Abstract
Context: The use of social marketing to modify lifestyle choices could be helpful in reducing youth obesity. Some or all of the 8 domains of the National Social Marketing Centre’s social marketing benchmark criteria (SMBC) are often used but not always defined in intervention studies. Objective: The aim of this review is to assess the effectiveness of European school-based interventions to prevent obesity relative to the inclusion of SMBC domains in the intervention. Data Sources: The PubMed, Cochrane, and ERIC databases were used. Study Selection: Nonrandomized and randomized controlled trials conducted from 1990 to April 2014 in participants aged 5 to 17 years were included. Data Extraction: After the study selection, the 8 domains of the SMBC were assessed in each included study. Results: Thirty-eight publications were included in the systematic review. For the meta-analysis, randomized controlled trials (RCTs) reporting body mass index or prevalence of overweight and obesity were considered. Eighteen RCTs with a total of 8681 participants included at least 5 SMBC. The meta-analysis showed a small standardized mean difference in body mass index of −0.25 (95%CI, −0.45 to −0.04) and a prevalence of overweight and obesity odds ratio of 0.72 (95%CI, 0.5–0.97). Conclusion: Current evidence indicates that the inclusion of at least 5 SMBC domains in school-based interventions could benefit efforts to prevent obesity in young people.
PROSPERO registration number: CRD42014007297.
Keywords: adolescents, children, Europe, obesity, school-based interventions, social marketing
INTRODUCTION
The prevalence of obesity, a major international public health problem, has nearly doubled in the last 3 decades, especially among children and adolescents.1 Overweight and obese young people are at greater risk of developing health problems that can become chronic by adulthood, harming health and well-being.1–4 According to the Childhood Obesity Surveillance Initiative of the World Health Organization,5 overweight is the most common childhood disorder in the European region.1,5 Once obesity is established, it is difficult to treat, and the rapidly rising rates of cases each year has created an urgent need for successful strategies and policies to address and reverse trends in weight gain, sedentary lifestyle, and unhealthy nutritional and life habits, especially in youth.6–9
Motivating individuals to make healthy personal lifestyle choices is critical, although determining the best method to achieve this goal is a challenge.6,9,10 A social marketing strategy based on influencing voluntary behavior to improve personal welfare is one possible tool with which to reduce youth obesity.10–13 The term social marketing was expressly defined by Kotler and Zaltman14 in 1971, who described it as “a social influence technology involving the design, implementation and control of programs aimed at increasing the acceptability of a social idea or practice in one or more groups of target adopters.” This term formed the basis of a book by Kotler et al.,15 and was redefined by Andreasen16 in 1994 as “the application of commercial marketing technologies to the analysis, planning, execution and evaluation of programs designed to influence the voluntary behavior of target audiences in order to improve their personal welfare and that of their society.” In general, social marketing is a pragmatic framework for understanding how and why individuals make lifestyle choices that result in intended or unintended consequences and for devising desirable alternatives.6,11,12
To help strengthen the use of effective social marketing strategies, the social marketing benchmark criteria (SMBC) were developed by the National Social Marketing Centre in the United Kingdom.17 The SMBC include the following 8 domains: customer or participant orientation, behavior, theory, insight, exchange, competition, segmentation, and a methods mix. The purpose of these domains is to support a better understanding of social marketing by defining their concepts and principles.17 The SMBC are not a description of a social marketing process but rather contribute to explaining the key domains that can increase the impact of a social marketing intervention.17
Many school-based interventions do not consciously use the SMBC, although some or all of the domains are present in the intervention designs.18 As far as can be determined, Gracia-Marco et al.18,19 are the only researchers who have reviewed the use of SMBC in the prevention of childhood obesity in community-based interventions. Their conclusion was that conscientiously applied SMBC could be useful in changing behaviors and improving health outcomes, but further research was needed.
Thus, it is important to review the effectiveness of social marketing as a methodology for school-based interventions aimed at reducing youth obesity, because the establishment of healthy habits by changing behaviors in school-aged children is a great challenge for health professionals.8,9,20 School environments provide a strong, ideal setting for implementing a range of different school-based activities to improve dietary behaviors and increase physical activity to promote healthy lifestyles. The school setting represents an important channel for facilitating behavioral change because of the broad access to large, similar, nonselected populations; moreover, beneficially altered behaviors of children and adolescents can persist into adulthood.8,21–23
Social marketing could represent a methodological challenge in determining whether greater SMBC inclusion improves the effectiveness of school-based interventions to reduce obesity. Thus, the hypothesis here is that, if school-based interventions include more of the SMBC domains, they will be more effective in preventing youth obesity. The aim of this review is to assess the effectiveness of European school-based interventions to prevent obesity relative to the inclusion of SMBC domains in the intervention.
This review has the PROSPERO registration number CRD42014007297.
METHODS
Search strategy
Electronic searches.
Three electronic databases were searched: PubMed, Cochrane Central Register of Controlled Trials, and ERIC. The search strategy was designed to be inclusive and based on the following:
PICOS elements (Table 1): population (“children” OR “adolescents”); intervention (“school-based intervention” OR “dietary school intervention” OR “physical activity school intervention” OR “school intervention” OR “school obesity prevention program”); comparison group (control groups without an intervention); outcomes (dietary, physical activity, and anthropometric measures [e.g., body mass index, or BMI] and prevalence of overweight and obesity at baseline and at the end of the intervention); and setting (“school”).
Table 1.
PICOS criteria used to define the research question for the systematic review
| Criteria | Description |
|---|---|
| Population | Children and/or adolescents |
| Intervention | School-based intervention; dietary school intervention; physical activity school intervention; school intervention; and/or school obesity prevention programs |
| Comparison group | Control groups without an intervention |
| Outcomes | Dietary, physical activity, and anthropometric (e.g., body mass index) measures; prevalence of overweight and obesity at baseline and at the end of the intervention |
| Setting | School-based interventions performed in Europe |
Studies conducted in Europe: The name of each European country was used in conjunction with the PICOS combinations of words in each search.
Social marketing interventions: Social marketing intervention studies in European countries were searched in the same electronic databases as those described above, using searches for “social marketing” AND “obesity” AND “country name.”
Studies not revealed in the original search: Additional eligible studies were identified from the references of selected articles or published reviews.
Selection criteria
Inclusion criteria.
The following types of interventions were eligible for inclusion: school-based interventions; school-based dietary interventions; school-based physical activity interventions that used approaches to increase physical activity, improve dietary behaviors, modify poor exercise or dietary behaviors, or a combination of these, aimed primarily at reducing or preventing obesity; interventions with a duration of at least 12 weeks, with no limit set for a maximum duration; studies that were published in the English language; and studies that were implemented in any European country from January 1990 to April 2014 (to focus on interventions conducted under contemporary epidemiological and environmental circumstances of childhood and adolescent obesity). Only studies that involved intervention and control groups were included.
Nonrandomized and/or randomized controlled trials (RCTs) that focused on the primary prevention of youth obesity were eligible for inclusion. Further inclusion criteria were as follows: children or adolescents who were normal weight, overweight, or obese, male or female, and aged 5 to 17 years at the start of the intervention (range represents average age range for school-aged students in Europe).
For inclusion in the systematic review, studies had to assess the following outcome measures: dietary behaviors or physical activity or both, at baseline and at the end of the intervention. Several studies have associated a change in specific behaviors (fruit and vegetable consumption, water consumption, physical activity, and sedentary activity levels) with weight-related measurements. As a result, the use of BMI and prevalence of overweight and obesity to assess the impact of changes on behavioral outcomes was considered appropriate.24–27 Randomized controlled trials in which the standardized mean difference (SMD) of BMI was reported or could be calculated and RCTs in which the odds ratio (OR) for the prevalence of overweight and obesity was included or could be calculated were included in the meta-analysis.
All of the interventions included in this review were analyzed in light of the characteristics and concepts of the SMBC, described in Table 2.
Table 2.
Characteristics and concepts of social marketing benchmark criteria, according to the National Social Marketing Centre (NSMC)
| Social marketing benchmark criterion | Characteristics of the criterion as defined by NSMC17 | Considerations when including this criterion in a health intervention10–13,18–20 |
|---|---|---|
| Customer orientation | Focuses on the audience. Fully understands the lives and behaviors of an audience, along with the issues important to that audience, using a mixture of data sources and research methods | Involves the target participants, their local community, and their environment. Considers the premise that all program planning decisions must emanate from a consideration of specific participant needs |
| Behavior | Aims to change people’s behavior | Clear, specific, measurable, and time-bound behavioral goals should be set, with baselines and key indicators established |
| Theory | Uses behavioral theories to understand behavior and inform the intervention | Used to inform both the understanding of the problem and the design of the program. Selecting and using behavioral theory for designing and applying an intervention involves assessing the underlying factors that could possibly influence behavior in a given situation |
| Insight | Identifies, using customer research on “actionable insights,” pieces of understanding that will lead to intervention development | Refers to a deep understanding of what moves and motivates the participants, including who and what influences the targeted behavior |
| Exchange | Considers benefits and costs of adopting and maintaining a new behavior; maximizes the benefits and minimizes the costs to create an attractive offer | Considers perceived/actual costs vs perceived/actual benefits. The perceived cost (which can be social, economic, physical) does not compensate for the perceived gain. The idea is that everyone in the intervention, including intermediaries and participants, should receive valued benefits in return for their efforts |
| Competition | Seeks to understand what competes for the audience’s time, attention, and inclination to behave in a particular way | Refers to the behavioral options that compete with public health recommendations and services. Identifies which products, behaviors, or services compete with those that the intervention is promoting, as well as how the benefits compare with those offered by competing behaviors. These behavioral options represent the difficulties and limitations that can be presented by the participants and/or the intermediaries |
| Segmentation | Avoids a “one size fits all” approach: identifies audience “segments,” which have common characteristics, and then tailors interventions appropriately | Does not only rely on traditional demographic, geographic, or epidemiological targeting. Draws on behavioral and psychographic data. Used to identify relatively homogeneous subgroups and to develop strategies designed specifically for each group of participants who share needs, wants, lifestyles, behaviors, and values and thus are likely to respond similarly to public health interventions |
| Methods mix | Uses a mixture of methods to create behavioral change. Does not rely solely on raising awareness | Uses all elements of the marketing mix (product, price, place, and promotion) and/or primary intervention methods (inform, educate, support, design, and control) |
Exclusion criteria.
The absence of one or more inclusion criteria was the principal exclusion criterion. Studies that involved 100 or fewer participants or included only overweight or obese children younger than 5 years or older than 17 years, as well as trials that evaluated only one gender, were excluded. Publications that reported preliminary or pilot results, protocols, follow-ups (considering data after the end of the intervention), or data from the intervention and control group children that were not extracted separately were also excluded. Gray literature, correspondence letters, governmental statistics overviews, book chapters, dissertations, and conference abstracts were excluded from this systematic review.
Data collection and analysis
Selection of studies.
First, the titles of all the studies identified by the electronic databases were screened. The abstracts of the studies with relevant titles were reviewed to select relevant studies on the basis of the inclusion criteria. If information in the title or abstract was insufficient, the full text was read to determine whether the inclusion criteria were met. The references of the identified studies were reviewed, and useful studies were selected. This selection process was performed by two reviewers (M.A.-M. and E.L.). In cases of disagreement, a third reviewer (L.T.) was consulted.
Data extraction and management.
Data extraction of every included study was performed by one reviewer (M.A.-M.). Adapted data extraction sheets were used, and particular items were identified, such as the following: name of the article; name of the intervention; authors; year of publication; year of intervention; city; country; study design; objective of the study; number of participant schools; age of participants; gender of participants; number of participants in the intervention group; number of participants in the control group; type of intervention; involvement (parents, family, teachers, community, specialists); socioeconomic considerations; duration of the intervention; measurement tools; outcomes of the study (any dietary and/or physical activity outcomes) at baseline and at the end of the intervention; technological approaches used in the implementation of the intervention; overweight or obesity measures, such as BMI or prevalence of overweight and obesity at baseline and at the end of the intervention; and the 8 SMBC domains (participant orientation, behavior, theory, insight, exchange, competition, segmentation, methods mix), described in Table 2.
The selection of the studies was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
Quality appraisal and risk of bias.
The quality assessment of the included school-based health-promotion studies was performed, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions,28 using the standardized framework of the Quality Assessment Tool for Quantitative Studies, developed by the Effective Public Health Practice Project.29 This tool yields an overall methodological rating of strong, moderate, or weak evidence in support of interventions; it can be applied to school-based interventions and consists of 8 categories: selection bias; study design; confounders; blinding; data collection methods; withdrawals and dropouts; intervention integrity; and analysis. For each category, the scores were summed according to the guidelines of the quality assessment tool, producing a global rating.29 Thus, for every intervention, each of the 8 categories was evaluated. Then, the quality of each included study was classified according to a 3-grade scale as follows: strong (4 or more strong category ratings and no weak ratings), moderate (1–3 strong category ratings and 1 weak rating), or weak (2 or more weak category ratings),28 as described in Table 3 and Table S1 in the Supporting Information online.
Table 3.
Studies analyzed for their use of the National Social Marketing Centre’s social marketing benchmark criteria (SMBC)
| Reference(s) | Intervention | Total SMBC | Social marketing benchmark criterion |
Results of quality appraisal | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Participant orientation | Behavior | Theory | Insight | Exchange | Competition | Segmentation | Methods mix | ||||
| Haerens et al. (2006),30,31 Haerens et al. (2007)32,33 | Physical activity and healthy food | 7 | ✓ | ✓ | ✓ | – | ✓ | ✓ | ✓ | Education | Moderate30; Moderate31; Strong32; Moderate33 |
| Sigmund et al. (2012)34 | Healthy Schools project | 5 | ✓ | ✓ | – | – | – | ✓ | ✓ | Education | Weak |
| Klakk et al. (2013)35 | CHAMPS study DK | 6 | ✓ | ✓ | – | – | ✓ | ✓ | ✓ | Support | Moderate |
| Simon et al. (2008)36 | ICAPS | 5 | ✓ | ✓ | – | – | ✓ | – | ✓ | Education | Strong |
| Thivel et al. (2011)37 | Physical activity program | 5 | ✓ | ✓ | – | – | – | ✓ | ✓ | Support | Weak |
| Graf et al. (2005)38 | CHILT | 4 | ✓ | ✓ | – | – | – | – | ✓ | Education | Weak |
| Muckelbauer et al. (2009)39 | Promotion of drinking water in schools | 8 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Education | Strong |
| Brandstetter et al. (2012)40 | URMEL-ICE | 7 | ✓ | ✓ | ✓ | – | ✓ | ✓ | ✓ | Education | Moderate |
| Siegrist et al. (2013)41 | JuvenTUM project | 5 | ✓ | ✓ | – | – | – | ✓ | ✓ | Education | Moderate |
| Angelopoulos et al. (2009)42 | CHILDREN study | 6 | ✓ | ✓ | ✓ | – | – | ✓ | ✓ | Education | Strong |
| Mihas et al. (2010)43 | VYRONAS | 6 | ✓ | ✓ | ✓ | – | – | ✓ | ✓ | Education | Weak |
| Kristjansdottir et al. (2010),44 Magnusson et al. (2011),45 Magnusson et al. (2012)46 | Lifestyle of 7- to 9-year-old children | 6 | ✓ | ✓ | ✓ | – | – | ✓ | ✓ | Education | Moderate44; Strong45; Moderate 46 |
| Centis et al. (2012)47 | Centro Salute G. C. Croce project | 5 | ✓ | ✓ | – | – | – | ✓ | ✓ | Education | Weak |
| Sacchetti et al. (2013)48 | School-based intervention of PE | 5 | ✓ | ✓ | – | – | – | ✓ | ✓ | Education | Moderate |
| Singh et al. (2007),49 Singh et al. (2009)50 | DOiT | 6 | ✓ | ✓ | – | – | ✓ | ✓ | ✓ | Education | Moderate49; Moderate50 |
| Martens et al. (2008)51 | Krachtvoer program | 6 | ✓ | ✓ | – | ✓ | – | ✓ | ✓ | Education | Moderate |
| Jurg et al. (2006)52 | JUMP-in | 6 | ✓ | ✓ | ✓ | – | – | ✓ | ✓ | Education | Weak |
| Jansen et al. (2011)53 | Lekker Fit! | 6 | ✓ | ✓ | ✓ | – | – | ✓ | ✓ | Support | Moderate |
| Ezendam et al. (2012)54 | FATaintPHAT | 6 | ✓ | ✓ | ✓ | – | – | ✓ | ✓ | Education | Moderate |
| Grydeland et al. (2013)55 | HEIA study | 6 | ✓ | ✓ | – | – | ✓ | ✓ | ✓ | Education | Moderate |
| Rosário et al. (2013)56 | Intervention through teachers | 6 | ✓ | ✓ | ✓ | – | – | ✓ | ✓ | Education | Strong |
| Llargues et al. (2011)57 | AVall study | 5 | ✓ | ✓ | – | – | – | ✓ | ✓ | Education | Strong |
| Tarro et al. (2014)58 | EdAl study | 7 | ✓ | ✓ | – | ✓ | ✓ | ✓ | ✓ | Education | Moderate |
| Sollerhed et al. (2008)59 | Expanded PE in primary school | 6 | ✓ | ✓ | – | – | ✓ | ✓ | ✓ | Support | Weak |
| Marcus et al. (2009)60 | STOPP | 7 | ✓ | ✓ | ✓ | – | ✓ | ✓ | ✓ | Education | Moderate |
| Kriemler et al. (2010)61 | KISS program | 7 | ✓ | ✓ | ✓ | – | ✓ | ✓ | ✓ | Support | Strong |
| Lakshman et al. (2010)62 | Top Grub card game | 7 | ✓ | ✓ | ✓ | – | ✓ | ✓ | ✓ | Education | Moderate |
| James et al. (2004)63 | CHOPPS | 5 | ✓ | ✓ | – | – | – | ✓ | ✓ | Education | Moderate |
| Breslin et al. (2012)64 | Sport for LIFE | 7 | ✓ | ✓ | ✓ | ✓ | – | ✓ | ✓ | Education | Strong |
| Sahota et al. (2001)65 | APPLES | 5 | ✓ | ✓ | – | – | – | ✓ | ✓ | Education | Weak |
| De Bourdeaudhuij et al. (2010)66 | HELENA study | 6 | ✓ | ✓ | ✓ | – | – | ✓ | ✓ | Education | Weak |
| Te Velde et al. (2008)67 | Pro Children Project | 7 | ✓ | ✓ | ✓ | – | ✓ | ✓ | ✓ | Education | Strong |
Abbreviation and symbols: PE, physical education; ✓, indicates presence of the criterion; –, indicates absence of the criterion.
Relation between number of SMBC used and study quality appraisal rating.
First, to obtain an initial sense of the importance of including SMBC domains in the design and implementation of an intervention, the average quality appraisal rating (weak = 1, moderate = 2, strong = 3) was calculated on the basis of the Quality Assessment Tool for Quantitative Studies29 and plotted according to the number of SMBC criteria used in each study.
Data processing for the meta-analysis.
Once studies that satisfied the inclusion criteria for a systematic review were selected, only the body weight–related measurements could be studied statistically, owing to high heterogeneity in the measures of behavioral outcomes. Therefore, the RCTs that reported BMI and/or prevalence of overweight and obesity at baseline and at the end of the intervention were included in the meta-analysis. A study was included in both analyses when it reported both of the aforementioned outcomes. For each such meta-analysis subgroup, homogeneity within each outcome was necessary. For each outcome, the effect size was calculated as shown below.
Body mass index.
The effect size considered for this outcome was the SMD of BMI. The included studies were those in which the SMD and its standard deviation (SD) or 95%CI were reported or could be calculated from the available data as the double difference effect size. First, the BMI mean difference (MD) within each group’s baseline and final data was calculated. Then, the pooled standard deviation (sdp) (Equation A) of each group’s baseline and final data was calculated.
| (A) |
n: number of participants
Finally, the SMD (Equation B) was obtained using both the MD of BMI (intervention and control) plus the final sdp of the two previously calculated sdp values.
| (B) |
To determine heterogeneity, I2 was calculated using the free statistical software R (https://www.r-project.org). Because I2 yielded a percentage greater than 85% (implying notable heterogeneity), the use of a random-effects model for this analysis was suggested.
Prevalence of overweight and obesity.
The effect size considered for this outcome was the OR of the number of cases of overweight and obesity at the end of the intervention. For the outcome of prevalence of overweight and obesity, the included studies were those in which the OR was reported or could be calculated from the available data using the classical OR approach. First, the final prevalence of overweight and obesity data with respect to the number of participants was collected for both the intervention and control groups. Afterward, the OR was calculated using Equation C,
| (C) |
where a is the final number of overweight or obese participants in the intervention group; b is the final number of nonoverweight or nonobese participants in the intervention group; c is the final number of overweight or obese participants in the control group; and d is the final number of nonoverweight or nonobese participants in the control group.
To determine heterogeneity, I2 was calculated using the free statistical software R. Because I2 yielded a percentage greater than 50% (implying heterogeneity), the use of a random-effects model for this analysis was also suggested.
The meta-analysis was synthesized for each outcome in two separate forest plots that show the specific effect size that each study has in favor of or against the intervention. Within each plot, the studies were subdivided according to the number of SMBC employed. Thus, it is possible to perform an analysis of the relationship between the effect size (dependent variable) and the SMBC (covariate).
Results from comparable studies were pooled in the statistical analysis using the Review Manager software (RevMan 5.3) from the Cochrane Collaboration.
Presence of SMBC domains vs absence of SMBC domains.
After the systematic review and meta-analysis, 4 SMBC domains (participant orientation, behavior, segmentation, and methods mix) were found to be present in all the included interventions. The remaining 4 SMBC domains (theory, insight, exchange, competition), which were variably present in the interventions, were analyzed on the basis of BMI or prevalence of overweight and obesity to determine whether the presence or absence of one of these SMBC domains affects the effectiveness of the intervention.
An additional meta-analysis was performed using each of the remaining 4 SMBC domains (theory, insight, exchange, and competition) as a principal variable (presence or absence) in relation to BMI and prevalence of overweight and obesity between interventions.
RESULTS OF THE SYSTEMATIC REVIEW
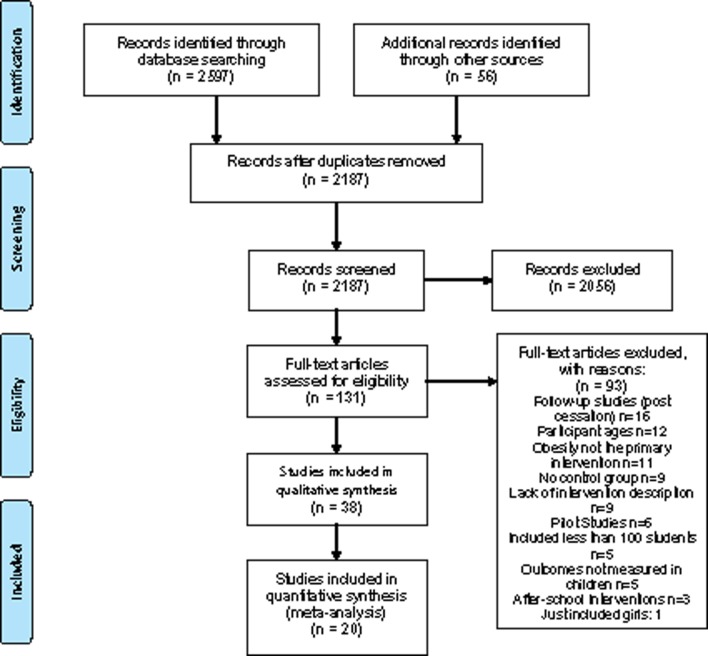
The systematic search identified 2187 references, of which 131 articles were included in the full-text review. After full-text review, 32 interventions (presented in 38 publications30–67) were found to meet the inclusion criteria and were included in the quality appraisal and qualitative analysis (Figure 1).
Figure 1.
PRISMA flow diagram used for the selection of studies.
The most relevant characteristics of the data extracted from the included studies are presented in Table S1 in the Supporting Information online. Of the 32 interventions implemented in European schools to promote healthy habits for obesity prevention, 27 were RCTs (32 040 participants) and 5 were nonrandomized (3018 participants), together including a total of 35 058 participants at baseline.
Results of the quality appraisal29 of the 38 publications were as follows: 9 received a weak quality global rating, 19 a moderate quality global rating, and 10 a strong quality global rating (Table 3 and Table S1 in the Supporting Information online).
Five of the 38 publications reported dietary-only interventions,39,51,62,63,67 11 reported physical activity–only interventions,35–38,41,48,52,55,59,61,66 and 22 described combined (dietary and physical activity) interventions.30–34,40,42–47,49,50,53,54,56–58,60,64,65
Twenty-nine studies used a health education method (classes or lessons)30–33,36,38–47,49–52,54,56–58,62–67; in 22 studies, the daily physical activity of the participants was increased as an intervention30–34,37,38,40,41,43–48,52,53,55,60,61,64,65; in 6 studies, the number of physical education lessons was increased as an intervention35,37,42,53,59,61; and in 7 studies, the availability of fruits, vegetables, or both was increased in the school setting.30–33,39,51,67 It should be noted that some of the interventions used more than one of these methods to deliver the intervention.
Regarding delivery of the intervention, 8 studies used a technological approach (computer or Internet-based) in the school setting,30–33,54,55,66,67 11 implemented an environmental change in the school to induce healthy habits,30–33,36,41,42,52,57,60,65 and the remaining 19 did not report the use of any delivery tool. No intervention used more than one method to deliver the intervention.
In 4 of the studies, the school teachers were not involved in the implementation of the interventions37,47,58,66; in 15 publications, parental support was considered or reported.36,38,39,44–46,48–50,54,59,62–64,66
Only one62 of the 38 publications mentioned the use of a social marketing approach for the design and implementation of the intervention. The rest of the studies did not specifically mention the SMBC; nevertheless, it was possible to identify these criteria according to Table 2 and as shown in Table 3.
One of the 38 publications reported 4 SMBC,38 9 publications reported 5 SMBC,34,36,37,41,47,48,57,63,65 16 publications reported 6 SMBC,35,42,43–46,50–56,59,66 11 publications reported 7 SMBC,30–33,40,58,60–62,64,67 and only 1 reported all 8 SMBC.39 All the publications reported the use of the 4 following SMBC: participant orientation, behavior, segmentation, and methods mix. Regarding the other 4 SMBC, 21 of the 38 publications reported the inclusion of the theory domain,30–33,39,40,42–46,52–54,56,60–62,64,66,67 4 publications mentioned the insight domain,39,51,58,64 17 publications reported the exchange domain,30–33,35,36,39,40,49,50,55,59–63,67 and 36 publications reported the competition domain.30–35,37,39–67
The relation between the number of SMBC and the quality appraisal rating of the included studies is shown in Figure 2: the greater the number of SMBC domains included, the more likely it is that a study has a strong quality appraisal rating as determined with the Effective Public Health Practice Project’s quality assessment tool.29
Figure 2.
Bar graph showing the relation between the number of social marketing benchmark criteria (SMBC) included in studies and the quality appraisal rating of the studies. Quality appraisal was performed using the Quality Assessment Tool for Quantitative Studies, developed by the Effective Public Health Practice Project29.
RESULTS OF THE META-ANALYSIS
After the systematic review and the SMBC assessment of the 38 included publications were conducted, RCTs that reported BMI and/or prevalence of overweight and obesity were selected for the meta-analysis.
In the analysis of BMI effect size, 2 interventions (Klakk et al.35 and Breslin et al.64) were excluded because they were not randomized, and 3 others (Brandstetter et al.,40 Sollerhed and Ejlertsson,59 and Sahota et al.65) were excluded because data were missing or mean or SD values were equal to zero. In the assessment of the effect size of prevalence of overweight and obesity, 2 publications (Sigmund et al.34 and Klakk et al.35) that had been selected were excluded due to lack of randomization. Thus, only 18 RCTs presented in 18 publications reported BMI and/or prevalence of overweight and obesity. Ten of these 18 RCTs reported both outcomes and consequently were considered in both meta-analyses (BMI and prevalence of overweight and obesity). A total of 20 publications were included in meta-analysis, 18 of which reported BMI (kg/m2) at baseline and at the end of the intervention and 12 of which reported prevalence of overweight and obesity (number of overweight/obese and nonoverweight/nonobese participants).
Presence of SMBC vs absence of SMBC
The systematic review and meta-analysis showed that 4 SMBC – participant orientation, behavior, segmentation, and methods mix – were present in at least all the included interventions. The remaining 4 SMBC domains (theory, insight, exchange, and competition) were analyzed to determine whether their presence or absence affects the effectiveness of the intervention. This additional analysis was performed using these 4 SMBC as variables in relation to BMI and prevalence of overweight and obesity between interventions. As a result, a meta-analysis was performed using each of these criteria as the principal variable (presence vs absence).
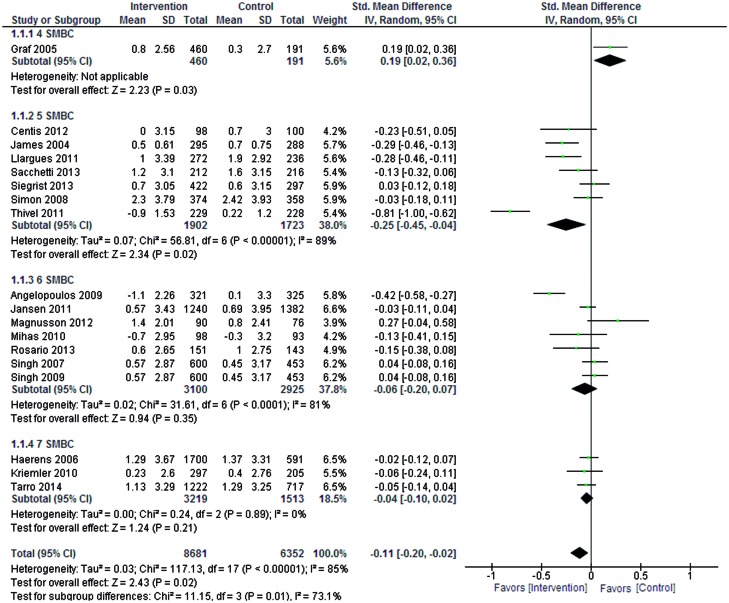
Body mass index
Eighteen RCTs with 8681 participants in total were included in the BMI meta-analysis. Figure 3 shows the forest plot resulting from the analysis of the 18 RCTs. The BMI SMD was categorized as negative (>0), minimal (> −0.2), small (−0.2 to −0.5), medium (−0.5 to −0.8), or large (< −0.8).68,69 The BMI SMD estimator showed that the interventions were, overall, minimally effective in reducing BMI in the intervention groups compared with the control groups (BMI SMD, −0.11; 95%CI, −0.20 to −0.02).
Figure 3.
Forest plot of randomized controlled trials that reported (1) body mass index as well as the standard mean difference (SMD) and its standard deviation (SD) or 95%CI; or (2) body mass index data from which the SMD and SD or 95%CI could be calculated. Abbreviation: SMBC, social marketing benchmark criteria.
When the BMI SMD in the intervention studies was analyzed according to the number of SMBC reported, a negative effectiveness was reported in the study that utilized only 4 SMBC (BMI SMD, 0.19; 95%CI, 0.02–0.36)38.
Moreover, intervention studies that implemented 5 SMBC reported a small effect size (BMI SMD, −0.25; 95%CI, −0.45 to −0.04). Studies that utilized 6 or 7 SMBC reported a minimal effect size (BMI SMD, −0.06, 95%CI, −0.20 to −0.07 and BMI SMD, −0.04; 95%CI, −0.10 to −0.02). In summary, the use of 5 SMBC is more likely to increase the effectiveness of interventions to reduce BMI.
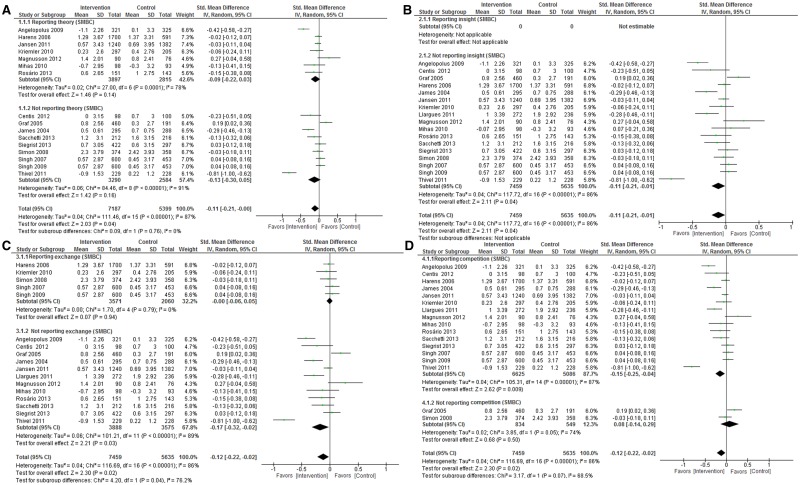
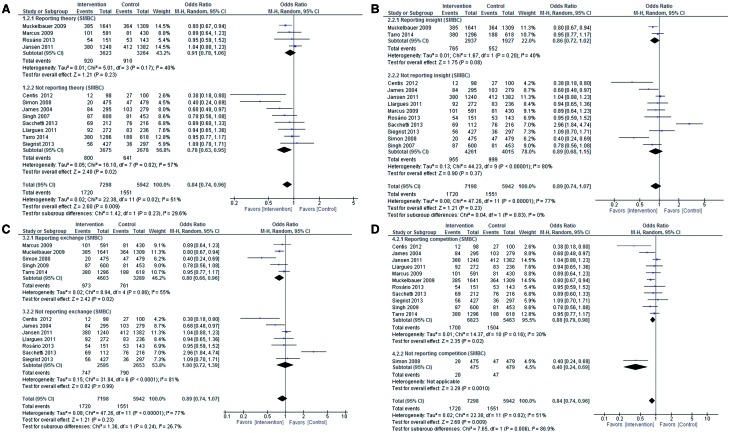
Figure 4 shows the effect of including each of the remaining 4 SMBC (theory, insight, exchange, and competition) on BMI SMD. Figure 4A shows that the presence or absence of the theory criterion is inconsequential. In Figure 4B (insight), no comparison was made because every study presented this criterion. Figure 4C (exchange) shows a small reduction, according to Cohen,68 in BMI SMD effect size (−0.17; 95%CI, −0.32 to −0.02) for the 13 studies in the analysis that did not report this criterion, a finding contrary to expectations. Finally, Figure 4D (competition) shows a small reduction in effect size (BMI SMD, −0.15; 95%CI, −0.25 to −0.04) in the 15 studies that did report this criterion.
Figure 4.
Forest plot results showing the effect (if any) of including the remaining 4 social marketing benchmark criteria (SMBC) (theory, insight, exchange, and competition) on BMI. Forest plots were constructed of randomized controlled trials that reported (1) body mass index as well as the standard mean difference (SMD) and its standard deviation (SD) or 95%CI; or (2) data related to the 4 remaining SMBC (A. theory; B. insight; C. exchange; D. competition) from which the SMD and SD or 95%CI could be calculated.
Prevalence of overweight and obesity
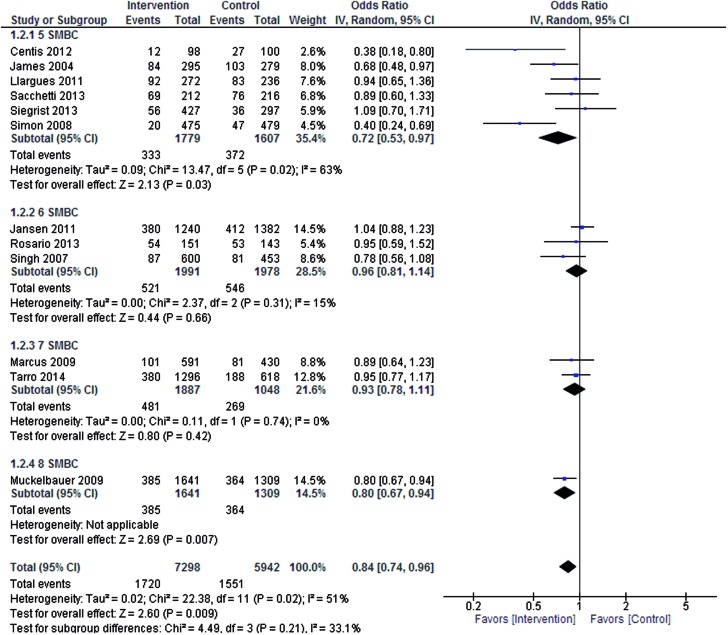
Twelve RTCs with a total of 7298 participants were included in this meta-analysis. Figure 5 shows the forest plot results of the analysis. The OR of prevalence of overweight and obesity yielded by the estimator (OR, 0.84; 95%CI, 0.74–0.96) implies that, overall, interventions have a 16% greater likelihood of reducing the prevalence of overweight and obesity compared with no intervention (control).
Figure 5.
Forest plot of randomized controlled trials that reported (1) prevalence of obesity and number of social marketing benchmark criteria (SMBC) as well as the odds ratio; or (2) data on the prevalence of overweight and obesity from which the odds ratio could be calculated.
An analysis of the effect size of the intervention studies in relation to the number of SMBC reported showed that interventions utilizing 5 SMBC had a greater likelihood of reducing the prevalence of overweight and obesity. The results imply that studies incorporating 5 SMBC (OR, 0.72; 95%CI, 0.53–0.97) were 28% more likely to be effective in reducing the prevalence of overweight and obesity. Only one school-based intervention included all 8 SMBC (OR, 0.80; 95%CI, 0.67–0.94), which, according to the analysis, resulted in a 20% greater likelihood of a reduction in the prevalence of overweight and obesity.
Moreover, school-based interventions that included 6 SMBC49,53,56, corresponded to a 4% likelihood of reducing the prevalence of overweight and obesity (OR, 0.96; 95%CI, 0.81–1.14), and those that included 7 SMBC58,60 corresponded to a 7% likelihood of reducing the prevalence of overweight and obesity (OR, 0.93; 95%CI, 0.78–1.11).
The studies that carried more weight in this meta-analysis (14.5% Jansen et al.,53 with 1382 participants, and 14.5% Muckelbauer et al.,39 with 1309 participants) show that an intervention using all 8 of the SMBC domains39 is more likely to reduce the prevalence of overweight and obesity in larger populations (OR, 0.80; 95%CI, 0.67–0.94) than interventions utilizing 653 SMBC domains (OR, 1.04; 95%CI, 0.88–1.23).
Figure 6 shows the effect of each of the remaining 4 SMBC (theory, insight, exchange, and competition) relative to the prevalence of overweight and obesity. Figure 6A (theory) shows that the presence or absence of this criterion is inconsequential. In Figure 6B (insight), results are similar to those obtained with the theory criterion. For Figure 6C (exchange), a lower likelihood of prevalence of overweight and obesity (OR, 0.80; 95%CI, 0.66–0.96) was found in the group of studies that report this criterion. Finally, in Figure 6D (competition), the results show that neither presence nor absence of this criterion affects the risk of obesity.
Figure 6.
Forest plot results showing the effect (if any) of including the remaining 4 social marketing benchmark criteria (SMBC) (theory, insight, exchange, and competition) on prevalence of overweight and obesity. Forest plots were constructed of randomized controlled trials that reported (1) prevalence of overweight and obesity as well as the odds ratio; or (2) data related to the 4 remaining SMBC (A. theory; B. insight; C. exchange; D. competition) from which the odds ratio could be calculated. Abbreviation: M-H, analysis model.
DISCUSSION
This systematic review of results from school-based interventions to prevent youth obesity in Europe confirms there are several well-known factors that increase the effectiveness of interventions, independent of the use of SMBC. These factors take various forms, such as use of the school setting,70 inclusion of teachers,71 inclusion of parents,72 and use of technological devices.73 Although some or all of these factors were incorporated into some of the interventions in this review, there is currently no identified reference methodology for school-based interventions that can be implemented universally to prevent childhood obesity.74
Several authors have identified key methodological elements that should be included in health interventions to prevent youth obesity, such as participant orientation,75,76 participant segmentation,75,76 the use of a theoretical framework,77 a focus on the intervention to change a specific behavior,20,21 consideration of the costs associated with the intervention,78,79 consideration of what motivates participants to change a behavior,80 consideration of the possible barriers faced by participants and intermediaries,81 and the inclusion of marketing elements in a methods mix.82 It is notable that these 8 key elements are the SMBC domains, whereas the social marketing methodological tool is little known and not widely used.
After an initial analysis comparing the number of included SMBC domains with the quality appraisal rating of each study, the results suggest that the inclusion of more SMBC domains resulted in a higher quality appraisal rating; consequently, the presence of SMBC domains could also benefit the quality of a study. Thus, the use of more SMBC domains may reflect a more informed methodological process in studies.
The results of the meta-analysis of 18 RCTs reporting BMI or prevalence of overweight and obesity as an outcome show that interventions with a large number of SMBC – specifically 5 or 8 domains – in design or implementation were more likely to favor the intervention group by reducing BMI or the prevalence of overweight and obesity.
Two key observations can be drawn from the meta-analysis. First, for studies that reported BMI as an outcome, the estimator favored the intervention; however, in the study that utilized only 4 SMBC,38 the control group exhibited a more significant reduction in BMI. In studies that reported the prevalence of overweight and obesity as an outcome, the estimator also favored interventions that included 5 SMBC domains, and in the only study that incorporated the use of all 8 SMBC,39 the intervention group was found to exhibit a more significant reduction in the prevalence of overweight and obesity. Overall, this meta-analysis supports the notion that school is a favorable setting for interventions to prevent obesity, especially when 5 or more SMBC are utilized.
Of the 18 RCTs included in the BMI meta-analysis, all reported at least the following 4 SMBC domains: participant orientation, behavior, segmentation, and methods mix. All but 1 study36 included the competition domain, and 7 based their school-based intervention on a theoretical framework.30,42,43,46,53,56,58 Only 1 study included the insight domain in the design,58 and 6 studies mentioned the exchange of the intervention.36,49,50,56,58,61 The effect size of implementation of 5 SMBC domains in school-based intervention studies was small, with a resulting BMI SMD of −0.25 (95%CI, −0.45 to −0.04).
Of the 12 RCTs included in the meta-analysis of the prevalence of overweight and obesity, all reported at least the following 4 SMBC domains: participant orientation, behavior, segmentation, and methods mix. Additionally, all but one36 of the 12 RCTs included the competition domain, 4 based their intervention on a theoretical framework,39,53,56,60 2 included the insight domain in the design,39,58 and 5 included the exchange of the intervention.49,58,60,61 Overall, the inclusion of at least 5 SMBC in the school-based interventions resulted in a reduction in the prevalence of overweight and obesity of approximately 28%.
When the relation of the presence or absence of each of the remaining 4 of 8 SMBC (theory, insight, exchange, and competition) to the outcome of either BMI or prevalence of overweight and obesity was analyzed, no differences were observed. Four SMBC (participant orientation, behavior, segmentation, and methods mix) were always included, whereas inclusion of each of the remaining 4 appears to be inconsequential although exchange is a desirable domain because of its likelihood to reduce the prevalence of overweight and obesity. This finding implies that, rather than considering the application of each remaining criterion individually, the effectiveness of using social marketing resides in including the most SMBC possible. Additionally, the conclusion is that, by considering any of the 4 always-included SMBC, a fifth criterion, i.e., any 1 of the remaining 4 SMBC (theory, insight, exchange, and competition), would be sufficient to observe an increase in the success of an intervention as described in the present meta-analysis. This observation suggests new methodological aspects that must be confirmed.
To reduce obesity, well-designed, well-implemented, and properly evaluated RCT interventions are indispensable. Many methodological challenges identified in school-based interventions74 could be addressed by the use of SMBC.
Social marketing characteristics and concepts can be used to deliver a health-promoting message, thus constituting a methodological tool to help individuals make healthy choices. They can be used both to send a beneficial message based on scientific information, and to help individuals receive the message through optimal methods of execution and communication.83 The use of social marketing concepts may save time and economic resources, aid in the construction of new strategies that can be shaped from existing effective programs and interventions, and prevent serious public health problems, such as childhood and adolescent obesity.12
Limitations
Several limitations were found during the development of this review. First, only one publication consciously used and described social marketing as a methodological tool.62 The lack of methodological descriptions in some publications was also a common limitation. Additionally, the use of different tools, which were not always validated, to evaluate the principal outcomes of school-based interventions made it difficult to compare results and estimate the effectiveness of the interventions.
Currently, there is no identified gold standard school-based intervention that can be implemented to prevent obesity and improve health habits.74 As a result, none of the interventions included in the systematic review and meta-analysis is considered a comparative gold standard.
A frequent limitation encountered during the selection process was the lack of uniformity in the use of the term follow-up in different studies. While some authors use it to describe the period from the beginning until the end of the intervention, others use it to describe the period after the intervention has ended.
Although quality appraisal was not a criterion for inclusion, several key methodological limitations were encountered: lack of description of blinding (n = 24), insufficient information to evaluate blinding (n = 5), lack of randomization (n = 6), lack of explanation of randomization (n = 11), nonvalidated or unreliable data collection (n = 9), and unreported dropouts (n = 10).
CONCLUSION
The inclusion of SMBC when designing interventions represents a valuable methodological tool that may increase the quality and effectiveness of school-based interventions aimed at improving healthy habits, ultimately resulting in positive changes in outcomes such as weight, BMI, or prevalence of overweight and obesity. The current evidence is sufficient to support the notion that at least 5 SMBC domains, regardless of which domains are chosen, must be included in the design of school-based interventions so that these interventions can benefit weight-related measures in young people. Furthermore, the inclusion of SMBC in school-based interventions will allow the health impact of social marketing to be assessed and validated.
Acknowledgments
The European Youth Tackling Obesity Project has received funding from the European Union Executive Agency for Health and Consumers Framework of Health Program 2008–2013. This project was conducted with the valuable collaboration of the National Children's Bureau (United Kingdom), Companhia de Ideias (Portugal), Komunikujeme (Czech Republic), the Technology Centre of Nutrition and Health (Spain), and Universitat Rovira I Virgili (Spain).
MA-M and CFM-G are the recipients of a fellowship award from the Mexican National Council of Science and Technology (CONACyT).
Declaration of interest. The authors have no relevant interests to declare.
References
- 1.World Health Organization, Regional Office for Europe. Obesity: data and statistics. http://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity/data-and-statistics. Published 2014. Accessed April 6, 2014.
- 2.Baker JL, Farpour-Lambert NJ, Nowicka P, et al. Evaluation of the overweight/obese child – practical tips for the primary health care provider: recommendations from the Childhood Obesity Task Force of the European Association for the Study of Obesity. Obes Facts. 2010;3:131–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bodzsar EB, Zsakai A. Recent trends in childhood obesity and overweight in the transition countries of Eastern and Central Europe. Ann Hum Biol. 2014;41:263–270. [DOI] [PubMed] [Google Scholar]
- 4.Kakinami L, Paradis G, O'Loughlin J, et al. Is the obesity epidemic worsening the cardiovascular risk factor profile of children? Evidence from two Québec samples measured 10 years apart. Ann Hum Biol. 2012;39:322–326. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization, Regional Office for Europe. WHO European Childhood Obesity Surveillance Initiative (COSI). http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/activities/monitoring-and-surveillance/who-european-childhood-obesity-surveillance-initiative-cosi. Published 2014. Accessed April 6, 2014.
- 6.Cairns G, Stead M. Symposium on “The challenge of translating nutrition research into public health nutrition". Session 5: Nutrition communication. Obesity and social marketing: works in progress. Proc Nutr Soc. 2009;68:11–16. [DOI] [PubMed] [Google Scholar]
- 7.Karnik S, Kanekar A. Childhood obesity: a global public health crisis. Int J Prev Med. 2012;3:1–7. [PMC free article] [PubMed] [Google Scholar]
- 8.Ben-Sefer E, Ben-Natan M, Ehrenfeld M. Childhood obesity: current literature, policy and implications for practice. Int Nurs Rev. 2009;56:166–173. [DOI] [PubMed] [Google Scholar]
- 9.Lobstein T, Baur LA. Policies to prevent childhood obesity in the European Union. Eur J Public Health. 2005;15:576–579. [DOI] [PubMed] [Google Scholar]
- 10.Evans WD, Christoffel KK, Necheles JW, et al. Social marketing as a childhood obesity prevention strategy. Obesity (Silver Spring) 2010;18(suppl 1):S23–S26. [DOI] [PubMed] [Google Scholar]
- 11.Hastings G, Haywood A. Social marketing and communication in health promotion. Health Promot Int. 1991;6:135–145. [Google Scholar]
- 12.Lefebvre RC, Flora JA. Social marketing and public health intervention. Health Educ Q. 1988;15:299–315. [DOI] [PubMed] [Google Scholar]
- 13.Storey JD, Saffitz GB, Rimón JG. Social marketing. In: Glanz K, Rimer BK, Viswanath K, eds. Health Behavior and Health Education. Theory, Research and Practice. San Francisco, CA: Jossey Bass; 2008:435–464. [Google Scholar]
- 14.Kotler P, Zaltman G. Social marketing: an approach to planned social change. J Mark. 1971;35:3–12. [PubMed] [Google Scholar]
- 15.Kotler P, Roberto EL, Roberto N. eds. Social Marketing Strategies for Changing Public Behavior. 2nd ed New York, NY: Free Press; 2002. [Google Scholar]
- 16.Andreasen A. Social marketing: definition and domain. J Public Policy Mark. 1994;13:108–114. [Google Scholar]
- 17.National Social Marketing Centre. NSMC website. NSMC benchmark criteria. http://www.socialmarketing-toolbox.com/content/nsmc-benchmark-criteria-0. 2010. Accessed April 18, 2014.
- 18.Gracia-Marco L, Vicente-Rodríguez G, Borys JM, et al. Contribution of social marketing strategies to community-based obesity prevention programmes in children. Int J Obes (Lond). 2011;35:472–479. [DOI] [PubMed] [Google Scholar]
- 19.Gracia-Marco L, Moreno LA, Vicente-Rodríguez G. Impact of social marketing in the prevention of childhood obesity. Adv Nutr. 2012;3:611S–615S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grier S, Bryant CA. Social marketing in public health. Annu Rev Public Health. 2005;26:319–339. [DOI] [PubMed] [Google Scholar]
- 21.Dietz WH., Jr Childhood obesity. Ann N Y Acad Sci. 1987;499:47–54. [DOI] [PubMed] [Google Scholar]
- 22.Dietz WH, Gortmaker SL. Preventing obesity in children and adolescents. Annu Rev Public Health. 2001;22:337–353. [DOI] [PubMed] [Google Scholar]
- 23.Ammerman AS, Lindquist CH, Lohr KN, et al. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: a review of the evidence. Prev Med. 2002;35:25–41. [DOI] [PubMed] [Google Scholar]
- 24.Rey-Lopez JP, Vicente-Rodriguez G, Biosca M, et al. Sedentary behaviour and obesity development in children and adolescents. Nutr Metab Cardiovasc Dis. 2008;18:242–251. [DOI] [PubMed] [Google Scholar]
- 25.de Souza MC, Eisenmann JC, e Santos DV, et al. Modeling the dynamics of BMI changes during adolescence. The Oporto Growth, Health and Performance Study. Int J Obes (Lond). 2015;39:1063–1069. [DOI] [PubMed] [Google Scholar]
- 26.Rito AI, Carvalho MA, Ramos C, et al. Program Obesity Zero (POZ) – a community-based intervention to address overweight primary-school children from five Portuguese municipalities. Public Health Nutr. 2013;16:1043–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lazorick S, Fang X, Hardison GT, et al. Improved body mass index measures following a middle school-based obesity intervention – the MATCH Program. J Sch Health. 2015;85:680–687. [DOI] [PubMed] [Google Scholar]
- 28.Armstrong R, Waters E, Doyle J, eds. Reviews in public health and health promotion. Chapter 21. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. Updated March 2011. London, UK: The Cochrane Collaboration. www.cochrane-handbook.org. Accessed February 5, 2014. [Google Scholar]
- 29.Effective Public Health Practice Project. Effective Public Health Practice Project–Quality Assessment Tool for Quantitative Studies. Hamilton, Ontario, Canada; 2010. http://www.ephpp.ca/PDF/Quality%20Assessment%20Tool_2010_2.pdf. Accessed May 6, 2014.
- 30.Haerens L, Deforche B, Maes L, et al. Body mass effects of a physical activity and healthy food intervention in middle schools. Obesity (Silver Spring). 2006;14:847–854. [DOI] [PubMed] [Google Scholar]
- 31.Haerens L, Deforche B, Maes L, et al. Evaluation of a 2-year physical activity and healthy eating intervention in middle school children. Health Educ Res. 2006;21:911–921. [DOI] [PubMed] [Google Scholar]
- 32.Haerens L, De Bourdeaudhuij I, Maes L, et al. School-based randomized controlled trial of a physical activity intervention among adolescents. J Adolesc Health. 2007;40:258–265. [DOI] [PubMed] [Google Scholar]
- 33.Haerens L, De Bourdeaudhuij I, Maes L, et al. The effects of a middle-school healthy eating intervention on adolescents’ fat and fruit intake and soft drinks consumption. Public Health Nutr. 2007;10:443–449. [DOI] [PubMed] [Google Scholar]
- 34.Sigmund E, El Ansari W, Sigmundová D. Does school-based physical activity decrease overweight and obesity in children aged 6–9 years? A two-year non-randomized longitudinal intervention study in the Czech Republic. BMC Public Health. 2012;12:570 doi:10.1186/1471-2458-12-570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klakk H, Chinapaw M, Heidemann M, et al. Effect of four additional physical education lessons on body composition in children aged 8–13 years – a prospective study during two school years. BMC Pediatr. 2013;13:170 doi:10.1186/1471-2431-13-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simon C, Schweitzer B, Oujaa M, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4-year randomized controlled intervention. Int J Obes (Lond). 2008;32:1489–1498. [DOI] [PubMed] [Google Scholar]
- 37.Thivel D, Isacco L, Lazaar N, et al. Effect of a 6-month school-based physical activity program on body composition and physical fitness in lean and obese schoolchildren. Eur J Pediatr. 2011;170:1435–1443. [DOI] [PubMed] [Google Scholar]
- 38.Graf C, Koch B, Falkowski G, et al. Effects of a school-based intervention on BMI and motor abilities in childhood. J Sports Sci Med. 2005;4:291–299. [PMC free article] [PubMed] [Google Scholar]
- 39.Muckelbauer R, Libuda L, Clausen K, et al. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics. 2009;123:e661–e667. [DOI] [PubMed] [Google Scholar]
- 40.Brandstetter S, Klenk J, Berg S, et al. Overweight prevention implemented by primary school teachers: a randomised controlled trial. Obes Facts. 2012;5:1–11. [DOI] [PubMed] [Google Scholar]
- 41.Siegrist M, Lammel C, Haller B, et al. Effects of a physical education program on physical activity, fitness, and health in children: the JuvenTUM project. Scand J Med Sci Sports. 2013;23:323–330. [DOI] [PubMed] [Google Scholar]
- 42.Angelopoulos PD, Milionis HJ, Grammatikaki E, et al. Changes in BMI and blood pressure after a school based intervention: the CHILDREN study. Eur J Public Health. 2009;19:319–325. [DOI] [PubMed] [Google Scholar]
- 43.Mihas C, Mariolis A, Manios Y, et al. Evaluation of a nutrition intervention in adolescents of an urban area in Greece: short- and long-term effects of the VYRONAS study. Public Health Nutr. 2010;13:712–719. [DOI] [PubMed] [Google Scholar]
- 44.Kristjansdottir AG, Johannsson E, Thorsdottir I. Effects of a school-based intervention on adherence of 7–9-year-olds to food-based dietary guidelines and intake of nutrients. Public Health Nutr. 2010;13:1151–1161. [DOI] [PubMed] [Google Scholar]
- 45.Magnusson KT, Sigurgeirsson I, Sveinsson T, et al. Assessment of a two-year school-based physical activity intervention among 7–9-year-old children. Int J Behav Nutr Phys Act. 2011;8:138 doi:10.1186/1479-5868-8-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Magnusson KT, Hrafnkelsson H, Sigurgeirsson I, et al. Limited effects of a 2-year school-based physical activity intervention on body composition and cardiorespiratory fitness in 7-year-old children. Health Educ Res. 2012;27:484–494. [DOI] [PubMed] [Google Scholar]
- 47.Centis E, Marzocchi R, Di Luzio R, et al. A controlled, class-based multicomponent intervention to promote healthy lifestyle and to reduce the burden of childhood obesity. Pediatr Obes. 2012;7:436–445. [DOI] [PubMed] [Google Scholar]
- 48.Sacchetti R, Ceciliani A, Garulli A, et al. Effects of a 2-year school-based intervention of enhanced physical education in the primary school. J Sch Health. 2013;83:639–646. [DOI] [PubMed] [Google Scholar]
- 49.Singh AS, Chin A, Paw MJ, et al. Short-term effects of school-based weight gain prevention among adolescents. Arch Pediatr Adolesc Med. 2007;161:565–571. [DOI] [PubMed] [Google Scholar]
- 50.Singh AS, Chin A, Paw MJ, et al. Dutch obesity intervention in teenagers: effectiveness of a school-based program on body composition and behavior. Arch Pediatr Adolesc Med. 2009;163:309–317. [DOI] [PubMed] [Google Scholar]
- 51.Martens MK, Van Assema P, Paulussen TG, et al. Krachtvoer: effect evaluation of a Dutch healthful diet promotion curriculum for lower vocational schools. Public Health Nutr. 2008;11:271–278. [DOI] [PubMed] [Google Scholar]
- 52.Jurg ME, Kremers SP, Candel MJ, et al. A controlled trial of a school-based environmental intervention to improve physical activity in Dutch children: JUMP-in, kids in motion. Health Promot Int. 2006;21:320–330. [DOI] [PubMed] [Google Scholar]
- 53.Jansen W, Borsboom G, Meima A, et al. Effectiveness of a primary school-based intervention to reduce overweight. Int J Pediatr Obes. 2011;6:e70–e77. [DOI] [PubMed] [Google Scholar]
- 54.Ezendam NP, Brug J, Oenema A. Evaluation of the web-based computer-tailored FATaintPHAT intervention to promote energy balance among adolescents: results from a school cluster randomized trial. Arch Pediatr Adolesc Med. 2012;166:248–255. [DOI] [PubMed] [Google Scholar]
- 55.Grydeland M, Bergh IH, Bjelland M, et al. Intervention effects on physical activity: the HEIA study – a cluster randomized controlled trial. Int J Behav Nutr Phys Act. 2013;10:17 doi:10.1186/1479-5868-10-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rosário R, Araújo A, Oliveira B, et al. Impact of an intervention through teachers to prevent consumption of low nutrition, energy-dense foods and beverages: a randomized trial. Prev Med. 2013;57:20–25. [DOI] [PubMed] [Google Scholar]
- 57.Llargues E, Franco R, Recasens A, et al. Assessment of a school-based intervention in eating habits and physical activity in school children: the AVall study. J Epidemiol Community Health. 2011;65:896–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tarro L, Llauradó E, Albaladejo R, et al. A primary-school-based study to reduce the prevalence of childhood obesity – the EdAl (Educació en Alimentació) study: a randomized controlled trial. Trials. 2014;15:58 doi:10.1186/1745-6215-15-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sollerhed AC, Ejlertsson G. Physical benefits of expanded physical education in primary school: findings from a 3-year intervention study in Sweden. Scand J Med Sci Sports. 2008;18:102–107. [DOI] [PubMed] [Google Scholar]
- 60.Marcus C, Nyberg G, Nordenfelt A, et al. A 4-year, cluster-randomized, controlled childhood obesity prevention study: STOPP. Int J Obes (Lond). 2009;33:408–417. [DOI] [PubMed] [Google Scholar]
- 61.Kriemler S, Zahner L, Schindler C, et al. Effect of school based physical activity programme (KISS) on fitness and adiposity in primary schoolchildren: cluster randomised controlled trial. BMJ. 2010;340:c785 doi:10.1136/bmj.c785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lakshman RR, Sharp SJ, Ong KK, et al. A novel school-based intervention to improve nutrition knowledge in children: cluster randomised controlled trial. BMC Public Health. 2010;10:123 doi:10.1186/1471-2458-10-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.James J, Thomas P, Cavan D, et al. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. BMJ. 2004;328:1237 doi:10.1136/bmj.38077.458438.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Breslin G, Brennan D, Rafferty R, et al. The effect of a healthy lifestyle programme on 8–9 year olds from social disadvantage. Arch Dis Child. 2012;97:618–624. [DOI] [PubMed] [Google Scholar]
- 65.Sahota P, Rudolf MC, Dixey R, et al. Randomised controlled trial of primary school based intervention to reduce risk factors for obesity. BMJ. 2001;323:1029–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.De Bourdeaudhuij I, Maes L, De Henauw S, et al. Evaluation of a computer-tailored physical activity intervention in adolescents in six European countries: the Activ-O-Meter in the HELENA intervention study. J Adolesc Health. 2010;46:458–466. [DOI] [PubMed] [Google Scholar]
- 67.Te Velde SJ, Brug J, Wind M, et al. Effects of a comprehensive fruit- and vegetable-promoting school-based intervention in three European countries: the Pro Children Study. Br J Nutr. 2008;99:893–903. [DOI] [PubMed] [Google Scholar]
- 68.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. [DOI] [PubMed] [Google Scholar]
- 69.Verstraeten R, Roberfroid D, Lachat C, et al. Effectiveness of preventive school-based obesity interventions in low- and middle-income countries: a systematic review. Am J Clin Nutr. 2013;96:415–438. [DOI] [PubMed] [Google Scholar]
- 70.Sharma M. School-based interventions for childhood and adolescent obesity. Obes Rev. 2006;7:261–269. [DOI] [PubMed] [Google Scholar]
- 71.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2011;12:CD001871 doi:10.1002/14651858.CD001871.pub3. [DOI] [PubMed] [Google Scholar]
- 72.Faith MS, Van Horn L, Appel LJ, et al. Evaluating parents and adult caregivers as “agents of change” for treating obese children: evidence for parent behavior change strategies and research gaps: a scientific statement from the American Heart Association. Circulation. 2012;125:1186–1207. [DOI] [PubMed] [Google Scholar]
- 73.Norman GJ, Zabinski MF, Adams MA, et al. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med. 2007;33:336–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Jones RA, Lubans DR, Morgan PJ, et al. School-based obesity prevention interventions: practicalities and considerations. Obes Res Clin Pract. 2014;8:e497–e510. [DOI] [PubMed] [Google Scholar]
- 75.Gonzalez-Suarez C, Worley A, Grimmer-Somers K, et al. School-based interventions on childhood obesity: a meta-analysis. Am J Prev Med. 2009;37:418–427. [DOI] [PubMed] [Google Scholar]
- 76.Henley N, Donovan R, Francas M. Developing and implementing communication messages. In: Doll L, Bonzo S, Mercy J, et al., eds. Handbook of Injury and Violence Prevention. New York, NY: Springer; 2007:433–447. [Google Scholar]
- 77.Forthofer MS, Bryant CA. Using audience-segmentation techniques to tailor health behavior change strategies. Am J Health Behav. 2000;24:36–43. [Google Scholar]
- 78.Baranowski T, Cullen KW, Nicklas T, et al. Are current health behavioral change models helpful in guiding prevention of weight gain efforts? Obes Res. 2003;11(suppl):23S–43S. [DOI] [PubMed] [Google Scholar]
- 79.John J, Wolfenstetter SB, Wenig CM. An economic perspective on childhood obesity: recent findings on cost of illness and cost effectiveness of interventions. Nutrition. 2012;28:829–839. [DOI] [PubMed] [Google Scholar]
- 80.Lefebvre C, Olander C, Levine E. The impact of multiple channel delivery of nutrition messages on student knowledge, motivation and behavior: results from the Team Nutrition pilot study. Soc Mark Q. 2000;5:90–98. [Google Scholar]
- 81.Hastings G. Competition in social marketing. Soc Mar Q. 2003;9:6–10. [Google Scholar]
- 82.Egger G, Donovan R, Spark R, eds. Health and the media. Principles and Practices for Health Promotion. 1st ed McGraw-Hill: Sydney, Australia; 1993. [Google Scholar]
- 83.Henley N, Raffin S. Social marketing to prevent childhood obesity. In: Waters E, Seidel JC, Swinburn SA, et al., eds. Preventing Childhood Obesity: Evidence Policy and Practice. Wiley-Blackwell: Singapore; 2010:243–252. [Google Scholar]