Abstract
Population-level strategies to improve healthy food choices are needed for obesity prevention. We conducted a randomized controlled trial of 2,672 employees at Massachusetts General Hospital who were regular customers of the hospital cafeteria with all items labeled green (healthy), yellow (less healthy), or red (unhealthy) to determine if social norm (peer-comparison) feedback with or without financial incentives increased employees’ healthy food choices. Participants were randomized in 2012 to three arms: 1) monthly letter with social norm feedback about healthy food purchases, comparing employee to “all” and to “healthiest” customers (feedback-only); 2) monthly letter with social norm feedback plus small financial incentive for increasing green purchases (feedback-incentive); or 3) no contact (control). The main outcome was change in proportion of green-labeled purchases at end of 3-month intervention. Post-hoc analyses examined linear trends. At baseline, the proportion of green-labeled purchases (50%) did not differ between arms. At end of the 3-month intervention, the percentage increase in green-labeled purchases was larger in the feedback-incentive arm compared to control (2.2% vs. 0.1%, P=0.03), but the two intervention arms were not different. The rate of increase in green-labeled purchases was higher in both feedback-only (P=0.04) and feedback-incentive arms (P=0.004) compared to control. At end of a 3-month wash-out, there were no differences between control and intervention arms. Social norms plus small financial incentives increased employees’ healthy food choices over the short-term. Future research will be needed to assess the impact of this relatively low-cost intervention on employees’ food choices and weight over the long-term.
Trial Registration: Clinical Trials.gov NCT01604499
Keywords: Food choice, worksite, obesity prevention, social norms, financial incentives
INTRODUCTION
Poor diet quality and increased energy intake are largely responsible for the rapid rise in obesity in the United States and worldwide.1,2 Preventing obesity at the population level will require widespread social, cultural, and environmental changes to promote consumption of healthy foods.2–5 Policy changes, such as calorie labeling and “junk food” taxes, have potential for improving population dietary choices.6,7 However, research evaluating the effectiveness of calorie labeling has been mixed,8–13 and taxation is still being actively debated in the United States.7 As policies evolve, new strategies to complement these approaches can be implemented by employers, institutions, and retailers to promote healthier food choices.2,3,14,15
Behavioral economists and psychologists have identified decision biases that contribute to unhealthy choices, including doing what is usual (status quo), placing disproportionate weight on the present and not considering the future (present-biased preferences), and being influenced by what others are doing (social norms).16–19 Field research has demonstrated that interventions to address status quo bias and present-biased preferences, including altering the food environment and providing simple messages (e.g. traffic lights), increase healthy food choices.20–25 Evidence from small experimental studies has shown that providing individuals with information about social norms influences the choice or quantity of food eaten.26–32
A social norm intervention has not yet been tested on a large scale to change food choices, but this strategy is already used to promote environmental energy conservation. The “Home Energy Report” is mailed to customers of utility companies and compares a household’s energy use to that of similar neighbors and to “energy-efficient” neighbors.33 A natural field experiment of 600,000 treatment and control households demonstrated that this program significantly reduced energy consumption.34 Financial incentives, another strategy to address decision biases, have been shown to improve several healthy behaviors.35–39 There is evidence that changing the price of foods, e.g. decreasing the cost of healthy foods, or offering “cash back” or rebate programs in grocery stores increase the purchase of healthy foods.40–46 The “Food Dudes” program demonstrated the effectiveness of using incentives as part of a multicomponent intervention to increase fruit and vegetable consumption among school-aged children.47
We hypothesized that a population of employees who were provided with social norm feedback about their healthy food choices compared to their peers would increase healthy foods purchased in a large worksite cafeteria and that adding a small financial incentive to the social norm feedback would further increase healthy purchases. Building on an established traffic-light food labeling system,20,22 we conducted a three-arm randomized trial comparing 1) social norm feedback about healthy cafeteria purchases; 2) social norm feedback plus small financial incentives to increase healthy food purchases; and 3) no feedback or incentives (control) over three months, followed by a three month wash-out period.
METHODS
This study was approved by the Partners Healthcare Institutional Review Board on May 18, 2012.
Setting and Participants
Massachusetts General Hospital is a 907 bed teaching hospital with over 24,000 employees. The hospital’s main cafeteria serves approximately 6,500 hospital employees, patients, and visitors every day of the week between 6:30 am and 8:00 pm. The cafeteria is owned and operated by the hospital, and no outside food vendors are located on campus. Hospital employees have the option of paying for cafeteria purchases by direct payroll deduction using a “platinum plate” card. In 2012, approximately 7,400 employees used a platinum plate card to pay for cafeteria purchases.
In 2010, all food and beverages in the cafeteria were labeled with a traffic-light scheme, and results from this intervention have been previously reported.20–22,25 Briefly, the traffic-light system was based on the United States Department of Agriculture dietary guidelines,48,49 and every item in the cafeteria was labeled as green, yellow, or red based on positive criteria (fruit/vegetable, whole grain, and lean protein/low-fat dairy as the main ingredient) and negative criteria (saturated fat and calories).20 The introduction of the traffic-light system in the cafeteria included permanent signage to explain and display the labels.
Recruitment and Randomization
Employees who used their platinum plate card for a minimum of three separate transactions per month in the main cafeteria during both July and August 2012 were eligible for participation in the study. On September 1, 2012, an “opt out” letter was mailed to these employees’ home addresses and briefly described study procedures. A phone number and a study identification number were provided, and the employee could opt out of the study by calling the number and referencing the study identification number. Employees were informed in the letter that if they did not call within the next two weeks, they would automatically be enrolled. Employees were excluded from the study if the letter was returned due to an incorrect address. Three weeks after the letters were mailed, all employees who did not opt out or were not excluded due to an incorrect address were randomly assigned to one of three arms: 1) feedback-only; 2) feedback-incentive; or 3) control, using simple randomization executed in Microsoft Excel (Redmond, WA).
Intervention
Feedback-only
The feedback-only arm received four letters over three months. Letters were mailed at the beginning of the month for October, November, and December 2012 and January 2013. Each letter presented a 3-column color bar graph describing: 1) the proportion of the employee’s cafeteria purchases from the prior month that were labeled red, yellow, and green; 2) the average proportion of red, yellow, and green purchases by all employees using platinum plate cards; and 3) the average proportion of purchases labeled red, yellow, and green among the “healthiest MGH eaters” (top quintile in percentage of green purchases). The letter also included a written description of the employee’s percentage of green (or healthy) items compared to the “healthiest eaters.” Each letter also included an explanation of the traffic-light labeling system. The January 1st letter informed the participant that he or she would not receive any further communication.
Feedback-incentive
Letters mailed to the feedback-incentive arm included the same information as the feedback-only arm, but these letters also included a statement that the employee could earn a reward by achieving a specific “green goal” in the following month. There were three possible goals: make 40%, 60%, or 80% of all cafeteria purchases in the month green-labeled items. An individual’s goal was determined based on the proportion of green items purchased in the prior month (e.g., purchasing 8 green items and 24 yellow/red items in one month would mean 8/32 or 25% green).
If an individual’s baseline green purchases were less than 40%, the first goal was 40%; if baseline purchases were between 40% and 59%, the first goal was 60%; and if baseline purchases were between 60–79%, the first goal was 80%. An employee could earn $10 toward his or her cafeteria account each time a threshold was passed, but he or she could only earn the incentive once for passing each threshold. If an employee increased past a threshold one month but then fell below the threshold in the next month, he or she would not earn any money for passing the same threshold again. However, if an employee passed a threshold once in one month and maintained above that threshold in the following month but did not pass the next threshold, the employee would earn $5. Employees who started above the top threshold of 80% green could earn $5 a month for maintaining at or above this level. The incentive system was designed so that employees who purchased the lowest proportion of green foods at the beginning of the study (less than 40% green) had the opportunity to earn the most reward money over the three months ($30 if all three thresholds were achieved). An employee was notified in the monthly letter that he or she had earned a reward, and the credit toward the platinum plate account was included as a line item in the weekly or monthly paycheck. The January 1st letter provided a summary of the total rewards earned by the participant during the study and informed the participant that he or she would not receive any more rewards or communication.
Control Arm
After the initial opt out letter, the control arm did not receive any further contact about the research study.
Outcomes
Data on employee age, sex, job type, and self-reported race/ethnicity (white, black, Asian, or Latino) were available from Human Resources files. Human resources data did not provide information on race and ethnicity separately. Job types were aggregated into five categories that roughly correlated with increasing educational attainment: service workers (manual and/or unskilled laborers); support staff; technicians (e.g., radiology technicians, respiratory therapists); professionals (e.g., occupational therapists, pharmacists); and management/faculty/nurses (e.g., hospital managers, faculty, physicians, nurses). Education was inconsistently reported by employees. For those who did report their education, 90% of service workers had a high school education or less, and 83% of professionals and management/faculty/nurses had a bachelor’s degree or higher.
Sales data from cafeteria cash registers were used to track study participants’ purchases throughout the study. The proportion of green, yellow, and red items purchased were calculated for each month of the study, from baseline (September 2012) to the end of the “wash-out” period (March 2013). The primary outcomes were changes in the monthly proportions of green items purchased at the end of the intervention (December 2012) compared to baseline (September 2012) and at the end of the wash-out period (March 2013) compared to baseline.
Based on inspection of the data, we conducted post-hoc analyses modeling separate linear trends for purchases by each study arm during the intervention and control periods. We also conducted a post-hoc sub-group analysis to examine the changes in green purchases by employees who made the healthiest and the least healthy cafeteria purchases at baseline. For these analyses, we assigned all study participants to quartiles of green purchases that were made during the baseline period. The first quartile included employees who had purchased the lowest proportion of green-labeled items (least healthy), and the fourth quartile included employees who had purchased the highest proportion of green-labeled items (healthiest).
Statistical analysis
For analyzing cafeteria purchases, the dependent variables were monthly proportions of green-labeled items. We compared within subject changes in the proportion of green-labeled food purchases across study arms using random-effects linear regressions, adjusting for repeated measures. The model included terms for study arm, month, and study arm-by-month interactions. Our primary outcomes were tested on the coefficient of the interaction terms at end of intervention and end of washout. For our post-hoc analysis of linear trends, we modeled study arm, study month (as a continuous variable), and study arm-by-month interactions. Changes in trends in the washout period were modeled by interacting the intervention period terms with an indicator for the washout time period, constraining the washout period trend to be continuous with the intervention period trend (linear spline). For analyses by quartile of healthy purchases, the models were adjusted for employee demographics and job type. We compared drop-out rates in the 3 study arms using a Pearson chi-square test. Among subjects randomized, our primary analyses focused on assessing intervention efficacy by using data from observed purchases for those subjects who did not actively opt out of the program. As a sensitivity analysis, we used multiple imputation to generate complete outcomes data on all subjects (N=2,672) including those who actively opted out of the program and those for whom purchases were not observed, either due to active drop-out, employment termination, or missing purchasing data.
We designed the study to detect a difference of 2.7 percentage points or larger in the average employee-level change between any two study arms (our primary analysis) using a two-sided test and P-value of 0.05 with 80% power in a sample size of 2,600 employees with a standard deviation for employee-level changes of 0.2 % (based on previous data). All analyses were conducted in 2014 using Stata 12.1 (Stata Corporation, College Station, TX).
RESULTS
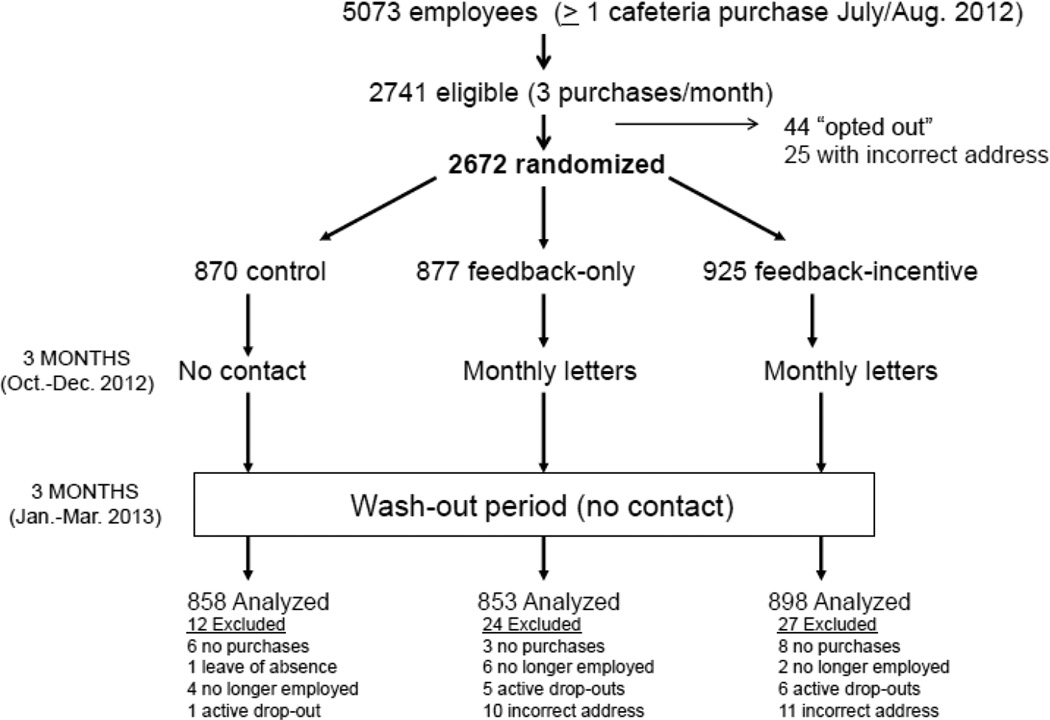
There were 2,741 employees identified who were eligible to participate in the study and to whom an “opt out” letter was mailed (Figure 1). Of these, 44 employees actively “opted out” of the study, and 25 employees did not have a correct home address on file and were excluded. A total of 2,672 employees were randomly assigned to one of the three treatment arms, and 63 employees were excluded from the final analyses (Figure 1). Due to the simple randomization scheme, there was variation in the number of employees assigned to each study arm. Dropout was slightly higher among the feedback-only and feedback-incentive arms than the control arm (2.7%, 2.9%, and 1.4%, P=0.07).
Figure 1. Study flow diagram.
This study took place at Massachusetts General Hospital in Boston, MA in 2012–2013.
Table 1 shows baseline demographic characteristics and cafeteria purchasing patterns. Demographics of employees in the study reflected overall hospital demographics. Study arms were similar except for small differences in distribution of job types. Study participants visited the cafeteria a mean of 12.2 times per month and purchased a mean of 30 items. Mean proportions of green, yellow, and red-labeled purchases were 50%, 32%, and 18% respectively.
Table 1.
Baseline characteristics and cafeteria purchasing patterns of employees.
| Control group (N=858) |
Feedback- only group (N=853) |
Feedback- incentive group (N=898) |
P value | |
|---|---|---|---|---|
| Sex, % | ||||
| Female | 72 | 73 | 72 | 0.80 |
| Male | 28 | 27 | 28 | |
| Age group, % | ||||
| 18–30 | 24 | 23 | 21 | |
| 31–40 | 28 | 28 | 29 | |
| 41–50 | 21 | 22 | 22 | 0.90 |
| 50 and over | 26 | 24 | 26 | |
| Unknown | 2 | 2 | 2 | |
| Race, % | ||||
| Black/African American | 12 | 10 | 9 | |
| Hispanic/Latino | 8 | 8 | 7 | |
| Asian | 5 | 7 | 7 | 0.21 |
| White | 73 | 69 | 72 | |
| Unknown | 4 | 5 | 4 | |
| Job type, % | ||||
| Service workers | 7 | 10 | 6 | |
| Administrative support | 11 | 11 | 11 | |
| Technicians | 10 | 9 | 11 | 0.005 |
| Professionals | 17 | 11 | 13 | |
| Management/faculty/nurses | 52 | 56 | 57 | |
| Unknown | 3 | 3 | 2 | |
| Proportion of purchases that are green, % | 49 | 50 | 50 | 0.73 |
| Proportion of purchases that are yellow, % | 33 | 32 | 32 | 0.42 |
| Proportion of purchases that are red, % | 17 | 18 | 18 | 0.75 |
| Visits to cafeteria, mean | 12.0 | 12.1 | 12.5 | 0.41 |
| Number of items purchased, mean | 30 | 29 | 31 | 0.31 |
| Amount spent in cafeteria per month, mean | $56.85 | $56.73 | $59.78 | 0.24 |
Totals may not add to 100% due to rounding.
This study took place at Massachusetts General Hospital in Boston, MA in 2012–2013.
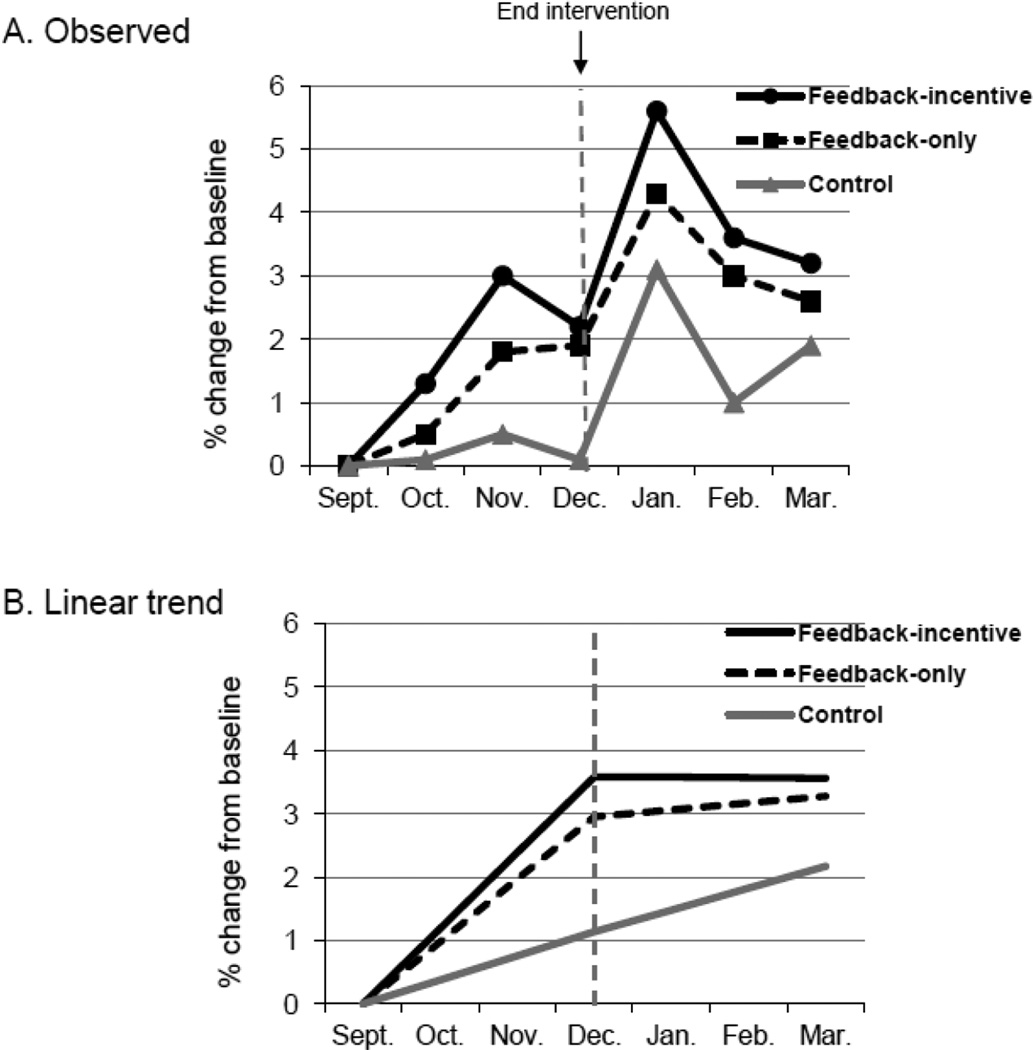
Change from baseline in the monthly proportion of green-labeled (healthy) purchases is shown in Figure 2 (Panel A). At end of the intervention (December) compared to baseline (September), the increase in percentage of green purchases was larger in the feedback-incentive arm (2.2%, P=0.03) and borderline in the feedback-only arm (1.8%, P=0.07) compared to control (0.1%); the two intervention arms were not significantly different from each other. At the end of the 3-month wash-out, there were no significant differences between the control and two intervention arms. Compared to control, the rate of increase in green purchases was higher during the intervention period for both feedback-only (P=0.04) and feedback-incentive arms (P=0.004), but during wash-out, the rates of change for both arms were not different from control (Panel B).
Figure 2.
Observed changes and linear trends in proportion of green-labeled (healthy) cafeteria purchases.
Panel A: P=0.03 for feedback-incentive vs. control (end of intervention); P=0.07 for feedback-only vs. control (end of intervention); P>0.10 for both intervention groups compared to control (end of wash-out).
Panel B: P=0.004 for linear trend of feedback-incentive vs. control and P=0.04 for linear trend of feedback-only vs. control during intervention period; P>0.10 for both comparisons during washout period.
This study took place at Massachusetts General Hospital in Boston, MA in 2012–2013.
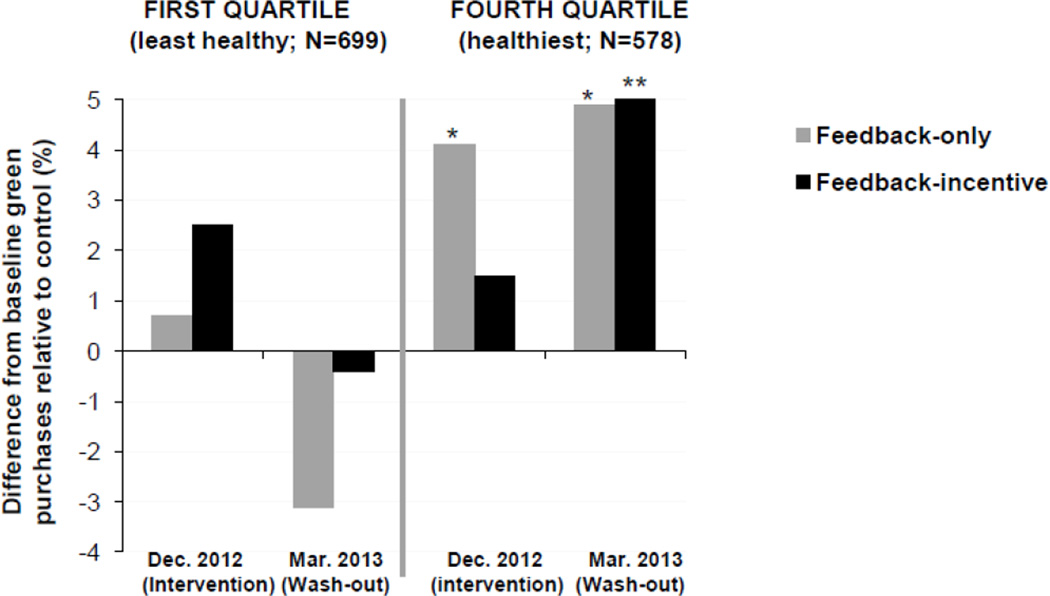
We conducted a sub-group analysis of employees by quartile of baseline healthy purchases. Employees in the least healthy quartile (N=699) had 21% green-labeled purchases at baseline, and employees in the healthiest quartile (N=578) had 82% green-labeled purchases. Employees from the least healthy quartile were more likely to be male, less than 40 years old, non-white, and from lower-educated job types compared to the healthiest quartile (Table 2). Figure 3 shows change in the percentage of green-labeled purchases for employees from the least healthy and healthiest quartiles. In the least healthy quartile, the intervention arms were not significantly different from control at the end of intervention or the end of wash-out. In the healthiest quartile, the difference between the feedback-only and control arm changes was significantly higher at the end of intervention (P=0.03) and end of wash-out (P=0.01); the difference between the feedback- incentive and control arm changes was significant only at the end of wash-out (P=0.006) (Figure 3).
Table 2.
Food purchases and employee demographics by baseline quartile of green (healthy) purchases.
| Least healthy-------------------------------Healthiest | |||||
|---|---|---|---|---|---|
| 1st quartile (N=699) |
2nd quartile (N=688) |
3rd quartile (N=576) |
4th quartile (N=578) |
P value | |
| Baseline food purchases | |||||
| Green, % | 21 | 43 | 59 | 82 | <0.001 |
| Yellow, % | 48 | 37 | 29 | 13 | <0.001 |
| Red, % | 31 | 19 | 12 | 5 | <0.001 |
| Sex, % | |||||
| Female | 65 | 69 | 78 | 80 | <0.001 |
| Male | 35 | 31 | 22 | 20 | |
| Age group, % | |||||
| 18–30 | 29 | 22 | 19 | 18 | |
| 31–40 | 31 | 28 | 28 | 23 | |
| 41–50 | 20 | 24 | 22 | 22 | <0.001 |
| 50 and over | 18 | 24 | 19 | 35 | |
| Unknown | 2 | 2 | 2 | 2 | |
| Race, % | |||||
| Black/African American | 18 | 10 | 6 | 5 | |
| Hispanic/Latino | 13 | 9 | 5 | 3 | |
| Asian | 5 | 7 | 8 | 6 | <0.001 |
| White | 60 | 70 | 78 | 83 | |
| Unknown | 5 | 4 | 4 | 3 | |
| Job type, % | |||||
| Service workers | 14 | 7 | 5 | 3 | |
| Administrative support | 16 | 11 | 9 | 7 | |
| Technicians | 15 | 11 | 8 | 6 | <0.001 |
| Professionals | 11 | 15 | 14 | 12 | |
| Management/faculty/nurses | 42 | 54 | 61 | 69 | |
| Unknown | 3 | 2 | 2 | 2 | |
Totals may not add to 100% due to rounding.
Total N is less than 2609 because not all subjects had purchases in the baseline month.
This study took place at Massachusetts General Hospital in Boston, MA in 2012–2013.
Figure 3.
Change from baseline in green-labeled (healthy) purchases by employees from the least healthy and healthiest quartiles of cafeteria purchases.
* P<0.05, adjusting for age, sex, race, job type, and part-time job status.
** P<0.01, adjusting for age, sex, race, job type, and part-time job status.
All comparisons in with no footnote have P >0.10.
This study took place at Massachusetts General Hospital in Boston, MA in 2012–2013.
We examined the mean number and amount of rewards earned by employees who were in the feedback-incentive arm (N=898) by quartile of green purchases. Overall, 509 (57%) earned at least one reward. Employees from the healthiest quartile earned a higher number of rewards than employees in the least healthy quartile (1.3 vs. 0.8 rewards, P<0.001), but the mean value of rewards earned per employee per month was similar ($8.47 vs. $8.40, p=0.82) (Table 3).
Table 3.
Rewards earned by feedback-incentive group (N=898) by quartile of baseline green purchases.
| Least healthy--------------------------Healthiest | |||||
|---|---|---|---|---|---|
| 1st quartile | 2nd quartile | 3rd quartile | 4th quartile | P-value | |
| Number of rewards earned overall, mean | 0.8 | 1.0 | 1.0 | 1.3 | <0.001 |
| Number of $5 rewards* earned, mean | 0.2 | 0.4 | 0.4 | 1.0 | <0.001 |
| Number of $10 rewards** earned, mean | 0.6 | 0.6 | 0.6 | 0.3 | <0.001 |
| Value of rewards earned, mean | $8.40 | $9.14 | $8.66 | $8.47 | 0.82 |
$5 rewards were earned for maintaining healthy purchases above a specific threshold in a month.
$10 rewards were earned for increasing healthy purchases above a specific threshold (increasing above a target of 40%, 60%, or 80% green purchases in a month).
This study took place at Massachusetts General Hospital in Boston, MA in 2012–2013.
We performed a sensitivity analysis using multiply imputed data for subjects who did not make cafeteria purchases. This analysis demonstrated that the effectiveness of the intervention was similar to the efficacy, with a mean improvement in green purchases for the feedback-incentive group compared to the control group (2.0% vs. 0.1%, p=0.04). We also looked at the mean number of cafeteria visits across each of the study arms during the intervention period and the washout period and found no significant changes in cafeteria visits across each of the study arms over time.
DISCUSSION
Social norm feedback plus small financial incentives resulted in healthier cafeteria purchases by employees over three months. This is the first study, to our knowledge, to use food purchasing data to provide consumers with individual social norm feedback and financial incentives to promote healthy food choices. Although absolute changes were small, this relatively “light touch” intervention resulted in a significant shift toward healthier food purchases by a large group of employees who had not sought out a healthy eating or wellness program. Healthy purchases increased over time in both the feedback only and feedback-incentive groups during the intervention period but then leveled off after the intervention ended. These findings suggest that a long-term strategy of providing monthly social norm and incentive feedback to employees could lead to larger changes in healthy eating patterns and improvements in health outcomes over time. The cost of providing on-going feedback and small incentives through monthly letters (or emails) is relatively small compared to the cost of other types of employee wellness programs, such as intensive exercise programs and nutrition counseling.
Providing financial incentives is a promising strategy for improving healthy food choices across the population.40–44 A large study in South Africa that provided “cash-back” rebates for healthy food purchases to 170,000 households resulted in an increase in the ratio of healthy to total food expenditure.46 Another large pilot study demonstrated that providing a small financial incentive for the purchase of fruits and vegetables by individuals participating in the Supplemental Nutrition Assistance Program (SNAP) resulted in a 26% increase in consumption of fruits and vegetables compared to a control group.45
Observational data has shown that obesity and food choices are associated with social connections,50,51 and experimental studies have demonstrated that social norms influence food choices.26–32 In our study, there were no significant differences between the intervention arms, suggesting that the incentives did not have a large incremental effect over social norms alone. Future studies should evaluate the long term effectiveness of using social norms to promote healthy food choices; if effective, this type of intervention could be applied more broadly, and at a lower cost, than financial incentives.
Disappointingly, in a post-hoc subgroup analysis, the incentives and social norm feedback did not produce significant changes in food choices by employees who made the least healthy purchases at baseline. These employees were more likely to be from non-white and lower-educated groups, populations at high risk of weight gain and obesity.52,53 It is possible that more intense approaches, such as higher incentives or a more immediate payment (e.g. at the point of purchase) as well as more targeted social norms (e.g. comparing to employees from the same job type rather than “all”), would have a stronger effect on healthy food choices among these groups. Adding educational messages targeting specific foods or suggesting healthier substitutes for unhealthy items such as sugar-sweetened beverages may also help reduce disparities in healthy choices.
This is a randomized study of a population of employees who did not “actively” enroll in a healthy eating or wellness program, thus strengthening the validity and generalizability of our findings. Although there appeared to be a post-holiday seasonal effect on healthy purchases during wash-out, similar changes were observed in all arms. A limitation is that we could only assess food purchases and not actual dietary intake. Study participants were employees from a large urban hospital, and findings may not be generalizable to non-employed populations. The cafeteria in this study offered many comparably priced green and red-labeled food items, and it is unlikely that the cost of healthy foods reduced the effect of the intervention. However in other settings that only offer high-priced healthy food options, cost could modify the effect of incentives to promote healthy choices.
CONCLUSIONS
Improving food choices at work is an important strategy for reducing obesity, diabetes, and cardiovascular diseases, and many worksite food services and cafeterias have implemented food labeling interventions, such as traffic-lights and calorie-labeling.15 Our results demonstrate that social norms plus small financial incentives increased employees’ healthy food choices over the short-term. However, future research will be needed to assess the impact of this relatively low-cost intervention on employees’ food choices and weight over the long-term. These types of strategies can be easily implemented using existing payment or loyalty card infrastructure in worksite, institutional, and retail (e.g. supermarket) settings. Engaging private and public-sector organizations to improve population-level food choices will increase the effectiveness of existing and future government-led policies to prevent obesity.
Supplementary Material
Highlights.
Employees were randomized to social norms; social norms plus incentives; or control.
Social norms plus small incentives increased healthy food choices over 3 months.
After 3-month washout, there were no longer any differences between groups.
Future research should test a longer-term strategy for this low-cost intervention.
Acknowledgments
We would like to thank Susan J. Barraclough, MS, RD, the Director of Nutrition and Food Services at Massachusetts General Hospital at the time of the study for her leadership, support, and oversight of the implementation and maintenance of the cafeteria intervention. We also thank Lillian Sonnenberg, DSc, RD for her contributions to the development and maintenance of the traffic-light labeling system in the cafeteria.
This research was supported by the Robert Wood Johnson Foundation’s Pioneer Portfolio and the Donaghue Foundation through the grant, “Applying Behavioral Economics to Perplexing Health and Health Care Challenges.” Dr. Thorndike was supported by the NIH/National Heart Lung and Blood institute grant K23 HL93221. Neither the NIH nor the Robert Wood Johnson and Donaghue Foundations had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial disclosures: The other authors have no financial disclosures to report.
References
- 1.McCrory MA, Suen VM, Roberts SB. Biobehavioral influences on energy intake and adult weight gain. J Nutr. 2002;132(12):3830S–3834S. doi: 10.1093/jn/132.12.3830S. [DOI] [PubMed] [Google Scholar]
- 2.Gortmaker SL, Swinburn BA, Levy D, et al. Changing the future of obesity: Science, policy, and action. Lancet. 2011;378(9793):838–847. doi: 10.1016/S0140-6736(11)60815-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swinburn B, Egger G. Preventive strategies against weight gain and obesity. Obes Rev. 2002;3(4):289–301. doi: 10.1046/j.1467-789x.2002.00082.x. [DOI] [PubMed] [Google Scholar]
- 4.Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: Shaped by global drivers and local environments. Lancet. 2011;378(9793):804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 5.Huang TT, Glass TA. Transforming research strategies for understanding and preventing obesity. JAMA. 2008;300(15):1811–1813. doi: 10.1001/jama.300.15.1811. [doi] [DOI] [PubMed] [Google Scholar]
- 6.Block JP, Roberto CA. Potential benefits of calorie labeling in restaurants. JAMA. 2014;312(9):887–888. doi: 10.1001/jama.2014.9239. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mozaffarian D, Rogoff KS, Ludwig DS. The real cost of food: Can taxes and subsidies improve public health? JAMA. 2014;312(9):889–890. doi: 10.1001/jama.2014.8232. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harnack LJ, French SA. Effect of point-of-purchase calorie labeling on restaurant and cafeteria food choices: A review of the literature. Int J Behav Nutr Phys Act. 2008;5:51. doi: 10.1186/1479-5868-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bassett MT, Dumanovsky T, Huang C, et al. Purchasing behavior and calorie information at fast-food chains in New York City, 2007. Am J Public Health. 2008;98(8):1457–1459. doi: 10.2105/AJPH.2008.135020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: A first look at the effects on low-income people in New York City. Health Aff (Millwood) 2009;28(6):w1110–w1121. doi: 10.1377/hlthaff.28.6.w1110. [DOI] [PubMed] [Google Scholar]
- 11.Pulos E, Leng K. Evaluation of a voluntary menu-labeling program in full-service restaurants. Am J Public Health. 2010;100(6):1035–1039. doi: 10.2105/AJPH.2009.174839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finkelstein EA, Strombotne KL, Chan NL, Krieger J. Mandatory menu labeling in one fast-food chain in king county, washington. Am J Prev Med. 2011;40:122–127. doi: 10.1016/j.amepre.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 13.Long MW, Tobias DK, Cradock AL, Batchelder H, Gortmaker SL. Systematic review and meta-analysis of the impact of restaurant menu calorie labeling. Am J Public Health. 2015;105(5):e11–e24. doi: 10.2105/AJPH.2015.302570. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yach D, Calitz C. New opportunities in the changing landscape of prevention. JAMA. 2014;312(8):791–792. doi: 10.1001/jama.2014.8900. [doi] [DOI] [PubMed] [Google Scholar]
- 15.Gardner CD, Whitsel LP, Thorndike AN, et al. Food-and-beverage environment and procurement policies for healthier work environments. Nutr Rev. 2014;72(6):390–410. doi: 10.1111/nure.12116. [doi] [DOI] [PubMed] [Google Scholar]
- 16.Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. JAMA. 2007;298(20):2415–2417. doi: 10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- 17.Thaler RH, Sunstein CR. Nudge: Improving decisions about health, wealth, and happiness. New York, New York: Penguin Group; 2009. [Google Scholar]
- 18.Miles S, Scaife V. Optimistic bias and food. Nutrition Research Reviews. 2003;16:3–19. doi: 10.1079/NRR200249. [DOI] [PubMed] [Google Scholar]
- 19.Schultz PW, Nolan JM, Cialdini RB, Goldstein NJ, Griskevicius V. The constructive, destructive, and reconstructive power of social norms. Psychol Sci. 2007;18(5):429–434. doi: 10.1111/j.1467-9280.2007.01917.x. doi: PSCI1917 [pii] [DOI] [PubMed] [Google Scholar]
- 20.Thorndike AN, Sonnenberg L, Riis J, Barraclough S, Levy DE. A 2-phase labeling and choice architecture intervention to improve healthy food and beverage choices. Am J Public Health. 2012;102(3):527–533. doi: 10.2105/AJPH.2011.300391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levy DE, Riis J, Sonnenberg LM, Barraclough SJ, Thorndike AN. Food choices of minority and low-income employees: A cafeteria intervention. Am J Prev Med. 2012;43(3):240–248. doi: 10.1016/j.amepre.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thorndike AN, Riis J, Sonnenberg LM, Levy DE. Traffic-light labels and choice architecture: Promoting healthy food choices. Am J Prev Med. 2014;46:143–149. doi: 10.1016/j.amepre.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hanks AS, Just DR, Wansink B. Smarter lunchrooms can address new school lunchroom guidelines and childhood obesity. J Pediatr. 2013;162(4):867–869. doi: 10.1016/j.jpeds.2012.12.031. [doi] [DOI] [PubMed] [Google Scholar]
- 24.Skov LR, Lourenco S, Hansen GL, Mikkelsen BE, Schofield C. Choice architecture as a means to change eating behaviour in self-service settings: A systematic review. Obes Rev. 2013;14(3):187–196. doi: 10.1111/j.1467-789X.2012.01054.x. [DOI] [PubMed] [Google Scholar]
- 25.Sonnenberg L, Gelsomin E, Levy DE, Riis J, Barraclough S, Thorndike AN. A traffic light food labeling intervention increases consumer awareness of health and healthy choices at the point-of-purchase. Preventive Medicine. 2013;57:253–257. doi: 10.1016/j.ypmed.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roth DA, Herman CP, Polivy J, Pliner P. Self-presentational conflict in social eating situations: A normative perspective. Appetite. 2001;36(2):165–171. doi: 10.1006/appe.2000.0388. [doi] [DOI] [PubMed] [Google Scholar]
- 27.Pliner P, Mann N. Influence of social norms and palatability on amount consumed and food choice. Appetite. 2004;42(2):227–237. doi: 10.1016/j.appet.2003.12.001. [doi] [DOI] [PubMed] [Google Scholar]
- 28.Mollen S, Rimal RN, Ruiter RA, Kok G. Healthy and unhealthy social norms and food selection. findings from a field-experiment. Appetite. 2013;65:83–89. doi: 10.1016/j.appet.2013.01.020. [doi] [DOI] [PubMed] [Google Scholar]
- 29.Prinsen S, de Ridder DT, de Vet E. Eating by example: Effects of environmental cues on dietary decisions. Appetite. 2013;70:1–5. doi: 10.1016/j.appet.2013.05.023. [doi] [DOI] [PubMed] [Google Scholar]
- 30.Robinson E, Harris E, Thomas J, Aveyard P, Higgs S. Reducing high calorie snack food in young adults: A role for social norms and health based messages. Int J Behav Nutr Phys Act. 2013;10 doi: 10.1186/1479-5868-10-73. 73-5868-10-73. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robinson E, Thomas J, Aveyard P, Higgs S. What everyone else is eating: A systematic review and meta-analysis of the effect of informational eating norms on eating behavior. J Acad Nutr Diet. 2014;114(3):414–429. doi: 10.1016/j.jand.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 32.Robinson E, Fleming A, Higgs S. Prompting healthier eating: Testing the use of health and social norm based messages. Health Psychol. 2014;33(9):1057–1064. doi: 10.1037/a0034213. [doi] [DOI] [PubMed] [Google Scholar]
- 33.Opower. [Accessed September 16, 2014]; Http://Opower.com/platform/computer-science. Accessed. [Google Scholar]
- 34.Allcott H. Social norms and energy conservation. Journal of Public Economics. 2011;95:1082–1095. [Google Scholar]
- 35.Higgins ST, Wong CJ, Badger GJ, Ogden DEH, Dantona RL. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year follow-up. J of Consulting and Clinical Psychology. 2000;68:64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- 36.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: A randomized trial. JAMA. 2008;300(22):2631–2637. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Volpp KG, Troxel AB, Pauly MV, et al. A randomized, controlled trial of financial incentives for smoking cessation. N Engl J Med. 2009;360(7):699–709. doi: 10.1056/NEJMsa0806819. [DOI] [PubMed] [Google Scholar]
- 38.Finkelstein EA, Brown DS, Brown DR, Buchner DM. A randomized study of financial incentives to increase physical activity among sedentary older adults. Prev Med. 2008;47(2):182–187. doi: 10.1016/j.ypmed.2008.05.002. [doi] [DOI] [PubMed] [Google Scholar]
- 39.Mitchell MS, Goodman JM, Alter DA, et al. Financial incentives for exercise adherence in adults: Systematic review and meta-analysis. Am J Prev Med. 2013;45(5):658–667. doi: 10.1016/j.amepre.2013.06.017. [doi] [DOI] [PubMed] [Google Scholar]
- 40.French SA, Jeffery RW, Story M, Hannan P, Snyder MP. A pricing strategy to promote low-fat snack choices through vending machines. Am J Public Health. 1997;87(5):849–851. doi: 10.2105/ajph.87.5.849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.French SA, Jeffery RW, Story M, et al. Pricing and promotion effects on low-fat vending snack purchases: The CHIPS study. Am J Public Health. 2001;91(1):112–117. doi: 10.2105/ajph.91.1.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Block JP, Chandra A, McManus KD, Willett WC. Point-of-purchase price and education intervention to reduce consumption of sugary soft drinks. Am J Public Health. 2010;100(8):1427–1433. doi: 10.2105/AJPH.2009.175687. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Michels KB, Bloom BR, Riccardi P, Rosner BA, Willett WC. A study of the importance of education and cost incentives on individual food choices at the Harvard School of Public Health cafeteria. J Am Coll Nutr. 2008;27(1):6–11. doi: 10.1080/07315724.2008.10719669. doi:27/1/6 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Epstein LH, Jankowiak N, Nederkoorn C, Raynor HA, French SA, Finkelstein E. Experimental research on the relation between food price changes and food-purchasing patterns: A targeted review. Am J Clin Nutr. 2012;95(4):789–809. doi: 10.3945/ajcn.111.024380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bartlett S, Klerman J, Wilde P, et al. Healthy incentives pilot (HIP) interim report. [Accessed September 16, 2014];Prepared by ABT Associates for the U S Department of Agriculture, Food and Nutrition Service. 2013 Jul; www.fns.usda.gov/research-and-analysis.
- 46.Sturm R, An R, Segal D, Patel D. A cash-back rebate program for healthy food purchases in south africa: Results from scanner data. Am J Prev Med. 2013;44(6):567–572. doi: 10.1016/j.amepre.2013.02.011. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morrill BA, Madden GJ, Wengreen HJ, Fargo JD, Aguilar SS. A randomized controlled trial of the Food Dudes program: Tangible rewards are more effective than social rewards for increasing short- and long-term fruit and vegetable consumption. J Acad Nutr Diet. 2015 doi: 10.1016/j.jand.2015.07.001. doi: S2212-2672(15)01118-1 [pii] [DOI] [PubMed] [Google Scholar]
- 48.United States Department of Agriculture. Dietary guidelines for Americans. [Updated 2005June 11, 2009]; http://www.mypyramid.gov/guidelines/index.html.
- 49.U.S. Department of Agriculture and U.S Department of Health and Human Services, editor. Dietary guidelines for Americans, 2010. 7th. Washington D.C.: U.S. Government Printing Office; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 51.Pachucki MA, Jacques PF, Christakis NA. Social network concordance in food choice among spouses, friends, and siblings. Am J Public Health. 2011;101(11):2170–2177. doi: 10.2105/AJPH.2011.300282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ball K, Crawford D. Socioeconomic status and weight change in adults: A review. Soc Sci Med. 2005;60(9):1987–2010. doi: 10.1016/j.socscimed.2004.08.056. doi: S0277-9536(04)00467-8 [pii] [DOI] [PubMed] [Google Scholar]
- 53.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.