Abstract
The premise of complete ossification of midpalatal suture in early adulthood still has its popularity, though conflicting data are emerging in the literature. A 49-year-old male and a 54-year-old female Iranian patient, both dentulous, were referred to a Maxillofacial Radiology Center to be evaluated for implant insertion. In cone-beam computed tomography (CBCT) evaluation, an in-ossified suture was found in anterior two-third of midpalatal region of both individuals. The application of clinical vignettes from CBCT findings for maxillofacial orthodontic and orthopedic purposes is of value. Existing cases of successful nonsurgical rapid palatal expansion of maxilla in adults could surrogate this dogma about timing for ossification of midpalatal suture which is considered as a purely chronologic-related phenomenon and transmitted masticatory forces may be one possible cause (functional hypothesis).
Keywords: Orthodontic, orthopedic, ossification, suture, treatment
INTRODUCTION
Based on a premise, passing the growth spurt make it theoretically almost impossible to move palatal halves away by conventional methods.[1] This timetable is about 12–13 and 14–15 years of age for female and male teenagers, respectively. Afterward, the rapid maxillary expansion (rapid palatal expansion [RPE]) with hyrax screws would be helpful.[1] It is presumed that palatal halves will eventually interdigitated to that degree that even heavy forces driven by hyrax will be of no benefit, nevertheless, surgical separation of maxillary vault from midline, so called surgically assisted RPE (SARPE) is the current possible option.[2] The latter is currently performed beyond the age of 19–20, when palatal shelves could be no more separated by in-office forces and appliances.[2]
If a clinical decision is merely based on a chronologic age, this could put the clinician in a great uncertainty about whether the suture is ossified. In case of immature suture, the patient may still benefit from the RPE by a hyrax screw costing about a few 100 dollars escaping from SARPE with considerable higher cost and co-morbidities.[2] These facts that many patients decline the surgical option and the existing of aged patients with incomplete midpalatal suture ossification should be reemphasized.[1,3] In these cases reports, a dogmatic slumber of a widely accepted misbelieves on midpalatal suture ossification timetable is reviewed and discussed.
CASE REPORT
The first case was a 49-year-old Iranian male patient and the second patient was a 54-year-old Iranian ethnic female individual, both were referred for implant surgery. The past dental and medical history was not significant except for cigarette smoking and mild coronary artery disease for the first patient and controlled diabetes mellitus receiving insulin injection for the second patient.
In cone-beam computed tomography (CBCT) scan of the first patient, there was a complete ossification beyond the maxillo-palatine suture at the posterior one-third and the rest of the suture appeared as two semi-parallel hyper-dense lines continued to the incisive canal [Figure 1].
Figure 1.
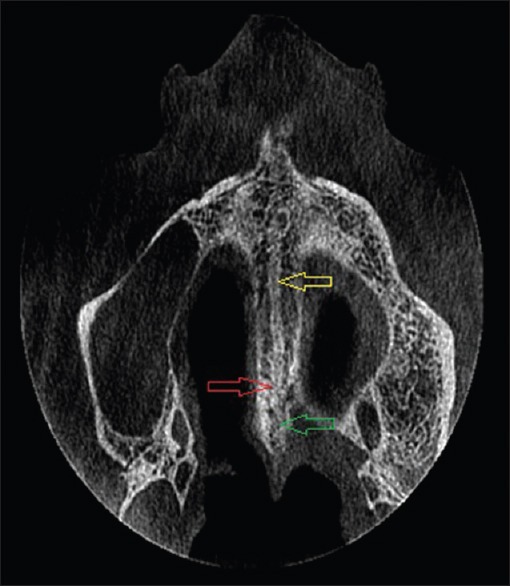
Paraxial view of the hard palate of the first patient. Note ossification at posterior portion and incomplete ossification at anterior portion. Yellow (superior) arrow points toward parallel hyper-dense lines with intermediate hypo-dense area. Red (middle) arrow indicates the location of maxilla-palatine suture and green (lower) arrow corresponds to posterior fusion of palatal halves
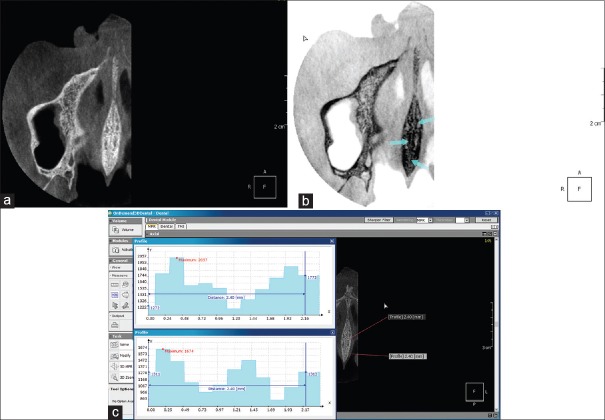
Evaluation of the second patient revealed the posterior third ossification which continued anteriorly as interdigitating cortical plates of approaching halves and also separated parallel lines [Figure 2a–c].
Figure 2.
(a-c) Axial cone-beam computed tomography slices of the second patient. (a) note the posterior fusion and interdigitating of more anterior parts. (b) Invert view. Note the fusion, parallel line portion, and interdigitating portion. Darker areas indicated denser parts (cortical vs. cancellous bone). (c) Comparison of gray scale range of two horizontal lines intersecting complete and incomplete fused parts. Darker areas indicated denser parts (cortical vs. cancellous bone). The center of these imaginary line was set at the midline bisecting the incisive foramen (i.e., corresponds to point 1.2 mm of the figure with 1.2 mm extension to each side)
DISCUSSION
In these two case presentations, incomplete ossification of midpalatal suture is reported in patients in their late 40's and mid 50's.
The direction of ossification is controversial. Schlegel et al. and Persson and Thilander believed that ossification is more profound in posterior region of the hard palate.[4,5] Related by Schlegel et al., ossification begins on oral side.[4] N’Guyen et al., however, discovered that ossification process was completed only in anterior third of the palate leaving the posterior third with just connective tissue and hyalinization in 20 human cadavers aged around 70.[6] On the contrary to N’Guyen et al., and in agreement with Persson and Thilander and Schlegel et al. interdigitation and commencing of maturation was noted in posterior portion in our reported cases, while there was no complete maturation in anterior region.
The rate and intensity of ossification are also influenced by gender, diet, and race.[1,2,4,6] The beginning of formation of the suture is well described prenatally by Latham.[7] He explained that the premaxilla (i.e., anterior to the incisive canal) forms at about 45 days and the two palatal shelves develop at about 12 weeks. This process will be further completed along with downward pushing of tongue and downward-inward movement of each shelf toward the other one. Melsen followed this process postnatally and described three distinct histological stages: Synfibrosis (broad gap with parallel border), synarthrosis (sinus pattern approximation of walls), and synostosis (complete interdigitation).[8]
Against the clarity about development onset of the hard palate, however, there is no census on time of the completion of ossification at midline fusion line. A great inter-individual variability is described in the literature for complete ossification of midpalatal suture.[4,5,8] Our cases still had a unossified suture at the age of 49 and 54 years.
Earliest histology proven reported ossification was related to a 16-year-old female patient in Melsen studied samples. Five out of 24 female patients aged 11–14 years had CBCT-based complete fusion of maxillary suture in Angelieri et al., study.[3] Of interest, even there were 54 and 71-year-old patients who had unossified sutures, reported by Schlegel et al., (i.e., histological study) and Korbmacher et al., (micro-computerized tomography study), respectively.[4,9] In addition, N’Guyen et al., studied 20 male cadavers aged over 70 years by both histological and radiographic methods.[6] Surprisingly, they elucidated that ossification was occurred only in anterior third and there was no ossification behind that portion.
As ossification progresses, interdigitation accentuates and the gap between two approaching sides decreases. Ultimately, two cortical layers fuse with a resultant hyper-dense midline.[1] Separation of two halves is feasibly possible in synfibrosis, more demanding in synarthrosis and almost impossible with conventional in-office methods in synostosis classification by Melsen.[8]
Regarding the in-ossified region (upper diagram), as presented in Figure 2c, the gray scale abruptly dropped at the midline surrounding by two peaks which were related to two hyper-dense walls of approaching shelves. A rather opposite pattern was observed for complete mature part with a relative hyper-dense area at almost midline surrounding by immediate hypo-dense adjacent areas. The peak measured density of midline infused part is around 1470 which is lower than approaching cortical layers in not ossified part with the peak measured density of 2057. One possible explanation for the lower density of midline in comparison to the adjacent outer cortical layers is that two midline cortical layers get revolutionized and are gradually displaced by the cancellous bone.[1]
The nidus for “Functional hypothesis” is originated from the observation of N’Guyen et al., who demonstrated the sutures without complete ossification beyond the 8th decade in humans.[6] They attributed these findings to the masticatory forces that are transmitted to the midline palate via alveolar bone.[6] This incident may have a benefit of shock-absorbing potential.[7] Both of our cases were dentulous without two or more adjacent missing teeth in posterior region. Hence, midpalatal suture is the solitary suture that may never ossify completely throughout life. With this regards, we call this suture as “Unique Functional Suture.”
Financial support and sponsorship
Nil.
Conflicts of interest
Authors declare no conflicts of interest.
REFERENCES
- 1.Stuart DA, Wiltshire WA. Rapid palatal expansion in the young adult: Time for a paradigm shift? J Can Dent Assoc. 2003;69:374–7. [PubMed] [Google Scholar]
- 2.Fricke-Zech S, Gruber RM, Dullin C, Zapf A, Kramer FJ, Kubien-Meesenburg D, et al. Measurement of the midpalatal suture width a comparison of flat-panel volume computed tomography to histomorphometric analysis in a porcine model. Angle Orthod. 2012;8:145–50. doi: 10.2319/040311-238.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Angelieri F, Cevidanes LH, Franchi L, Gonçalves JR, Benavides E, McNamara JA., Jr Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2013;144:759–69. doi: 10.1016/j.ajodo.2013.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schlegel KA, Kinner F, Schlegel KD. The anatomic basis for palatal implants in orthodontics. Int J Adult Orthodon Orthognath Surg. 2002;17:133–9. [PubMed] [Google Scholar]
- 5.Persson M, Thilander B. Palatal suture closure in man from 15 to 35 years of age. Am J Orthod. 1977;72:42–52. doi: 10.1016/0002-9416(77)90123-3. [DOI] [PubMed] [Google Scholar]
- 6.N’Guyen T, Ayral X, Vacher C. Radiographic and microscopic anatomy of the mid-palatal suture in the elderly. Surg Radiol Anat. 2008;30:65–8. doi: 10.1007/s00276-007-0281-6. [DOI] [PubMed] [Google Scholar]
- 7.Latham RA. The development, structure and growth pattern of the human mid-palatal suture. J Anat. 1971;108(Pt 1):31–41. [PMC free article] [PubMed] [Google Scholar]
- 8.Melsen B. Palatal growth studied on human autopsy material. A histologic microradiographic study. Am J Orthod. 1975;68:42–54. doi: 10.1016/0002-9416(75)90158-x. [DOI] [PubMed] [Google Scholar]
- 9.Korbmacher H, Schilling A, Püschel K, Amling M, Kahl-Nieke B. Age-dependent three-dimensional microcomputed tomography analysis of the human midpalatal suture. J Orofac Orthop. 2007;68:364–76. doi: 10.1007/s00056-007-0729-7. [DOI] [PubMed] [Google Scholar]