Abstract
Hepatic steatosis is defined as intrahepatic fat of at least 5% of liver weight. Simple accumulation of triacylglycerols in the liver could be hepatoprotective; however, prolonged hepatic lipid storage may lead to liver metabolic dysfunction, inflammation, and advanced forms of nonalcoholic fatty liver disease. Nonalcoholic hepatic steatosis is associated with obesity, type 2 diabetes, and dyslipidemia. Several mechanisms are involved in the accumulation of intrahepatic fat, including increased flux of fatty acids to the liver, increased de novo lipogenesis, and/or reduced clearance through β-oxidation or very-low-density lipoprotein secretion. This article summarizes the mechanisms involved in the accumulation of triacylglycerols in the liver, the clinical implications, and the prevention of hepatic steatosis, with a focus on the role of mitochondrial function and lifestyle modifications.
Keywords: Mitochondria, hepatic steatosis, mitochondrial trifunctional protein, β-oxidation, fatty acids, exercise, diet, fatty liver, triacylglycerol
Nonalcoholic hepatic steatosis is present in 33% of the adult population in the United States1 and is characterized by the accumulation of triacylglycerol (TAG)-rich macrovesicular and/or microvesicular lipid droplets within the hepatocytes, in the absence of inflammation or liver injury. Hepatic steatosis or fatty liver is defined as intrahepatic TAG of at least 5% of liver weight or 5% of hepatocytes containing lipid vacuoles in the absence of a secondary contributing factor such as excess alcohol intake, viral infection, or drug treatments. Liver steatosis is graded based on the percentage of fat within the hepatocytes: grade 0 (healthy, <5%), grade 1 (mild, 5%-33%), grade 2 (moderate, 34%-66%), and grade 3 (severe, >66%).2 Initially, TAG synthesis and accumulation of fat in the liver are thought to be hepatoprotective; however, excess intrahepatic fat content is a risk factor for disease progression.3 Simple hepatic steatosis is a reversible condition that can be corrected by lifestyle modifications such as physical activity and dietary interventions.
Increased caloric intake and reduced physical activity in recent years have undoubtedly contributed to increased obesity and a parallel increase in the prevalence of nonalcoholic fatty liver disease (NAFLD). NAFLD is now the most important cause of chronic liver disease worldwide, manifested by a spectrum of liver abnormalities in the absence of excess alcohol consumption. NAFLD includes hepatic steatosis, defined by intracellular accumulation of TAG in the liver, which may progress to nonalcoholic steatohepatitis (NASH), fibrosis, cirrhosis, and hepatocellular carcinoma. NAFLD is considered the hepatic manifestation of the metabolic syndrome, which is defined by the presence of central obesity, insulin resistance, hyperlipidemia, hyperglycemia, and hypertension. NAFLD is present in 70% of overweight individuals, 70% of diabetic subjects, and up to 90% of morbidly obese individuals. Studies have shown a strong association between NAFLD and insulin resistance even in the absence of obesity. Alarming data indicate that NAFLD is also present in 3% to 10% of normal-weight children and 50% of obese children.4 Furthermore, recent studies suggest that metabolic abnormalities might start early in life in utero and cause NAFLD in children.5
Pathogenesis of Hepatic Steatosis
The liver does not store TAG in normal conditions; however, under stressed settings such as in obesity or with high fat/high carbohydrate intake, abnormal lipid metabolism leads to ectopic hepatic lipid accumulation. In a study comparing subjects with low (3%) and high (17%) intrahepatic TAG levels, individuals with steatosis had 50% higher rates of lipolysis and 30% higher rates of gluconeogenesis, with enhanced mitochondrial oxidative metabolism leading to oxidative stress and liver damage.6 Intrahepatic fat and visceral fat have been shown to be independently associated with metabolic dysfunctions.7 However, weight loss through reducing visceral fat by omentectomy or following Rouxen-Y surgery has not improved peripheral and hepatic insulin sensitivity.8 In addition, other studies suggest that intrahepatic fat, and not visceral fat, correlates with multiorgan insulin resistance and could be directly associated with the dyslipidemia associated with hepatic steatosis.9,10 Dyslipidemia and hyperglycemia are present in approximately 60% of patients with fatty liver.11 Lipid accumulation in the liver is also associated with lipotoxicity due to increased endoplasmic reticulum stress, mitochondrial stress, and impaired mitophagy.12 Thus, increased hepatic TAG could trigger metabolic dysfunction leading to insulin resistance, dyslipidemia, cardiovascular disease, and progression to NASH, cirrhosis, and hepatocellular carcinoma.12
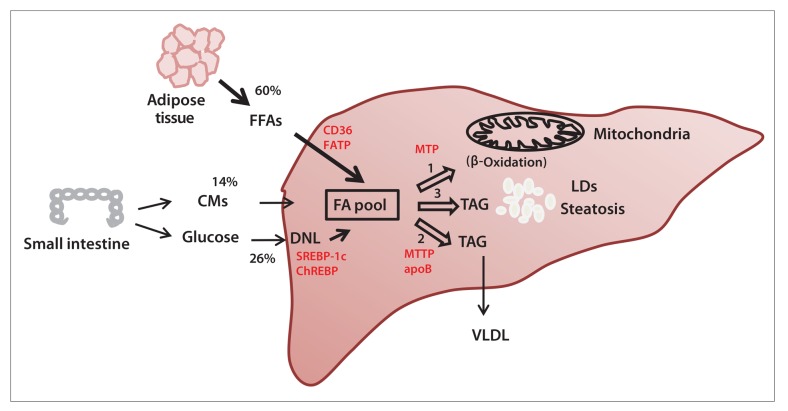
Hepatic free fatty acids (FFAs) can be derived from the diet, adipose tissue lipolysis, and/or de novo lipogenesis. FFAs are then oxidized through β-oxidation, esterified into TAG, and packaged into lipoproteins to be either secreted or stored as lipid droplets (Figure 1). Accumulation of TAG in the liver and the subsequent hepatocellular damage are multifactorial and may involve multiple organs. In addition to the environmental factors, several genetic defects have been shown to be associated with hepatic steatosis.13 Disorders in genes involved in fatty acid uptake, hepatic TAG secretion, and fatty acid oxidation lead to hepatic steatosis.13
Figure 1.
The pathogenesis of hepatic steatosis. Under physiologic conditions, the hepatic fatty acid (FA) pool is the result of a balance between FA influx from the diet and adipose tissue lipolysis, de novo lipogenesis (DNL), and disposal of FAs through β-oxidation or very-low-density lipoprotein (VLDL) assembly and secretion. Increased uptake and reduced clearance of FAs lead to the accumulation of lipid droplets (LDs) and hepatic steatosis. In red are some important proteins involved in the different pathways.
ApoB, apolipoprotein B; CD36, fatty acid translocase; ChREBP, carbohydrate-responsive element—binding protein; CMs, chylomicrons; FATP, fatty acid transport protein; FFAs, free fatty acids; MTP, mitochondrial trifunctional protein; MTTP, microsomal triglyceride transfer protein; SREBP-1c, sterol regulatory element—binding protein 1c; TAG, triacylglycerol.
Role of Fatty Acid Uptake and Trafficking in Hepatic Steatosis
Fatty acid uptake across the plasma membrane of hepatocytes is mediated by membrane proteins such as the fatty acid transport proteins (FATPs) and fatty acid translocase (CD36). The liver expresses 2 of the FATPs: FATP1 and FATP5. Genetic deletion of FATP2 or FATP5 in mice reduces fatty acid uptake by the liver.14,15 Overexpression of FATP5 in mammalian cells increases fatty acid uptake.15 Conversely, FATP5 deletion reduces long-chain fatty acid uptake in FATP5-knockout livers.15 Silencing FATP5 also reverses already-established NAFLD in mice.16 CD36 is expressed in a variety of tissues, including the intestine, adipose tissue, and muscle. The expression of CD36 in the liver is low but increases with obesity and high-fat diets.17,18 Uptake of long-chain fatty acids and lipid accumulation in the liver are directly related to CD36 expression. Similar to the findings in rodent studies, liver biopsies from patients with NAFLD show higher levels of CD36 compared with biopsies from control subjects, highlighting the clinical relevance of CD36 in fatty liver.10,19-21 Tissue distribution of CD36 in subjects with high intrahepatic fat content compared with its distribution in individuals with normal intrahepatic TAG levels has shown an increase in CD36 mRNA and protein levels in the muscle and a decrease in adipose tissue levels.10 Although this study did not show levels of CD36 in the liver, it suggests that alterations in fatty acid uptake in the adipose tissue could be involved in hepatic TAG accumulation by redirecting plasma fatty acid uptake from adipose tissue toward other tissues such as the muscle and liver.10 Furthermore, increased CD36 expression and fatty acid uptake by adipose tissue with peroxisome proliferator—activated receptor-γ agonist in patients with type 2 diabetes is accompanied by reduced hepatic steatosis and improved insulin sensitivity.22-24 Cytosolic fatty acid-binding proteins (FABPs) also play an important role in the trafficking of fatty acids in the liver. Mammalian livers express a single FABP (L-FABP), which enhances long-chain fatty acid uptake.25,26 Mice deficient in L-FABP are protected against diet-induced hepatic steatosis.27,28
Role of De Novo Lipogenesis in Hepatic Steatosis
Lipogenesis generates fatty acids from excess carbohydrates and consists of multiple reactions that take place initially in the mitochondrial matrix and continue in the cytosol. Acetylated coenzyme A (acetyl-CoA) is condensed with oxaloacetate to form tricarboxylate citrate, which is oxidized by the tricarboxylic acid (TCA) cycle. In the case of excess cellular energy, citrate is exported into the cytosol to generate acetyl-CoA, which is subsequently converted to malonyl-CoA by acetyl-CoA carboxylase and then to palmitic acid by fatty acid synthase.29 De novo lipogenesis is activated by high glucose intake and high plasma glucose levels (Figure 1). Glucose regulates carbohydrate-responsive element–binding protein, which in turn regulates lipogenic genes. Plasma glucose levels also affect the expression of lipogenic enzymes by stimulating the release of insulin and inhibiting the release of glucagon from the pancreas. The effect of insulin on the expression of lipogenic genes is regulated by sterol regulatory element–binding protein 1c (SREBP-1c).29 In a recent study comparing subjects with high liver fat content to individuals with low liver fat content (control subjects), people with high liver fat levels had greater fatty acid synthesis than control subjects.30 In control subjects, the contribution of de novo lipogenesis to hepatic fat content is very small in the fasted state (<5% for very-low-density lipoprotein [VLDL]-TAG); however, a higher proportion was found in the fed state (23% for VLDL-TAG), especially with a carbohydrate-rich diet.31-33 In obese hypertriglyceridemic and hyperinsulinemic patients with steatosis, approximately 14% of fat in the liver originated from the diet, 60% from circulating FFAs, and 26% from de novo lipogenesis. In addition, subjects with steatosis had higher nocturnal plasma FFA levels, and the contribution from de novo lipogenesis was not suppressed with fasting, suggesting an important role for lipogenesis in hepatic steatosis.30,34 Thus, in addition to FFA flux to the liver, increased lipogenesis appears to be an important contributor to hepatic TAG levels in fatty liver.34,35
Role of Hepatic Triacylglycerol Assembly and Secretion in Hepatic Steatosis
The assembly and secretion of VLDLs requires the function of apolipoprotein B (apoB) and microsomal triglyceride transfer protein (MTTP).36 Patients with a defect in apoB or MTTP are unable to export lipids from the liver and, hence, develop hepatic steatosis.37-39 Sustained silencing of apoB or MTTP in mice induces hepatic TAG accumulation.40 In addition, apoB100 has been shown to be required for increased VLDL secretion in ob/ob mice, a rodent model for hepatic steatosis.41 A recent study by Fabbrini and colleagues demonstrated that intrahepatic TAG content is a better predictor for VLDL-TAG secretion than visceral fat.10,42 Subjects with high liver fat content have increased VLDL secretion and impaired insulin action; however, increased hepatic VLDL output is insufficient to normalize liver fat content in people with NAFLD. The secretion of VLDL-TAG increased proportionally with intrahepatic TAG content but reached a plateau when hepatic fat content exceeded 10%.42 The increase in VLDL-TAG is primarily due to increased contribution from nonsystemic fatty acids derived from de novo lipogenesis and lipolysis of intrahepatic and intra-abdominal fat; the contribution of fatty acids from nonsystemic sources was 60% in subjects with high intrahepatic fat compared with 35% in subjects with normal hepatic fat content.42 Genetic studies indicate an association of CD36 with the secretion of VLDL in humans.43 Our recent study showed that CD36 deficiency aggravates hepatic steatosis in ob/ob mice, suggesting that CD36 impacts hepatic lipid metabolism by regulating both fatty acid uptake and VLDL secretion.18
Role of Fatty Acid Oxidation in Hepatic Steatosis
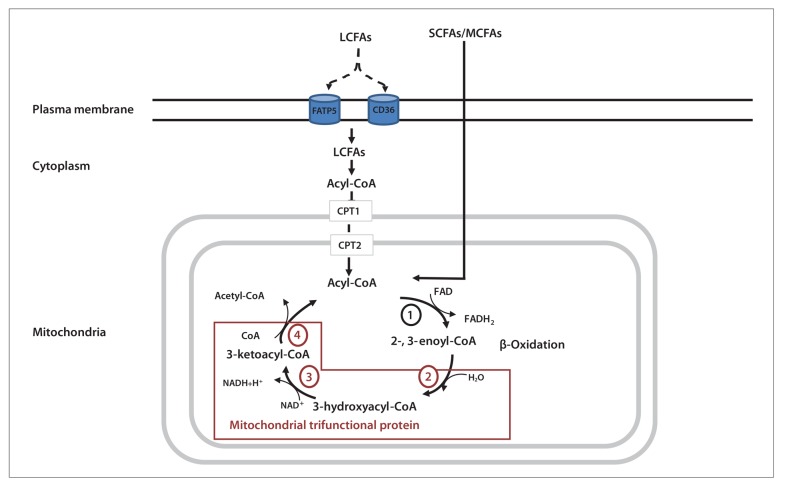
There is a unity of findings suggesting that mitochondrial dysfunction has a key role in the development of hepatic steatosis.44,45 The best-known pathway for fatty acid oxi dation and generation of energy in the form of adenosine triphosphate (ATP) takes place in the mitochondria (Figure 2). Short- and medium-chain fatty acids cross the plasma membrane passively while long-chain fatty acids are activated to acyl-CoA molecules by specific acyl-CoA synthases. Acyl-CoA enters the mitochondrial matrix via a carnitine palmitoyltransferase 1 (CPT1) and CPT2 shuttle mechanism. The β-oxidation of fatty acids consists of 4 enzymatic reactions (Figure 2). The first reaction is catalyzed by carbon length–specific acyl-CoA dehydro- genases. The last 3 reactions for long-chain fatty acids are catalyzed by the mitochondrial trifunctional protein (MTP), which consists of 3 enzymes: a long-chain enoyl- CoA hydratase catalyzing the second step, a long-chain L3-hydroxyacyl-CoA dehydrogenase catalyzing the third step, and a 3-ketoacyl-CoA thiolase catalyzing the fourth and final step. Acyl-CoAs enter the β-oxidation cycle to generate acetyl-CoA. Reduced nicotinamide adenine dinucleotide (NADH) and flavin adenine dinucleotide (FADH2), generated by both β-oxidation and the TCA cycle, deliver their electrons and protons to the mito- chondrial respiratory chain to generate NAD+, FAD, and ATP.46 The excess influx of fatty acids to the liver over loads the mitochondria, leading to the accumulation of incompletely oxidized substrates such as fatty acids and diacylglycerides with increased production of reactive oxygen species.47-49
Figure 2.
Mitochondrial fatty acid oxidation. Short- and medium-chain fatty acids (SCFAs/MCFAs) traverse the plasma membrane passively while long-chain fatty acids (LCFAs) require membrane transporters (fatty acid translocase [CD36] and fatty acid transport protein 5 [FATP5]). LCFAs are acylated in the cytosol and then enter the mitochondria, helped by the carnitine acyl-transferases (carnitine palmitoyltransferases) CPT1 and CPT2. The β-oxidation of acyl-coenzyme A (acyl-CoA) takes place in the mitochondria and consists of 4 reactions, with the last 3 catalyzed by the mitochondrial trifunctional protein. β-Oxidation spiral leads to the formation of acetyl-CoA, nicotinamide adenine dinucleotide (NADH), and flavin adenine dinucleotide (FADH2) from each oxidation cycle. NADH and FADH2 are used by the mitochondrial respiratory chain to generate adenosine triphosphate.
Studies from our group at the University of Missouri document a role for mitochondrial dysfunction in the development of steatosis. Mice heterozygous for MTP that were fed a low-fat chow diet developed insulin resistance and hepatic steatosis in parallel by 9 months of age.50 This primary defect in mitochondrial β-oxidation also causes hepatic insulin resistance, which is selective to impairments in hepatic glycogen metabolism and independent from factors that are known to cause hepatic insulin resistance, such as diacylglyceride and ceramide accumulation in the liver.51
Clinical Implications of Hepatic Steatosis and Steatohepatitis
Hepatic Steatosis, Steatohepatitis, Cirrhosis, and Liver-Related Mortality
NAFLD is a spectrum of liver disorders that encompasses the presence of simple hepatic steatosis and hepatic ste- atohepatitis with or without fibrosis.52 Hepatic steatosis is often considered a benign condition. The risk of development of cirrhosis in patients with simple fatty liver disease is 0.5% to 1%.53 However, once the initiation of necro- inflammation occurs, with ballooning hepatocyte degeneration and Mallory-Denk bodies in the absence of excess alcohol consumption (>20 g/d), the condition is known as NASH54 and the natural history of NAFLD changes, with increased risk of progression to fibrosis and cirrhosis.55 NASH is a stage within the spectrum of NAFLD, and steatosis remains a hallmark of the disease. Patients with NASH and cirrhosis may go on to develop consequences of portal hypertension such as ascites, variceal bleeding, and portosystemic encephalopathy. Follow-up of patients with NASH and fibrosis demonstrates that almost 20% of these individuals become cirrhotic within 5 to 10 years.55 In a population-based study of 420 patients diagnosed with NAFLD between 1980 and 2000 in Olmsted County, Minnesota, mortality among NAFLD patients was higher than in the general population, and liver-related death was a leading cause of mortality.56 In a more recent international collaborative study, 247 patients with NAFLD and advanced liver disease F3 (bridging fibrosis)/F4 (cirrhosis) followed for a mean of 85.6 months were compared with 264 patients with hepatitis C virus infection who had similar Child-Pugh classification at enrollment.57 Patients with NAFLD had lower rates of liver-related complications and hepatocellular carcinoma than patients with hepatitis C virus infection but similar overall mortality. These studies suggest that patients with NASH or NASH with fibrosis or cirrhosis are at risk of poor clinical outcomes.
Hepatic Steatosis and Malignancy
Hepatic steatosis is independently associated with increased systemic inflammation.58 NASH and metabolic syndrome are associated with decreased serum adiponectin, increased serum tumor necrosis factor a, and increased leptin, which predispose patients to alterations in cell growth, angiogenesis, and immune function. Of interest, NASH without significant fibrosis or cirrhosis is associated with hepatocellular carcinoma.59 Furthermore, hepatic steatosis is a significant risk factor for developing hepatocellular carcinoma independent of age, sex, obesity, fibrosis stage, and response to interferon therapy in patients with chronic hepatitis C virus.60 Approximately 14% of patients with NASH-induced cirrhosis go on to develop hepatocellular carcinoma.61 Patients who develop hepatocellular carcinoma in the background of metabolic syndrome are predominantly male, older than those who develop hepatocellular carcinoma secondary to other causes, and have well-differentiated tumors in early stages at diagnosis.62,63
Hepatic Steatosis, Hepatic Resection, and Liver Transplantation
Macrovesicular steatosis is an important criterion defining extended-criteria donor organs. Several studies have reported a poor impact of steatosis on postoperative morbidity and mortality after liver resection.64 A national analysis of the Scientific Registry of Transplant Recipients demonstrated that macrovesicular steatosis of greater than 30% was an independent predictor of reduced 1-year graft survival.65 Steatotic livers are particularly vulnerable to ischemia/reperfusion injury, resulting in an increased risk of postoperative morbidity and mortality after liver surgery, including liver transplantation.66 In a retrospective review of 450 living liver donors who underwent right hepatectomy, a mild degree of hepatic steatosis was associated with higher postoperative peak aspartate and alanine aminotransferase values.67 Furthermore, biliary complications remain a persistent problem in orthotopic liver transplantation. The presence of macrovesicular steatosis in 20% to 50% of a liver graft emerged as a newly defined risk factor for postoperative biliary complications in 175 adult patients undergoing living donor liver transplantation.68 Thus, hepatic steatosis poses a challenge after liver resection or transplantation.
Prevention of Hepatic Steatosis
A negative by-product of our modern civilization is little need for physical activity and an increased risk of chronic disease, such as heart disease, insulin resistance, type 2 diabetes, and NAFLD. Physical inactivity is one of the causes of these associated metabolic disorders and is an actual known leading cause of death in the United States.69-74
Given the fact that more than 95% of US adults do not get the recommended amount of physical activity per week, it is no surprise that NAFLD prevalence is also on the rise.75 Although recent studies have indicated the utility of vitamin E therapy, pioglitazone, or 6-ethylchenodeoxycholic acid (obeticholic acid) in treating select adult populations of NASH patients,76,77 the present gold-standard treatment strategy for NAFLD remains lifestyle modification to increase physical activity and reduce energy intake. Several recent reviews have focused on the beneficial effects of diet and exercise in the treatment of NAFLD.71,78-80 The general consensus statement by the American Association for the Study of Liver Diseases indicates that weight loss of 3% to 5% of body weight by diet alone or in combination with increased physical activity can effectively reduce hepatic steatosis; greater amounts of weight loss (up to 10%) by the same means may be needed to improve other components of NASH; exercise alone has thus far only been proven effective for lowering hepatic steatosis; and the direct effects of exercise training on the treatment of inflammation and fibrosis remain unknown.52 With this emphasis on diet and exercise as a treatment strategy, the next section of this article focuses on the use of lifestyle modifications as a preventive tactic for hepatic steatosis. We also explore the potential mechanistic differences between diet and exercise interventions in NAFLD prevention and whether the protective effects persist should the healthy lifestyle cease, focusing primarily on work conducted by our group.
Exercise, Diet, and Prevention of Hepatic Steatosis
Low levels of habitual physical activity and/or poor fitness are routinely linked to increased NAFLD prevalence.81-83 NAFLD patients are known to have lower amounts of daily physical activity than patients without fatty liver disease.84 Less physically active individuals also exhibit higher rates of hepatic FFA uptake compared with more active individuals, a factor known to significantly contribute to hepatic steatosis.34,85 In addition, a recent study in monozygotic twin pigs found that the more active pig in each pair had 18% greater maximal oxygen uptake and approximately 25% less hepatic fat content than the less active animal.86 Furthermore, a recent retrospective cross-sectional study suggests that meeting the recommendations for vigorous physical activity (>75 min/wk) is associated with a significant reduction in the odds of hepatic steatosis progressing to NASH and that exceeding the vigorous activity guidelines (>150 min/wk) is associated with decreased odds of having fibrosis.87 Interestingly, meeting or exceeding the recommendations for moderate intensity activity (>150 min/wk) was not associated with a reduced incidence of NASH or fibrosis. This retrospective analysis points to the potential clinical utility of vigorous, high-intensity exercise training in the management of NASH, but randomized clinical trials are necessary.
The Otsuka Long-Evans Tokushima fatty (OLETF) rat is a commonly studied animal model of obesity; this animal is selectively bred for null expression of the cholecystokinin-1 receptor. This animal therefore exhibits hyperphagia, which leads to the progressive development of obesity, insulin resistance, type 2 diabetes, and fatty liver.71,88 In fact, hepatic steatosis is present 4 to 5 weeks postweaning in sedentary, hyperphagic OLETF rats and progresses to marked micro- and macrovascular steatosis, hepatocyte ballooning, perivenular fibrosis, and a mild NASH phenotype by 40 weeks of age.88-90 These pathologic events appear to be related to hepatic mitochondrial dysfunction, which precedes hepatic steatosis development.88 In addition, other major pathways known to contribute to NAFLD are altered in this model, including upregulation in markers of hepatic de novo lipogenesis and fatty acid uptake and downregulation in markers of hepatic TAG export.71,88-90
A unique characteristic of the OLETF rat compared with other obese rodent models is an inherent ability to maintain daily physical activity levels using voluntary running wheels.91,92 When the rat is allowed to voluntarily exer cise, body weight is suppressed,93 whole body insulin sensitivity is enhanced, and the development of type 2 diabetes is prevented.88,94 In addition, daily exercise completely prevents the development of hepatic steatosis in this model despite the animal remaining hyperphagic.69,71,90 These protective effects are due in large part to the prevention of obesity, as well as to exercise-induced enhancement of hepatic mitochondrial metabolism and reductions in hepatic de novo lipogenesis and FATPs.69,89 Perhaps it is not surprising that when the hyperphagia and excess weight gain are prevented by dietary restrictions, hepatic steatosis is also completely prevented.71,95 This suggests that prevention of excess weight gain by diet or exercise has similar effectiveness in the prevention of hepatic steatosis in this model. This seems plausible in humans as well, given that only 10% to 15% of lean individuals have fatty liver disease compared with 75% to 100% of obese and morbidly obese individuals.96 However, despite similar hepatic phenotypes in exercised and dietarily restricted animals, exercise increases hepatic mitochondrial function and content, further suppresses hepatic de novo lipogenesis, and offers additional health benefits for glucose control compared with a restricted diet alone.71 Moreover, dietary restriction appears to upregulate the machinery for lipogenesis (SREBP-1c, mammalian target of rapamycin), which could have potential negative consequences should ad libitum feeding resume. This is important given the fact that greater than 25% of hepatic TAG accumulation can be accounted for by de novo lipogenesis,34 and the fact that subjects with high hepatic fat have higher lipogenesis compared with people with lower intrahepatic fat.30 Recent studies indicate that caloric restriction with reduced carbohydrates differentially alters insulin resistance and intrahepatic fat.97,98
Collectively, encouraging an adequate diet and appropriate physical activity will likely promote a healthy lifestyle and also prevent the development of hepatic steatosis. Furthermore, the type of lifestyle modifications that an individual chooses could impact the long-term sustainability of the initial improvements.
Intermittent Lifestyle Modifications and Hepatic Steatosis
Determining the residual benefits of previous lifestyle modifications is another important consideration in preventing hepatic steatosis, given the difficulty in sustaining healthy dietary and physical activity habits indefinitely. It is unclear how long a person is protected against hepatic steatosis development after he or she stops exercising or maintaining a dietary regimen. To our knowledge, studies of this nature have not been done in humans, but they are definitely warranted. To begin to address these questions and gain some mechanistic understanding of the process, our group examined this issue and found that physically active rodents were completely protected against hepatic steatosis development after 7 days of being transitioned to a sedentary condition.69 However, with longer-term inactivity of 4 weeks, significant hepatic TAG accumulation occurred, although levels still remained markedly lower than in chronically sedentary animals.89 These findings are in agreement with other work showing that it may take up to 6 weeks of inactivity to see increases in hepatic TAG in previously trained rats.99 On the other hand, the lasting protective effects of previous dietary restriction do not appear as promising as the effects of prior exercise. Despite a similar magnitude of protection against NAFLD with dietary restriction as with exercise, the beneficial effects of 12 weeks of dietary restriction in the OLETF rat do not appear to be as well maintained, with a greater magnitude of hepatic TAG accumulation occurring with a 4-week return of ad libitum feeding following dietary restriction (R. Scott Rector, unpublished observations).
These findings give us some insight into the potential residual benefits of prior exercise vs prior dietary restriction on hepatic steatosis development from both peripheral and hepatic-specific alterations. Despite being hyperphagic, the active animals were protected against weight gain, adiposity gain, and increases in serum insulin in the short-term inactivity window of 7 days.69 In addition, with the exception of serum insulin levels, which returned to sedentary levels, there was only a partial loss in the other factors with 4 weeks of inactivity, with weight and adiposity remaining largely suppressed compared with weight and adiposity in chronically sedentary animals.89 However, many of the exercise-induced increases in indices of hepatic mitochondrial function were rapidly lost with inactivity, including total mitochondrial palmitate oxidation and β-hydroxyacyl dehydrogenase and citrate synthase activity.93,100 On the other hand, there was a sustained reduction in markers of hepatic fatty acid uptake and lipogenesis (fatty acid synthase, stearoyl-CoA desaturase 1 [SCD-1], acetyl-CoA carboxylase, SREBP-1c, and CD36) following 4 weeks of physical inactivity.100 SREBP-1c is considered to be a primary transcription factor controlling lipogenesis, and because acetyl-CoA carboxylase and fatty acid synthase are the first 2 committed steps in de novo fatty acid synthesis, their continued suppression likely contributes to the residual benefits of physical activity in its suppression of hepatic TAG accumulation. Hepatic SCD-1 is known to contribute to the abnormal partitioning of fatty acids by increasing acetyl-CoA carboxylase activity and decreasing fatty acid oxidation, shunting substrates to fatty acid synthesis.101,102 Interestingly, activity-induced reductions in hepatic SCD-1 protein content were completely maintained following 4 weeks of physical inactivity and hyperphagia. These findings differ dramatically from those observed in previously dietarily restricted animals, where a 4-week return to ad libitum feeding resulted in a greater degree of weight gain and fat mass gain and in the return of hepatic acetyl-CoA carboxylase, fatty acid synthase, and SCD-1 to levels approaching those in the chronically sedentary, hyperphagic animals (R. Scott Rector, unpublished observations). Collectively, regardless of the preventive strategy, a relatively short-term transition to an unhealthy lifestyle causes hepatic steatosis development in the OLETF rat. Prior physical activity may offer more persistent protection, in part due to a continued suppression of de novo lipogenesis, but the consequences of the interaction between hyperphagia and a sedentary state appear to promote the development of, and likely the future progression of, hepatic steatosis. These data strongly suggest that sudden transition to a sedentary lifestyle and overnutrition increases susceptibility to hepatic steatosis.
Conclusion
The pathogenesis of hepatic steatosis involves multiple pathways, including fatty acid uptake, de novo lipogenesis, mitochondrial fatty acid oxidation, and lipoprotein secretion. Hepatic steatosis is often considered a benign condition; however, once the initiation of inflammation occurs, there is an increased risk of progression to fibrosis and cirrhosis. Lifestyle modifications and dietary interventions that optimize the function of these pathways would be beneficial in preventing hepatic steatosis and more advanced forms of NAFLD.
Footnotes
The authors have no relevant conflicts of interest to disclose. Dr Rector receives salary support from a Veterans Health Administration Career Development Award (VHA CDA-2 Award 1299-03).
References
- 1.Mehta SR, Thomas EL, Bell JD, Johnston DG, Taylor-Robinson SD. Non-invasive means of measuring hepatic fat content. World J Gastroenterol. 2008;14(22):3476–3483. doi: 10.3748/wjg.14.3476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qayyum A, Nystrom M, Noworolski SM, Chu P, Mohanty A, Merriman R. MRI steatosis grading: development and initial validation of a color mapping system. AJR Am J Roentgenol. 2012;198(3):582–588. doi: 10.2214/AJR.11.6729. [DOI] [PubMed] [Google Scholar]
- 3.Fartoux L, Chazouillères O, Wendum D, Poupon R, Serfaty L. Impact of steatosis on progression of fibrosis in patients with mild hepatitis C. Hepatology. 2005;41(1):82–87. doi: 10.1002/hep.20519. [DOI] [PubMed] [Google Scholar]
- 4.Tominaga K, Kurata JH, Chen YK, et al. Prevalence of fatty liver in Japanese children and relationship to obesity. An epidemiological ultrasonographic survey. Dig Dis Sci. 1995;40(9):2002–2009. doi: 10.1007/BF02208670. [DOI] [PubMed] [Google Scholar]
- 5.Brumbaugh DE, Friedman JE. Developmental origins of nonalcoholic fatty liver disease. Pediatr Res. 2014;75(1-2):140–147. doi: 10.1038/pr.2013.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sunny NE, Parks EJ, Browning JD, Burgess SC. Excessive hepatic mitochondrial TC cycle and gluconeogenesis in humans with nonalcoholic fatty liver disease. Cell Metab. 2011;14(6):804–810. doi: 10.1016/j.cmet.2011.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gastaldelli A, Cusi K, Pettiti M, et al. Relationship between hepatic/visceral fat and hepatic insulin resistance in nondiabetic and type 2 diabetic subjects. Gastroenterology. 2007;133(2):496–506. doi: 10.1053/j.gastro.2007.04.068. [DOI] [PubMed] [Google Scholar]
- 8.Fabbrini E, Tamboli RA, Magkos F, et al. Surgical removal of omental fat does not improve insulin sensitivity and cardiovascular risk factors in obese adults. Gastroenterology. 2010;139(2):448–455. doi: 10.1053/j.gastro.2010.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korenblat KM, Fabbrini E, Mohammed BS, Klein S. Liver, muscle, and adipose tissue insulin action is directly related to intrahepatic triglyceride content in obese subjects. Gastroenterology. 2008;134(5):1369–1375. doi: 10.1053/j.gastro.2008.01.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fabbrini E, Magkos F, Mohammed BS, et al. Intrahepatic fat, not visceral fat, is linked with metabolic complications of obesity. Proc Natl Acad Sci US. 2009;106(36):15430–15435. doi: 10.1073/pnas.0904944106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37(4):917–923. doi: 10.1053/jhep.2003.50161. [DOI] [PubMed] [Google Scholar]
- 12.Neuschwander-Tetri BA. Hepatic lipotoxicity and the pathogenesis of nonal-coholic steatohepatitis: the central role of nontriglyceride fatty acid metabolites. Hepatology. 2010;52(2):774–788. doi: 10.1002/hep.23719. [DOI] [PubMed] [Google Scholar]
- 13.Hooper AJ, Adams LA, Burnett JR. Genetic determinants of hepatic steatosis in man. J Lipid Res. 2011;52(4):593–617. doi: 10.1194/jlr.R008896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Falcon A, Doege H, Fluitt A, et al. FATP2 is a hepatic fatty acid transporter and peroxisomal very long-chain acyl-CoA synthetase. Am J Physiol Endocrinol Metab. 2010;299(3):E384–E393. doi: 10.1152/ajpendo.00226.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doege H, Baillie RA, Ortegon AM, et al. Targeted deletion of FATP5 reveals multiple functions in liver metabolism: alterations in hepatic lipid homeostasis. Gastroenterology. 2006;130(4):1245–1258. doi: 10.1053/j.gastro.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 16.Doege H, Grimm D, Falcon A, et al. Silencing of hepatic fatty acid transporter protein 5 in vivo reverses diet-induced non-alcoholic fatty liver disease and improves hyperglycemia. J Biol Chem. 2008;283(32):22186–22192. doi: 10.1074/jbc.M803510200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koonen DP, Jacobs RL, Febbraio M, et al. Increased hepatic CD6 expression contributes to dyslipidemia associated with diet-induced obesity. Diabetes. 2007;56(12):2863–2871. doi: 10.2337/db07-0907. [DOI] [PubMed] [Google Scholar]
- 18.Nassir F, Adewole OL, Brunt EM, Abumrad NA. CD36 deletion reduces VLDL secretion, modulates liver prostaglandins, and exacerbates hepatic steatosis in ob/ob mice. J Lipid Res. 2013;54(11):2988–2997. doi: 10.1194/jlr.M037812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bugianesi E, Gastaldelli A, Vanni E, et al. Insulin resistance in non-diabetic patients with non-alcoholic fatty liver disease: sites and mechanisms. Diabetologia. 2005;48(4):634–642. doi: 10.1007/s00125-005-1682-x. [DOI] [PubMed] [Google Scholar]
- 20.Musso G, Gambino R, Cassader M. Recent insights into hepatic lipid metabolism in non-alcoholic fatty liver disease (NAFLD) Prog Lipid Res. 2009;48(1):1–26. doi: 10.1016/j.plipres.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 21.Miquilena-Colina ME, Lima-Cabello E, Sánchez-Campos S, et al. Hepatic fatty acid translocase CD6 upregulation is associated with insulin resistance, hyperinsulinaemia and increased steatosis in non-alcoholic steatohepatitis and chronic hepatitis C. Gut. 2011;60(10):1394–1402. doi: 10.1136/gut.2010.222844. [DOI] [PubMed] [Google Scholar]
- 22.Kolak M, Yki-Järvinen H, Kannisto K, et al. Effects of chronic rosiglitazone therapy on gene expression in human adipose tissue in vivo in patients with type 2 diabetes. J Clin Endocrinol Metab. 2007;92(2):720–724. doi: 10.1210/jc.2006-1465. [DOI] [PubMed] [Google Scholar]
- 23.Tiikkainen M, Häkkinen AM, Korsheninnikova E, Nyman T, Mäkimattila S, Yki-Järvinen H. Effects of rosiglitazone and metformin on liver fat content, hepatic insulin resistance, insulin clearance, and gene expression in adipose tissue in patients with type 2 diabetes. Diabetes. 2004;53(8):2169–2176. doi: 10.2337/diabetes.53.8.2169. [DOI] [PubMed] [Google Scholar]
- 24.Belfort R, Harrison SA, Brown K, et al. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N Engl J Med. 2006;355(22):2297–2307. doi: 10.1056/NEJMoa060326. [DOI] [PubMed] [Google Scholar]
- 25.Martin GG, Danneberg H, Kumar LS, et al. Decreased liver fatty acid binding capacity and altered liver lipid distribution in mice lacking the liver fatty acid-binding protein gene. J Biol Chem. 2003;278(24):21429–21438. doi: 10.1074/jbc.M300287200. [DOI] [PubMed] [Google Scholar]
- 26.Wolfrum C, Buhlmann C, Rolf B, Börchers T, Spener F. Variation of liver-type fatty acid binding protein content in the human hepatoma cell line HepG2 by peroxisome proliferators and antisense RNA affects the rate of fatty acid uptake. Biochim Biophys Acta. 1999;1437(2):194–201. doi: 10.1016/s1388-1981(99)00008-6. [DOI] [PubMed] [Google Scholar]
- 27.Newberry EP, Xie Y, Kennedy SM, Luo J, Davidson NO. Protection against Western diet-induced obesity and hepatic steatosis in liver fatty acid-binding protein knockout mice. Hepatology. 2006;44(5):1191–1205. doi: 10.1002/hep.21369. [DOI] [PubMed] [Google Scholar]
- 28.Baumgardner JN, Shankar K, Hennings L, Badger TM, Ronis MJ. A new model for nonalcoholic steatohepatitis in the rat utilizing total enteral nutrition to overfeed a high-polyunsaturated fat diet. Am J Physiol Gastrointest Liver Physiol. 2008;294(1):G27–G38. doi: 10.1152/ajpgi.00296.2007. [DOI] [PubMed] [Google Scholar]
- 29.Ameer F, Scandiuzzi L, Hasnain S, Kalbacher H, Zaidi N. De novo lipogenesis in health and disease. Metabolism. 2014;63(7):895–902. doi: 10.1016/j.metabol.2014.04.003. [DOI] [PubMed] [Google Scholar]
- 30.Lambert JE, Ramos-Roman MA, Browning JD, Parks EJ. Increased de novo lipogenesis is a distinct characteristic of individuals with nonalcoholic fatty liver disease. Gastroenterology. 2014;146(3):726–735. doi: 10.1053/j.gastro.2013.11.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hudgins LC, Seidman CE, Diakun J, Hirsch J. Human fatty acid synthesis is reduced after the substitution of dietary starch for sugar. Am J Clin Nutr. 1998;67(4):631–639. doi: 10.1093/ajcn/67.4.631. [DOI] [PubMed] [Google Scholar]
- 32.Schwarz JM, Linfoot P, Dare D, Aghajanian K. Hepatic de novo lipogenesis in nor-moinsulinemic and hyperinsulinemic subjects consuming high-fat, low-carbohydrate and low-fat, high-carbohydrate isoenergetic diets. Am J Clin Nutr. 2003;77(1):43–50. doi: 10.1093/ajcn/77.1.43. [DOI] [PubMed] [Google Scholar]
- 33.Vedala A, Wang W, Neese RA, Christiansen MP, Hellerstein MK. Delayed secretory pathway contributions to VLDL-triglycerides from plasma NEFA, diet, and de novo lipogenesis in humans. J Lipid Res. 2006;47(11):2562–2574. doi: 10.1194/jlr.M600200-JLR200. [DOI] [PubMed] [Google Scholar]
- 34.Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest. 2005;115(5):1343–1351. doi: 10.1172/JCI23621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Diraison F, Moulin P, Beylot M. Contribution of hepatic de novo lipogenesis and reesterification of plasma non esterified fatty acids to plasma triglyceride synthesis during non-alcoholic fatty liver disease. Diabetes Metab. 2003;29(5):478–485. doi: 10.1016/s1262-3636(07)70061-7. [DOI] [PubMed] [Google Scholar]
- 36.Sundaram M, Yao Z. Recent progress in understanding protein and lipid factors affecting hepatic VLDL assembly and secretion. Nutr Metab (Lond). 2010;7(1):35. doi: 10.1186/1743-7075-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Welty FK. Hypobetalipoproteinemia and abetalipoproteinemia. Curr Opin Lipidol. 2014;25(3):161–168. doi: 10.1097/MOL.0000000000000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tarugi P, Lonardo A, Ballarini G, et al. Fatty liver in heterozygous hypobetali-poproteinemia caused by a novel truncated form of apolipoprotein B. Gastroenterology. 1996;111(4):1125–1133. doi: 10.1016/s0016-5085(96)70082-3. [DOI] [PubMed] [Google Scholar]
- 39.Schonfeld G. Familial hypobetalipoproteinemia: a review. J Lipid Res. 2003;44(5):878–883. doi: 10.1194/jlr.R300002-JLR200. [DOI] [PubMed] [Google Scholar]
- 40.Tep S, Mihaila R, Freeman A, et al. Rescue of Mtp siRNA-induced hepatic steatosis by DGAT2 siRNA silencing. J Lipid Res. 2012;53(5):859–867. doi: 10.1194/jlr.M021063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen Z, Newberry EP, Norris JY, et al. ApoB100 is required for increased VLDL-triglyceride secretion by microsomal triglyceride transfer protein in ob/ob mice. J Lipid Res. 2008;49(9):2013–2022. doi: 10.1194/jlr.M800240-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fabbrini E, Mohammed BS, Magkos F, Korenblat KM, Patterson BW, Klein S. Alterations in adipose tissue and hepatic lipid kinetics in obese men and women with nonalcoholic fatty liver disease. Gastroenterology. 2008;134(2):424–431. doi: 10.1053/j.gastro.2007.11.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Love-Gregory L, Sherva R, Schappe T, et al. Common CD36 SNPs reduce protein expression and may contribute to a protective atherogenic profile. Hum Mol Genet. 2011;20(1):193–201. doi: 10.1093/hmg/ddq449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nassir F, Ibdah JA. Role of mitochondria in nonalcoholic fatty liver disease. Int J Mol Sci. 2014;15(5):8713–8742. doi: 10.3390/ijms15058713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nassir F, Ibdah JA. Role of mitochondria in alcoholic liver disease. World J Gastroenterol. 2014;20(9):2136–2142. doi: 10.3748/wjg.v20.i9.2136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ibdah JA, Bennett MJ, Rinaldo P, et al. A fetal fatty-acid oxidation disorder as a cause of liver disease in pregnant women. N Engl J Med. 1999;340(22):1723–1731. doi: 10.1056/NEJM199906033402204. [DOI] [PubMed] [Google Scholar]
- 47.Cheng Z, Ristow M. Mitochondria and metabolic homeostasis. Antioxid Redox Signal. 2013;19(3):240–242. doi: 10.1089/ars.2013.5255. [DOI] [PubMed] [Google Scholar]
- 48.Koves TR, Ussher JR, Noland RC, et al. Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Cell Metab. 2008;7(1):45–56. doi: 10.1016/j.cmet.2007.10.013. [DOI] [PubMed] [Google Scholar]
- 49.Sookoian S, Rosselli MS, Gemma C, et al. Epigenetic regulation of insulin resistance in nonalcoholic fatty liver disease: impact of liver methylation of the peroxisome proliferator-activated receptor γ coactivator 1α promoter. Hepatology. 2010;52(6):1992–2000. doi: 10.1002/hep.23927. [DOI] [PubMed] [Google Scholar]
- 50.Ibdah JA, Perlegas P, Zhao Y, et al. Mice heterozygous for a defect in mitochondrial trifunctional protein develop hepatic steatosis and insulin resistance. Gastroenterology. 2005;128(5):1381–1390. doi: 10.1053/j.gastro.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 51.Rector RS, Morris EM, Ridenhour S, et al. Selective hepatic insulin resistance in a murine model heterozygous for a mitochondrial trifunctional protein defect. Hepatology. 2013;57(6):2213–2223. doi: 10.1002/hep.26285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55(6):2005–2023. doi: 10.1002/hep.25762. [DOI] [PubMed] [Google Scholar]
- 53.Adams LA, Angulo P. Recent concepts in non-alcoholic fatty liver disease. Diabet Med. 2005;22(9):1129–1133. doi: 10.1111/j.1464-5491.2005.01748.x. [DOI] [PubMed] [Google Scholar]
- 54.Neuschwander-Tetri BA, Caldwell SH. Nonalcoholic steatohepatitis: summary of an AASLD Single Topic Conference. Hepatology. 2003;37(5):1202–1219. doi: 10.1053/jhep.2003.50193. [DOI] [PubMed] [Google Scholar]
- 55.Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116(6):1413–1419. doi: 10.1016/s0016-5085(99)70506-8. [DOI] [PubMed] [Google Scholar]
- 56.Adams LA, Lymp JF, St Sauver J, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129(1):113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 57.Bhala N, Angulo P, van der Poorten D, et al. The natural history of non alcoholic fatty liver disease with advanced fibrosis or cirrhosis: an international collaborative study. Hepatology. 2011;54(4):1208–1216. doi: 10.1002/hep.24491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ndumele CE, Nasir K, Conceiçao RD, Carvalho JA, Blumenthal RS, Santos RD. Hepatic steatosis, obesity, and the metabolic syndrome are independently and additively associated with increased systemic inflammation. Arterioscler Thromb Vasc Biol. 2011;31(8):1927–1932. doi: 10.1161/ATVBAHA.111.228262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bullock RE, Zaitoun AM, Aithal GP, Ryder SD, Beckingham IJ, Lobo DN. Association of non-alcoholic steatohepatitis without significant fibrosis with hepatocellular carcinoma. J Hepatol. 2004;41(4):685–686. doi: 10.1016/j.jhep.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 60.Kurosaki M, Hosokawa T, Matsunaga K, et al. Hepatic steatosis in chronic hepatitis C is a significant risk factor for developing hepatocellular carcinoma independent of age, sex, obesity, fibrosis stage and response to interferon therapy. Hepatol Res. 2010;40(9):870–877. doi: 10.1111/j.1872-034X.2010.00692.x. [DOI] [PubMed] [Google Scholar]
- 61.Önnerhag K, Nilsson PM, Lindgren S. Increased risk of cirrhosis and hepatocellular cancer during long-term follow-up of patients with biopsy-proven NAFLD. Scand J Gastroenterol. 2014;49(9):1111–1118. doi: 10.3109/00365521.2014.934911. [DOI] [PubMed] [Google Scholar]
- 62.Duan XY, Qiao L, Fan JG. Clinical features of nonalcoholic fatty liver disease-associated hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2012;11(1):18–27. doi: 10.1016/s1499-3872(11)60120-3. [DOI] [PubMed] [Google Scholar]
- 63.Starley BQ, Calcagno CJ, Harrison SA. Nonalcoholic fatty liver disease and hepatocellular carcinoma: a weighty connection. Hepatology. 2010;51(5):1820–1832. doi: 10.1002/hep.23594. [DOI] [PubMed] [Google Scholar]
- 64.Gomez D, Malik HZ, Bonney GK, et al. Steatosis predicts postoperative morbidity following hepatic resection for colorectal metastasis. Br J Surg. 2007;94(11):1395–1402. doi: 10.1002/bjs.5820. [DOI] [PubMed] [Google Scholar]
- 65.Spitzer AL, Lao OB, Dick AA, et al. The biopsied donor liver: incorporating macrosteatosis into high-risk donor assessment. Liver Transpl. 2010;16(7):874–884. doi: 10.1002/lt.22085. [DOI] [PubMed] [Google Scholar]
- 66.Tashiro H, Kuroda S, Mikuriya Y, Ohdan H. Ischemia–reperfusion injury in patients with fatty liver and the clinical impact of steatotic liver on hepatic surgery. Surg Today. 2014;44(9):1611–1625. doi: 10.1007/s00595-013-0736-9. [DOI] [PubMed] [Google Scholar]
- 67.Shin YH, Ko JS, Kim GS, et al. Impact of hepatic macrovesicular and microve- sicular steatosis on the postoperative liver functions after right hepatectomy in living donors. Transplant Proc. 2012;44(2):512–515. doi: 10.1016/j.transproceed.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 68.Li HY, Wei YG, Li B, et al. Impact of graft steatosis on the post-transplantation biliary complications for living donor liver transplant recipients in China. Hepato- gastroenterology. 2012;59(116):1194–1197. doi: 10.5754/hge11134. [DOI] [PubMed] [Google Scholar]
- 69.Booth FW, Laye MJ, Lees SJ, Rector RS, Thyfault JP. Reduced physical activity and risk of chronic disease: the biology behind the consequences. Eur J Appl Physiol. 2008;102(4):381–390. doi: 10.1007/s00421-007-0606-5. [DOI] [PubMed] [Google Scholar]
- 70.Thyfault JP, Rector RS, Noland RC. Metabolic inflexibility in skeletal muscle: a prelude to the cardiometabolic syndrome? J Cardiometab Syndr. 2006;1(3):184–189. doi: 10.1111/j.1559-4564.2006.05629.x. [DOI] [PubMed] [Google Scholar]
- 71.Rector RS, Thyfault JP. Does physical inactivity cause nonalcoholic fatty liver disease? J Appl Physiol (1985). 2011;111(6):1828–1835. doi: 10.1152/japplphysiol.00384.2011. [DOI] [PubMed] [Google Scholar]
- 72.Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2(2):1143–1211. doi: 10.1002/cphy.c110025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 74.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207–2212. [PubMed] [Google Scholar]
- 75.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 76.Sanyal AJ, Chalasani N, Kowdley KV, et al. NASH CR. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010;362(18):1675–1685. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Neuschwander-Tetri BA, Loomba R, Sanyal AJ, et al. for the NAH Clinical Research Network. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial [published online November 7][2014] Lancet. doi:10.1016/ S0140-6736(14)61933-4. [DOI] [PMC free article] [PubMed]
- 78.Johnson NA, Keating SE, George J. Exercise and the liver: implications for therapy in fatty liver disorders. Semin Liver Dis. 2012;32(1):65–79. doi: 10.1055/s-0032-1306427. [DOI] [PubMed] [Google Scholar]
- 79.Ascensão A, Martins MJ, Santos-Alves E, et al. Modulation of hepatic redox status and mitochondrial metabolism by exercise: therapeutic strategy for liver diseases. Mitochondrion. 2013;13(6):862–870. doi: 10.1016/j.mito.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 80.Johnson NA, George J. Fitness versus fatness: moving beyond weight loss in nonalcoholic fatty liver disease. Hepatology. 2010;52(1):370–381. doi: 10.1002/hep.23711. [DOI] [PubMed] [Google Scholar]
- 81.Perseghin G, Lattuada G, De Cobelli F, et al. Habitual physical activity is associated with intrahepatic fat content in humans. Diabetes Care. 2007;30(3):683–688. doi: 10.2337/dc06-2032. [DOI] [PubMed] [Google Scholar]
- 82.Church TS, Kuk JL, Ross R, Priest EL, Biltoft E, Blair SN. Association of car-diorespiratory fitness, body mass index, and waist circumference to nonalcoholic fatty liver disease. Gastroenterology. 2006;130(7):2023–2030. doi: 10.1053/j.gastro.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 83.Hsieh SD, Yoshinaga H, Muto T, Sakurai Y. Regular physical activity and coronary risk factors in Japanese men. Circulation. 1998;97(7):661–665. doi: 10.1161/01.cir.97.7.661. [DOI] [PubMed] [Google Scholar]
- 84.Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, et al. Role of leisure-time physical activity in nonalcoholic fatty liver disease: a population-based study. Hepatology. 2008;48(6):1791–1798. doi: 10.1002/hep.22525. [DOI] [PubMed] [Google Scholar]
- 85.Hannukainen JC, Nuutila P, Borra R, et al. Increased physical activity decreases hepatic free fatty acid uptake: a study in human monozygotic twins. J Physiol. 2007;578(pt 1):347–358. doi: 10.1113/jphysiol.2006.121368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hannukainen JC, Borra R, Linderborg K, et al. Liver and pancreatic fat content and metabolism in healthy monozygotic twins with discordant physical activity. J Hepatol. 2011;54(3):545–552. doi: 10.1016/j.jhep.2010.07.029. [DOI] [PubMed] [Google Scholar]
- 87.Kistler KD, Brunt EM, Clark JM, Diehl AM, Sallis JF, Schwimmer JB. Physical activity recommendations, exercise intensity, and histological severity of nonalcoholic fatty liver disease. Am J Gastroenterol. 2011;106(3):460–468. doi: 10.1038/ajg.2010.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rector RS, Thyfault JP, Uptergrove GM, et al. Mitochondrial dysfunction precedes insulin resistance and hepatic steatosis and contributes to the natural history of nonalcoholic fatty liver disease in an obese rodent model. J Hepatol. 2010;52(5):727–736. doi: 10.1016/j.jhep.2009.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Linden MA, Fletcher JA, Morris EM, et al. Combining metformin and aerobic exercise training in the treatment of type 2 diabetes and NAFLD in OLETF rats. Am J Physiol Endocrinol Metab. 2014;306(3):E300–E310. doi: 10.1152/ajpendo.00427.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sheldon RD, Laughlin MH, Rector RS. Reduced hepatic eNOS phosphorylation is associated with NAFLD and type 2 diabetes progression and is prevented by daily exercise in hyperphagic OLETF rats. J Appl Physiol (1985). 2014;116(9):1156–1164. doi: 10.1152/japplphysiol.01275.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bi S, Scott KA, Hyun J, Ladenheim EE, Moran TH. Running wheel activity prevents hyperphagia and obesity in Otsuka Long-Evans Tokushima Fatty rats: role of hypothalamic signaling. Endocrinology. 2005;146(4):1676–1685. doi: 10.1210/en.2004-1441. [DOI] [PubMed] [Google Scholar]
- 92.Stern JS, Johnson PR. Spontaneous activity and adipose cellularity in the genetically obese Zucker rat (fafa) Metabolism. 1977;26(4):371–380. doi: 10.1016/0026-0495(77)90104-4. [DOI] [PubMed] [Google Scholar]
- 93.Rector RS, Thyfault JP, Morris RT, et al. Daily exercise increases hepatic fatty acid oxidation and prevents steatosis in Otsuka Long-Evans Tokushima Fatty rats. Am J Physiol Gastrointest Liver Physiol. 2008;294(3):G619–G626. doi: 10.1152/ajpgi.00428.2007. [DOI] [PubMed] [Google Scholar]
- 94.Rector RS, Uptergrove GM, Morris EM, et al. Daily exercise vs. caloric restriction for prevention of nonalcoholic fatty liver disease in the OLETF rat model. Am J Physiol Gastrointest Liver Physiol. 2011;300(5):G874–G883. doi: 10.1152/ajpgi.00510.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fletcher JA, Meers GM, Laughlin MH, Ibdah JA, Thyfault JP, Rector RS. Modulating fibroblast growth factor 21 in hyperphagic OLETF rats with daily exercise and caloric restriction. Appl Physiol Nutr Metab. 2012;37(6):1054–1062. doi: 10.1139/h2012-091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bellentani S, Marino M. Epidemiology and natural history of non-alcoholic fatty liver disease (NAFLD) Ann Hepatol. 2009;8(suppl 1):S4–S8. [PubMed] [Google Scholar]
- 97.Haufe S, Engeli S, Kast P, et al. Randomized comparison of reduced fat and reduced carbohydrate hypocaloric diets on intrahepatic fat in overweight and obese human subjects. Hepatology. 2011;53(5):1504–1514. doi: 10.1002/hep.24242. [DOI] [PubMed] [Google Scholar]
- 98.Kirk E, Reeds DN, Finck BN, Mayurranjan SM, Patterson BW, Klein S. Dietary fat and carbohydrates differentially alter insulin sensitivity during caloric restriction. Gastroenterology. 2009;136(5):1552–1560. doi: 10.1053/j.gastro.2009.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Yasari S, Paquette A, Charbonneau A, Gauthier MS, Savard R, Lavoie JM. Effects of ingesting a high-fat diet upon exercise-training cessation on fat accretion in the liver and adipose tissue of rats. Appl Physiol Nutr Metab. 2006;31(4):367–375. doi: 10.1139/h06-032. [DOI] [PubMed] [Google Scholar]
- 100.Linden MA, Meers GM, Ruebel ML, et al. Hepatic steatosis development with four weeks of physical inactivity in previously active, hyperphagic OLETF rats. Am J Physiol Regul Integr Comp Physiol. 2013;304(9):R763–R771. doi: 10.1152/ajpregu.00537.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hulver MW, Berggren JR, Carper MJ, et al. Elevated stearoyl-CoA desaturase-1 expression in skeletal muscle contributes to abnormal fatty acid partitioning in obese humans. Cell Metab. 2005;2(4):251–261. doi: 10.1016/j.cmet.2005.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dobrzyn P, Dobrzyn A, Miyazaki M, et al. Stearoyl-CoA desaturase 1 deficiency increases fatty acid oxidation by activating AMP-activated protein kinase in liver. Proc Natl Acad Sci US. 2004;101(17):6409–6414. doi: 10.1073/pnas.0401627101. [DOI] [PMC free article] [PubMed] [Google Scholar]