Abstract
Borderline personality disorder (BPD) is a barrier to treatment, yet the relationship between BPD features and other psychopathology symptoms in a residential addictions treatment samples is understudied. Using a sample of adults enrolled in a residential drug treatment facility measured at baseline and 2–3 month follow-up, we examined the prospective relationship between BPD features and five indices of psychopathology: depression, anxiety, interpersonal sensitivity, hostility, and psychoticism, as well as psychopathology global severity. There was no effect of time on any of the forms of psychopathology, but females reported higher levels of BPD features, anxiety symptoms, and interpersonal sensitivity than males. A series of latent change score models indicated that BPD features predicted increases in all psychopathology scales at follow-up, while the reverse was not true. These results suggest that targeting BPD features in residential drug treatment facilities may reduce the emergence of new psychopathology in the short-term.
Keywords: borderline personality disorder, longitudinal, residential, psychopathology
Borderline personality disorder (BPD) is a debilitating condition characterized by instability in a number of domains, including interpersonal and affective functioning, self-concept, and cognition (American Psychological Association [APA], 2000). It is a disorder of particular concern, as those with BPD engage in elevated levels of problematic behaviors, including gambling, binge eating, reckless driving, substance use, non-suicidal self-injury, and suicide attempts (APA, 2000; Coid, Yang, Tyrer, Roberts, & Ullrich, 2006; Crawford et al., 2005; Lenzenweger, Lane, Loranger, & Kessler, 2007; Torgersen, Kringlen, & Cramer, 2001). Moreover, those with BPD frequently present with comorbid psychopathology. BPD is associated with increased rates of anxiety, depression, dysthymia, antisocial personality, and substance use disorder (SUD) diagnoses (Becker, Grilo, Edell, & McGlashan, 2000; Grant et al., 2008; Pepper, Klein, Anderson, Riso, Ouimette, & Lizard, 1995; Trull, Sher, Minks-Brown, Durbin, & Burr, 2000; Zanarini et al., 1998a; Zanarini et al., 1998b; Zimmerman & Mattia, 1999).
Of these comorbidities, the relationship between BPD and SUDs is among the strongest. Indeed, the prevalence of BPD in residential addiction samples and psychiatric settings ranges from 20% to as high as 61.5% (APA, 2000; Bornovalova et al., 2008; DeJong, van den Brink, Harteveld, van der Wielen, 1993; Grilo et al., 1997). Compared to those without a BPD diagnosis, people who meet criteria for BPD are 5 to 10 times more likely to meet criteria for a lifetime drug or alcohol dependence diagnosis, and are 2 to 3 times more likely to develop a new SUD diagnosis than those with other personality disorders (Grant et al., 2008; Links, Heslegrave, Mitton, Vanreekum, & Patrick, 1995; Stepp, Trull, & Sher, 2005; Tragesser, Sher, Trull, & Park, 2007; Tragesser, Trull, Sher, & Park, 2008; Trull, Waudby, & Sher, 2004; Trull, Jahng, Tomko, Wood, & Sher, 2010). The issue of co-occurring disorders is a cause for concern, as those that meet criteria for BPD and a comorbid SUD exhibit a more severe and persistent course, higher rates of risk behavior and tertiary psychopathology (e.g., criminal, health risk, and suicidal behavior, anxiety, depression), worse treatment compliance, and elevated incidence of premature treatment termination and relapse than those diagnosed with BPD or a SUD in isolation (Bornovalova & Daughters, 2007; Darke, Ross, Williamson, Mills, Havard, & Teesson 2007; Gratz & Tull, 2011; Linehan et al., 1999; Links et al., 1995; Martinez-Raga, Marshall, Keaney, Ball, & Strang, 2002; Stone, 1990; van den Bosch, Verheul, Schippers, & van den Brink, 2002; Yen et al., 2003). Thus, BPD features are a barrier to the success of treatment. This is especially true for those with BPD in residential drug treatment centers, as these individuals have higher rates of comorbidity and greater treatment dropout (Tull & Gratz, 2012; Zanarini et al., 1998b).
Although the relationship between BPD and comorbid psychopathology in residential addictions samples is very well documented, two important limitations in this literature remain. First, this research has largely focused on long-term outcomes, such as relapse and treatment dropout (Bornovalova & Daughters, 2007; Darke et al., 2007; Linehan et al., 1999; Links et al., 1995; Martinez-Raga, Marshall, Keaney, Ball, & Strang, 2002; Stone, 1990; van den Bosch, Verheul, Schippers, & van den Brink, 2002; Yen et al., 2003). However, more proximal outcomes (e.g., depression, anxiety) in relation to BPD have been largely unexplored, despite the fact that they occur at rates ranging from 25% to 61% in residential treatment facilities and are 4.7 times more prevalent in addictions samples than in community samples (Hasin & Nunes, 1997; Huang et al., 2006; Kessler et al., 2003; Nunes, Sullivan, & Levin, 1997; Regier et al., 1990; Rounsaville et al., 1991). These findings have important implications for treatment settings, as many residential addictions facilities have begun to treat both SUDs and the comorbid psychopathology that may contribute to relapse (e.g., anxiety, depression; Harrison et al., 2008; Kosten, Rounsaville, Kleber, 1986; Moore, Young, Barrett, & Osborn, 2009; Willinger et al., 2002; Yong, Barrett, Engelhardt, & Moore, under review). It is possible that BPD features serve as an additional barrier to treatment due to their impact on the maintenance of these forms of comorbid psychopathology. The answer to this question has direct clinical applications for residential addition treatment settings. Indeed, if BPD features are contributing to an increase in comorbid psychopathology, treatment facilities may benefit from utilizing treatments that specifically target BPD features.
More broadly, the stability of BPD features over 2–3 months in residential addictions settings remains unexplored. While research has shown that BPD features may be less stable in terms of severity and expression than previously thought (Grilo et al., 2004), it is important to replicate this pattern among those in treatment for SUDs. In addition, existing research has mainly examined the long-term (e.g., 1–5 year follow-ups) relationships between BPD and comorbid psychopathology (Gunderson et al., 2006; Links, Heslegrave, Mitton, Vanreekum, & Patrick, 1995; Stepp, Trull, & Sher, 2005; Tragesser, Sher, Trull, & Park, 2007; Tragesser, Trull, Sher, & Park, 2008; Trull, Waudby, & Sher, 2004; Zanarini, Frankenburg, Hennen, & Silk, 2003). Of course, it is important to understand the BPD-psychopathology relationships over the course of several years. However, it is possible that the instability in functioning of those with BPD features may produce a distinct pattern of relationships in the shorter term, especially given the fact that BPD features and diagnoses can change in as little as 6 months (Grilo et al., 2004; Shea et al., 2002; Svartberg, Stiles, Seltzer, 2005). In other words, the instability in functioning for those with BPD features may lend itself to the development of psychopathology over a period of 4–5 years, but this possibility has yet to be tested with shorter time intervals.
Current Study
In the current study, we utilized a sample of men and women in a residential substance abuse treatment facility assessed at baseline and 2–3 month follow-up. First, we examined whether there were mean-level changes in BPD features and a number of psychopathological outcomes, including depression, anxiety, interpersonal sensitivity, hostility, and psychoticism, as well as an index of global severity, as a function of time and gender. Second, we used latent change score modeling to examine the relationship between initial levels of BPD and psychopathology and latent changes in their cross-lagged counterparts. As a function of recruiting participants from an active residential treatment setting, we predicted that mean levels of psychopathology and BPD features would decrease over time. Finally, consistent with previous research in community samples, we expected that BPD features would be longitudinally associated with greater changes in psychopathology and global severity (Grant et al., 2008).
Method
Sample
Participants included 235 adult (Mean age = 30.06; SD = 8.41) males and females (53% female) recruited at a residential substance abuse treatment facility in the greater Tampa Bay area. 69.4% of the participants identified themselves as Caucasian, 13.5% identified as Black/African American, and 17.1% identified as Hispanic/Latino. Most participants (66%) had a GED/high school diploma or below and 74.4% were reportedly single. Residents at the facility were eligible for participation in the research protocol after completing the first phase of treatment and thus, had not been using any substances for at least two weeks. Participants were considered ineligible if they met criteria for psychosis on the Mini-International Neuropsychiatric Interview for DSM-IV (MINI; Sheehan, et al., 1998), a semi-structured clinical interview. Participants first completed the baseline assessment, and subsequently completed the follow-up session approximately 2–3 months later while still enrolled in the treatment program. There was a variable interval between assessment points due to participant availability (M = 58.83; SD = 27.63). To control for this variability the follow-up variables were conditioned on time by regressing each variable on the number of days between assessments. This procedure has been used successfully in previous longitudinal research (Bornovalova et al., 2009; Hicks, Durbin, Blonigen, Iacono, & McGue, 2012). For each assessment, participants were compensated $20, which was deposited into their accounts at the facility. Assessments consisted of a battery of measures, both in survey and interview form by trained research assistants. The retention rate for follow-up was 79%. There were few differences between participants that completed both baseline and follow-up and those that completed only the baseline assessment in demographic variables (i.e., age, sex, marital/relationship status, ethnicity/race, SES, education) and psychopathology (ps > .05). The one exception to this was hostility [t(1) = 2.98, p = .003], with participants that only completed baseline reporting higher hostility (M = 3.60, SD = 3.81) than those that completed both baseline and follow-up (M = 2.08, SD = 2.74).
Measures
Diagnostic Status
To assess diagnostic status for psychopathology the Structured Clinical Interview for DSM-IV Axis II Disorders (First, Gibbon, Spitzer, Williams & Benjamin, 1997) for BPD and the MINI for depression (lifetime and current major depressive disorder), and anxiety disorders (lifetime panic disorder, current post-traumatic stress disorder, current generalized anxiety disorder) were administered at baseline.1 Rates of psychopathology were high at baseline, with 51.3%, 19.2%, 52.0%, and 46.7% of participants meeting criteria for BPD, current depression, lifetime depression, and any anxiety disorder, respectively. Two independent raters coded all diagnostic interviews for reliability. The inter-rater reliabilities, or kappas (κs), ranged from .74–1.0.
The Minnesota Borderline Personality Disorder Scale (MBPD)
The MBPD was used to examine BPD features (Bornovalova, Hicks, Patrick, Iacono, & McGue, 2011). The MBPD is a validated measure of BPD features that was developed using 19 items from the Multidimensional Personality Questionnaire (Tellegen, 1982), a well-validated measure of normative personality traits. Prior work has shown that the MBPD is moderately to highly associated with known correlates of BPD, including alcohol and substance use disorders, major depressive disorder, anxiety disorders, eating disorders, interpersonal problems, impulsivity and antisocial behaviors (Bornovalova et al., 2011; Bornovalova et al., 2012; Rojas et al., 2013; Rojas et al., under review). Further, there is substantial support for the MBPD representing a dimensional measure of BPD features, as it has shown strong correlations with other well-established dimensional measures of BPD, including the Inventory for Interpersonal Problems-BPD scale (IIP-BPD; Lejuez et al., 2003; Pilkonis, Yookung, Proietti, & Barkham, 1996), the Personality Assessment Inventory-Borderline scale (PAI-BOR; Morey, 1991), and with DSM-IV based BPD diagnostic interview (r = .80–.89 with PAI-BOR and estimated PAI-BOR; r = .60–.66 with DSM-IV diagnostics; r = .60 with IIP-BPD). These correlations are representative of both normative and clinical samples, including samples of substance users (Bornovalova et al., 2011; Bornovalova et al., 2012; Rojas et al., 2013; Rojas et al., under review). Items were coded as either true (1) or false (0) and were summed to attain a final score. Internal consistency of the MBPD was high for baseline (Cronbach’s alpha = .74) and follow up (Cronbach’s alpha = .75), as was test-retest reliability (r = .70).
Brief Symptom Inventory
To measure multiple domains of psychopathology, we utilized the Brief Symptom Inventory (BSI; Derogatis, 1983). The BSI is a self-report measure consisting of 53 items that is used to assess psychological distress in nine different dimensions, including somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism. The BSI has been shown to have high internal consistency and concurrent validity (Hathaway, & McKinley, 1951; Boulet and Boss, 1991). Items on the BSI are rated on 5-point scale that ranges from 0 to 4, with 0 signifying “never” and 4 “always”. One of the items on the anxiety subscale (“Feeling tense or keyed up”) and two on the hostility (“Feeling easily annoyed or irritated”, and “Having urges to beat, injure, or harm someone”) subscale overlapped with items on the MBPD (“There are days when I’m ‘on edge’ all of the time”, “Often when I get angry I am ready to hit someone”, and “Minor setbacks sometimes irritate me too much”). These items were removed from the anxiety and hostility scale, but not the MBPD to reduce the likelihood of obtaining inflated estimates of the association between the scales.
Given the similarity between the phobic anxiety, anxiety, somatization, and obsessive-compulsive scales, a composite was created by summing the subscale scores. A principal components analysis was conducted to ensure that all constructs represented the same anxiety factor. All factor loadings for baseline and follow up were greater than .88. Similarly, there was conceptual overlap between the psychoticism scale and the paranoid ideation scale. The principal components analysis revealed that both variables loaded onto the same psychoticism factor at baseline and follow-up (all factor loadings > .94). These composites will be referred to as anxiety and psychoticism throughout the text. Internal consistency at baseline (Depression = .88; Anxiety = .96; Interpersonal Sensitivity = .87; Hostility = .80; Psychoticism = .87) and follow-up (Depression = .84; Anxiety = .94; Interpersonal Sensitivity = .80; Hostility = .80; Psychoticism = .86) was high.
Data Analytic Strategy
We first utilized a series of repeated measures analysis of variance (ANOVA) to examine mean-level change in all study variables over time by gender, while controlling for socioeconomic status (composite of income and education status) and age (see Table 1 for means and standard deviations). After examining change in psychopathology, a series of latent change score models were fitted in R using the statistical package OpenMx (Boker et al., 2011) to examine the prospective relationships between baseline measures of BPD features and psychopathology and the changes that occur in these constructs across assessment points. This modeling technique allows one to examine the statistical properties of change in repeated measures assessments by removing the individual-level change in a construct that may be related to the initial level (McArdle, 2009). In other words, one is able to examine the effect of the initial level of one variable on a base-free measure of change in an alternative variable on a subsequent measurement occasion. A path diagram of the bivariate models utilized is presented in Figure 1.
Table 1.
Means and Standard Deviations by Gender
| Psychopathology | Time 1 | Time 2 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Males | Females | Combined | Males | Females | Combined | |
| BPD | 9.28 (4.50) | 10.93 (4.14) | 10.11 (4.43) | 9.11 (4.63) | 10.26 (4.61) | 9.71 (4.65) |
| Depression | 6.67 (6.50) | 7.99 (5.75) | 7.30 (6.15) | 5.39 (5.82) | 6.04 (5.01) | 5.82 (5.26) |
| Anxiety | 20.92 (18.81) | 29.19 (21.69) | 24.61 (20.49) | 17.14 (15.48) | 23.60 (17.28) | 20.98 (16.94) |
| Interpersonal Sensitivity | 5.14 (4.38) | 4.27 (4.29) | 4.72 (4.35) | 3.37 (2.17) | 4.30 (3.56) | 4.11 (3.82) |
| Hostility | 2.23 (3.00) | 2.78 (3.23) | 2.42 (3.07) | 2.02 (2.74) | 2.61 (2.94) | 2.38 (2.83) |
| Psychoticism | 9.87 (8.55) | 11.41 (8.66) | 10.44 (8.55) | 9.20 (7.74) | 10.14 (8.31) | 9.70 (8.09) |
| Global Severity Index | 55.04 (47.40) | 62.94 (56.06) | 58.47 (45.25) | 42.96 (39.40) | 53.11 (38.13) | 50.68 (38.47) |
Note: BPD = borderline personality disorder features.
Figure 1.
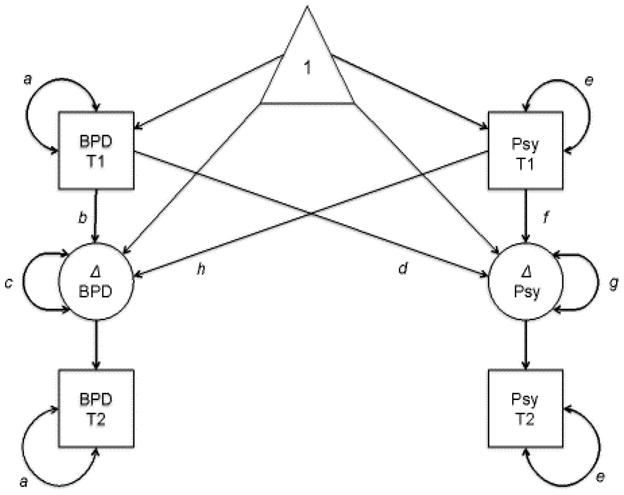
A descriptive latent change score model representing longitudinal relationships between borderline personality disorder features (BPD) and latent changes (Δ) in psychopathology (Psy) at baseline (T1) and follow-up (T2). Parameters a through h were analyzed in our model. Standardized path estimates, standard errors, and significance for each form of psychopathology are presented in Table 3. Paths from the constant (triangle) represent mean estimates with a standardized value of zero and are not included in Table 3.
We modeled a subsequent measurement (BPD T2) as the sum of an unobserved (latent) change variable (ΔBPD) and the initial value (BPD T1). By fixing the regression paths to 1, (i.e., BPD T2 = 1*BPD T1 + 1*ΔBPD), the latent change score (ΔBPD) is explicitly modeled as those sources of variation in the subsequent value (BPD T2) that are not identical to the initial value (BPD T1; McArdle & Nesselroade 1994). The b and f parameters in Figure 1 represent these regressions. The a and e parameters in Figure 1 define the variance of the initial values, while c and g represent the remaining error variance that contribute to the latent change scores (ΔBPD and ΔPsy). By adding a set of fixed unit values (=1) from the error to the latent change score (ΔBPD), we include the effect of the change score (ΔBPD) that is not accounted for by any part of initial scores (BPD T1) on the subsequent measurement (BPD T2). With this base-free measure of change, we examined the paths from the initial values (BPD T1 and Psy T1) to the unmeasured, latent changes (paths d and h in Figure 1). Each measure was also used as a single indicator for a latent variable at each time point, which included residualized error that was fixed to be equal across time 1 and time 2 scores. This allowed us to control for measurement error given the differences in reliability across the measure of BPD features and measures of psychopathology. Thus, we were able to disentangle the effects of two baseline measurements on a single subsequent measure of psychological functioning. This modeling technique allowed us to best represent the data and examine whether or not there were meaningful changes in psychopathology or BPD as a function of initial BPD features and psychopathology scores. Finally, we tested if these models fit differently for each gender, using a critical significance value of p < .01 due to conducting multiple tests of fit.
Results
Results from the repeated measures ANOVAs are presented in Table 2: there were no mean-level changes in BPD features or any outcomes over time. Gender differences were observed for several variables (Table 2). Females were higher than males on BPD features and anxiety at both time points. Females were also higher than males on interpersonal sensitivity at follow-up, but not baseline. Effect sizes for all gender differences were in the moderate range. There were no gender × time interactions.
Table 2.
Results of Repeated Measures ANOVAs for Change over Time by Gender
| Psychopathology | Time | Gender | Time X Gender |
|---|---|---|---|
| BPD | F(1) = 2.91, d = .29 | F(1) = 5.52, d = .41* | F(1) = .97, d = .17 |
| Depression | F(1) = .52, d = .14 | F(1) = 2.54, d =.30 | F(1) = 1.24, d =.21 |
| Anxiety | F(1) = .10, d =.06 | F(1) = 5.26, d =.43* | F(1) = 1.10, d =.19 |
| Interpersonal Sensitivity | F(1) = .08, d =.06 | F(1) = 8.87, d =.55** | F(1) = 1.71, d = .25 |
| Hostility | F(1) = .90, d =.18 | F(1) = .01, d = .00 | F(1) = 1.88, d = .016 |
| Psychoticism | F(1) = .004, d =.00 | F(1) = .55, d =.14 | F(1) = .52, d =.13 |
| Global Severity Index | F(1) = .16, d =.06 | F(1) = 3.80, d =.35 | F(1) = 2.33, d =.29 |
Note: Analyses were completed controlling for age and socioeconomic status. BPD = borderline personality disorder features;
p < .05,
p < .01.
Next, across all latent change score models, there were no gender differences in model fit (all Δχ2(1) < 4.04, all ps > .01). Thus, a latent change score model was fit for each outcome in relation to BPD features with path weights estimated for the entire sample. Table 3 presents the standardized estimates and standard errors for each parameter in our latent change score models by variable. The letters for each estimate represent the parameters presented in Figure 1. Significance level was set to p<.01 in all of our models to account for the large number of parameter estimates included. Initial level of BPD features was negatively related to latent changes in BPD features across all models, as represented by parameter b. This result was consistent across all forms of psychopathology as well, with a negative relationship between initial level of psychopathology and latent change in psychopathology. These results suggest that those highest in BPD features and psychopathology experienced fewer changes in their maladaptive functioning between baseline and follow-up than did those with less severe psychological symptoms. In terms of initial levels of BPD features and psychopathology predicting changes in one another, all models provided evidence that BPD features longitudinally predict changes in psychopathology. On the other hand, none of the initial values for psychopathology longitudinally predicted changes in BPD features. In other words, those high in BPD features predicted greater changes in symptoms of comorbid psychopathology, while those low in BPD features had fewer changes in symptoms of comorbid psychopathology.
Table 3.
Standardized Path Estimates and Standard Errors for Latent Change Score Models
| Path | Psychopathology
|
|||||
|---|---|---|---|---|---|---|
| Depression | Anxiety | Sense | Hostility | Psych | GSI | |
| a | 1.0 (.10)* | 1.0 (.10)* | 1.0(.10)* | 1.0(.10)* | 1.0(.10)* | 1.0 (.10)* |
| b | −.58(.11)* | −.58(.11) * | −.56(.11)* | −.58(.10)* | −.56(.12)* | −.59 (.11)* |
| c | .27(.03)* | .28(.03) * | .27(.03)* | .27(.03)* | .27(.03)* | .28 (.03)* |
| d | .24(.07)* | .33(.07) * | .27(.08)* | .29(.09)* | .35(.08)* | .35 (.07)* |
| e | 1.0(.10)* | 1.0(.10) * | 1.0(.10)* | 1.0(.10)* | 1.0(.10)* | 1.0 (.10)* |
| f | −.79(.08)* | −.79(.09)* | −.75(.09)* | −.66(.11)* | −.73(.09)* | −.79 (.08)* |
| g | .39(.05)* | .36(.04) * | .35(.04)* | .31(.04)* | .36(.04)* | .35 (.04)* |
| h | .20(.12) | .20(.14) | .13(.13) | .30(.13) | .10(.14) | .22 (.14) |
Note: Sense = interpersonal sensitivity; Psych = psychoticism; GSI = global severity index;
p < .01.
Discussion
The current study examined changes in BPD and psychopathology in an at-risk, residential addictions sample, as well as the longitudinal relationships between initial levels and changes in BPD and psychopathology. First, results indicated that rates of psychopathology remained stable over the follow-up period. This finding is consistent with research on the short-term temporal stability of the BSI subscales among healthy adults, which found no changes in subscale scores over time (Houghton et al., 2013). However, the lack of change in psychological symptoms is somewhat surprising, given that the participants were engaged in substance use treatment over the course of the assessment period, and drug treatment programs often alleviate secondary psychological distress (see e.g., Moos, Moos, & Andrassy, 1999). This particular treatment program may simply not be effective in delivering these benefits. Alternatively, participants enrolled in the current study may have been particularly unresponsive to treatment. Finally, consistent with previous reports, females had higher levels of BPD features, anxiety, and interpersonal sensitivity features than males.
The latent change score models revealed a pattern of interesting and consistent results. We found that across every one of the latent change score models BPD features at baseline longitudinally predicted changes in psychopathology. In contrast, none of the indices of psychopathology longitudinally predicted changes in BPD features. These findings suggest that the relationship between BPD features and psychopathology is unidirectional. In other words, BPD features are antecedents (as opposed to consequences) of symptomatic “flare-ups”, or short-term, isolated changes in psychopathology (e.g., depression symptoms), over the short-term in residential drug treatment facilities. These findings are consistent with evidence from long term studies, which suggest that BPD features predict the emergence of other psychopathology symptoms over a 6-year period (Bornovalova, Arango, Hicks, McGue, & Iacono, 2012; Gunderson et al., 2004; Gunderson et al., 2006; Zanarini, Frankenburg, Hennen, Silk, 2003). It is possible that BPD features predispose individuals to an unstable psychopathological profile in the short-term, which contributes to more permanent changes in their psychopathological features. Lastly, there were no gender differences in the latent change score models. These results suggest that while females and males might differ in their overall levels of psychopathology and pathological features, the relationships between indices of psychopathology and BPD features are largely consistent across gender.
Our findings from the latent change score models have clinical implications. In particular, results suggest that BPD features may function as a barrier to addictions treatment by facilitating flare-ups in psychopathology symptoms. This finding is consistent with previous work; for instance, a previous study reported that improvements in major depressive disorder were predicted by prior improvements in BPD features (Gunderson et al., 2004). Together, these results suggest that effective treatment of BPD features in addictions samples may lead to subsequent reductions in other forms of psychopathology and problem behavior. In turn, this may improve long-term outcomes such as resistance to relapse (Bradizza, Stasiewicz, & Paas, 2006). Alternatively, these results may suggest that symptoms of other forms of psychopathology are inherent in the BPD construct (e.g., suicidality and feelings of emptiness overlap BPD and depression), such that by treating BPD features, one is also treating problems characteristic of other disorders.
Despite the strong pattern of results, these findings are qualified by certain limitations. First, all data were obtained via self-report questionnaires. While self-reports for these constructs have been shown to represent levels of psychopathology accurately, research indicates that informant reports provide unique information in measuring Axis I and II psychopathology (Burt, Krueger, McGue, & Iacono, 2001; Burt, Krueger, McGue, & Iacono, 2001; Hopwood et al., 2008; Oltmanns & Turkheimer, 2009). Thus, future research would benefit from a multi-modal assessment (simultaneously collecting self-report, clinical interviews and informant reports) of BPD features and co-occurring psychopathology.
Second, these data were limited in that they were collected exclusively from adult participants (mean age = 30.06); as such, we cannot speak to questions of etiology or development. In other words, we are unable to determine whether BPD features or other types of psychopathology “came first”. Third, our sample only included waves of data at baseline and 2–3 month follow-up. While the results largely support a change in psychopathology as a function of BPD features in the short-term, future research would benefit from examining these changes using data collected at more than two time points. A sample with three or more occasions would allow one to determine the shape of change in these variables over the short-term, and would offer more predictive utility in examining change in psychopathology across various intervals of time.
Lastly, the data are limited in that the current measures differ in their psychometric – in particular, temporal stability - properties. Specifically, the items on the MBPD measure BPD features as a dispositional variable, whereas the BSI items ask participants to report on their psychopathology symptoms over the past week. These psychometric differences are reflected in the data, such that there is little variability and large stability in the MBPD and large variability and instability in the BSI subscales. This is a cause for concern, as it leaves little variance in the MBPD for the BSI scales to predict at follow-up. In other words, it is possible that, had measures with similar temporal stability been used, psychopathology symptoms would have predicted an increase in BPD symptoms. For instance, symptom-based measures of BPD (e.g., SCID-II, The Structured Interview for the DSM-III Personality Disorders) have stability coefficients that are comparable to coefficients of depression, anxiety, and other psychopathological features (Stangl, Pfohl, Zimmerman, Bowers, & Corenthal, 1985; Zanarini & Frankenburg, 2001). Future research would benefit from replicating these results with measures that ask participants to report on their symptom presentation across equal intervals of time.
Despite these limitations, the results provide important information regarding the observation of psychopathology over the short-term in a residential addiction sample. They offer important information in considering residential substance use treatment paradigms for those presenting with BPD features and comorbid psychopathology, particularly in understanding why some residents experience occasional psychopathology flare-ups. By using these results to modify current approaches to treatment in these samples, we may be able to greatly reduce the enormous healthcare burden of those presenting with this unique and problematic set of symptoms.
Footnotes
Diagnostic data were obtained solely at baseline.
Author Note: Data for this project were collected at the University of South Florida. All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. No conflict of interest exists for any of the authors.
References
- American Psychological Association. Diagnostic and statistical manual of mental disorders text revision. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Becker DF, Grilo CM, Edell WS, McGlashan TH. Comorbidity of borderline personality disorder with other personality disorders in hospitalized adolescents and adults. American Journal of Psychiatry. 2000;157:2011–2016. doi: 10.1176/appi.ajp.157.12.2011. [DOI] [PubMed] [Google Scholar]
- Boker S, Neale M, Maes H, Wilde M, Spiegel M, Brick T, … Fox J. OpenMx: an open source extended structural equation modeling framework. Psychometrika. 2011;76(2):306–317. doi: 10.1007/s11336-010-9200-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Daughters S. How does dialectical behavior therapy facilitate treatment retention among individuals with comorbid borderline personality disorder and substance use disorders? Clinical Psychology Review. 2007;27:923–943. doi: 10.1016/j.cpr.2007.01.013. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Gratz KL, Daughters SB, Nick B, Delany-Brumsey A, Lynch TR, Kosson D, Lejuez CW. A multimodal assessment of the relationship between emotion dysregulation and borderline personality disorder among inner-city substance users in residential treatment. Journal of Psychiatric Research. 2008;42:717–726. doi: 10.1016/j.jpsychires.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Arango A, Hicks BM, McGue M, Iacono WG. Longitudinal Influences of Co-Occurring Psychopathology on the Stability and Change of Borderline Personality Disorder Traits. Oral paper presented at the 26th meeting for Society for Research in Psychopathology. [Google Scholar]
- Bornovalova MA, Hicks BM, Iacono WG, McGue M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: A longitudinal twin study. Development And Psychopathology. 2009;21(4):1335–1353. doi: 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Patrick CJ, Iacono WG, McGue M. Development and validation of the Minnesota borderline personality disorder scale. Assessment. 2011;18(2):234–252. doi: 10.1177/1073191111398320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Huibregtse BM, Hicks BM, Keyes M, McGue M, Iacono W. Tests of a direct effect of childhood abuse on adult borderline personality disorder traits: A longitudinal discordant twin design. Journal of Abnormal Psychology. 2012 doi: 10.1037/a0028328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Iacano WG, McGue M. Longitudinal twin study of borderline personality disorder treats and substance use in adolescence: developmental change, reciprocal effects, and genetic and environmental influences. Personality Disorders: Theory, Research, and Treatment. 2012;4:23–32. doi: 10.1037/a0027178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt SA, Krueger RF, McGue M, Iacono WG. Sources of covariation among ADHD, CD, and ODD: The importance of shared environment. Journal of Abnormal Psychology. 2001;110:516–525. doi: 10.1037/0021-843X.110.4.516. [DOI] [PubMed] [Google Scholar]
- Burt SA, Krueger RF, McGue M, Iacono WG. Parent-child conflict and the comorbidity among childhood externalizing disorders. Archives of General Psychiatry. 2003;60:505–513. doi: 10.1001/archpsyc.60.5.505. [DOI] [PubMed] [Google Scholar]
- Bradizza CM, Stasiewicz PR, Paas ND. Relapse to alcohol and drug use among individuals diagnosed with co-occurring mental health and substance use disorders: A review. Clinical Psychology Review. 2006;26:162–178. doi: 10.1016/j.cpr.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Boulet J, Boss MV. Reliability and validity of the Brief Symptom Inventory. Psychological Assessment. 1991;3:433–437. [Google Scholar]
- Coid J, Yang M, Tyrer P, Roberts A, Ullrich S. Prevalence and correlates of personality disorder among adults aged 16 to 74 in Great Britain. British Journal of Psychiatry. 2006;188:423–431. doi: 10.1192/bjp.188.5.423. [DOI] [PubMed] [Google Scholar]
- Crawford TN, Cohen P, Johnson JG, Kasen S, First MB, Gordon K, et al. Self-reported personality disorder in the children in the community sample: convergent and prospective validity in late adolescence and adulthood. Journal of Personality Disorders. 2005;19:30–52. doi: 10.1521/pedi.19.1.30.62179. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Williamson A, Mills K, Havard A, Teesson M. Patterns and correlates of attempted suicide by heroin users over a 3-year period: Findings from the Australian Treatment Outcome Study. Drug and Alcohol Dependence. 2007;87:146–152. doi: 10.1016/j.drugalcdep.2006.08.010. [DOI] [PubMed] [Google Scholar]
- DeJong CAJ, van den Brink W, Harteveld FM, van der Wielen GM. Personality disorders in alcoholics and drug addicts. Comprehensive Psychiatry. 1993;34:87–94. doi: 10.1016/0010-440x(93)90052-6. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. The Symptom Checklist-90-R (SCL-90-R) 1975. [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological medicine. 1983;3:595–605. [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JB, Benjamin LS. User’s guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Grant B, Chou S, Goldstein R, Huang B, Stinson F, Saha T, … Ruan WJ. Prevalence, correlates, disability, and comorbidity of DSM–IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychology. 2008;69:533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Tull M. The impact of borderline personality disorder on residential substance abuse treatment dropout among men. Drug and Alcohol Dependence. 2011 doi: 10.1016/j.drugalcdep.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Martino S, Walker ML, Becker DF, Edell WS, McGlashan TH. Controlled study of psychiatric comorbidity in psychiatrically hospitalized young adults with substance use disorders. American Journal of Psychiatry. 1997;154:1305–1307. doi: 10.1176/ajp.154.9.1305. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Shea MT, Sanislow CA, Skodol AE, Gunderson JG, Stout RL, Pagano ME, Yen S, Morey LC, Zanarini MC, McGlashan TH. Two-year stability and change of schizotypal, borderline, avoidant and obsessive-compulsive personality disorders. Journal of Consulting and Clinical Psychology. 2004;72(5):767–775. doi: 10.1037/0022-006X.72.5.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunderson JG, Morey LC, Stout RL, Skodol AE, Shea MT, McGlashan TH, … Bender DS. Major depressive disorder and borderline personality disorder revisited: longitudinal interactions. Journal of Clinical Psychiatry. 2004;65(8):1049–1056. doi: 10.4088/jcp.v65n0804. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Weinberg I, Daversa M, Kueppenbender KD, Zanarini MC, Shea MT, Skodol AE, Sanislow CA, Yen S, Morey LC, Grilo CM, McGlashan TH, Stout RL, Dyck I. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. American Journal of Psychiatry. 2006;163(7):1173–1178. doi: 10.1176/ajp.2006.163.7.1173. [DOI] [PubMed] [Google Scholar]
- Harrison M, Moore KA, Young MS, Flink D, Ochshorn E. Implementing the Comprehensive, Continuous, Integrated Service of Care model for individuals with co-occurring disorders: Preliminary findings from a residential facility serving homeless individuals. Journal of Dual Diagnosis. 2008;4(3):238–259. [Google Scholar]
- Hasin DS, Nunes EV. Comorbidity of alcohol drug and psychiatric disorders: epidemiology. In: Kranzler HR, Rounsaville BJ, et al., editors. Dual diagnosis and treatment: substance abuse and psychiatric disorders. New York, NY: Marcel Decker, Inc; 1997. pp. 1–31. [Google Scholar]
- Hathaway SR, McKinley JC. Minnesota Multiphasic Personality Inventory manual (Revised) San Antonio, TX: Psychological Corporation; 1951. [Google Scholar]
- Hicks BM, Durbin C, Blonigen DM, Iacono WG, McGue M. Relationship between personality change and the onset and course of alcohol dependence in young adulthood. Addiction. 2012;107(3):540–548. doi: 10.1111/j.1360-0443.2011.03617.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood CJ, Morey L, Edelen M, Shea M, Grilo C, Sanislow C, … Skodol AE. A comparison of interview and self-report methods for the assessment of borderline personality disorder criteria. Psychological Assessment. 2008;20:81–85. doi: 10.1037/1040-3590.20.1.81. [DOI] [PubMed] [Google Scholar]
- Houghton F, Keane N, Lewis C, Murphy N, Houghton S, Dunne C. Temporal stability of the Brief Symptom Inventory 18 among Irish college students over four weeks. Social Behavior And Personality. 2013;41(2):197–198. doi: 10.2224/sbp.2013.41.2.197. [DOI] [Google Scholar]
- Huang B, Dawson DA, Stinson FS, Hasin DS, Ruan WJ, Saha TD, … Grant BF. Prevalence, correlates, and comorbidity of nonmedical prescription drug use and drug use disorders in the United States: results of the National Epidemiologic Survey on alcohol and related conditions. Journal of Clinical Psychiatry. 2006;67:1062–1073. doi: 10.4088/jcp.v67n0708. [DOI] [PubMed] [Google Scholar]
- Kessler KC, Berglund P, Delmer O, Jin R, Koretz D, Merikangas KR, … Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) Journal of American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kosten TR, ROunsaville BJ, Kleber HD. A 2.5-year follow-up of depression, life crises, and treatment effects on abstinence among opioid addicts. Archives of General Psychiatry. 1986;43:733–738. doi: 10.1001/archpsyc.1986.01800080019003. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Daughters SB, Nowak JA, Lynch T, Rosenthal M, Kosson D. Examining the inventory of interpersonal problems as a tool for conducting analogue studies of mechanisms underlying Borderline Personality Disorder. Journal Of Behavior Therapy And Experimental Psychiatry. 2003;34(3–4):313–324. doi: 10.1016/j.jbtep.2003.11.002. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Lane MC, Loranger AW, Kessler RC. DSM-IV personality disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;62:553–564. doi: 10.1016/j.biopsych.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM, Schimdt H, III, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialetical behavior therapy for patients with borderline personality disorder and drug dependence. American Journal of Addiction. 1999;8:279–292. doi: 10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Links PS, Heslegrave R, Mitton J, Vanreekum R, Patrick J. Borderline psychopathology and recurrences of clinical disorders. Journal of Nervous and Mental Disease. 1995;183:582–586. doi: 10.1097/00005053-199509000-00004. [DOI] [PubMed] [Google Scholar]
- Martinez-Raga J, Marshall E, Keaney F, Ball D, Strang J. Unplanned versus planned discharges from in-patient alcohol detoxification: Retrospective analysis of 470 first-episode admissions. Alcohol and Alcoholism. 2002;37:277–281. doi: 10.1093/alcalc/37.3.277. [DOI] [PubMed] [Google Scholar]
- McArdle JJ, Nesselroade JR. Structuring data to study development and change. In: Cohen SH, Reese HW, editors. Life-span Developmental Psychology: Methodological Innovations. Hillsdale, NJ: Erlbaum; 1994. pp. 223–267. [Google Scholar]
- McArdle JJ. Latent variable modeling of difference and changes with longitudinal data. Annual Review of Psychology. 2009;60:577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]
- Moore KA, Young MS, Barrett B, Ochshorn E. Twelve-month follow-up of integrated treatment for homeless individuals with co-occurring disorders. Journal of Social Service Research. 2009;4(35):1–14. [Google Scholar]
- Moos RH, Moos BS, Andrassy JM. Outcomes of four treatment approaches in community residential programs for patients with substance use disorders. Psychiatric Services. 1999;50(12):1577–1583. doi: 10.1176/ps.50.12.1577. [DOI] [PubMed] [Google Scholar]
- Morey L. Personality Assessment Inventory professional manual. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 5. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- Nunes EV, Sullivan MA, Levin FR. Treatment of depression in patients with opiate dependence. Biological Psychiatry. 2004;56:793–802. doi: 10.1016/j.biopsych.2004.06.037. [DOI] [PubMed] [Google Scholar]
- Oltmanns TF, Turkheimer E. Person perception and personality pathology. Current Directions in Psychological Science. 2009;18:32–36. doi: 10.1111/j.1467-8721.2009.01601.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper CM, Klein DM, Anderson RL, Riso LP, Ouimette PC, Lizard H. DSM-III-R axis II comorbidity in dysthymia and major depression. American Journal of Psychiatry. 1995;152:239–247. doi: 10.1176/ajp.152.2.239. [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Yookyung K, Proietti JM, Barkham M. Scales for personality disorders developed from the inventory of interpersonal problems. Journal of Personality Disorders. 1996;10(4):355–369. [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. Journal of American Medical Association. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Rojas E, Cummings J, Bornovalova MA, Hopwood C, Racine SE, Keel PK, Sisk CL, Neale MB, Burt AS, Klump KK. A Further Validation of the Minnesota Borderline Personality Disorder Scale. Personality Disorders: Theory, Research, and Treatment. doi: 10.1037/per0000036. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas E, Cummings J, Bornovalova MA, Hopwood C, Racine SE, Keel PK, Sisk CL, Neale MB, Burt AS, Klump KK. A Further Validation of the Minnesota Borderline Personality Disorder Scale. Personality Disorders: Theory, Research, and Treatment. doi: 10.1037/per0000036. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojas EC, Hicks BM, Stark S, Bornovalova MA. Elaborating on the Construct Validity of the MBPD: A Multi-sample, Longitudinal Examination. Psychological Assessment. doi: 10.1037/pas0000061. Under review. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Anton SF, Carroll K, Budde D, Prusoff BA, Gawin F. Psychiatric diagnoses of treatment-seeking cocaine abusers. Archives of General Psychiatry. 1991;48:43–51. doi: 10.1001/archpsyc.1991.01810250045005. [DOI] [PubMed] [Google Scholar]
- Shea MT, Stout R, Gunderson J, Morey LC, Grilo CM, McGlashan T, … Keller MB. Short-term diagnostic stability of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. American Journal of Psychiatry. 2002;159:2036–2041. doi: 10.1176/appi.ajp.159.12.2036. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan K, Amorim P, Janavs J, Weiller E, … Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- Stangl D, Pfohl B, Zimmerman M, Bowers W, Corenthal C. A structured interview for the DSM-III personality disorders: a preliminary report. Archives of General Psychiatry. 1985;42(6):591. doi: 10.1001/archpsyc.1985.01790290073008. [DOI] [PubMed] [Google Scholar]
- Stepp SD, Trull TJ, Sher K. Borderline personality features predict alcohol use problems. Journal of Personality Disorders. 2005;19:711–722. doi: 10.1521/pedi.2005.19.6.711. [DOI] [PubMed] [Google Scholar]
- Stone M. The fate of borderline patients: Successful outcome and psychiatric practice. New York, NY: Guilford Press; 1990. [Google Scholar]
- Svartberg M, Stiles TC, Seltzer MH. Randomized, controlled trial of the effectiveness of short-term dynamic psychotherapy and cognitive therapy for cluster C personality disorders. The American Journal of Psychiatry. 2005;161:810–817. doi: 10.1176/appi.ajp.161.5.810. [DOI] [PubMed] [Google Scholar]
- Tellegen A. Brief manual for the Multidimensional Personality Questionnaire. University of Minnesota; Minneapolis: 1982. Unpublished manuscript. [Google Scholar]
- Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Archives of General Psychiatry. 2001;58:590–596. doi: 10.1001/archpsyc.58.6.590. [DOI] [PubMed] [Google Scholar]
- Tragesser SL, Sher K, Trull TJ, Park A. Personality disorder symptoms, drinking motives, and alcohol use and consequences: Cross-sectional and prospective mediation. Experimental and Clinical Psychopharmacology. 2007;15:282–292. doi: 10.1037/10641297.15.3.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tragesser SL, Trull TJ, Sher K, Park A. Drinking motives as mediators in the relation between personality disorder symptoms and alcohol use disorder. Journal of Personality Disorders. 2008;22:525–537. doi: 10.1521/pedi.2008.22.5.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ, Sher KJ, Minks-Bown C, Durbin J, Burr R. Borderline personality disorder and substance use disorders: A review and integration. Clinical Psychology Review. 2000;20:235–253. doi: 10.1016/s0272-7358(99)00028-8. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Waudby C, Sher K. Alcohol and substance use disorders and personality disorder symptoms. Experimental and Clinical Psychopharmacology. 2004;12:65–75. doi: 10.1037/1064-1297.12.1.65. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Jahng S, Tomko R, Wood P, Sher K. Revised NESARC personality disorder diagnoses: gender, prevalence, and comorbidity with substance dependence disorders. Journal of Personality Disorders. 2010;24:412–426. doi: 10.1521/pedi.2010.24.4.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Gratz KL. The impact of borderline personality disorder on residential substance abuse treatment dropout among men. Drug and alcohol dependence. 2012;121(1):97–102. doi: 10.1016/j.drugalcdep.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Bosch L, Verheul R, Schippers G, van den Brink W. Dialetical behavior therapy of borderline patients with and without substance use problems: Implementation and long-term effects. Addictive Behaviors. 2002;27:911–923. doi: 10.1016/s0306-4603(02)00293-9. [DOI] [PubMed] [Google Scholar]
- Willinger U, Lenzinger E, Hornik K, Fischer G, Schönbeck G, Aschauer HN, Meszaros K. Anxiety as a predictor of relapse I detoxified alcohol-dependent patients. Alcohol and Alcoholism. 2002;37:609–612. doi: 10.1093/alcalc/37.6.609. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea T, Pagano M, Sanislow CA, Grilo CM, McGlashan TH, Skodol AE, … Morey LC. Axis I and Axis II disorders as predictors of prospective suicide attempts: Findings from the Collaborative Longitudinal Personality Disorders Study. Journal of Abnormal Psychology. 2003;112:375–381. doi: 10.1037/0021-843X.112.3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young MS, Barrett BA, Engelhardt M, Moore KA. Six-month outcomes of an integrated assertive community treatment team with a housing first approach serving adults with co-occurring substance use and mental health disorders who experienced long-term homelessness. Journal of Dual Diagnosis under review. [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. American Journal of Psychiatry. 1998a;155:1733–1739. doi: 10.1176/ajp.155.12.1733. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis II comorbidity of borderline personality disorder. Comprehensive Psychiatry. 1998b;39:296–302. doi: 10.1016/s0010-440x(98)90038-4. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR. Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Comprehensive psychiatry. 2001;42(5):369–374. doi: 10.1053/comp.2001.24556. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Silk KR. The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. American Journal of Psychiatry. 2003;160:274–283. doi: 10.1176/appi.ajp.160.2.274. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Mattia JI. Axis I diagnostic comorbidity and borderline personality disorder. Comprehensive Psychiatry. 1999;40:245–252. doi: 10.1016/s0010-440x(99)90123-2. [DOI] [PubMed] [Google Scholar]


