Abstract
Background:
Old pelvis fractures are among the most challenging fractures to treat because of their complex anatomy, difficult-to-access surgical sites, and the relatively low incidence of such cases. Proper evaluation and surgical planning are necessary to achieve the pelvic ring symmetry and stable fixation of the fracture. The goal of this study was to assess the use of three-dimensional (3D) printing techniques for surgical management of old pelvic fractures.
Methods:
First, 16 dried human cadaveric pelvises were used to confirm the anatomical accuracy of the 3D models printed based on radiographic data. Next, nine clinical cases between January 2009 and April 2013 were used to evaluate the surgical reconstruction based on the 3D printed models. The pelvic injuries were all type C, and the average time from injury to reconstruction was 11 weeks (range: 8–17 weeks). The workflow consisted of: (1) Printing patient-specific bone models based on preoperative computed tomography (CT) scans, (2) virtual fracture reduction using the printed 3D anatomic template, (3) virtual fracture fixation using Kirschner wires, and (4) preoperatively measuring the osteotomy and implant position relative to landmarks using the virtually defined deformation. These models aided communication between surgical team members during the procedure. This technique was validated by comparing the preoperative planning to the intraoperative procedure.
Results:
The accuracy of the 3D printed models was within specification. Production of a model from standard CT DICOM data took 7 hours (range: 6–9 hours). Preoperative planning using the 3D printed models was feasible in all cases. Good correlation was found between the preoperative planning and postoperative follow-up X-ray in all nine cases. The patients were followed for 3–29 months (median: 5 months). The fracture healing time was 9–17 weeks (mean: 10 weeks). No delayed incision healing, wound infection, or nonunions occurred. The results were excellent in two cases, good in five, and poor in two based on the Majeed score.
Conclusions:
The 3D printing planning technique for pelvic surgery was successfully integrated into a clinical workflow to improve patient-specific preoperative planning by providing a visual and haptic model of the injury and allowing patient-specific adaptation of each osteosynthesis implant to the virtually reduced pelvis.
Keywords: Old Fracture, Pelvis, Preoperative Planning, Surgery, Three-dimensional Printing
INTRODUCTION
The treatment of old pelvic fractures is challenging for surgeons because of significant intraoperative difficulties and postoperative uncertainties. Few treatment cases have been reported in the literature. Thus, there is no widely accepted treatment strategy for old pelvic fractures. The primary goals of pelvic surgery are to restore the integrity and symmetry of the pelvic ring, paying careful attention managing soft tissue, to facilitate a rapid postoperative recovery with early rehabilitation, and to achieve a long-term functioning hip joint.[1,2] Proper patient evaluation and surgical planning are necessary to achieve these goals. To obtain the best outcomes, a wide range of preoperative planning techniques can be applied, some of which provide surgeons with an opportunity to practice and refine the planned procedure. Such practice may improve the surgeon's efficiency in the operating room, shorten the operative time, and reduce the incidence of iatrogenic complications. The traditional two-dimensional images often fail to capture the complex pelvic anatomy, whereas three-dimensional (3D) imaging technology and software expands the capabilities of planning and surgical practice alike. Because proprietary hardware, software, and service products can be costly, it is important to combine open reduction and internal fixation with 3D printing technology to economically and effectively prepare for the surgical reconstruction of complex pelvic deformities.[3,4] In the present paper, we describe a technique to prepare for the surgical reconstruction of deformed pelvises. This technique provided us with an affordable, reproducible, and personalized 3D printed template of the pelvis before surgical intervention, allowing us to preoperatively practice and refine our surgical approach.
METHODS
Production and assessment of the three-dimensional printed models
Each patient's pelvis was scanned using computed tomography (CT). The CT scans were processed using the open-source software Blender, a DICOM image processing software for Windows XP. The resultant files were uploaded and printed with a CANVBOT-D900MN [Figure 1] through a commercial company (Guangruide Technology Co., Ltd., Beijing, China) that provides public access to 3D printing. The 3D printing processing chain includes: CT scanning, Blender processing, mesh processing, and 3D printing. We performed the file processing ourselves and printed the models through Guangruide Technology.
Figure 1.
The three-dimensional printer used (CANVBOT-D900MN, Guangruide Technology Co., Ltd., China).
Sixteen dried human cadaveric pelvises (supplied by Beijing Anatomic Association) were used to confirm the anatomical accuracy of the 3D models printed based on radiographic data. First, a section of a real cadaver pelvis was scanned using CT. A 3D printed model was then produced of the open section of the pelvis. The model was then validated by making measurements using digital electronic vernier calipers at defined intervals (from the tip of the ischial spine to the tip of the anterior inferior spine) along the model bones and at the same points on the real cadaver pelvis. Two observers independently measured the same segments three times each [Figure 2]. Differences between the pelvis and model measurements were assessed using a paired Student's t-test.
Figure 2.

The real acetabulum and the three-dimensional printed model.
Patients and data acquisition
Between January 2009 and April 2013, nine patients (seven males and two females) with a median age of 47 years (range: 14–51 years) were prospectively included in this study after obtaining informed consent. According to Tile classification, the pelvic injuries were type C in all nine patients (C3 in four cases, C2 with an acetabular fracture in two cases, C1 with an acetabular fracture in two cases, and C3 with a T-shaped fracture in one case). All patients underwent a whole pelvic CT scan (Sensation 64, Siemens Medical Solutions, Erlangen, Germany) on the day of admission according to the standard hospital trauma protocol. Near-isotropic axial-oriented CT images with a slice thickness of 1 mm were reconstructed using a bone kernel for sharp depiction of the bone fragment edges. The data were transferred to a picture archiving and communication system, and then we produced a model of preoperative use according to the 3D print processing workflow.
Surgical reconstruction guided by preoperative planning and intraoperative navigation using the three-dimensional printed models
The mobile fragments of the model were virtually reduced by translation and rotation operations to change the position and alignment, and the final reduction was assessed for “best fit” apposition and restoration of the anatomic architecture. The surgery was simulated using a 3D printed template. Once a satisfactory correction was achieved in the skeletal geometry, measurements of the shape of the elements to be resected were taken and analyzed for subsequent 3D templating and in vivo surgical application. With this technique, we were able use the virtual skeletal model to determine the osteotomy position and angle required to create the best wedge resection geometry for surgically correcting the deformed pelvis, even before taking the patient into the operating room.
The printed anatomic templates were used to select the best incision placement, instrumentation, osteotomy, and placement of the internal fixation devices. Kirschner wire (K-wire) axis guides were inserted to replicate the apices of the identified resection geometry. The osteotomies were performed from the anterior or posterior approaches, directed toward the central axis guidewires, as determined by the measured landmarks. Once the simulated surgical reduction was reproduced on the physical anatomic template, the osteosynthesis plating system was assembled by referencing the printed template. Next, the best plating construct was determined, and the internal fixation implant was sterilized and stored until intraoperative application to the patient. After practicing on the printed template models of the patient's pelvis, the patient was taken into the operating room where the surgical plan was executed. The planned approach was marked on the pelvis using fluoroscopic image intensification localization of the underlying bone and joint structures. Dissection was then performed to expose the malunion and nonunion sites. Once the deformity was exposed, the planned osteotomy was marked again under fluoroscopic guidance. Axis guide pins, 2.0-mm K-wires, were placed at the distal and proximal apices of the planned osteotomy based on the information from the preoperative computer simulations and physical bone model manipulations. The planned osteotomy was then performed, and the anterior ring reduced into anatomic alignment in all three planes relative to the posterior ring. The osteotomy was refined through reciprocal planning to ensure good bone-to-bone contact, and then inter-fragmental compression screw fixation was applied across the osteotomy interface. After placement of the internal fixation screws that stabilized the reduced osteotomy, the previously constructed and sterilized the plate was applied.
Evaluation
The bone and model measurement were compared to assess the anatomical accuracy of the 3D printed models. In addition, the time needed for producing the 3D printed models (building the patient-specific models from the CT datasets and the 3D printing itself), as well as the fracture union time, was recorded. In all patients, a follow-up CT was performed two to four days after the surgery. Hip function was assessed using the Majeed score. A qualitative visual analysis of the accuracy of the internal fixation was performed using hybrid renderings of the postoperative CT and respective preoperative planning guide, after manually registering the pelvic bones into the same space. The placement of the osteosynthesis implants was then compared on these renderings.
Statistical analysis
All data analyses were performed in SPSS version 17.0 software (SPSS Inc., Chicago, IL, USA). The Student's t-test was used to compare the measurements made on the 3D printed models to those from the cadaveric bones. P < 0.05 was considered statistically significant. The clinical data are reported as mean ± standard deviation (SD).
RESULTS
No statistical difference (P = 0.7943) in dimensions between the printed models and the original cadaver pelvis was found, indicating that the accuracy of the 3D printed models was within specification. Model production based on CT DICOM imaging data took 7 hours (range: 6–9 hours). The printed 3D preoperative planning was feasible in all cases. The selected surgical approach, osteotomy, and placement of the fixation plate on the pelvic ring showed very good matches between the planning and actual execution in all nine cases. A good correlation was found when comparing the postoperative follow-up CT scans to the respective preoperative planning templates. In addition, the anatomical landmark-based measurements were helpful for intraoperative navigation. The patients were followed for 3–29 months (median: 5 months). The fracture healing time was 9–17 weeks (mean: 10.7 weeks). None of the patients showed delayed healing of the incision, wound infection, or fracture nonunion. At the last follow-up, the results were excellent in two cases, good in five cases, and poor in two cases based on the Majeed scores.
Illustrative case
A 46-year-old female patient presented 8 months after being injured in a car accident. The CT scan showed a vertically displaced fracture involving the iliac blade starting 3 cm below the iliac crest and extending forward, reaching up to the acetabular roof and triradiate cartilage, involving both the anterior and posterior columns. There was a mild protrusion of the femoral head, and the fracture line extension was present until the superior pubic rami [Figure 3a–c].
Figure 3.
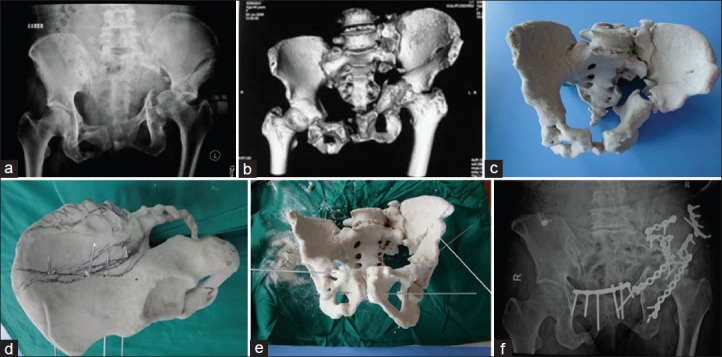
(a) Preoperative plain film X-ray; (b) Preoperative three-dimensional (3D) computed tomography; (c) 3D print model; (d and e) The preoperative osteotomy, reduction, and fixation virtual operation on the model; (f) After successful completion of the operation.
The preoperative surgical planning for the pelvis included the following sequential steps: 3D reconstruction and segmentation of the CT scan data, surgical simulation, template design, sizing and alignment of the implant, and 3D printing of the templates [Figure 3d]. The CT scanning of all sections was performed with 1 mm-thick slices. During the preoperative planning process, a template was used to contour the 3.5 mm-thick reconstruction plate. The screw sizes were determined preoperatively, and the position of the plate and holes was also chosen and marked with indelible ink on the 3D model [Figure 3e and f]. An ilioinguinal approach was used to anteriorly expose the fracture site. The total surgical time required was 4 hours and 10 minutes. Of this time, the instrumentation took only 20 minutes. The blood loss during the procedure was approximately 1000 ml, and the patient was transfused with six units of whole blood.
DISCUSSION
Deformity after pelvic fracture is a common problem, and the correction of such deformities for old pelvic fractures is very difficult because on the one hand the multiple areas around the fracture line of the pelvic ring need to be reopened or osteotomized, but on the other hand, the severe contracture of the soft tissue requires extensive lysis. The many nerves, blood vessels, and other important structures surrounding the pelvic area further increase the difficulty of the operation and treatment risks. Because of the lack of a sufficient number of cases and the difficulty in treating this kind of injury, the surgical outcome is typically not satisfactory. Kanakaris et al. performed a meta-analysis of 25 papers on old pelvic fractures between 1965 and 2008, including a total of 437 cases of pelvic malunion or nonunion cases. The total healing rate was 86.1%, and the pain relief rate was 93%, with a satisfaction rate of 79% and only 50% of the patients returned to their pre-injury activity level. However, there was a high incidence of complications, including nerve injury in 5.3%, deep venous thrombosis in 5%, pulmonary embolism in 1.9%, and deep wound infections in 1.6%.[5] Deformities after pelvic fracture are usually 3D complex, including rotation and shortening deformities in different planes, compounded by the difficult-to-understand 3D anatomy of the pelvis.[3,4,6] Routine imaging examinations, including anteroposterior and inlets/outlets X-ray, CT scanning and 3D reconstruction, give valuable information on pelvic deformities, but may not be able to provide sufficient information for preoperative planning in cases of old pelvic fractures with complicated 3D deformities. Strict preoperative planning is obviously a crucial step for pelvic surgery. Therefore, 3D printing technology has been applied to assist the surgeon and to improve the precision of the operative procedure. We used 3D printing technology to assist in preoperative planning for old pelvic fractures from 2007, and the initial results of this clinical application are reported herein.
3D printing technology provides doctors with more choices. Based on the imaging data, 3D printing technology can provide a true-size model for the doctors to use, making the preoperative planning more direct and accurate. 3D modeling has been used for preoperative planning of complex cranio-maxillofacial surgeries since the 1990s.[7,8] In addition, 3D printing technology has been used for preoperative planning before intracranial aneurysm[9] and living donor liver transplantation.[10] There have also been reports of the use of 3D printing technology for orthopedic surgery. Cimerman and Kristan introduced a surgical planning software for pelvic and acetabular fractures with a mouse-based CAD-style interface.[11] In 20 cases of acetabular fracture, Hurson et al. obtained 3D printed models based on 3D CT data and compared to the traditional imaging examination (anteroposterior, Judet oblique, CT). They found an increased consistency of acetabular fracture classification based on the 3D printing model, indicating that this technology is helpful for doctors to understand the morphological characteristics of complex fractures.[12] Despite the rapid advances in the operative application of 3D printing technology in recent years, surgical simulation and planning based on 3D printed models is rarely used routinely in the clinic. There are many different reasons for the slow adoption of such technologies.[13,14] One important factor may be the reservation of surgeons to explore new technologies because they are devoted to their technical skills and performance. The most difficult step during the production algorithm was the segmentation process, which should be performed by computer engineers and controlled by radiologists.[15,16] Another reason for the slow adoption is the proprietary nature of these technologies can result in a process that is costly, and third party payers are unlikely to reimburse this expense. Therefore, the cost would have to be passed on to the patients, care facilities, or even absorbed by the surgeon, limiting application of this type of technology outside of the research team.[17,18,19]
In 2009, we developed an experimental computer program in collaboration with computer engineers from TINAVI Inc. that enables the performance of a virtual operation on an injured pelvis, and all the steps can be performed by a surgeon. The purpose of the software was to allow the performance of all the steps of the 3D printing procedure on a standard PC computer. This application combined open-source, freeware, and proprietary software with the hardware (the printer used to manufacture the physical model of the pelvis). This method can be used with minimal costs. All the steps can be performed on a standard personal computer by the surgeon who is doing the preoperative planning. This is a novel development because the segmentation can be performed by the surgeon instead of a computer engineer. In that way, all the fracture lines can be studied in 3D during the segmentation process. The procedure is quick and easy. We currently use this program routinely in all pelvic fractures, and in most other difficult articular fractures as well. We also trained three surgeons to use the program independently using a one-day course composed of theoretical and practical exercises.
In the present study, the planned fracture fixation resulted in acceptable hip function according to the Majeed score in all nine cases. A good correlation was found between the preoperative planning and the respective postoperative follow-up CT scans. The approach, osteotomy, and placement of the fixation plate on the pelvic ring showed very good matches between the planning and actual execution. We found no serious postoperative complications, such as deep infections or failure of the osteosynthesis implants. Thus, the physical 3D models produced by 3D printing can be successfully applied preoperatively to determine the amount, position, and extent of the fractures, and to determine the level and direction of the osteotomy site and the osteotomy line. The model was useful to plan the surgical procedure and to determine whether only an anterior or both anterior and posterior surgical entries would be required. Such models can also be successfully applied during the surgical procedure to aid communication between surgical team members by demonstrating the orientation relative to patient anatomy and assisting in bending the reconstruction plates. In other studies, the application of the 3D printed model resulted in a clear reduction in surgery time, surgeon fatigue, and blood loss.[20,21]
The limitations of this study include the small number of patients and the absence of long-term follow-up data. Furthermore, the variability in the injury patterns made it difficult to perform quantitative correlations. Therefore, we were only able to show our initial experiences in the present study, and a larger patient population is needed to further assess this tool for clinical use.
During the preoperative planning process for old pelvic fractures, 3D printing technology is a useful supplement to conventional imaging examination.[2,6,14] 3D models can help the operating doctor to understand complicated deformities of pelvic fractures by osteotomy simulation, operation, and fixation in order to understand the feasibility of the operation scheme, shorten the operation time, improve the final fracture reduction and fixation, and ultimately improve the operation outcome for patients.
ACKNOWLEDGMENTS
We thank Mr. Xin-Hao Wang from Guangruide Technology Co. for assistance with the 3D printing. The data analysis was supported in part by Bin-Bin Wang from the Medical Robotic Engineering Laboratory, TINAVI Medical Technology Co., Ltd.
Footnotes
Edited by: Huan Liu
Source of Support: This study was supported by grants from the National Natural Science Foundation of China (No. F010401) and the Beijing Municipal Committee of Science and Technology (No. Z131110002813121).
Conflict of Interest: None declared.
REFERENCES
- 1.Deng A, Xiong R, He W, Wei D, Zeng C. Postoperative rehabilitation strategy for acetabular fracture: Application of 3D printing technique (in Chinese) J Southern Med Univ. 2014;34:591–3. [PubMed] [Google Scholar]
- 2.Halvorson JJ, Lamothe J, Martin CR, Grose A, Asprinio DE, Wellman D, et al. Combined acetabulum and pelvic ring injuries. J Am Acad Orthop Surg. 2014;22:304–14. doi: 10.5435/JAAOS-22-05-304. [DOI] [PubMed] [Google Scholar]
- 3.Holubar SD, Hassinger JP, Dozois EJ, Camp JC, Farley DR, Fidler JL, et al. Virtual pelvic anatomy and surgery simulator: An innovative tool for teaching pelvic surgical anatomy. Stud Health Technol Inform. 2009;142:122–4. [PubMed] [Google Scholar]
- 4.Shen F, Chen B, Guo Q, Qi Y, Shen Y. Augmented reality patient-specific reconstruction plate design for pelvic and acetabular fracture surgery. Int J Comput Assist Radiol Surg. 2013;8:169–79. doi: 10.1007/s11548-012-0775-5. [DOI] [PubMed] [Google Scholar]
- 5.Kanakaris NK, Angoules AG, Nikolaou VS, Kontakis G, Giannoudis PV. Treatment and outcomes of pelvic malunions and nonunions: A systematic review. Clin Orthop Relat Res. 2009;467:2112–24. doi: 10.1007/s11999-009-0712-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weaver MJ, Brubacher JW, Vrahas MS. Application of epoxy resin to a solid-foam pelvic model: Creating a dry-erase pelvis. Am J Orthop (Belle Mead NJ) 2014;43:521–3. [PubMed] [Google Scholar]
- 7.Poukens J, Haex J, Riediger D. The use of rapid prototyping in the preoperative planning of distraction osteogenesis of the cranio-maxillofacial skeleton. Comput Aided Surg. 2003;8:146–54. doi: 10.3109/10929080309146049. [DOI] [PubMed] [Google Scholar]
- 8.Wilde F, Cornelius CP, Schramm A. Computer-assisted mandibular reconstruction using a patient-specific reconstruction plate fabricated with computer-aided design and manufacturing techniques. Craniomaxillofac Trauma Reconstr. 2014;7:158–66. doi: 10.1055/s-0034-1371356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Erbano BO, Opolski AC, Olandoski M, Foggiatto JA, Kubrusly LF, Dietz UA, et al. Rapid prototyping of three-dimensional biomodels as an adjuvant in the surgical planning for intracranial aneurysms. Acta Cir Bras. 2013;28:756–61. doi: 10.1590/s0102-86502013001100002. [DOI] [PubMed] [Google Scholar]
- 10.Zein NN, Hanouneh IA, Bishop PD, Samaan M, Eghtesad B, Quintini C, et al. Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transpl. 2013;19:1304–10. doi: 10.1002/lt.23729. [DOI] [PubMed] [Google Scholar]
- 11.Cimerman M, Kristan A. Preoperative planning in pelvic and acetabular surgery: The value of advanced computerised planning modules. Injury. 2007;38:442–9. doi: 10.1016/j.injury.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 12.Hurson C, Tansey A, O’Donnchadha B, Nicholson P, Rice J, McElwain J. Rapid prototyping in the assessment, classification and preoperative planning of acetabular fractures. Injury. 2007;38:1158–62. doi: 10.1016/j.injury.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 13.Won SH, Lee YK, Ha YC, Suh YS, Koo KH. Improving pre-operative planning for complex total hip replacement with a Rapid Prototype model enabling surgical simulation. Bone Joint J. 2013;95-B:1458–63. doi: 10.1302/0301-620X.95B11.31878. [DOI] [PubMed] [Google Scholar]
- 14.Zhang YZ, Lu S, Chen B, Zhao JM, Liu R, Pei GX. Application of computer-aided design osteotomy template for treatment of cubitus varus deformity in teenagers: A pilot study. J Shoulder Elbow Surg. 2011;20:51–6. doi: 10.1016/j.jse.2010.08.029. [DOI] [PubMed] [Google Scholar]
- 15.Sicurezza E, Palazzo G, Leonardi R. Three-dimensional computerized tomographic orbital volume and aperture width evaluation: A study in patients treated with rapid maxillary expansion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:503–7. doi: 10.1016/j.tripleo.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 16.Citak M, Gardner MJ, Kendoff D, Tarte S, Krettek C, Nolte LP, et al. Virtual 3D planning of acetabular fracture reduction. J Orthop Res. 2008;26:547–52. doi: 10.1002/jor.20517. [DOI] [PubMed] [Google Scholar]
- 17.Modabber A, Ayoub N, Möhlhenrich SC, Goloborodko E, Sönmez TT, Ghassemi M, et al. The accuracy of computer-assisted primary mandibular reconstruction with vascularized bone flaps: Iliac crest bone flap versus osteomyocutaneous fibula flap. Med Devices (Auckl) 2014;7:211–7. doi: 10.2147/MDER.S62698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mazzoni S, Marchetti C, Sgarzani R, Cipriani R, Scotti R, Ciocca L. Prosthetically guided maxillofacial surgery: Evaluation of the accuracy of a surgical guide and custom-made bone plate in oncology patients after mandibular reconstruction. Plast Reconstr Surg. 2013;131:1376–85. doi: 10.1097/PRS.0b013e31828bd6b0. [DOI] [PubMed] [Google Scholar]
- 19.Ciocca L, Mazzoni S, Fantini M, Persiani F, Baldissara P, Marchetti C, et al. A CAD/CAM-prototyped anatomical condylar prosthesis connected to a custom-made bone plate to support a fibula free flap. Med Biol Eng Comput. 2012;50:743–9. doi: 10.1007/s11517-012-0898-4. [DOI] [PubMed] [Google Scholar]
- 20.Starosolski ZA, Kan JH, Rosenfeld SD, Krishnamurthy R, Annapragada A. Application of 3-D printing (rapid prototyping) for creating physical models of pediatric orthopedic disorders. Pediatr Radiol. 2014;44:216–21. doi: 10.1007/s00247-013-2788-9. [DOI] [PubMed] [Google Scholar]
- 21.Tam MD. Building virtual models by postprocessing radiology images: A guide for anatomy faculty. Anat Sci Educ. 2010;3:261–6. doi: 10.1002/ase.175. [DOI] [PubMed] [Google Scholar]


