Abstract
Background
The purpose of this study was to detect chronic obstructive pulmonary disease (COPD) among smokers seeking treatment for the first time in a smoking cessation clinic and to assess the predictors of positive screening.
Methods
This study was based on a multicenter survey with questionnaires (Richmond, Fagerstrom, clinical signs) and spirometry miniaturized. Data were analyzed with SAS® by Pearson chi-square test, the test of analysis of variance, Spearman correlation coefficient, and multivariate logistic regression step down.
Findings
1918 patients were assessed for eligibility and only 1737 were included. The report forced expiratory volume in 1 second (FEV1/FEV6) was < 0.8 for 33.2% of smokers and < 0.7 for 7.5% of them. People with likely COPD had more dyspnea (P < 0.010) and chronic bronchitis (CB) (P < 0.010). In multivariate analysis, CB, duration of smoking history since longer than 30 years, and dyspnea significantly increased the risk of being detected as COPD. The odds ratios of the above factors were 2.9, 4.1, and 4.5, respectively.
Conclusion
7.5% of smokers were likely COPD. Patient’s risk factors, such as the presence of CB, smoking addiction for longer than 30 years, or dyspnea, were predictive of a positive screening for COPD.
Keywords: Diagnosis, Prevention/control, Smoking cessation, Tobacco use disorder
Introduction
The chronic obstructive pulmonary disease (COPD) is defined as a forced expiratory volume (FEV) to forced vital capacity ratio of < 70% after administration of bronchodilators.1 This disease is complicated by pathological changes of the lung and systemic effects that can make the poor prognosis for some patients.2 The prevalence of this disease is estimated at 7.5% [95% confidence interval (CI) = 6-9.2] for COPD and 6.4% (95% CI = 5.3-7.7) for chronic bronchitis (CB). The epidemiological projections predict that by 2020 COPD will be the third leading cause of death worldwide and the fifth leading cause of years lost by premature death or disability. CB is a COPD condition diagnosed clinically, whereas COPD diagnosis is based on a pulmonary function tests (PFT).3 For screening purposes, approximate values of the VC can be used, e.g., FEV in 6 seconds (FEV6).4-6
The prevalence of COPD in smokers is higher than that of the general population.7 Therefore, this population should be targeted for screening.8 This screening is especially important due to the following potential factors: underestimation of COPD prevalence, late diagnosis due to low detection rate of bronchial flow, and lack of health care for half of the patients.9
According to the literature, COPD has a high prevalence among smokers due to the severe evolution of the disease and high rate of undiagnosed disease. The goal of our study was to detect COPD among patients consulting for the first time in a smoking cessation clinic and to study the predictors of positive screening for COPD.
Methods
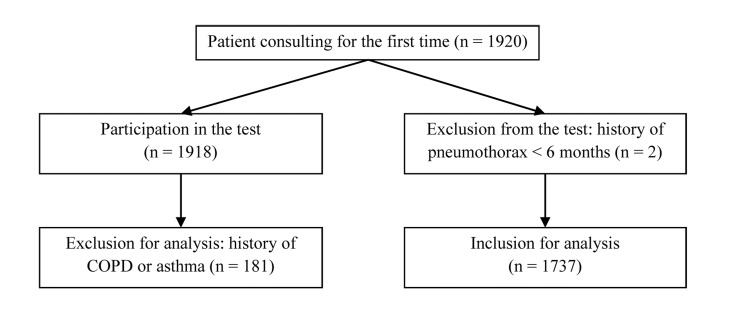
This was a prospective multicenter study of 1918 smokers selected from 16 French smoking cessation clinics between January and December 2009. Inclusion criteria were active smokers, coming for the first time in one of these clinics, and who consented to take part in the study. The exclusion criterion was a history of pneumothorax of < 6 months. Furthermore, after patient’s eligibility assessment, those with known COPD or asthma prior to the first consultation were excluded from data processing to avoid possible selection bias. Figure 1 describes the flow of patients from selection to data analysis. This study was in accordance with ethical standards of hospitals. Subjects were informed, and consent was obtained.
Figure 1.
Flow of the patients throughout the study COPD: Chronic obstructive pulmonary disease
During the visit, the nurse or physician completed a questionnaire collecting the date of consultation, age, and sex of the patient, the duration of tobacco use, the presence or absence of history of diagnosed COPD and the results of previous PFT, the presence of clinical signs (cough, dyspnea, and sputum), the motivation to quit according to the score of Richmond et al.,10 the addiction score of Fagerstrom and Schneider,11 the rate of carbon monoxide (CO) in exhaled air, the height of the person (in cm) and the results of lung function.
CB was recorded only if it had lasted for at least 3 months during 2 consecutive years. A cough was recorded only if the duration of symptoms was shorter than that defined above. Dyspnea was assessed by the 0-4 scale of the Medical Research Council.12 The CO in exhaled air was measured with a CO meter. The result was expressed in parts per million (ppm).
Lung function was measured by a spirometer (NEO 6®, Eness, France) in all clinics. The collected data were: FEV1, FEV6, and the ratio of FEV1/FEV6. A tobacco specialist nurse or physician helped the patient with this examination, which was repeated 3 times to achieve consistent results. The theoretical values were calculated using the ECSC (European Coal and Steel Community) standard.13
The results were entered into Excel® (version 2007, Microsoft Office, Redmond, Washington, USA) spreadsheet and were analyzed using SAS® software (version 9.4, SAS Institute, Cary, NC, USA) France. However, the patients with a known history of COPD were excluded from this step. Based on the spirometric data and the clinical scores, we allocated the patients into two groups: likely COPD and unlikely COPD. The likely COPD group was defined as an FEV1/FEV6 < 0.70. The unlikely COPD group was defined as the FEV1/FEV6 ≥ 0.70. In the unlikely COPD group, two subgroups were defined as the FEV1/FEV6 > 0.70 < 0.79; and the FEV1/FEV6 ≥ 0.8.
Several classes of variables were defined to assure homogeneous data. Age was divided into four classes: < 30, > 30 < 39, > 40 < 59, and > 60 years. Duration of smoking was also divided into four classes: 0-9, 10-19, 20-29, and > 30 years. People with a Richmond’s score > 8 were considered highly motivated and, conversely, those with scores ≤ 5 were considered to be lowly motivated to quit. Those with scores equal to 6, 7, or 8 were considered to be moderately motivated. People with a Fagerstrom’s score ≥ 7 were considered to be a high addict; those with scores ≤ 2 were considered to be not addicted; those with scores equal to 3, 4, 5, or 6 were considered to be a lowly addict.
For each quantitative variable, we calculated the mean ± standard deviation (SD), and the median (range). In addition, we analyzed the relationship between the EFR data and gender, age, duration of smoking, clinical signs, and the scores of Richmond and Fagerstrom tests. We used the Pearson chi-square test for the comparison between the categorical variables. The test of analysis of variance or t-test was used for the comparison between qualitative and quantitative variables. The Spearman correlation coefficient was used to compare the quantitative variables. We took as our threshold of significance: P < 0.050.
Finally, we performed a multivariate analysis using logistic regression step down to identify the variables predictors of COPD. Each variable with a P < 0.200 in univariate analysis was used for multivariate analysis.
Results
There were 16 participating clinics. Overall, the sample consisted of 1918 individuals, mostly women. There were 1000 (52.1%) women and 918 (47.9%) men. 181 (9.47%) patients had a history of COPD. These individuals were excluded from the calculations. Of the 1737 people with no history of COPD, 1671 were classified into two groups of unlikely COPD and likely COPD: 1546 (92.5%) in the former and 125 (7.5%) in the latter group. In the unlikely group, 429 (25.7%) had the FEV1/FEV6 between 0.71 and 0.79, and 1117 (66.8%) the FEV1/FEV6 ≥ 0.8. In total, 33.2% of patients had the FEV1/FEV6 < 0.8.
The mean age was 44.3 years (± 12.3) with a median of 44 years (range 11-85). The mean duration of smoking was 26.1 years (± 11.7) with a median of 26 years (range 0-64). Duration of smoking was significantly lower in women: 23 versus 26 years (P < 0.010).
Patient’s symptoms are displayed in table 1. The majority of patients had a CB (67.2%) or a cough (84.9%).
Table 1.
Frequency of patient’s symptoms in analyzed sample (n = 1737)
| Symptoms | n (%) |
|---|---|
| Cough | |
| Yes | 1475 (84.9) |
| No | 262 (15.1) |
| CB | |
| Yes | 1167 (67.2) |
| No | 570 (32.8) |
| Dyspnea | |
| Yes | 826 (47.6) |
| Stage 1 | 536 (30.9) |
| Stage 2 | 212 (12.2) |
| Stage 3 | 55 (3.2) |
| Stage 4 | 16 (0.9) |
| No | 911 (67.9) |
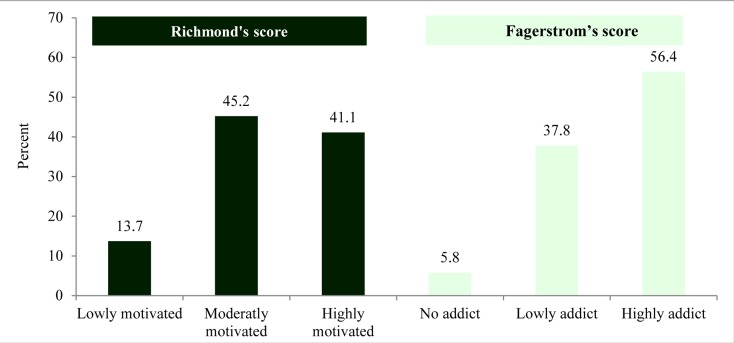
Motivation/addiction
Motivation mean was 7.8 ± 2.0, the median was 8.00 (range 0-10) (Figure 2). For addiction, the mean was 6.4 ± 2.3, the median was 7.00 (range 0-10). Motivation was significantly related to addiction: higher the addiction score, lower was the motivation to quit; Spearman correlation coefficient (r = -0.08) (P < 0.010).
Figure 2.
Results of Richmond’s score and of Fagerstrom’s score
Addiction was inversely related to the ratio FEV1/FEV6: lower the ratio, stronger was the addiction; r = −0.14 (P < 0.010). Moreover, addiction was strongly related to age and duration of tobacco use: older and longer duration of tobacco use were related to stronger addiction: r = 0.05 (P < 0.040) and r = 0.10 (P < 0.010). Fagerstrom ýscore was lower for women than for men (P < 0.010).
Results of lung function
The FEV1/FEV6 was inversely related to age, duration of smoking, addiction, and gender. Older, longer duration of smoking and stronger addiction were related to a lower FEV1/FEV6: respectively, r = −0.30, −0.32, and -0.14 (P < 0.010 for each item). Women had a higher ratio than men: 6.3 versus 6.7 (P < 0.010). There was a significance difference between the likely COPD group and unlikely COPD group in regard to symptoms and smoking duration (Table 2).
Table 2.
Comparison of patient’s symptoms between the two groups
| Patient symptoms | Unlikely COPD group |
Likely COPD group |
P (Between group comparison) |
|---|---|---|---|
| n (%) | n (%) | ||
| Cough | |||
| Yes | 458 (29.6) | 84 (66.8) | < 0.010 |
| No | 1088 (70.4) | 41 (33.2) | |
| CB | |||
| Yes | 153 (9.9) | 50 (40.1) | < 0.010 |
| No | 1393 (90.1) | 75 (59.9) | |
| Dyspnea | |||
| Yes | 495 (32.0) | 98 (78.1) | < 0.010 |
| No | 1051 (68.0) | 27 (21.9) | |
| Tobacco use | |||
| < 10 years | 137 (8.8) | 3 (2.6) | < 0.010 |
| 10-19 years | 441 (28.5) | 16 (12.8) | |
| 20-29 years | 527 (34.2) | 31 (24.7) | |
| ≥ 30 years | 441 (28.5) | 75 (59.9) |
COPD: Chronic obstructive pulmonary disease; CB: Chronic bronchitis
For the level of CO in exhaled air, there was no significant difference between the groups (P = 0.100): 83.3% had an increased CO level in unlikely COPD group versus 87.4% in likely COPD group.
The multivariate analysis showed that the variables: the presence of CB, dyspnea, and smoking duration > 30 years were strongly associated with having a COPD (Table 3).
Table 3.
Predictors of chronic obstructive pulmonary disease (COPD) (positive screening) in likely COPD group
| Items | OR | CI 95% |
|---|---|---|
| CB | 2.9 | 2.0-4.3 |
| Smoking > 30 years | 4.1 | 1.7-9.9 |
| Dyspnea | 4.5 | 3.1-6.4 |
OR: Odds ratio; CI: Confidence interval; CB: Chronic bronchitis
Discussion
Our study involved 1737 smokers with no known history of COPD. Of these, 7.5% smokers were in the likely COPD group, and 33.2% had the FEV1/FEV6 < 0.8. In these patients, motivation and FEV1/FEV6 decreased with increasing addiction score. Addiction score was proportionally related to the duration of smoking. The FEV1/FEV6 decreased with increasing age, duration of smoking, and addiction score. Women had a higher FEV1/FEV6 ratio and a lower Fagerstrom score than men. Smokers with lower FEV1/FEV6 ratio had more clinical symptoms than the others. Those with CB, those smoking for at least 30 years, and those with dyspnea were more likely to have COPD than others. Patients with the cough or dyspnea or CB and those smoking for at least 30 years had a higher risk (or tendency) to have the FEV1/FEV6 < 0.7 than the other smokers.
The prevalence of COPD was poor in this study. Our sample does not seem to be representative of the general population of smokers, but rather that of smoking cessation clinics. For example, our sample consisted of 52.1% women, whereas, in the literature, smokers are mostly men. Women in our sample had a Fagerstrom score and a ratio of FEV1/FEV6 higher than the men. This result was consistent with the results by Zielinski et al., which showed the presence of airflow limitation for 23.9% of men versus 15.7% of women (P < 0.001).6 The high proportion of women in our population thus suggests that the prevalence of COPD in the likely COPD group underestimates the prevalence in the general population of smokers mainly consisted of men.
It might seem that the lack of exclusion of people with a history of COPD in this study could induce a selection bias. However, this parameter was taken into account when developing the study, and these patients were excluded from our results. The strength of our study relies on its multicentric design thus involving a large number of investigating centers. This choice was made to harmonize practices thus avoiding a bias in information collection. Moreover, our study was based on validated methods. Indeed, we used standardized and validated scales of Richmond and Fagerstrom, which allowed the comparison of our results with those of the literature.14
For practical reasons, we used a mini spirometer to measure. Then, the results were expressed as an index of FEV1/VC. Indeed, several studies have shown that the FEV6 is an approximate value of VC.15,16 In addition, measurements obtained through mini spirometry often vary from one test to another. To reduce this variability of measures, a physician or a nurse helped the patients to use the mini spirometer. Under the control of a tobacco specialist, repeated efforts were made until achieving consistent results. This quality control of the measures, which is not reported in most studies, allowed us to have reliable data and to minimize the classification bias. To meet the definition of COPD, miniaturized spirometry measurements must be confirmed with complete PFT.17 This is a limitation of this study. The sensitivity and specificity of the FEV1/FEV6 in detecting obstructive airway were 94.0 and 93.1%, respectively. Thus, the result of positive screening test was consistent with the definition of COPD. This type of measure is also used for the general population.18
Given the importance and the underestimation of COPD prevalence in this population and the potential complications, it seems ethically legitimate to undertake such screening in smokers. Furthermore, some studies have shown that screening for COPD improves the rate of smoking cessation.19-21 Indeed, having a positive screening decreases the patient’s smoking risk denial. This denial has been described as the main obstacle to smoking cessation in a few studies.22 In our study, the motivation of likely COPD smokers was lower than the unlikely COPD smokers. We did not perform further data collection and analysis to evaluate whether the positive screening had an impact both on the motivation and the success of smoking cessation.
To date, there has been no negative impact of COPD screening on smoking cessation reported in the literature. Given the above fact as well as the severity of COPD, our study objective and design seemed to be well-founded. Indeed, we observed a direct individual benefit of such screening. Furthermore, a recent review showed that the decrease in FEV in smokers is a marker of early mortality from all causes.19 Moreover, this screening seems necessary since COPD is highly undiagnosed and, consequently, often untreated.9 In addition, an Australian study comparing the effectiveness of opportunistic screening with a selected or organized screening showed to be more effective on disease control in case of opportunistic screening.23 Although opportunistic screening does not parallel our screening method, it further supports the effectiveness of screening for COPD in smoking cessation clinics. These results show the value of screening in smoking cessation clinics.
Our results highlight three clinical criteria predictive of a positive screening: the presence of dyspnea, CB, and smoking for longer than 30 years. Therefore, these results differ from the criteria generally used for targeted screening. In particular, aged older than 40 years has been commonly regarded as a COPD risk factor.17 Furthermore, a COPD screening study in tobacco control in Poland on 110355 smokers has shown that the prevalence of airflow limitation was significantly correlated with age over 40 years and the fact to have smoked more than 10 pack-years.6 Our results are not only consistent with that of the literature6,24 but also complement them and provide the practitioners with additional information, i.e., predictive factors of positive COPD screening. Our results showed a relation between the age and duration of smoking. However, this correlation varies according to the diversity in addiction history, i.e., tobacco addiction may indeed start early or late in life. In line with epidemiological studies, our results designated the duration of smoking as the main risk factor for COPD. Our results showed the complementarity of various parameters in the practice of targeted screening.
Conclusion
Our study showed that 7.5% of the smokers of smoking cessation clinics were likely COPD, and 33.2% had the FEV1/FEV6 lowered (< 0.80). Patients with CB, or a smoking history for longer than 30 years, or dyspnea were more likely to have a positive screening. These criteria could be used as the predictors of COPD for targeted screening in tobacco control.
Acknowledgments
16 smoking cessation clinics: two in Paris, Rennes, and Clermont-Ferrand; one in Brest, Epinal, Lesparre-Medoc, Le Chesnay, Morlaix, Colmar, Valves, Lannion and Bressuire Langon. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. Technical appendix, statistical code, and dataset available from the corresponding author at Dryad repository, who will provide a permanent, citable, and open access home for the dataset.
Footnotes
Conflicts of Interest
The Authors have no conflict of interest.
REFERENCES
- 1.Lemarié E, Valeyr B. Recommandations de la Société de Pneumologie de Langue Françaisesur la prise en charge de la BPCO (mise à jour 2009). Revue des Maladies Respiratoire. 2010;27(Suppl 1):S70–S73. [Google Scholar]
- 2.A Guide for Health Care Professionals. Global initiative for chronic obstructive lung disease [Online]. 2011. Available from: URL: http://www.goldcopd.org/uploads/users/files/GOLD_Pocket_May2512.pdf.
- 3.Enright PL, Kaminsky DA. Strategies for screening for chronic obstructive pulmonary disease. Respir Care. 2003;48(12):1194–201. [PubMed] [Google Scholar]
- 4.Peiffer G, Perriot J, Heno G. Détection précoce de la BPCO. Le Courrier de addictions. 2010;12(2):19–22. [Google Scholar]
- 5.Swanney MP, Jensen RL, Crichton DA, Beckert LE, Cardno LA, Crapo RO. FEV6 Is an acceptable surrogate for FVC in the spirometric diagnosis of airway obstruction and restriction. American Journal of Respiratory and Critical Care Medicine. 2000;162(3):917–9. doi: 10.1164/ajrccm.162.3.9907115. [DOI] [PubMed] [Google Scholar]
- 6.Zielinski J, Bednarek M, Gorecka D, Viegi G, Hurd SS, Fukuchi Y, et al. Increasing COPD awareness. Eur Respir J. 2006;27(4):833–52. doi: 10.1183/09031936.06.00025905. [DOI] [PubMed] [Google Scholar]
- 7.Service évaluation technologique. Guide méthodologique: comment évaluer a priori un programme de dépistage? [Online]. 2004. Available from: URL: http://www.bib-bop.org/base_bib/bib_detail.php?ref=2675&titre=guide-methodologique--comment-evaluer-a-priori-un-programme-de-depistage.
- 8.Raherison C. Facteurs étiologiques et épidémiologie des bronchopneumopathies chroniques obstructives (BPCO) [Online]. 2009. Available from: URL: http://www.emconsulte.com/article/199985/facteurs-etiologiqueset-epidemiologie-des-broncho.
- 9.Mannino DM, Gagnon RC, Petty TL, Lydick E. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2000;160(11):1683–9. doi: 10.1001/archinte.160.11.1683. [DOI] [PubMed] [Google Scholar]
- 10.Richmond RL, Kehoe LA, Webster IW. Multivariate models for predicting abstention following intervention to stop smoking by general practitioners. Addiction. 1993;88(8):1127–35. doi: 10.1111/j.1360-0443.1993.tb02132.x. [DOI] [PubMed] [Google Scholar]
- 11.Fagerstrom KO, Schneider NG. Measuring nicotine dependence: a review of the Fagerstrom Tolerance Questionnaire. J Behav Med. 1989;12(2):159–82. doi: 10.1007/BF00846549. [DOI] [PubMed] [Google Scholar]
- 12.Launois C, Barbe C, Bertin E, Nardi J, Perotin JM, Dury S, et al. The modified Medical Research Council scale for the assessment of dyspnea in daily living in obesity: a pilot study. BMC Pulm Med. 2012;12:61. doi: 10.1186/1471-2466-12-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl. 1993;16:5–40. [PubMed] [Google Scholar]
- 14.Meneses-Gaya IC, Zuardi AW, Loureiro SR, Crippa JA. Psychometric properties of the Fagerstrom Test for Nicotine Dependence. J Bras Pneumol. 2009;35(1):73–82. doi: 10.1590/s1806-37132009000100011. [DOI] [PubMed] [Google Scholar]
- 15.Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–76. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- 16.Vandevoorde J, Verbanck S, Schuermans D, Kartounian J, Vincken W. FEV1/FEV6 and FEV6 as an alternative for FEV1/FVC and FVC in the spirometric detection of airway obstruction and restriction. Chest. 2005;127(5):1560–4. doi: 10.1378/chest.127.5.1560. [DOI] [PubMed] [Google Scholar]
- 17.Durand-Zaleski I, Bastuji-Garin S. Evaluation of diagnostic or screening procedures. Validity of tests, sensitivity, specificity, predictive values. Definition and indications for mass screening. Rev Prat. 2000;10(50):1155–8. [PubMed] [Google Scholar]
- 18.Nelson SB, LaVange LM, Nie Y, Walsh JW, Enright PL, Martinez FJ, et al. Questionnaires and pocket spirometers provide an alternative approach for COPD screening in the general population. Chest. 2012;142(2):358–66. doi: 10.1378/chest.11-1474. [DOI] [PubMed] [Google Scholar]
- 19.Young RP, Hopkins R, Eaton TE. Forced expiratory volume in one second: not just a lung function test but a marker of premature death from all causes. Eur Respir J. 2007;30(4):616–22. doi: 10.1183/09031936.00021707. [DOI] [PubMed] [Google Scholar]
- 20.Gorecka D, Bednarek M, Nowinski A, Puscinska E, Goljan-Geremek A, Zielinski J. Diagnosis of airflow limitation combined with smoking cessation advice increases stop-smoking rate. Chest. 2003;123(6):1916–23. doi: 10.1378/chest.123.6.1916. [DOI] [PubMed] [Google Scholar]
- 21.Bednarek M, Gorecka D, Wielgomas J, Czajkowska-Malinowska M, Regula J, Mieszko-Filipczyk G, et al. Smokers with airway obstruction are more likely to quit smoking. Thorax. 2006;61(10):869–73. doi: 10.1136/thx.2006.059071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weinstein ND, Marcus SE, Moser RP. Smokers' unrealistic optimism about their risk. Tob Control. 2005;14:55–9. doi: 10.1136/tc.2004.008375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Walters JA, Hansen EC, Johns DP, Blizzard EL, Walters EH, Wood-Baker R. A mixed methods study to compare models of spirometry delivery in primary care for patients at risk of COPD. Thorax. 2008;63(5):408–14. doi: 10.1136/thx.2007.082859. [DOI] [PubMed] [Google Scholar]
- 24.Buffels J, Degryse J, Heyrman J, Decramer M. Office spirometry significantly improves early detection of COPD in general practice: the DIDASCO Study. Chest. 2004;125(4):1394–9. doi: 10.1378/chest.125.4.1394. [DOI] [PubMed] [Google Scholar]