Abstract
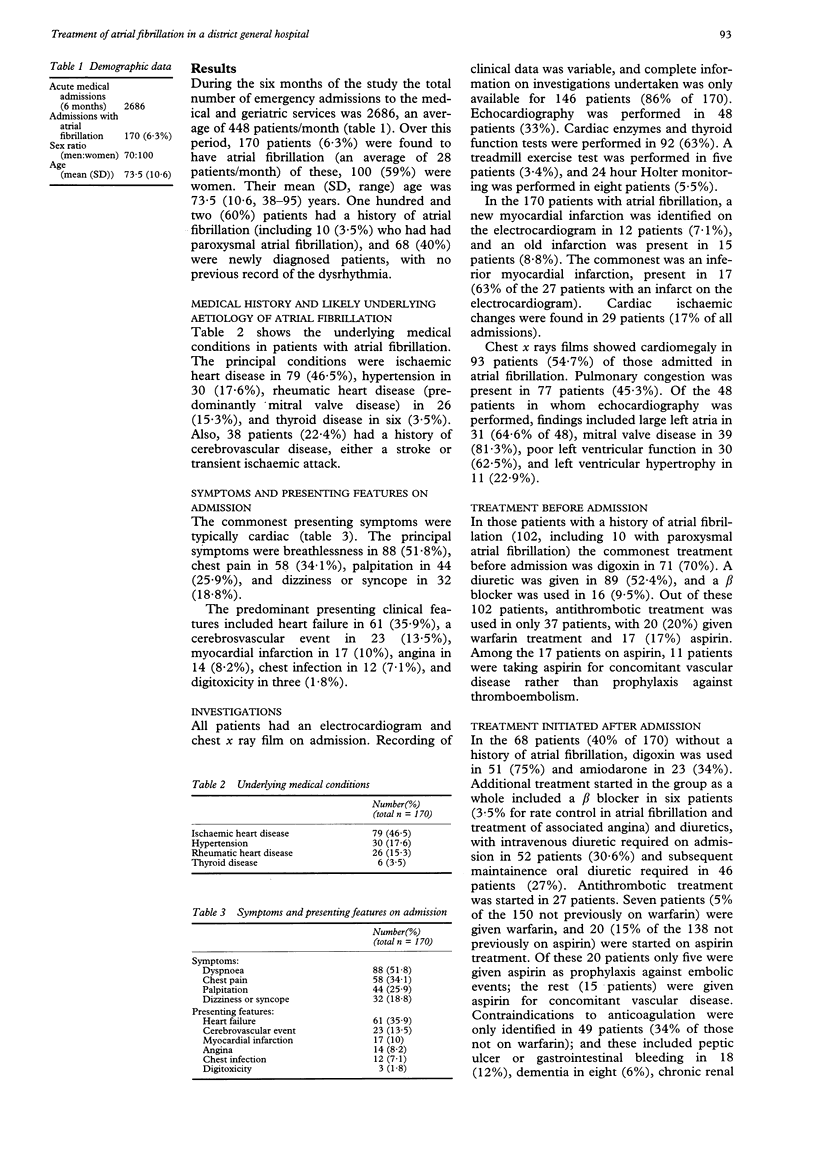
OBJECTIVE--To assess current strategies used to investigate and manage acute atrial fibrillation in hospital. DESIGN--Prospective survey of all acute admissions over 6 months. SETTING--District general hospital serving a population of 230,000 in north east Glasgow. SUBJECTS--2686 patients admitted as emergency cases over 6 months. RESULTS--Of the 2686 patients, 170 (age range 38-95, mean (SD) 73.5 (10.6) years; 70 men (41%) and 100 women (59%)) were admitted with atrial fibrillation. The principal underlying medical conditions were ischaemic heart disease in 79 (46.5%), rheumatic heart disease in 26 (15.3%), and thyroid disease in six (3.5%). Cardiac failure was present on admission in 61 (36%), cerebrovascular events in 23 (14%), and myocardial infarction in 17 (10%). Of those with a history of atrial fibrillation (102 (60%) including 10 with paroxysmal atrial fibrillation) treatment on admission included digoxin in 71 (70%), warfarin in 20 (20%), and aspirin in 17 (17%); the aspirin was predominantly given for concomitant vascular disease. The mean (SD) inpatient stay was 16 days (19.7) (range 1-154) largely due to the patients with stroke. Thyroid function tests were performed in only 63% and echocardiography in 33%. Overall, the rate of introduction of anticoagulation (seven patients) and attempted cardioversion (21 patient: 19 pharmacological and two electrical) was surprisingly low. Only 49 patients (34% of those not on warfarin) had contraindications to anticoagulation: these included peptic ulcer or gastrointestinal bleeding in 18 (12%), dementia in eight (6%), chronic renal failure or dialysis in eight (6%), and alcohol excess in four (3%). CONCLUSION--Standard investigations were inadequately used in patients with atrial fibrillation and there was a reluctance to perform cardioversion or to start anticoagulant treatment.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dunn M., Alexander J., de Silva R., Hildner F. Antithrombotic therapy in atrial fibrillation. Chest. 1989 Feb;95(2 Suppl):118S–127S. doi: 10.1378/chest.95.2_supplement.118s. [DOI] [PubMed] [Google Scholar]
- Forfar J. C., Miller H. C., Toft A. D. Occult thyrotoxicosis: a correctable cause of "idiopathic" atrial fibrillation. Am J Cardiol. 1979 Jul;44(1):9–12. doi: 10.1016/0002-9149(79)90243-1. [DOI] [PubMed] [Google Scholar]
- Goldberg R. J., Seeley D., Becker R. C., Brady P., Chen Z. Y., Osganian V., Gore J. M., Alpert J. S., Dalen J. E. Impact of atrial fibrillation on the in-hospital and long-term survival of patients with acute myocardial infarction: a community-wide perspective. Am Heart J. 1990 May;119(5):996–1001. doi: 10.1016/s0002-8703(05)80227-3. [DOI] [PubMed] [Google Scholar]
- Lipkin D. P., Frenneaux M., Stewart R., Joshi J., Lowe T., McKenna W. J. Delayed improvement in exercise capacity after cardioversion of atrial fibrillation to sinus rhythm. Br Heart J. 1988 May;59(5):572–577. doi: 10.1136/hrt.59.5.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe G. D. Antithrombotic treatment and atrial fibrillation. BMJ. 1992 Dec 12;305(6867):1445–1446. doi: 10.1136/bmj.305.6867.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parameshwar J., Poole-Wilson P. A., Sutton G. C. Heart failure in a district general hospital. J R Coll Physicians Lond. 1992 Apr;26(2):139–142. [PMC free article] [PubMed] [Google Scholar]
- Petersen P., Boysen G., Godtfredsen J., Andersen E. D., Andersen B. Placebo-controlled, randomised trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study. Lancet. 1989 Jan 28;1(8631):175–179. doi: 10.1016/s0140-6736(89)91200-2. [DOI] [PubMed] [Google Scholar]
- Rebello R., Brownlee W. C. Intermittent ventricular standstill during chronic atrial fibrillation in patients with dizziness or syncope. Pacing Clin Electrophysiol. 1987 Nov;10(6):1271–1276. doi: 10.1111/j.1540-8159.1987.tb04963.x. [DOI] [PubMed] [Google Scholar]
- Wolf P. A., Abbott R. D., Kannel W. B. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991 Aug;22(8):983–988. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- Wolf P. A., Dawber T. R., Thomas H. E., Jr, Kannel W. B. Epidemiologic assessment of chronic atrial fibrillation and risk of stroke: the Framingham study. Neurology. 1978 Oct;28(10):973–977. doi: 10.1212/wnl.28.10.973. [DOI] [PubMed] [Google Scholar]
- Wolf P. A., Kannel W. B., McGee D. L., Meeks S. L., Bharucha N. E., McNamara P. M. Duration of atrial fibrillation and imminence of stroke: the Framingham study. Stroke. 1983 Sep-Oct;14(5):664–667. doi: 10.1161/01.str.14.5.664. [DOI] [PubMed] [Google Scholar]



