Abstract
Objective
Eating disorders (EDs) are serious problems among college-age women and may be preventable. An indicated on-line eating disorder (ED) intervention, designed to reduce ED and comorbid pathology, was evaluated.
Method
206 women (M age = 20 ± 1.8 years; 51% White/Caucasian, 11% African American, 10% Hispanic, 21% Asian/Asian American, 7% other) at very high risk for ED onset (i.e., with high weight/shape concerns plus a history of being teased, current or lifetime depression, and/or non-clinical levels of compensatory behaviors) were randomized to a 10-week, Internet-based, cognitive-behavioral intervention or wait-list control. Assessments included the Eating Disorder Examination (EDE to assess ED onset), EDE-Questionnaire, Structured Clinical Interview for DSM Disorders, and Beck Depression Inventory-II.
Results
ED attitudes and behaviors improved more in the intervention than control group (p = 0.02, d = 0.31); although ED onset rate was 27% lower, this difference was not significant (p = 0.28, NNT = 15). In the subgroup with highest shape concerns, ED onset rate was significantly lower in the intervention than control group (20% versus 42%, p = 0.025, NNT = 5). For the 27 individuals with depression at baseline, depressive symptomatology improved more in the intervention than control group (p = 0.016, d = 0.96); although ED onset rate was lower in the intervention than control group, this difference was not significant (25% versus 57%, NNT = 4).
Conclusions
An inexpensive, easily disseminated intervention might reduce ED onset among those at highest risk. Low adoption rates need to be addressed in future research.
Keywords: eating disorders, prevention, internet
Approximately 2-4% of young adults suffer from eating disorders (EDs) (Hudson, Hiripi, Pope, & Kessler, 2007) and many more young women suffer from “partial syndrome” or subclinical EDs. The peak age of onset is around 16 to 20 years of age, about the same time when many young women leave home and start college (Striegel-Moore et al, 2003). Unhealthful weight regulation practices and body image concerns, which predispose young women to clinical and subclinical EDS are common among high school and college students (Jacobi, Hayward, de Zwaan, Kraemer, Agras, 2004; Stice, 2002). In recent years, a number of potentially modifiable risk factors for EDs have been identified. Across populations and in longitudinal studies, excessive weight and shape concerns have been consistently associated with the onset of subclinical and clinical eating disorders (Jacobi et al 2004; Killen et al., 1996; Stice, 2002; Stice & Shaw, 2002; Taylor et al., 2006). Given their importance as a risk factor, many investigators have attempted to reduce weight and shape concerns. In a large, two-site prospective randomized controlled trial (RCT), an on-line cognitive-behavioral preventive intervention called StudentBodies™ was efficacious in reducing high weight/shape concerns and ED onset in at-risk women with (a) a body mass index ≥25 at baseline, and (b) any baseline compensatory behaviors (the effect of which emerged at only one study site) compared to a wait list control condition over three years (Taylor et al., 2006). Baseline compensatory behaviors were defined as self-induced vomiting, laxative use, diuretic use, diet pill use, or driven exercise endorsed at a frequency or duration below clinical or subthreshold DSM-IV-TR ED diagnostic criteria (i.e., less than 1 time per week or for less than three months). A secondary analysis of moderators of ED onset using data from this trial also showed that at 3-year follow-up, critical comments/teasing about eating from a teacher, coach, or sibling and lifetime depression were the most potent risk factors for ED onset (Jacobi et al., 2011). Combining results across the main outcome analyses and secondary analysis of moderators, approximately 50% of the participants in the previous trial met criteria for one of these three additional risk factors. Thus, the necessary next step was to develop a preventive intervention that would modify the risk factors associated with increased likelihood of ED onset (i.e., low, non-clinical levels of compensatory behaviors at baseline, critical comments/teasing about eating from a teacher, coach, or sibling, and lifetime depression). The population for whom this type of intervention would be relevant could be considered at very high risk for ED onset, as these are individuals presenting with the risk factor of weight/shape concerns as well as one or more of the three additional risk factors.
Accordingly, data from the previous trial suggest targeted intervention for individuals at very high risk may be beneficial for preventing ED onset and for conserving resources for those most in need, thus maximizing cost-benefit. Toward this end, Student Bodies™ was enhanced into Image and Mood (IaM)™, an indicated online preventive intervention aimed to address both the general ED risk factors (i.e., high weight and shape concerns) and the factors identified in our previous study that confer additional risk. The purpose of this study was to (1) evaluate the efficacy of IaM in preventing ED onset, (2) determine the intervention's impact on reducing ED risk, ED pathology, and associated comorbidities (e.g. depression) and (3) examine moderators of outcome to determine whether subgroups exist who may benefit from a more personalized intervention. Our study is one of the few RCTs to examine the effects of an intervention designed to impact moderators identified in a previous controlled trial and to address comorbid depression. Our primary hypothesis was that, compared to a usual care group, participants in the intervention condition would have a significantly lower incidence of EDs at two-year follow-up. Our secondary hypothesis was that, compared to a usual care group, participants in the intervention condition would have a significantly lower scores on measures of ED risk (as measured by the Weight Concerns Scale; WCS; Killen et al., 1996), ED pathology (as measured by the Eating Disorder Examination Questionnaire; EDE-Q; Fairburn & Beglin, 1994; 2008; Luce & Crowther, 1999), and on depression (as measured by the Beck Depression Inventory-II; BDI-II; Beck, Steer & Garbin, 1988). Analyses examining moderators of outcome were considered exploratory.
Method
Participants
Participants were women aged 18 to 25 at very high risk of developing an ED. The upper age cutoff was used to focus the sample on a peak time of ED onset, with the understanding that the college years may extend beyond age 22 for some individuals and but that few individuals experience an ED onset after age 25 (Striegel-Moore et al., 2003). Participants were potentially eligible to enroll in the study if they endorsed high weight/shape concerns [defined as scoring ≥47 on the WCS (Jacobi et al., 2004; Killen et al., 1996)] and endorsed at least one of three risk factors: history of critical comments/teasing about eating from a teacher, coach, or sibling, current or lifetime depression, and/or low, non-clinical levels of compensatory behaviors (Jacobi et al., 2011; Taylor et al., 2006). All three screening items were assessed as yes/no. Participants were excluded if they met criteria for a clinical or subclinical DSM-IV-TR ED (American Psychiatric Association, 2000), had been treated for an ED within the past six months, were actively suicidal or bipolar, or had psychotic symptoms. Participants were included if they had low levels of compensatory behaviors defined as having less than 1 compensatory behavior/week on average for 3 months (but more than zero episodes over this timeframe) and not, in other ways, meeting diagnosis of a subthreshold or clinical DSM-IV-TR ED. Individuals who were excluded for meeting criteria for a subthreshold or clinical ED were provided referral information for seeking services at their campus counseling center as well as treatment resources in the local community if this information was requested. Participants with a history of ED were included if they had not been treated in the past six months.
Participants were recruited mainly via study flyers and e-mails from 14 colleges and universities in the San Francisco and Saint Louis metropolitan areas. Recruitment materials advertised the study by saying, “Researchers are studying the benefits of a program on improving body image and healthy coping skills.” Recruitment materials also included information about compensation for completing assessments, contact information for the study research assistant, and information about how to contact the Institutional Review Board with any research-related questions about participants' rights as a study subject. The institutional review boards at all participating sites approved the study; all participants provided informed consent.
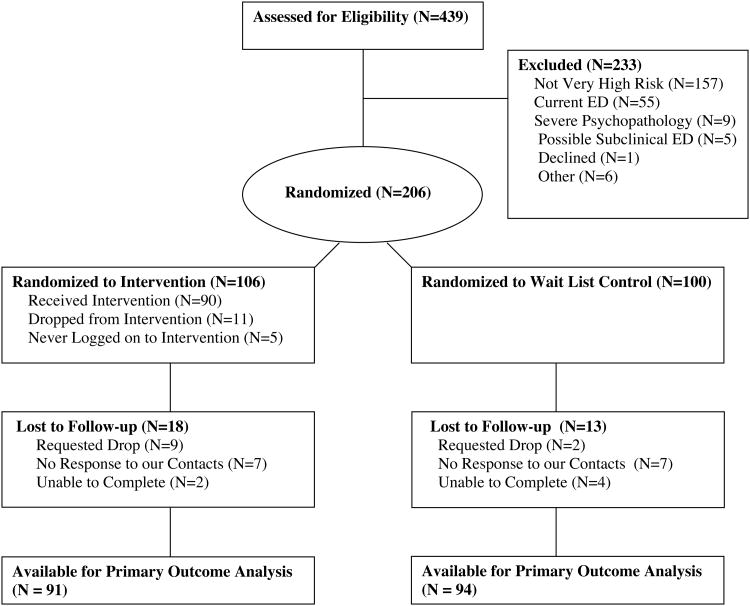
The study design was a RCT with 1:1 allocation to the online intervention or to a waitlist control condition. Participants with a history of an ED were stratified in the randomization across conditions, given the heightened risk for ED relapse in this subgroup. Randomization was performed using computer-generated random-number sequences in SPSS (SPSS Inc, Chicago, Il). An investigator at the data-coordinating site performed the randomization; this individual was not involved with assessments or intervention delivery. Assessors were blinded to participants' randomization condition. Participants were assessed at baseline, 3 months post-randomization, and at 1 and 2 years follow-up. Baseline assessments were conducted in person; follow-up assessments were conducted in person or by telephone to sustain retention among individuals who may have moved (e.g., after graduating college) over the study duration. Over 50% of follow-up assessments were conducted by telephone. Participants completed assessments between September, 2009 and April, 2012. Participants were paid $25 upon completion of each assessment; participants were not compensated for completing the intervention. Figure 1 presents a CONSORT flow diagram.
Figure 1. CONSORT Diagram for a Study Evaluating the Efficacy of an Online Intervention to Prevent the Onset of EDs among College-Age Women Compared to a Wait List Control.
Measures
The WCS was used to screen for “high risk” (score ≥47) (Jacobi, Abascal, & Taylor. 2004; Killen et al., 1996; Taylor et al., 2006). The WCS was derived from a principle components analysis of an extensive list of self-reported ED attitudes and behaviors (Killen et al 1993). The goal was to create a relatively brief, but psychometrically sound, instrument that did not overlap with other dimensions of ED pathology like purging, restraint, excessive exercise, and binge eating. The scale was found to have excellent stability (r = .71 for a 7-month interval and r =.74 for a 12 month interval; Killen et al., 1994 and 1996, respectively) and to be sensitive to treatment differences (Taylor et al., 2006). Jacobi et al (2004) used a ROC analysis to determine the best cut-off to distinguish those who developed an ED from those who did not. This analysis showed that a WCS criterion of ≥ 47 had a sensitivity of 79%, a specificity of 67% and a positive predictive value of 13%.
The EDE 12th Edition Diagnostic Version (Fairburn & Cooper, 1993; Rizvi, Peterson, Crow, & Agras, 2000) is a semi-structured interview that generates ED diagnoses based on DSM-IV-TR criteria. The EDE has good validity and inter-rater reliability (Cooper, Cooper & Fairburn, 1993; Vaught, Agras, Bryson, Crow, Halmi, Mitchell, 2008). The EDE was used for diagnosing EDs and assessing ED behaviors at baseline and follow-up. Additionally, at the 1-and 2-year follow-up assessments, a time-line follow-back method (Maisto, Sobell, Cooper & Sobell, 1982) was used to retrospectively assess ED attitudes and behaviors on a monthly basis over the past 12 months to calculate time to ED onset. The procedure began with an assessment of the past four weeks and then moved back, month-by-month, over the relevant assessment period using a calendar as a guide. The calendar included holidays, academic dates, and important personal events to prompt participants to the relevant timeframe. This approach has been shown to be reliable for measuring behaviors over the preceding year (Maisto et al., 1982); however, the validity of this approach for EDs has not been examined. Training in the EDE consisted of assessors reviewing an EDE training guide and then participating in an in-person training session with a trained assessor. Following the training, assessors listened to and co-rated two EDE interviews, observed an EDE assessment, and then were observed conducting two EDE assessments by a supervisor. Assessors were encouraged to note when they had trouble with scoring any behaviors (e.g., whether or not an episode constituted an objective binge episode), and these were then rated blindly by three observers, with the final coding based on consensus. Responses to the EDE were used to diagnose participants with a clinical ED or an eating disorder not otherwise specified (EDNOS) diagnosis. Individuals who endorsed criteria consistent with the following definitions were considered to meet criteria for a subthreshold ED (to align with the diagnostic criteria outlined in the DSM-IV-TR; American Psychiatric Association, 2004): (Criteria A) ≥12 objective bulimic episodes in the past three months or ≥8 objective bulimic episodes in the past month; (Criteria B) ≥12 episodes of purging in the past three months or ≥8 episodes of purging in the past month, or extreme dietary restriction or no eating at all outside of bulimic episodes; and (Criteria C) endorsement of shape and weight as one of or the main aspect of self-evaluation over the past three months. Purging was defined as self-induced vomiting, laxative misuse, diuretic misuse, or driven exercise. These definitions were also used to distinguish between individuals with full-syndrome EDs and those without full-syndrome EDs who endorsed compensatory behaviors at baseline (per our study entry criteria).
Depression and anxiety diagnoses were assessed at baseline with the Structured Clinical Interview for DSM-IV Axis I Disorders (First, Spitzer, Gibbon, & Williams, 2002). The EDE-Q (Fairburn & Beglin, 1994; 2008; Luce & Crowther, 1999) was used to measure changes in ED attitudes and behaviors. The EDE-Q has good internal consistency and test-retest reliability (.81 to .94 over two weeks; Luce and Crowther, 1999), and data suggest that the EDE-Q is highly correlated with the EDE for measuring global and subscale scores (Berg et al., 2012; Fairburn & Beglin, 1994). The Eating Disorder Inventory (EDI-2) (Garner 1991) Drive for Thinness and Perfectionism subscales were used to measure these domains. The EDI-2 has good test-retest reliability (.81 to .89 for the scales; Thiel & Paul, 2006). The Clinical Impairment Assessment (CIA; Bohn et al., 2008; Vannucci et al., 2012), a 16-item, self-report questionnaire designed to measure psychosocial impairment due to eating disorder features in the past 28 days, was used to assess psychosocial impairment due to ED pathology. The CIA has demonstrated high levels of internal consistency (Cronbach's alphas for the three subscales were 0.92, 0.85, and 0.86), test-retest reliability (one month intra-class correlation coefficient of 0.86), construct validity, and discriminant validity in community and clinical samples of young women (Bohn et al., 2008; Vannucci, et al., 2012). Participants also reported whether they sought treatment for an ED, for weight-related reasons, or for other psychiatric concerns.
Other measures included the BDI-II (Beck, Steer & Garbin, 1988), the State-Trait Anxiety Inventory (Spielberger, 1983), and four subscales of the Brief Cope (i.e., substance use coping, active coping, emotional support coping, and positive reframing; Carver, 1997). Participants reported the number of times in the past week and month they consumed four or more drinks in one sitting, as well as the number of drinks they typically consumed in one week (Wechsler, Davenport, Dowdall, Moeykens, & Castillo, 1994). Psychometric data are not available on this instrument.
Body mass index (BMI) at baseline was calculated based on objective height and weight measurements. Height was measured to the nearest millimeter using a calibrated stadiometer. Weight was measured to the nearest 0.1 kg using a digital scale. Participants were weighed by trained research assistants wearing lightweight indoor clothing without shoes or coats. Participants provided objective or self-report height and weight measurements at the follow-up assessments depending on whether they were assessed in person or via telephone, respectively.
All measures (except participant demographics) were assessed at all time points, with the EDE time-back method used only at the follow-up assessments.
Intervention
IaM was derived from StudentBodies,™ an 8-week, Internet-based, structured cognitive-behavioral program combined with an online, asynchronous, moderated discussion group (Beintner et al., 2012; Kass et al., 2014; Taylor et al., 2006). (Asynchronous means that participants could read and add comments to the Discussion Board at any time, 24/7. This is in contrast to a synchronous group in which participants would be invited to comment during a set-time frame in conjunction with a program moderator.) The main focus of the original program was to reduce weight and shape concerns, to teach healthy eating strategies, and to help participants stop or avoid any compensatory behaviors, based on cognitive-behavioral treatment strategies outlined by Fairburn (1995) such as self-monitoring, establishing a regular pattern of eating, decreasing dietary restraint, and cognitive restructuring. For this study, StudentBodies™ was expanded to 10 sessions and content was infused throughout the intervention to address the risk factors identified previously (Jacobi et al., 2011). To address the risk factor of “criticism about eating from a coach, teacher, or sibling” content was added throughout the program to help users better manage criticism from others, improve interpersonal functioning, and increase social support. Negative affect, as reflected in a history of or current depression, was addressed with a cognitive-behavioral approach using skills to improve affect regulation and increase social support, with added strategies from interpersonal psychotherapy. Participants were instructed on the cognitive theory of change and were taught to identify automatic thoughts via self-monitoring and behavioral skills (e.g., thought stopping, generating alternatives), behavioral activation (e.g., engaging in health-promoting, enjoyable activities), problem solving (e.g., time management, graded task breakdown), and stress management (e.g., relaxation training). Consistent with the focus on college-age women, content was included about coping with the transition to college (e.g., new environment, increased workload and expectations) and changes in interpersonal relationships (e.g., living with roommate, moving away from home). Individuals were also taught how to observe, describe, and label emotions, to identify precursors to problematic emotional responses, to reduce vulnerability to intense emotions (e.g., improving sleep patterns), to increase positive emotional events, and to change their emotional experience. Weekly symptom checklists were administered to all program users online via the intervention for participants to self-monitor ED behaviors and negative affect over the duration of the 10 week intervention; program moderators provided feedback at two time points during the intervention. These checklists were designed to help participants self-monitor their symptoms but were not used for data analysis purposes.
The 10-week intervention was administered to all participants in this condition, with sessions released once per week for 10 weeks. Participants were informed that each session would take an average of 30 minutes to complete (based on pilot data using IaM and past trials of Student Bodies). However, participants were also informed they could access the intervention at any time, by reviewing past content or the current week's materials, such that they were not limited to only 30 minutes. Participants were also encouraged to post at least once each week to the Discussion Board.
After program completion, monthly e-mail prompts were sent to participants for nine months to provide brief psychoeducation about ED pathology and maintaining cognitive-behavioral strategies and to remind participants about the ability to continue using the program over the course of the year.
Program Moderators
Program moderators sent emails announcing the release of new weekly program sessions and monthly booster sessions and monitored the Discussion Board daily. Specifically, program moderators logged in to the Discussion Board at least one time each day to ensure participants' postings were safe and appropriate; moderators also posted session-related questions once per week to the Discussion Board and commented on user responses to encourage continued dialogue among users. Postings were based on a manual from previous trials using Student Bodies.
Program moderators also compiled and e-mailed personalized feedback based on participants' symptom checklists two times over the 10 weeks of the program (i.e., following week 5 and week 10). Feedback aimed to reinforce participants' self-monitoring and help participants to reduce binge eating and compensatory behaviors and improve affect via the intervention. Participants were given positive reinforcement for areas in which they were doing well and were referred to specific aspects of the program to review content for areas in which they were struggling. Program moderators were graduate students in clinical psychology training programs, supervised by licensed clinical psychologists or psychiatrists. Program moderators tracked the time spent providing moderation or supervision.
Waitlist control condition
The waitlist control group was only contacted at the time of assessments and was offered the intervention at the end of the study, after the 2-year follow-up assessment was completed.
Data Analysis
The sample size was based on having 80% power to detect a 20% difference at 2 years, assuming 10% of intervention and 30% of the control participants would develop an ED during follow-up and that there would be a drop-out rate of 25% at follow-up. The rate of onset in the control population was estimated from Jacobi et al. (2011) and Taylor et al. (2006). Analyses were intent to treat. Intervention effects on weight, shape, and eating concerns (based on the WCS, EDE-Q, EDI, and CIA) and on comorbid pathology (based on the BDI-II, STAI, Brief Cope, and binge drinking) were examined with mixed effects models to account for the longitudinal data structure of multiple observation points across time nested within individual study participants. Cohen's d was calculated by dividing the mixed effects model derived intervention effect estimate by the pooled standard deviation of the particular measure at baseline.
Cox regression models were used to conduct the primary analysis assessing intervention effect on rate of ED onset during follow-up. All baseline measures were entered as potential moderators, including site (Kraemer, Wilson, Fairburn, & Agras, 2002). Potential intervention effect moderators were examined separately with Cox regression by entering the main effect of the potential moderator and the interaction effect (potential effect moderator × intervention condition) with ED onset as the dependent variable, controlling for study site. Variables significantly correlated with intervention condition at baseline were excluded from further moderation analyses. Number needed to treat (NNT), defined as the average number of participants who need to be treated to prevent one new case, was calculated for significant intervention effects.
Results
Participants
In total, 106 participants were randomized to the intervention condition and 100 to the control condition. Participants had a mean age of 20 years (SD = 1.8) at baseline. Baseline characteristics are presented in Table 1. The sample was 51% White/Caucasian, 11% African Amerian, 10% Hispanic, 21% Asian/Asian American, and 7% identified as an “Other” race or ethnicity. Approximately 35% of the sample endorsed only one of the three additional risk factors, 43% endorsed two risk factors, and 22% endorsed all three risk factors. There were no significant differences between conditions on any demographic variables. Of note, 6% subjects in the control group and 3.7% in the treatment group had a history of an ED but no treatment in the past 6 months. However, as the number of individuals with a history of an ED is small, we were unable to evaluate differences in rates of ED onset by intervention condition.
Table 1. Baseline characteristics.
| Intervention Condition (n=106) | Wait-list Control Condition (n=100) | |
|---|---|---|
| Age, years, mean (±SD) | 20.2 (1.8) | 20.5 (1.9) |
| BMI, mean (±SD) | 24.7 (4.6) | 25.3 (5.6) |
| Race/Ethnicity, n (%) | ||
| White/Caucasian | 67 (63.2%) | 38 (38.0%) |
| Black/African American | 14 (13.2%) | 9 (9.0%) |
| Hispanic/Mexican | 4 (3.8%) | 17 (17.0%) |
| Asian/Asian American | 14 (13.2%) | 29 (29.0%) |
| Mixed/Other | 7 (6.6%) | 7 (7.0%) |
| Parent Education, n (%) | ||
| Less than High School | 1 (0.9%) | 3 (3.0%) |
| High School Graduate | 4 (3.8%) | 5 (5.0%) |
| Some College | 29 (27.4%) | 21 (21.0%) |
| College Graduate | 21 (19.8%) | 17 (17.0%) |
| Some Graduate School | 1 (0.9%) | 2 (2.0%) |
| Graduate Degree | 49 (46.2%) | 52 (52.0%) |
| Do Not Know | 1 (0.9%) | 0 (0.0%) |
| History of an eating disorder, n (%) | 4 (3.8%) | 6(6.0%) |
| History of weight-related teasing*, n (%) | 89 (84.0%) | 72 (72.0%) |
| Current or past depression*, n (%) | 60 (56.6%) | 63 (63.0%) |
| Low-level compensatory behaviors*, n (%) | 58 (54.7%) | 45 (45.0%) |
Based on self-reported responses onthe entry screening tool
Of the 206 participants enrolled in the study, 21 (9.7%) were dropouts, defined as individuals who requested to drop out of the study or individuals for whom no follow-up data were available. There were no significant differences on baseline measures between dropouts and participants who remained in the trial. There were significant baseline differences between conditions in reported levels of coping by substance use. Specifically, intervention group participants endorsed higher levels of coping by substance use (difference = 0.47; 95% CI = 0.15-0.79; d = 0.40). Therefore, primary outcome analyses comparing intervention with control group outcomes were adjusted for baseline substance use coping.
Program Adherence
Eleven intervention participants dropped out of the intervention and five never logged on. Of the remaining 90 participants, 56% completed at least half of all intervention sessions (mean = 6.1; SD 2.4; range 1-10). Participants posted an average of 3.2 (SD = 4.5) posts to the Discussion Board.
Time Spent Moderating the Program
Program moderators spent an average of 48.8 minutes per participant implementing the program. The clinical supervisor spent about 15 minutes per week for 10 weeks to supervise a cohort averaging 18 participants. This translates to 8.3 minutes per participant of supervision time.
Based on current hourly moderator rates of $20 per hour, the cost per participant for moderation was $16.30. The supervisor was paid $80 per hour; thus, time for supervision was approximately $9.60 per participant. Accordingly, total cost per participant was $26.
Eating Disorder Risk Factors and Other Variables
Comparisons among participants who completed assessments at all time points (n = 133 to 138, depending on the measure) indicated the intervention had a significant effect on EDE-Q global score, with a between-group effect size of d = 0.31 (see Tables 2 & 3). The intervention group also had significantly greater reductions in EDE-Q Restraint and Weight Concern subscale scores, as well as EDI Drive for Thinness subscale scores, compared to the control group. There were no significant between group changes differences on other measures, including the WCS, the EDE-Q Eating Concern subscale, and the EDE-Q Shape Concern subscale. Comparisons among participants who completed assessments at all time points (n = 133 to 138, depending on the measure) indicated both groups had reductions in depressive symptoms, anxiety, and binge drinking (see Table 3). Analyses also revealed both groups evidenced improved coping, with the exception that using substances to cope increased slightly over time in the control group and decreased slightly over time in the treatment group (between-group d = 0.51; see Table 3).
Table 2. Outcomes for Participants in the Intervention Condition Compared to the Wait List Control Condition.
| Variable | Intervention(IaM) Mean (±SD) | Control (Wait List) Mean (±SD) |
|---|---|---|
| WCS | ||
| Baseline | 57.00 (15.10) | 59.40 (17.90) |
| Post | 51.20 (14.60) | 55.40 (16.30) |
| 1 year | 45.10 (17.70) | 50.20 (19.80) |
| 2 years | 42.90 (18.60) | 46.30 (19.40) |
| EDE-Q Restraint | ||
| Baseline | 2.30 (1.20) | 2.13 (1.20) |
| Post | 1.53 (1.20) | 1.87 (1.20) |
| 1 year | 1.14 (1.20) | 1.52 (1.30) |
| 2 years | 1.17 (1.10) | 1.52 (1.30) |
| EDE-Q Eating Concern | ||
| Baseline | 1.24 (1.10) | 1.24 (1.00) |
| Post | 0.79 (0.67) | 1.17 (1.00) |
| 1 year | 0.56 (0.59) | 0.75 (0.83) |
| 2 years | 0.50 (0.56) | 0.78 (0.92) |
| EDE-Q Weight Concern | ||
| Baseline | 3.11 (1.10) | 3.08 (1.40) |
| Post | 2.23 (0.97) | 2.70 (1.30) |
| 1 year | 1.96 (1.10) | 2.27 (1.30) |
| 2 years | 1.92 (1.20) | 2.19 (1.40) |
| EDE-Q Shape Concern | ||
| Baseline | 2.55 (1.20) | 2.85 (1.50) |
| Post | 1.97 (1.00) | 2.57 (1.40) |
| 1 year | 1.48 (1.00) | 2.12 (1.40) |
| 2 years | 1.58 (1.20) | 1.95 (1.40) |
| EDE-Q Global | ||
| Baseline | 2.29 (0.92) | 2.33 (1.10) |
| Post | 1.62 (0.77) | 2.09 (1.00) |
| 1 year | 1.26 (0.75) | 1.68 (1.10) |
| 2 years | 1.29 (0.82) | 1.62 (1.10) |
| EDI Drive for Thinness | ||
| Baseline | 3.67 (0.76) | 3.60 (0.94) |
| Post | 3.10 (0.80) | 3.48 (0.88) |
| 1 year | 2.95 (0.98) | 3.05 (1.00) |
| 2 years | 2.75 (0.95) | 2.94 (0.98) |
| EDI Perfectionism | ||
| Baseline | 4.21 (1.20) | 4.25 (1.00) |
| Post | 4.12 (1.30) | 4.28 (1.20) |
| 1 year | 4.27 (1.20) | 4.17 (1.10) |
| 2 years | 4.16 (1.20) | 4.22 (1.20) |
| CIA | ||
| Baseline | 10.00 (8.00) | 12.30 (9.10) |
| Post | 8.33 (7.10) | 10.50 (8.40) |
| 1 year | 4.31 (7.10) | 6.94 (9.10) |
| 2 years | 4.07 (6.70) | 6.36 (8.90) |
| COPE Active Coping | ||
| Baseline | 6.08 (1.60) | 5.97 (1.40) |
| Post | 6.16 (1.40) | 6.16 (1.50) |
| 1 year | 6.18 (1.60) | 6.60 (1.30) |
| 2 years | 6.33 (1.60) | 6.55 (1.30) |
| COPE Substance Use Coping | ||
| Baseline | 2.93 (1.60) | 2.39 (0.96) |
| Post | 2.76 (1.40) | 2.47 (0.95) |
| 1 year | 2.60 (1.10) | 2.45 (1.10) |
| 2 years | 2.78 (1.20) | 2.76 (1.40) |
| COPE Emotional Support Coping | ||
| Baseline | 5.59 (1.90) | 6.00 (1.90) |
| Post | 5.90 (1.80) | 5.95 (1.80) |
| 1 year | 6.34 (1.60) | 5.87 (1.80) |
| 2 years | 6.00 (1.80) | 6.08 (1.90) |
| COPE Positive Reframing Coping | ||
| Baseline | 5.60 (1.80) | 5.49 (1.80) |
| Post | 5.50 (1.70) | 5.53 (1.70) |
| 1 year | 5.55 (1.80) | 5.75 (1.60) |
| 2 years | 5.75 (1.60) | 6.00 (1.90) |
| BDI-II | ||
| Baseline | 9.20 (8.40) | 11.10 (9.20) |
| Post | 9.30 (8.30) | 9.30 (8.70) |
| 1 year | 7.70 (7.80) | 9.10 (9.00) |
| 2 years | 7.40 (6.19) | 8.30 (9.00) |
| STAI - State | ||
| Baseline | 41.60 (9.60) | 43.00 (8.90) |
| Post | 41.60 (10.8) | 42.60 (10.80) |
| 1 year | 39.20 (8.90) | 39.40 (9.50) |
| 2 years | 38.90 (9.10) | 40.40 (10.70) |
| STAI - Trait | ||
| Baseline | 42.10 (11.20) | 43.00 (12.40) |
| Post | 43.20 (12.40) | 43.20 (12.40) |
| 1 year | 40.20 (10.80) | 39.60 (12.70) |
| 2 years | 39.20 (11.20) | 39.50 (12.70) |
| Binge Drinking Episodes | ||
| Baseline | 2.08 (2.80) | 1.47 (2.30) |
| Post | 1.41 (2.10) | 1.42 (1.90) |
| 1 year | 1.64 (2.00) | 1.88 (2.60) |
| 2 years | 1.78 (2.40) | 1.61 (2.20) |
| BMI | ||
| Baseline | 24.00 (4.20) | 25.00 (5.50) |
| Post | --- | --- |
| 1 year | 24.50 (4.30) | 24.90 (5.40) |
| 2 years | 24.20 (4.70) | 24.90 (5.70) |
Note. WCS: Weight Concerns Scale; EDE-Q: Eating Disorder Examination - Questionnaire; EDI: Eating Disorder Inventory; CIA: Clinical Impairment Assessment; COPE: Brief Coping scales; BDI-II: Beck Depression Inventory-II; STAI: State-Trait Anxiety Inventory; BMI: Body Mass Index
Table 3. Estimated Effects of Intervention on Eating Disorder Risk Factors and Comorbidities.
| Intercept* (SE) | β (Intervention)** (SE) | t-score for β (Intervention) (df ≈ 201) | Effect size (d); p-value | |
|---|---|---|---|---|
| WCS | -8.31 (2.05) | -1.29 (2.86) | -0.45 | 0.08; .653 |
| EDE-Q | ||||
| Restraint | -0.41 (0.12) | -0.41 (0.17) | -2.37 | 0.36; .019 |
| Eating Concern | -0.29 (0.09) | -0.22 (0.13) | -1.72 | 0.22; .088 |
| Shape Concern | -0.56 (0.11) | -0.25 (0.16) | -1.54 | 0.20; .124 |
| Weight Concern | -0.66 (0.10) | -0.33 (0.15) | -2.21 | 0.27; .028 |
| Global Score | -0.48 (0.09) | -0.29 (0.13) | -2.32 | 0.31; .021 |
| EDI | ||||
| Perfectionism | -0.08 (0.07) | -0.01 (0.11) | -0.11 | 0.01; .915 |
| Drive for Thinness | -0.40 (0.07) | -0.21 (0.11) | -1.98 | 0.24; .049 |
| CIA | -4.26 (0.70) | 0.43 (0.99) | 0.44 | -0.11; .661 |
| COPE | ||||
| Active Coping | 0.50 (0.14) | -0.32 (0.20) | -1.59 | 0.21; .114 |
| Positive Coping | 0.36 (0.13) | -0.41 (0.21) | -1.97 | -0.24; .048 |
| Emotional Coping | -0.05 (0.16) | 0.49 (0.22) | 2.24 | 0.27; .026 |
| Subst. Use Coping | 0.30 (0.10) | -0.53 (0.18) | -2.99 | 0.42; .003 |
| BDI-II | -2.2 (0.63) | 0.54 (0.90) | 0.60 | 0.06; .549 |
| STAI | ||||
| State | -2.21 (0.87) | 0.74 (1.17) | 0.63 | -0.08; .528 |
| Trait | -2.11 (0.86) | 0.19 (1.13) | 0.17 | -0.02; .863 |
| Binge Drinking Episodes | ||||
| Binges, in last month | -0.09 (0.23) | -0.30 (0.30) | -1.02 | -0.11; .311 |
| BMI | -0.15 (0.22) | -0.02 (0.28) | -0.07 | 0.00; .947 |
Note.WCS: Weight Concerns Scale; EDE-Q: Eating Disorder Examination - Questionnaire; EDI: Eating Disorder Inventory; CIA: Clinical Impairment Assessment; COPE: Brief Coping scales; BDI-II: Beck Depression Inventory-II; STAI: State-Trait Anxiety Inventory; BMI: Body Mass Index
Intercept = Control group average difference between post-intervention assessment scores and baseline score, adjusted for baseline COPE substance use scores, study site, and baseline WCS scores.
β (Intervention) = Additive effect of intervention on average difference between post-intervention assessment scores and baseline score, adjusted for baseline COPE substance use scores, study site, and baseline WCS scores.
Effects of the Intervention on Eating Disorder Onset Rate
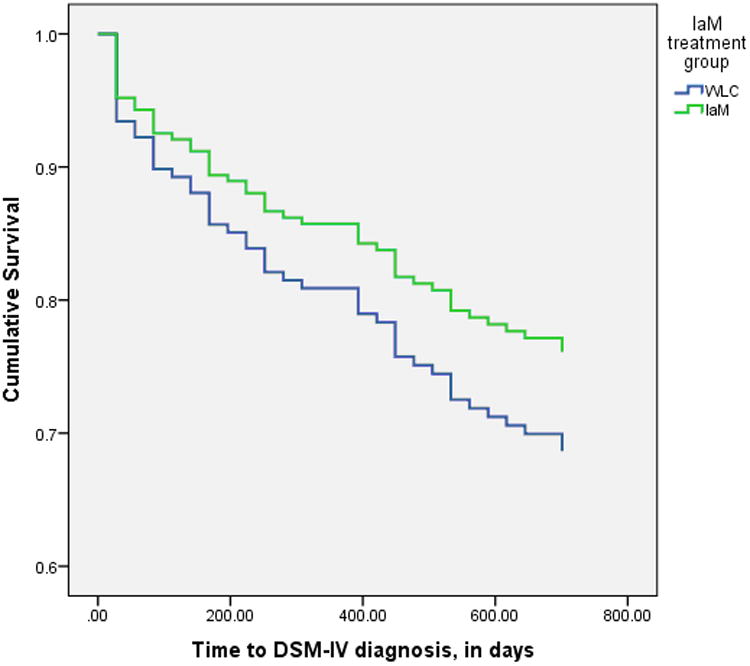
One- and/or two-year follow-up data were available for 185 participants (90%), with 51 participants (28%) becoming ED cases. In the intervention group, there were 22/91 (24%) new ED cases, all of whom met criteria for EDNOS. In the control group, there were 29/94 (31%) new ED cases, all of whom met criteria for EDNOS with the exception of one anorexia nervosa case (see Figure 2). The rate of ED onset was 27% lower in the intervention group (HR = 0.73; 95% CI = 0.41 to 1.29), although this difference was not statistically significant (p = 0.28; NNT = 15), controlling for study site and baseline substance use coping.
Figure 2. Survivalas a Non-eating Disorder Case for Participants in the Intervention vs Control Condition Through 2 Years.
To examine potential moderators, baseline variables that might theoretically affect outcomes were examined in univariate analyses (BDI-II, EDI, DERS, STAI-state and trait, ISI, Drinking, EDEQ scales and total, CIA, PSS and coping scales), in line with past research (Kraemer et al., 2002; Jacobi et al., 2011). Four variables demonstrated treatment moderation effects that were significant at a type one error rate of 0.05: BDI-II scores, p = 0.035; EDE-Q Weight Concern subscale scores, p = 0.031; EDE-Q Shape Concern subscale scores, p = 0.007, EDE=Q global score, p = 0.43; and Cope substance use, p = .012. Only the moderator effect of EDE-Q Shape Concern was significant at an alpha level of 0.01. Given the use of multiple testing, we decided to include only EDE-Q Shape Concern scores in further exploratory moderator analyses. Because we wanted a measure that might have some clinical relevance, we choose an EDE-Q cutoff score of >3.0, which indicates moderate to severe shape concerns, to identify a subgroup who may have been more likely to benefit from the experimental intervention using a standard item that is easily scored.
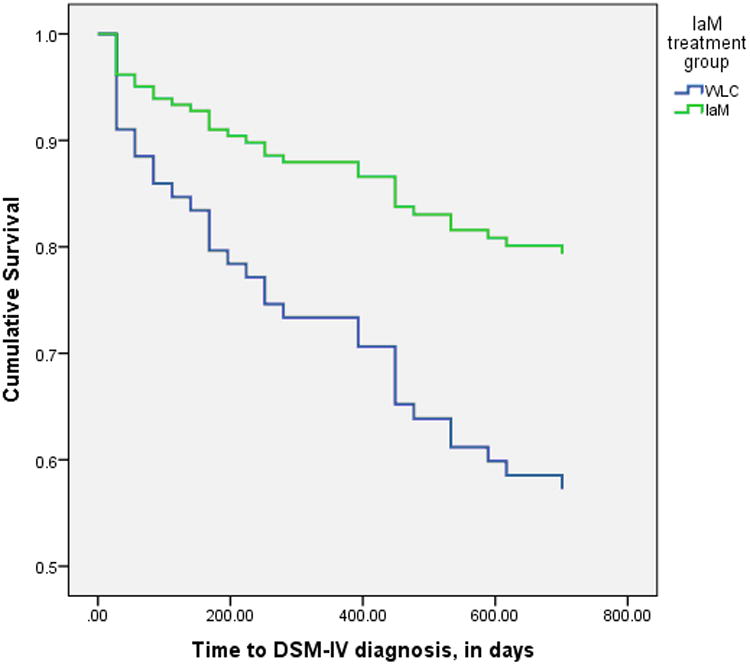
In the subgroup of 116 participants with EDE-Q Shape Concern scores >3.0, there were 107 (92%) with follow-up data, of whom 33 met criteria for ED onset during follow-up. Specifically, of the 33 participants who met ED onset criteria within this subgroup of 107 participants, 11/54 (20%) intervention and 22/53 (42%) control group participants met ED criteria during follow-up (NNT = 5). The rate of ED onset in this subgroup was 59% lower among intervention compared with control group participants (HR = 0.41; 95% CI = 0.19 to 0.88; p = 0.025), controlling for study site and baseline substance use coping (see Figure 3). The mixed effects model estimated effect of intervention on EDE-Q Shape Concern on average across post-intervention measures was significant (β = -0.52; SE = 0.21; t = -2.52; p = 0.013; d = 0.58). There was no significant relationship between adherence and EDE-Q scores at one year.
Figure 3. Survival as a Non-Eating Disorder Case for Participants at Very High Risk of Eating Disorders (56% of the Sample) in the Intervention vs Control Condition Through 2 Years.
Treatment-Seeking
Over two years, 13 intervention and 17 control group participants reported seeking face-to-face treatment for an ED or other psychiatric or weight-related problem. In the first year, 18 intervention and 17 control group participants reported using a self-help manual, videotape, or website.
Comorbid Depression among Intervention and Control Participants
At baseline, 99 participants endorsed current or lifetime depression, with 34 participants meeting criteria for ED onset during 2-year follow-up. Specifically, of these 34 participants who endorsed depression at baseline, 15/52 (29%) intervention and 19/47 (40%) control group participants developed an ED, a non-significant difference between the intervention and control groups (HR = 0.66; 95% CI = 0.33 to 1.32; p = 0.24). We also examined the effects of the intervention for the 27 individuals who were depressed at baseline. By 2-year follow-up, among the 22 (81%) participants who were depressed at baseline and with follow-up data, 2/8 (25%) intervention and 8/14 (57%) control group participants developed an ED (NNT = 4), a nonsignificant difference (HR = 0.34, 95% CI = 0.07 to 1.61; p = 0.17). In the subgroup of participants depressed at baseline, there was a significant intervention group effect on reduction in BDI-II scores, estimated with a mixed effects model adjusted for site (12.4 compared to 3.4 point reduction; β = -9.0; SE = 3.8; t = -2.38; p = 0.026; d = 0.96).
Discussion
This is one of the first studies to conduct a RCT targeting a sub-population at highest risk for a disorder based on previous risk factor analyses of a trial. We found that individuals who received an online preventive intervention had a significantly greater reduction in ED attitudes and behaviors (as measured by EDE-Q Global) than participants assigned to a wait list control condition over two-year follow-up, and the effect size of d = 0.31 was moderate in size, but there were no significant differences in ED onset (24% versus 31% in the intervention and control group, respectively). Also, the intervention did not produce significant-between group changes in most measures, including the WCS, the EDE-Q Eating Concern subscale, and the EDE-Q Shape Concern subscale. Exploratory moderator analyses revealed 56% of the full sample was at highest risk for ED onset, based on high shape concerns. In this sub-group with elevated EDE-Q Shape Concern scores with follow-up data, rate of ED onset was significantly lower in the intervention group (20%) compared to the control group (42%). Taken together, data from this study suggest the IaM intervention might be particularly beneficial for participants who present at very high risk for an ED and who also endorse high shape concerns (i.e., EDE-Q Shape Concern scores >3.0), although this would need to be confirmed in a randomized trial. Identification of high weight and shape concerns using two brief, self-report assessments (i.e., the Weight Concerns Scale, to determine scores ≥47, and the EDE-Q, to determine Shape Concern subscale scores >3.0) may be beneficial for streamlining screening procedures for delivering an indicated preventive intervention.
For primary outcome analyses of reducing ED onset, only two studies have demonstrated that a preventive intervention yields a significant reduction in rate of onset of EDs (Stice, Marti, Spoor, Presnell, & Shaw, 2008, Martinsen, Bahr, Børresen, Holme, Pensgaard, Sundgot-Borgen, 2014). In the Stice et al (2008) study, 481 adolescent girls (mean age 17 at baseline) were randomized to the primary dissonance-based preventive intervention, to one of two comparison intervention groups, or to an assessment-only control group. All intervention groups achieved about an equal effect at three years follow-up. Rates of ED onset were reduced from about 16% in the control group to about 7% in the treatment groups, with the NNT equaling about 11. In the Martinsen et al (2014) study, 464 first-year student athletes were randomized by school to a control or intervention condition. The intervention was based on social learning theory and was provided over the course of the school year. Among females, there were no new cases of ED in the intervention schools, while 13% at the control schools had developed and fulfilled the DSM-IV criteria for EDNOS or bulimia nervosa, with the NNT equaling about 8. In the current study, the NNT for the primary analysis was 15; if the intervention is delivered to the group at highest risk (i.e., with the study entry criteria plus EDE-Q Shape Concern scores >3.0), the NNT would be 5. These findings suggest that the primary outcome results of the current trial are not dissimilar from those from those obtained in the trial by Stice et al. (2008) (i.e., NNT = 15 versus 11) and indicate that conserving intervention delivery resources to those most in need (i.e., those at highest risk) would be the most cost-effective approach.
The present study was designed to determine if a RCT would confirm findings suggested from a moderator analysis (Jacobi et al., 2011; Taylor et al., 2008). Though often recommended, few studies attempt to examine moderator effects identified in previous randomized trials, making the current trial unique in its study design and aim. The moderators were combined both from Jacobi et al. (2011) and Taylor et al. (2006) and were used for power calculations in the current trial. Based on our power calculations, we assumed 10% of intervention and 30% of control participants would develop an ED during follow-up. The actual rate was 24% for the intervention and 31% for the control group, suggesting that the treatment group did not do as well as expected. One quarter onset among intervention participants represents a high proportion of the sample. Even among the subgroup of individuals with high shape concerns for whom the intervention was associated with significantly lower ED onset compared to the control condition, 20% of participants had an ED onset over two years. These findings suggest the intervention could be improved. Greater adherence, both to the program and at follow-up, might have improved outcomes. Although our rates of program adherence (i.e., with 56% of users who logged on or did not drop out completing half or more of the program) are similar to rates for manualized treatments for EDs delivered in person or online (Beintner, Jacobi, & Schmidt, 2014), more exposure to the program might have produced a greater effect. Importantly, future research should address problems with adoption and identify strategies to increase low adoption rates. For example, opportunities to increase program relevance and accessibility, such as through mobile platforms and tailored intervention content to specific risk or symptom profiles, may make the intervention more appealing to a college-age population, leading to enhanced adoption and retention. Advancements in Internet-based technologies that enable content tailoring based on programmed algorithms have the potential to increase capacity for personalized intervention. Most drop-outs occur in the first few sessions, so addressing user concerns early on might benefit outcome as well. Another strategy would be to carefully monitor students in prevention programs and refer to more intensive care when symptoms worsen (Jones et al., 2014; Wilfley, Agras, & Taylor, 2013). Also, the program might include even more intense interventions for those depressed at baseline, such as through tailored delivery based on presenting comorbid status. Improving the salience of the Discussion Board might also have been of benefit, given past results showing the clinical utility of this feature (Kass et al., 2014). In this sample, Discussion Board use was rather low, with participants posting an average only 3.2 (SD = 4.5) posts to the discussion board over the course of the intervention.
With that said, it is also possible that the main outcome findings were not significant given the high degree of improvement in the control group. Unlike previous trials (e.g. Taylor et al., 2006), the control group exhibited significant reductions in measures of weight and shape concerns and ED behaviors. The reasons for these differences in improvement are not clear, as the mean levels at baseline were similar to previous trials and participants were recruited in similar ways. Given the rising rates and severity of mental health problems in the college population (Hunt & Eisenberg, 2010), it is possible that campus wellness programming may have increased or other interventions might have become available in the time between our current and previous prevention trial, although our data suggest that participants did not use self-help and other programs.
It is also interesting to note that of the 22 intervention group participants who developed an ED, 11 participants had high Shape Concern scores, suggesting that 11 participants did not have high Shape Concern scores but still developed an ED. As this trial was an indicated prevention trial, we expected a proportion of individuals in both conditions would develop an ED over the two year study duration (as noted in our power calculation). Results from the moderator analysis suggest that endorsing constructs captured via the EDE-Q Shape Concern subscale that are not reflected in the WCS (such as a preoccupation with shape/weight, desire for a flat stomach, concerns with self or others seeing their body) may indicate heightened ED risk. However, the rates of ED onset observed in the 11 participants with low EDE-Q Shape Concern scores may be driven by having the other predisposing risk factors for ED onset that represented the study entry criteria. The effects of this exploratory analysis may also be due to chance given multiple tests of moderators, despite using a more conservative alpha threshold for detecting significance in the moderator analyses.
Although both groups showed overall improvements in symptoms of depression, anxiety, sleep, binge drinking, and coping, the intervention had a significant effect on reducing depressive symptomatology for individuals who were depressed at baseline, with a very large controlled effect size (d = 0.96). It is possible the added content infused throughout the program targeting interpersonal functioning and affect regulation was helpful for improving depressive symptomatology among this group (Rieger et al., 2010; Wilfley, Iacovino, & Van Buren, 2012). Furthermore, the rate of ED onset in individuals depressed at baseline in the intervention group was 18% compared to 50% in the controlled group, a large but non-significant difference (NNT = 4; p = 0.17). These findings are consistent with studies of clinical EDs that have shown depression and negative affect are highly comorbid with EDs (Eisenberg, Hunt, & Speer, 2013; Stice, 2001), and it is possible power was too low in this subgroup to detect a significant finding. However, it is critical to note that the effect size of needing to treat only four cases to prevent an ED has important clinical impact, especially given the low cost of the intervention. Concurrent interventions to treat or prevent depression relapse may increase the efficacy of ED prevention for individuals with a history of or current depression at baseline.
The cost of moderation was estimated to be $26 per participant. Assuming that 13 individuals would need to be treated to prevent one ED case, the cost for preventing a case would be about $338, not including indirect costs such as software use fees. Given that the intervention was most effective for the group with high shape concerns, a more effective use of resources might be to provide the intervention only to this subgroup, where treating five individuals can prevent one case, and to monitor the other half of the population for worsening of symptoms. In this approach, the cost to prevent one ED case would be $130, suggesting indicated intervention for ED prevention would reduce cost delivery.
A study limitation was the follow-up period was only two years. Previous moderator analyses used to model the effect of the intervention were based on 3-year follow-up data (Jacobi et al., 2011; Taylor et al., 2006). Significant overall differences might have been apparent at three years. Another limitation is the overall rate of ED onset was high for this population, and the intervention was somewhat less efficacious than anticipated. As suggested above, it may be important to address comorbidities more effectively than was done in this program, particularly on-going depression. Low adoption should be addressed in future research as well. Additional limitations include that the validity of the EDE time-back method has not been examined and there were no inter-reliability checks of the EDE. Finally, despite using a conservative significance threshold for the exploratory moderator analyses to reduce potential for observing chance findings, it is possible these findings are due to chance or that low power due to the lower incidence of EDs in the subgroup with EDE-Q Shape Concern scores ≤3 precluded detecting differences between the intervention and control groups, which would otherwise remove the effect of the exploratory moderator analysis. Strengths of the study are that the population was recruited from 14 colleges and universities in two states and was 49% non-White/Caucasian, suggesting results might be generalizable to a number of colleges and universities and to a wide range of individuals. However, it is important to note that recruitment from 14 universities may have resulted in inconsistent and/or low numbers of participants from each individual university, possibly introducing sample bias.
Taken together, these results suggest an online preventive intervention can prevent ED onset in individuals at highest risk for EDs (i.e., individuals at very high risk who also have elevated shape concerns), and the overall rates of NNT compare favorably to those demonstrated by the Stice et al., 2008 interventions. As the IaM™ intervention is relatively inexpensive to deliver and suitable for rapid dissemination given the accessible online format, this work informs efforts to expand indicated ED preventive care delivery through identifying opportunities that aim to personalize intervention, conserve resources for those at highest risk, and maximize costs. Our data also suggest the intervention reduces depressive symptomatology among individuals at high risk for EDs and with depression, although these results need to be replicated in a larger controlled trial.
Public Health Significance.
This study suggests that an on-line prevention program might reduce ED onset and reduce depressive symptomatology among college age women at highest risk of developing EDs.
Acknowledgments
Portions of this work were presented at the 16th Annual Meeting of the Eating Disorders Research Society, Boston, MA, USA and at the 20th Annual Meeting of the Eating Disorders Research Society, San Diego, CA, USA. We would also like to thank our consultants Drs. Alison Field and Ruth Weissman, as well as Dr. Ellen Fitzsimmons-Craft for her feedback on the manuscript and Danielle Ryu and Kristina Saffran for assistance with manuscript preparation.
Drs. Taylor and Wilfley receive funding from the National Institutes of Health, and research support for this trial was provided by R01 MH081125, K24 MH070446, T32 HL007456, and T32 HS000078. Dr. Wilfley receives consultation fees from Shire Phamaceuticals.
Footnotes
Declaration of interest: The other authors report no financial relationships with commercial interests.
Trial Registration: clinicaltrials.gov Identifier: NCT00934583
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th., text rev. Washington, D. C: 2000. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Reviews. 1988;8:77–100. doi: 10.1016/0272-7358(88)90050-5. [DOI] [Google Scholar]
- Beintner I, Jacobi C, Schmidt UH. Participation and outcome in manualized self-help for bulimia nervosa and binge eating disorder - a systematic review and meta-regression analysis. Clinical Psychology Reviews. 2014;34:158–176. doi: 10.1016/j.cpr.2014.01.003. [DOI] [PubMed] [Google Scholar]
- Berg KC, Peterson CB, Frazier P, Crow SJ. Convergence of scores on the interview and questionnaire versions of the Eating Disorder Examination: A meta-analytic review. Psychological Assessment. 2011;23:714–724. doi: 10.1037/a0023246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohn K, Doll HA, Cooper Z, O'Connor ME, Palmer KL, Fairburn CG. The measure of impairment due to eating disorder psychopathology. Behaviour Research and Therapy. 2008;46:1105–111. doi: 10.1016/j.brat.2008.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol's too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Cooper PJ, Fairburn CG. The validity of the eating disorder examination and its subscales. British Journal of Psychiatry. 1993;154:807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- Eisenberg D, Hunt J, Speer N. Mental health in American colleges and universities: Variation across student subgroups and across campuses. Journal of Nervous and Mental Disorders. 2013;201:60–67. doi: 10.1097/NMD.0b013e31827ab077. [DOI] [PubMed] [Google Scholar]
- Fairburn CB. Overcoming Binge Eating. New York City, New York: Guilford Press; 1995. [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorder psychopathology: Interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16:363–370. [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Cognitive Behavior Therapy and Eating Disorders. New York: Guilford Press; 2008. Eating Disorder Examination Questionnaire (6.0) [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment and Treatment. 12th. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York; Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Garner DM. EDI-2, Eating disorder inventory-2 Professional manual. 2. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 61:348–58. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. Journal of Adolescent Health. 2010;46:3–10. doi: 10.1016/j.jadohealth.2009.08.008. [DOI] [PubMed] [Google Scholar]
- Jacobi C, Abascal L, Taylor CB. Screening for eating disorders and high risk behavior: Caution. International Journal of Eating Disorders. 2004;36:273–288. doi: 10.1002/eat.20048. [DOI] [PubMed] [Google Scholar]
- Jacobi C, Fittig E, Bryson SW, Wilfley D, Kraemer HC, Taylor CB. Who is really at risk? Identifying risk factors for subthreshold and full syndrome eating disorders in a high-risk sample. Psychological Medicine. 2011;41:1939–1949. doi: 10.1017/S0033291710002631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for general taxonomy. Psychological Bulletin. 2004;130:19–65. doi: 10.1037/0033-2909.130.1.19. doi.org/10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]
- Jones M, Kass AE, Trockel M, Glass AI, Wilfley DE, Taylor CB. A population-wide screening and tailored intervention platform for eating disorders on college campuses: The Healthy Body Image program. Journal of American College Health. 2014;62:351–356. doi: 10.1080/07448481.2014.901330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kass AE, Trockel M, Safer DL, Sinton MM, Cunning D, Rizk MT, et al. Taylor CB. Internet-based preventive intervention for reducing eating disorder risk: A randomized controlled trial comparing guided with unguided self-help. Behaviour Research and Therapy. 2014;63:90–98. doi: 10.1016/j.brat.2014.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killen JD, Taylor CB, Hayward C, Haydel KF, Wilson DM, Hammer L, Strachowski D. Weight concerns influence the development of eating disorders: A 4-year prospective study. Journal of Consulting and Clinical Psychology. 1996;64:936–940. doi: 10.1037//0022-006x.64.5.936. Doi.org/1o.1037/0022-006X.64.5.936. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–83. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Luce KH, Crowther JH. The reliability of the Eating Disorder Examination-Self-Report Questionnaire Version (EDE-Q) International Journal of Eating Disorder. 1999;23:349–351. doi: 10.1002/(SICI)1098-108X(199904)25:3<349∷AID-EAT15>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Sobell LC, Cooper AM, Sobell MB. Comparison of two techniques to obtain retrospective reports of drinking behavior from alcohol abusers. Addictive Behaviors. 1982;7:33–38. doi: 10.1016/0306-4603(82)90022-3. doi.org/10.1037/0022-006X.47.1.106. [DOI] [PubMed] [Google Scholar]
- Martinsen M, Bahr R, Børresen R, Holme I, Pensgaard AM, Sundgot-Borgen J. Preventing eating disorders among young elite athletes: a randomized controlled trial. Medicine and Science in Sports and Exercise. 2014;46:435–47. doi: 10.1249/MSS.0b013e3182a702fc. [DOI] [PubMed] [Google Scholar]
- Rieger E, Van Buren DJ, Bishop M, Tanofsky-Kraff M, Welch R, Wilfley DE. An eating disorder-specific model of interpersonal psychotherapy (IPT-ED): Causal pathways and treatment implications. Clinical Psychology Reviews. 2010;30:400–410. doi: 10.1016/j.cpr.2010.02.001. [DOI] [PubMed] [Google Scholar]
- Rizvi SL, Peterson CB, Crow SJ, Agras WS. Test-retest reliability of the eating disorder examination. International Journal of Eating Disorders. 2000;28:311–316. doi: 10.1002/1098-108X(200011)28:3<311∷AID-EAT8>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Spielberger CD. State-Trait Anxiety Inventory. Palo Alto: Consulting Psychologists Press; 1983. [Google Scholar]
- Stice E. A prospective test of the dual-pathway model of bulimic pathology: Mediating effects of dieting and negative affect. Journal of Abnormal Psychology. 2001;110:124–135. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- Stice E. Risk and maintenance factors for eating pathology: a meta-analytic review. Psychological Bulletin. 2002;128:825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti CN, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:329–40. doi: 10.1037/0021-843X.110.1.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw HE. Role of body dissatisfaction in the onset and maintenance of eating pathology: A synthesis of research findings. Journal of Psychosomatic Research. 2002;53:985–993. doi: 10.1016/S0022-3999(02)00488-9. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Dohm FA, Kraemer HC, Taylor CB, Daniels S, Crawford PB, Schreiber GB. Eating disorders in white and black women. American Journal of Psychiatry. 2003;160:1326–1331. doi: 10.1176/appi.ajp.160.7.1326. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Bryson S, Celio Doyle AA, Luce KH, Cunning D, Abascal LB, et al. Wilfley DE. The adverse effect of negative comments about weight and shape from family and siblings on women at high risk for eating disorders. Pediatrics. 2006;118:731–8. doi: 10.1542/peds.2005-1806. [DOI] [PubMed] [Google Scholar]
- Taylor CB, Bryson S, Luce KH, Cunning D, Doyle AC, Abascal LB, et al. Wilfley DE. Prevention of eating disorders in at-risk college-age women. Archives of General Psychiatry. 2006;63:881–888. doi: 10.1001/archpsyc.63.8.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiel A, Paul T. Test-retest reliability of the Eating Disorder Inventory 2. Journal of Psychosomatic Rsearch. 2006;61:567–9. doi: 10.1016/j.jpsychores.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Vannucci A, Kass AE, Sinton MM, Aspen VA, Weisman H, Bailey JO, et al. Taylor CB. An examination of the clinical impairment assessment among women at high risk for eating disorder onset. Behaviour Research and Therapy. 2012;50:407–414. doi: 10.1016/j.brat.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaught AS, Agras WS, Bryson SW, Crow SJ, Halmi KA, Mitchell JE. Changes in psychopathology and symptom severity in bulimia nervosa between 1993 and 2003. International Journal of Eating Disorders. 2008;41:113–7. doi: 10.1002/eat.20464. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Davenport A, Dowdall G, Moeykens B, Castillo S. Health and behavioral consequences of binge drinking in college: A national survey of students at 140 campuses. Journal of the American Medical Association. 1994;272:1672–1677. doi: 10.1001/jama.1994.03520210056032. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Agras WS, Taylor CB. Reducing the burden of eating disorders: A model for population-based prevention and treatment for university and college campuses. International Journal of Eating Disorders. 2013;46:529–532. doi: 10.1002/eat.22117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilfley DE, Iacovino JM, Van Buren DJ. Interpersonal psychotherapy for eating disorders. In: Markowitz JC, Weissman MM, editors. The Casebook of Interpersonal Psychotherapy. New York: Oxford University Press; 2012. [Google Scholar]