Abstract
Aim and Objectives:
This study evaluated the efficacy of oral methylprednisolone and diclofenac sodium on post-operative sequelae after third molar surgery.
Settings and Design:
A randomized double-blind clinical trial was conducted (with institutional and university approval for dissertation) to evaluate the effect of methylprednisolone with diclofenac sodium (group A) as compared with diclofenac sodium and placebo (group B) on three variables: Pain, swelling and trismus, after third molar surgery.
Materials and Methods:
Thirty consecutive consenting patients for surgical removal of mandibular impacted third molar were randomly placed into two groups of 15 each (groups A and B). Pain, swelling and trismus were observed by visual analog scale, facial measurements and inter-incisal opening. Scores were recorded after 24 and 72 h and on the seventh post-operative day. Results were subjected to the Chi-square test and independent sample t-test (P = 0.05).
Results:
Mean difference in pain experienced between the two groups was statistically significant at 24 h (P = 0.015) and 72 h (P = 0.001) and on the seventh day (P = 0.005). Difference in inter-incisal distance was insignificant (P = 0.239) pre-operatively, but significant after 24 h (P = 0.014) and 72 h (P = 0.001) and on the seventh post-operative day (P = 0.001). Mean difference in swelling was highly significant after 24 h (P = 0.001) and 72 h (P = 0.0001) and on the seventh post-operative day (P = 0.047).
Conclusions:
The combination of oral dose of methylprednisolone (a corticosteroid) diclofenac sodium (a non-steroidal anti-inflammatory drug) was found to be more effective than diclofenac sodium alone on the sequelae of surgical removal of impacted mandibular third molar.
Keywords: Glucocorticosteroid, non-steroidal anti-inflammatory drug, pain, swelling, trismus
INTRODUCTION
Surgical removal of impacted third molars is a commonly performed procedure.[1] However, it is also associated with variable post-operative consequences like pain, swelling and trismus.[1,2,3,4] Corticosteroids are some of the most common pharmaceutical agents employed to manage these sequelae.[5,6,7] Of these, methylprednisolone is a highly selective, intermediate acting, synthetic glucocorticosteroid, more potent than hydrocortisone and dexamethasone.[8,9,10] Surprisingly, few studies have evaluated the use of oral methylprednisolone alone or in combination with popular non-steroidal anti-inflammatory drugs (NSAIDs), in spite of obvious benefits. This study evaluates the efficacy of Methylprednisolone alone and in combination with diclofenac sodium.
MATERIALS AND METHODS
This study was conducted as part of a dissertation, after approval by the ethical committee of the concerned institution and university, and with detailed, written, informed consent from each patient.
Inclusion criteria
Thirty consenting patients in the age group of 18-50 years, with clinical and radiographic presence of bony impaction of the third molar, were included in this study. Only impacted teeth, asymptomatic at the time of surgery and requiring surgical removal (including bone removal), were included. These 30 patients were randomly allotted to one of the two experimental groups of 15 each, namely the methylprednisolone and the diclofenac sodium group A and the diclofenac sodium and the placebo group B.
Exclusion criteria
Patients who were excluded from the study were those with any systemic disease, with clinical symptoms in the third molar at the time of presentation, pre-existing chronic infection, giving a history of use of corticosteroids over the previous 3 months or allergy to the drug. Pregnant and lactating women were also excluded from the study.
Radiographic records were made using Orthopantomogram and Intraoral Periapical Radiograph. Pre-operative investigations were performed after taking consent of the patient and their case histories.
The details recorded pre-operatively included the tooth to be removed, type of impaction, inter-incisal distance (IID) and facial baseline measurement (FM). FM was determined by a modification of the tape measuring method described by Gabka and Matsumara.[11] Three measurements were made between five reference points: Mandibular angle (G), tragus (T), lateral canthus of the eye (L), outer corner of the mouth (A) and soft tissue pogonion (P) by using a measuring tape to follow the contour of the face [Figure 1]. The sum of all measurements (FM1 + FM2 + FM3) was taken as the facial size (FM). IID was evaluated by measuring the distance on maximal opening between the right maxillary and mandibular incisor with a vernier caliper [Figure 2].[11]
Figure 1.

Three facial measurements between five reference points: Mandibular angle (G), tragus (T), lateral canthus of the eye (L), outer corner of the mouth (A) and soft tissue pogonion (P) using a measuring tape
Figure 2.

Measuring maximal distance between the right maxillary and the mandibular incisor with a vernier caliper
All surgeries were carried out by the same surgeon. Under aseptic condition and under local anesthesia, a modified Terrance Ward's incision was placed and the mucoperiosteal flap was raised.[12] Bone buccal and distal to the tooth was removed using a bur and the tooth was delivered out of the socket. The socket was debrided and complete hemostasis was achieved. After wound closure with a 3-0 black silk suture material, a wet gauze pack was placed. Post-operative instructions were given. All the patients were given tablets of diclofenac sodium 50 mg orally three times a day for 3 days and amoxicillin 500 mg three times a day orally for 5 days. Patients in the group A were additionally prescribed tablets of methylprednisolone 8 mg orally three times a day for 3 days, whereas patients in group B were given placebo tablets (sugar pills) in similar dosage. Patients were recalled after 24 and 72 h and on the seventh post-operative day for follow-up.
Pain, IID and swelling (FM) were recorded after 24 and 72 h and the on seventh post-operative day. Pain was recorded using a pre-calibrated 100 mm Visual Analogue Scale (VAS). The end points of the scale were “no pain” and “pain could not be worse.” The means from the VAS were classified as none/no pain (0-10 mm), mild pain (11-30 mm), moderate pain (31–60 mm) and severe pain (61-100 mm).[13] FM and IID were measured as done previously.
All patients were given a questionnaire to evaluate the post-operative morbidity and their quality of life following the surgical procedure, and it was correlated with the clinical presentation.
Statistics
The results were evaluated on the basis of the Chi-square test (for possible association between two categorical variables) and the independent sample t-test (to test the equality of the two samples) (P = 0.05).
RESULTS
The methylprednisolone–diclofenac sodium group (group A) and the NSAID only (diclofenac sodium) group (group B) consisted of 15 patients each. The age range of the patients in group A was 19-40 years, with a mean age of 25.9 years whereas in group B, it was 19-35 years, with a mean age of 25.4 years, with no significant difference (P = 0.781) in both groups as found through the t-test. Nor was any significant difference (P = 0.456) found in the number of patients in each sex between the two groups, based on a Chi-squared statistic.
In both the groups, seven patients (46.7%) had their left and eight patients (53.3%) had their right mandibular third molars extracted, with an insignificant mean difference (P = 0.587) on applying the Chi-square test.
Pain
In group A [Graph 1], the mean pain on the VAS was 26.26±14.64 mm after 24 h, which lies in the range of “mild pain.” After 72 h, it was 11.06 ± 10.27 mm (no pain to mild pain), with 0.6 ± 1.45 mm (no pain) on the seventh day. In group B, mean pain seen was 50 ± 18.92 mm (moderate pain) after 24 h, 28.46 ± 13.42 mm (mild pain) after 72 h and 9.53 ± 9.79 mm (i.e. no pain) on the seventh day. After applying the Chi-square test, it was statistically analyzed that the mean difference in pain experienced between the two groups was significant (P = 0.015) at 24 h, whereas it was highly significant at 72 h (P = 0.001) and on the seventh day (P = 0.005).
Graph 1.
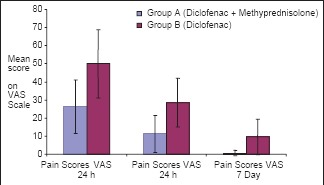
Comparing mean pain experienced on the VAS by patient group A and patients group B
Inter-incisal distance
In group A [Graph 2], the mean inter-incisal distance (MIID) pre-operatively was 47.26 ± 4.62 mm, 37.33±3.97 mm after 24 h, 43.93±4.008) mm after 72 h and 46.86±4.79 mm on the seventh post-operative day. In group B, MIID measured pre-operatively was 45.33±4.169 mm, 32.06 ± 6.67 mm after 24 h, 36.86±6.446) mm after 72 h and 42.53±5.488 mm on the seventh post-operative day. The mean difference in inter-incisal distance between the two groups after applying the independent sample t-test was statistically insignificant (P = 0.239) pre-operatively, but was statistically significant after 24 (P = 0.014) and 72 h (P = 0.001) and on the seventh post-operative day (P = 0.001).
Graph 2.
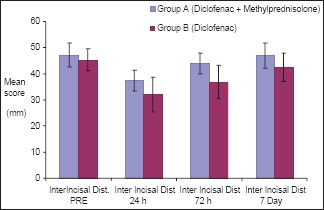
Comparing the mean inter-incisal distance between group A and group B
Facial swelling
In group A [Graph 3], mean FM measured pre-operatively was 379.6±23.36 mm, 391.2±24.119 mm after 24 h, 382.86±23.18) mm after 72 h and 380.2±23.32 on the seventh post-operative day. In group B, the mean FM measured pre-operatively was 355.4±24.49 mm, 383.3±25.93 mm after 24 h, 371.53±23.76 mm after 72 h and 357.73±24.38 mm on the seventh post-operative day. The mean difference in change in FM between the two groups after applying the independent sample t-test was statistically highly significant after 24 h (P = 0.001) and 72 h (P = 0.0001), and still significant on the seventh post-operative day (P = 0.047).
Graph 3.
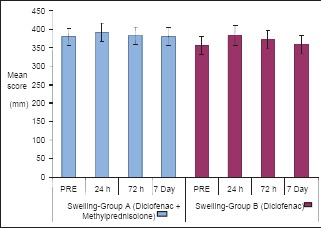
Comparing the mean facial measurement between group A and group B
No post-operative complications were found in any of the two groups. The wound healing was found to be satisfactory in all the patients.
DISCUSSION
Extraction of the third molar, as with any surgical procedure, results in an intense inflammatory response that consists of edema, erythema, pain, rise in temperature and loss of function. Pain reaches its peak at 6 h post-operatively and swelling reaches its maximum on the first post-operative evening and remains at a high level until the fourth day.[4] Extending a surgical procedure more than 10 min results in more post-operative sequelae.[14] An ideal drug for administration after the surgical removal of an impacted lower third molar should alleviate pain, reduce inflammation, trismus, facilitate healing and cause no undesirable side-effects.[6]
It is now universal knowledge that steroids reduce post-operative complications. In spite of their obvious numerous benefits, their use is mostly limited by most surgeons due to their association with a host of potential side-effects, most of which are relative to mineralocorticoid activity and and/or chronic dosing regimens.[15,16] Hypothalmic–pituitary-adrenal (HPA) axis suppression, which is a significant phenomenon only with chronic dosing, should not, however, be a contraindication to the use of steroids in third molar surgery.[15,16,17] Corticosteroid doses for less than 5-7 days result in insignificant HPA suppression and cortisol levels return to the normal value in 5-7 days.[6,18,19,20] Such short-term steroid therapy is safe in the absence of contraindications to its use, as listed by Pederson et al.[21] In this study, glucocorticosteroids for only 3 days were given to minimize potential side-effects and true contraindications.
Methylprednisolone is five times more potent than hydrocortisone and has non-existent mineral-corticoid action.[8,9] Al-Khateeb et al. conducted a randomized study to determine the efficacy of dexamethasone versus methylprednisolone, and concluded that pain and trismus was more reduced in the methylprednisolone group.[10] Several other research articles have also shown that swelling and pain that developed after third molar removal were significantly reduced by methylprednisolone,[22,23] Therefore, methylprednisolone was the drug of choice among steroids.
For steroids, different modes of administration have been conducted and recommended in different studies. The IV route offers instantaneous blood levels, but while high-dosing IV studies have demonstrated significant short-term improvements, the effects were not sustained. Rebound swelling can occur if the duration of use is inadequate; therefore, it is important to maintain the levels of short-duration steroid formulations for more than 1 day.[1,24,25] The IM route provides an anti-inflammatory effect for long, but it may cause a higher risk of adrenaline suppression. Other hindrances to percutaneous routes include necessary operator experience, armamentarium and patient discomfort.[7]
The convenience of oral dosing, in contrast, has general appeal,[7] With the oral route, glucocorticosteroids are rapidly and almost completely absorbed, making them as effective as parenteral avenues.[7] Post-operative dosing was also found to be successfully effective.[7,26] Therefore, in the present study, the oral route and post-operative dosing were selected.
Methyprednisolone has an intermediate half-life of 18-36 h.[9] When glucocorticosteroids are orally administered, repeated dosing is required to maintain adequate blood levels throughout the immediate post-operative period.[7] There is a need to continue corticosteroid therapy for a minimum of 3 days because swelling in patients treated with steroids does not appear to peak until the third day after surgery.[1,25] Previous investigations, however, are not convincing regarding clinical improvement following oral administration because of low dosing schedules and short observation periods.[15,18,22,27,28] Corticosteroid doses to be significantly effective should range from 80 to 625 mg hydrocortisone equivalent anti-inflammatory dosage, which in case of methylprednisolone is 16–125 mg.[28] It has also been corroborated that a dosage of methylprednisolone of less than or equal to 40 mg does not produce any adverse systemic effects.[29] Therefore, in the present study, 24 mg of methylprednisolone was given in three divided doses for three days and no side-effects were observed following administration of the steroid. It has been established that tapering off doses is not mandatory in short-term dosing.[30] In this research too, steroid was terminated without tapering dose.
A few authors believe that corticosteroids are the drug of choice in preventing edema; however, NSAIDs may be required for better pain relief.[22,23,31] Diclofenac is known to possess both analgesic and anti-inflammatory effects. Previous studies have proven that diclofenac sodium reduces pain and swelling more, if not equally effective, when compared with other single anti-inflammatory drugs and/or fixed drug combinations after impacted third molar removal.[13,28,32,33,34] It can therefore be used as an agent to control post-operative sequelae and was the NSAID of choice for this study. Of its three dispensable forms, namely intravenous infusion, soft gel and tablets, per-oral tablets were favored because of the limited duration of action and higher cost of treatment with infusions and gel.[35,36] Further, pre-operative use of NSAIDs may not offer a pre-emptive analgesic effect in patients who have had adequate analgesia during the surgery.[37] Continued use of analgesic drugs during the post-operative period is therefore recommended by most authors, and was followed in the present study too.
While the sample size for this study is not large by any means, it was nevertheless adequate for statistical purposes, given the implied limitation of time period in a dissertation. A placebo group comprising of patients not being given NSAIDs was thought implausible and corrupt on moral and ethical grounds, because pain follows this kind of surgery, even if the severe post-operative pain is of a short duration.
Calibrating and measuring pain is always a difficult proposition. Of the various pain scales available for adults, namely, VAS, verbal numerical rating scale and verbal descriptor scale, the VAS was chosen for this study. It is a pain scale where each patient indicates his/her perceived pain intensity along a 100 mm horizontal line.[38] Whether it is a linear scale or not, or whether the data are ratio or ordinal, is still debatable. But, it is undoubtedly the most widely used and popular pain scale, which correlates well with acute pain and with minimal error, and easily lends itself to statistical analysis as well.[38]
Simultaneous administration of glucocorticosteroid may synergize the anti-inflammatory effect of NSAIDs and contribute to the reduction of inflammatory exudates as well as edema and pain.[5] Therefore, the co-administration of diclofenac and methylprednisolone may be expected to reduce post-operative pain more than that achieved with either of them alone. Evidence supporting this postulation was provided by Bamgbose et al., Buyukkurt et al., Hyrkas et al., Schultze-Mosgau et al. (1995) and others, who found the NSAID–steroid combination to be better than NSAID alone in the treatment of post-operative pain, trismus and swelling after dental surgical procedures.[5,36,39,40] Our results corroborate this theory.
It is well known that steroids suppress immune function, increasing the potential risk of infection. However, use of usual dosages of corticosteroids over 3-4 days has no significant adverse effects on wound healing, as further emphasized by our study.[19,20] We did not encounter any cases of infection, especially in the combination group, because glucocorticosteroids were used only for 3 days and also because antibiotics were administered to both the groups.
CONCLUSION
It was concluded that a single class of drugs is not maximally effective in controlling both post-operative pain and swelling and trismus. The combination of diclofenac sodium (a NSAID) and methylprednisolone (a corticosteroid) is more effective than diclofenac sodium alone in the sequelae of oral surgical procedures. Therefore, this pharmaceutical combination should be considered for the attenuation of post-operative sequelae in healthy patients undergoing surgical removal of the impacted third molar.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
ACKNOWLEDGMENT
The authors would like to express their heartfelt gratitude to Dr. Hemant Batra and Dr. Rahul Datta for their constant help, guidance and support during the conduction of this study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Ness GM, Peterson LJ. Impacted Teeth. In: Miloro M, Ghali GE, Larsen PE, Waite PD, editors. Peterson's principles of oral and maxillofacial surgery. Vol. 1. Hamilton, London: B.C. Decker Inc; 2004. p. 149. [Google Scholar]
- 2.Pogrel MA. Kaban LB, Pogrel MA, Perrot DH. Complications in oral and maxillofacial surgery. Philadelphia: W.B. Saunders; 1997. Complications of third molar surgery; p. 65. [Google Scholar]
- 3.Krekmanov L, Nordenram A. Postoperative complications after surgical removal of mandibular third molars. Int J Oral Maxillofac Surg. 1986;15:25. doi: 10.1016/s0300-9785(86)80007-2. [DOI] [PubMed] [Google Scholar]
- 4.Berge TI, Boe OE. Predictor evaluation of postoperative morbidity after surgical removal of mandibular third molar. Acta Odontol Scand. 1994;52:162. doi: 10.3109/00016359409027591. [DOI] [PubMed] [Google Scholar]
- 5.Bamgbose BO, Akinwande JA, Adeyemo WL, Ladeinde AL, Arotiba GT, Ogunlewe MO. Effects of co-administered Dexamethasone and Diclofenac potassium on pain, swelling and trismus following third molar surgery. Head Face Med. 2005;1:11. doi: 10.1186/1746-160X-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Troullos ES, Hargreaves MK, Butler DP, Dionne RA. Comparison of non steroidal anti-inflammatory drugs, ibuprofen and flurbiprofen, with Methylprednisolone and placebo for acute pain, swelling and trismus. J Oral Maxillofac Surg. 1990;48:945–52. doi: 10.1016/0278-2391(90)90007-o. [DOI] [PubMed] [Google Scholar]
- 7.Montgomery MT, Hogg JP, Roberts DL, Redding SW. The use of glucoticosteroids to lessen the inflammatory sequelae following third molar surgery. J Oral Maxillofac Surg. 1990;48:179–87. doi: 10.1016/s0278-2391(10)80207-1. [DOI] [PubMed] [Google Scholar]
- 8.Esen E, Tasar F, Akhan O. Determination of the anti-inflammatory effects of methylprednisolone on the sequelae of third molar surgery. J Oral Maxillofac Surg. 1999;57:1201–6. doi: 10.1016/s0278-2391(99)90486-x. [DOI] [PubMed] [Google Scholar]
- 9.Schimmer BP, Parker LL. Hardman JG, Limbird LE. Goodman and Gilman's The pharmacological basis of therapeutics. New York: McGraw-Hill; 2001. Adrenocortical steroids and their synthetic analogues; p. 1587. [Google Scholar]
- 10.Al-Khateeb TL, Marouf FA, Mahmoud MA. Clinical evaluation of dexamethasone vs methylprednisolone for reducing postoperative inflammatory sequelae following third molar surgery amongst preschool children in Jeddah, Saudi Arabia. Saudi Dent J. 1996;8:13. [Google Scholar]
- 11.Ustun Y, Erdogan O, Esen E, Karsli ED. Comparison of the effects of 2 doses of Methylprednisolone on pain, swelling, and trismus after third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:535–9. doi: 10.1016/S1079210403004645. [DOI] [PubMed] [Google Scholar]
- 12.Howe GL. The management of impacted mandibular third molar. In: Howe GL, editor. Minor oral surgery. Bombay, India: Varghese Publishing House; 1988. p. 109. [Google Scholar]
- 13.Henrikson PA, Thilander H, Wahlander LA. Voltaren as analgesic after surgical removal of a lower wisdom tooth. Int J Oral Surg. 1985;14:333–8. doi: 10.1016/s0300-9785(85)80022-3. [DOI] [PubMed] [Google Scholar]
- 14.Hellem S, Nordenram A. Prevention of postoperative symptoms by general antibiotic treatment symptoms by general antibiotic treatment and local bandage in removal of mandibular third molar. Int J Oral Surg. 1973;2:273–8. doi: 10.1016/s0300-9785(73)80022-5. [DOI] [PubMed] [Google Scholar]
- 15.Nathanson NR, Scifert DM. Betamethasone in dentistry. A clinical report. Oral Surg Oral Med Oral Pathol. 1964;18:715–21. doi: 10.1016/0030-4220(64)90469-4. [DOI] [PubMed] [Google Scholar]
- 16.Novak E, Stubbs SS, Seckman CE, Hearron MS. Effects of a single large intravenous dose of methylprednisolone sodium succinate. Clin Pharmacol Ther. 1970;11:711–7. doi: 10.1002/cpt1970115711. [DOI] [PubMed] [Google Scholar]
- 17.Mitchell JA, Warner TD. Cyclo-oxygenase-2: Pharmacology, physiology, biochemistry and relevance to NSAIDS therapy. Br J Pharmacol. 1999;128:1121–32. doi: 10.1038/sj.bjp.0702897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hooley JR, Francis FH. Betamethasone in traumatic oral surgery. J Oral Surg. 1969;27:398–403. [PubMed] [Google Scholar]
- 19.Gersema L, Baker K. Use of corticosteroids in oral surgery. J Oral Maxillofac Surg. 1992;50:270–7. doi: 10.1016/0278-2391(92)90325-t. [DOI] [PubMed] [Google Scholar]
- 20.Butler RC, Vorono AA, Finstuen K. Dosage effect of pulsed steroid therapy on serum cortisol levels in oral and maxillofacial surgery patients. J Oral Maxillofac Surg. 1993;51:750–3. doi: 10.1016/s0278-2391(10)80414-8. [DOI] [PubMed] [Google Scholar]
- 21.Pedersen A. Decadronphosphate in the relief of complaints after third molar surgery: A double-blind, controlled trial with bilateral oral surgery. Int J Oral Surg. 1985;14:235–40. doi: 10.1016/s0300-9785(85)80034-x. [DOI] [PubMed] [Google Scholar]
- 22.Holland CS. The influence of methylprednisolone on postoperative swelling following oral surgery. Br J Oral Surg. 1987;25:293–9. doi: 10.1016/0266-4356(87)90068-4. [DOI] [PubMed] [Google Scholar]
- 23.Beirne OR, Hollander B. The effect of Methylprednisolone on pain, trismus and swelling after removal of third molars. Oral Surg Oral Med Oral Pathol. 1986;61:134–8. doi: 10.1016/0030-4220(86)90173-8. [DOI] [PubMed] [Google Scholar]
- 24.Neupert EA, 3rd, Lee JW, Philput CB, Gordon JR. Evaluation of dexamethasone for reduction of postsurgical sequelae of third molar removal. J Oral Maxillofac Surg. 1992;50:1177–82. doi: 10.1016/0278-2391(92)90149-t. [DOI] [PubMed] [Google Scholar]
- 25.Milles M, Desjardins J. Reduction of postoperative facial swelling by low dose methylprednisolone. J Oral Maxillofac Surg. 1993;51:987–91. doi: 10.1016/s0278-2391(10)80041-2. [DOI] [PubMed] [Google Scholar]
- 26.Skjelbred P, Lokken P. Reduction of pain and swelling by a corticosteroid injected 3 hours after surgery. Eur J Clin Pharmacol. 1982;21:141–6. doi: 10.1007/BF00545968. [DOI] [PubMed] [Google Scholar]
- 27.Linenberg WB. The clinical evaluation of dexamethasone in oral surgery. Oral Surg Oral Med Oral Pathol. 1965;20:6. [Google Scholar]
- 28.Caci F, Gluck GM, Hackensack NJ. Double blind study of Prednisolone and Papase as inhibitors of complications after oral surgery. J Am Dent Assoc. 1976;93:325–7. doi: 10.14219/jada.archive.1976.0484. [DOI] [PubMed] [Google Scholar]
- 29.Campbell WI, Kendrick RW. Postoperative dental pain, a comparative study of anti-inflammatory and analgesic agents. Ulster Med J. 1991;60:39–43. [PMC free article] [PubMed] [Google Scholar]
- 30.Alexander RE, Throndson RR. A review of perioperative corticosteroid use in dentoalveolar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:406–15. doi: 10.1067/moe.2000.109778. [DOI] [PubMed] [Google Scholar]
- 31.Bahn SL. Glucocorticosteroids in dentistry. J Am Dent Assoc. 1982;105:476–81. doi: 10.14219/jada.archive.1982.0357. [DOI] [PubMed] [Google Scholar]
- 32.Bailey BM, Zaki G, Rotman H, Woodwards RT. A double-blind comparative study of soluble Aspirin and Diclofenac dispersible in the control of post-extraction pain after removal of impacted third molars. Int J Oral Maxillofac Surg. 1993;22:238. doi: 10.1016/s0901-5027(05)80645-9. [DOI] [PubMed] [Google Scholar]
- 33.Sisk A, Bonnington GJ. Evaluation of Methylprednisolone and Flurbiprofen for inhibition of post-operative inflammatory response. Oral Surg Oral Med Oral Pathol Oral Radiol. 1985;60:137. doi: 10.1016/0030-4220(85)90281-6. [DOI] [PubMed] [Google Scholar]
- 34.Walton GM, Rood JP, Snowdon AT, Rickwood D. Ketorolac and diclofenac for postoperative pain relief following oral surgery. Br J Oral Maxillofac Surg. 1993;31:158–60. doi: 10.1016/0266-4356(93)90115-d. [DOI] [PubMed] [Google Scholar]
- 35.Zuniga JR, Phillips CL, Shugars D, Lyon JA, Peroutka SJ, Swarbrick J, et al. Analgesic safety and efficacy of Diclofenac sodium softgels on post-operative third molar extraction pain. J Oral Maxillofac Surg. 2004;62:806–15. doi: 10.1016/j.joms.2003.12.019. [DOI] [PubMed] [Google Scholar]
- 36.Hyrkas T, Ylipaavalniemi P, Oikarinen VJ, Paakkari I. Preoperative intravenous Diclofenac for post-operative pain prevention in outpatients. Br J Oral Maxillofac Surg. 1993;31:35. doi: 10.1016/0266-4356(93)90189-4. [DOI] [PubMed] [Google Scholar]
- 37.Zacharias M, Hunter KM, Baker AB. Effectiveness of preoperative analgesics on postoperative dental pain: A study. Anesth Prog. 1996;43:92–6. [PMC free article] [PubMed] [Google Scholar]
- 38.Myles PS, Troedel S, Boquest M, Reeves M. The pain visual analog scale: Is it linear or non-linear? Anesth Analg. 1999;89:1517–20. doi: 10.1097/00000539-199912000-00038. [DOI] [PubMed] [Google Scholar]
- 39.Buyukkurt MC, Gungormus M, Kaya O. The effect of a single dose Prednisolone with and without diclofenac on pain, trismus and swelling after removal of mandibular third molars. J Oral Maxillofac Surg. 2006;64:1761–6. doi: 10.1016/j.joms.2005.11.107. [DOI] [PubMed] [Google Scholar]
- 40.Schultze-Mosgau S, Schmelzeisen R, Frolich JC, Schmele H. Use of Ibuprofen and Methylprednisolone for the prevention of pain and swelling after removal of impacted third molars. J Oral Maxillofac Surg. 1995;53:2–7. doi: 10.1016/0278-2391(95)90486-7. [DOI] [PubMed] [Google Scholar]


