We highly appreciate the willingness of the authors to reanalyze the Prevention and Observation of Surgical Endpoints (PROSE) dataset reported by Domchek et al. (1) and the cohort used by Kauff et al. (2) according to our proposed design (3), which the authors summarized very well in three points (second sentence in the Correspondence). By using risk-reducing salpingo-oophorectomy (RRSO) as a time-dependent variable in the reanalyses, immortal person-time bias (third point) was avoided in both studies. It remains unclear, however, why in the PROSE reanalysis the observation did not start at the age of DNA testing (second point). In this way, overselection of breast cancer (BC) cases in the non-RRSO group (first point) may still have resulted in an overestimation of BC risk reduction after RRSO (“cancer-induced testing bias”). The original Kauff study was already free of this type of bias. The reanalysis of the Kauff data is now restricted to BRCA1/2 mutation carriers who were unaffected at start of the observation, and also the immortal time bias is avoided. Remarkably, given the relatively short follow-up period after RRSO (2.5 years in the original analysis), the risk estimate remains (statistically nonsignificantly) decreased (hazard ratio [HR] = 0.50, 95% confidence interval [CI] = 0.20 to 1.25).
In a recent prospective analysis of EMBRACE, Mavaddat et al. (4) avoided all types of bias that we described (points 1 through 3) and showed a hazard ratio of 0.62 (95% CI = 0.35 to 1.09). It may be that the association between RRSO and first BC risk is not stable during follow-up, with limited BC risk reduction during the first years after RRSO and more decreased BC risk later on. The start of observation in the Mavaddat study was the date of baseline questionnaire, which was actually after the DNA test result and—for part of the participants—after undergoing RRSO. This way, Mavaddat et al. may have evaluated BC risk after a longer time period following RRSO, while we evaluated the first years after RRSO (mean observation period after RRSO = 4.9 years, range = 0.3 to 16.2),
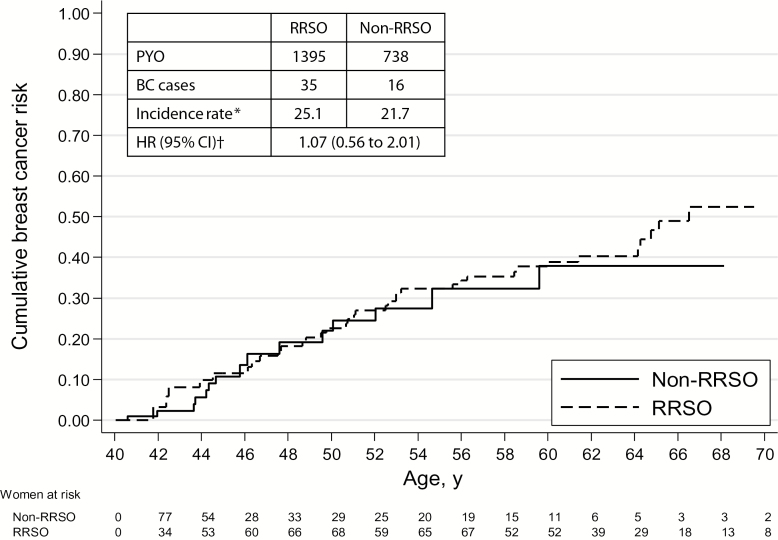
Concerning the issue of the graphical presentation of the cumulative BC risks in the RRSO group and the non-RRSO group, we like to dispel the misconception regarding the use of the landmark method. To graph the cumulative BC risk curves, we used the Simon and Makuch method (5), an alternative method of the landmark method (6). Still, we agree with the authors that the estimated curve of the RRSO group may be unstable because the numbers of carriers undergoing RRSO is very small at the beginning of the curve. Therefore, we reanalyzed the data starting the observation period at the age of DNA test result or the age of 40 years and estimated an HR of 1.07 (95% CI = 0.56 to 2.01) (Figure 1).
Figure 1.
Cumulative breast cancer risk curves for BRCA1/2 mutation carriers (≥40 years) selected from the Hereditary Breast and Ovarian Cancer Research Group Netherlands cohort opting for risk-reducing salpingo-oophorectomy (RRSO) vs not opting for risk-reducing salpingo-oophorectomy (non-RRSO). *per 1000 person-years of observation. †Univariate analysis. The observation period started at the age of DNA result or the age of 40 years, whichever came first. A robust variance-covariance estimation method was used to correct for nonindependence of observations in women from the same family. BC = breast cancer; CI = confidence interval; HR = hazard ratio; PYO = person-years of observation; RRSO = risk-reducing salpingo-oophorectomy.
In conclusion, because the reanalysis of the PROSE data still deviates from our approach with respect to the start of observation, the discussion regarding the influence of different methodological procedures on estimates of the association between RRSO and first BC risk is still ongoing. To facilitate better-tailored counseling regarding risk-reducing strategies, confirmation of the presence or absence of BC risk reduction after RRSO, particularly in relation to follow-up time afterwards, is warranted for BRCA1/2 mutation carriers. Besides larger study populations to improve power, consensus on the most appropriate start of observation in retrospective studies is definitely needed to obtain more conclusive results.
References
- 1. Domchek SM, Friebel TM, Singer CF, et al. Association of Risk-Reducing Surgery in BRCA1 or BRCA2 Mutation Carriers With Cancer Risk and Mortality. J Am Med Assoc. 2010;304 (9):967–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kauff ND, Domchek SM, Friebel TM, et al. Risk-reducing salpingo-oophorectomy for the prevention of BRCA1- and BRCA2-associated breast and gynecologic cancer: A multicenter, prospective study. J Clin Oncol. 2008;26 (8):1331–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Heemskerk-Gerritsen BAM, Seynaeve C, van Asperen CJ, et al. Breast Cancer Risk After Salpingo-Oophorectomy in Healthy BRCA1/2 Mutation Carriers: Revisiting the Evidence for Risk Reduction. J Natl Cancer Inst. 2015;107 (5):djv033 doi:10.1093/jnci/djv033. [DOI] [PubMed] [Google Scholar]
- 4. Mavaddat N, Peock S, Frost D, et al. Cancer Risks for BRCA1 and BRCA2 Mutation Carriers: Results From Prospective Analysis of EMBRACE. J Natl Cancer Inst. 2013;105 (11):812–822. [DOI] [PubMed] [Google Scholar]
- 5. Simon R, Makuch RW. A Non-Parametric Graphical Representation of the Relationship between Survival and the Occurrence of an Event - Application to Responder Versus Non-Responder Bias. Stat Med. 1984;3 (1):35–44. [DOI] [PubMed] [Google Scholar]
- 6. Dafni U. Landmark Analysis at the 25-Year Landmark Point. Circ Cardiovasc Qual Outcomes. 2011;4 (3):363–371. [DOI] [PubMed] [Google Scholar]