Abstract
Spinal fractures have been recognized as a major health concern. Our purposes were to evaluate the trends in the incidence and mortality of spinal fractures between 2008 and 2012 and predict the number of spinal fractures that will occur in Korea up to 2025, using nationwide data from the National Health Insurance Service (NHIS). A nationwide data set was evaluated to identify all new visits to medical institutes for spinal fractures in men and women aged 50 years or older between 2008 and 2012. The incidence, mortality rates and estimates of the number of spinal fractures were calculated using Poisson regression. The number of spinal fractures increased over the time span studied. Men and women experienced 14,808 and 55,164 vertebral fractures in 2008 and 22,739 and 79,903 in 2012, respectively. This reflects an increase in the incidence of spinal fractures for both genders (men, 245.3/100,000 in 2008 and 312.5/100,000 in 2012; women, 780.6/100,000 in 2008 and 953.4/100,000 in 2012). The cumulative mortality rate in the first year after spinal fractures decreased from 8.51% (5,955/69,972) in 2008 to 7.0% (7,187/102,642) in 2012. The overall standardized mortality ratio (SMR) of spinal fractures at 1 year post-fracture was higher in men (7.76, 95% CI: 7.63-7.89) than in women (4.70, 95% CI: 4.63-4.76). The total number of spinal fractures is expected to reach 157,706 in 2025. The incidence of spinal fractures increased in Korea in the last 5 years, and the socioeconomic burden of spinal fractures will continue to increase in the near future.
Keywords: Spinal Fracture; Mortality; Projection; Osteoporosis, Korea
INTRODUCTION
A spinal compression fracture is one of the most serious osteoporotic fractures, and it is a major health concern worldwide. Several studies have reported that osteoporotic spinal fracture is associated with adverse effects, such as increased back pain (1), decreased quality of life (2), and increased mortality (3,4,5,6,7).
To manage the socioeconomic burden of spinal fractures, basic epidemiologic data, such as the current incidence and future projections, should be examined. Although some previous studies have evaluated the incidence of spinal fractures, they did not investigate nationwide trends over long time periods (6,8,9). Although several epidemiological studies have been conducted to determine trends in the incidence of osteoporotic hip fracture (10,11), there has been no similar study concerning spinal fractures.
The purposes of this study were to investigate trends in the incidence and mortality of spinal fractures in Koreans aged 50 years or older from 2008 to 2012, and to estimate the socioeconomic burden of spinal fractures up to the year 2025, using nationwide data from the National Health Insurance Service (NHIS).
MATERIALS AND METHODS
Patients aged 50 years and older with spinal fractures were identified from a nationwide database collected by the National Health Insurance Service (NHIS) of Korea between 2008 and 2012. The Korean National Health Insurance program covers 100% of the population for any medical procedure with the exception of cosmetic surgery and services for traffic accidents. All clinics and hospitals submit data on inpatients and outpatients, including data on diagnoses (as defined by the International Classification of Diseases, 10th revision (ICD-10)), demographic information, and medical costs, for claims. Therefore, virtually all information about patients and diseases is available from the Korean NHIS database, which has been used in several epidemiological studies (3,12,13,14,15).
To identify patients with spinal fractures, we searched for claims listing an ICD-10 code of S22.0 (fracture of the thoracic spine), S22.1 (multiple fractures of the thoracic spine), S32.0 (fracture of the lumbar spine), M48.4 (fatigue fracture of vertebra) and M48.5 (collapsed vertebra, not elsewhere classified (NEC)). To ensure the specificity of our cohort, each fracture code had to be accompanied by a physician claim for site-specific fracture reduction or fixation (such as vertebroplasty or kyphoplasty) and radiologic imaging study code (3).
These data were retrospectively evaluated to determine the annual age- and gender-specific incidence and mortality of spinal fractures in individuals aged 50 years or older between 2008 and 2012.
To determine trends in the incidence of spinal fractures, patients were categorized by age (subdivided into 5-year increments) and gender, and age-adjusted/gender-specific incidences (per 100,000 person-years) were calculated. NHIS data were merged with national mortality data obtained from the National Statistical Office to determine the survival status of individual patients 12 months after spinal fractures. The one-year mortality rate was calculated and presented in 10-year age intervals. In order to identify increases in mortality following spinal fractures, the standardized mortality ratio (SMR) (the ratio of observed mortality to expected mortality, matched for age and gender group) was calculated in 10-year age intervals. Expected mortality was calculated using age- and gender-specific mortality rates for the general population.
A projection of the incidence of spinal fractures up to the year 2025 was based on identified trends in the incidence of spinal fractures from 2008 to 2012. Population projections and estimated demographic information up to the year 2025 were obtained from the Korean Statistical Information Service. The projected number of spinal fractures was estimated by applying fracture incidence estimated from the Poisson distribution to the projected population data for each age and gender group. The projected total number of fractures is the sum of the projected number of fractures in each age and gender group. The number of men and women in each age group was obtained from the ‘Statistics Korea’ web site (http://www.kosis.kr), the official web site of the Central Government Organization for Statistics (16). All database management and analyses were performed using SAS statistical package version 9.4 (SAS Institute, Cary, NC, USA).
Ethics statement
The study protocol was approved by the NHIS institutional review board (number: NHIS-2015-4-001). Informed consent was exempted by the board.
RESULTS
Incidence of spinal fractures
Amongst Koreans 50 years of age and older, the overall incidence of spinal fractures was 603 per 100,000 person-years from 2008 to 2012, and the gender-specific incidence was 283.8 per 100,000 person-years for men and 878.1 per 100,000 person-years for women. The number of spinal fractures in men and women increased, from 14,808 and 55,164 in 2008 to 22,739 and 79,903 in 2012, respectively. The incidence of spinal fractures in men increased from 245.3/100,000 in 2008 to 312.5/100,000 in 2012, while the incidence of spinal fractures in women increased from 780.6/100,000 in 2008 to 909.3/100,000 in 2012. During the study period, the annual incidence of spinal fractures in women was consistently 3 times higher than that in men in Korea (Table 1).
Table 1. Gender-specific incidence (per 100,000 person years) and one year mortality of patients with spinal fractures from 2008 to 2012.
| Year | Population | No. of Fracture (death*) | Incidence (per 100,000) | Mortality (%) | ||||
|---|---|---|---|---|---|---|---|---|
| Man | Woman | Men | Women | Men | Women | Men | Women | |
| 2008 | 6,037,749 | 7,067,828 | 14,808 (2,150) | 55,164 (3,805) | 245.3 | 780.6 | 14.52 | 6.90 |
| 2009 | 6,328,756 | 7,377,054 | 16,638 (2,276) | 60,475 (3,946) | 262.9 | 819.9 | 13.68 | 6.53 |
| 2010 | 6,631,086 | 7,699,702 | 19,308 (2,776) | 70,038 (4,476) | 291.2 | 909.8 | 14.38 | 6.39 |
| 2011 | 6,958,793 | 8,043,184 | 20,824 (2,833) | 73,117 (4,442) | 299.3 | 909.3 | 13.60 | 6.08 |
| 2012 | 7,276,836 | 8,383,224 | 22,739 (2,834) | 79,903 (4,353) | 312.5 | 953.4 | 13.64 | 5.45 |
*Number of death after spinal fracture; Mortality is accumulated over one year follow-up period.
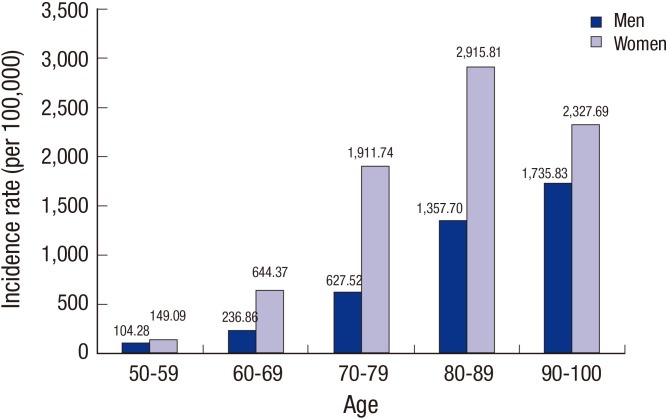
The proportion of spinal fractures incidence in each decile showed similar pattern during the 5 years study period. Although the mean age-specific incidence by decile in woman increased from 149.09/100,000 for those aged 50-59 to 2915.81/100,000 for those aged 80-89 then decreasing 2327.69/100,000 for those aged 90-100, the mean age-specific incidence by decile in man increased from 104.28/100,000 for those aged 50-59 to 1735.83/100,000 for those aged 90-100 (Fig. 1).
Fig. 1.
Age-specific incidence of spinal fractures in Koreans aged 50 years and older from 2008 to 2012.
Mortality and SMR after spinal fractures
The cumulative mortality rate in the first year after spinal fractures decreased from 8.51% (5,955/69,972) in 2008 to 7.0% (7,187/102,642) in 2012. Mortality rates in both genders showed a decreasing trend. According to gender, the average one-year mortality rates were 13.64% for men and 6.21% for women (Table 1). The one-year mortality rate of men was 2.2 times higher than that of women.
The overall SMR was higher in men (7.76, 95% CI: 7.63-7.89) than in women (4.70, 95% CI: 4.63-4.76) and it gradually declined with age. With the exception of women aged 50-59, the SMR of men was consistently higher than that of women. The SMRs of spinal fractures patients were higher than those of the general population for all age brackets (Table 2).
Table 2. Mortality and average standard mortality ratio (SMRs) adjusted for gender and age at 1-year follow-up.
| Sex | Age, yr | Mortality (%) | 95% CI | SMRs | 95% CI |
|---|---|---|---|---|---|
| Men | 50-59 | 4.94 | 4.62-5.28 | 8.34 | 7.80-8.92 |
| 60-69 | 8.90 | 8.52-9.30 | 6.84 | 6.55-7.15 | |
| 70-79 | 14.76 | 14.35-15.17 | 4.04 | 3.92-4.15 | |
| 80-89 | 23.55 | 22.86-24.27 | 2.52 | 2.44-2.59 | |
| 90-100 | 36.35 | 33.73-39.19 | 1.56 | 1.45-1.68 | |
| ≥ 50 | 13.64 | 13.41-13.88 | 7.76 | 7.63-7.89 | |
| Women | 50-59 | 1.76 | 1.61-1.94 | 8.79 | 8.04-9.69 |
| 60-69 | 2.73 | 2.60-2.85 | 5.70 | 5.43-5.95 | |
| 70-79 | 5.10 | 4.99-5.22 | 2.85 | 2.79-2.92 | |
| 80-89 | 10.53 | 10.32-10.75 | 1.64 | 1.61-1.68 | |
| 90-100 | 20.94 | 20.02-21.89 | 1.09 | 1.04-1.14 | |
| ≥ 50 | 6.21 | 6.12-6.29 | 4.70 | 4.63-4.76 | |
| Total | 50-59 | 3.07 | 2.91-3.24 | 7.75 | 7.34-8.18 |
| 60-69 | 4.26 | 4.13-4.40 | 4.89 | 4.74-5.05 | |
| 70-79 | 6.91 | 6.79-7.03 | 2.69 | 2.64-2.73 | |
| 80-89 | 12.76 | 12.55-12.98 | 1.74 | 1.71-1.77 | |
| 90-100 | 23.55 | 22.66-24.47 | 1.17 | 1.13-1.22 | |
| ≥ 50 | 7.83 | 7.74-7.91 | 5.14 | 5.08-5.19 |
SMR, standard mortality ratio; CI, confidence interval.
Projection of spinal fractures
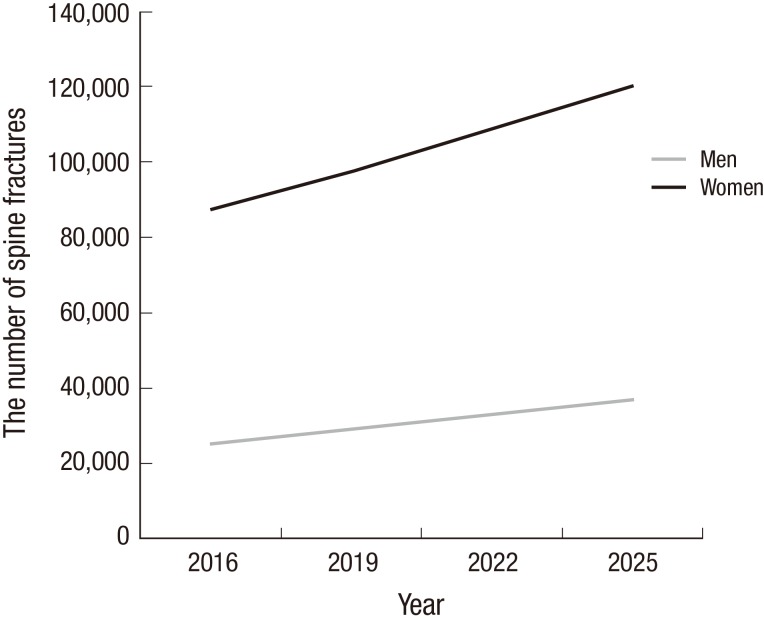
From 2016 to 2025, the population of Korea is expected to increase by only 2.3%, and population demographics are expected to undergo extreme changes. The population aged ≥ 50 years will increase by an estimated 27%. The population aged ≥ 70 and ≥ 90 years will increase by 42.2% and 101.7%, respectively.
Our model predicts a substantial increase in the number of spinal fractures in the near future owing to the aging population. From 2012 to 2025, the number of spinal fractures in men is expected to increase from 22,739 in 2012 to 37,040 in 2025, while the number of spinal fractures in women is expected to increase from 79,903 in 2012 to 120,666 in 2025 (Fig. 2).
Fig. 2.
Estimated number of spinal fractures in Korea up to the year 2025.
DISCUSSION
This study, which used data from nationwide insurance claims, demonstrated that the total incidence of vertebral fracture increased in the Korean population aged 50 years and older from 2008 to 2012. It also estimated the increase in the number of spinal fractures up to the year 2025. The gender-specific incidences of spinal fractures were 953.1/100,000 for women and 312.5/100,000 for men in 2012. These incidences are higher than those reported in other countries with populations at intermediate or high risk of osteoporotic fracture, including Finland (183/100,000 for women and 83/100,000 for men), Japan (322.5/100,000 for women and 134.7/100,000 for men), and Hong Kong (508/100,000 for women and 194/100,000 for men) (17,18,19). We cannot directly compare our findings with those from other countries, because the incidence of spinal fractures varies according to study design, definition of fracture, and survey protocol. However, our findings suggest that Korea is no longer a country with a low risk of osteoporotic fracture.
There have been several previous studies on trends in the incidence of spinal fractures (20,21,22,23). An epidemiological study showed that the incidence of vertebral fracture decreased in both genders over the last decade in Iceland (20). However, our study demonstrated that the incidence of spinal fractures increased during the study period. This finding concurs with the results of other recent epidemiological studies, in which it was concluded that the incidence of spinal fractures has increased with time (21,22,23) and the incidence and socioeconomic burden of spinal fractures will increase in the foreseeable future (24,25,26).
The one-year mortality rate of spinal fractures varies considerably; depending on the study, it ranged from 1.9% to 42% (6,27,28). In this study, the mean one-year mortality rate over the 5 years study period was 7.8%. However, cumulative one-year mortality rate showed a decreasing trend, from 8.51% (5,955/69,972) in 2008 to 7.0% (7,187/102,642) in 2012. Our results showed that men are at a substantially higher risk of mortality than women, and this was maintained after adjusting for mortality rates in the general population using SMR. These findings are consistent with those of many other studies (29,30). Although it is difficult to determine precisely why spinal fracture patients have a higher mortality rate than the general population, the explanation may have to do with underlying comorbidities and/or complications associated with prolonged hospital stays (31,32).
In parallel with the predicted increase in the number of spinal fractures, the socioeconomic burden of spinal fractures on the health care system will continue to increase. A main problem is that the Korean population is rapidly aging. Our projections may apply to countries with similar demographic structures, such as Japan, China, and Taiwan (33,34,35). The future burden of spinal fractures may also increase in such countries.
This study had several limitations. First, we could not evaluate bone mineral density (BMD). It is possible that spinal fractures caused by high-energy trauma were included in this study, because it is impossible to distinguish between high- and low-energy fractures using only data from the ICD-10 coding system. However, to exclude non-osteoporotic fractures, we included only data from patients aged 50 years or older; that particular inclusion criterion has been used in previous epidemiological studies on osteoporotic spinal fractures (3,15,36). Second, some patients with osteoporotic spinal fractures may not be included in the nationwide database. Patients with non-symptomatic or mildly symptomatic spinal fractures may not be included, because only patients who visited a clinic or hospital were entered into the NHIS database.
Despite these limitations, to our knowledge, this is the first epidemiological nationwide study to present trends in the incidence of spinal fractures over a long (5-year) time period, and the first to predict the future burden of spinal fractures in an Asian country. Moreover, this is the first study worldwide that presents the future burden of spinal fractures based on national health insurance claims data. We anticipate that our results will be quite useful in establishing appropriate general health strategies to manage the burdens associated with spinal fractures.
ACKNOWLEDGMENT
The national insurance claim data used in this research were provided by the Korean National Health Insurance Service (NHIS).
Footnotes
Funding: This research was supported by a grant from the Korean Health Technology R&D Project through the Korean Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare (grant number: HI13C1522).
DISCLOSURE: No benefits in any form have been received or will be received from any commercial party related directly or indirectly to the subject of this article.
AUTHOR CONTRIBUTION: Study design: Kim TY, Jang S, Lee YK, Ha YC. Data acquisition: Cho EH, Lee A. Data analysis: Kim HY, Jang S, Park C, Park EJ, Kim TY. Writing manuscript: Kim TY, Ha YC, Park C. Approval of final manuscript and ensuring research integrity: all authors.
References
- 1.Cheung G, Chow E, Holden L, Vidmar M, Danjoux C, Yee AJ, Connolly R, Finkelstein J. Percutaneous vertebroplasty in patients with intractable pain from osteoporotic or metastatic fractures: a prospective study using quality-of-life assessment. Can Assoc Radiol J. 2006;57:13–21. [PubMed] [Google Scholar]
- 2.Salaffi F, Cimmino MA, Malavolta N, Carotti M, Di Matteo L, Scendoni P, Grassi W, Italian Multicentre Osteoporotic Fracture Study Group The burden of prevalent fractures on health-related quality of life in postmenopausal women with osteoporosis: the IMOF study. J Rheumatol. 2007;34:1551–1560. [PubMed] [Google Scholar]
- 3.Lee YK, Jang S, Jang S, Lee HJ, Park C, Ha YC, Kim DY. Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int. 2012;23:1859–1865. doi: 10.1007/s00198-011-1833-5. [DOI] [PubMed] [Google Scholar]
- 4.Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ., 3rd Population-based study of survival after osteoporotic fractures. Am J Epidemiol. 1993;137:1001–1005. doi: 10.1093/oxfordjournals.aje.a116756. [DOI] [PubMed] [Google Scholar]
- 5.Ensrud KE, Thompson DE, Cauley JA, Nevitt MC, Kado DM, Hochberg MC, Santora AC, 2nd, Black DM, Fracture Intervention Trial Research Group Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. J Am Geriatr Soc. 2000;48:241–249. doi: 10.1111/j.1532-5415.2000.tb02641.x. [DOI] [PubMed] [Google Scholar]
- 6.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 7.Hasserius R, Karlsson MK, Nilsson BE, Redlund-Johnell I, Johnell O, European Vertebral Osteoporosis Study Prevalent vertebral deformities predict increased mortality and increased fracture rate in both men and women: a 10-year population-based study of 598 individuals from the Swedish cohort in the European Vertebral Osteoporosis Study. Osteoporos Int. 2003;14:61–68. doi: 10.1007/s00198-002-1316-9. [DOI] [PubMed] [Google Scholar]
- 8.Lau E, Ong K, Kurtz S, Schmier J, Edidin A. Mortality following the diagnosis of a vertebral compression fracture in the Medicare population. J Bone Joint Surg Am. 2008;90:1479–1486. doi: 10.2106/JBJS.G.00675. [DOI] [PubMed] [Google Scholar]
- 9.Bouza C, López T, Palma M, Amate JM. Hospitalised osteoporotic vertebral fractures in Spain: analysis of the national hospital discharge registry. Osteoporos Int. 2007;18:649–657. doi: 10.1007/s00198-006-0292-x. [DOI] [PubMed] [Google Scholar]
- 10.Chen IJ, Chiang CY, Li YH, Chang CH, Hu CC, Chen DW, Chang Y, Yang WE, Shih HN, Ueng SW, et al. Nationwide cohort study of hip fractures: time trends in the incidence rates and projections up to 2035. Osteoporos Int. 2015;26:681–688. doi: 10.1007/s00198-014-2930-z. [DOI] [PubMed] [Google Scholar]
- 11.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 12.Sung SK, Lee SG, Lee KS, Kim DS, Kim KH, Kim KY. First-year treatment adherence among outpatients initiating antihypertensive medication in Korea: results of a retrospective claims review. Clin Ther. 2009;31:1309–1320. doi: 10.1016/j.clinthera.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Lee YK, Ha YC, Park C, Yoo JJ, Shin CS, Koo KH. Bisphosphonate use and increased incidence of subtrochanteric fracture in South Korea: results from the National Claim Registry. Osteoporos Int. 2013;24:707–711. doi: 10.1007/s00198-012-2016-8. [DOI] [PubMed] [Google Scholar]
- 14.Lee YK, Yoon BH, Nho JH, Kim KC, Ha YC, Koo KH. National trends of surgical treatment for intertrochanteric fractures in Korea. J Korean Med Sci. 2013;28:1407–1408. doi: 10.3346/jkms.2013.28.9.1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim SH, Ko YB, Lee YK, Hong SW, Choi HJ, Ha YC, Shin CS. National utilization of calcium supplements in patients with osteoporotic hip fracture in Korea. J Bone Metab. 2013;20:99–103. doi: 10.11005/jbm.2013.20.2.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Statistics Korea. Korean Statistical Information Service. [accessed on 9 September 2015]. Available at http://www.kosis.kr/
- 17.Koski AM, Patala A, Patala E, Sund R. Incidence of osteoporotic fractures in elderly women and men in Finland during 2005-2006: a population-based study. Scand J Surg. 2014;103:215–221. doi: 10.1177/1457496914525554. [DOI] [PubMed] [Google Scholar]
- 18.Sakuma M, Endo N, Oinuma T, Endo E, Yazawa T, Watanabe K, Watanabe S. Incidence and outcome of osteoporotic fractures in 2004 in Sado City, Niigata Prefecture, Japan. J Bone Miner Metab. 2008;26:373–378. doi: 10.1007/s00774-007-0841-1. [DOI] [PubMed] [Google Scholar]
- 19.Bow CH, Cheung E, Cheung CL, Xiao SM, Loong C, Soong C, Tan KC, Luckey MM, Cauley JA, Fujiwara S, et al. Ethnic difference of clinical vertebral fracture risk. Osteoporos Int. 2012;23:879–885. doi: 10.1007/s00198-011-1627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Siggeirsdottir K, Aspelund T, Jonsson BY, Mogensen B, Gudmundsson EF, Gudnason V, Sigurdsson G. Epidemiology of fractures in Iceland and secular trends in major osteoporotic fractures 1989-2008. Osteoporos Int. 2014;25:211–219. doi: 10.1007/s00198-013-2422-6. [DOI] [PubMed] [Google Scholar]
- 21.Wang H, Li C, Xiang Q, Xiong H, Zhou Y. Epidemiology of spinal fractures among the elderly in Chongqing, China. Injury. 2012;43:2109–2116. doi: 10.1016/j.injury.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 22.Oinuma T, Sakuma M, Endo N. Secular change of the incidence of four fracture types associated with senile osteoporosis in Sado, Japan: the results of a 3-year survey. J Bone Miner Metab. 2010;28:55–59. doi: 10.1007/s00774-009-0097-z. [DOI] [PubMed] [Google Scholar]
- 23.Cooper C, Atkinson EJ, Kotowicz M, O’Fallon WM, Melton LJ., 3rd Secular trends in the incidence of postmenopausal vertebral fractures. Calcif Tissue Int. 1992;51:100–104. doi: 10.1007/BF00298496. [DOI] [PubMed] [Google Scholar]
- 24.Gauthier A, Kanis JA, Jiang Y, Martin M, Compston JE, Borgström F, Cooper C, McCloskey EV. Epidemiological burden of postmenopausal osteoporosis in the UK from 2010 to 2021: estimations from a disease model. Arch Osteoporos. 2011;6:179–188. doi: 10.1007/s11657-011-0063-y. [DOI] [PubMed] [Google Scholar]
- 25.Cawston H, Maravic M, Fardellone P, Gauthier A, Kanis JA, Compston J, Borgström F, Cooper C, McCloskey E. Epidemiological burden of postmenopausal osteoporosis in France from 2010 to 2020: estimations from a disease model. Arch Osteoporos. 2012;7:237–246. doi: 10.1007/s11657-012-0102-3. [DOI] [PubMed] [Google Scholar]
- 26.Piscitelli P, Brandi M, Cawston H, Gauthier A, Kanis JA, Compston J, Borgström F, Cooper C, McCloskey E. Epidemiological burden of postmenopausal osteoporosis in Italy from 2010 to 2020: estimations from a disease model. Calcif Tissue Int. 2014;95:419–427. doi: 10.1007/s00223-014-9910-3. [DOI] [PubMed] [Google Scholar]
- 27.Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B. Excess mortality after hospitalisation for vertebral fracture. Osteoporos Int. 2004;15:108–112. doi: 10.1007/s00198-003-1516-y. [DOI] [PubMed] [Google Scholar]
- 28.Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D. Risk of mortality following clinical fractures. Osteoporos Int. 2000;11:556–561. doi: 10.1007/s001980070075. [DOI] [PubMed] [Google Scholar]
- 29.Ioannidis G, Papaioannou A, Hopman WM, Akhtar-Danesh N, Anastassiades T, Pickard L, Kennedy CC, Prior JC, Olszynski WP, Davison KS, et al. Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. CMAJ. 2009;181:265–271. doi: 10.1503/cmaj.081720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teng GG, Curtis JR, Saag KG. Mortality and osteoporotic fractures: is the link causal, and is it modifiable? Clin Exp Rheumatol. 2008;26:S125–37. [PMC free article] [PubMed] [Google Scholar]
- 31.Papaioannou A, Adachi JD, Parkinson W, Stephenson G, Bédard M. Lengthy hospitalization associated with vertebral fractures despite control for comorbid conditions. Osteoporos Int. 2001;12:870–874. doi: 10.1007/s001980170039. [DOI] [PubMed] [Google Scholar]
- 32.Ismail AA, O’Neill TW, Cooper C, Finn JD, Bhalla AK, Cannata JB, Delmas P, Falch JA, Felsch B, Hoszowski K, et al. Mortality associated with vertebral deformity in men and women: results from the European Prospective Osteoporosis Study (EPOS) Osteoporos Int. 1998;8:291–297. doi: 10.1007/s001980050067. [DOI] [PubMed] [Google Scholar]
- 33.Si L, Winzenberg TM, Jiang Q, Chen M, Palmer AJ. Projection of osteoporosis-related fractures and costs in China: 2010-2050. Osteoporos Int. 2015;26:1929–1937. doi: 10.1007/s00198-015-3093-2. [DOI] [PubMed] [Google Scholar]
- 34.Shao CJ, Hsieh YH, Tsai CH, Lai KA. A nationwide seven-year trend of hip fractures in the elderly population of Taiwan. Bone. 2009;44:125–129. doi: 10.1016/j.bone.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 35.Tsukutani Y, Hagino H, Ito Y, Nagashima H. Epidemiology of fragility fractures in Sakaiminato, Japan: incidence, secular trends, and prognosis. Osteoporos Int. 2015;26:2249–2255. doi: 10.1007/s00198-015-3124-z. [DOI] [PubMed] [Google Scholar]
- 36.Park C, Ha YC, Jang S, Jang S, Yoon HK, Lee YK. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab. 2011;29:744–751. doi: 10.1007/s00774-011-0279-3. [DOI] [PubMed] [Google Scholar]