Abstract
Purpose
The aim of the present study was to assess patient satisfaction with pynk: Breast Cancer Program for Young Women so as to determine how the program might be improved and to provide feedback to donors.
Methods
All pynk patients who had consented to have their information entered in our database and who supplied us with their e-mail address were invited to complete a 58-item online questionnaire consisting of multiple choice and open-ended questions. Domains included demographics, provision of written and spoken information, support, infertility risk, research awareness, attitudes toward discharge, and general feedback.
Results
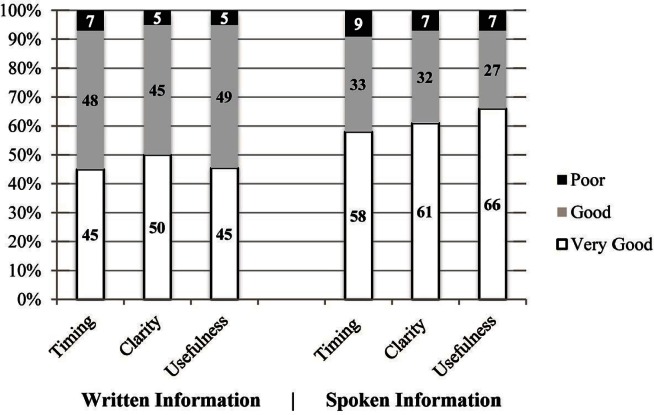
Of 120 pynk patients approached, 61 (51%) participated. More than 90% were satisfied or very satisfied with the timing, usefulness, and clarity of spoken and written information given, and 69% found the service and support provided by the nurse navigator to be the most helpful component of the program. Of those who had received systemic therapy, 93% recalled a health care provider initiating a discussion of the risk of treatment-related infertility, and 67% were referred to a fertility clinic. On the negative side, 11%–27% were unaware of various services provided by pynk, and 11% were unaware of pynk’s ongoing research. One third of patients were unhappy or ambivalent about the prospect of discharge from the program.
Conclusions
Patient satisfaction with this novel program for young women with breast cancer is high. This study highlights the critical role that the nurse navigator plays in patient support and dissemination of information. In contrast to other reported surveys of young cancer patients, pynk patients are routinely given the opportunity to undergo fertility preservation.
Keywords: Breast cancer, young women, support groups, oncofertility, psychosocial interventions, nurse navigator
INTRODUCTION
Breast cancer is the most common cancer in women, and it is the 2nd leading cause of cancer death in Canadian women1. Approximately 7% of female breast cancer patients are diagnosed at 40 years of age or younger2. The breast cancer incidence in young women varies with ethnicity and increases with lower socioeconomic status3. Although 88% of young breast cancer patients now survive more than 5 years1, this particular age group suffers more than older women both physiologically (from more-aggressive local and systemic treatment, and premature ovarian failure) and psychologically (from body image changes, relationship distress, marital strain, childcare issues, and alienation from healthy peers)4,5. Moreover, survival is lower in this population than in their older counterparts.
In 2001, in a study conducted by the Canadian Breast Cancer Network and the Ontario Breast Cancer Community Research Initiative called Nothing Fit Me6, Canadian women who had been diagnosed with breast cancer before the age of 40 reported that the care provided by their health care professionals did not meet their complex needs. Survey responders emphasized that supports were inadequate and that information specific to their age group about topics such as the effects of adjuvant chemotherapy on fertility and the methods of coping with both emotional and relationship distress was lacking. These women also recommended the provision of peer support groups and a nurse navigator to guide them through diagnosis, treatment, and recovery.
In 2008, in response to the Nothing Fit Me findings, a multidisciplinary committee from the Odette Cancer Centre at Sunnybrook Health Sciences Centre (consisting of representatives from medical, radiation, and surgical oncology; nursing; psychology and social work; and young breast cancer survivors) created pynk: Breast Cancer Program for Young Women.
The first program of its kind in Canada, pynk seeks to optimize care and support, to facilitate research, and to educate health care professionals about the treatment and unique needs of women diagnosed with breast cancer at age 40 or younger. It employs a full-time nurse navigator and provides formal support services and information relevant to the unique issues faced by this population. The program also encourages patients to participate in research studies focusing on younger women with breast cancer, a population greatly underrepresented in most breast cancer studies. Details of the services offered by pynk were described in detail in a previous issue of this journal4, but are summarized here.
The nurse navigator is the linchpin of pynk. She establishes the first line of contact with incoming patients and serves as a primary contact for any questions or concerns that arise throughout the course of the patient’s diagnosis, treatment, and follow-up. She is responsible for ensuring that all appropriate consultations take place (including fertility, genetics, and plastic surgery), and she helps the patients navigate the complexities of the cancer care system. The nurse navigator also provides informal support, information, and advice to patients and their families.
A variety of more formal support services are also provided by pynk. The Peer Support program pairs incoming patients with patients who share similar demographics and who have already completed active treatment. Incoming pynk patients also are encouraged to meet with a social worker who provides emotional support and guidance about financial issues. Additionally, a psychologist and a psychiatrist are both available on site as needed. The nurse navigator facilitates a monthly support group called “In the pynk,” and leads periodic workshops about sexuality issues.
Each new patient coming to pynk is supplied with an information package that includes fertility preservation information and a booklet that specifically addresses the unique emotional and physical needs of young women with breast cancer. Mothers with young children are given age-appropriate books to help them discuss their cancer diagnosis and treatment with their children. Information about community resources for young women with breast cancer, such as free babysitting services for financially needy mothers, is also provided.
Because more patients have been entering pynk and the capacity of the nurse navigator has been pushed to its maximum, it has become necessary to discharge, back to the care of their family physician, at a minimum of 5 years after their diagnosis, patients who have not experienced a recurrence and who have no active cancer-related issues.
In its 7 years of operation, pynk has provided services to more than 255 women in the Greater Toronto Area. In 2010, about 30 months after the program was launched, the program underwent a formal independent review from the perspective of the various health care providers who treat breast cancer at our institution. The review consisted of face-to-face interviews with a representative sample of stakeholders from each discipline, plus the members of the pynk executive. Based on that review, a number of changes were made, including an increase in the availability of the nurse navigator from part time to full time.
In 2013, 5 years after pynk was launched, a decision was made to formally review the program from the patient perspective to determine whether pynk was serving the needs of the patients and how the program might be improved. Results of the survey would also be presented in a formal program update to past donors and would be used as part of a presentation to potential future donors. Young women with breast cancer typically have multiple demands on their time, which makes conducting telephone interviews or focus groups with this population difficult. A decision was therefore made to survey the pynk patients with a relatively brief online questionnaire.
PURPOSE
The aims of the study were to assess patient satisfaction with pynk: Breast Cancer Program for Young Women so as to determine how the program might be improved and to provide feedback to donors.
METHODS
Questionnaire Development
The research study was approved by the Sunnybrook Health Sciences Centre Research Ethics Board.
The multidisciplinary pynk committee, consisting of a medical oncologist, nurse navigator, psychologist, social worker, research coordinator, breast cancer survivors, and research students drafted a set of survey objectives and question categories based on a literature review and issues that had been discussed in the monthly committee meetings since the inception of the program.
From September 2013 to January 2014, the pynk committee reviewed successive drafts of the survey to evaluate its clarity, coverage of the issues, potential for bias, and sensitivity of the language used. A pilot study was not conducted. The committee also made every effort to minimize the survey length. Modifications based on the committee’s suggestions were implemented and a final draft of the survey was produced. The final survey covered 8 domains: demographics, adequacy of support provided by the program in general and by the nurse navigator in particular, usefulness of the information given, frequency of pre-treatment fertility discussions and consultations, patient awareness of and participation in pynk research studies, attitudes toward “graduation” from the program, and general comments and suggestions.
The 58 items in the final questionnaire consisted of 43 multiple-choice questions, which include scaled (Likert) questions and 15 open-ended questions that gave participants the option of providing more detailed answers. All patients who did not receive chemotherapy or hormone treatment were automatically excluded from the fertility questions on the survey, because those questions did not apply to them. It was estimated that completion of the survey would take approximately 15 minutes. The survey was entered online using Survey-Monkey (Palo Alto, CA, U.S.A.).
Patients and Study Design
Each pynk patient is asked, at one of her initial appointments, for written consent to have her clinical information uploaded to the pynk database and to be approached for research studies. Of the 178 pynk patients in the database at the time the present study was conducted, all 120 living and eligible patients were invited by e-mail to complete the online patient satisfaction survey. To be eligible, patients had to have given permission to be contacted for research studies (with a contact e-mail address) and had to have been diagnosed at least 1 year earlier (so that adjuvant chemotherapy and radiation treatment would have been completed). The survey was presented with an introductory letter indicating that the estimated time of completion was 15 minutes, that responses were anonymous, and that completion of the survey would demonstrate consent. Respondents were provided with the option of receiving a copy of the final survey results. The survey was open to respondents from January 2014 to June 2014. Reminders were sent by e-mail every month during that period to all 120 potential participants because, to ensure complete anonymity, no system was created for tracking individuals who had or had not completed the survey.
Data Analysis
Descriptive statistics were calculated for all variables of interest. Continuous measures such as age were summarized as means with standard deviation; categorical measures were summarized using counts and percentages. For comparisons of ordinal scores between groups (for example native versus non-native English speakers), a Wilcoxon rank-sum test was used. For comparison of two binary or categorical variables, chi-square tests were used (in the case of small numbers, Fisher exact tests were used instead). Statistical significance was accepted at a p value of less than 0.05. All analyses were carried out using the SAS software application (version 9.3: SAS Institute, Cary, NC, U.S.A.).
RESULTS
Of the 120 pynk patients selected for participation in the survey, 61 completed the questionnaire. Not all participants completed every question, because some questions were inapplicable; other questions might have been accidently missed or intentionally skipped.
Demographics
Table i summarizes participant characteristics. Average age at diagnosis was 35.6 years (range: 21–40 years), and average age at the time of survey completion was 37.7 years (range: 23–44 years). Most patients (75%) spoke English as a first language, and of those with another first language, most indicated that they understood written and spoken English “very well.” No patient required help completing the survey. When comparing the demographics of the pynk patients in the database as a whole to the respondent cohort, the demographics were nearly identical, with no significant differences in age, education, and ethnicity.
TABLE I.
Participant demographics
| Demographic category | Total respondents (n) | Responses [n (%)] |
|---|---|---|
| First language | 60 | |
| English | 45 (75) | |
| Other | 15 (25) | |
| Relationship status | 60 | |
| Married or common law | 40 (67) | |
| In relationship or engaged | 4 (7) | |
| Separated or divorced | 7 (12) | |
| Single or never married | 9 (15) | |
| Children | 60 | |
| None | 19 (32) | |
| One | 18 (30) | |
| Two | 21 (35) | |
| Three | 2 (3) | |
| Highest level of education | 61 | |
| University or college undergraduate | 34 (56) | |
| Postgraduate degree | 19 (31) | |
| Trade, vocational diploma, or certification | 2 (3) | |
| High-school diploma | 6 (10) | |
| Place of diagnosis | 60 | |
| Sunnybrook Hospital | 21 (35) | |
| Other | 39 (65) | |
| Location of surgery | 60 | |
| Sunnybrook Hospital | 35 (58) | |
| Other | 25 (42) | |
| Chemotherapy | 60 | |
| Yes | 53 (88) | |
| No | 7 (12) |
Written and Spoken Information
Figure 1 shows responses about the information supplied by pynk. More than 90% of respondents were satisfied or very satisfied with the timing, usefulness, and clarity of the written and verbal information received. Those questions were rated on a scale of 1–10, with 10 being the most ideal timing, the most beneficial or useful information, and the highest clarity. The interest of the patients in receiving written information in the format of a pamphlet or booklet at one of their first appointments scored 7.7 on average, and interest in written information on the pynk Web site, with various resources and links, scored 7.8 on average.
FIGURE 1.
Evaluation of information.
Approximately half the patients (26 of 53) found the verbal information received from their health care providers to be upsetting. Some of these patients mentioned in their comments that it was disturbing to learn about or to talk about their cancer, especially at a time of great anxiety. However, others commented that they found the information to be empowering.
No significant differences (p = 0.89 by Fisher exact test) were found between patients for whom English was and was not a first language with respect to responses to questions about the timing, clarity, or usefulness of written or spoken information. However, a trend was observed for patients who did not speak English as a first language to prefer written information in the form of a pamphlet and for patients who spoke English as a first language to prefer online resources.
Support
Tables ii and iii summarize responses about the use and usefulness of the pynk support services. Almost 90% of participants found the pynk nurse to be helpful or very helpful, and almost 70% found her to be the most useful component of the program. Psychology and social work were the optional services most frequently used by patients. When provided with the opportunity to elaborate on their answers, a few patients commented that they wanted to attend the monthly “In the pynk” support group, but that the hospital was too far away to reach without a car. Some mentioned that the nurse navigator had become like a second mother to them during treatment and that they loved the friends made through peer support. Additionally, several patients commented that the social worker was helpful in assisting with resources for financial aid.
TABLE II.
Evaluation of support
| PYNK support service | Total respondents (n) | Responses [n (%)] |
|---|---|---|
| Nurse navigator | 54 | |
| Very helpful | 41 (76) | |
| Helpful | 7 (13) | |
| Somewhat helpful | 4 (7) | |
| Not helpful | 2 (4) | |
| Most helpful time of supporta | 61 | |
| Throughout the entire process | 31 (51) | |
| After diagnosis but before treatment | 12 (20) | |
| During active treatment | 12 (20) | |
| After active treatment | 6 (10) | |
| Most helpful aspect of PYNKa | 60 | |
| PYNK nurse | 42 (70) | |
| Specialized care for young women | 13 (22) | |
| Group meetings | 3 (5) | |
| The medical oncologist | 2 (3) |
Multiple responses allowed.
TABLE III.
Awareness and use of specialized PYNK services
| Service | Total respondents (n) | Responses [n (%)] | ||
|---|---|---|---|---|
|
| ||||
| Used | Knew service was available but did not need it | Did not know about service | ||
| Peer support | 47 | 15 (32) | 27 (57) | 5 (11) |
| Psychologist | 49 | 22 (45) | 19 (39) | 8 (16) |
| Psychiatrist | 41 | 7 (17) | 23 (56) | 11 (27) |
| Social worker | 47 | 20 (43) | 23 (49) | 4 (9) |
| “In the PYNK” | 49 | 18 (37) | 27 (55) | 4 (8) |
Fertility
Table iv summarizes responses to questions concerning discussion of the possible detrimental effects of systemic therapy on fertility and referral for a fertility preservation consultation. Of patients eligible to respond, 93% recalled an oncology health care provider initiating, before treatment started, a discussion about the possible detrimental effect that systemic therapy might have on future fertility. We observed no significant association between being approached by the pynk nurse, the medical oncologist, or other medical professionals and the likelihood either of receiving a fertility clinic referral or of attending a fertility consultation after referral. Similarly, we observed no association between the perceived clarity of spoken information and the likelihood of attending a fertility consultation (p = 0.36). Women who were 35 years of age or older at diagnosis were more likely than younger women to attend a fertility consultation (p = 0.01). All 14 women who reported having received written materials about fertility preservation reported that the materials were “useful “or “very useful.”
TABLE IV.
Evaluation of fertility information and services
| Variable | Total respondents (n) | Responses [n (%)] |
|---|---|---|
| Treatment | 56 | |
| Chemotherapy alone | 20 (36) | |
| Hormone treatment alone | 5 (9) | |
| Both | 30 (54) | |
| Neither | 1 (2) | |
| Discussion on fertility before treatment | 55 | |
| Yes | 51 (93) | |
| Do not remember | 3 (5) | |
| No | 1 (2) | |
| Health care provider who initiated fertility discussion | 49 | |
| Medical oncologist | 23 (47) | |
| PYNK nurse | 15 (31) | |
| Both PYNK nurse and medical oncologist | 3 (6) | |
| Surgeon | 4 (8) | |
| Other | 4 (8) | |
| Offered referral to fertility clinic | 55 | |
| Yes | 37 (67) | |
| No | 18 (33) | |
| Written materials on fertility preservation given | 21 | |
| Yes | 14 (67) | |
| No | 7 (33) | |
| Patients attended fertility consultation after referral | 37 | |
| Yes | 22 (59) | |
| No | 14 (38) | |
| Not stated | 1 (3) | |
| Reasons for declining consultationa | ||
| Did not want to delay treatment | 9 | |
| Too expensive | 5 | |
| Afraid treatment might make the cancer more likely to come back | 5 | |
| Afraid future pregnancy might make the cancer more likely to come back | 4 | |
| Not interested in having more children | 3 |
Multiple responses allowed.
Research
When asked whether they were aware of any research being conducted by pynk, 49% (30 of 61) reported that they were aware of ongoing research, 34% (21 of 61) that they were unsure, and 16% (10 of 61) that they were unaware of any research being conducted by pynk. Of the 30 women who were aware of research being conducted by pynk, 26 (87%) reported that they had been involved in past pynk research, 3(10%) were unsure about their participation in past pynk research, and 1(3%) reported that they had not been involved in past pynk research. Of the 26 women who had participated in prior pynk research, the number of studies, questionnaires, etc., offered to the patient were reported to be enough by 23 (88%)and too many by 3 (12%). Several women commented that they were interested in participating in more research studies that would help to improve breast cancer outcomes in young women. Other research areas mentioned by patients to be of interest to them were nutrition and the effects of treatment on fertility.
Discharge from PYNK
All but 1 pynk patient had a family doctor. When asked about the prospect of “graduating” from pynk, 19 of 54 respondents (35%) reported that it made them happy because it would indicate that they were well and were expected to stay well; 11 (20%) were neither happy nor unhappy about the prospect; 19 (35%) were unhappy with the prospect either because they were not confident that their family doctor would be able to provide adequate follow-up care or because they simply preferred to be followed at the cancer centre; and 5 (9%) reported that graduation did not apply to them because they had ongoing health issues such as metastatic disease. When asked how far in advance of “graduation” they would like to be notified, 29 of 53 respondents (55%) chose 6 months beforehand, 12 (23%) chose 1 year beforehand, and 12 (23%) said that no advance notice was necessary.
General Comments
When provided with the opportunity to elaborate on how pynk could improve, some women suggested employing more nurse navigators. Others suggested opening programs like pynk, with or without the monthly support groups, across the country in various geographic areas. A few women recommended building a network of young breast cancer patients who could support each other either in person or online.
DISCUSSION
The present study is the first to explore pynk: Breast Cancer Program for Young Women from the patient perspective, and the results show that a large proportion of the patients are satisfied with the program. The 58-item questionnaire provided thorough coverage of all major topics relevant to pynk. The 61 participants in the study were found to be a representative sample of the eligible pynk population as a whole: well-educated women, most with a university, college, or postgraduate degree, married or living in a common law relationship with children at the time of diagnosis. The major limitation of the study is that approximately 13% of the young women in pynk declined to have their clinical information entered into the pynk database and would not have been eligible for the survey. Furthermore, compared with patients who did not agree to give their e-mail address to the pynk nurse (and who were therefore not eligible for the present study), those who did agree might have been intrinsically more satisfied with the program.
A 2014 Canadian survey showed that, despite great effort to improve the care provided to young women diagnosed with breast cancer, many gaps still exist7. For example, young patients require continual dialogue, teaching, and emotional support from the beginning of their diagnosis and throughout the rest of their breast cancer journey, but those needs are not currently being met. To mitigate the gaps, the study investigators suggested that a nurse navigator be assigned to patients immediately after diagnosis to help map the cancer system and to provide practical support. The nurse navigator would be able to address concerns pertaining specifically to young breast cancer patients, such as early menopause, infertility resulting from chemotherapy, and psychological distress.
It is therefore not surprising that the most helpful aspect of pynk overall was reported to be the nurse navigator; most patients appreciated having her involved right from the time of diagnosis. Although the issue was not specifically addressed in the survey, the abandonment in 2013 of the earlier system of assigning a primary nurse to each cancer patient has led pynk patients to become increasingly dependent on the pynk nurse navigator. As the number of women in the program grows, having a single full-time nurse to satisfy the needs of all the patients will become impossible, even if all appropriate patients are discharged from the program after 5 years. More donor funding (upon which pynk relies entirely) would allow for an additional nurse to be hired, which would undoubtedly result in even better care and greater patient satisfaction.
In addition to providing adequate medical treatment, cancer programs should provide sufficient and appropriate information about the disease and available treatment options8. Davies et al.9 and Husson et al.10 demonstrated that patient satisfaction is greater when the information provided matches the patient’s needs. Satisfaction with information has been shown to be associated with better illness perception and better health-related quality of life9,10. The high rate of satisfaction that our patients expressed about the information they received is gratifying, because studies have shown that cancer patients are generally not satisfied with the information provided by health care professionals11.
Many studies have shown that worry about future fertility is very prevalent among young breast cancer patients12, because most are treated with gonadotoxic chemotherapy, and many are also treated with hormonal therapy, which delays their childbearing, with a consequent age-related decline in ovarian function13. The American Society of Clinical Oncology has recommended that health care providers discuss the risk of treatment-related infertility and fertility preservation options with young cancer patients as soon as possible after diagnosis14. Unfortunately, the literature suggests that such discussions often do not occur, leading to great frustration and disappointment once active treatment is complete15,16.
An important priority during the development of pynk was to ensure that the potential impact of treatment on fertility was discussed with all patients. The survey indicated that the latter goal has been successfully achieved, with 93% of patients reporting that they were approached to discuss the potential effects of their cancer treatment on their fertility before chemotherapy or hormone therapy was initiated. The survey also showed that, after that discussion, an appropriate number of patients (based on patient parity and age of the children) were referred to a fertility clinic. The fact that women who were 35 years of age or older were more likely than younger women to attend a fertility consultation is not surprising, given that women in the upper age range are more likely than younger women to become infertile after systemic therapy. However, because chemotherapy also reduces the fertility of younger women, and can render them completely infertile, it is important for health care professionals to ensure that younger women who choose to decline fertility consultation are making informed decisions. A significant number of women (25%) chose to forego the consult because they did not wish to delay their treatment. Rather than delay a routine discussion of fertility issues until the medical oncology consult, initiation of the discussion by either the nurse navigator or a member of the surgical team would help to eliminate that barrier to fertility preservation.
Several other findings from this study will be helpful for the pynk program. The lack of awareness on the part of a significant percentage of the patients about the availability of various formal support services—including peer support, psychology, psychiatry, social work, and the monthly “In the pynk” group meetings—suggests that greater attention has to be paid to informing patients about those services. It is quite conceivable that the patients received written or verbal information about them at some point in time, but that they were too anxious to pay attention to or to retain the information. Provision of information about those resources in more than one format (for example, as both written and verbal information) or at several points in time, or both, might be helpful.
The lack of awareness about pynk’s research studies on the part of approximately one third of the patients was surprising, in that all pynk patients are approached about one or more research studies. As with the support services, participation in research studies could be re-communicated to young women with breast cancer who initially decline (perhaps because they are initially too anxious); based on responses to our survey, young breast cancer patients as a group are very interested in participating in research focused on their age group.
Increasing attention is being paid to designing research studies that address gaps in the understanding of the optimal management of young breast cancer patients. The positive study by the International Breast Cancer Study Group aims to determine the safety of interrupting a woman’s adjuvant hormone therapy after 18 or 30 months so that she can have a baby. The multi-institutional pan-Canadian ruby study (Reducing the Burden of Breast Cancer in Young Women, http://www.womensresearch.ca/ruby-study), jointly funded by the Canadian Institutes of Health Research and the Canadian Breast Cancer Foundation, will create a prospective cohort of 1200 breast cancer patients, diagnosed at age 40 or younger and recruited over a period of 4 years, for whom extensive clinical data, stored blood, and tumour tissue will be available for current and future studies (pynk will be a major recruiter to ruby). Current ruby studies include the prevalence of mutations in genes other than BRCA among young breast cancer patients; effects of lifestyle factors on breast cancer recurrence; and factors that predict treatment-related infertility. Moreover, patient-reported outcomes, consisting of a broad range of psychosocial questionnaires, will be collected at baseline and at several follow-up intervals. Future research should include determining how the beneficial aspects of pynk can be adapted to smaller centres, in which a dedicated nurse navigator or a special program for young women with breast cancer (or both) is not practical.
CONCLUSIONS
The multifaceted pynk: Breast Cancer Program for Young Women initiative provides unique patient-centred care to breast cancer patients in the greater Toronto area. In the present study, we thoroughly evaluated patient satisfaction with pynk and found it to be high. The results of our study affirm the critical role of the nurse navigator in the program. Our study also showed that, in contrast to the literature showing low rates of health-care-initiated discussion of fertility issues with young cancer patients, pynk has been able to make such discussions “routine.”
It is most encouraging that, since the inception of pynk, several other centres worldwide have established specialized programs for young women with breast cancer. With the continual growth and development of pynk and programs like it, young breast cancer patients will be assured of receiving state-of-the art cancer care with optimal supports for themselves and for their families.
CONFLICT OF INTEREST DISCLOSURES
We have read and understood Current Oncology’s policy on disclosing conflict of interest, and we declare that we have none.
REFERENCES
- 1.Canadian Cancer Society’s Steering Committee on Cancer Statistics . Canadian Cancer Statistics 2014. Toronto, ON: Canadian Cancer Society; 2014. [Google Scholar]
- 2.Gelmon K, Partridge AH, Morrow M, Davidson NE. ASCO Educational Book 2005. Alexandria, VA: ASCO; 2005. Breast cancer in young women: epidemiology, treatment, and survivorship issues. In: American Society of Clinical Oncology (asco) pp. 61–7. [Google Scholar]
- 3.Shavers VH, Harlan LC, Stevens J. Racial/ethnic variation in clinical presentation, treatment, and survival among breast cancer patients under age 35. Cancer. 2003;97:134–47. doi: 10.1002/cncr.11051. [DOI] [PubMed] [Google Scholar]
- 4.Ali A, Warner E. pynk: breast cancer program for young women. Curr Oncol. 2013;20:34–9. doi: 10.3747/co.20.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Partridge A, Gelber S, Peppercorn J, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22:4174–83. doi: 10.1200/JCO.2004.01.159. [DOI] [PubMed] [Google Scholar]
- 6.Gould J, Grassau P, Manthorne J, Gray RE, Fitch MI. “Nothing fit me”: nationwide consultations with young women with breast cancer. Health Expect. 2006;9:158–73. doi: 10.1111/j.1369-7625.2006.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pedersen E, Hack T, McClement S, Taylor-Brown J. An exploration of the patient navigator role: perspectives of younger women with breast cancer. Oncol Nurs Forum. 2014;41:77–88. doi: 10.1188/14.ONF.77-88. [DOI] [PubMed] [Google Scholar]
- 8.Rehnberg G, Absetz P, Aro A. Women’s satisfaction with information at breast biopsy in breast cancer screening. Patient Educ Couns. 2001;42:1–8. doi: 10.1016/S0738-3991(99)00118-4. [DOI] [PubMed] [Google Scholar]
- 9.Davies NJ, Kinman G, Thomas RJ, Bailey T. Information satisfaction in breast and prostate cancer patients: implications for quality of life. Psychooncology. 2008;17:1048–52. doi: 10.1002/pon.1305. [DOI] [PubMed] [Google Scholar]
- 10.Husson O, Thong MS, Mols F, Oerlemans S, Kaptein AA, van de Poll-Franse LV. Illness perceptions in cancer survivors: what is the role of information provision? Psychooncology. 2013;22:490–8. doi: 10.1002/pon.3042. [DOI] [PubMed] [Google Scholar]
- 11.Harrison JD, Young JM, Price MA, Butow PN, Solomon MJ. What are the unmet supportive care needs of people with cancer? A systematic review. Support Care Cancer. 2009;17:1117–28. doi: 10.1007/s00520-009-0615-5. [DOI] [PubMed] [Google Scholar]
- 12.Peate M, Meiser B, Hickey M, Friedlander M. The fertility-related concerns, needs and preferences of younger women with breast cancer: a systematic review. Breast Cancer Res Treat. 2009;116:215–23. doi: 10.1007/s10549-009-0401-6. [DOI] [PubMed] [Google Scholar]
- 13.Stearns V, Schneider B, Henry NL, Hayes DF, Flockhart DA. Breast cancer treatment and ovarian failure: risk factors and emerging genetic determinants. Nat Rev Cancer. 2006;6:886–93. doi: 10.1038/nrc1992. [DOI] [PubMed] [Google Scholar]
- 14.Lee SJ, Schover LR, Partridge AH, et al. on behalf of the American Society of Clinical Oncology American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917–31. doi: 10.1200/JCO.2006.06.5888. [DOI] [PubMed] [Google Scholar]
- 15.Quinn GP, Vadaparampil ST, Lee JH, et al. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol. 2009;27:5952–7. doi: 10.1200/JCO.2009.23.0250. [DOI] [PubMed] [Google Scholar]
- 16.Goldfarb SB, Dickler MN, McCabe MS, et al. Oncology physicians’ knowledge, attitudes, and practices regarding fertility preservation [abstract e19525] J Clin Oncol. 2010;28 [Available online at: http://meetinglibrary.asco.org/content/47557-74; cited 22 November 2012] [Google Scholar]