Abstract
The Framingham Risk equation uses sex, age, smoking, total cholesterol, high-density lipoprotein (HDL) cholesterol and systolic blood pressure to predict 10-year risk of coronary heart disease (FR-10). The American Heart Association’s Ideal Cardiovascular Health (IDEAL) score uses smoking, total cholesterol, fasting glucose, blood pressure, body mass index (BMI), diet, and physical activity to encourage a healthy cardiovascular phenotype. This study aimed to compare 6-month changes in the FR-10 vs. IDEAL score among young adults with BMI ≥25 to <40 kg/m2 enrolled in a behavioral weight loss intervention at the University of Pittsburgh (2010–12). Medians [25th, 75th percentiles] are reported. Weight decreased by 8 kg [−12, −4] among 335 participants. Of 7 possible points, IDEAL score was 4 [3, 4] at baseline, improved (i.e., increased) by 1 [0, 2] over 6 months, and improved in 64.2% and worsened in 6.6% of participants (p<0.001). IDEAL classification of BMI, physical activity, total cholesterol, blood pressure and glucose improved (all p<0.001), but not of smoking or diet (both p≥0.05). FR-10 was <1% at baseline for 88.1% of participants and changed in few participants (improved, i.e. decreased, in 7.5%, worsened in 1.8%, p<0.001). Among young adults with overweight or obesity enrolled in a weight loss intervention, IDEAL detected positive changes in a majority of participants while the FR-10 did not. These findings suggest that IDEAL score may be more sensitive to positive cardiovascular health changes resulting from a behavioral intervention in this population.
Keywords: prevention, lifestyle, obesity, risk factors, young adults, cardiovascular health
INTRODUCTION
In 2010, the Strategic Impact Goal statement from the American Heart Association defined a ‘new concept, cardiovascular health,’ which is measured using a seven-item composite score of modifiable health behaviors (smoking, physical activity, diet, and obesity) and clinical risk factors (blood pressure, total cholesterol, and fasting glucose).(Lloyd-Jones et al., 2010) Each component has a threshold which is considered ‘ideal,’ i.e., the most healthy classification. There are also intermediate and poor classifications. This new concept promotes primordial prevention, which is a preventative strategy that targets risk reduction at the population level by preventing risk factors for disease rather than the disease itself. Subsequent reports have supported that the ‘Ideal Cardiovascular Health’ (IDEAL) score predicts future cardiovascular disease outcomes.(Folsom et al., 2011; Laitinen et al., 2012; Yang et al., 2012)
The Framingham Risk Score equation is a standard clinical tool used to predict the 10-year risk of coronary heart disease (FR-10) based on sex, age, total cholesterol, high-density lipoprotein (HDL) cholesterol, systolic blood pressure, and smoking,(2001) with the goal of its implementation being primary prevention of disease. The Framingham Risk equation has demonstrated utility for coronary heart disease risk prediction across diverse populations.(D’Agostino et al., 2001) Yet, because age does not contribute substantially to the score among younger people who also typically have few or no laboratory or clinical risk factors, it may not be a useful measure to demonstrate improvement in younger people who may have a low baseline score. It may be, therefore, that a measure like the IDEAL score, which includes more behaviors that are associated with cardiovascular disease, is more useful than the Framingham risk classification to assess cardiovascular health changes in young people.
The purpose of this study was to compare changes in the IDEAL score and FR-10 in young adults with overweight or obesity at low risk of coronary heart disease during the first 6-months of a behavioral weight loss trial.
Methods
Participants and Setting
This analysis used data from 335 participants enrolled in the Innovative Approaches to Diet, Exercise, and Activity (IDEA) Study, a 2-year, randomized, behavioral weight loss intervention for overweight or obese young adults described in detail elsewhere.(Jakicic et al., 2015) Basic inclusion criteria included age 18–35 years and body mass index (BMI) between 25.0 to <40.0 kg/m2. Participants were excluded for the following: past or planned weight loss surgery; recent weight loss >5%; currently pregnant, gave birth in the past 6 months or lactating within the past 3 months; use of medications that could affect metabolism, heart rate, or responses to exercise; treatment for psychological issues or use of psychotropic drugs; use of hypertension or diabetes medications; resting blood pressure ≥ 160 mmHg (systolic) or ≥ 90 mmHg (diastolic); or any history of heart disease, angina, heart attack, stroke, or cancer.
Although participants were randomized to one of two intervention arms, all participants received the same behavioral weight loss intervention for the first 6 months.(Jakicic et al., 2015) Briefly, participants attended weekly group meetings and received a prescription to decrease caloric intake (1200–1800 kilocalories/day) and progressed to 300 minutes/week of moderate-to-vigorous intensity physical activity (MVPA) with a goal to achieve a 10% weight loss over 2 years. To be included in this analysis comparing 6-month changes in the IDEAL score vs. FR-10, participants had to have complete baseline and 6-month data for all variables in the cardiovascular risk scores (described below).
Measurements
Smoking habits and sex were self-reported. Age was confirmed using government-issued identification. BMI was calculated as kg/m2 with weight measured by a calibrated, digital scale and height measured using a wall-mounted stadiometer in bare feet and wearing a lightweight hospital gown. Body fat (%) was measured by a total body scan with a GE Lunar iDXA dual-energy x-ray absorptiometer (Lunar, Inc). Cardiorespiratory fitness was evaluated by a graded, exercise test to 85% of age-predicted maximal heart rate (calculated as 220 bpm minus age). The test used a standardized protocol on a motorized treadmill on which participants began at 0% grade and 80.4 meters/minute and grade was increased by 1% every minute until the target heart rate was achieved. A Vmax® Encore metabolic cart (CareFusion, San Diego, CA) measured oxygen consumption (VO2 85%) in mL/kg·min at the point of test termination. Blood pressure was the average of two automated measures that differed by <10 mmHg for systolic blood pressure and ≤6 mmHg for diastolic blood pressure taken after a 5-minute rest period. Blood samples were obtained at each visit after a confirmed, 12-hour fast. Glucose, total cholesterol, and high density lipoprotein (HDL) cholesterol were measured by standard methods.(Allain et al., 1974; Bondar and Mead, 1974; Bucolo and David, 1973; Friedewald et al., 1972)
Dietary intake was evaluated by the Dietary History Questionnaire II, a validated food frequency questionnaire developed by the National Cancer Institute that assesses frequency and amount of foods consumed over the past month.(Thompson et al., 2002) DietCalc software (version 1.5.0) was used to analyze the data.
MVPA participation was determined by objective measurement with a SenseWear Armband (SWA) (BodyMedia, Inc.) that did not provide feedback to participants. The SWA is a small, multi-sensor device worn on the midline of the triceps with an elastic band that captures acceleration along with heat flux, skin temperature, and galvanic skin response. Participants were instructed to wear the armband at all times for 7 days except when bathing, swimming, or sleeping. Data were included if participants had ≥10 hours/day of wear time on ≥4 days. The SWA has been validated for assessing free-living, total energy expenditure using doubly labelled water as the gold standard, with recent studies showing correlations ranging from 0.73–0.89.(Johannsen et al., 2010; Koehler et al., 2011; Mackey et al., 2011) Data were processed using proprietary algorithms provided by the manufacturer (SenseWear Professional version 7.0) that give estimates of energy expenditure for each minute of wear time, which were converted to metabolic equivalents (METs). Moderate intensity physical activity (MPA) was defined as activity with an intensity of ≥3 to <6 METs and vigorous intensity physical activity (VPA) as activity with an intensity of ≥6 METs. Only MVPA accumulated in bouts of ≥10 minutes was considered, which is consistent with current physical activity recommendations.(United States. Department of Health and Human Services., 2008) In addition, self-reported MVPA performed in bouts of ≥10 minutes was assessed by the Global Physical Activity Questionnaire.(Bull et al., 2009)
The IDEAL score was computed as the sum of the 7 components in which the ideal threshold was met (i.e., 1 point for each; score range: 0 to 7)(Lloyd-Jones et al., 2010): 1) never smoked or quit ≥12 months ago, 2) BMI <25 kg/m2, 3) meeting ≥4 of 5 dietary components (≥2 servings/week of fish, <36 oz/week of sugar-sweetened beverages, ≥3 oz/day of whole grains, ≥4.5 cups/day of fruits and vegetables, and <1500 mg/day of sodium), 4) minutes of MPA plus 2 times minutes of VPA ≥150 minutes/week (2009), 5) blood pressure <120/80 mmHg without antihypertensive medication, 6) fasting glucose <100 mg/dL without glucose-lowering medication, and 7) total cholesterol <200 mg/dL without lipid-lowering medication. Because some recommendations use a higher cutoff for sodium intake (e.g. Institute of Medicine (Bibbins-Domingo, 2014)), a sensitivity analysis examined the effects of changing the upper limit of sodium intake to <2300 mg/day. Also, because some researchers have criticized the use of objectively-monitored MVPA since physical activity recommendations were largely based on self-reported data (Cowell, 2010), self-reported recreational and transportation MVPA from the Global Physical Activity Questionnaire replaced the objectively-measured MVPA in a second sensitivity analysis. Lastly, an alternative IDEAL score (IDEAL14) was computed by assigning 2 points for each component classified as ‘ideal’ (above) and 1 point for each component that met an intermediate classification (i.e., former smoking of ≤ 12 months; BMI 25–<30 kg/m2, meeting 2–3 of 5 dietary components; 1–149 minutes/week of MVPA as defined above; blood pressure 120–139/<90 mmHg without antihypertensive medication or treated to goal; fasting glucose 100–125 mg/dL without glucose-lowering medication or treated to goal; total cholesterol 200–239 mg/dL without lipid-lowering medication or treated to goal).(Lloyd-Jones et al., 2010) The FR-10 was calculated as the individual risk (%) of coronary heart disease in the next 10 years using published regression equations.(2001)
Statistical Analysis
Because both intervention groups in the IDEA Study received an identical intervention for the first 6 months, results are reported for the groups combined. All continuous variables were checked for normality and nonparametric statistics were used when appropriate. Descriptive statistics (frequencies and percentages, medians [25th and 75th percentiles], minima and maxima) summarized baseline characteristics.
Because only 2% of participants (n=6) had a FR-10 of >1% at either time point, values of 1% or greater were collapsed for comparison across time. Statistical significance of baseline to 6 months changes were assessed with the McNemar’s test of marginal homogeneity for dichotomous variables (i.e., FR-10 <1% vs. ≥1% and components of the IDEAL score), the Bowker’s test of marginal homogeneity for categorical variables (i.e., IDEAL score) and the Wilcoxon signed-rank test for continuous variables (i.e., behavioral intervention targets and cardiovascular risk factors). Association between changes in the IDEAL score and FR-10 were evaluated with Spearman’s correlations.
Analyses were conducted using SAS version 9.3 (SAS Institute). All reported p-values are two-sided; p-values less than 0.05 are considered to be statistically significant.
Results
Of 470 participants enrolled, 335 were included in the current analysis (Table 1). Of those excluded, 46 did not complete the 6-month follow-up visit and 89 were missing at least one component of at least one of the risk scores at baseline or 6 months. For those attending visits, missing MVPA was the most commonly missing component (n=13 at baseline, n=30 at 6 months).
Table 1.
Baseline Characteristics of Participants (n=335)
| Gender | ||
| Male | 106 | (31.6%) |
| Female | 229 | (68.4%) |
| Age, years, median (25th, 75th percentile) | 30.9 | (27.4, 33.7) |
| Race | ||
| White | 273 | (81.5%) |
| Non-white | 62 | (18.5%) |
| Current Smoker | 25 | (7.5%) |
| Education | ||
| High school graduate or equivalent | 71 | (21.2%) |
| College Degree or greater | 264 | (78.8%) |
| BMI, kg/m2, median (25th, 75th percentile) | 31.2 | (28.4, 34.3) |
| BMI, kg/m2 | ||
| 24*–29.9 | 135 | (40.3%) |
| 30–34.9 | 127 | (37.9%) |
| 35–39.9 | 73 | (21.8%) |
Data presented as number of participants, with percentages in parentheses, unless otherwise noted.
Abbreviations: BMI, body mass index.
Participants were deemed eligible based on body mass index between 25.0 and <40.0 kg/m2 at the time of study orientation; however, one participant had a body mass index of 24.4 kg/m2 (<25.0 kg/m2) at the time of baseline assessment.
6-month Changes in Behaviors and Cardiovascular Risk
After 6 months, at least 75% of those included in the analyses decreased caloric intake, increased MVPA, and decreased weight and at least 50% of participants decreased percentage of calories from fat (all p<0.001, Table 2). In addition, other cardiovascular risk factors improved including measures of adiposity, blood pressure, total cholesterol, and fasting glucose (all p<0.001). The median change in cardiorespiratory fitness was an increase of 3.6 mL/kg·min. (p<0.001).
Table 2.
Baseline, 6-month, and Change in Cardiovascular Risk Factors (n=335)
| Baseline | 6-month | Change | P* | |
|---|---|---|---|---|
| Behavioral Intervention Targets | ||||
| Total Caloric Intake, kcal/day | 1684 (1241, 2300) | 1312 (974, 1771) | −371 (−757, −35) | <0.001 |
| Calories from Fat, % | 35.6 (30.9, 39.0) | 31.8 (27.7, 35.7) | −3.7 (−7.7, 0.3) | <0.001 |
| MVPA, min/week† | 92 (26, 186) | 223 (105, 393) | 109 (10, 252) | <0.001 |
| Weight, kg | 90.5 (79.6, 101.7) | 80.5 (71.9, 91.2) | −8.2 (−12.3, −4.4) | <0.001 |
| Other Cardiovascular Risk Factors | ||||
| BMI, kg/m2 | 31.2 (28.4, 34.3) | 27.9 (25.4, 31.1) | −3.0 (−4.3, −1.5) | <0.001 |
| Body fat, % | 42.0 (37.5, 46.4) | 37.6 (31.3, 43.3) | −4.0 (−6.8. −2.0) | <0.001 |
| Systolic Blood Pressure, mmHg | 114 (108, 122) | 110 (105, 117) | −5 (−9, 1) | <0.001 |
| Diastolic Blood Pressure, mmHg | 70 (65, 76) | 67 (62, 72) | −3 (−7, 1) | <0.001 |
| Total Cholesterol, mg/dL | 180 (161, 201) | 164 (148, 185) | −13 (−30, 0) | <0.001 |
| HDL Cholesterol, mg/dL | 51 (41, 63) | 52 (43, 62) | 0 (−5, 5) | 0.67 |
| Fasting Glucose, mg/dL | 93 (88, 99) | 89 (84, 94) | −4 (−8, 1) | <0.001 |
| VO2 85%, mL/kg·min‡ | 26.2 (22.9, 30.1) | 29.3 (25.4, 35.5) | 3.6 (0.9, 6.5) | <0.001 |
Data are presented as median (25th, 75th percentile)
Abbreviations: BMI, body mass index; MVPA, moderate-to-vigorous intensity physical activity
Wilcoxon signed rank test for continuous variables.
MVPA accumulated in bouts of ≥10 minutes by the SenseWear armband. Value reported is minutes of moderate intensity physical activity + 2 x minutes of vigorous intensity physical activity.
Oxygen uptake during graded exercise test at 85% of age-predicted maximal heart rate. Missing in 6 participants.
Overall Cardiovascular Risk Estimates
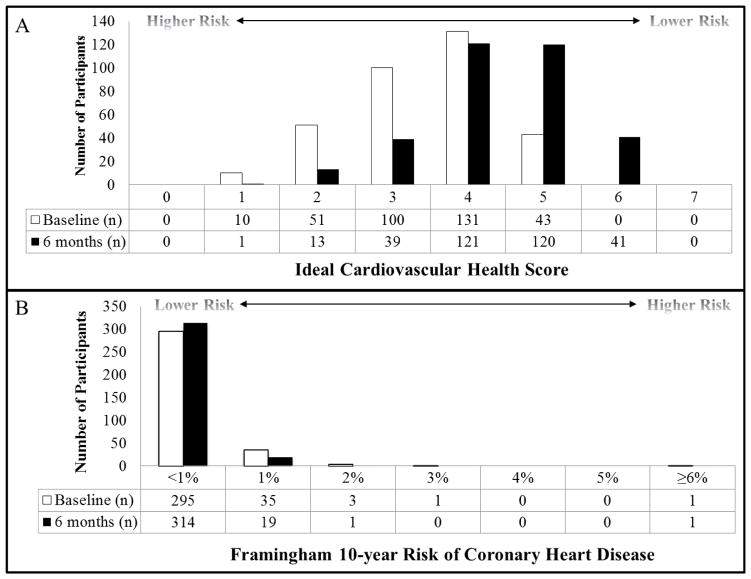
Prior to the weight loss program, the median (25th, 75th percentile) IDEAL score was 4 [3, 4] of 7 possible points (note that participants in the study could have a maximum of 6 points at baseline based on eligibility criteria for BMI). At 6 months, the median IDEAL score was 4 [4, 5] with a median change of 1 [0, 2]. During the intervention, IDEAL score improved in 64.2% and worsened in 6.6% of participants (p<0.001, see Supplemental Table).
For the FR-10 before the intervention began, more than 88.1% of the participants were in the lowest risk category (<1%) and 11.9% of participants had estimated 10-year risk of coronary heart disease ≥1%. At 6 months, few participants changed risk categories. FR-10 improved in 7.5% of participants and worsened in 1.8% of participants (p<0.001, see Supplemental Table).
The distributions of the IDEAL score and FR-10 at baseline and 6-months are displayed in Figure 1. The shift of the distribution of the IDEAL score to a higher score reflects the positive change in overall cardiovascular phenotype. There was also significant improvement in FR-10, though 86.3% of participants were in the lowest risk category at both baseline and 6 months. The correlation between 6-month changes in IDEAL and FR-10 was rs = −0.43 (p<0.001).
Figure 1.
Baseline and 6-month distribution of (A) American Heart Association Ideal Cardiovascular Health (IDEAL) Score and (B) the 10-year risk of coronary heart disease (%) as predicted by the Framingham Risk equation (FR-10) in 335 overweight and obese young adults enrolled in a behavioral weight loss intervention.
Results were comparable using IDEAL14 (14-point scale) Participants had a median (25th, 75th percentile) score of 9 [8, 10] at baseline which changed by 1 [0, 2] over 6 months to 11 [9,11]. IDEAL14 improved in 73.7% and worsened in 9.6%. The correlations between 6-month changes in IDEAL14 and FR-10 was rs = −0.49 (p<0.001).
Ideal Cardiovascular Health Components
At baseline, reflecting inclusion criteria of the study, most participants met ideal criteria for blood pressure, fasting glucose, and total cholesterol, while only one met the IDEAL criterion for BMI (Table 3). Less than 10% of the participants were current smokers at baseline and only about one third met the ideal criterion for physical activity. No participants met the ideal criterion for diet.
Table 3.
Baseline and 6-month Prevalence of Meeting Ideal Cardiovascular Health Score Components
| Baseline | 6-month | |
|---|---|---|
| Ideal Health Components | ||
| Smoking (Never or Quit >12 months ago) | 304 (90.8%) | 311 (92.8%) |
| BMI (<25 kg/m2)* | 1 (0.3%) | 72 (21.5%) |
| MVPA (≥150 minutes/week)† | 112 (33.4%) | 233 (69.6%) |
| Blood Pressure (<120/80 mmHg) | 228 (68.1%) | 273 (81.5%) |
| Fasting Glucose (<100 mg/dL) | 263 (78.5%) | 301 (89.9%) |
| Total Cholesterol (<200 mg/dL) | 243 (72.5%) | 284 (84.8%) |
| Healthy Diet (≥4 of 5 components) | 0 (0%) | 0 (0%) |
| Diet Components | ||
| Fruits & Vegetables (≥4.5 cups/day) | 47 (14.0%) | 50 (14.9%) |
| Sugar-Sweetened Beverages (<36 oz/week) | 257 (76.7%) | 298 (89.0%) |
| Whole Grains (≥ 3 oz/day) | 3 (0.9%) | 1 (0.6%) |
| Fish (≥ 2 servings/week) | 55 (16.4%) | 70 (20.9%) |
| Sodium (<1500 mg/day) | 34 (10.2%) | 56 (16.7%) |
Data is presented as n (%)
Abbreviations: BMI, body mass index; MVPA, moderate-to-vigorous intensity physical activity
Participants were deemed eligible based on body mass index between 25.0 and <40.0 kg/m2 at the time of study orientation; however, one participant had a body mass index of 24.4 kg/m2 (<25.0 kg/m2) at the time of baseline assessment.
MVPA accumulated in bouts of ≥10 minutes by the BodyMedia SenseWear armband. Value reported is minutes of moderate intensity physical activity + 2 x minutes of vigorous intensity physical activity.
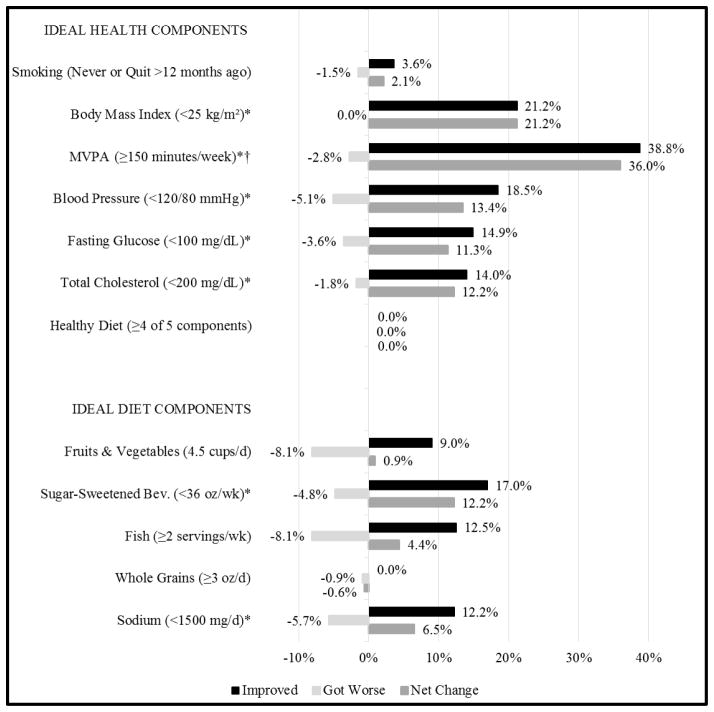
Just over one fifth of participants achieved ideal BMI during the first 6 months of the intervention. Moreover, despite over half of participants having ideal blood pressure, fasting glucose, and total cholesterol at baseline, significant improvements were still observed for these components (Figure 2). Smoking was infrequent and not targeted by the intervention, but 11 of the 30 smokers quit, whereas 4 participants started smoking. Significantly more participants who were not meeting the ideal MVPA criterion at baseline began meeting it (38.8%) as compared to the 2.8% who were meeting it at baseline but not at follow-up, as measured by the objective monitor. In a sensitivity analysis in which self-reported MVPA was substituted for the objective measure, 40.1% began meeting the ideal criterion for MVPA at 6 months whereas 5.1% stopped meeting it (p=0.001).
Figure 2.
Six-month changes in Ideal Cardiovascular Health Components Ideal Diet Components in 335 overweight and obese young adults enrolled in a behavioral weight loss intervention.
†Moderate-to-vigorous intensity physical activity (MVPA) accumulated in bouts of ≥10 minutes by the BodyMedia SenseWear armband (minutes of vigorous intensity physical activity were multiplied by 2).
*p<0.01 for change using McNemar’s test
No participants met the ideal diet criterion at baseline or 6 months (Table 3). However, 35.2% met more of the dietary components at 6 months than at baseline whereas 18.2% met fewer (p<0.001). Out of five possible, the number of ideal dietary components met was 1 [1, 2] at baseline changed by 0 [0, 1] over 6 months (p<0.001). Significant improvements were observed in sugar-sweetened beverage and sodium consumption (Figure 2). At both baseline and 6 months, over three fourths of participants met the ideal criterion for sugar-sweetened beverages, but few achieved other ideal dietary components (Table 3). In a sensitivity analysis using a higher limit of 2300 mg/day for the sodium recommendation, 0% had ideal diet (meeting at least 4 of 5 dietary components) at baseline and 0.9% had ideal diet at 6 months (0.9% no to yes; 0% yes to no). Again using the higher sodium limit, the number of ideal dietary components met was 2 [1, 2] at baseline, with a change of 0 [0, 1] (p <0.001) over 6 months. Specifically for sodium intake, 34.9% of participants consumed <2300 mg/day at baseline and 51.6% at 6 months (25.1% no to yes; 8.4% yes to no; p<0.001).
Framingham Risk Equation Components
Six-month changes in categorization of clinical risk factors that were then used to calculate FR-10 occurred for age, total cholesterol, and systolic blood pressure. While all participants aged 6 months during the intervention, the age category only worsened in 4.8% of participants (p=0.02), which resulted in a higher FR-10 for 0.9% of participants. Total cholesterol changed to a category indicating improvement for 35.5% of participants and worsened in 6.9% participants (p<0.001). Systolic blood pressure category improved in 12.2% of participants and worsened in 3.9% of participants (p=0.008). No significant changes in FR-10 categorizations occurred for smoking (p=0.52) or HDL cholesterol (p=0.39).
Discussion
The main finding of this study is that the IDEAL score registered beneficial changes in a majority of young adults at low 10-year risk of coronary heart disease during the first 6-months of a lifestyle intervention. The change in IDEAL score was primarily due to reduction in BMI and increased activity, though more participants improved than worsened on the laboratory and clinical measures. Over half of the participants observed an improvement in the IDEAL score, and this was observed in a context in which more than half of the sample was classified as ‘ideal’ for 4 or more components at baseline. These findings are consistent with the concept of primordial prevention; the IDEAL score tracks progress towards preventing or reducing risk factors for coronary heart disease and not just clinical outcomes. As compared to the FR-10 which did not change for most participants, the IDEAL score appears to be useful to show progress toward improved cardiovascular health at the group level, especially among younger, largely healthy populations with low short-term risk of coronary heart disease.
The baseline IDEAL score in this sample recruited for a weight loss intervention can be compared to young adult (20–39 years old) men and women in the general, U.S. population as estimated from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008.(Shay et al., 2012) Although, our sample was heavier, by design, (i.e., the baseline prevalence of IDEAL BMI was <1% in our study vs. 37% and 45% for young men and women, respectively, from NHANES(Shay et al., 2012)), the IDEAL score and components suggest our sample was not unhealthier in other ways. Similar to the median IDEAL score of 4 in our study, Shay et al., reported that young women most frequently had an IDEAL score of 4 to 5 and young men a score of 3 to 4.(Shay et al., 2012) The proportion of young adults in our study population meeting ideal smoking criteria (i.e., non-smoking) was substantially higher (91%) than among young men (60%) and women (69%) from NHANES. The prevalence of other IDEAL components in our study was either between estimates for men and women from NHANES (fasting glucose, blood pressure) or within 15% of the estimated prevalence of both men and women (total cholesterol, diet, and physical activity by self-report). Ideal diet was achieved in <1% of our study population, similar to that of young men and women in NHANES.
One other study has evaluated the impact of a lifestyle intervention on IDEAL. The STRIP study conducted in Turku, Finland randomized families of infants to dietary counselling or a control condition with the primary aim to prevent the development of atherosclerosis.(Pahkala et al., 2013) Using measurements during adolescence, the risk of meeting fewer than 4 IDEAL components was 1.35 times higher (95% confidence interval, 1.04–1.77) in control vs. intervention participants. Though the STRIP study differs from ours due to a younger study population and the comparison across randomized groups, the results are consistent with ours showing that the IDEAL score does detect changes in cardiovascular health following a lifestyle intervention in a young, healthy population.
The FR-10 has been shown to improve more markedly in lifestyle interventions with older or higher risk populations.(Maruthur et al., 2009; Shlay et al., 2011; Wister and Wanless, 2007) In the PREMIER lifestyle intervention trial among middle-aged adults with Pre- or Stage I hypertension, the average FR-10 was 1.95% at baseline and decreased by 12–14% over 6 months.(Maruthur et al., 2009) Because the FR-10 was so low at the beginning of the current study, a floor effect occurred where most participants were already at the optimal (<1%) level and thus could not improve.
Cook et al., demonstrated the important concept that, while a reduction of 2 mmHg in diastolic blood pressure would have a larger relative impact for reducing coronary heart disease events among individuals with hypertension vs. individuals with normal blood pressure, the absolute benefit of such a reduction on the population level would be greater among normotensive individuals because there are more people in the lower-risk stratum.(Cook et al., 1995) Recognizing that a population-wide, primordial prevention approach to reduce the development of cardiovascular risk factors could have a smaller relative but perhaps substantial absolute effect, the American Heart Association has launched the ‘Simple 7’ program in which individuals can monitor their personal IDEAL score and track progress (mylifecheck.heart.org) as a compliment to primary/secondary prevention strategies. The results of the current study add support to this initiative by demonstrating that a majority of individuals improved the IDEAL score (reflecting primordial prevention) but not the FR-10 (reflecting primary prevention) in this low-risk population.
Yet, though the IDEAL score may detect changes in cardiovascular health, the degree to which improved cardiovascular health is a motivation for lifestyle change in young adults is unclear. Young adults often do not understand their personal risk for developing cardiovascular diseases or the long-term effects of risk factors (e.g. high blood pressure or cholesterol).(Deskins et al., 2006; Mosca et al., 2000) Thus, use of the IDEAL score coupled with education about the lifetime risks of cardiovascular disease could be an important area for future research.
Strengths of the current study are the large sample of overweight and obese young adults who will likely be large contributors to the future burden of cardiovascular disease, and best practice assessment methods for most of the IDEAL and FR-10 criteria. We were able to evaluate alternative definitions for ideal sodium and physical activity, finding that alternative definitions did not affect our conclusions. Several limitations also deserve comment. The current study does not evaluate the effectiveness of the IDEAL score as a population measure, but rather encourages further research into the utility of the IDEAL score and the Simple 7 program as a motivational tool within behavioral interventions. This intervention study had the primary outcome of weight loss 2 years after randomization, via a decrease in caloric consumption, a decrease in fat consumption, and an increase in sustained bouts of MVPA, so not all of the components of the IDEAL score were targeted. This could underestimate the potential effect of a 6-month lifestyle intervention on the IDEAL score. Also, this study did not include a control condition which limits the interpretation of 6-month changes in IDEAL, FR-10, and components of these scores. However, lack of a control group did not impact the comparison of change in scores (FR-10 and IDEAL) within the same population. Lastly, we used dietary food frequency questionnaires, which could introduce error in measurement and bias due to self-report, though our results are comparable to population estimates.
Conclusion
The results of the current study suggest that the IDEAL score could aid in the pursuit of primordial prevention of cardiovascular disease in populations who are young or have low short-term risk. Future research should investigate the effect of the IDEAL score and the Simple 7 program alone or as a component of a behavioral intervention to improve cardiovascular health.
Supplementary Material
Highlights.
Framingham 10-yr risk of heart disease (FR-10) is often low (<1%) in young adults.
IDEAL, but not the FR-10, improved in most young adults in a weight loss trial.
IDEAL could be more useful for detecting cardiovascular change in young adults.
Acknowledgments
We would like to thank the Co-Investigators, staff and students at the Physical Activity and Weight Management Research Center and the Epidemiology Data Center at the University of Pittsburgh, and participants of the IDEA study.
Funding Source
This study was supported by the National Heart, Lung, and Blood Institute (RO1 # HL64991) and the American Heart Association (12BGIA9410032).
Abbreviations
- FR-10
Framingham 10-yr predicted risk of coronary heart disease
- IDEAL
American Heart Association’s Ideal Cardiovascular Health Score
- MVPA
Moderate-to-vigorous intensity physical activity
- VO2 85%
Oxygen uptake during graded exercise test at 85% of age-predicted maximal heart rate
Footnotes
Clinical Trials Registration: NCT00177762 http://clinicaltrials.gov/show/NCT01131871
Conflicts of Interest and Disclosures
Dr. Barone Gibbs reports grants from American Heart Association, during the conduct of the study; grants from HumanScale, outside the submitted work.
Dr. King reports grants from American Heart Association, grants from NHLBI, during the conduct of the study.
Dr. Belle reports grants from NHLBI, during the conduct of the study.
Dr. Jakicic reports grants from American Heart Association, grants from National Institutes of Health (NIH - NHLBI), during the conduct of the study; grants from National Institutes of Health, grants from Ethicon/Covidien, grants from Jawbone/BodyMedia, grants from Weight Watchers International, personal fees from Weight Watchers International, non-financial support from ILSI North America Energy Balance and Physical Activity Committee, grants from Human Scale, outside the submitted work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 2.2008 Physical Activity Guidelines for Americans. Journal of Cardiovascular Nursing. 2009;24:2–3. [Google Scholar]
- 3.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20:470–5. [PubMed] [Google Scholar]
- 4.Bibbins-Domingo K. The Institute of Medicine Report Sodium Intake in Populations: Assessment of Evidence Summary of Primary Findings and Implications for Clinicians. Jama Internal Medicine. 2014;174:136–37. doi: 10.1001/jamainternmed.2013.11818. [DOI] [PubMed] [Google Scholar]
- 5.Bondar RJ, Mead DC. Evaluation of glucose-6-phosphate dehydrogenase from Leuconostoc mesenteroides in the hexokinase method for determining glucose in serum. Clin Chem. 1974;20:586–90. [PubMed] [Google Scholar]
- 6.Bucolo G, David H. Quantitative determination of serum triglycerides by the use of enzymes. Clin Chem. 1973;19:476–82. [PubMed] [Google Scholar]
- 7.Bull FC, Maslin TS, Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. 2009;6:790–804. doi: 10.1123/jpah.6.6.790. [DOI] [PubMed] [Google Scholar]
- 8.Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–9. [PubMed] [Google Scholar]
- 9.Cowell HA. Physical activity guidelines for Americans and a review of scientific literature used. Nova Science Publishers; Hauppauge, N.Y: 2010. [Google Scholar]
- 10.D’Agostino RB, Sr, Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286:180–7. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 11.Deskins S, Harris CV, Bradlyn AS, Cottrell L, Coffman JW, Olexa J, Neal W. Preventive care in Appalachia: use of the theory of planned behavior to identify barriers to participation in cholesterol screenings among West Virginians. J Rural Health. 2006;22:367–74. doi: 10.1111/j.1748-0361.2006.00060.x. [DOI] [PubMed] [Google Scholar]
- 12.Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–6. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 14.Jakicic J, King AC, Marcus MD, Davis KK, Hesel D, Rickman AD, Gibbs BB, Rogers RJ, Wahed A, et al. Short-Term Weight Loss with Diet and Physical Activity in Young Adults: the IDEA Study. Obesity (Silver Spring) 2015 doi: 10.1002/oby.21241. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johannsen DL, Calabro MA, Stewart J, Franke W, Rood JC, Welk GJ. Accuracy of armband monitors for measuring daily energy expenditure in healthy adults. Med Sci Sports Exerc. 2010;42:2134–40. doi: 10.1249/MSS.0b013e3181e0b3ff. [DOI] [PubMed] [Google Scholar]
- 16.Koehler K, Braun H, de Marees M, Fusch G, Fusch C, Schaenzer W. Assessing energy expenditure in male endurance athletes: validity of the SenseWear Armband. Med Sci Sports Exerc. 2011;43:1328–33. doi: 10.1249/MSS.0b013e31820750f5. [DOI] [PubMed] [Google Scholar]
- 17.Laitinen TT, Pahkala K, Magnussen CG, Viikari JS, Oikonen M, Taittonen L, Mikkila V, Jokinen E, Hutri-Kahonen N, et al. Ideal cardiovascular health in childhood and cardiometabolic outcomes in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation. 2012;125:1971–8. doi: 10.1161/CIRCULATIONAHA.111.073585. [DOI] [PubMed] [Google Scholar]
- 18.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 19.Mackey DC, Manini TM, Schoeller DA, Koster A, Glynn NW, Goodpaster BH, Satterfield S, Newman AB, Harris TB, et al. Validation of an armband to measure daily energy expenditure in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:1108–13. doi: 10.1093/gerona/glr101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maruthur NM, Wang NY, Appel LJ. Lifestyle interventions reduce coronary heart disease risk: results from the PREMIER Trial. Circulation. 2009;119:2026–31. doi: 10.1161/CIRCULATIONAHA.108.809491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mosca L, Jones WK, King KB, Ouyang P, Redberg RF, Hill MN, Dis AHAWH. Awareness, perception, and knowledge of heart disease risk and prevention among women in the United States. Archives of Family Medicine. 2000;9:506–15. doi: 10.1001/archfami.9.6.506. [DOI] [PubMed] [Google Scholar]
- 22.Pahkala K, Hietalampi H, Laitinen TT, Viikari JS, Ronnemaa T, Niinikoski H, Lagstrom H, Talvia S, Jula A, et al. Ideal cardiovascular health in adolescence: effect of lifestyle intervention and association with vascular intima-media thickness and elasticity (the Special Turku Coronary Risk Factor Intervention Project for Children [STRIP] study) Circulation. 2013;127:2088–96. doi: 10.1161/CIRCULATIONAHA.112.000761. [DOI] [PubMed] [Google Scholar]
- 23.Shay CM, Ning H, Allen NB, Carnethon MR, Chiuve SE, Greenlund KJ, Daviglus ML, Lloyd-Jones DM. Status of cardiovascular health in US adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125:45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shlay JC, Barber B, Mickiewicz T, Maravi M, Drisko J, Estacio R, Gutierrez G, Urbina C. Reducing cardiovascular disease risk using patient navigators, Denver, Colorado, 2007–2009. Preventing chronic disease. 2011;8:A143. [PMC free article] [PubMed] [Google Scholar]
- 25.Thompson FE, Subar AF, Brown CC, Smith AF, Sharbaugh CO, Jobe JB, Mittl B, Gibson JT, Ziegler RG. Cognitive research enhances accuracy of food frequency questionnaire reports: results of an experimental validation study. J Am Diet Assoc. 2002;102:212–25. doi: 10.1016/s0002-8223(02)90050-7. [DOI] [PubMed] [Google Scholar]
- 26.United States. Department of Health and Human Services. 2008 physical activity guidelines for Americans: be active, healthy, and happy! U.S. Dept. of Health and Human Services; Washington, DC: 2008. [Google Scholar]
- 27.Wister AV, Wanless D. A health profile of community-living nonagenarians in Canada. Canadian journal on aging = La revue canadienne du vieillissement. 2007;26:1–18. doi: 10.3138/01v7-0287-9231-q854. [DOI] [PubMed] [Google Scholar]
- 28.Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, Gillespie C, Merritt R, Hu FB. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307:1273–83. doi: 10.1001/jama.2012.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.