Abstract
Study Objectives:
Examine the relationship between self-reported sleep parameters and indicators of resilience in a US military population (n = 55,021).
Methods:
Longitudinal analyses (2001–2008) were conducted using subjective data collected from Millennium Cohort Study questionnaires and objective data from military records that included demographics, military health, and deployment information. Subjective sleep duration and insomnia symptoms were collected on the study questionnaire. Resilience metrics included lost work days, self-rated health, deployment, frequency and duration of health care utilization, and early discharge from the military. Generalized estimating equations and survival analyses were adjusted for demographic, military, behavioral, and health covariates in all models.
Results:
The presence of insomnia symptoms was significantly associated with lower self-rated health, more lost work days, lower odds of deployment, higher odds of early discharge from military service early, and more health care utilization. Those self-reporting < 6 h (short sleepers) or > 8 h (long sleepers) of sleep per night had similar findings, except for the deployment outcome in which those with the shortest sleep were more likely to deploy.
Conclusions:
Poor sleep is a detriment to service members' health and readiness. Leadership should redouble efforts to emphasize the importance of healthy sleep among military service members, and future research should focus on the efficacy of interventions to promote healthy sleep and resilience in this population.
Commentary:
A commentary on this article appears in this issue on page 963.
Citation:
Seelig AD, Jacobson IG, Donoho CJ, Trone DW, Crum-Cianflone NF, Balkin TJ. Sleep and health resilience metrics in a large military cohort. SLEEP 2016;39(5):1111–1120.
Keywords: cohort, military, resilience, sleep
Significance.
This paper is the first to examine whether sleep, a modifiable factor, is predictive of resilience among a military population. We examined several outcomes that are indicators of resilience, including lost work days, self-rated health, deployment, early separation from the military, and healthcare utilization in relation to sleep duration and insomnia symptoms. Results showed that those reporting insomnia symptoms were less resilient. The relationship between resilience and sleep duration was less clear, but generally revealed a U-shaped association with both short and long sleepers less resilient than those sleeping 7 h per night. Recommendations include education on the effects of sleep on health, well-being, and operational readiness; and implementation of interventions designed to promote and maintain healthy sleep in this population.
INTRODUCTION
For many military service members, the past decade has been characterized by multiple deployments to combat zones, with multiple exposures to the considerable psychological and physical stressors that characterize asymmetric warfare. Accordingly, the military has become increasingly focused on enhancing resilience, “the mental, physical, emotional, and behavioral ability to face and cope with adversity, adapt to change, recover, learn, and grow from temporary setbacks” of service members.1 Although definitions of resilience can often infer one's ability to bounce back from a specific adverse event, the current programs the military employ are focused on being resilient to a number of adverse events ranging from major traumas to daily stressors. Programs such as the Army Resilience program have been developed as population-based prevention programs in which all soldiers are required to participate, and are aimed at teaching service members to be resilient to a number of potential stressors such as deployment, relationship problems, and daily hassles. One modifiable factor that may contribute to resilience among service members is sleep.
Military service men and women are especially prone to sleep loss and sleep disruption2–5 and this is likely due to the nature of military operations, which commonly require shiftwork and rapid deployment across multiple time zones and field training or sea duty (i.e., nonsleep- conducive environments), as well as potential comorbidities. Research among civilian populations suggests that long-term sleep restriction and/or sleep disruption are associated with many physical and psychological problems, including mood disturbances and other mental illness, metabolic syndrome/weight gain/obesity, diabetes, and heart disease as well as risk-taking behavior, emotional lability, and generally reduced levels of alertness and cognitive performance.6–14 Additionally, among military and veteran populations, poor sleep and insomnia have been associated with posttraumatic stress disorder (PTSD), pain, depression, mood, and hyper-tension4,5,15,16 Thus, promotion of healthy sleep has become a primary objective of Healthy People 2020, a program initiated by the US Department of Health and Human Services aimed at identifying and prioritizing the nation's leading health promotion and disease prevention goals.17 In addition, sleep has been afforded “equal billing” with exercise and nutrition as one of the three pillars of the US Army Surgeon General's public health campaign, the Performance Triad.18
The Millennium Cohort Study,19,20 a prospective study of mental and physical health among US service members that began in 2001, provides an important data source that allows the longitudinal investigation of the association between self-reported sleep parameters and a variety of health, behavioral, and career outcomes. Although a recent study revealed that 35% to 65% of military service members experience no symptoms, or only transient negative effects of deployment,21 previous analyses of Millennium Cohort data have revealed that predeployment reports of sleep disturbance are predictive of postdeployment mental health problems (e.g., PTSD, depression, anxiety).22 These findings suggest that although resilience to deployment-related stressors may be common for some service members, predeployment sleep disturbance constitutes a significant risk factor for postdeployment problems.
Findings from civilian epidemiological studies suggest a variety of factors associated with resilience, although the factors that determine individual resilience in a military population remain largely unknown. A study of civilians revealed that those who were resilient after personally experiencing the events of 9/11 were significantly less likely to be female, have depression, or use marijuana; were middle aged (45–54 y) and significantly more likely to be in the highest income group ($100,000+).23 Additionally, those with a history of trauma prior to 9/11 and those who experienced additional trauma or stressors after 9/11 were less likely to be resilient.23 Unfortunately, these studies did not account for sleep prior to a traumatic event or prior to the onset of psychological symptoms. Additionally, these studies took into account resilience among civilians following potentially traumatic events, such as the death of a family member or living in New York City on 9/11, but the experiences of US service members, especially those deployed to combat zones, are undoubtedly different. In addition to the stressful experiences of the general population such as financial problems, death of a loved one, illness, marital stress, and many others, military service members have additional stressors unique to deployments and combat exposure; and frequent moves that may involve long separations from family. In addition to these occupational experiences being stressful, they are frequently not controlled by the service member due to service time obligations.
Due to the diverse experiences of service members, resilience is difficult to measure. As such, the current study examined a diverse set of physical, psychological, and behavioral indicators of resilience as outcome measures to represent this multifaceted construct in a military population-based cohort.24 The hypotheses tested in this study are as follows: service members with the shortest sleep and those with insomnia symptoms are more likely to (A) report worse self-rated general health, (B) have more lost work days, (C) not deploy, (D) leave military service prior to completion of one's service term, and (E) have more healthcare visits and/or days hospitalized compared to those with healthy sleep patterns.
METHODS
Study Population
The study population consists of participants of the Millennium Cohort Study. Briefly, the Millennium Cohort Study includes men and women from all branches of military service, as well as Reservists and National Guardsmen, and follows these participants over time using questionnaires, even after they have left the military. Additional details regarding study methodology have been published elsewhere.19,20,25 Beginning in mid-2001, more than 200,000 military personnel on active service rosters were invited to participate in the first panel of the Millennium Cohort Study and 77,047 (36.0%) enrolled. After the initial enrollment of these participants, additional subjects were enrolled in subsequent panels, but only those subjects enrolled in the first panel who completed the first follow-up survey (n = 55,021) were eligible for the current analyses to allow for longitudinal modelling.
The variation in study samples for the models assessing general health (n = 50,425), lost work days (n = 51,622), and deployment (n = 52,021) is due to differences in the number missing each outcome. The study population for models examining separation from military (n = 22,196), medical visits (n = 10,190), and hospitalizations (n = 10,613) were restricted to active duty personnel as these data are incomplete for Reserve/Guard. Additionally, the medical outcome populations were further restricted to those who had completed three consecutive surveys to ensure equal follow-up time for these outcomes.
Sleep Measures
Sleep duration and insomnia symptoms were the independent variables for all hypotheses tested in this study. Both sleep measures were collected from the Millennium Cohort Study questionnaires. Sleep duration was determined with the question: “Over the past month, how many hours of sleep did you get in an average 24-h period?” Participants indicated their number of sleep hours in 1-h increments. The variable was categorized into five levels: < 6, 6, 7, 8, or > 8 h. The reference group was 7 h based on prior examinations of this cohort that found the majority of participants sleep 6–7 h per night, and based on prior research suggesting that 7 h is a healthy sleep duration for many people.4,22,26,27 Insomnia symptoms were assessed using questions from two validated instruments, the PRIME-MD Patient Health Questionnaire (PHQ) for anxiety screen and the PTSD Checklist–Civilian Version (PCL-C).28–33 The PHQ includes the item: “Over the last 4 weeks, how often have you experienced trouble falling asleep or staying asleep?” with three response options: “not at all,” “several days,” or “more than half the days.” The PCL-C includes the item: “In the past month, have you had trouble falling asleep or staying asleep?” with five response options: “not at all,” “a little bit,” “moderately,” “quite a bit,” or “extremely.” Participants with insomnia symptoms were defined as those who responded “moderately” or higher on the PCL-C sleep item or “several days” or more on the PHQ anxiety sleep item. Due to the different response options and skip patterns included in these questions, the two insomnia measures were combined, with participants categorized as having no insomnia symptoms (reference group), insomnia symptoms on one screening instrument, or insomnia symptoms on both screening instruments.4,22,34,35
For the main analyses, sleep duration and insomnia symptoms were assessed as two separate variables. In addition, sub-analyses were conducted to evaluate the combined effects of both measures. Sleep duration and insomnia symptoms were combined into five categories: healthy sleep (7–8 h and no insomnia symptoms), short sleep only (6 h or less per night and no insomnia), insomnia only (7–8 h of sleep and insomnia symptoms), short sleep and insomnia (6 h or less per night and insomnia), and long sleep (sleep greater than 8 h, with or without insomnia).
In addition to the independent variables of interest, sleep duration and insomnia symptoms, sleep apnea was also included in these models as a covariate. Sleep apnea was defined as an affirmative response of being told by a doctor or other medical professional that the study participant had the condition.
Resilience Outcome Measures
Several physical and mental variables were evaluated as indices of resilience.
Self-Rated General Health
Hypothesis A: Those who report short sleep or insomnia symptoms are more likely to have worse self-rated general health. Self-rated general health was assessed using a one-item question on the Medical Outcomes Study 36-Item Short Form Health Survey for Veterans36,37 (SF-36V): “In general, would you say your health is?”; response options were excellent, very good, good, fair, and poor. For these analyses, the response options were collapsed into excellent/very good, good, and fair/poor.38,39
Lost Work Days
Hypothesis B: Those who report short sleep or insomnia symptoms are more likely to have more lost work days. Lost work days were assessed using the Millennium Cohort survey question, “Over the past 3 years, approximately how many days were you unable to work or perform your usual activities because of illness or injury? (excluding lost time for pregnancy or childbirth).” The response options were none, 1 day, 2–5 days, 6–10 days, 11–15 days, 16–20 days, 21 days or more, and were categorized into four groups: none, 1–5 days (1 work week), 6–20 days (2–4 work weeks), 21+ days (more than 4 work weeks).
Deployment
Hypothesis C: Those who report short sleep or insomnia symptoms are less likely to deploy. Given that predeployment health assessments and training must be completed in order to be eligible for deployment, passing these assessments provides some assurance of nominal physical and mental fitness prior to deployment. The Defense Manpower Data Center (DMDC) provided electronic personnel files including in and out of theater deployment dates. Deployment (yes/no) was defined as deployment in support of the operations in Iraq and Afghanistan that occurred after enrollment in the Cohort.
Completion of Service Term
Hypothesis D: Those who report short sleep or insomnia symptoms are more likely to separate from the military prior to completing their service term. A service member may choose or be asked to leave service prior to the completion of their obligated term for a myriad of reasons. Thus, completing one's term suggests the individual was resilient to any obstacles causing early attrition (separation). DMDC provided electronic personnel files, including separation records. Separation from service was assessed among active duty participants only because the details regarding reasons for separation were limited to these individuals. Reasons for separation from service and corresponding dates were examined, and subjects were classified as either early separators or those who completed their service term or were still on active duty.
Health Care Utilization
Hypothesis E: Those who report short sleep or insomnia symptoms have more outpatient medical visits and/or longer hospitalization. The Military Health System Data Repository (MDR) provided electronic medical records for care received at military treatment facilities as well as claims billed through TRICARE, the health care benefit program used by active duty military members. As such, health care provided outside of the Military Health System for Reserve/National Guard members and veterans could not be completely captured, so this outcome was also assessed among only active duty subjects. Health care utilization was defined in two ways: cumulative number of days hospitalized and cumulative number of outpatient visits from 2001–2008 using dates provided in MDR inpatient and outpatient records.40,41 International Classification of Diseases, Ninth Edition Diagnostic codes 630–679 and 740–799, which include complications of pregnancy, childbirth or puerperium, congenital anomalies, perinatal issues, and symptoms, signs, and ill-defined conditions, were excluded from the outcomes.
Analytic Plan
Covariates
Several important demographic factors, military characteristics, and behavioral and health variables that may affect indices of resilience were examined in both the univariate and multivariable analyses described below.
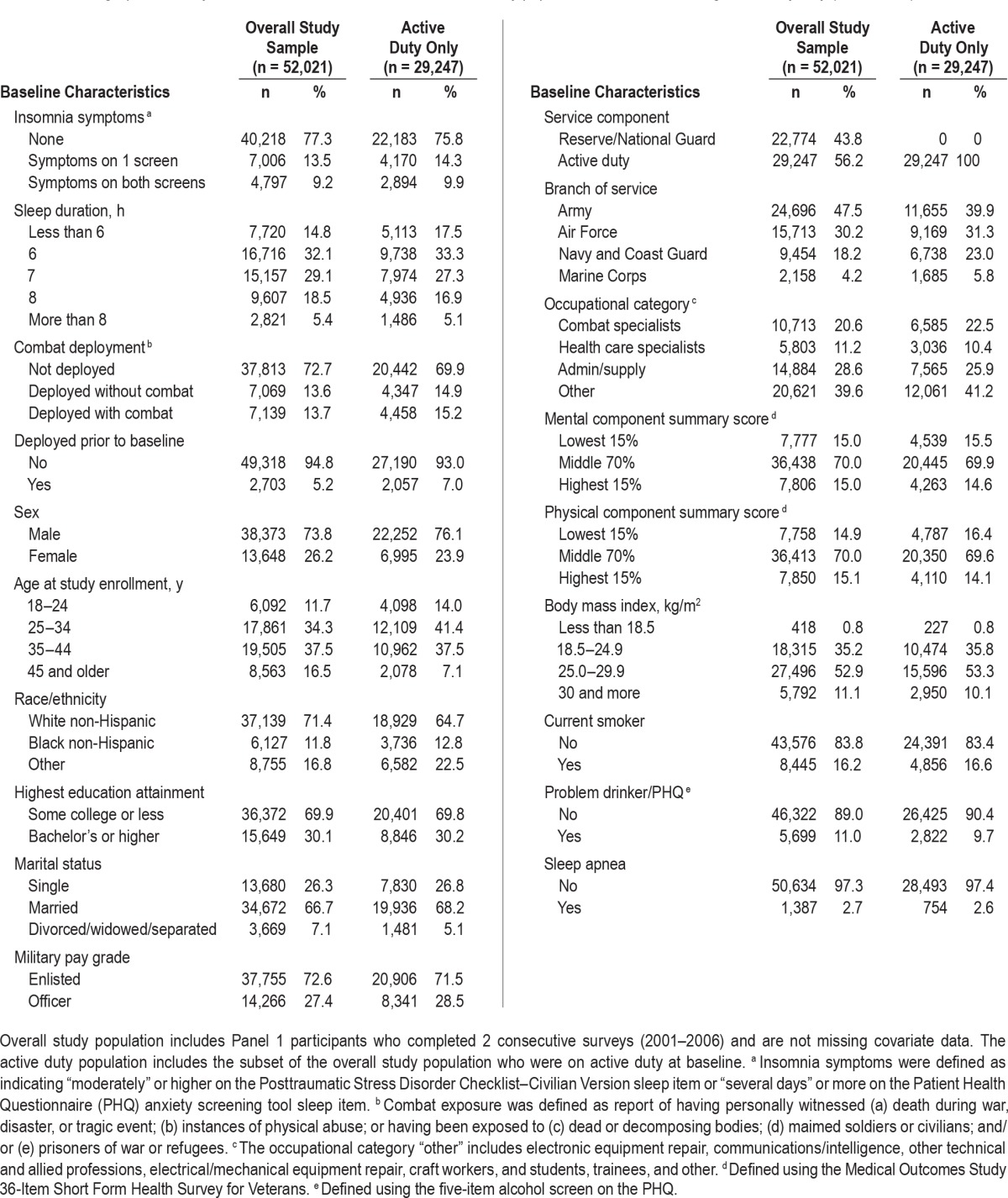
Demographic data (see Table 1 for categories) included sex, age at study enrollment, race/ethnicity, highest educational attainment, and marital status. Military-specific measures included service branch, pay grade, service component, deployment prior to study enrollment, combat deployment since enrollment, and military occupation. All of the demographics, as well as service branch, service component, pay grade, deployment dates, and military occupation were determined using DMDC records.
Table 1.
Demographic, military, behavioral, and health characteristics of study population: overall and among active duty only (2001–2008).
Combat exposure information was collected on the survey and defined as at least one report of having personally witnessed (1) death during war, disaster, or tragic event; (2) instances of physical abuse; or having been exposed to (3) dead or decomposing bodies, (4) maimed soldiers or civilians, and/ or (5) prisoners of war or refugees. These exposures were evaluated at the time of the postdeployment survey, and were determined to have occurred during the 3-y time frame overlapping their deployment.
Health and behavioral variables were collected from the survey. Current smokers were those who reported smoking at least 100 cigarettes in their lifetime and reported they had either not tried to quit or had been unsuccessful at quitting. Physical and mental component summary scores and self-rated general health were determined using the SF-36V. Problem drinking was collected from the PHQ 5-item measure of potential alcohol abuse, and was defined by at least one affirmative response to any of the five items indicating engagement in risky drinking behaviors more than one time over the past year.
Statistical Analysis
Univariate examinations of both sleep variables (sleep duration and insomnia symptoms) with each of the six study outcomes were conducted. Subsequently, multivariable, longitudinal modeling techniques that take into account within-subject correlation were used to examine the relationship between healthy sleep and each of the outcomes as described in the next paragraphs. For all models, the independent variables were measured at baseline and the outcome at the first follow-up. For participants who had additional follow-up, time-varying covariates were measured again at the first follow-up and the outcome was measured again at the second follow-up.
For hypotheses A (Poor sleep is associated with worse self-rated general health) and B (Poor sleep is associated with more lost work days), generalized estimating equations models were used with a cumulative logit distribution to accommodate the ordinal response categories, and the odds ratios represented inclusion in the next higher category, with very good/excellent self-rated health and no lost work days as the lowest categories. Sleep measures, covariates, number of lost work days, and self-rated health were allowed to vary over time in these models. Additionally, the self-rated health model included one additional variable, baseline general health, which contributed to the variation in the number of participants. The dichotomous outcome for hypothesis C (Poor sleep is associated with deployment) required generalized estimating equations with repeated measures to be employed to allow sleep measures, covariates, and deployment status to vary over time.
For hypothesis D (Poor sleep associated with leaving military service prior to completion of one's service term), Cox proportional hazards modeling was used for early separation because exact dates of separation were available. Person-days for each participant were calculated from the date of the baseline survey to the date of separation, or the last completed survey date for those remaining on active duty. Subjects were categorized as early separators if they left military service prior to completing their term of service and separated for a negative reason, such as alcoholism, unsatisfactory performance, disability, or misconduct. Early separators were compared with those who had completed their service obligation (retired or separated from service after completing their full service obligation) or if they remained on active duty. Individuals who were separated early for neutral or positive reasons (e.g., pregnancy, early release for school, homosexuality) were excluded from these models (n = 343). Hypothesis E (Poor sleep is associated with more outpatient medical visits and/or days of hospitalization) was examined using two separate outcomes of number of outpatient visits and number of days hospitalized. Generalized estimating equations with Poisson distribution were used to examine both outcomes in which relative risk estimates were interpreted as the percentage increase or decrease in number of outpatient visits or days hospitalized.
For the primary analyses, sleep duration and insomnia symptoms were entered into models as two separate time-varying independent variables, assessed at baseline and at the first follow-up. Sleep, combat deployment, smoking status, and problem drinking were included as time-varying covariates, and the remaining variables were fixed at baseline. Sub-analyses examining the combined effects of sleep duration and insomnia were performed in an identical manner, but the combined sleep variable was entered in place of the sleep duration and insomnia symptoms variables. Sample sizes for the adjusted models vary due to different numbers of missing outcome data. Data management and all statistical models were run using SAS (version 9.3, SAS Institute, Inc., Cary, NC, USA).
RESULTS
The demographic, military, behavioral, health, and sleep characteristics of the study populations are described in Table 1. The study population for models including both active duty and Reserve/Guard personnel had the following characteristics: 74% male, 46% under age 35 y at enrollment, 71% white/ non-Hispanic, 56% serving on active duty, 73% enlisted, and 27% of the population deployed, with about half of those deployed reporting combat exposures. Twenty-nine percent of the population reported sleeping 7 h per night, 23% reported insomnia symptoms on at least one screening tool, and 3% reported sleep apnea. Those participants included in the active duty only models [hypotheses D (separation from military service) and hypothesis E (health care utilization)] were nearly identical to the main study sample with respect to the characteristics measured in these analyses.
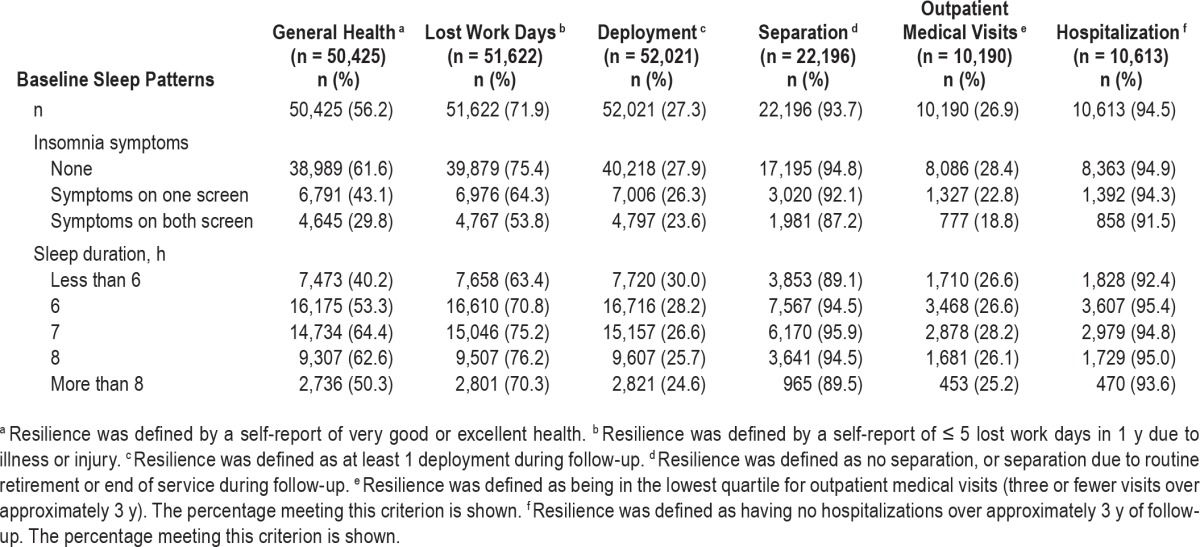
Table 2 shows the study population for each outcome modeled and the percentage in the most resilient group, by sleep characteristics. For each outcome, those with no insomnia symptoms had the highest proportion of participants in their respective resilient categories (e.g., very good or excellent health, no more than 5 days of lost work) and the percentage of individuals in the most resilient category decreased as the number of insomnia symptoms increased. Because there is no optimal number of outpatient visits, for the purposes of Table 2, the percentage of people who were in the lowest quartile for visits (three visits) is shown. For every outcome except deployment, the relationship between the most resilient group and hours of sleep constituted a U-shaped curve, with reduced resilience evident with both shorter and longer sleep durations. For the deployment model the relationship was linear, with the highest proportion of deployers reported sleeping less than 6 h per night, whereas the lowest proportion of deployers reported sleeping more than 8 h per night.
Table 2.
Baseline sleep characteristics and proportion meeting the resilience definition for each outcome.
Adjusted associations for the resilience metrics among the full study population (hypotheses A-C) are shown in Table 3. Sleep parameters were significantly associated with self-rated health, lost work days, and deployment. Results showed that those who reported insomnia symptoms on both screening tools had 44% lower odds of being in a higher category of better general health [odds ratio (OR): 0.56, 95% confidence interval (CI): 0.53, 0.59, hypothesis A], a 41% lower odds of being in a lower category of lost work days (OR: 0.59, 95% CI: 0.56, 0.62, hypothesis B), and 27% lower odds of deploying (OR: 0.73, 95% CI: 0.68, 0.78, hypothesis C) compared with those who did not report insomnia symptoms. Similar results, but with slightly smaller effect sizes, were found when comparing those with insomnia symptoms on one screening tool with those with no insomnia symptoms. This pattern of results was also consistent for those reporting sleep apnea. However, the sleep duration findings were less consistent for these outcomes. For general health, compared with those who reported sleeping 7 h, those who slept 6 h or less than 6 h, had 14% and 26% lower odds of being in a higher general health category (OR: 0.86, 95% CI: 0.83, 0.89 and OR: 0.74, 95% CI: 0.71, 0.78), respectively, and those who reported sleeping more than 8 h had 21% lower odds of being in a higher general health category (OR: 0.79, 95% CI: 0.74, 0.85). For lost work days, those who slept less than 6 h were less likely to report fewer lost work days (OR: 0.90, 95% CI: 0.86, 0.94), whereas those who slept 8 h were more likely to report fewer lost work days (OR: 1.11, 95% CI: 1.07, 1.16), compared with those who slept 7 h. However, compared with those sleeping 7 h, those sleeping 6 h or less than 6 h were 12% (OR: 1.12, 95% CI: 1.08, 1.17) and 27% (OR: 1.27, 95% CI: 1.21, 1.34) more likely to deploy, respectively. These results prompted us to determine the proportion of people who deployed within 90 days of reporting on their sleep duration and found that 41% of those who slept 6 h or less deployed within 90 days.
Table 3.
Adjusted odds of fewer lost work days, better general health, and deployment in relation to insomnia symptoms and sleep duration.
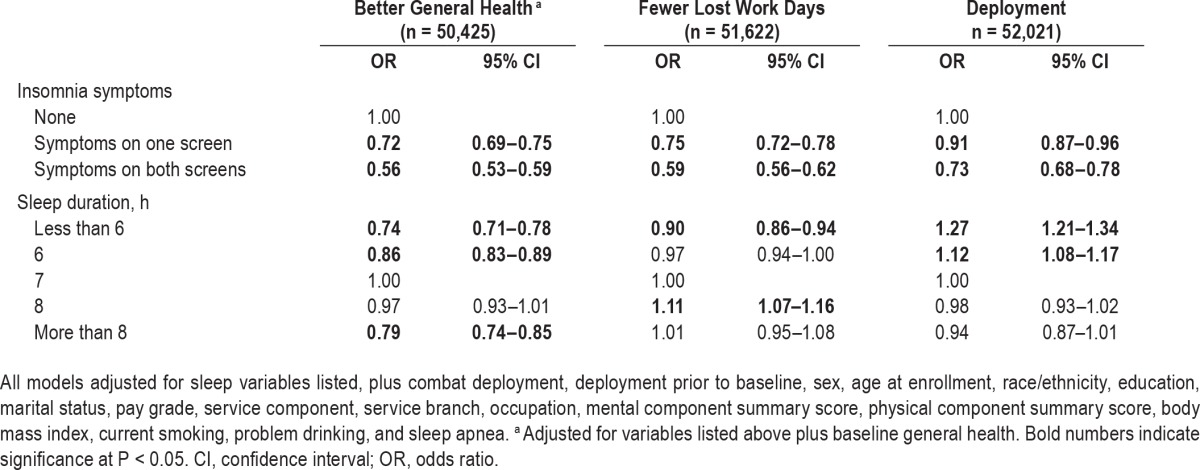
Table 4 presents the adjusted associations for the resilience indicators gathered on the active duty study population. Sleep parameters were significantly associated with early separation from the military, and the number of outpatient visits and days of hospitalization. For the early separation model (hypothesis D), those reporting insomnia symptoms on one scale were 25% more likely to separate early (hazard ratio [HR] 1.25, 95% CI, 1.08–1.45) than those with no insomnia symptoms, and those reporting symptoms on both scales were 78% more likely to separate early than those with no symptoms (HR 1.78, 95% CI, 1.52–2.08). Sleep duration was also associated with early separation. Compared with those reporting 7 h of sleep, participants sleeping less than 6 h per night had a 30% greater probability of separating early (HR 1.30, 95% CI, 1.10–1.55), and those sleeping 8 h or more than 8 h per night had a 27% (HR 1.27, 95% CI, 1.05–1.54) and 37% (HR 1.37, 95% CI, 1.07–1.77) higher probability of separating early, respectively. Sleep apnea was not associated with early separation.
Table 4.
Adjusted risk of outpatient medical visits, length of hospitalization and early separation from the military in relation to insomnia symptoms and sleep duration among active duty US service members.
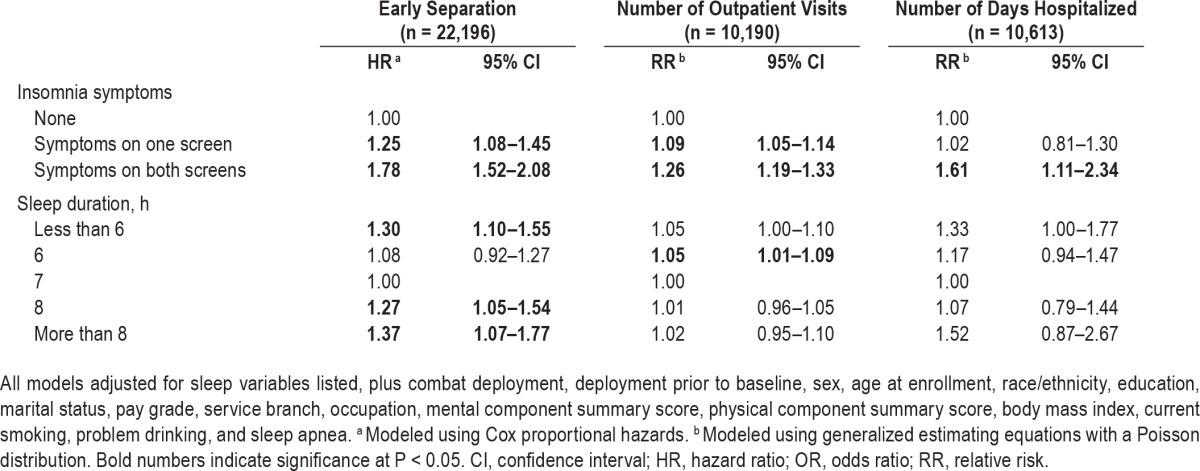
For the outpatient and hospitalization models (hypothesis E, Table 4), subjects with insomnia symptoms on both scales were more likely than those with no insomnia symptoms to have more outpatient medical visits (relative risk [RR] 1.26, 95% CI, 1.19–1.33) and were more likely to spend more days hospitalized (RR 1.61, 95% CI, 1.11–2.34), and those with symptoms on one scale were 9% more likely to have more outpatient medical visits (RR 1.09, 95% CI, 1.05–1.14). Additionally, those were 5% more likely to have more medical visits (RR 1.05, 95% CI, 1.01–1.09). Sleep apnea was not associated with number of days hospitalized, but was associated with a higher likelihood of outpatient visits (RR 1.19, 95% CI, 1.10–1.29). In the survival model, the proportional hazards assumption was met for all baseline covariates.
The subanalysis examining the combined effects of sleep duration and insomnia symptoms showed consistent results. Those who had short sleep duration (≤ 6 h) and insomnia symptoms were the least likely to be in the indicator for resilience category for all outcomes except deployment. Those who reported short sleep and insomnia were not significantly different from healthy sleepers in relation to deployment, and those who had short sleep only had the highest odds for deployment (results not shown).
DISCUSSION
Resilience encompasses mental, behavioral, and physical characteristics. Although sleep is associated with the development of medical conditions including mental disorders,2–12,22 it was previously unclear whether sleep characteristics play a role in resilience metrics. The current findings suggest that poor sleep is an important factor for health and is associated with a comprehensive set of measures that broadly reflect the hypothetical construct of resilience, including more lost work days, worse self-rated health, lower likelihood of deploying, early separation from the military, and more health care utilization.
Findings show that the majority of the population do not report any insomnia symptoms and report between 6 and 7 h of average nightly sleep. Moreover, a large proportion of these subjects meet the criteria for resilience set forth in this study. However, for each resilience indicator, those who reported insomnia symptoms were significantly less likely to be in the resilient category than those who did not report insomnia. This was also true for the small proportion of subjects reporting physician-diagnosed sleep apnea (∼3%), except there was no association between sleep apnea and days of hospitalization. It is notable that although sleep apnea was independently associated with nearly all of the resilience indices, the inclusion of this variable for adjustment in the models did not affect appreciably the magnitude, strength, or direction of the associations between the outcomes and insomnia symptoms or sleep duration.
The association between self-reported sleep duration and several measures of resilience was characterized by a U-shaped relationship: those who slept the least (less than 6 h) were less likely to have better self-rated health, fewer lost work days, and were more likely to have more medical visits and to separate from the military early or for a negative reason. Interestingly, however, those who slept 6 h or less than 6 h per night were also significantly more likely to deploy. This could be indicative of short sleep due to the increased workload that often comes with preparing for a deployment, rather than signifying sleep disturbance, especially given that those experiencing insomnia symptoms were less likely to deploy. We examined this possibility by determining the percentage of people who deployed within 90 days of submitting their survey by sleep duration categories and found that 22% of those reporting less than 6 h of sleep and 19% of those reporting 6 h of sleep hours deployed within 90 days, revealing that deployment was relatively imminent for 41% of short sleepers.
Findings for those sleeping more than 7 h per night were less consistent, but indicate that those who slept the longest were significantly less likely to have better health, more likely to miss work, or separate early from the military. The U-shaped distribution for these outcomes could be due to an underlying disorder such as depression or other mood disorder that was not fully accounted for by the inclusion of the mental component summary score in the models.42–44 The U-shaped distribution found in our study is similar to other outcomes in sleep research, including mortality.26,27 One consideration for military personnel is that many aspects of military life are beyond the control of the military member; for example, frequent moves (often every 2–3 y), deployments, training schedules, or occupation changes that can directly or indirectly affect the number of hours available for sleep.4,45 Additionally, a culture that lauds short sleep as a sign of increased stamina or toughness may contribute to the high proportion of short sleepers, especially in relation to the deployment outcome, as military personnel may be sleeping less as required by their predeployment training and scheduling, and also they may be choosing to sleep less as a signal to others that they are tough and ready for deployment.46
The current study has several notable strengths. First, the Millennium Cohort Study participants represent all branches of the military and both active duty and Reserve/Guard personnel. Thorough evaluations of possible biases suggest the cohort is representative of military personnel in terms of demographic and mental health characteristics and reliable health and exposure reporting.20,47–53 Another strength is its longitudinal design, with 7 y of follow-up, facilitating the ability to assess the associations between sleep and resilience metrics both within and between individuals. Moreover, the use of six different outcome measures provided a relatively comprehensive representation of resilience in a military population. Last, this study utilized two measures of sleep: average hours of sleep (quantity) and symptoms of insomnia (quality) over time.
Despite its strengths, the present study also has several important limitations. First, a standardized measure of resilience was not employed. Although standardized resilience scales are fairly new and their validity is still uncertain, especially among a military population, future research with military populations should use standardized scales if possible. Standardized resilience metrics will better allow cross-study comparisons and development of general principles related to resilience. The sleep measures included were self-reported and not verified through actigraphy; hence, it is possible that actual sleep times differed from those reported.54 In addition, sleep patterns over the past month were reported on the survey and may not be indicative of usual sleep during the entirety of each 3-y period between surveys. Last, the study sample was limited to active duty service members for some of the analyses; as such, the conclusions with regard to outpatient visits, hospitalizations, and early separation from the military may not be generalizable to Reservists and National Guardsmen.
In summary, the findings from this longitudinal study underscore the integral role of sleep as a modifiable predictor of resilience indices in military personnel, a relationship that is likely to generalize broadly to both military and civilian populations and their respective operational environments. Although causal relationships were not determined in the current study, one implication of these findings is that interventions that improve the sleep of individuals in operational environments may pay significant long-term dividends in terms of individual well-being, efficient use of military training dollars, and attendant organizational strength and readiness, a possibility that should be explored in future studies.
DISCLOSURE STATEMENT
This was not an industry supported study. The Millennium Cohort Study is funded through the Military Operational Medicine Research Program of the US Army Medical Research and Materiel Command, Fort Detrick, Maryland, and the Bureau of Medicine and Surgery, under Work Unit No. 60002. The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of the Army, Department of Defense, Department of Veterans Affairs, or the US Government. Approved for public release; distribution is unlimited. US Government Work (17 USC 105). Not copyrighted in the US. This research has been conducted in compliance with all applicable federal regulations governing the protection of human subjects in research (Protocol NHRC.2000.0007). The authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- BMI
body mass index
- DMDC
Defense Manpower Data Center
- MDR
Military Health Service Data Repository
- PCL-C
PTSD Checklist–Civilian Version
- PHQ
Patient Health Questionnaire
- PTSD
posttraumatic stress disorder
- SF-36V
Medical Outcomes Study 36-Item Short Form Health Survey for Veterans
REFERENCES
- 1.Ready and Resilient (R2) [Accessed 12/5/2014]. http://garrison.leavenworth.army.mil/Who-We-Are/Ready-and-Resilient.aspx.
- 2.Ulmer CS, Van Voorhees E, Germain AE, et al. A comparison of sleep difficulties among Iraq/Afghanistan theater veterans with and without mental health diagnoses. J Clin Sleep Med. 2015;11:995–1005. doi: 10.5664/jcsm.5012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med. 2008;173:230–5. doi: 10.7205/milmed.173.3.230. [DOI] [PubMed] [Google Scholar]
- 4.Seelig AD, Jacobson IG, Smith B, et al. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33:1615–22. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mysliwiec V, McGraw L, Pierce R, Smith P, Trapp B, Roth BJ. Sleep disorders and associated medical comorbidities in active duty military personnel. Sleep. 2013;36:167–74. doi: 10.5665/sleep.2364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Santhi N, Horowitz TS, Duffy JF, Czeisler CA. Acute sleep deprivation and circadian misalignment associated with transition onto the first night of work impairs visual selective attention. PLoS One. 2007;2:e1233. doi: 10.1371/journal.pone.0001233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1:e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kendall AP, Kautz MA, Russo MB, Killgore WDS. Effects of Sleep Deprivation on Lateral Visual Attention. Int J Neurosci. 2006;116:1125–38. doi: 10.1080/00207450500513922. [DOI] [PubMed] [Google Scholar]
- 9.Killgore WDS, Balkin TJ, Wesensten NJ. Impaired decision making following 49 h of sleep deprivation. J Sleep Res. 2006;15:7–13. doi: 10.1111/j.1365-2869.2006.00487.x. [DOI] [PubMed] [Google Scholar]
- 10.Dinges DF, Pack F, Williams K, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep. 1997;20:267–77. [PubMed] [Google Scholar]
- 11.Basner M, Rubinstein J, Fomberstein KM, et al. Effects of night work, sleep loss and time on task on simulated threat detection performance. Sleep. 2008;31:1251–9. [PMC free article] [PubMed] [Google Scholar]
- 12.McKenna BS, Dicjinson DL, Orff HJ, Drummond SP. The effects of one night of sleep deprivation on known-risk and ambiguous-risk decisions. J Sleep Res. 2007;16:245–52. doi: 10.1111/j.1365-2869.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- 13.Singh M, Drake CL, Roehrs T, Hudgel DW, Roth T. The association between obesity and short sleep duration: a population-based study. J Clin Sleep Med. 2005;1:357–63. [PubMed] [Google Scholar]
- 14.Chaput JP, Despres JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31:517–23. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jenkins MM, Colvonen PJ, Norman SB, Afari N, Allard CB, Drummond SP. Prevalence and mental health correlates of insomnia in first-encounter veterans with and without military sexual trauma. Sleep. 2015;38:1547–54. doi: 10.5665/sleep.5044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ulmer CS, Bosworth HB, Germain A, et al. Associations between sleep difficulties and risk factors for cardiovascular disease in veterans and active duty military personnel of the Iraq and Afghanistan conflicts. J Behav Med. 2015;38:544–55. doi: 10.1007/s10865-015-9627-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U S Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020. [Accessed September 22, 2014]. http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=38. [PubMed]
- 18.Office of the Surgeon General Public Affairs. Army Medicine Launches Performance Triad Pilot Program. [Accessed September 22, 2014]. http://www.army.mil/article/111317/Army_Medicine_launches_Performance_Triad_Pilot_Program/
- 19.Gray GC, Chesbrough KB, Ryan MA, et al. The Millennium Cohort Study: a 21-year prospective cohort study of 140,000 military personnel. Mil Med. 2002;167:483–8. [PubMed] [Google Scholar]
- 20.Ryan MA, Smith TC, Smith B, et al. Millennium Cohort: enrollment begins a 21-year contribution to understanding the impact of military service. J Clin Epidemiol. 2007;60:181–91. doi: 10.1016/j.jclinepi.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 21.Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Ann Rev Clin Psychol. 2011;7:511–35. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- 22.Gehrman P, Seelig AD, Jacobson IG, et al. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep. 2013;36:1009–18. doi: 10.5665/sleep.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bonanno GA, Galea S, Bucciarelli A, Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J Consult Clin Psychol. 2007;75:671–82. doi: 10.1037/0022-006X.75.5.671. [DOI] [PubMed] [Google Scholar]
- 24.Ready and Resilient. [Accessed October 14, 2015]. http://www.army.mil/readyandresilient.
- 25.Jacobson IG, Ryan MA, Hooper TI, et al. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA. 2008;300:663–75. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 27.Kripke DF, Langer RD, Elliott JA, Klauber MR, Rex KM. Mortality related to actigraphic long and short sleep. Sleep Med. 2011;12:28–33. doi: 10.1016/j.sleep.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 29.Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183:759–69. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- 30.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272:1749–56. [PubMed] [Google Scholar]
- 31.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weathers FW, Litz BT. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. Paper presented at: 9th Annual Meeting of the International Society for Traumatic Stress Studies; 1993; San Antonio, Texas. S. HD. [Google Scholar]
- 33.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34:669–73. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 34.Boyko EJ, Seelig AD, Jacobson IG, et al. Sleep characteristics, mental health, and diabetes risk: a prospective study of U.S. military service members in the Millennium Cohort Study. Diabetes Care. 2013;36:3154–61. doi: 10.2337/DC13-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams EC, Frasco MA, Jacobson IG, et al. Risk factors for relapse to problem drinking among current and former US military personnel: a prospective study of the Millennium Cohort. Drug Alcohol Depend. 2015;148:93–101. doi: 10.1016/j.drugalcdep.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 36.Stewart AL, Hays RD, Ware JE., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Med Care. 1988;26:724–35. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 37.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 38.Crimmins EM, Kim JK, Sole-Auro A. Gender differences in health: results from SHARE, ELSA and HRS. Eur J Public Health. 2011;21:81–91. doi: 10.1093/eurpub/ckq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nishi A, Kawachi I, Shirai K, Hirai H, Jeong S, Kondo K. Sex/gender and socioeconomic differences in the predictive ability of self-rated health for mortality. PLoS One. 2012;7:e30179. doi: 10.1371/journal.pone.0030179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wells TS, Jacobson IG, Smith TC, et al. Prior health care utilization as a potential determinant of enrollment in a 21-year prospective study, the Millennium Cohort Study. Eur J Epidemiol. 2008;23:79–87. doi: 10.1007/s10654-007-9216-0. [DOI] [PubMed] [Google Scholar]
- 41.White MR, Jacobson IG, Smith B, et al. Health care utilization among complementary and alternative medicine users in a large military cohort. BMC Complement Altern Med. 2011;11:27. doi: 10.1186/1472-6882-11-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kripke DF, Brunner R, Freeman R, et al. Sleep Complaints of Postmenopausal Women. Clin J Womens Health. 2001;1:244–52. doi: 10.1053/cjwh.2001.30491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Watson NF, Harden KP, Buchwald D, et al. Sleep duration and depressive symptoms: a gene-environment interaction. Sleep. 2014;37:351–8. doi: 10.5665/sleep.3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaplan KA, Harvey AG. Hypersomnia across mood disorders: a review and synthesis. Sleep Med Rev. 2009;13:275–85. doi: 10.1016/j.smrv.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 45.Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34:1189–95. doi: 10.5665/SLEEP.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miller NL, Shattuck LG. Sleep patterns of young men and women enrolled at the United States Military Academy: results from year 1 of a 4-year longitudinal study. Sleep. 2005;28:837–41. doi: 10.1093/sleep/28.7.837. [DOI] [PubMed] [Google Scholar]
- 47.Riddle JR, Smith TC, Smith B, et al. Millennium Cohort: the 2001-2003 baseline prevalence of mental disorders in the U.S. military. J Clin Epidemiol. 2007;60:192–201. doi: 10.1016/j.jclinepi.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 48.Smith B, Leard CA, Smith TC, Reed RJ, Ryan MA. Anthrax vaccination in the Millennium Cohort: validation and measures of health. Am J Prev Med. 2007;32:347–53. doi: 10.1016/j.amepre.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 49.Smith B, Smith TC, Gray GC, Ryan MA. When epidemiology meets the Internet: web-based surveys in the Millennium Cohort Study. Am J Epidemiol. 2007;166:1345–54. doi: 10.1093/aje/kwm212. [DOI] [PubMed] [Google Scholar]
- 50.Smith B, Wingard DL, Ryan MA, Macera CA, Patterson TL, Slymen DJ. U.S. military deployment during 2001-2006: comparison of subjective and objective data sources in a large prospective health study. Ann Epidemiol. 2007;17:976–82. doi: 10.1016/j.annepidem.2007.07.102. [DOI] [PubMed] [Google Scholar]
- 51.Smith TC, Jacobson IG, Smith B, Hooper TI, Ryan MA, Team FT. The occupational role of women in military service: validation of occupation and prevalence of exposures in the Millennium Cohort Study. Int J Environ Health Res. 2007;17:271–84. doi: 10.1080/09603120701372243. [DOI] [PubMed] [Google Scholar]
- 52.Smith TC, Smith B, Jacobson IG, Corbeil TE, Ryan MA for the Millennium Cohort Study Team. Reliability of standard health assessment instruments in a large, population-based cohort study. Ann Epidemiol. 2007;17:525–32. doi: 10.1016/j.annepidem.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 53.LeardMann CA, Smith B, Smith TC, Wells TS, Ryan MA. Smallpox vaccination: comparison of self-reported and electronic vaccine records in the millennium cohort study. Hum Vaccin. 2007;3:245–51. doi: 10.4161/hv.4589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gehrman P, Matt GE, Turingan M, Dinh Q, Ancoli-Israel S. Towards an understanding of self-reports of sleep. J Sleep Res. 2002;11:229–36. doi: 10.1046/j.1365-2869.2002.00306.x. [DOI] [PubMed] [Google Scholar]


