Abstract
Influenza vaccination is an effective strategy to reduce morbidity and mortality, particularly for those who have decreased lung functions. This study was to identify the factors that affect vaccination coverage according to the results of pulmonary function tests depending on the age. In this cross-sectional study, data were obtained from 3,224 adults over the age of 40 who participated in the fifth National Health and Nutrition Examination Survey and underwent pulmonary function testing in 2012. To identify the factors that affect vaccination rate, logistic regression analysis was conducted after dividing the subjects into two groups based on the age of 65. Influenza vaccination coverage of the entire subjects was 45.2%, and 76.8% for those aged 65 and over. The group with abnormal pulmonary function had a higher vaccination rate than the normal group, but any pulmonary dysfunction or history of COPD did not affect the vaccination coverage in the multivariate analysis. The subjects who were 40-64 years-old had higher vaccination coverage when they were less educated or with restricted activity level, received health screenings, and had chronic diseases. Those aged 65 and over had significantly higher vaccination coverage only when they received regular health screenings. Any pulmonary dysfunction or having COPD showed no significant correlation with the vaccination coverage in the Korean adult population.
Keywords: Influenza; Vaccination; Respiratory Function Test; Respiratory Disease, Chronic Obstructive
Graphical Abstract
INTRODUCTION
Influenza infection increases the incidence of complications and mortality in people with a weak immune system or chronic diseases. However, the coverage of influenza vaccine at the time of influenza spreading significantly reduced morbidity and mortality due to influenza infection (1). Influenza vaccination is cost-effective (2) and safe (3), and is known to reduce unnecessary hospitalization due to influenza infection in the elderly and cardiopulmonary disease patients (4,5). Vaccination is strongly recommended for the patients with emphysema, chronic bronchitis and asthma, who can experience acute exacerbation of symptoms.
To increase influenza vaccination coverage for the people with decreased pulmonary function due to respiratory diseases or smoking, it is essential to research on the actual vaccination status and factors affecting it. In Korea, influenza vaccination is provided free of charge for adults age 65 or higher. This strategy can affect vaccination coverage according to age groups, but has never been considered as a relevant factor in the past. Previous studies were on influenza vaccination status only in elderly over 65 years of age (6), and factors affecting influenza vaccination coverage in adults over 18 years (7). A recent study analyzed what affects influenza vaccination coverage in adults under 65 years of age based on national health and nutrition survey (8), but there was no study comparing the vaccination coverage in relation to pulmonary functions. Therefore, the purpose of this study was to analyze the actual vaccination status of the people with decreased pulmonary functions who are vulnerable to influenza infection, among Korean adults over the age of 40, according to the type of their lung dysfunction. In addition, we compared the factors that affect vaccination uptake in different age groups that are divided by the age of 65.
MATERIALS AND METHODS
Study participants
We used data from the Korean National Health and Nutrition Survey (KNHANES) in 2012. The KNHANES is an annual survey to assess health conditions, health related behaviors, and the nutritional status of Korean people. Multi-stage stratified sampling method was used to make it represent Korean people's health and nutrition level in the survey. The data needed for this study was analyzed after getting the approval to use the raw data through the National Health and Nutrition Survey website (9).
Among the 8,058 subjects in the 2012 KNHANES, we selected adults over the age of 40 who underwent pulmonary function test. Those whose results of pulmonary function test were missing (n = 1,109) and those whose results showed to be undeterminable including mixed pulmonary dysfunction (n = 68) were excluded. When variables on influenza vaccination were missing (n = 62) and the subjects did not know whether they had been vaccinated (n = 39), their data were also excluded from the study; finally 3,224 subjects (1,347 males, 1,877 females) were selected for this study.
Variable measurement
Influenza vaccination was assessed by the question ‘Have you ever received the influenza vaccination for last 12 months?’ If the answer was ‘yes’, they were considered to have received the influenza vaccination. The results of pulmonary function test, and chronic obstructive pulmonary disease diagnosis were included as independent variables. Pulmonary dysfunction was classified into normal, restrictive, and obstructive pattern according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification (10).
Socio-demographic characteristics such as gender, age, residential neighborhoods, administrative area, marital status, education level, and income level were included as covariates. Health behaviors, such as smoking and regular health screening were selected. Presence of comorbid conditions including hypertension, diabetes, dyslipidemia, myocardial infarction or angina, tuberculosis, asthma, chronic renal failure and cancer, self-perceived health status recognition, and activity limitation were also selected as covariates.
Residential neighborhoods were divided into major cities including Seoul and 6 major metropolitan areas and others. Administrative district was divided into dong and eup/myeon. Level of education was classified into less than middle school, high school graduates, and more than college graduates. Total household income was categorized into quartiles (low, mid-low, mid-high, and high). Smoking status was classified as smoker (both current and past smoker) and non-smoker. Self-perceived health status was classified into two levels according to the responses to the question “How do you assess your own health status?” One included those who answered as very good, good, or average; the other included those who responded as poor or very poor. Chronic diseases including hypertension, diabetes, dyslipidemia, ischemic heart disease, pulmonary tuberculosis, asthma, chronic renal failure and any cancers diagnosed by physicians were questioned. If a participant said ‘yes’ to any kinds of chronic disease, he or she was regarded as having the chronic disease. KNHANES was conducted after receiving approval by the institutional review board of Korean Centers for Disease Control and Prevention (2012-01EXP-01-2C).
Statistical analysis
We performed the descriptive analysis for influenza vaccination coverage considering sample weighting (wt_pft) to minimize selection errors. χ2 test was used to compare the vaccination coverage in each variable. Logistic regression analysis was used to analyze the vaccination coverage adjusting for socio-demographic variables, health behavior variables, co-morbidities status, screening results and diagnosis of chronic obstructive pulmonary disease. Unadjusted and adjusted odds ratios (OR) and 95% confidence intervals (CI) were presented. As adults aged 65 and over receive free influenza vaccination through the national immunization program for elderly every year, the vaccination coverage was expected to differ from other age groups; subjects were divided into two groups based on the age of 65, and the results were compared. SAS Enterprise Guide Version 5.1 (SAS Institute Inc., Cary, NC, USA) was used for all statistical analysis. It was determined that there was a statistically significant difference when the P value was < 0.05.
Ethics statement
This study was conducted under approval by the institutional review board of Korean Centers for Disease Control and Prevention for KNHANES (2012-01EXP-01-2C). Informed consent was exempted by the board.
RESULTS
General characteristics and vaccination coverage
There were 1,347 males and 1,877 females among the subjects, and 1,013 elderly (31.4%) were in the age 65 years or older. Influenza vaccination coverage was 40.2% in the whole subjects and 78.3% among the elderly in the age 65 years or older group. When we compared the vaccinated and the unvaccinated, a significant difference in all characteristics except for marital status and tuberculosis history were noted. For those who were females, over 65 years of age, living in the areas other than metropolis, living in eup/myeon, with the lower the level of education or household income, non-smokers, with recognition of self-perceived health status as poor, receiving regular health checkup, with activity restricted, with history of chronic diseases except tuberculosis, influenza vaccination coverage was significantly higher. Influenza vaccination rate was also higher among those who had abnormal lung function and had COPD (Table 1). Notably, those who had COPD were only 0.6% of the subjects, although nearly a quarter of the subjects had abnormal lung function either restrictive or obstructive.
Table 1. Influenza vaccination coverage rates according to the characteristics of respondents in 2012 KNHANES.
| Parameters | Unweighted frequency (estimated proportion %) | P | |
|---|---|---|---|
| Vaccinated (n = 1,458) | Unvaccinated (n = 1,766) | ||
| Gender | < 0.001 | ||
| Male | 560 (35.3) | 787 (64.7) | |
| Female | 898 (44.7) | 979 (55.3) | |
| Age | < 0.001 | ||
| 40-64 | 680 (28.0) | 1531 (72.0) | |
| ≥ 65 | 778 (78.3) | 235 (21.7) | |
| Residential neighborhood | 0.005 | ||
| Metropolis | 633 (36.1) | 848 (63.9) | |
| Others | 825 (43.7) | 918 (56.3) | |
| Administrative areas | 0.016 | ||
| Dong | 1,097 (38.0) | 1,420 (62.0) | |
| Eup/Myeon | 361 (47.6) | 346 (52.4) | |
| Marital status | 0.075 | ||
| Married | 1,447 (40.6) | 1,737 (59.4) | |
| Unmarried | 10 (22.6) | 29 (77.4) | |
| Education level | < 0.001 | ||
| ≤ Middle school | 902 (55.7) | 627 (44.3) | |
| High school | 351 (30.1) | 638 (69.9) | |
| ≥ College | 202 (24.9) | 496 (75.1) | |
| Household income level | < 0.001 | ||
| Low | 431 (62.5) | 223 (37.5) | |
| Middle low | 402 (44.3) | 419 (55.7) | |
| Middle high | 296 (32.7) | 477 (67.3) | |
| High | 312 (28.2) | 624 (71.8) | |
| Smoking | < 0.001 | ||
| Current or former smokers | 528 (35.6) | 737 (64.4) | |
| Nonsmokers | 930 (44.1) | 1,029 (55.9) | |
| Self-perceived health status | < 0.001 | ||
| Average or better | 1,086 (37.4) | 1,485 (62.6) | |
| Poor | 371 (51.8) | 281 (48.2) | |
| Regular health check-up | 0.001 | ||
| Yes | 1,100 (43.1) | 1,177 (56.9) | |
| No | 357 (34.5) | 589 (65.5) | |
| Restricted activity | < 0.001 | ||
| Yes | 210 (58.4) | 122 (41.6) | |
| No | 1,245 (38.1) | 1,643 (61.9) | |
| Chronic diseases | |||
| Hypertension | < 0.001 | ||
| Yes | 627 (57.8) | 394 (42.2) | |
| No | 831 (33.4) | 1,372 (66.6) | |
| Diabetes | < 0.001 | ||
| Yes | 214 (57.9) | 134 (42.1) | |
| No | 1,244 (38.4) | 1,632 (61.6) | |
| Dyslipidemia | < 0.001 | ||
| Yes | 348 (57.0) | 204 (43.0) | |
| No | 1,110 (37.4) | 1,562 (62.6) | |
| Myocardial infarction or angina | < 0.001 | ||
| Yes | 95 (68.2) | 41 (31.8) | |
| No | 1,363 (39.2) | 1,725 (60.8) | |
| Pulmonary tuberculosis | 0.188 | ||
| Yes | 77 (33.7) | 101 (66.3) | |
| No | 1,381 (40.6) | 1,665 (59.4) | |
| Asthma | 0.042 | ||
| Yes | 80 (50.9) | 53 (49.1) | |
| No | 1,378 (39.8) | 1,713 (60.2) | |
| Chronic renal failure | 0.033 | ||
| Yes | 18 (64.3) | 10 (35.7) | |
| No | 1,440 (40.1) | 1,756 (59.9) | |
| Cancer | 0.005 | ||
| Yes | 101 (55.1) | 65 (44.9) | |
| No | 1,357 (39.6) | 1,701 (60.4) | |
| COPD | 0.035 | ||
| Yes | 14 (69.0) | 5 (31.0) | |
| No | 1,443 (40.1) | 1,760 (59.9) | |
| Pulmonary function | < 0.001 | ||
| Normal | 996 (37.1) | 1,380 (62.9) | |
| Restrictive | 169 (43.4) | 177 (56.6) | |
| Obstructive | 293 (53.8) | 209 (46.2) | |
KNHANES, Korean National Health and Nutrition Survey; COPD, chronic obstructive pulmonary diseases.
Influenza vaccination coverage according to the pulmonary function and COPD diagnosis
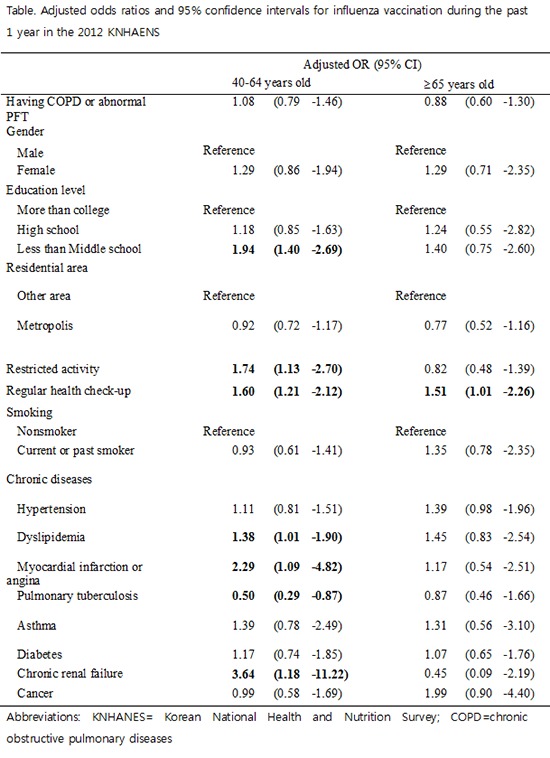
Because there were few subjects who were diagnosed with COPD by doctors, they were combined with those who had abnormal lung function and analyzed. Influenza vaccination coverage was not related to having COPD or abnormal lung function in both younger (40-64 years old) and elderly (65 years or older) population. Multiple logistic regression analysis showed similar results (Table 2).
Table 2. Unadjusted and adjusted odds ratios and 95% confidence intervals for influenza vaccination during the past 1 year in the 2012 KNHANES.
| Variables | 40-64 yr old | ≥ 65 yr old | ||
|---|---|---|---|---|
| UOR (95% CI) | AOR (95% CI) | UOR (95% CI) | AOR (95% CI) | |
| Having COPD or abnormal PFT | 1.13 (0.84-1.51) | 1.08 (0.79-1.46) | 0.85 (0.61-1.19) | 0.88 (0.60-1.30) |
| Gender | ||||
| Male | Reference | Reference | Reference | Reference |
| Female | 1.41 (1.12-1.77) | 1.29 (0.86-1.94) | 1.19 (0.85-1.67) | 1.29 (0.71-2.35) |
| Education level | ||||
| More than college | Reference | Reference | Reference | Reference |
| High school | 1.24 (0.91-1.68) | 1.18 (0.85-1.63) | 1.31 (0.60-2.89) | 1.24 (0.55-2.82) |
| Less than middle school | 2.33 (1.70-3.18) | 1.94 (1.40-2.69) | 1.43 (0.79-2.59) | 1.40 (0.75-2.60) |
| Residential area | ||||
| Other area | Reference | Reference | Reference | Reference |
| Metropolis | 0.82 (0.64-1.04) | 0.92 (0.72-1.17) | 0.78 (0.52-1.17) | 0.77 (0.52-1.16) |
| Restricted activity | 2.18 (1.43-3.33) | 1.74 (1.13-2.70) | 0.86 (0.51-1.44) | 0.82 (0.48-1.39) |
| Regular health check-up | 1.58 (1.20-2.10) | 1.60 (1.21-2.12) | 1.51 (1.03-2.22) | 1.51 (1.01-2.26) |
| Smoking | ||||
| Nonsmoker | Reference | Reference | Reference | Reference |
| Current or past smoker | 0.74 (0.59-0.93) | 0.93 (0.61-1.41) | 1.04 (0.74-1.46) | 1.35 (0.78-2.35) |
| Chronic diseases | ||||
| Hypertension | 1.53 (1.17-2.01) | 1.11 (0.81-1.51) | 1.46 (1.03-2.08) | 1.39 (0.98-1.96) |
| Dyslipidemia | 1.80 (1.33-2.43) | 1.38 (1.01-1.90) | 1.65 (0.97-2.81) | 1.45 (0.83-2.54) |
| Myocardial infarction or angina | 2.82 (1.30-6.13) | 2.29 (1.09-4.82) | 1.24 (0.58-2.65) | 1.17 (0.54-2.51) |
| Pulmonary tuberculosis | 0.53 (0.31-0.90) | 0.50 (0.29-0.87) | 0.77 (0.42-1.43) | 0.87 (0.46-1.66) |
| Asthma | 1.56 (0.85-2.84) | 1.39 (0.78-2.49) | 1.17 (0.50-2.70) | 1.31 (0.56-3.10) |
| Diabetes | 1.66 (1.09-2.53) | 1.17 (0.74-1.85) | 1.25 (0.77-2.02) | 1.07 (0.65-1.76) |
| Chronic renal failure | 4.92 (1.46-16.50) | 3.64 (1.18-11.22) | 0.45 (0.11-1.81) | 0.45 (0.09-2.19) |
| Cancer | 1.16 (0.69-1.94) | 0.99 (0.58-1.69) | 1.72 (0.80-3.66) | 1.99 (0.90-4.40) |
KNHANES, Korean National Health and Nutrition Survey; UOR, unadjusted odds ratio; CI, confidence interval; AOR, adjusted OR; COPD, chronic obstructive pulmonary diseases; PFT, pulmonary function test.
Other factors that affect vaccination coverage
In logistic regression analysis, factors affecting influenza vaccination rate were remarkably different according to age groups. In the group with ages between 40 and 65, those with less than middle school graduation were more likely to get vaccination than college graduates (aOR = 1.94; 95% CI 1.40-2.69). In addition, those who received regular health checkup (aOR = 1.60; 95% CI 1.21-2.12), and those who had restricted activity (aOR = 1.74; 95% CI 1.13-2.70) had significantly higher vaccination coverage. Those who had a history of dyslipidemia (aOR = 1.38; 95% CI 1.01-1.90), myocardial infarction or angina (aOR = 2.29; 95% CI 1.09-4.82), and chronic renal failure (aOR = 3.64; 95% CI 1.18-11.22) had higher vaccination coverage than those who had no such diseases. Interestingly, those who had pulmonary tuberculosis history (aOR = 0.50; 95% CI 0.29-0.87) were less likely to get vaccinated than those who had not. For those aged 65 years or older, any covariates including socio-demographic, health behavior, co-morbidities status, or screening results did not affect the vaccination coverage except among those who received regular health checkup (aOR = 1.51; 95% CI 1.01-2.26) (Table 2).
DISCUSSION
This study aimed to identify the influenza vaccination status of the people with decreased pulmonary functions or having COPD, a high risk population for influenza infection and its complications. Generally, subjects with normal pulmonary function were less likely to get vaccinated and those who had obstructive pulmonary dysfunction were more likely to get vaccinated. However, any pulmonary dysfunction or history of COPD did not affect the vaccination coverage in the multivariate analysis. Factors affecting influenza vaccination rate were remarkably different for younger population and elderly. For example, those with chronic diseases such as dyslipidemia, ischemic heart diseases and chronic renal failure had significantly higher vaccination coverage only in younger population. This is the first study, to the best of our knowledge, to investigate influenza vaccination coverage related to pulmonary function among Korean adults after age stratification.
People with pulmonary dysfunction are more likely to have symptoms and use health care services regularly, thereby have more chance to get vaccinated (1,11,12,13,14). Previous research showed that asthma patients had significantly higher vaccination coverage than healthy people (8) or that there had been no significant correlations between lung disease and vaccination coverage (6,7). The current research observed that influenza vaccination was higher among those with impaired lung function and diagnosed as COPD by doctors than subjects with normal pulmonary function. However, having COPD or pulmonary dysfunction was not a significant determinant for vaccination coverage in the multivariate analysis. This finding may be attributable to under-diagnosis of COPD (15,16). It was also notable that only a few subjects from people with abnormal lung function were diagnosed with COPD by doctors in the current study. Without performing spirometry, physicians were likely to underestimate their patients’ disease severity or inadequately recommend their patients’ treatment options (17). If diagnosis of COPD using breathing test can increase vaccination rates as in the study abroad (18), more spirometry should be implemented in primary care setting to increase the vaccination uptake as well as to confirm the diagnosis.
Our vaccination coverage rate among adults aged 65 or older (76.8%) was comparable to vaccination rate of 77.2% among adults aged 65 and over from the previous research using national sample in 2009 (6). Prevalence of influenza vaccination increased with age as in the previous studies (6,7,8,19), which is partly because adults aged 65 and over can receive free influenza vaccination through national immunization program for elderly, and partly because they have more utilization for medical services. The vaccination coverage rate is price sensitive and free or reimbursed vaccination has been reported as one of the strongest incentives to increase the vaccination of the young adults in Hong Kong (20). A study for influenza vaccination of cancer survivors also revealed that younger population had significantly lower vaccination coverage than elderly patients who had greater accessibility to vaccination by no cost (21). National health insurance coverage for vaccination regardless of age may be an effective strategy to increase the influenza vaccination uptake among high risk population of influenza such as people with chronic lung diseases or cancer survivors.
Vaccination rate was also higher among those who received regular health checkups regardless of age. People who receive regular health checkups are more likely to take care for their health, thereby get more information about vaccination from health professionals or have the chance to get vaccinated. Regular health checkups can be used as a chance to recommend or implement the influenza vaccination for high risk populations, because both are effective health promotion strategies.
Different characteristics were noted that affect vaccination coverage according to age groups in this study. For those aged 65 years and over, there was no significant difference among the vaccinated and the unvaccinated except regular health checkups, as in the previous study (6). However, there were some disparities in influenza vaccination coverage for young adults. Lower education level was associated with more vaccination among group with ages between 40 and 65. Some explanations include the fact that national free vaccination policy targets vulnerable social groups with lower education level. Or those who had lower education tend to assess themselves as relatively unhealthy and are more likely to get vaccination. This finding may be related with the fact that young adults who reported their activity level as restricted due to any cause or who had chronic diseases such as dyslipidemia, heart disease, and chronic renal disease got more vaccination in the present study. Previous reports on the relation between education and vaccination coverage showed conflicting results. Several studies from Korea (6,8) and China (22) revealed that lower education level was associated with higher vaccination coverage. In a multi-center study, there was no difference in the vaccination rate according to education level among patients with chronic kidney disease and asthma, but lower education was related to more influenza vaccination for diabetics (23). The effect of education on vaccination coverage was differently expressed among the European countries and could not be explained solely on the basis of economic characteristics of these countries (24,25). Further studies are needed to investigate the reasons why persons with high education level in relatively young ages refrain from getting immunization. It is notable that history of tuberculosis was associated with low vaccination rate, unlike other chronic disease which is an important attribute for vaccination receipt. Little has been studied about influenza vaccination coverage among patients with history of pulmonary tuberculosis. Those who have past history of tuberculosis may not feel any need for immunization because they do not perceive themselves as sick people. Further studies are needed to investigate the specific reasons why they do not get immunized against influenza.
There are several limitations to be considered in our study. Although we used data from a nationwide representative survey, it is difficult to establish causal and sequential relationships because of the nature of the cross-sectional design of the study. Since vaccination receipt and history of morbidity were based on self-report, these information can be vulnerable to recall bias. As we did not include the subjects aged below 40 years, we cannot broaden our interpretation to them. We could not estimate the impact of an active promotion for influenza vaccination and government’s education campaign since influenza pandemic in 2009-2010 which could have been a great influence on vaccination receipt (26).
Despite these limitations, we found that pulmonary dysfunction or having COPD did not significantly affect influenza vaccination coverage using the data of the 5th National Health and Nutrition Survey. Influenza vaccination coverage was considerably different when people were divided into groups, based on the age of 65. More recommendation of influenza vaccination needs to be encouraged for people with decreased pulmonary function due to smoking or chronic pulmonary diseases.
Footnotes
Funding: The authors have no potential conflicts of interest to declare.
AUTHOR CONTRIBUTION: Conception and design: Cha SH, Yoo S. Analysis and interpretation of data: Cha SH, Paik JH, Jeon YJ. Writing or revision of the manuscript: Cha SH, Lee MR, Yang H, Yoo S. Study supervision: Park SG, Yoo S. Approval of final manuscript: all authors.
References
- 1.Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community-dwelling elderly. N Engl J Med. 2007;357:1373–1381. doi: 10.1056/NEJMoa070844. [DOI] [PubMed] [Google Scholar]
- 2.Rothberg MB, Rose DN. Vaccination versus treatment of influenza in working adults: a cost-effectiveness analysis. Am J Med. 2005;118:68–77. doi: 10.1016/j.amjmed.2004.03.044. [DOI] [PubMed] [Google Scholar]
- 3.Ting SC, Crooks SW, South G. The effect of influenza vaccination on the incidence of chronic obstructive pulmonary disease exacerbations in the immediate postvaccination period. J Epidemiol Community Health. 2011;65:157–159. doi: 10.1136/jech.2009.092296. [DOI] [PubMed] [Google Scholar]
- 4.Simonsen L, Viboud C, Taylor R. Influenza vaccination in elderly people. Lancet. 2005;366:2086. doi: 10.1016/S0140-6736(05)67884-1. [DOI] [PubMed] [Google Scholar]
- 5.Park SC, Cheong HJ, Sohn JW, Choi SJ, Eom JS, Woo HJ, Chun BC, Kim WJ. Efficacy of influenza vaccination among chronic ill patients: retrospective case control study. Infect Chemother. 2004;36:207–212. [Google Scholar]
- 6.Lim J, Eom CS, Kim KH, Kim S, Cho B. Coverage of influenza vaccination among elderly in South Korea: a population based cross sectional analysis of the season 2004–2005. J Korean Geriatr Soc. 2009;13:215–221. [Google Scholar]
- 7.Kee SY, Lee JS, Cheong HJ, Chun BC, Song JY, Choi WS, Jo YM, Seo YB, Kim WJ. Influenza vaccine coverage rates and perceptions on vaccination in South Korea. J Infect. 2007;55:273–281. doi: 10.1016/j.jinf.2007.04.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park MB, Kim CB, Joo HS. Factors influencing on influenza vaccination coverage. J Korea Contents Assoc. 2013;13:300–311. [Google Scholar]
- 9.Ministry of Health and Welfare (KR) Korea National Health and Nutrition Examination Survey. Available at http://knhanes.cdc.go.kr.
- 10.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: update 2013. Available at http://www.goldcopd.org.
- 11.Kroneman M, van Essen GA, John Paget W. Influenza vaccination coverage and reasons to refrain among high-risk persons in four European countries. Vaccine. 2006;24:622–628. doi: 10.1016/j.vaccine.2005.08.040. [DOI] [PubMed] [Google Scholar]
- 12.Blank PR, Schwenkglenks M, Szucs TD. Influenza vaccination coverage rates in five European countries during season 2006/07 and trends over six consecutive seasons. BMC Public Health. 2008;8:272–282. doi: 10.1186/1471-2458-8-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blank PR, Schwenkglenks M, Szucs TD. Disparities in influenza vaccination coverage rates by target group in five European countries: trends over seven consecutive seasons. Infection. 2009;37:390–400. doi: 10.1007/s15010-009-8467-y. [DOI] [PubMed] [Google Scholar]
- 14.Linn ST, Guralnik JM, Patel KV. Disparities in influenza vaccine coverage in the United States, 2008. J Am Geriatr Soc. 2010;58:1333–1340. doi: 10.1111/j.1532-5415.2010.02904.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoo KH, Kim YS, Sheen SS, Park JH, Hwang YI, Kim SH, Yoon HI, Lim SC, Park JY, Park SJ, et al. Prevalence of chronic obstructive pulmonary disease in Korea: the fourth Korean National Health and Nutrition Examination Survey, 2008. Respirology. 2011;16:659–665. doi: 10.1111/j.1440-1843.2011.01951.x. [DOI] [PubMed] [Google Scholar]
- 16.Hill K, Goldstein RS, Guyatt GH, Blouin M, Tan WC, Davis LL, Heels-Ansdell DM, Erak M, Bragaglia PJ, Tamari IE, et al. Prevalence and underdiagnosis of chronic obstructive pulmonary disease among patients at risk in primary care. CMAJ. 2010;182:673–678. doi: 10.1503/cmaj.091784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mapel DW, Dalal AA, Johnson P, Becker L, Hunter AG. A clinical study of COPD severity assessment by primary care physicians and their patients compared with spirometry. Am J Med. 2015;128:629–637. doi: 10.1016/j.amjmed.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 18.Mowls DS, Cheruvu VK, Zullo MD. Influenza vaccination in adults with chronic obstructive pulmonary disease: the impact of a diagnostic breathing test on vaccination rates. PLoS One. 2013;8:e67600. doi: 10.1371/journal.pone.0067600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dower J, Donald M, Begum N, Vlack S, Ozolins I. Patterns and determinants of influenza and pneumococcal immunisation among adults with chronic disease living in Queensland, Australia. Vaccine. 2011;29:3031–3037. doi: 10.1016/j.vaccine.2011.01.116. [DOI] [PubMed] [Google Scholar]
- 20.Yeung MP, Ng SK, Tong ET, Chan SS, Coker R. Factors associated with uptake of influenza vaccine in people aged 50 to 64 years in Hong Kong: a case-control study. BMC Public Health. 2015;15:617. doi: 10.1186/s12889-015-1990-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choi KH, Park SM, Lee K, Lee JH, Park JS. Influenza vaccination and associated factors among Korean cancer survivors: a cross-sectional analysis of the Fourth & Fifth Korea National Health and Nutrition Examination Surveys. J Korean Med Sci. 2014;29:1061–1068. doi: 10.3346/jkms.2014.29.8.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zheng Y, Yang P, Wu S, Ma C, Seale H, Macintyre CR, Wang Q. A cross-sectional study of factors associated with uptake of vaccination against influenza among older residents in the postpandemic season in Beijing, China. BMJ Open. 2013;3:e003662. doi: 10.1136/bmjopen-2013-003662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kee SY, Cheong HJ, Chun BC, Kim WJ. Influenza vaccination coverage rate and factors associated with vaccination in people with chronic disease. Infect Chemother. 2011;43:406–411. [Google Scholar]
- 24.Damiani G, Federico B, Visca M, Agostini F, Ricciardi W. The impact of socioeconomic level on influenza vaccination among Italian adults and elderly: a cross-sectional study. Prev Med. 2007;45:373–379. doi: 10.1016/j.ypmed.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 25.Endrich MM, Blank PR, Szucs TD. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine. 2009;27:4018–4024. doi: 10.1016/j.vaccine.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 26.Sevencan F, Ertem M, Özçullu N, Dorman V, Kubat NK. The evaluation of the opinions and attitudes of healthcare personnel of the province Diyarbakir against influenza A (H1N1) and the vaccination. Hum Vaccin. 2011;7:945–951. doi: 10.4161/hv.7.9.16368. [DOI] [PubMed] [Google Scholar]


