Abstract
The main purpose of this study was to examine the relationships between religiosity, social support, diabetes care and control and self-rated health of people living in Mexico who have been diagnosed with diabetes. Structural equation modeling was used to examine these associations using the Mexican Health and Aging Study, a national representative survey of older Mexicans. Findings indicate that emotional support from one’s spouse/partner directly affects diabetes care and control and health. Although there is no direct relationship between religiosity and health, religiosity was positively associated with diabetes care and control, but not significantly related to health.
Keywords: Religiosity, Social support, Diabetes self-management behaviors, Older Mexicans, Health outcomes
Introduction
A large body of literature has established the relationships between religiosity and health (Krause 2011; Krause and Bastida 2012; Salmoirago-Blotcher et al. 2011; Williams and Sternthal 2007), social support and health (Rosland et al. 2008; Uchino 2006) and self-management and health (Casagrande et al. 2013). But only a few studies have explored how these constructs interact for people with diabetes (Thomas and Washington 2012; Yuniarti et al. 2012). In addition, no previous research has explored these relationships among older Hispanics. The purpose of this study is to examine the relationships between social support, religiosity, care and health in older Mexicans that have been diagnosed with diabetes.
Background
Diabetes mellitus is a major public health challenge in Mexico. Recent estimates from the Mexican Health and Nutrition Survey (Encuesta Nacional de Salud y Nutrición; ENSA-NUT) suggest that 9 % of adults have been diagnosed with diabetes mellitus (Instituto Nacional de Salud Pública 2012). Mortality trends by age group show that diabetes primarily affects adults of working age and older adults; in fact, diabetes is among the three major causes of death for older adults (Instituto Nacional de Estadística y Geografía (INEGI) 2013). The impact of the disease on health care and hospitalization is substantial; the mean length of hospital stay for people with diabetes is 6.1 days compared to 3.5 days for people without diabetes (Rull et al. 2005). In 2006, total costs of diabetes care was USD $1164.8 million dollars in Mexico (Barquera et al. 2013). With an increasing percentage of older adults in Mexico predicted over the next few decades, the number of people with diabetes is likely to increase, and thus healthcare costs will also be likely to increase.
People with diabetes can reduce complications by managing and controlling their diabetes; they may need to follow a diet and exercise plan to help them control their glucose levels (Shrivastava et al. 2013). A limited number of studies have examined diabetes treatment and care among Mexicans. However, general findings from the literature suggest that Mexicans do not always have the knowledge or motivation to engage in self-management or comply with their treatment. For example, a study done by Baca Martínez et al. (2008) with a sample of 94 older adults 60 years and older, with a diabetes duration of at least 6 years or more, found that the majority lacked knowledge regarding biomedical treatment, exercise, diet and feet care. Surprisingly, 38 % mentioned that nobody had provided information regarding diabetes self-management. The data on specific practices are equally dramatic. Similarly, a study done using the ENSANUT by Rivera-Hernandez (2014) found that a very small percentage of older adults follow diabetes treatment and care guidelines.
Maintaining good diabetes management can be a complicated and frustrating task (Glasgow et al. 2001), and people with this condition may need support from family, friends and organizations to successfully manage their diabetes and to achieve good health outcomes. Social support has long been associated with health (Uchino 2006). The concept of social support is often related to different characteristics, which include network characteristics (size, strength), social relationships and ties (Ritter 1998). Social support may work via different processes. Social support buffers or moderates the effects of stress (Wallston et al. 1983), influences feelings of self-worth and self-efficacy (Callaghan and Morrissey 1993) and mediates by adherence lifestyle behaviors (Toljamo and Hentinen 2001). Due to the diversity in its definitions, social support is often operationalized with many measures including dichotomous indicators, scales and/or survey instruments. Furthermore, the differences in these definitions are also related to social networks, which may be considered to be a different construct. Although the meaning and operationalization of the construct are still evolving and debated, social support has been found to have positive influence with morbidity and mortality, including diabetes (Reblin and Uchino 2008; Rees et al. 2010). It has been found that diabetic people satisfied with the support received experience a better quality of life, and greater amount of support is related to better self-care practices with respect to exercise and diet (Tang et al. 2008). In fact, support from family and friends and professional support significantly predicted healthy eating and metabolic control (Whittemore et al. 2005).
Generally, religion is positively associated with health outcomes and well-being (Ellison and Levin 1998; Ferraro and Albrecht-Jensen 1991). Religious indicators (e.g., importance of religion, religious attendance, affiliation, membership and beliefs) seem to have salutary health effects on different conditions including some types of cancer, cardiovascular diseases, hypertension and stroke, as well as other general health problems (Levin and Schiller 1987). There is a significant interest in trying to understand the religion and health association. Several mechanisms by which religion may influence health have been discussed, including health behaviors and practices, psychosocial effects, psycho-dynamic processes and transcendental power (George et al. 2002; Idler et al. 2003). Given the multidimensionality of this construct and the wide range of possible pathways associated between religion and health, this is a complex area of study.
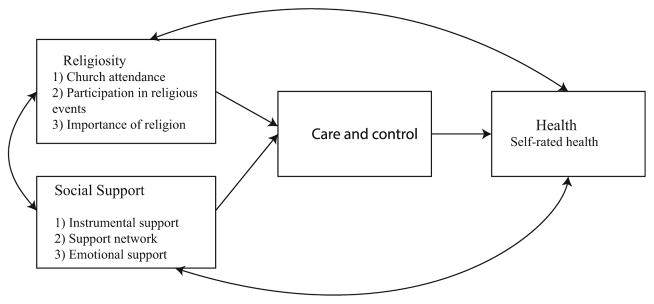
Some studies have started to explore religiosity and support together (Keating 2013; Krause and Hayward 2013). For example, using a sample of 132 African-Americans with diabetes, Watkins et al. (2013) found that social support from church members and religious beliefs were associated with aspects of diabetes care. However, not many studies have looked at the interrelationship among these constructs and health among Mexicans. Given the importance that Mexicans with diabetes place on religiosity (Tejada Tayabas et al. 2006) and social support (Salcedo-Rocha et al. 2008), the purpose of the present study was to examine the relationship between a composite measure of religiosity, multidimensional measures of social support (among those who have full support system), diabetes care and control and self-rated health of adults living in Mexico (see Fig. 1). Built on the studies mentioned above, the following predictions can be made:
Fig. 1.
Illustrates the conceptual model among religiosity, social support, self-management and health. Note It shows the main effects of religiosity and social support on self-rated health, and the mediator effect of self-management between religiosity and social support for people with diabetes. There are several self-reported characteristics that will be used as controls including demographic characteristics, comorbidities and risk factors
-
H1
Older Mexicans with diabetes with social support are more likely to have better diabetes care and control.
-
H2
Mexican adults with diabetes with social support are more likely to be healthier.
-
H3
Higher levels of religiosity are associated with better diabetes care and control.
-
H4
Those with higher levels of religiosity are more likely to rate themselves healthier.
-
H5
Higher levels of diabetes care and control are positively associated with better health.
-
H6
The effects of social support and religiosity are mediated by diabetes care and control.
Methodology
Data and Sample
Data came from the Mexican Health and Aging Study (MHAS) 2003 (MHAS 2013). Modeled after the US Health and Retirement Survey (HRS), the sample of Mexicans was 50 years and older from urban and rural areas from all 32 states in Mexico. The baseline data were collected in 2001 (N = 9719 households) with follow-up in 2003 (N = 8583 households). The questionnaire contains information in multiple domains including socio-demographics, health, healthcare services, housing, income, assets and pensions. Because social support and religiosity variable were only available in the second wave, the current study focused on Mexican older adults with diabetes in 2003. Of the 2216 (16 %) people with diabetes in the MHAS, 364 people provided information on support, religiosity variables and other covariates of interest.
Measures
Health
The dependent variable of primary interest in this study was the response to the single question: “Would you say your health is excellent, very good, good, fair or poor?” Among those with diabetes in this sample (2216), .4, 1 and 14 % reported their health as excellent, very good and good, whereas 57 and 28 % reported their health as fair and poor, respectively. A similar trend was found for the final sample. Therefore, this variable was trichotomized as (1) poor versus (2) fair versus (3) excellent/very good/good.
Religiosity
A composite score of religiosity was created using the three measures of religiosity included in the MHAS [the measures included subjective religiosity (the sense of religion’s importance), and/organizational religiosity (e.g., attendance at religious services)]. The questionnaire items that directly measure religiosity were: (1) “Do you attend religious services?” (Yes vs. No); (2) “How frequently do you participate in events organized by your church?” Never versus once in a while/once or more per week; (3) “How important is religion in your life?” Very important versus somewhat important/not important at all. These three items were added together to construct a religiosity index, and scores could range from 0 to 3. Similar indices have been used before (Preston et al. 2013).
Social Support
This study used three different measures of social support: support network size, instrumental support and emotional support.
Support network size was measured by adding the following items regarding connection in the community: (1) “Do you have good friends in the neighborhood?” and (2) “Do you have neighbors or friends you can count on for help?” Scores could range from 0 to 2.
Instrumental support was measured by adding the following items: (1) the financial support or in-kind support that you receive from your children, sons/daughters-in-law and grandchildren (and those of your spouse), would you say it is more than sufficient/suffi-cient vs. not sufficient; (2) the help with household chores, errands and transportation you received from your children, sons/daughters-in-law and grandchildren (and those of your spouse), would you say it is more than sufficient/sufficient versus not sufficient (based on the small percentage, <5 % of people who answered sufficient, these two responses were added together).
Finally, emotional support was assessed using a scale combining three different measures of support from respondents: (1) spouse, (2) children and (3) friends/acquaintances at work. The questions were asked only if the respondent had a spouse, children and coworkers. The three sets of four questions included information as to whether the (spouse; children; coworker) understand feelings about things; whether they can confide in (spouse; children; coworker) if they have a serious problem; whether (spouse; children; coworker) listen to their problems; and whether the [spouse; children; coworker] disappoint them (see Exhibit 1 in the “Appendix” for full questions). The first three items were reverse-coded, so those who perceived greater support had higher scores. Similar measures have been used before (Ekas et al. 2010).
Diabetes Care and Control
Self-management was measured adding the following dichotomous items: (1) Are you currently taking any oral medication in order to control your diabetes? Yes versus no; (2) Do you follow a special diet to control your diabetes? Yes versus no; (3) Do you measure your blood sugar level or urine sugar level? Never versus often/occasionally; (4) Is your diabetes under control? Yes versus no. Scores could range from 0 to 4. Similar indices have been used before (Lutfiyya et al. 2009).
Demographic Characteristics, Comorbidities and Health Risk Factors
There were several self-reported characteristics that were used as controls including demographic characteristics (sex, age, education, income). The MHAS research team created the income variable by calculating and totaling information on participant’s and spouse’s labor, family help and business income minus business expenditures (for more details about missing and imputing values, see MHAS 2013). The income variable was measured using tertiles to measure low, medium and high status. Number of chronic conditions included hypertension, heart disease, respiratory illness, arthritis and stroke. In addition, feeling pain and fatigue were also added. Smoking was measured by the following questions: Have you ever smoked cigarettes? Yes versus no, and drinking was measured by a question about whether and what the respondent drinks (beer, wine, liquor or pulque), yes versus no (McGowan 2013; Neylon et al. 2013).
Analysis
Structural equation modeling was used to examine specific hypotheses among religiosity, social support, diabetes care and control and health, while controlling for demographic characteristics, comorbidities and health risk factors. The approach was based on two steps. First, underlying constructs of emotional support (from spouse, children and coworkers) and their observed variables were evaluated using confirmatory factor analysis (CFA). This is referred to as the measurement model. Second, the hypotheses about the relationships between the latent factors and observed variables were tested in the structural model. In this step, all hypothesized paths were included first. Then, nonsignificant paths (p >.05) were fixed to zero to create a simplified and more parsimonious model. This reduced model was retested for model fit.
Due to the categorical nature of the data, maximum likelihood (ML) should not be used to estimate model fit (Brown 2006). The robust weighted least square (WLSM) estimator was used to obtain parameter estimates. WLSM is recommended for working with categorical data (Muthén and Muthén 1998). Several indices were used to estimate the fit of these models: Chi-square, root mean squared error of approximation (RMSEA), Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI) (Bollen 1989). RMSEA indicates model discrepancy per degrees of freedom, with values<.06 being indicative of good model fit. The CFI and TLI compare the fit of the estimated model to the null model, with values of .95 or higher being indicative of good model fit (Hu and Bentler 1999). SEM analyses were performed using Mplus 7 (Muthén and Muthén 1998).
Results
Of the 2216 people with diabetes in the MHAS 2003, there were 364 people 50 years and older who completed information on support, religiosity variables and other covariates of interest. Approximately 15 % rated their health as good, very good or excellent, and 38 % did not have other major chronic conditions. Only 19 % scored high on the self-management index. The majority of the sample was women (62 %), and the mean age was 62 (SD = 7.75). Good support network, family support and religiosity levels were most frequently reported among people in this subsample (59, 56 and 67 %, respectively). Further descriptive statistics for the study sample are presented in Table 1. Participants who did not answer support variables were similar to those who did. Analysis of variance (ANOVA), Chi-square and Kruskal–Wallis tests were conducted to assess relationships between the dependent and the independent variables. Self-rated health was associated with perceived emotional support from children (p = .02, Kruskal–Wallis test) and marginally associated with perceived emotional support from partners (p = .06, Kruskal–Wallis test). Self-rated health was also associated with diabetes care and control (p = .01, Chi squared test), age (p = .04, ANOVA test), education (p <.0001, ANOVA test), comorbidities (p <.0001, ANOVA test), fatigue (p <.0001, Chi-squared test) and pain (p <.0001, Chi-squared test). Diabetes care and control was significantly associated with religiosity (p = .02, Chi-squared test), fatigue (p = .05, Chi-squared test) and drinking (p = .003, Chi-squared test).
Table 1.
Characteristics of the study subsample (n = 364) from the MHAS of Mexicans with diabetes
| Variable | Mean |
|---|---|
| Self-rated health (%) | |
| Good/very good/excellent | 15.11 |
| Fair | 54.12 |
| Poor | 30.77 |
| Diabetes care and control (%) | |
| Good self-management | 19.51 |
| Fair self-management | 42.03 |
| Poor self-management | 38.46 |
| Religiosity (%) | |
| Very religious | 67.03 |
| Religious | 22.25 |
| Least religious | 10.71 |
| Instrumental support (%) | |
| Good family support | 56.04 |
| Fair family support | 14.01 |
| Poor family support | 29.95 |
| Support network (%) | |
| Good support network | 58.79 |
| Fair support network | 27.20 |
| Poor support network | 14.01 |
| Emotional support from spouse | 10.43 (2.11) |
| Emotional support from children | 10.79 (1.74) |
| Emotional support from coworkers | 9.59 (2.10) |
| Demographic | |
| Age | |
| Mean in years ± SD | 61.88 (7.75) |
| Education | |
| Mean in years ± SD | 4.51 (3.97) |
| Gender (%) | |
| Female | 62.09 |
| Income (%) | |
| High income tertile | 33.79 |
| Medium income tertile | 33.24 |
| Low income tertile | 33.79 |
| Comorbidities and risk factors | |
| Number of chronic conditions (%) | |
| 0 | 38.46 |
| 1 | 42.03 |
| 2 or more | 19.51 |
| Fatigue (%) | 35.44 |
| Pain (%) | 54.95 |
| Smoking (%) | 35.99 |
| Drinking (%) | 18.68 |
SEM
Measurement Model
The measurement model for the three emotional support latent variables was first estimated. Latent constructs were allowed to correlate freely since it was suspected that they would be correlated with each other. The model fit showed a good fit for the data with a χ2 (48) = 58.37, p >.05; RMSEA = .02, CFI = .99, TLI = .99. All the factor loadings from observed variables were significantly different from 0, indicating that the latent factors were measured by the observed variables.
SEM of Self-Rated Health for People with Diabetes
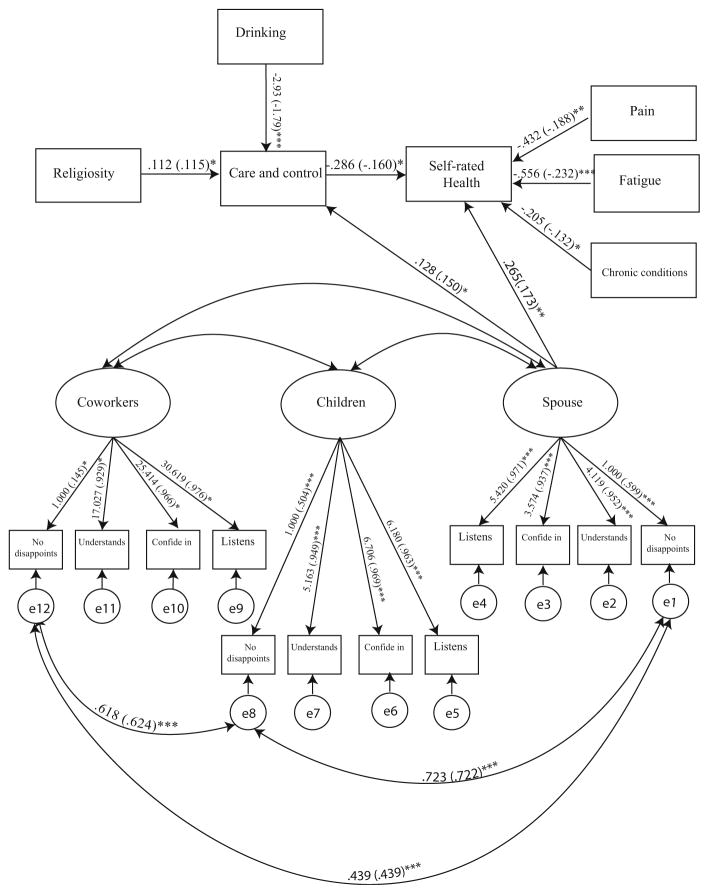
The original, hypothesized SEM model included all emotional support scales from spouse, children and coworkers, instrumental support and support network. This hypothesized model was examined to test the relationship between variables and constructs. Indices in this model were generally in the range of the recommended values, thereby indicating a good fit [i.e., χ2 (230) = 274.15, p <.05; RMSEA = .02, CFI = .99, TLI = .99]. Although all the paths were estimated in the model, only significant paths are shown in this figure to get a better understanding of how social support, religiosity and diabetes care and control influence health. Nonsignificant paths were constrained to zero, creating a refined and more parsimonious model. Fit indices for the final reduced model were good [χ2 (253) = 297.64, p <.05; RMSEA = .02, CFI = .99, TLI = .99]. The reduced model is shown in Fig. 2. There was not a significant difference in model fit between the full and reduced models [Δ χ2 (23) = 24.84, p >.05]; therefore, the simpler model was retained.
Fig. 2.
“Trimmed” structural equation model of the relationship between social support, religiosity, self-management and health. Note Numbers in parenthesis are the standardized values
Assessment of Study Hypotheses
Optional support from husband was related to diabetes care and control (β = .15 p = .02). Other support constructs such as emotional support from children and coworkers, instrumental support and support network were not associated with diabetes care and control. Emotional support from spouse was the only support variable that was associated with health (β = .17 p = .01). The results did not show any other significant paths between other emotional constructs of social support, instrumental support, support network and health. Religiosity was positively associated with diabetes care and control (β = .11 p = .01), but not significantly related to health. Those who have good diabetes care and control were more likely to have worse health (β = −.16 p = .01). According to these results, the effects of social support on health were not mediated by diabetes care and control, whereas religiosity seems to be associated with health via diabetes care and control (Table 2).
Table 2.
The results of the hypothesized relationships between social support, religiosity, self-management and self-rated health for older Mexicans with diabetes
| Variables | Health | Self-management |
|---|---|---|
| Social support variables | ||
| Emotional support spouse | Significant | Significant |
| Emotional support children | Not significant | Not significant |
| Emotional support coworkers | Not significant | Not significant |
| Instrumental support | Not significant | Not significant |
| Support network | Not significant | Not significant |
| Religiosity | Not significant | Significant |
| Self-management | Significant | N/A |
Emotional support from spouse had a direct effect on self-management and health. Religiosity had only a significant effect on self-management. Religiosity showed a marginality significant indirect effect through self-management on health. No indirect effects between social support and health were found
Discussion
The goal of the present study was to examine the relationships between social support, religiosity, diabetes care and control and self-rated health among Mexican adults with diabetes and to investigate whether religiosity and/or social support work wholly or partially on self-rated health. The conceptual model proposed in this study suggested a direct relationship between social support and health, and religiosity and health, as well as relationships between social support and religiosity to diabetes care and control. Finally, an association between diabetes care and control and health was drawn. The results supported some of the hypothesis. Findings indicate that emotional support from spouse/partner directly affects diabetes care and control and health. However, there is no direct relationship between religiosity and health and other forms of social support on health. Finally, the effects of social support to health are not mediated by diabetes care and control. Health only appears to be potentially mediated by religiosity. It is important to mention that the findings discussed in this study are limited by the nature of the sample used. Although not uncommon for older adults in Mexico (INEGI 2005), there were 364 people in the sample who could potentially have a full support system. Including emotional support measures enables a deeper examination of the quality of the support received and how they affect self-management and health for people with diabetes.
Effects of Social Support on Diabetes Care and Control and Health
Family support has been associated with self-care behaviors such as diet and exercise and fewer barriers to diabetes care (Strom and Egede 2012). Researchers have previously reported that a supportive relationship is one of the most important sources of support during diabetes management (Franks et al. 2012). Trief et al. (2004) found that supportive marriages are a strong predictor of self-care activities; a plausible explanation for this is that intimacy is related to adaptation. When a partner develops diabetes, changes must occur and there could be situations generating stresses and strains. Partners might be expected to be involved in medication administration, preparing diabetic-friendly meals and exercise activities. When these changes are experienced with a supportive partner and the couple works together to make these adjustments, the partner with diabetes may feel motivated to adhere to treatment (Franks et al. 2012). The converse may happen if the partner with diabetes is working alone with his/her care regimen. A distant/conflicted relationship may also cause frustration, dissatisfaction and a lack of motivation to follow recommendations (Iida et al. 2013).
With regard to social support and health, familial support has also been shown to be strongly related to good health outcomes (Westaway et al. 2005). The current study suggests that close and affectionate relationships seem to play a key role for the health of older Mexicans with diabetes. Although one may expect that support is directly related to health (e.g., glycemic control) through self-care behaviors such as glucose testing, diet and exercise (Brody et al. 2008), this appeared not to be the case for people in this sample. Those who have emotional support from their spouse were more likely to engage in self-care activities, but self-care activities were not subsequently associated with good health. Effects of emotional support have also been explained in relation to psychological well-being (Goetz et al. 2012). In addition, other factors not accounted for in this study may mediate the relationship between emotional support and health. Future studies should add dimensions of glycemic control, quality of life and psychological well-being.
Earlier evidence has shown the importance of peer support on diabetes management (Pendley et al. 2002). However, in a clinical trial, Smith et al. (2011) found that peer support has no impact on health outcomes for people with diabetes. In this particular sample of married people, coworkers and friends may lack knowledge about diabetes and self-care behaviors and the importance of disease management and adherence to regimens may not offer support that is positive or negative to diabetes compliance (Rosland et al. 2008). Since most of the studies done with perceived support from peers and/or friends have been done with children and younger people with type 1 diabetes (Palladino and Helgeson 2012), future studies should also evaluate the role of social support from coworkers and friends in self-care behaviors and health for older Mexicans with diabetes.
Religiosity and Self-Management Relationship
Another finding of the present study was the positive association between religiosity and self-care behaviors. This finding is not surprising as previous studies have reported that religion influences health practices of people with diabetes (Newlin et al. 2008). Taken together, the evidence shows that higher levels of religiosity promote healthier behaviors in Hispanics. This is consistent with findings from Hill et al. (2006). They reported that religious involvement predicted higher rates of physical activity and lower levels of smoking and drinking in people living in Texas.
Contrary to what one might expect, there was no direct relationship between religiosity and health. Prior studies have reported that religious attendance and subjective religiosity seem to be associated with self-rated health. Green et al. (2004) found that Latino elders who reported religious affiliation were more likely to rate their health as fair or poor, but those who reported that religion was very important were less likely to rate their health as fair/poor. Due to the complexity of diabetes self-management and the important role of self-care practices in preventing morbidity and mortality, researchers need to better understand religiosity and social support and other mechanisms that impact the self-management and health of this chronic condition.
Several studies have used church attendance as the main measure of religiosity. An important contribution of this study is the one composite measure of religiosity that included items such as church attendance, importance or religion, and attendance to church activities was used to test paths between self-management and health. Religiosity needs to be explored using multiple and more diverse measures of religiosity, and research should move beyond using religious attendance as a sole indicator of this complex measure.
Self-Management and Health
Contrary to what one may expect, self-rated health was negatively associated with self-management. Self-management in the present study was operationalized with an index of four items. Items were separated to explore whether a single item was the source of this negative association; however, all items were negatively correlated with self-rated health. Also, these correlations were inversely related for the full sample of people with diabetes.
A likely explanation for these findings is that most prior studies were clinical trials with few participants and longitudinal data. In the present study, older adults may report their health fair/poor because of limiting factors such as diet, exercise or other management behaviors. The rigorousness of these activities for management of health may affect their perspective of their health. Self-care activities such as diet and glucose testing may be perceived as a burden and a constant reminder of being sick. Also, managing the day-today aspects of diabetes could be considered draining and stressful. So individuals who may be actively involved in self-management may think of diabetes self-management as a rigorous process that they have to follow because they are ill. Another possibility is that adults with negative self-perceptions of health may overcompensate with excessive self-care activities. Individuals with severe diabetes, especially those whose health is poor, may be proceeding with a healthier diet, monitoring blood sugars and try to keep their diabetes under control and to improve health outcomes. Finally, duration of the disease may also have an influence on participant responses. Those who have had the disease longer and have diabetes complications may rate their health poorer than those who are newly diagnosed. It will be interesting to determine how these and other psychosocial measures contribute or influence to health perceptions. The use of longitudinal measures to investigate the causal relationships may also be required.
Limitations and Future Directions
There are several limitations to this study. First, the study did not solely use people diagnosed with diabetes as originally intended. The sample was reduced to those who have children, were married and have friends and acquaintances at work. Further research with a larger and more diverse population is needed beyond people with partners and children and to enhance the generalizability of the results. Future interventions may focus on identifying couples that need to be enrolled in diabetes education classes and assess emotional support, self-management and health outcomes.
Second, some would suggest that self-report health status and diagnostic information are a limitation relative to biological measures such as HbA1c or blood pressure or even other direct measures. However, gathering clinical parameters such as these requiring careful protocols also have limitations, including cost, multiple blood pressure measures and even fasting glucose (McFall et al. 2014) as is done in National Health and Nutrition Examination Survey (NHANES) or specialized diagnosis services designed to minimize diagnostic errors. Furthermore, numerous epidemiologic studies from the Alameda County to Health and Retirement Survey (HRS) to NHANES have relied upon self-report information pertaining to the presence of disease. In fact, Medicare Consumer Assessment of Health-care Providers and Systems (CAHPS) case mix adjustment includes self-rated health (Farley et al. 2011). Finally, self-reported health has been repeatedly shown to be strongly predictive of hospitalizations and survival, and the only reasonable way to obtain information about individuals’ health habits is to ask them (Chamberlain et al. 2013; Kennedy et al. 2001; Nielsen 2015).
Finally, since the data were cross-sectional, (1) all the parameters were reported at one point in time, (2) causal inferences cannot be made, (3) there may be issues around endogeneity, and (4) the findings could be due to other factors (e.g., stress, coping and psychological distress) that could mediate the relationship between social support, religiosity, self-management and health. A longitudinal study should help to shed light on potential factors associated with religiosity, social support and health. Longitudinal analysis could help us understand how social support increases or decreases after someone has been diagnosed with diabetes. It may also provide information about the severity and the duration of the disease and how this influences the quality of the support received, religiosity levels, self-management behaviors and health.
Implications
Despite the limitations, these findings suggest the importance of spousal support in diabetes management and health and religiosity in diabetes management. Diabetes education classes should be available and open to people with diabetes and their partners. Physicians, nurses, diabetes educators and other health professionals should discuss support available in patients’ lives and the importance of support from family members in diabetes self-management and health. Religious leaders and health professionals could also emphasize how these sources of support may benefit treatment adherence for people with diabetes. Similarly, religious practitioners may also discuss the influence of religion and self-care activities for church members and the community. Engaging members with diabetes and other chronic conditions in prayer groups, bible studies and other services may increase their ability to cope with the disease and provide sources of social support. This may also suggest the importance of establishing partnerships with religious institutions and the medical community. These partnerships may increase health promotion programs for people with diabetes and provide holistic care in healthcare organizations.
Acknowledgments
I want to thank Drs. Suzanne Kunkel, Scott Brown, Robert Applebaum, Jennifer Bulanda, John Bailer and the anonymous reviewer for their valuable feedback on this project. This project was supported by Grant Number T32HS000011 from the Agency for Healthcare Research and Quality and The New York Community Trust, Fahs-Beck Fund for Research and Experimentation. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Appendix
Exhibit 1
About your spouse…
How much does your spouse understand your feelings about things? Would you say…a lot, little, or not at all
How much can you confide in him/her if you have a serious problem? Would you say…a lot, little, or not at all
How much does your spouse listen if you need to talk about your worries? Would you say…a lot, little, or not at all
How often does he/she disappoint you when you are counting him/her? Would you say…a lot, little, or not at all
About your children…
How much do they understand your feelings about things? Would you say…a lot, little, or not at all
How much can you confide in them if you have a serious problem? Would you say…a lot, little, or not at all
How much do they listen if you need to talk about your worries? Would you say…a lot, little, or not at all
How often do they disappoint you when you are counting on them? Would you say…a lot, little, or not at all
About your friends, acquaintances, or companions at work
How much do they understand your feelings about things? Would you say…a lot, little, or not at all
How much can you confide in them if you have a serious problem? Would you say…a lot, little, or not at all
How much do they listen if you need to talk about your worries? Would you say…a lot, little, or not at all
How often do they disappoint you when you are counting on them? Would you say…a lot, little, or not at all
References
- Baca Martínez B, Bastidas Loaíza MJ, del R, Aguilar M, De La Cruz Navarro MDJ, Gonzáles Delgado MD, Uriarte Ontiveros S, Flores PF. Nivel de conocimientos del diabético sobre su auto cuidado. Enfermería Global. 2008 doi: 10.6018/eglobal.7.2.14691. [DOI] [Google Scholar]
- Barquera S, Campos-Nonato I, Aguilar-Salinas C, Lopez-Ridaura R, Arredondo A, Rivera-Dom-marco J. Diabetes in Mexico: Cost and management of diabetes and its complications and challenges for health policy. Globalization and Health. 2013;9:3. doi: 10.1186/1744-8603-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- Brody GH, Kogan SM, Murry VM, Chen Y, Brown AC. Psychological functioning, support for self-management, and glycemic control among rural African American adults with diabetes mellitus type 2. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2008;27(1 Suppl):S83–S90. doi: 10.1037/0278-6133.27.1.S83. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. New York: Guilford Press; 2006. [Google Scholar]
- Callaghan P, Morrissey J. Social support and health: A review. Journal of Advanced Nursing. 1993;18(2):203–210. doi: 10.1046/j.1365-2648.1993.18020203.x. [DOI] [PubMed] [Google Scholar]
- Casagrande SS, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1C, blood pressure, and LDL goals among people with diabetes, 1988–2010. Diabetes Care. 2013;36(8):2271–2279. doi: 10.2337/dc12-2258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain AM, McNallan SM, Dunlay SM, Spertus JA, Redfield MM, Moser DK, et al. Physical health status measures predict all-cause mortality in patients with heart failure. Circulation Heart Failure. 2013;6(4):669–675. doi: 10.1161/CIRCHEARTFAILURE.112.000291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekas NV, Lickenbrock DM, Whitman TL. Optimism, social support, and well-being in mothers of children with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2010;40(10):1274–1284. doi: 10.1007/s10803-010-0986-y. [DOI] [PubMed] [Google Scholar]
- Ellison CG, Levin JS. The religion-health connection: Evidence, theory, and future directions. Health Education and Behavior. 1998;25(6):700–720. doi: 10.1177/109019819802500603. [DOI] [PubMed] [Google Scholar]
- Farley DO, Elliott MN, Haviland AM, Slaughter ME, Heller A. Understanding variations in medicare consumer assessment of health care providers and systems scores: California as an example. Health Services Research. 2011;46(5):1646–1662. doi: 10.1111/j.1475-6773.2011.01279.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro KF, Albrecht-Jensen CM. Does religion influence adult health? Journal for the Scientific Study of Religion. 1991;30(2):193–202. doi: 10.2307/1387213. [DOI] [Google Scholar]
- Franks MM, Seda Z, Seidel AJ, Shields CG, Oates SK, Boushey CJ. Table for two: Diabetes distress and diet-related interactions of married patients with diabetes and their spouses. Families, Systems, and Health. 2012;30(2):154–165. doi: 10.1037/a0028614. [DOI] [PubMed] [Google Scholar]
- George LK, Ellison CG, Larson DB. Explaining the relationships between religious involvement and health. Psychological Inquiry. 2002;13(3):190–200. doi: 10.1207/S15327965PLI1303_04. [DOI] [Google Scholar]
- Glasgow RE, Toobert DJ, Gillette CD. Psychosocial barriers to diabetes self-management and quality of life. Diabetes Spectrum. 2001;14(1):33–41. doi: 10.2337/diaspect.14.1.33. [DOI] [Google Scholar]
- Goetz K, Szecsenyi J, Campbell S, Rosemann T, Rueter G, Raum E, et al. The importance of social support for people with type 2 diabetes—A qualitative study with general practitioners, practice nurses and patients. GMS Psycho-Social-Medicine. 2012 doi: 10.3205/psm000080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green BL, Lewis RK, Wang MQ, Person S, Rivers B. Powerlessness, destiny, and control: The influence on health behaviors of African Americans. Journal of Community Health. 2004;29(1):15–27. doi: 10.1023/b:johe.0000007442.70657.75. [DOI] [PubMed] [Google Scholar]
- Hill TD, Burdette AM, Ellison CG, Musick MA. Religious attendance and the health behaviors of Texas adults. Preventive Medicine. 2006;42(4):309–312. doi: 10.1016/j.ypmed.2005.12.005. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- Idler EL, Musick MA, Ellison CG, George LK, Krause N, Ory MG, et al. Measuring multiple dimensions of religion and spirituality for health research conceptual background and findings from the 1998 General Social Survey. Research on Aging. 2003;25(4):327–365. doi: 10.1177/0164027503025004001. [DOI] [Google Scholar]
- Iida M, Stephens MAP, Franks MM, Rook KS. Daily symptoms, distress and interaction quality among couples coping with type 2 diabetes. Journal of Social and Personal Relationships. 2013;30(3):293–300. doi: 10.1177/0265407512455308. [DOI] [Google Scholar]
- INEGI. Los Adultos Mayores en México. Perfilsociodemográfico al inicio del siglo XXI. 2005 Retrieved from http://www.inegi.gob.mx/prod_serv/contenidos/espanol/bvinegi/productos/censos/poblacion/adultosmayores/Adultos_mayores_web2.pdf.
- Instituto Nacional de Estadística y Geografía (INEGI) Estadísticas demográficas 2011. INEGI; 2013. pp. 1–234. (No. 304.6021072) Retrieved from http://www.inegi.org.mx/prod_serv/contenidos/espanol/bvinegi/productos/continuas/vitales/demograficas/2011/cua_est_dem2011.pdf. [Google Scholar]
- Instituto Nacional de Salud Pública. ENSANUT. 2012 Retrieved November 1, 2013, from http://ensanut.insp.mx/
- Keating DM. Spirituality and support: A descriptive analysis of online social support for depression. Journal of Religion and Health. 2013;52(3):1014–1028. doi: 10.1007/s10943-012-9577-x. [DOI] [PubMed] [Google Scholar]
- Kennedy BS, Kasl SV, Vaccarino V. Repeated hospitalizations and self-rated health among the elderly: A multivariate failure time analysis. American Journal of Epidemiology. 2001;153(3):232–241. doi: 10.1093/aje/153.3.232. [DOI] [PubMed] [Google Scholar]
- Krause N. Religion and health: Making sense of a disheveled literature. Journal of Religion and Health. 2011;50(1):20–35. doi: 10.1007/s10943-010-9373-4. [DOI] [PubMed] [Google Scholar]
- Krause N, Bastida E. Religion and health among older Mexican Americans: Exploring the influence of making mandas. Journal of Religion and Health. 2012;51(3):812–824. doi: 10.1007/s10943-010-9389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause N, Hayward RD. Church-based social support, religious commitment, and health among older Mexican Americans. Journal of Social and Personal Relationships. 2013 doi: 10.1177/0265407513494952. [DOI] [Google Scholar]
- Levin JS, Schiller PL. Is there a religious factor in health? Journal of Religion and Health. 1987;26(1):9–36. doi: 10.1007/BF01533291. [DOI] [PubMed] [Google Scholar]
- Lutfiyya MN, Patel YR, Steele JB, Tetteh BS, Chang L, Aguero C, et al. Are there disparities in diabetes care? A comparison of care received by US rural and non-rural adults with diabetes. Primary Health Care Research and Development. 2009;10(04):320–331. doi: 10.1017/S146342360999017X. [DOI] [Google Scholar]
- McFall SL, Conolly A, Burton J. Collecting biomarkers using trained interviewers. Lessons learned from a pilot study. Survey Research Methods. 2014;8(1):57–65. [Google Scholar]
- McGowan P. The challenge of integrating self-management support into clinical settings. Canadian Journal of Diabetes. 2013;37(1):45–50. doi: 10.1016/j.jcjd.2013.01.004. [DOI] [PubMed] [Google Scholar]
- MHAS. MHAS. 2013 Retrieved December 10, 2013, from http://www.mhasweb.org/
- Muthén LK, Muthén BO. Mplus user’s guide. 1998, 2012 Retrieved from http://www.statmodel.com/download/usersguide/Mplus%20user%20guide%20Ver_7_r6_web.pdf.
- Newlin K, Melkus GD, Tappen R, Chyun D, Koenig HG. Relationships of religion and spirituality to glycemic control in Black women with type 2 diabetes. Nursing Research. 2008;57(5):331–339. doi: 10.1097/01.NNR.0000313497.10154.66. [DOI] [PubMed] [Google Scholar]
- Neylon OM, O’Connell MA, Skinner TC, Cameron FJ. Demographic and personal factors associated with metabolic control and self-care in youth with type 1 diabetes: A systematic review. Diabetes/Metabolism Research and Reviews. 2013;29(4):257–272. doi: 10.1002/dmrr.2392. [DOI] [PubMed] [Google Scholar]
- Nielsen TH. The relationship between self-rated health and hospital records. Health Economics. 2015 doi: 10.1002/hec.3167. [DOI] [PubMed] [Google Scholar]
- Palladino DK, Helgeson VS. Friends or foes? A review of peer influence on self-care and glycemic control in adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2012;37(5):591–603. doi: 10.1093/jpepsy/jss009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pendley JS, Kasmen LJ, Miller DL, Donze J, Swenson C, Reeves G. Peer and family support in children and adolescents with type 1 diabetes. Journal of Pediatric Psychology. 2002;27(5):429–438. doi: 10.1093/jpepsy/27.5.429. [DOI] [PubMed] [Google Scholar]
- Preston JL, Ritter RS, Hepler J. Neuroscience and the soul: Competing explanations for the human experience. Cognition. 2013;127(1):31–37. doi: 10.1016/j.cognition.2012.12.003. [DOI] [PubMed] [Google Scholar]
- Reblin M, Uchino BN. Social and emotional support and its implication for health. Current Opinion in Psychiatry. 2008;21(2):201–205. doi: 10.1097/YCO.0b013e3282f3ad89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees CA, Karter AJ, Young BA. Race/ethnicity, social support, and associations with diabetes self-care and clinical outcomes in NHANES. The Diabetes Educator. 2010;36(3):435–445. doi: 10.1177/0145721710364419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritter C. Social supports, social networks, and health behaviors. In: Gochman DS, editor. Health behavior. Springer; US: 1998. pp. 149–161. Retrieved from http://link.springer.com/chapter/10.1007/978-1-4899-0833-9_8. [Google Scholar]
- Rivera-Hernandez M. Depression, self-esteem, diabetes care and self-care behaviors among middle-aged and older Mexicans. Diabetes Research and Clinical Practice. 2014 doi: 10.1016/j.diabres.2014.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosland AM, Kieffer E, Israel B, Cofield M, Palmisano G, Sinco B, et al. When is social support important? The association of family support and professional support with specific diabetes self-management behaviors. Journal of General Internal Medicine. 2008;23(12):1992–1999. doi: 10.1007/s11606-008-0814-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rull JA, Aguilar-Salinas CA, Rojas R, Rios-Torres JM, Gómez-Pérez FJ, Olaiz G. Epidemiology of type 2 diabetes in Mexico. Archives of Medical Research. 2005;36(3):188–196. doi: 10.1016/j.arcmed.2005.01.006. [DOI] [PubMed] [Google Scholar]
- Salcedo-Rocha AL, de Alba-García JEG, Sevila E. Cultural domain of self-care in type 2 diabetes patients with and without blood glucose control in Mexico. Revista de Saúde Pública. 2008;42(2):256–264. doi: 10.1590/S0034-89102008000200010. [DOI] [PubMed] [Google Scholar]
- Salmoirago-Blotcher E, Fitchett G, Ockene JK, Schnall E, Crawford S, Granek I, et al. Religion and healthy lifestyle behaviors among postmenopausal women: The women’s health initiative. Journal of Behavioral Medicine. 2011;34(5):360–371. doi: 10.1007/s10865-011-9322-z. [DOI] [PubMed] [Google Scholar]
- Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. Journal of Diabetes and Metabolic Disorders. 2013;12(1):14. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SM, Paul G, Kelly A, Whitford DL, O’Shea E, O’Dowd T. Peer support for patients with type 2 diabetes: Cluster randomised controlled trial. BMJ : British Medical Journal. 2011 doi: 10.1136/bmj.d715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strom JL, Egede LE. The impact of social support on outcomes in adult patients with type 2 diabetes: A systematic review. Current Diabetes Reports. 2012;12(6):769–781. doi: 10.1007/s11892-012-0317-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang TS, Brown MB, Funnell MM, Anderson RM. Social support, quality of life, and self-care behaviors among african americans with type 2 diabetes. The Diabetes Educator. 2008;34(2):266–276. doi: 10.1177/0145721708315680. [DOI] [PubMed] [Google Scholar]
- Tejada Tayabas LM, Grimaldo Moreno BE, Maldonado Rodríguez O. Percepciones de enfermos diabéticos y familiares acerca del apoyo familiar y el padecimiento. 2006 Retrieved October 24, 2013, from http://www.respyn.uanl.mx/vii/1/comunicaciones/percepeciones_diabetes.htm.
- Thomas CJ, Washington TA. Religiosity and social support: Implications for the health-related quality of life of African American hemodialysis Patients. Journal of Religion and Health. 2012;51(4):1375–1385. doi: 10.1007/s10943-011-9483-7. [DOI] [PubMed] [Google Scholar]
- Toljamo M, Hentinen M. Adherence to self-care and social support. Journal of Clinical Nursing. 2001;10(5):618–627. doi: 10.1046/j.1365-2702.2001.00520.x. [DOI] [PubMed] [Google Scholar]
- Trief PM, Ploutz-Snyder R, Britton KD, Weinstock RS. The relationship between marital quality and adherence to the diabetes care regimen. Annals of Behavioral Medicine. 2004;27(3):148–154. doi: 10.1207/s15324796abm2703_2. [DOI] [PubMed] [Google Scholar]
- Uchino BN. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Wallston BS, Alagna SW, DeVellis BM, DeVellis RF. Social support and physical health. Health Psychology. 1983;2(4):367–391. doi: 10.1037/0278-6133.2.4.367. [DOI] [Google Scholar]
- Watkins YJ, Quinn LT, Ruggiero L, Quinn MT, Choi YK. Spiritual and religious beliefs and practices and social support’s relationship to diabetes self-care activities in African Americans. The Diabetes Educator. 2013;39(2):231–239. doi: 10.1177/0145721713475843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westaway MS, Seager JR, Rheeder P, Van Zyl DG. The effects of social support on health, well-being and management of diabetes mellitus: A black South African perspective. Ethnicity and Health. 2005;10(1):73–89. doi: 10.1080/1355785052000323047. [DOI] [PubMed] [Google Scholar]
- Whittemore R, Melkus GD, Grey M. Metabolic control, self-management and psychosocial adjustment in women with type 2 diabetes. Journal of Clinical Nursing. 2005;14(2):195–203. doi: 10.1111/j.1365-2702.2004.00937.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Sternthal MJ. Spirituality, religion and health: Evidence and research directions. Medical Journal of Australia. 2007;186(10) doi: 10.5694/j.1326-5377.2007.tb01040.x. Retrieved from https://www.mja.com.au/journal/2007/186/10/spirituality-religion-and-health-evidence-and-research-directions. [DOI] [PubMed] [Google Scholar]
- Yuniarti KW, Dewi C, Ningrum RP, Widiastuti M, Asril NM. Illness perception, stress, religiosity, depression, social support, and self management of diabetes in Indonesia. International Journal of Research Studies in Psychology. 2012 doi: 10.5861/ijrsp.2012.185. [DOI] [Google Scholar]