum total of 25 min/occasion. Specifically, participants were instructed to build up to their target heart rate (i.e., 70–85% of their maximal heart rate) and maintain this effort for brief periods of 3–4 min before decreasing the intensity and lowering their heart rate for a similar interval period. This form of high-intensity interval walking has been shown to be feasible in many populations, including sedentary adults (Lunt et al., 2014) and produces similar or superior outcomes (i.e., fitness, body composition, glycemic control, and cardiovascular health) to moderate-intensity continuous exercise (Guiraud et al., 2012; Karstoft et al., 2013; Kilpatrick, Jung, & Little, 2014; Morikawa et al., 2011; Nemoto, Gen-no, Masuki, Okazaki, & Nose, 2007). Participants were instructed in the use of electronic heart rate monitors to track heart rate and were given behavioral guidelines for increasing or decreasing their heart rate appropriately (e.g., walking faster or up a hill to increase their heart rate and decreasing walking speed and resistance to lower their heart rate). Weekly exertion and heart rate goals were provided to participants, who recorded their progress on walking logs that were submitted to the project director weekly. Specifically, weekly walking logs included daily recordings of the participants’ total walk time in minutes, the maximal rating of perceived exertion, and the maximum heart rate monitored. These weekly goals were gradually increased throughout the duration of the intervention to build participant tolerance for this new behavior (i.e., vigorous PA).
2.2. Measures
2.2.1. Ratings of perceived exertion
Participants were asked to monitor their maximum rating of perceived exertion (RPE) during the walking program using the Borg Scale (Borg, 1970), which provides qualitative descriptors of perceived effort, along with paired numeric ratings. Walking program instructions included target peak exertion levels for each walk; during the first week, the target peak was 13 (somewhat hard) and increased weekly for 4 weeks, after which the target peak remained at 17 (very hard) for the second half of the intervention.
2.2.2. Heart rate
Participants used electronic heart rate monitors (Omron HR-100C) during their fitness walking to gauge whether or not they were reaching their target heart rate. Participants’ initial maximal heart rates (HRmax) were estimated using a standard formula (220-age=HRmax; American College of Sports Medicine, 2013). Participants were asked to gradually increase their target heart rate, beginning at the pulse rate (or beats per minute) associated with 70% HRmax and moving up to 85% HRmax over the 10-week intervention. The data were collected via self-reported logs that participants completed weekly, not directly downloaded from the monitors themselves. Participants recorded observed heart rates from the Omron electronic heart rate monitors on paper and pencil logs provided by the study, and turned these in during group sessions.
2.2.3. CRF
CRF was measured both pre- and post-intervention using the Rockport 1-mile walk test (Kline et al., 1987), which measures the time it takes to walk 1 mile “at best effort,” as well as the individual’s heart rate during the walk. The CRF measures derived from the walk test included the walk test time (total minutes and seconds) and estimated aerobic capacity (VO2max), which was calculated using a previously validated sex-specific formula that is based on the participant’s heart rate during the test and their weight, age, and walk test time.4 The validity for this estimation formula was initially established with validation and cross-validation groups (Kline et al., 1987). The correlations between the estimated VO2max and actual VO2max (i.e., measured through direct gas exchange) were high for both groups (n = 174; r=.93 and n = 169; r=.92, respectively). In addition, this measure has been further validated by numerous researchers for a variety of samples, including young and older adults (Fenstermaker, Plowman, & Looney, 1992; Hageman, Walker, Pullen, & Pellerito, 2001; O’Hanley et al., 1987). This measure extends the results of previous research using self-reported PA data through its measurement of an objective indicator of health and fitness. In addition, it offers some benefits over the direct measurement of maximal oxygen uptake, which requires extensive and expensive laboratory staff and equipment. Given its validity as a measurement of estimated aerobic capacity and its cost effectiveness, the Rockport 1-mile walk test is a sensible choice, especially compared to objective measurements, for feasibility trials such as this. In the current study, the test was conducted in a standardized manner, and participants were outfitted with an Omron HR-100C electronic heart rate monitor during the walk test, which provided a measure of their heart rate.
2.2.4. Psychological flexibility
Two separate measures of psychological flexibility were used in the trial. The Acceptance and Action Questionnaire-II (AAQ-II; Bond et al., 2011) is a 7-item Likert scale measure of general psychological flexibility, with good structure (i.e., unidimensional), reliability (α =.84 [.78–.88]), and validity. Higher scores indicate lower levels of flexibility. Engagement in acceptance of exercise-related internal experiences was measured using the Physical Activity Acceptance Questionnaire (PAAQ; Butryn et al., 2014). The PAAQ (mean α =.79) includes ratings of 5 items on a 7-point Likert scale, with higher scores indicating greater acceptance of internal barriers for PA (Butryn et al., 2011; Forman et al., 2009; Goodwin, Forman, Herbert, Butryn, & Ledley, 2012).
2.2.5. Treatment acceptability
Treatment acceptability was evaluated after the intervention using the following two questions, each measured on a 5-point Likert-scale (1 = not at all, 3 = somewhat, 5 = very): “How helpful did you find the strategies (e.g., acceptance, values, and defusion) for responding to urges or desires pushing you to make unhealthy choices regarding your physical activity?” and “How satisfied were you with the approach we used to help you make changes in your physical activity level?” These items were based on those developed by Forman et al. (2009) and used by others (e.g., Goodwin et al., 2012) to evaluate acceptance-based behavioral medicine treatments. There are no psychometric data available for these items.
2.3. Statistical analyses
Standardized forms and procedures were used to collect data, which were double-entered into Microsoft Excel to ensure accuracy. The data were exported to PASW 18 (IBM Corp., 2009) for analyses. Listwise deletion was used for the primary and secondary analyses. Missing data did not exceed 5.3% for any item. Paired sample t-tests were used to analyze the mean change (baseline to post-intervention) on measures of CRF and psychological flexibility.
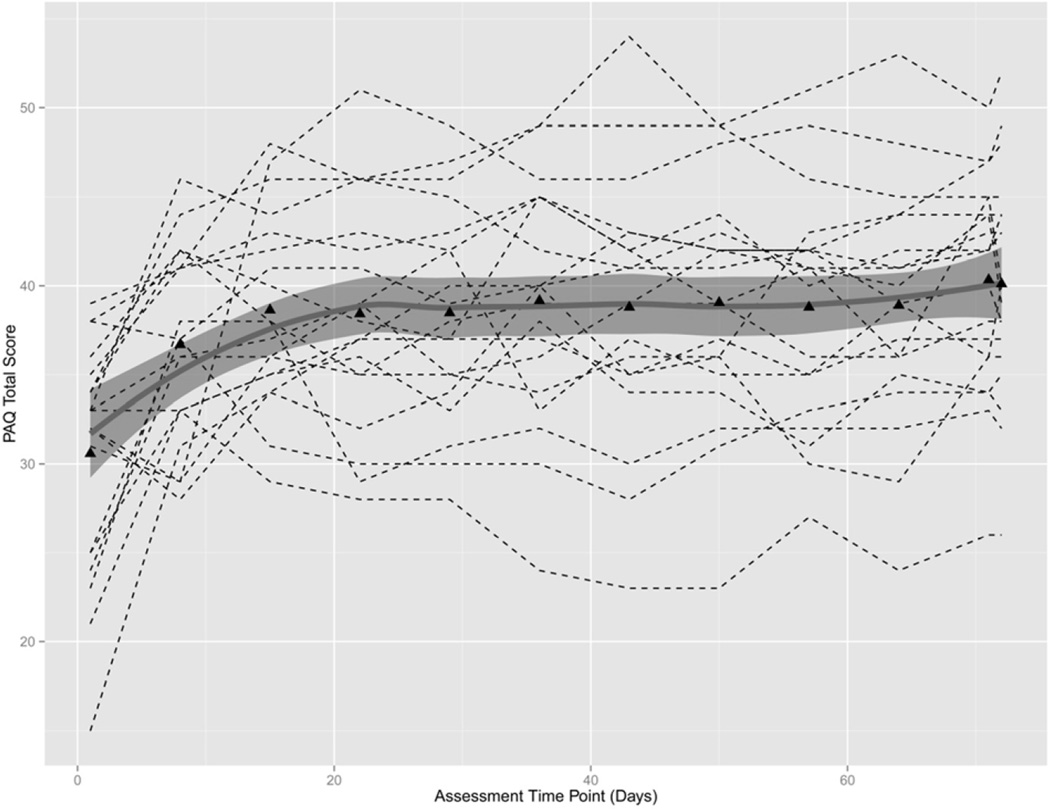
Growth curve modeling was used to examine the change over time in the PAAQ. A plot of these data over time showed substantial nonlinearity. To account for this, we used a latent basis growth curve model to model change over time and 95% confidence intervals (CIs) for parameters were estimated via 2000 bootstrap samples. Growth curve analyses were conducted using Mplus v7.2 software (Muthén and Muthén, 2014), and Full Information Maximum Likelihood was used to handle missing data.
3. Results
Independent sample t-tests were used to assess the baseline differences between completers and non-completers (defined as participants who initiated treatment but did not complete the 10-week intervention) for the following variables: age, baseline walk time, weight (kg), estimated VO2max, AAQ-II, PAAQ, ethnicity, income, education, sex, and marital status. No statistically significant differences were found for any of the analyses performed (all ps > .05).
The average walk adherence rate (calculated by dividing the number of walking sessions completed during the 10-week intervention by the number of prescribed sessions) was 89.30%. In addition, participants were found to have 92% compliance with weekly maximum heart rate goals and 80% adherence to RPE goals. The correlation between average weekly compliance for heart rate goals and PAAQ change was −.36 (p = .133). Bootstrapping this correlation with 10,000 bootstrap samples resulted in a significant correlation (95% CI [−.866, −.097]). The correlation between average weekly compliance for RPE and PAAQ change was −.39 (p = .096). Bootstrapping this correlation with 10,000 bootstrap samples resulted in a significant correlation (95% CI [− .750, − .061]). The average group session attendance rate was 85.50%. When questioned about the acceptability of the intervention in promoting adherence to the prescribed program, participants reported finding the strategies used in the treatment mostly helpful (M=3.84, SD=.68), and they reported feeling mostly satisfied (M=4.32, SD=.58).
The results of the analyses indicated a significant, large-sized (Cohen, 1988) decrease of 64.69 seconds in total walk test time [p = .0002, d=.645] and a significant and medium-sized increase of 2.9 ml/kg/min in estimated VO2max [p=.0007, d= −.43]. On average, participants increased their estimated VO2max from 24.43 ml/ kg/min to 27.34 ml/kg/min. Analyses indicated a non-significant, medium-sized increase in general psychological flexibility (AAQ-II) [p = .26, d=.37] and a significant, large-sized increase in exercise-related psychological flexibility (PAAQ) [p< .0001, d= −2.09] (see Table 3).
Table 3.
Baseline and post-intervention measures for primary and secondary outcomes.
| Measure | Baseline |
Post-intervention |
Paired t-test (df = 18) |
||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | T | p | d | |
| 1-mile walk time (s) |
980.95 | 99.34 | 916.26 | 102.54 | 4.61 | <.01 | .64 |
| Estimated VO2max (ml/kg/ min) |
24.43 | 6.71 | 27.34 | 6.83 | − 4.05 | <.01 | − .43 |
| AAQ II | 17.84 | 7.45 | 10.53 | 27.25 | 1.18 | .26 | .37 |
| PAAQ | 3.14 | .92 | 5.04 | .90 | −9.19 | <.01 | −2.09 |
Note: Higher scores on the AAQ-II indicate greater psychological inflexibility, while higher scores on the PAAQ indicate greater psychological flexibility. The table includes results for analyses conducted with the completer sample.
Data from the 12 PAAQ assessments were plotted and showed substantial nonlinear change, with most of the change occurring during the first 3 weeks of the intervention (see Fig. 2). The results from the latent basis growth curve analysis showed significant mean change over time (mean slope factor=8.5, 95% CI [2.6, 13.8]); however, there was also significant variability in this change (variance of slope factor=34.5, 95% CI [6.5, 87.8]). There was a significant intercept mean (mean intercept factor=31.2, 95% CI [23.2, 36.5]). The model fit was less than adequate (RMSEA=.253, CFI=.780, SRMR = .324). The correlation between the change in PAAQ and the change in estimated VO2max (as calculated by the baseline scores minus the post-intervention scores) was .26 (p = .27). Bootstrapping this correlation with 10,000 bootstrap samples resulted in a non-significant correlation 95% CI [−.017, .730].
Figure 2.
PAAQ plotted over time, with means, lowess curve, and 95% confidence interval shading.
4. Discussion
4.1. Study outcomes
In this study, we demonstrated the feasibility and acceptability of a mindfulness- and acceptance-based treatment through participant retention, attendance, and adherence. Attrition was 21.0%, very near the a priori estimated rate of 20% on the basis of the results of previous trials (e.g., Dunn et al., 1999), and no significant demographic differences were identified between completers and non-completers. The high rates of participant attendance and adherence to the walking program (i.e., walking sessions, maximum heart rate goals, and RPE goals) demonstrate the feasibility and acceptability of both the therapeutic intervention and the PA portion of the trial. Treatment acceptability was further supported by the high self-reported ratings of satisfaction with, and the perceived helpfulness of, the therapeutic intervention. This study joins a growing body of literature regarding the feasibility and acceptability of mindfulness and acceptance-based interventions, particularly in the area of health behavior change in at-risk populations (e.g., Goodwin et al., 2012; Forman et al., 2009).
The results of this study also provide initial findings to encourage further research. Completers showed a significant increase in CRF, as assessed by both walk test-derived outcomes (walk test time and estimated VO2max). On average, participants increased their estimated VO2max, demonstrating an almost full MET gain (>4/5ths of a MET). From a public health perspective, this gain approaches a clinically meaningful health benefit, as a 1 MET increase is associated with an 8–20% reduction in cardiovascular and all-cause mortality for men and women (Myers et al., 2002, 2004, 2015; Swain and Franklin, 2006). The results also demonstrated an increase in psychological flexibility related to PA, reflecting a decrease in the avoidance of exercise-related internal experiences. Changes in global psychological flexibility were in the expected direction but did not reach significance, perhaps because of the behavior-specific psychological flexibility targeted by the treatment.
Results from the growth curve modeling of the PAAQ suggest several interesting effects. First, the significant mean and variance of the slope factor suggest that changes in the experiential acceptance of PA occurred within- and between-persons, indicating that the PAAQ changed over time for individuals but that this change was different for different people. Second, the significant mean of the intercept factor suggests that where you start out initially in terms of your PAAQ score predicts where you will end up in the future, indicating that those with higher mean PAAQ scores will have a higher PAAQ score at the end of the intervention. Fig. 2 shows that most of the change in the PAAQ occurred within the first or second week of the intervention. In addition, there was significant heterogeneity in the change over time for this variable. The mean value of the PAAQ at post-test was 40.1 (SD = 6.4), but the lowest score was 26 (over two standard deviations from the mean) and the highest was 52 (almost two standard deviations from the mean). Recent research suggests that PA interventions in particular produce heterogeneous outcomes, even under strict protocol conditions in which treatment fidelity is high (Winett et al., 2014). Understanding and predicting this heterogeneity could allow researchers to provide more effective interventions. One method of identifying and predicting this heterogeneity is through the use of growth mixture models (Ram and Grimm, 2007). This study lacked the sample size to conduct these analyses; however, when sufficiently powered, this method could allow researchers to identify subgroups of people (i.e., responders vs. non-responders) and use baseline characteristics to predict participants’ subgroups. The heterogeneity in the PAAQ and the estimated VO2max was also likely a factor for the non-significant correlation between the two variables. Future research with larger sample sizes may identify a significant correlation between these variables.
4.2. Strengths and limitations
This study had several strengths that are worth noting. First, this is the first study to investigate the feasibility of ACT to increase adherence to an interval walking program aimed at increasing CRF. Exercise science research has found that interval training is an effective and efficient form of PA that can have a significant impact on physiological health (Karstoft et al., 2013; Morikawa et al., 2011; Nemoto et al., 2007); however, despite evidence of the benefits of vigorous PA, the rates of adherence to this behavior are low. The use of both interval training and vigorous PA demonstrates that the intervention employed in the current study was grounded in the latest exercise science research (DeFina et al., 2015; Karstoft et al., 2014; Myers et al., 2015). In addition, the use of an objective measure for the primary outcome (i.e., CRF) as opposed to a self-reported measure is a substantial strength of this study that allows for a more reliable measure of actual health outcomes. Finally, the use of growth curve modeling of psychological flexibility allows for a better understanding of how this construct changes over time. The use of these more intensive longitudinal analytic approaches allows for a better understanding of the growth of psychological flexibility by participants throughout the intervention, as well as inter-individual variability in this change.
These strengths notwithstanding, there were several limitations worth noting that are generally inherent to small feasibility and acceptability studies of innovative therapy. Most notably, the lack of a control group limits the causal claims that can be made on the basis of the results of this open trial, as changes may be attributed to the passage of time or to non-specific therapeutic effects. In addition, this trial lacked a long-term follow-up. However, a randomized controlled trial with long-term follow-up assessment points would have been inappropriately matched to this stage of research development. This study’s main goal was to establish the feasibility and acceptability of our intervention and to provide initial data on which future studies can build to solidify efficacy, effectiveness, and eventual translation into practice.
Another critical limitation relates to the measure used for primary outcome variables: a field test was used to measure estimated VO2max rather than a measure of direct gas exchange. While the validation studies for the Rockport 1-mile walk test show high correlations between the estimated and actual measures of VO2max, direct gas exchange continues to be the gold standard for measuring CRF. Furthermore, the behavior-specific measure of psychological flexibility used (the PAAQ) has yet to be subjected to rigorous psychometric testing; the general measure, although it has strong psychometric properties, failed to achieve significance, perhaps indicating limited sensitivity to the behavior-specific avoidance targeted by the treatment.
While the sample was homogeneous (i.e., educated, middle-aged, white females), which limits the generalizability of our findings, it also provides valuable information regarding the demographic to which this type of intervention might appeal the most and therefore, is more likely to continue engagement. In addition, although the treatment manual was revised on the basis of a consensus between two ACT-trained therapists and input from expert reviewers, only one therapist was available for intervention administration; thus, therapist effects could not be assessed directly.
4.3. Future directions
This open trial demonstrated the initial feasibility and acceptability of the use of a contextual CBT approach to increasing fitness-directed walking in a sedentary adult sample. The results need to be replicated and extended in larger randomized control trials with diverse participants and state-of-the-art measures (i.e., accelerometers). Carroll and Nuro (2002), in their stage model for psychotherapy development, suggested that the purpose of the second stage of manual development includes trials to build further efficacy for treatment. During this phase, a clear differentiation of the treatment condition from the control or comparison condition is necessary to establish treatment efficacy. Trials that include commonly used therapy techniques for health behavior change as usual care conditions would help to further establish the efficacy of this new intervention. Following this efficacy phase, continued research with different samples (i.e., health disparity samples or those with high-risk disease profiles) would serve to increase the generalizability of the results.
Further studies are needed to understand the mechanisms of change in this intervention. In future studies, the use of individual measures of constructs used in the therapy protocol (i.e., mindfulness, acceptance, cognitive defusion, and values) could help to explicate the differential impact each construct has on the behavior change process. In addition, the manual was designed specifically in a modular format to allow for flexibility in the order in which the constructs are presented. Changing this order may elucidate the importance of the constructs at differing times in the behavior change process. Given that most of the change in the PAAQ occurred within the first one or two treatment sessions, future studies should examine the utility of brief ACT interventions and account for the nonlinear change in the PAAQ by using non-parametric tests or modeling the nonlinear change via latent basis models. In addition, future studies could use growth mixture modeling to identify subgroups of individuals who show unique PAAQ trajectories and try to predict these subgroups to identify individuals who will be more responsive to an ACT intervention. Given the non-significant correlation between change scores for the PAAQ and the estimated VO2max, future research that is focused on efficacy trials for this intervention should explore the relationships among these variables to determine whether greater acceptance of barriers to PA is a mediator of the relationship between the intervention and CRF.
Consistent with the results of previous trials (e.g., Butryn et al., 2011; Forman et al., 2009; Gregg et al., 2007), this study’s findings support the feasibility and acceptance of mindfulness and acceptance-based contextual therapies in the field of behavioral medicine, particularly for health behavior change. In addition, the feasibility and acceptability of these therapies were demonstrated with a previously sedentary sample, supporting a focus on identified at-risk populations for whom experiential avoidance may be high, such as in cases of chronic pain or progressing disability (Gifford et al., 2004; Vowles and McCracken, 2008).
Acknowledgments
The first author is supported by National Cancer Institute Grant R25T CA057730. This research was also supported in part by the Center for Energy Balance in Cancer Prevention and Survivorship, which is supported by the Duncan Family Institute for Cancer Prevention and Risk Assessment. The University of Texas MD Anderson Cancer Center is supported in part by the National Institutes of Health through Cancer Center Support Grant CA016672.
Footnotes
One MET is equivalent to a VO2 of 3.5 ml/kg/min or the energy expenditure of sitting at rest.
Estimated VO2max=132.853 – (.1692 × body weight in kg)–(.3877 × age) + (6.315 for men)–(3.2649 × time in min) –(.1565 h).
Effect sizes were calculated according to the method suggested by Dunlop et al. (1996).
References
- American College of Sports Medicine. ACSM’s resource manual for guidelines for exercise testing and prescription. 7th ed. Philadelphia, PA: Lippincott, Williams, & Wilkins; 2013. [Google Scholar]
- Blair SN, Church TS. The importance of physical activity and cardiorespiratory fitness for patients with type 2 diabetes. Diabetes Spectrum. 2003;16:236–240. [Google Scholar]
- Blair SN, Kohl HW, 3rd, Paffenbarger RS, Jr, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality: A prospective study of healthy men and women. Journal of the American Medical Association. 1989;262(17):2395–2401. doi: 10.1001/jama.262.17.2395. [DOI] [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Zettle RD. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: A revised measure of psychological flexibility and experiential avoidance. Behavior Therapy. 2011;42(4):676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Borg G. Perceived exertion as an indicator of somatic stress. Scandinavian Journal of Rehabilitative Medicine. 1970;2:92. [PubMed] [Google Scholar]
- Bricker J, Wyszynski C, Comstock B, Heffner JL. Pilot randomized controlled trial of web-based Acceptance and Commitment Therapy for smoking cessation. Nicotine and Tobacco Research. 2013;15(10):1756–1764. doi: 10.1093/ntr/ntt056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butryn ML, Arigo D, Raggio GA, Kaufman AI, Kerrigan SG, Forman EM. Measuring the ability to tolerate activity-related discomfort: Initial validation of the physical activity acceptance questionnaire (PAAQ) Journal of Physical Activity and Health. 2014 doi: 10.1123/jpah.2013-0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butryn ML, Forman E, Hoffman K, Shaw J, Juarascio A. A pilot study of Acceptance and Commitment Therapy for promotion of physical activity. Journal of Physical Activity and Health. 2011;8(4):516–522. doi: 10.1123/jpah.8.4.516. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nuro KF. One size cannot fit all: A stage model for psychotherapy manual development. Clinical Psychology: Science and Practice. 2002;9:396–406. [Google Scholar]
- Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: A randomized controlled trial. Journal of the American Medical Association. 2007;297(19):2081–2091. doi: 10.1001/jama.297.19.2081. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- DeFina LF, Haskell WL, Willis BL, Barlow CE, Finley CE, Levine BD, Cooper KH. Physical activity versus cardiorespiratory fitness: Two (partly) distinct components of cardiovascular health? Progress in Cardiovascular Diseases. 2015;57(4):324–329. doi: 10.1016/j.pcad.2014.09.008. [DOI] [PubMed] [Google Scholar]
- Dhurandhar NV, Schoeller D, Brown AW, Heymsfield SB, Thomas D, Sørensen TIA, Allison DB. Energy balance measurement: When something is not better than nothing. International Journal of Obesity. 2014 [Google Scholar]
- Duncan GE, Anton SD, Sydeman SJ, Newton RL, Jr, Corsica JA, Durning PE, Perri MG. Prescribing exercise at varied levels of intensity and frequency: A randomized trial. Archives of Internal Medicine. 2005;165(20):2362–2369. doi: 10.1001/archinte.165.20.2362. [DOI] [PubMed] [Google Scholar]
- Dunlop WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. [Google Scholar]
- Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, 3rd, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: A randomized trial. Journal of the American Medical Association. 1999;281(4):327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- Ekkekakis P. Pleasure and displeasure from the body: Perspectives from exercise. Cognition and Emotion. 2003;17(2):213–239. doi: 10.1080/02699930302292. [DOI] [PubMed] [Google Scholar]
- Ekkekakis P, Hall EE, Petruzello SJ. The relationship between exercise intensity and affective responses demystified: To crack the 40-year-old nut, replace that 40-year-old nutcracker. Annals of Behavioral Medicine. 2008;35:136–149. doi: 10.1007/s12160-008-9025-z. [DOI] [PubMed] [Google Scholar]
- Fenstermaker KL, Plowman SA, Looney MA. Validation of the Rockport Fitness Walking Test in females 65 years and older. Research Quarterly for Exercise and Sport. 1992;63:322–327. doi: 10.1080/02701367.1992.10608749. [DOI] [PubMed] [Google Scholar]
- Forman EM, Butryn M, Hoffman KL, Herbert JD. An open trial of an acceptance-based behavioral treatment for weight loss. Cognitive and Behavioral Practice. 2009;16:223–235. [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Antonuccio DO, Piasecki MM, Rasmussen-Hall ML, Palm KM. Acceptance-based treatment for smoking cessation. Behavior Therapy. 2004;35:689–705. [Google Scholar]
- Goodwin CL, Forman EM, Herbert JD, Butryn ML, Ledley GS. A pilot study examining the initial effectiveness of acceptance based behavior therapy for modifying diet and physical activity among cardiac patients. Behavior Modification. 2012;36(2):199–217. doi: 10.1177/0145445511427770. [DOI] [PubMed] [Google Scholar]
- Gregg JA, Callaghan GM, Hayes SC, Glenn-Lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2007;75(2):336–343. doi: 10.1037/0022-006X.75.2.336. [DOI] [PubMed] [Google Scholar]
- Guiraud T, Nigam A, Gremeaux V, Meyer P, Juneau M, Bosquet L. High-intensity interval training in cardiac rehabilitation. Sports Medicine. 2012;42(7):587–605. doi: 10.2165/11631910-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Hageman PA, Walker SN, Pullen CH, Pellerito P. Test-retest reliability of the Rockport Fitness Walking Test and other fitness measures in women ages 50-69 year. Journal of Geriatric Physical Therapy. 2001;24(2):7–11. [Google Scholar]
- Hayes SC. Acceptance and Commitment Therapy, Relational Frame Theory, and the third wave of behavior therapy. Behavior Therapy. 2004;35:639–665. doi: 10.1016/j.beth.2016.11.006. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Stroshal KD, Wilson KG. Acceptance and commitment therapy. New York: Guilford Press; 1999. [Google Scholar]
- Hayes SC, Villatte M, Levin M, Hildebrandt M. Open, aware, and active: Contextual approaches as an emerging trend in the behavioral and cognitive therapies. Annual Review of Clinical Psychology. 2011;7:141–168. doi: 10.1146/annurev-clinpsy-032210-104449. [DOI] [PubMed] [Google Scholar]
- Helmerhorst HJ, Brage S, Warren J, Besson H, Ekelund U. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. International Journal of Behavioral Nutrition and Physical Activity. 2012;9(1):103–157. doi: 10.1186/1479-5868-9-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corp. PASW statistics for windows, version 18.0. Chicago: SPSS Inc; 2009. [Google Scholar]
- Karstoft K, Winding K, Knudsen SH, James NG, Scheel MM, Olesen J, Solomon TP. Mechanisms behind the superior effects of interval vs continuous training on glycaemic control in individuals with type 2 diabetes: A randomised controlled trial. Diabetologia. 2014;57(10):2081–2093. doi: 10.1007/s00125-014-3334-5. [DOI] [PubMed] [Google Scholar]
- Karstoft K, Winding K, Knudsen SH, Knudsen SH, Nielsen JS, Thomsen C, Solomon TP. The effects of free-living interval-walking training on glycemic control, body composition, and physical fitness in type 2 diabetic patients: A randomized controlled trial. Diabetes Care. 2013;36:228–236. doi: 10.2337/dc12-0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick MW, Jung ME, Little JP. High-intensity interval training: A review of physiological and psychological responses. ACSM’s Health Fitness Journal. 2014;18(5):11–16. [Google Scholar]
- Kline GM, Porcari JP, Hintermeister R, Freedson PS, Ward A, McCarron RF, Rippe JM. Estimation of VO2max from a one-mile track walk, gender, age, and body weight. Medicine and Science in Sports and Exercise. 1987;19(9):253–259. [PubMed] [Google Scholar]
- Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, Sone H. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. Journal of the American Medical Association. 2009;301(19):2024–2035. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- Lee DC, Sui X, Ortega FB, Kim YS, Church TS, Winett RA, Blair SN. Comparisons of leisure-time physical activity and cardiorespiratory fitness as predictors of all-cause mortality in men and women. British Journal of Sports Medicine. 2011;45(6):504–510. doi: 10.1136/bjsm.2009.066209. [DOI] [PubMed] [Google Scholar]
- Lee IM, Sesso HD, Oguma Y, Paffenbarger RS., Jr Relative intensity of physical activity and risk of coronary heart disease. Circulation. 2003;107(8):1110–1116. doi: 10.1161/01.cir.0000052626.63602.58. [DOI] [PubMed] [Google Scholar]
- Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: A preliminary test of a theoretical model. Annals of Behavioral Medicine. 2009;37(1):58–69. doi: 10.1007/s12160-009-9083-x. [DOI] [PubMed] [Google Scholar]
- Lundgren T, Dahl J, Melin L, Kies B. Evaluation of acceptance and commitment therapy for drug refractory epilepsy: A randomized controlled trial in South Africa—A pilot study. Epilepsia. 2006;47(12):2173–2179. doi: 10.1111/j.1528-1167.2006.00892.x. [DOI] [PubMed] [Google Scholar]
- Lunt H, Draper N, Marshall HC, Logan FJ, Hamlin MJ, Shearman JP, Frampton CM. High intensity interval training in a real world setting: a randomized controlled feasibility study in overweight inactive adults, measuring change in maximal oxygen uptake. PLoS One. 2014;9(1) doi: 10.1371/journal.pone.0083256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken LM, MacKichan F, Eccleston C. Contextual cognitive-behavioral therapy for severely disabled chronic pain sufferers: Effectiveness and clinically significant change. European Journal of Pain. 2007;11(3):314–322. doi: 10.1016/j.ejpain.2006.05.004. [DOI] [PubMed] [Google Scholar]
- Moffitt R, Mohr P. The efficacy of a self-managed Acceptance and Commitment Therapy intervention DVD for physical activity initiation. British Journal of Health Psychology. 2015;20(1):115–129. doi: 10.1111/bjhp.12098. [DOI] [PubMed] [Google Scholar]
- Morikawa M, Okazaki K, Masuki S, Kamijo YI, Yamazaki T, Genno H, Nose H. Physical fitness and indices of lifestyle-related diseases before and after interval walking training in middle-aged and older males and females. British Journal of Sports Medicine. 2011;45(3):216–224. doi: 10.1136/bjsm.2009.064816. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus (version 7.2) [computer software] Los Angeles, CA: Muthén & Muthén; 2014. [Google Scholar]
- Myers J, Kaykha A, George S, Abella J, Zaheer N, Lear S, Froelicher V. Fitness versus physical activity patterns in predicting mortality in men. American Journal of Medicine. 2004;117(12):912–918. doi: 10.1016/j.amjmed.2004.06.047. [DOI] [PubMed] [Google Scholar]
- Myers J, McAuley P, Lavie CJ, Despres JP, Arena R, Kokkinos P. Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: Their independent and interwoven importance to health status. Progress in Cardiovascular Diseases. 2015;57(4):306–314. doi: 10.1016/j.pcad.2014.09.011. [DOI] [PubMed] [Google Scholar]
- Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. Newly England Journal of Medicine. 2002;346(11):793–801. doi: 10.1056/NEJMoa011858. [DOI] [PubMed] [Google Scholar]
- Nemoto K, Gen-no HM, Masuki S, Okazaki K, Nose H. Effects of high-intensity interval walking training on physical fitness and blood pressure in middle-aged and older people. Mayo Clinic Proceedings. 2007;82(7):803–811. doi: 10.4065/82.7.803. [DOI] [PubMed] [Google Scholar]
- O’Hanley S, Ward A, Zwiren L, McCarron R, Ross J, Rippe JM. Validation of a one-mile walk test in 70-79 year olds. Medicine and Science in Sports and Exercise. 1987;19:S28. [PubMed] [Google Scholar]
- Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. International Journal of Behavioral Nutrition and Physical Activity. 2008;5(1):56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram N, Grimm K. Using simple and complex growth models to articulate developmental change: Matching theory to method. International Journal of Behavioral Development. 2007;31(4):303–316. [Google Scholar]
- Ruiz FJ. A review of acceptance and commitment therapy (ACT) empirical evidence: Correlational, experimental psychopathology, component and outcome studies. International Journal of Psychology and Psychological Therapy. 2010;10(1):125–162. [Google Scholar]
- Ruiz FJ. Acceptance and commitment therapy versus traditional cognitive behavioral therapy: A systematic review and meta-analysis of current empirical evidence. International Journal of Psychology and Psychological Therapy. 2012;12(3):333–357. [Google Scholar]
- Sesso HD, Paffenbarger RS, Lee IM. Physical activity and coronary heart disease in men the Harvard Alumni Health Study. Circulation. 2000;102(9):975–980. doi: 10.1161/01.cir.102.9.975. [DOI] [PubMed] [Google Scholar]
- Sloane R, Snyder DC, Demark-Wahnefried W, Lobach D, Kraus WE. Comparing the 7-day PAR with a triaxial accelerometer for measuring time in exercise. Medicine and Science in Sports and Exercise. 2009;41(6):1334–1340. doi: 10.1249/MSS.0b013e3181984fa8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swain DP, Franklin BA. Comparison of cardioprotective benefits of vigorous versus moderate intensity aerobic exercise. American Journal of Cardiology. 2006;97(1):141–147. doi: 10.1016/j.amjcard.2005.07.130. [DOI] [PubMed] [Google Scholar]
- Tanasescu M, Leitzmann MF, Rimm EB, Willett WC, Stampfer MJ, Hu FB. Exercise type and intensity in relation to coronary heart disease in men. Journal of the American Medical Association. 2002;288(16):1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, Moore L. Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite. 2009;52(2):396–404. doi: 10.1016/j.appet.2008.11.012. [DOI] [PubMed] [Google Scholar]
- Vowles KE, McCracken LM. Acceptance and values-based action in chronic pain: A study of treatment effectiveness and process. Journal of Consulting and Clinical Psychology. 2008;76(3):397–407. doi: 10.1037/0022-006X.76.3.397. [DOI] [PubMed] [Google Scholar]
- Williams PT, Thompson PD. The relationship of walking intensity to total and cause-specific mortality. Results from the National Walkers’ Health Study. PLoS One. 2013;8(11):e81098. doi: 10.1371/journal.pone.0081098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winett RA, Davy BM, Savla J, Marinik EL, Winett SG, Baugh ME, Flack KD. Using response variation to develop more effective, personalized behavioral medicine?: Evidence from the Resist Diabetes Study. Translational Behavioral Medicine. 2014;4:1–6. doi: 10.1007/s13142-014-0263-2. [DOI] [PMC free article] [PubMed] [Google Scholar]