ABSTRACT
Reassortment between H5 or H9 subtype avian and mammalian influenza A viruses (IAV) can generate a novel virus that causes disease and transmits between mammals. Such information is currently not available for H7 subtype viruses. We evaluated the ability of a low-pathogenicity North American avian H7N3 virus (A/shorebird/Delaware/22/2006) to reassort with mammalian or avian viruses using a plasmid-based competition assay. In addition to genome segments derived from an avian H7N9 virus, the H7N3 virus reassorted efficiently with the PB2, NA, and M segments from the 2009 pandemic H1N1 (PH1N1) virus. In vitro and in vivo evaluation of the H7N3:PH1N1 (7 + 1) reassortant viruses revealed that the PB2, NA, or M segments from PH1N1 largely do not attenuate the H7N3 virus, whereas the PB1, PA, NP, or NS genome segments from PH1N1 do. Additionally, we assessed the functionality of the H7N3:PH1N1 7 + 1 reassortant viruses by measuring the inflammatory response in vivo. We found that infection with wild-type H7N3 resulted in increased inflammatory cytokine production relative to that seen with the PH1N1 strain and that the increase was further exacerbated by substitution of PH1N1 PB2 but not NA or M. Finally, we assessed if any adaptations occurred in the individually substituted segments after in vivo inoculation and found no mutations, suggesting that PH1N1 PB2, NA, and M are genetically stable in the background of this H7N3 virus. Taking the data together, we demonstrate that a North American avian H7N3 IAV is genetically and functionally compatible with multiple gene segments from the 2009 pandemic influenza virus strain without prior adaptation.
IMPORTANCE The 2009 pandemic H1N1 virus continues to circulate and reassort with other influenza viruses, creating novel viruses with increased replication and transmission potential in humans. Previous studies have found that this virus can also reassort with H5N1 and H9N2 avian influenza viruses. We now show that several genome segments of the 2009 H1N1 virus are also highly compatible with a low-pathogenicity avian H7N3 virus and that these reassortant viruses are stable and not attenuated in an animal model. These results highlight the potential for reassortment of H1N1 viruses with avian influenza virus and emphasize the need for continued surveillance of influenza viruses in areas of cocirculation between avian, human, and swine viruses.
INTRODUCTION
Reassortment of influenza A viruses (IAVs) produces diversity and antigenic novelty within circulating strains, sometimes leading to the emergence of pandemic viruses that cause widespread disease in humans. Avian IAV subtypes, including H5, H7, and H9, have caused sporadic but sometimes fatal disease in humans (1, 2). Zoonosis of these viruses or derivative lineages formed via reassortment with strains capable of human-to-human transmission may lead to the emergence of novel viruses with pandemic potential (3). Indeed, multiple bird-origin viruses, most notably H5N1 and H9N2 strains, were able to cause disease in mammals and had limited but enhanced transmission potential following experimental reassortment with the 2009 pandemic H1N1 (PH1N1) virus (2, 4). Genetically diverse IAVs may therefore gain the ability to induce disease and transmit between mammals if an appropriate genetic constellation is assembled through reassortment.
H7 subtype viruses intermittently infect and cause disease in humans following contact with infected birds (1, 5). Outbreaks of H7 viruses in humans have occurred in geographically distinct areas, including The Netherlands (2003), Canada (2004), Mexico (2012), and China (2013) (6). Sporadic infections such as these, which sometimes result in severe disease, suggest that introduction of a H7 subtype virus capable of sustained transmission between humans has the potential to initiate a significant outbreak. Recently, a reassortant, low-pathogenicity H7N9 virus emerged in China with a case-fatality rate of approximately 25%, making this the most severe and sustained incursion of H7 subtype viruses into the human population (7). Although person-to-person transmission has not been consistently demonstrated, the virus is capable of limited transmission in guinea pig and ferret models without prior adaptation, suggesting the potential acquisition of transmission-related adaptations through mutation or reassortment (7–10). The sustained and ongoing geographic cocirculation of H7-bearing viruses with the PH1N1 strain poses a risk for reassortment that may create H7-bearing viruses containing one or more PH1N1-origin gene segments (11).
Reassortment of IAV genes, including those endemic in animal reservoirs, has given rise to pandemic IAVs, most recently, PH1N1 in 2009 (12). In each case, antigenic shift of external proteins occurred as well as transfer of gene segments encoding internal and nonstructural proteins. PH1N1 resulted from three independent reassortment events involving genes from swine, human, and avian viruses. This triple-reassortant swine-origin IAV, first identified in Mexico, consists of PB2, PB1, PA, hemagglutinin (HA), NP, and NS derived from a North American swine virus isolate and the NA and M segments from an Eurasian lineage swine influenza virus (12). Further reassortment events between PH1N1 and swine IAV have resulted in the creation of variant H1N1v, H2N1v, and H3N2v viruses capable of causing disease in humans. All variant viruses contain segment 7 (M) of PH1N1, which has been shown to confer aerosol transmissibility to previously nontransmissible viruses (13, 14). The widespread distribution of PH1N1 coupled with its high rate of reassortment with environmental viruses suggests the potential for the emergence of novel PH1N1 segment-containing IAV genome constellations with increased virulence or transmissibility in humans.
North American H7N3 IAVs cocirculate with PH1N1; however, the ability of these avian viruses to reassort with PH1N1, modify virologic traits, and induce disease in mammals is not known. This study was initially designed to identify the genome segments derived from diverse bird- and human-origin IAV that were most compatible with an avian-origin LPAI (low-pathogenicity avian influenza) H7N3 virus. We devised a competitive reverse genetics strategy to examine selection of a single genome segment when multiple versions of that segment are present in a cell, mimicking cellular coinfection. We found that PH1N1 PB2, NA, and M genome segments are capable of outcompeting the parental H7N3 strain and additional heterologous segments of diverse origins in competitive reverse genetic experiments. As a result of the competitive reverse genetic studies, we generated and characterized the parental H7N3 and PH1N1 viruses and seven H7N3:PH1N1 (7 + 1) reassortant viruses. Characterization of single-segment reassortants demonstrated that multiple genome segments from PH1N1 either enhanced (PB2) or maintained (NA or M) H7N3 replication and virulence in a mouse model of infection. Finally, adaptation of substituted PH1N1 segments was not required for function within the H7N3 backbone, suggesting that these newly formed genomic constellations are genetically and functionally stable.
MATERIALS AND METHODS
Biosafety and ethical considerations.
All experiments were carried out under conditions of enhanced biosafety level 2 (BSL2) containment and approved by the Washington University in Saint Louis Institutional Biosafety Committee. The H7N3 virus A/shorebird/Delaware/22/2006 used in this study is neuraminidase inhibitor sensitive, as are all the reassortant H7N3 viruses that were generated and used in this study. Additionally, the parental H7N3 virus has a genetic signature indicative of an α-2,3-sialic acid (avian receptor) binding preference and does not bear a multibasic cleavage site; therefore, we reasonably anticipated that these experiments, in which this H7 HA was maintained, would not result in increased host range or transmission to a new (mammalian) host. Finally, the NA gene of A/Memphis/03/2008 (H1N1) was excluded from this study due to a H274Y mutation that confers resistance to neuraminidase inhibitors (15).
Viruses.
The following viruses were used in this study: A/shorebird/Delaware/22/2006 (H7N3), A/California/04/2009 (PH1N1), A/mallard/Alberta/177/2004 (H7N9), A/Memphis/03/2008 (SH1N1), and A/Puerto Rico/08/1934 (PR8H1N1). For SH1N1, H7N3, and H7N9, cDNA for all gene segments was cloned into the bidirectional pHW2000 plasmid and used to generate influenza viruses as previously described (16). Richard Webby at St. Jude Children's Research Hospital kindly provided the reverse genetic plasmids for PH1N1 and PR8H1N1. Plasmid-derived A/shorebird/Delaware/22/2006 (H7N3) and A/California/04/2009 (PH1N1) viruses and all of the H7N3:PH1N1 7 + 1 single-reassortant viruses were generated using the 293T-Madin-Darby canine kidney cell (MDCK) coculture system, and supernatant was injected into 10-day-old embryonated chicken eggs for 48 h at 35°C (Cackle Hatcheries, IA, USA). Allantoic fluid containing the infectious virus was harvested and stored at −80°C. The viral titer (50% tissue culture infectious dose [TCID50]) was determined using MDCK cells, and viral stock used in this study was titrated at least twice independently. Single-reassortant viruses on the background of H7N3 possessing a single genome segment from PH1N1 used in this study have been named with the following convention—seven segments from the H7N3 virus plus the substituted PH1N1 segment in subscript (for example, H7N3NA).
Cells.
MDCK cells were maintained in minimal essential medium (MEM) with 5% fetal bovine serum (FBS), vitamins, l-glutamine (Invitrogen), penicillin, and streptomycin. 293T cells were maintained in Opti-MEM with 10% FBS, l-glutamine, penicillin, and streptomycin. A549 cells were maintained in Dulbecco's minimal essential medium (DMEM) with 10% FBS, vitamins, l-glutamine, penicillin, streptomycin, 25 mM HEPES, and nonessential amino acids (NEAA).
Competitive reverse genetic assay.
A competitive reverse genetic assay was developed to evaluate the ability of avian and human IAV genome segments to reassort in the context of an avian H7N3 viral background (Fig. 1A). 293T-MDCK cocultures were transfected with pHW2000 plasmids (1 μg per segment) containing seven genome segments of H7N3 virus plus four (for NA segment due to exclusion of NA from SH1N1) or five (e.g., PB2) plasmids carrying a single genome segment from different avian and human influenza viruses. All transfections included the wild-type H7N3 (H7N3WT) segment in addition to those from divergent strains. Because of biosafety considerations, we did not evaluate the HA genome segment. The total amount of cotransfected plasmid DNA for the 8th segment (1 μg) was divided equally among the four or five studied viruses, including the parental strain. The DNA was mixed at a 1:2 ratio with Trans-IT LT1 (Mirus) in Opti-MEM for 20 min at room temperature and added to the culture medium. Following an overnight incubation, the cell culture medium was removed and 1 ml of fresh Opti-MEM supplemented with penicillin, streptomycin, and l-glutamine was added. Twenty-four hours later, an additional 1 ml of Opti-MEM with 1 μg/ml tosylsulfonyl phenylalanyl chloromethyl ketone (TPCK)-trypsin (Worthington) was added. Forty-eight hours later, supernatants were collected, and cell debris was removed by centrifugation at 1,200 × g and frozen at −80°C until further analysis. Clonal viral populations were isolated by limiting dilution assay using MDCK cells, and then viral RNA (vRNA) was extracted, reverse transcribed using a vRNA-specific primer, and amplified with segment-specific PCR primers. Genome segment amplicons were genotyped by either restriction fragment length polymorphism (RFLP) analysis or Sanger sequencing. RFLP analysis was performed with one to four different restriction enzymes, yielding a unique fragment length pattern for each segment and strain, as follows: PB2 (EcoRI, HindIII, and BamHI); PB1 (HindIII); PA (BamHI, HindIII, and XbaI); NP (BamHI and BglII); NA (BamHI, BglII, EcoRI, and BsmBI); and M (BamHI, HindIII, XcmI, and PvuII). All restriction enzymes were obtained from New England BioLabs and used according to their instructions. The NS gene segment was genotyped by Sanger sequencing. Competitive reverse genetic assays were completed at least twice independently for each genome segment. On average, we tested 48 clonal viruses per genome segment with a minimum of 24 (M segment) and a maximum of 71 (PA segment) viruses.
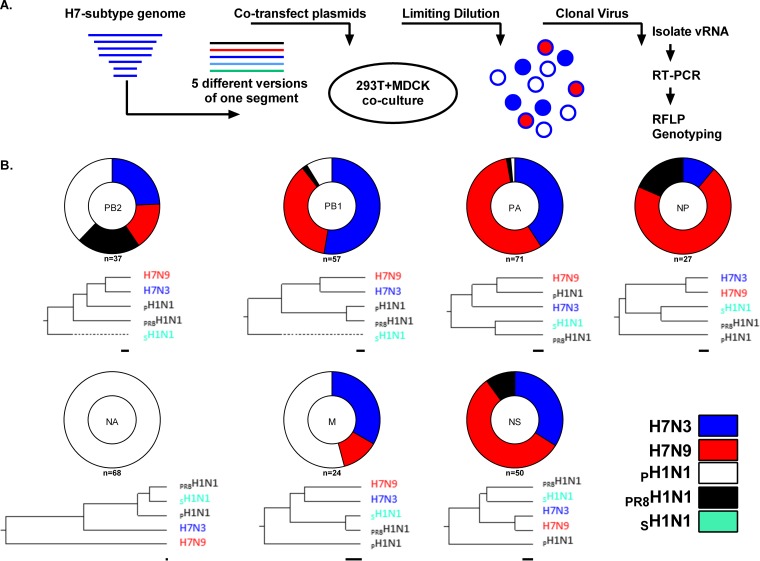
FIG 1.
A North American H7N3 virus preferentially selects avian and 2009 pandemic H1N1 genome segments following competitive transfection. (A) Seven genome segments derived from strain A/shorebird/Delaware/22/2006 (H7N3) were cotransfected with four (NA only) or five variants of the eighth genome segment. These variants included the homologous gene segment from A/shorebird/Delaware/22/2006 (H7N3) as well as those of A/mallard/Alberta/177/2004 (H7N9), A/Memphis/03/2008 (SH1N1), A/California/04/2009 (PH1N1), and A/Puerto Rico/08/1934 (PR8H1N1) virus. Following transfection, individual virus particles were cultured in MDCK cells using a limiting dilution assay. Virus-positive wells were identified by HA assay, and the remaining supernatant was used to purify viral RNA. cDNA was generated using a universal influenza primer, and the segment of interest was amplified using segment-specific PCR primers and analyzed by restriction length fragment polymorphism (RFLP). RT-PCR, reverse transcription-PCR. (B) Pie charts depicting the relative distribution of four or five gene segments that were identified among the competitive reverse genetics-derived H7 viruses. The results represent the cumulative distribution of results from two or more independently repeated experiments; 334 viruses in total were sampled. The NA gene of A/Memphis/03/2008 (NA-inhibitor insensitive) was excluded from these analyses. Phylogenetic trees for each corresponding segment illustrate the genetic relationships between the assayed segments (bootstrapped 1,000×). The line beneath each phylogenetic tree represents 1 nucleotide substitution per 100 nucleotides.
Virus genome sequence analysis.
After expansion of virus in eggs, the nucleotide identity of the singly substituted genome segment in each H7N3:PH1N1 7 + 1 single-reassortant virus was verified by Sanger sequencing. Viral genomic RNA was extracted and reverse transcribed as described above. Segment-specific PCR was conducted, and the resulting amplicon was purified by agarose gel electrophoresis and then submitted for sequencing with an overlapping panel of sequencing primers derived from the parental PH1N1 virus consensus sequence. We then assembled contiguous sequences for each segment and aligned them to the parental segment for analysis. The same sample preparation and analysis methods were used for materials derived from homogenate.
Multistep growth curves of influenza A virus.
MDCK or A549 cells (2 × 105) were seeded in 24-well plates and inoculated the next day with 50 TCID50 (MDCK) or 105 TCID50 (A549) of IAV. MDCK cells were washed once with phosphate-buffered saline (PBS) before the inoculum was added into MEM containing penicillin, streptomycin, l-glutamine, and vitamins plus 0.1% bovine serum albumin (M0.1B) for 1 h at 37°C. After 1 h, the cells were washed once with PBS and 1.0 ml of M0.1B with 1 μg/ml TPCK-trypsin was added to each well. A549 cells were washed once in DMEM containing penicillin, streptomycin, l-glutamine, and vitamins plus 0.1% bovine serum albumin and NEAA (D0.1B) prior to inoculation with virus diluted in D0.1B. After 1 h at 37°C, the A549 cells were washed once with D0.1B and 1.0 ml of D0.1B with 0.5 μg/ml TPCK-trypsin was added to each well. Culture supernatants from either cell type were collected at 24 and 48 h postinfection (hpi), and the amount of infectious virus was quantified by titration on MDCK cells. The results are the averages of two to three experiments, each performed in duplicate.
Phylogenetic analysis of IAV segments.
Nucleotide alignments were generated for complete genome segments using the ClustalW algorithm in Lasergene MegAlign (version 11.1.0; DNASTAR, Inc.), bootstrapped 1,000×, and used to construct neighbor-joining phylogenetic trees.
TCID50 assay.
Confluent monolayers of MDCK cells were grown overnight in 96-well plates. The next day, the cells were washed with PBS and inoculated with 10-fold serial dilutions (10−1 to 10−8) of culture supernatant, allantoic fluid, or lung homogenate for 1 h in M0.1B at 37°C and 5% CO2. After 1 h, the inoculum was removed and replaced with M0.1B supplemented with 1 μg/ml TPCK-trypsin and incubated for 72 h. The presence of virus was determined by hemagglutination assay using 0.5% turkey red blood cells. The TCID50 was determined by the Reed-Muench method (17).
Intranasal inoculation of mice with influenza viruses.
Male C57BL/6J mice (6 to 8 weeks of age) were bred in-house in a barrier facility at Washington University School of Medicine, St. Louis, MO, USA. The mice received food and water ad libitum, and all experiments were conducted in accordance with rules of the Institutional Animal Care and Use Committee. Mice were inoculated intranasally with 103 or 104 TCID50 units of IAV–30 μl of sterile PBS after sedation with 2,2,2-tribromoethanol (Avertin; Sigma-Aldrich, MO, USA). Morbidity and mortality following intranasal inoculation were monitored for 7 days (104 TCID50) or 14 days (103 TCID50). To assess lung viral titers, mice inoculated with 104 TCID50 were sacrificed on days 3 or 7 postinoculation and the entire lung was collected, homogenized in 1.0 ml of infection media, cleared by centrifugation at 1,000 × g for 5 min, and stored in aliquots at −80°C. Experiments in which an inoculum of 104 TCID50 was used were terminated at 7 days postinoculation. All mice survived to this point, at which time total lung tissue was harvested. Experiments in which an inoculum of 103 TCID50 was used were terminated at 14 days postinoculation. Viral titers from lung homogenates were determined by TCID50 assay. The results from the lung titrations are averages of at least two independent experiments.
Cytokine array.
Cytokine and chemokine production in lung homogenates was measured using a 23-plex cytokine array (Bio-Plex Pro Mouse Cytokine 23-plex assay; Bio-Rad) according to the manufacturer's protocol. The cytokine screen included inteleukin-1α (IL-1α), IL-1β, IL-2, IL-3, IL-4, IL-5, IL-6, IL-9, IL-10, IL-12p40, IL-12p70, IL-13, IL-17, eotaxin, granulocyte colony-stimulating factor(G-CSF), granulocyte-macrophage colony-stimulating factor (GM-CSF), gamma interferon (IFN-γ), KC, monocyte chemoattractant protein 1 (MCP-1), MIP-1α, MIP-1β, RANTES, and tumor necrosis factor alpha (TNF-α). As many samples fell below the limit of detection, we excluded a number of the cytokines (IL-2, IL-3, IL-4, IL-9, and IL-17) from our analysis. Results from the cytokine array are the averages of at least two independent experiments (for day 3, for wild-type H7N3 [H7N3WT], n = 6, for H7N3PB2, n = 5, for H7N3NA, n = 6, for H7N3M, n = 5, and for PH1N1WT, n = 7; for day 7, for H7N3WT, n = 5, for H7N3PB2, n = 7, for H7N3NA, n = 7, for H7N3M, n = 4, and for PH1N1WT, n = 10).
Influenza A virus minigenome reporter assay.
The PB2, PB1, PA, and NP genes from H7N3 and PH1N1 were cloned into the pcDNA3.1+ (Invitrogen) mammalian expression vector from the corresponding pHW2000 plasmid. The PA of pH1N1 containing the P295L mutation was cloned from the reassortant H7N3PA virus generated in this study. The pLuci plasmid was kindly provided by H.-L. Yen (Hong Kong University, Hong Kong, China) and contains the firefly luciferase gene flanked by the noncoding regions of the NP gene segment in the negative orientation under the control of a human RNA polymerase I promoter. Cells were maintained at 37°C for the duration of the experiment. A Renilla luciferase expression plasmid was included for normalization. 293T cells were seeded into 24-well plates and transfected with PB2, PB1, PA, and NP expression plasmids (83 ng/plasmid) along with the two luciferase-containing plasmids (total of 500 ng DNA) using TransIT-LT1 in each well. The following day, the medium was changed and cells were incubated for 48 h, harvested, and lysed for analysis of luciferase activities (Promega). Each combination of polymerase proteins (set of plasmids) was examined in duplicate, and each procedure was repeated independently in three or more separate experiments. The relative light units (RLU) for firefly luciferase activity were normalized to the RLU for Renilla luciferase activity within the same sample to account differences in transfection efficiency between wells and experiments. Polymerase activity was normalized to that of the parental H7N3 polymerase proteins.
Statistical analysis.
All statistical analyses were performed using GraphPad Prism 6.0 software. The Mann-Whitney U test was used to determine the statistical significance of the results of comparisons of lung virus titers. One-way analysis of variance (ANOVA) was used with Dunnett's multiple-comparison test to determine the statistical significance of the results of comparisons of cytokine and chemokine production levels in lung homogenates, with all comparisons made to H7N3WT for the indicated day. Two-way ANOVA was used in the analysis of weight loss differences following influenza A virus infections in mice. Student's t test was used to assess statistical differences between conditions in the minigenome reporter assay, with all comparisons made to the wild-type combination of H7N3 proteins.
RESULTS
A North American H7 virus preferentially selects avian and 2009 pandemic H1N1 genome segments under competitive conditions.
Previous studies examining the reassortment potential of H5 and H9 subtype avian IAV and human-derived IAV reported high compatibility between diverse bird- and human-origin genome segments (2, 4, 15, 16). However, it remains unclear if H7 subtype viruses can undergo similar reassortment events with other avian and human IAV. The recent emergence of H7N9 in China demonstrates that H7 subtype viruses can infect humans and, if they acquire the ability to transmit between humans through reassortment, may pose a significant public health threat. Therefore, we sought to determine if North American H7 subtype viruses are capable of extensive reassortment with human or mammalian viruses.
We developed a competitive reverse genetics assay to evaluate the ability of heterologous genome segments from human and avian viruses to reassort efficiently with a North American low-pathogenicity H7N3 virus (Fig. 1A). Seven genome segments of A/shorebird/Delaware/22/2006 (H7N3) were maintained as a constant background, while multiple versions of the 8th segment from H7N3, A/California/04/2009 (PH1N1), A/Puerto Rico/08/1934 (PR8H1N1), A/mallard/Alberta/144/2007 (H7N9), or A/Memphis/3/2008 (SH1N1) were included in equimolar ratios. Phylogenetic trees were constructed for each genome segment to illustrate the genetic relationship to the H7N3 segment (Fig. 1B). Pools of infectious viruses were rescued and subjected to limiting dilution assays to culture clonal viral populations and to identify the segment of interest by via RFLP analysis or Sanger sequencing.
A total of 334 viruses were analyzed for 7 genome segments in the context of H7N3 virus (HA was excluded). We observed a high frequency of isolated viruses containing reassorted genome segments from avian H7N3-derived (29%) or H7N9-derived (34%) sources (Fig. 1B). In particular, the PB1, PA, NP, and NS reassorted genome segments were predominantly (81%) of avian virus origin. In contrast, as shown by examination of the identity of competitively selected segments, the PB2, NA, and M genome segments were derived mostly from mammalian IAV, with a clear bias toward the PH1N1 virus. The NA gene of PH1N1 was identified in 100% (68/68) of the NA gene-reassorted H7 viruses, while the M and PB2 gene segments constituted 55% (13/24) and 35% (14/37) of the examined H7 viruses, respectively. Combined, 32% of all isolated H7 viruses contained genome segments derived from PH1N1, suggesting a high degree of compatibility between H7N3 and PH1N1 virus. Genome segments from PR8H1N1 were identified sporadically, at a rate of 5% (15/334), among the H7N3 viruses. Of these, 8 contained the PB2 gene of PR8H1N1. Finally, 0% (0/266) of the genome segments from SH1N1 were identified among the H7 viruses, suggesting a low level of genetic compatibility between human H1N1 viruses circulating prior to 2009 and avian H7N3 virus.
Most H7N3:PH1N1 7 + 1 viruses replicate efficiently in MDCK cells.
We observed a high degree of genetic compatibility between genome segments of PH1N1 and H7N3 viruses in our competitive reverse genetics assay and sought to determine the replicative ability of each single-reassortant virus bearing individual PH1N1 segments in the background of H7N3. All 7 + 1 reassortant viruses were generated independently by reverse genetics and amplified in chicken eggs. We inoculated MDCK cells with 50 TCID50 and collected supernatant at 24 and 48 hpi (Fig. 2A and B, respectively). H7N3 virus replicated to high titers at 24 hpi (107.8/ml) and 48 hpi (107.9/ml). In contrast, PH1N1 virus replicated to significantly lower titers at 24 (105.8/ml) and 48 hpi (106.4/ml) (P < 0.01 for both time points). H7 viruses containing the NA (H7N3NA) or M (H7N3M) gene segment of PH1N1 virus grew to similar titers (P > 0.2) at 24 hpi (107.6/ml for H7N3NA and 107.3/ml for H7N3M) and 48 hpi (108.2/ml for H7N3NA and 108.1/ml for H7N3M). The titers of H7N3 reassortant viruses containing the PB2 (H7N3PB2; 106.8/ml), PA (H7N3PA, 105.9/ml), NP (H7N3NP,105.7/ml), or NS (H7N3NS,106.3/ml) gene segment of PH1N1 were significantly lower than those seen with the H7N3 parental virus at 24 hpi (P < 0.001) but not at 48 hpi (P > 0.15). Finally, the virus titer of H7N3PB1 was significantly (P < 0.001) lower than that seen with parental H7N3 at 24 and 48 hpi (104.4/ml and 104.6/ml, respectively). Overall, our results indicate that most H7N3 viruses possessing a single genome segment of PH1N1 are able to replicate efficiently in a MDCK cell culture system and that the NA gene and M gene of PH1N1 did not attenuate H7N3 virus in vitro.
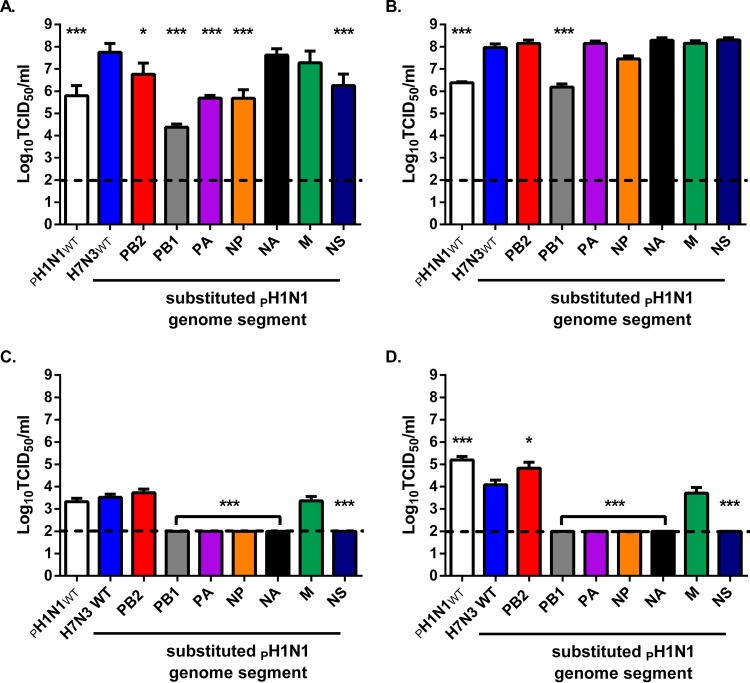
FIG 2.
Several H7 single-gene reassortant viruses possessing a PH1N1 segment replicate efficiently in mammalian tissue culture. (A and B) MDCK cells were inoculated with 50 TCID50 of the indicated virus, and the virus titer (TCID50 per milliliter) in the supernatant was determined at 24 h (A) or 48 h (B) postinoculation by virus titration assay performed on MDCK cells. (C and D) A549 cells were inoculated with 105 TCID50 of the indicated virus, and the virus titer (TCID50 per milliliter) in the supernatant was determined at 24 h (C) or 48 h (D) postinoculation by virus titration assay on MDCK cells. The limit of detection was 100 TCID50 (dotted line). The data represent geometric means + standard errors of the means of results determined with four samples derived from two or three independent experiments performed in duplicate (*, P < 0.05; ***, P < 0.005 [compared to H7N3 values]).
The majority of H7N3:PH1N1 7 + 1 viruses are attenuated in A549 cells.
Next, we measured replication of the 7 + 1 reassortant viruses in a human lung epithelial cell line (A549). H7N3 virus replicated to 103.5 TCID50/ml at 24 hpi and 104.0 TCID50/ml at 48 hpi. PH1N1 virus replicated to titers that were equivalent to those seen with H7N3 virus at 24 hpi (103.7 TCID50/ml) and that were significantly higher at 48 hpi (105.2 TCID50/ml; P < 0.05). H7N3 virus containing the M segment of pH1N1 (H7N3M) was able to grow in A549 cells, although the growth was less efficient that of the wild-type H7N3 virus at 48 hpi (103.5 TCID50/ml; P < 0.05). The 7 + 1 reassortant virus containing the PB2 genome segment of PH1N1 replicated to titers that were equivalent to those seen with the H7N3 virus at 24 hpi (103.7/ml) and higher at 48 hpi (104.7/ml; P < 0.05). Finally, we did not detect replicating virus from the H7N3PB1, H7N3PA, H7N3NP, H7N3NA, or H7N3NS reassortant viruses in culture supernatant at either time point postinoculation. These data suggest that the majority of the gene segments of PH1N1 attenuate H7N3 virus growth in human cells.
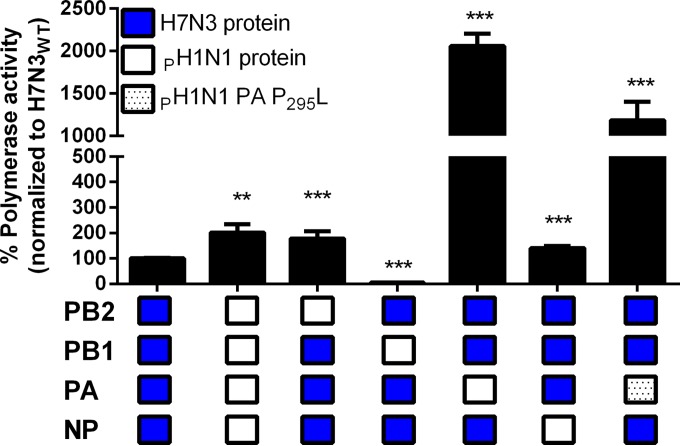
PB2, PA, and NP segments of PH1N1 increase H7N3 polymerase activity in human cells.
We employed a minigenome reporter assay to assess the polymerase activity of different viral polymerase complexes in human 293T cells. We found that the full complement of PH1N1 proteins generated greater reporter activity than did the H7N3 polymerase proteins (1.8-fold increase, P < 0.01; Fig. 3). Substitution of the PB2 or NP protein with those from PH1N1 increased polymerase activity by 1.8-fold (P < 0.01) or 1.4-fold (P < 0.001), respectively. The PA of PH1N1 increased the polymerase activity more than 20-fold (P < 0.001). We also evaluated a PA protein of PH1N1 containing a proline-to-leucine substitution at position 295 (P295L). This mutation was selected for H7N3PA virus cultured in 10-day-old embryonated chicken eggs. The polymerase activity of the mutant PA remained more than 10-fold (P < 0.001; Fig. 3) greater than that of the H7N3 protein complex. Interestingly, substitution of PH1N1 PB1 into a majority H7N3 polymerase complex resulted in a 25-fold reduction in polymerase activity (P < 0.001). To examine if this was due to strain-dependent differences in PB1 protein expression, we analyzed protein expression by flow cytometry (mean fluorescence intensity [MFI]) using His-tagged versions of the PB1 of H7N3 and PH1N1 virus. We did not observe a difference in MFI between these two proteins (data not shown), suggesting that the 25-fold difference in reporter activity is due to inherent differences in compatibility between the polymerase proteins. Overall, the H7N3 virus appears well adapted to mammalian cells and the introduction of the PB1 of PH1N1 severely attenuates the H7N3 virus.
FIG 3.
PA protein from pandemic H1N1 virus increases the polymerase activity of H7N3 in human 293T cells. (A) A reporter assay was used to measure the relative levels of polymerase activity of different polymerase protein complex combinations between H7N3 and PH1N1 viruses, including PH1N1 PA P295L, as described in Materials and Methods. The relative polymerase activity data were first normalized to the Renilla activity and compared to that of a full set of H7N3 polymerase proteins. Blue boxes represent H7N3 proteins, white boxes represent pH1N1 proteins, and spotted white boxes represent pH1N1 PA-P295L. Data represent the average normalized values from three or five experiments performed in duplicate (**, P < 0.01; ***, P < 0.005 [compared to H7N3 values]).
H7N3:PH1N1 7 + 1 reassortant viruses induce distinct morbidities in vivo.
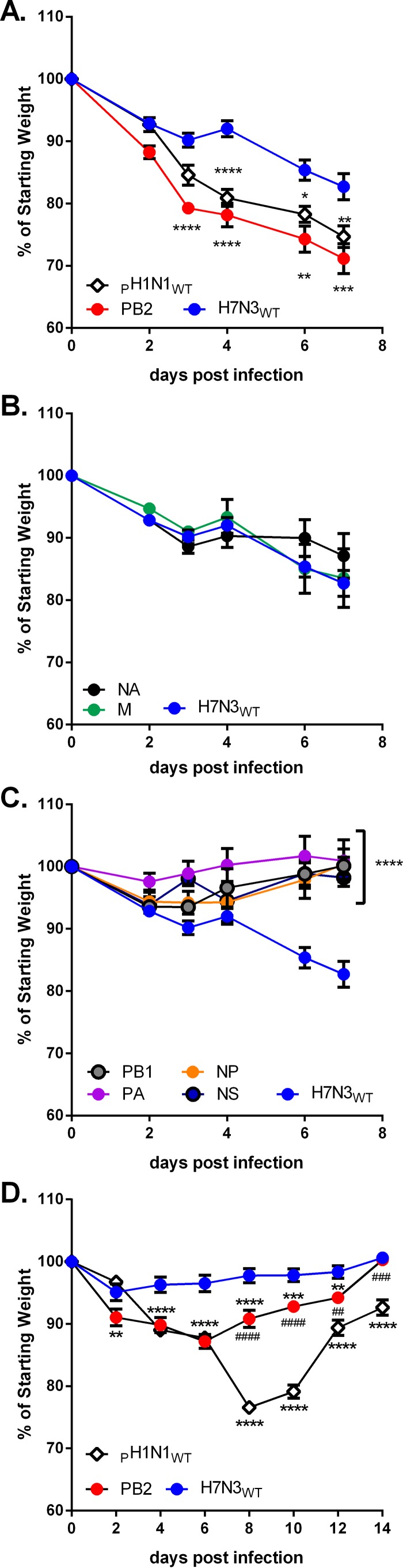
Given the high degree of functional compatibility between PH1N1 and H7N3 virus in vitro, we next determined the relative levels of fitness of these H7N3 viruses containing individual gene segments of PH1N1 in vivo. C57BL/6J mice were inoculated intranasally with either parental (H7N3 or PH1N1) or single-segment-reassortant viruses, and the mice were weighed at regular intervals for 1 week (104 dose) or 2 weeks (103 dose) depending on the inoculum size. Mice inoculated with 104 TCID50 of H7N3 demonstrated substantial weight loss beginning at 3 days postinfection (dpi) (10%) that continued until the experiment was ended at 7 dpi (21%). Inoculation with 104 TCID50 of PH1N1 induced up to 30% weight loss relative to the starting weight within 7 days (Fig. 4A), demonstrating that the PH1N1 virus is more pathogenic in mice than the avian H7N3 virus. H7N3 viruses containing single gene segments for PH1N1 differed in their ability to cause weight loss. Inoculation with 103 or 104 TCID50 of H7N3 virus containing the PB2 segment of PH1N1 induced significantly (P < 0.05) more weight loss than inoculation with the H7N3 virus, including rapid weight loss (>20%) within the first 3 days following inoculation (Fig. 4A). Importantly, the H7N3PB2 virus was significantly (P < 0.005, days 8 and 10; P < 0.01, days 12 and 14) less virulent than the PH1N1 virus at the lower inoculum (Fig. 4D). Inoculation with 104 H7N3NA or H7N3M resulted in levels of weight loss that were equivalent to those seen with H7N3 at all times (Fig. 4B; P > 0.1). Inoculation with reassortant H7N3 viruses possessing the PB1, PA, NP, or NS of PH1N1 did not induce appreciable weight loss at any day postinoculation, suggesting that these gene segments from PH1N1 attenuate H7N3 virulence in vivo.
FIG 5.
Reassortant H7 viruses containing PH1N1 PB2, NA, or M induce considerable morbidity in mice. (A to C) Groups of male C57BL/6J mice were inoculated intranasally with 104 TCID50 of the indicated viruses, and weight loss was measured for 7 days. Morbidity is displayed as percentages of original body weight remaining for mice inoculated with the indicated virus that showed weight loss that was significantly greater than (A), equal to (B), or significantly less than (C) that seen with the parental H7N3 virus. (D) Male C57BL/6J mice were inoculated intranasally with 103 TCID50 of H7N3, PH1N1, or H7N3 containing the PB2 segment of PH1N1 (H7N3PB2), and weight loss was measured for 14 days. The data represent the averages and standard errors of the means of results determined for at least six animals from two or more independently performed experiments per virus. (*, P < 0.05; **, P < 0.01; ***, P < 0.005; ****, P < 0.001 [compared to H7N3 values]; ##, P < 0.01; ###, P < 0.005; ####, P < 0.001 [compared to PH1N1 values].)
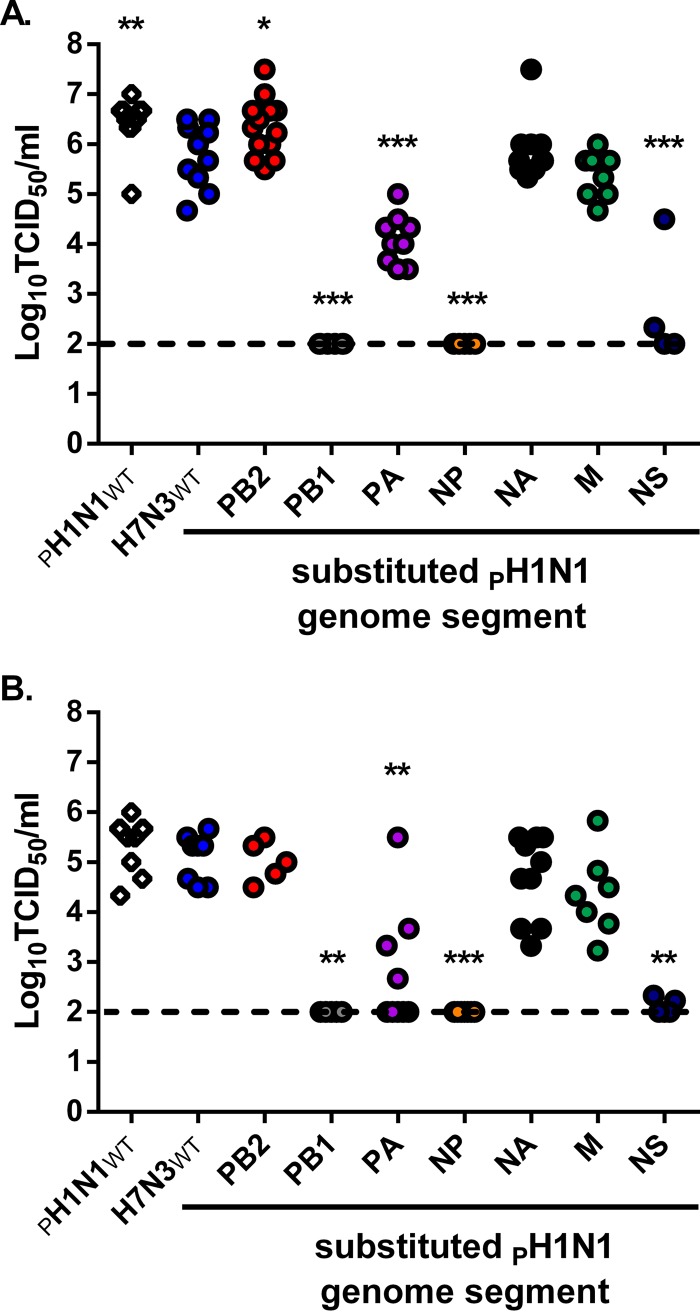
H7N3 reassortant viruses possessing PH1N1 PB2, NA, or M do not attenuate replication in vivo.
To further evaluate the compatibility between H7N3 and PH1N1 viruses, we measured virus titers in lung tissue 3 and 7 dpi with 104 TCID50 of all parental and single-gene reassortants. Lung viral titers 3 days after PH1N1 virus inoculation (106.4/ml) were significantly (P < 0.005) higher than those seen after H7N3 virus inoculation (105.9/ml; Fig. 5A). However, this difference in virus load disappeared by day 7 for H7N3 (105.3/ml) and PH1N1 (105.7/ml) (P > 0.15; Fig. 5B). The virus load in lungs of H7N3PB2-infected animals was significantly higher at 3 dpi (106.5/ml; P < 0.05) but not at 7 dpi (105.0/ml; P > 0.15) than that seen with H7N3 virus. Importantly, the viral load in H7N3PB2-infected lungs was similar to that of PH1N1 virus at day 3. Inoculation with H7N3NA or H7N3M resulted in lung virus titers similar to those seen with H7N3 at both 3 dpi (105.7/ml for H7N3NA and 105.5/ml for H7N3M) and 7 dpi (105.2/ml for H7N3NA and 104.3/ml for H7N3M) (P > 0.05 for all comparisons). H7N3 reassortant viruses bearing the PA or NS gene segment of PH1N1 replicated in vivo; however, the virus titers were significantly lower at 3 dpi (104.0/ml for H7N3PA and 102.2/ml for H7N3NS; P < 0.005 and P < 0.01, respectively) and 7 dpi (102.0/ml for H7N3PA and 102.0/ml for H7N3NS; P < 0.005 and P < 0.005, respectively) than the H7N3 virus titers (Fig. 5). Finally, H7N3NP and H7N3PB1 viruses were never detected at 3 or 7 dpi. These results suggest that the PB2, NA, and M genes of PH1N1 are genetically and functionally compatible with the remaining segments of an avian H7 IAV.
FIG 5.
H7N3 replicates extensively in the lungs of C57BL/6J mice, and PH1N1 PB2, NA, or M does not attenuate H7N3 replication. Male C57BL/6J mice were inoculated with 104 TCID50 of H7N3, PH1N1, or the indicated reassortant virus, and lung viral titers were quantified 3 and 7 days postinoculation. Virus titer present in whole-lung homogenate at day 3 (A) or day 7 (B) was determined by virus titration assay performed on MDCK cells and expressed as TCID50 per milliliter. Viral titers were derived from results determined for five or more mice from two or more independently performed experiments. The limit of detection was 100 TCID50 (dotted line). (*, P < 0.05; **, P < 0.01; ***, P < 0.005 [compared to H7N3 values].)
PH1N1 PB2, NA, or M shows no signs of genetic adaptation in the context of a predominantly H7N3 genome constellation.
We analyzed the nucleotide sequence of substituted PH1N1 gene segments in the context of the H7N3:PH1N1 7 + 1 viruses after passage in eggs and replication in mice. Six of the seven PH1N1 gene segments contained no nucleotide changes upon culture in eggs. A single point mutation was found in the PA gene of PH1N1 (P295L) in H7N3PA grown 48 h in eggs. This same mutation was identified a second time following an independent attempt to rescue virus with a genetic sequence identical to that of the original PH1N1 PA gene. To analyze genetic stability in vivo, we isolated RNA from lungs of mice infected 7 days with H7N3PB2 (n = 3), H7N3NA (n = 3), and H7N3M (n = 3). No nucleotide changes were found in any of the PB2, NA, or M genes of PH1N1 in the context of the H7N3 virus. Taken together, these data suggest that the PH1N1 gene segments are genetically stable and highly functional in the context of an avian H7N3 virus.
H7N3 and reassortant viruses that contain PH1N1 PB2, NA, or M viruses induce robust inflammatory cytokine and chemokine responses in vivo.
The virulence and fitness of an influenza virus in the mouse model are often associated with elevated production of proinflammatory cytokines and chemokines (18–20). To further evaluate the functional compatibility between PH1N1 and H7N3 genes, we quantified the inflammatory response in lung tissue 3 and 7 days postinoculation with the three most virulent H7N3:PH1N1 7 + 1 reassortant viruses (H7N3PB2, H7N3NA, and H7N3M) and compared the response to that of parental H7N3 and PH1N1 virus. The parental H7N3 virus induced significantly (P < 0.05) higher concentrations of inflammatory mediators, such as IL-12(p40), than PH1N1 early following inoculation (day 3) (Table 1). Infection with H7N3PB2 induced higher concentrations of key inflammatory mediators, including CCL2, CCL3, and CCL5, than infection with H7N3 (P < 0.05) (Table 2). H7N3PA replication was attenuated in vivo, and this virus correspondingly induced significantly lower levels of many inflammatory cytokines than H7N3 (P < 0.05). By 7 days postinfection, PH1N1-infected lungs had higher concentrations of cytokines than parental H7N3-infected lungs, while H7N3PB2 produced even more exacerbated responses in many mediators, including IL-10, CCL2, CCL3, CCL5, and TNF-α (P < 0.05 to P < 0.001 relative to H7N3 results). H7N3NA and H7N3M elicited inflammatory responses that more closely resembled the profile of H7N3 than PH1N1 at both time points following infection.
TABLE 1.
Inflammatory cytokine and chemokine levels in total lung homogenates 3 days after intranasal inoculation with parental H7N3, PH1N1, and reassortant viruses
| Cytokine (pg/ml) | Concentration (pg/ml) (mean ± SEM) in mouse lung after inoculation witha: |
||||
|---|---|---|---|---|---|
| H7N3WT virus (n = 6) | H7N3PB2 virus (n = 5) | H7N3NA virus (n = 6) | H7N3M virus (n = 5) | PH1N1WT virus (n = 7) | |
| IL-1α | 267 ± 5 | 32 ± 4 | 23 ± 6 | 33 ± 7 | 12 ± 5 |
| IL-1β | 360 ± 112 | 436 ± 57 | 494 ± 73 | 498 ± 66 | 169 ± 22 |
| IL-5 | 294 ± 95 | 529 ± 56** | 423 ± 45 | 356 ± 58 | 29 ± 13* |
| IL-6 | 228 ± 69 | 363 ± 78 | 451 ± 49* | 288 ± 57 | 70 ± 30 |
| IL-10 | 21 ± 3 | 20 ± 2 | 16 ± 2 | 20 ± 2 | 13 ± 4 |
| IL-12p40 | 253 ± 63 | 421 ± 65* | 244 ± 36 | 383 ± 51 | 85 ± 24* |
| IL-12p70 | 100 ± 27 | 48 ± 7 | 44 ± 8 | 55 ± 12 | 63 ± 36 |
| IL-13 | 52 ± 3 | 64 ± 5 | 45 ± 5 | 48 ± 5 | 26 ± 3* |
| Eotaxin | 462 ± 97 | 613 ± 24 | 732 ± 60* | 570 ± 107 | 175 ± 25** |
| G-CSF | 268 ± 78 | 579 ± 113* | 336 ± 92 | 263 ± 22 | 249 ± 91 |
| GM-CSF | 67 ± 11 | 65 ± 5 | 57 ± 6 | 50 ± 6 | 46 ± 13 |
| IFN-γ | 9 ± 1 | 20 ± 3*** | 7 ± 1 | 9 ± 3 | 5 ± 1 |
| KC | 370 ± 88 | 435 ± 119 | 456 ± 95 | 533 ± 52 | 151 ± 56 |
| CCL2 | 586 ± 129 | 3,145 ± 716* | 1,115 ± 84 | 758 ± 99 | 835 ± 292 |
| CCL3 | 52 ± 16 | 125 ± 18* | 77 ± 24 | 65 ± 21 | 22 ± 8 |
| CCL4 | 72 ± 20 | 128 ± 34 | 84 ± 17 | 68 ± 6 | 44 ± 8 |
| CCL5 | 89 ± 13 | 148 ± 27* | 125 ± 25 | 105 ± 31 | 66 ± 24 |
| TNF-α | 172 ± 49 | 123 ± 12 | 126 ± 21 | 100 ± 9 | 262 ± 52 |
*, P < 0.05; **, P < 0.01; ***, P < 0.005 (compared to H7N3 values).
TABLE 2.
Inflammatory cytokine and chemokine levels in total lung homogenates 7 days after intranasal inoculation with parental H7N3, PH1N1, and reassortant viruses
| Cytokine (pg/ml) | Concentration (pg/ml) (mean ± SEM) in mouse lung after inoculation witha: |
||||
|---|---|---|---|---|---|
| H7N3WT virus (n = 5) | H7N3PB2 virus (n = 7) | H7N3NA virus (n = 7) | H7N3M virus (n = 4) | PH1N1WT virus (n = 10) | |
| IL-1α | 13 ± 1 | 48 ± 4*** | 22 ± 8 | 32 ± 2*** | 31 ± 2* |
| IL-1β | 313 ± 80 | 669 ± 77 | 337 ± 99 | 840 ± 51* | 519 ± 112 |
| IL-5 | 131 ± 35 | 120 ± 23 | 313 ± 95 | 178 ± 36 | 235 ± 35 |
| IL-6 | 198 ± 39 | 148 ± 35 | 355 ± 105 | 183 ± 45 | 790 ± 85*** |
| IL-10 | 62 ± 6 | 247 ± 63*** | 76 ± 27 | 109 ± 16 | 123 ± 12 |
| IL-12p40 | 328 ± 78 | 462 ± 66 | 218 ± 52 | 713 ± 122** | 313 ± 39 |
| IL-12p70 | 44 ± 9 | 104 ± 24* | 63 ± 10 | 37 ± 3 | 82 ± 14 |
| IL-13 | 92 ± 14 | 248 ± 19* | 92 ± 16 | 193 ± 10 | 123 ± 44 |
| Eotaxin | 1,678 ± 563 | 465 ± 89*** | 464 ± 94*** | 432 ± 88*** | 393 ± 55*** |
| G-CSF | 288 ± 53 | 289 ± 87 | 333 ± 127 | 490 ± 141 | 1,362 ± 105*** |
| GM-CSF | 46 ± 6 | 80 ± 7 | 37 ± 3 | 105 ± 4 | 152 ± 85 |
| IFN-γ | 46 ± 12 | 63 ± 27 | 24 ± 18 | 51 ± 1 | 276 ± 96 |
| KC | 196 ± 65 | 351 ± 54 | 284 ± 130 | 153 ± 59 | 338 ± 80 |
| CCL2 | 750 ± 25 | 2,580 ± 610** | 402 ± 198 | 201 ± 114 | 2,273 ± 288* |
| CCL3 | 172 ± 18 | 2,544 ± 610*** | 96 ± 35 | 737 ± 243 | 692 ± 171 |
| CCL4 | 196 ± 41 | 156 ± 35 | 99 ± 63 | 69 ± 13* | 110 ± 20 |
| CCL5 | 692 ± 78 | 1,672 ± 333* | 271 ± 193 | 593 ± 116 | 294 ± 65 |
| TNF-α | 161 ± 27 | 478 ± 99** | 221 ± 44 | 167 ± 21 | 307 ± 35 |
*, P < 0.05; **, P < 0.01; ***, P < 0.005 (compared to H7N3 values).
DISCUSSION
The ongoing reassortment of avian and human IAV threatens human populations worldwide as evidenced by numerous recent zoonotic events (21). Along with H5 and H9 subtypes, H7 subtype viruses are thought to be candidates for generating a pandemic IAV. We sought to determine the potential for reassortment between a low-pathogenicity North American avian H7N3 virus and diverse avian and mammalian virus isolates. Our studies identified a clear bias toward reassortment of H7N3 with gene segments derived from the 2009 pandemic H1N1 (PH1N1) virus but not other mammalian virus isolates. We found that single-reassortant H7N3 viruses containing PB2, NA, or M segments of PH1N1 do not attenuate the H7N3 virus in vitro or in vivo. Our results highlight the potential for environmental reassortment that can lead to the introduction of antigenically novel viruses capable of inducing disease in mammals and may inform future surveillance efforts. Moreover, these findings support the potential for emergence of future prepandemic viruses in avian populations without prior mammalian adaptation.
We used a novel plasmid-based genetic screen to assess the compatibility of human and avian genome segments in the context of a low-pathogenicity North American H7N3 virus. We found that PH1N1 genome segments were selected most frequently among mammal-derived segments, suggesting a high degree of functional compatibility of these segments with the H7N3 virus compared to prepandemic human isolates. We found no instances of seasonal H1N1 (SH1N1) gene segments reassorting with the avian virus and observed inclusion of genes from the PR8H1N1 strain only seldom. This striking difference suggests that the current H1N1 virus (PH1N1) is more likely to reassort with other viruses and create novel pandemic viruses. While the mechanism underlying this preference is unknown, it is plausible that the extended adaptation of gene segments of SH1N1 to the human host and other segments of SH1N1 has decreased its ability to reassort with avian or other human viruses. In contrast, gene segments of PH1N1 are found in many different virus isolates, validating the ability to reassort rapidly with other strains of influenza virus.
We observed a high frequency of H7N3 and H7N9 segment selection in instances in which these segments were closely related (Fig. 1B). However, high nucleotide similarity to the parental H7N3 segment, for example, in the M and NA segments, did not result in high rates of selection in all instances. This difference perhaps indicates that, within this system, structural and functional contacts between proteins or RNA genome segments, and not specifically relatedness, drive viral replication and therefore selection.
Historically, reassortment of influenza viruses has been studied using coinfection models. These experiments provided important information about the natural evolution of IAV; however, they are less controlled and potentially more hazardous if either or both IAVs have previously been shown to transmit between mammals. We provide an alternative method to study influenza reassortment and argue that these experiments not only are safer but also address a different question: what are the molecular requirements for a single gene segment to compete with and reassort into an existing virus genome? Knowing the key features in a genome segment that promotes or inhibits reassortment will result in a better understanding of the process as a whole and therefore improve our predictions of the outcome of experimental and natural coinfections.
These studies identified two pandemic IAV gene segments, NA and M, which in the context of H7N3 virus do not impact viral replication in MDCK cells or pathogenesis in mice. The compatibility of these genes with H7N3 is of interest given their prior association with increased transmission of the 2009 pandemic H1N1 compared with putative pandemic progenitors (22). Multiple independent reassortment events between human and swine influenza viruses resulted in the creation of novel genome constellations (H1N1v, H2N1v, and H3N2v) capable of aerosol transmission from pig to human due to acquisition of PH1N1 M. Previous investigations of potential reassortment between a highly pathogenic avian H5N1 influenza virus and PH1N1 demonstrated high compatibility between H5N1 and the NA and M segments of PH1N1 (23). The resulting reassortant viruses similarly did not have altered in vitro replication relative to wild-type H5N1 virus. To further experimentally corroborate the importance of this segment in PH1N1 transmission, multiple studies engineered reassortant viruses that either gained or lost the ability to transmit between mammals following manipulation of M (22, 24). In combination with M, NA was capable of enhancing the transmission of PH1N1 through altered receptor-destroying activity (NA) and filamentous-particle morphology (M) that change virus release from the respiratory tract of infected animals compared to results seen with diverse contemporary swine isolates. Although our studies did not examine virion morphology or respiratory shedding, additional studies in a model more suitable for examining such phenotypes may provide insights into the activity of these genes in the genetic background of an avian influenza virus.
The potential for transmission of H7-bearing viruses has been demonstrated experimentally (25). Since other North American H7-HA are able to bind both avian and mammalian receptors, additional adaptations or acquisition of other gene segments via reassortment may be critical to achieve sustained mammalian transmission (26–28). Other avian viral subtypes (i.e., H9N2 and H5N1) can reassort with PH1N1 and achieve contact or respiratory droplet transmission (2, 4, 15). Additionally, reassortant viruses possessing PH1N1 M are capable of directly infecting humans from pigs (29). Our studies show that H7N3 viruses possessing PB2, NA, or M from PH1N1 are not attenuated in vivo and induce disease comparable to that seen with wild-type H7N3 without adaptation. Further studies of these viruses and other similar single-reassortant avian viruses in mammalian transmission models are required to understand the constellation of reassortants that are potential sources of new zoonoses.
PB2 is the only PH1N1 gene segment that increased virulence and replication in vivo relative to that of wild-type H7N3 despite attenuation in vitro. Previous studies have identified several amino acid substitutions that are associated with efficient replication in mammalian cells, including G590S, Q591R, E627K, and D701N (30–33). The PB2 of H7N3 virus contains all avian virus residues, while the PB2 of PH1N1 has the G590S and Q591R substitutions. Based on this information, we anticipated that the PB2 of PH1N1 would increase replication of the H7N3 7 + 1 virus in mammalian cells. As increased viral replication may exacerbate initial inflammatory responses and lead to subsequent morbidity (18, 20), we assessed the abundance of cytokines and chemokines present in whole-lung homogenate at two points following infection. Mammal-adapted PH1N1 PB2 increased induction of proinflammatory cytokines IL-6, CCL2, and CCL3 early (day 3) during infection. CCL2 levels also correlated well with morbidity when assessed later during infection at 7 dpi, likely due to increased viral replication early following inoculation. Importantly, while morbidity and viral titer were increased relative to parental H7N3 levels, substitution of PH1N1PB2 did not induce morbidity equivalent to that seen with parental PH1N1 at a low-inoculum dose.
While most H7N3 7 + 1 reassortant viruses did not contain mutations in the PH1N1 gene segment, we repeatedly recovered H7N3PA virus containing an amino acid substitution at position 295 (P295L). In a unique isolate from the 2009 pandemic—A/Tennessee/560/09 (H1N1)—mouse adaptation introduced the inverse mutation PA L295P (34). Upon further examination, creation of a virus with only this mutation led to increased viral replication in normal human bronchial epithelial (NHBE) cells (35). In a different study, the same group described L295P as contributing to increased and prolonged viral shedding and disease in both donor and contact ferrets (36). Additionally, in the same polymerase assay that we utilized, A/Tennessee/560/09 PA L295P increased reporter activity in the context of other A/Tennessee/560/09 proteins and the coexpressed level of PB2 but not of NP (34). The importance of this residue had not to our knowledge been examined in the context of A/California/04/09 PA before this report, though it may be surmised that the P295L mutation is detrimental to PA function in the mammalian host and perhaps was selected for due to interaction with the avian host during growth in chicken eggs or with a component of the H7N3 polymerase complex.
In the context of the H7N3 polymerase complex, this mutation reduced the polymerase activity 2-fold (Fig. 3). At this time we cannot address if the observed differences in polymerase activity were due to altered protein half-life, expression level, or the inherent enzymatic activity of PH1N1 PA in either H7N3 or PH1N1 complexes. It is not known if this mutation affected the virulence of H7N3PA in mice, but, on the basis of published data, we expect that an H7N3 virus containing the wild-type PA of PH1N1 (P295) would be more virulent.
Taking the data together, we have established that the 2009 pandemic H1N1 virus has a high degree of compatibility with a North American LPAI H7N3 virus. Further, the single genome segment reassortant viruses containing the PH1N1 segment(s) most frequently selected (PB2, NA, or M) establish productive infection in the mouse respiratory tract, induce morbidity and disease, and persist for at least 1 week, potentially allowing dissemination to others by contact or respiratory transmission. Future studies may examine the potential for transmission of these H7 viruses containing single genes from 2009 pandemic H1N1. These studies emphasize the need for continued surveillance of the avian IAV reservoir and the critical importance of identifying reassortant viruses that contain genomic signatures associated with mammalian disease and transmission.
ACKNOWLEDGMENTS
G.D.W. was supported in part by the Victoria J. Fraser, M.D. Fellowship for Graduate Studies in Infectious Diseases and the Division of Biology and Biomedical Sciences at Washington University School of Medicine.
Finally, we are thankful for the technical assistance of Traci Bricker.
REFERENCES
- 1.Yu H, Cowling BJ, Feng L, Lau EHY, Liao Q, Tsang TK, Peng Z, Wu P, Liu F, Fang VJ, Zhang H, Li M, Zeng L, Xu Z, Li Z, Luo H, Li Q, Feng Z, Cao B, Yang W, Wu JT, Wang Y, Leung GM. 2013. Human infection with avian influenza A H7N9 virus: an assessment of clinical severity. Lancet 382:138–145. doi: 10.1016/S0140-6736(13)61207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kimble JB, Angel M, Wan H, Sutton TC, Finch C, Perez DR. 2014. Alternative reassortment events leading to transmissible H9N1 influenza viruses in the ferret model. J Virol 88:66–71. doi: 10.1128/JVI.02677-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Itoh Y, Shinya K, Kiso M, Watanabe T, Sakoda Y, Hatta M, Muramoto Y, Tamura D, Sakai-Tagawa Y, Noda T, Sakabe S, Imai M, Hatta Y, Watanabe S, Li C, Yamada S, Fujii K, Murakami S, Imai H, Kakugawa S, Ito M, Takano R, Iwatsuki-Horimoto K, Shimojima M, Horimoto T, Goto H, Takahashi K, Makino A, Ishigaki H, Nakayama M, Okamatsu M, Takahashi K, Warshauer D, Shult PA, Saito R, Suzuki H, Furuta Y, Yamashita M, Mitamura K, Nakano K, Nakamura M, Brockman-Schneider R, Mitamura H, Yamazaki M, Sugaya N, Suresh M, Ozawa M, Neumann G, Gern J, Kida H, Ogasawara K, Kawaoka Y. 2009. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature 460:1021–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Y, Zhang Q, Kong H, Jiang Y, Gao Y, Deng G, Shi J, Tian G, Liu L, Liu J, Guan Y, Bu Z, Chen H. 2013. H5N1 Hybrid viruses bearing 2009/H1N1 virus genes transmit in guinea pigs by respiratory droplet. Science 340:1459–1463. doi: 10.1126/science.1229455. [DOI] [PubMed] [Google Scholar]
- 5.Wu A, Su C, Wang D, Peng Y, Liu M, Hua S, Li T, Gao GF, Tang H, Chen J, Liu X, Shu Y, Peng D, Jiang T. 2013. Sequential reassortments underlie diverse influenza H7N9 genotypes in China. Cell Host Microbe 14:446–452. doi: 10.1016/j.chom.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Kapczynski DR, Pantin-Jackwood M, Guzman SG, Ricardez Y, Spackman E, Bertran K, Suarez DL, Swayne DE. 2013. Characterization of the 2012 highly pathogenic avian influenza H7N3 virus isolated from poultry in an outbreak in Mexico: pathobiology and vaccine protection. J Virol 87:9086–9096. doi: 10.1128/JVI.00666-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watanabe T, Kiso M, Fukuyama S, Nakajima N, Imai M, Yamada S, Murakami S, Yamayoshi S, Iwatsuki-Horimoto K, Sakoda Y, Takashita E, McBride R, Noda T, Hatta M, Imai H, Zhao D, Kishida N, Shirakura M, de Vries RP, Shichinohe S, Okamatsu M, Tamura T, Tomita Y, Fujimoto N, Goto K, Katsura H, Kawakami E, Ishikawa I, Watanabe S, Ito M, Sakai-Tagawa Y, Sugita Y, Uraki R, Yamaji R, Eisfeld AJ, Zhong G, Fan S, Ping J, Maher EA, Hanson A, Uchida Y, Saito T, Ozawa M, Neumann G, Kida H, Odagiri T, Paulson JC, Hasegawa H, Tashiro M, Kawaoka Y. 2013. Characterization of H7N9 influenza A viruses isolated from humans. Nature 501:551–555. doi: 10.1038/nature12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gabbard JD, Dlugolenski D, Van Riel D, Marshall N, Galloway SE, Howerth EW, Campbell PJ, Jones C, Johnson S, Byrd-Leotis L, Steinhauer DA, Kuiken T, Tompkins SM, Tripp R, Lowen AC, Steel J. 2014. Novel H7N9 influenza virus shows low infectious dose, high growth rate, and efficient contact transmission in the guinea pig model. J Virol 88:1502–1512. doi: 10.1128/JVI.02959-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Belser JA, Gustin KM, Pearce MB, Maines TR, Zeng H, Pappas C, Sun X, Carney PJ, Villanueva JM, Stevens J, Katz JM, Tumpey TM. 2013. Pathogenesis and transmission of avian influenza A (H7N9) virus in ferrets and mice. Nature 501:556–559. doi: 10.1038/nature12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Richard M, Schrauwen EJA, de Graaf M, Bestebroer TM, Spronken MIJ, van Boheemen S, de Meulder D, Lexmond P, Linster M, Herfst S, Smith DJ, van den Brand JM, Burke DF, Kuiken T, Rimmelzwaan GF, Osterhaus ADME, Fouchier RAM. 2013. Limited airborne transmission of H7N9 influenza A virus between ferrets. Nature 501:560–563. doi: 10.1038/nature12476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bahl J, Krauss S, Kühnert D, Fourment M, Raven G, Pryor SP, Niles LJ, Danner A, Walker D, Mendenhall IH, Su YCF, Dugan VG, Halpin RA, Stockwell TB, Webby RJ, Wentworth DE, Drummond AJ, Smith GJD, Webster RG. 2013. Influenza A virus migration and persistence in North American wild birds. PLoS Pathog 9:e1003570. doi: 10.1371/journal.ppat.1003570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith GJD, Vijaykrishna D, Bahl J, Lycett SJ, Worobey M, Pybus OG, Ma SK, Cheung CL, Raghwani J, Bhatt S, Peiris JSM, Guan Y, Rambaut A. 2009. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature 459:1122–1125. doi: 10.1038/nature08182. [DOI] [PubMed] [Google Scholar]
- 13.Nelson MI, Vincent AL, Kitikoon P, Holmes EC, Gramer MR. 2012. Evolution of novel reassortant A/H3N2 influenza viruses in North American swine and humans, 2009–2011. J Virol 86:8872–8878. doi: 10.1128/JVI.00259-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pascua PNQ, Song MS, Lee JH, Baek YH, Kwon HI, Park SJ, Choi EH, Lim GJ, Lee OJ, Kim SW, Kim CJ, Sung MH, Kim MH, Yoon SW, Govorkova EA, Webby RJ, Webster RG, Choi YK. 2012. Virulence and transmissibility of H1N2 influenza virus in ferrets imply the continuing threat of triple-reassortant swine viruses. Proc Natl Acad Sci U S A 109:15900–15905. doi: 10.1073/pnas.1205576109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kimble JB, Sorrell E, Shao H, Martin PL, Perez DR. 2011. Compatibility of H9N2 avian influenza surface genes and 2009 pandemic H1N1 internal genes for transmission in the ferret model. Proc Natl Acad Sci U S A 108:12084–12088. doi: 10.1073/pnas.1108058108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li C, Hatta M, Nidom CA, Muramoto Y, Watanabe S, Neumann G, Kawaoka Y. 2010. Reassortment between avian H5N1 and human H3N2 influenza viruses creates hybrid viruses with substantial virulence. Proc Natl Acad Sci U S A 107:4687–4692. doi: 10.1073/pnas.0912807107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reed LJ, Muench H. 1938. A simple method of estimating fifty per cent endpoints. Am J Hyg 27:285–297. http://aje.oxfordjournals.org/content/27/3/493.extract. [Google Scholar]
- 18.Boon AC, Williams RW, Sinasac DS, Webby RJ. 2014. A novel genetic locus linked to pro-inflammatory cytokines after virulent H5N1 virus infection in mice. BMC Genomics 15:1017. doi: 10.1186/1471-2164-15-1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Walsh KB, Teijaro JR, Wilker PR, Jatzek A, Fremgen DM, Das SC, Watanabe T, Hatta M, Shinya K, Suresh M, Kawaoka Y, Rosen H, Oldstone MBA. 2011. Suppression of cytokine storm with a sphingosine analog provides protection against pathogenic influenza virus. Proc Natl Acad Sci U S A 108:12018–12023. doi: 10.1073/pnas.1107024108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shoemaker JE, Fukuyama S, Eisfeld AJ, Zhao D, Kawakami E, Sakabe S, Maemura T, Gorai T, Katsura H, Muramoto Y, Watanabe S, Watanabe T, Fuji K, Matsuoka Y, Kitano H, Kawaoka Y. 2015. An ultrasensitive mechanism regulates influenza virus-Induced inflammation. PLoS Pathog 11:e1004856. doi: 10.1371/journal.ppat.1004856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Capua I, Munoz O. 2013. Emergence of influenza viruses with zoonotic potential: open issues which need to be addressed. A review. Vet Microbiol 165:7–12. doi: 10.1016/j.vetmic.2013.01.044. [DOI] [PubMed] [Google Scholar]
- 22.Lakdawala SS, Lamirande EW, Suguitan AL, Wang W, Santos CP, Vogel L, Matsuoka Y, Lindsley WG, Jin H, Subbarao K. 29 December 2011. Eurasian-origin gene segments contribute to the transmissibility, aerosol release, and morphology of the 2009 pandemic H1N1 influenza virus. PLoS Pathog doi: 10.1371/journal.ppat.1002443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schrauwen EJA, Bestebroer TM, Rimmelzwaan GF, Osterhaus ADME, Fouchier RAM, Herfst S. 2013. Reassortment between avian H5N1 and human influenza viruses is mainly restricted to the matrix and neuraminidase gene segments. PLoS One 8:e59889. doi: 10.1371/journal.pone.0059889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chou Y, Albrecht RA, Pica N, Lowen AC, Richt JA, García-Sastre A, Palese P, Hai R. 2011. The M segment of the 2009 new pandemic H1N1 influenza virus is critical for its high transmission efficiency in the guinea pig model. J Virol 85:11235–11241. doi: 10.1128/JVI.05794-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sutton TC, Finch C, Shao H, Angel M, Chen H, Capua I, Cattoli G, Monne I, Perez DR. 2014. Airborne transmission of highly pathogenic H7N1 influenza virus in ferrets. J Virol 88:6623–6635. doi: 10.1128/JVI.02765-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schrauwen EJ, Fouchier RA. 2014. Host adaptation and transmission of influenza A viruses in mammals. Emerg Microbes Infect 3:e9. doi: 10.1038/emi.2014.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Belser JA, Davis CT, Balish A, Edwards LE, Zeng H, Maines TR, Gustin KM, Martinez IL, Fasce R, Cox NJ, Katz JM, Tumpey TM. 2013. Pathogenesis, transmissibility, and ocular tropism of a highly pathogenic avian influenza A (H7N3) virus associated with human conjunctivitis. J Virol 87:5746–5754. doi: 10.1128/JVI.00154-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Belser JA, Blixt O, Chen L-M, Pappas C, Maines TR, Van Hoeven N, Donis R, Busch J, McBride R, Paulson JC, Katz JM, Tumpey TM. 2008. Contemporary North American influenza H7 viruses possess human receptor specificity: implications for virus transmissibility. Proc Natl Acad Sci U S A 105:7558–7563. doi: 10.1073/pnas.0801259105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kitikoon P, Vincent AL, Gauger PC, Schlink SN, Bayles DO, Gramer MR, Darnell D, Webby RJ, Lager KM, Swenson SL, Klimov A. 2012. Pathogenicity and transmission in pigs of the novel A(H3N2)v influenza virus isolated from humans and characterization of swine H3N2 viruses isolated in 2010–2011. J Virol 86:6804–6814. doi: 10.1128/JVI.00197-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mehle A, Doudna JA. 2009. Adaptive strategies of the influenza virus polymerase for replication in humans. Proc Natl Acad Sci U S A 106:21312–21316. doi: 10.1073/pnas.0911915106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yamada S, Hatta M, Staker BL, Watanabe S, Imai M, Shinya K, Sakai-Tagawa Y, Ito M, Ozawa M, Watanabe T, Sakabe S, Li C, Kim JH, Myler PJ, Phan I, Raymond A, Smith E, Stacy R, Nidom CA, Lank SM, Wiseman RW, Bimber BN, O'Connor DH, Neumann G, Stewart LJ, Kawaoka Y. 2010. Biological and structural characterization of a host-adapting amino acid in influenza virus. PLoS Pathog 6:e1001034. doi: 10.1371/journal.ppat.1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gabriel G, Dauber B, Wolff T, Planz O, Klenk H-D, Stech J. 2005. The viral polymerase mediates adaptation of an avian influenza virus to a mammalian host. Proc Natl Acad Sci U S A 102:18590–18595. doi: 10.1073/pnas.0507415102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hatta M, Gao P, Halfmann P, Kawaoka Y. 2001. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science 293:1840–1842. doi: 10.1126/science.1062882. [DOI] [PubMed] [Google Scholar]
- 34.Ilyushina NA, Khalenkov AM, Seiler JP, Forrest HL, Bovin NV, Marjuki H, Barman S, Webster RG, Webby RJ. 2010. Adaptation of pandemic H1N1 influenza viruses in mice. J Virol 84:8607–8616. doi: 10.1128/JVI.00159-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ducatez MF, Ilyushina NA, Fabrizio TP, Rehg JE, Bovin NV, Webster RG, Webby RJ. 2012. Both influenza hemagglutinin and polymerase acidic genes are important for delayed pandemic 2009 H1N1 virus clearance in the ferret model. Virology 432:389–393. doi: 10.1016/j.virol.2012.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ilyushina NA, Ducatez MF, Rehg JE, Marathe BM, Marjuki H, Bovin NV. 2010. Does pandemic A/H1N1 virus have the potential to become more pathogenic? MBio 1:(5)e00249-10. doi: 10.1128/mBio.00249-10. [DOI] [PMC free article] [PubMed] [Google Scholar]