Abstract
With the growing use of ultrasound for pain management, we are interested in how to teach and practice ultrasound-guided procedures. Ethically, we should not insert a needle in a patient until after much practice on a phantom. Several types of phantoms have been introduced for ultrasound training, including water, agar/gelatin, elastomeric rubber, and meat phantoms and cadavers. The ideal phantom is similar to human tissue, is readily available and inexpensive, can be used repeatedly, provides tactile feedback, will hold a needle in place, does not generate needle tracks, and is not a health hazard. Several studies have shown the effectiveness of phantoms for improving the proficiency of novices. We hope that the application of phantoms in education leads to improved proficiency and increased patient safety.
Keywords: Gelatin, Phantom, Proficiency, Resident training, Simulation, Ultrasound
INTRODUCTION
The rapid growth of the use of ultrasound in pain management has raised concern about how to teach and practice ultrasound-guided procedures. Novices usually train for ultrasound-guided procedures in cadaver workshops or by performing the procedures on patients. However, cadavers are not readily available [1], and it is not advisable to practice first-time needle placement on a patient. Therefore, we need to use ultrasound phantoms. Numerous phantoms have been introduced for ultrasound training, including water, agar/gelatin, Blue, and meat phantoms and cadavers. This article gives an overview of phantoms for ultrasound guidance and their application in education.
CHARACTERISTICS OF A GOOD PHANTOM
The more of the following characteristics that an ultrasound phantom has, the more ideal it is [2]. A good phantom (a) has the echogenicity of human tissues, (b) is readily available and (c) inexpensive, (d) can be used repeatedly, (e) provides tactile feedback, (f) will hold a needle in place, (g) does not generate needle tracks, and (h) does not cause exposure to potential health hazards. To my knowledge, there has been no study that demonstrated the comparisons of characteristics between different models. Table 1 shows the grading of these attributes of ultrasound phantoms.
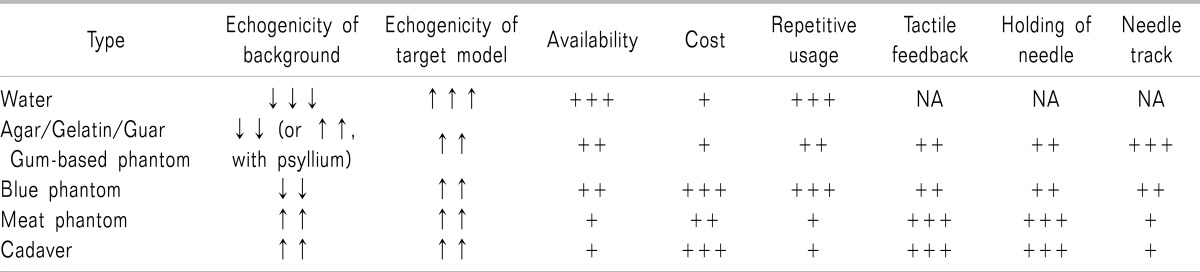
Table 1. Grading of Attributes in Various Ultrasound Phantoms.
↑: hyperechogenic, ↓: hypoechogenic, +: lowest grade, +++: highest grade, NA: not applicable.
1. Water
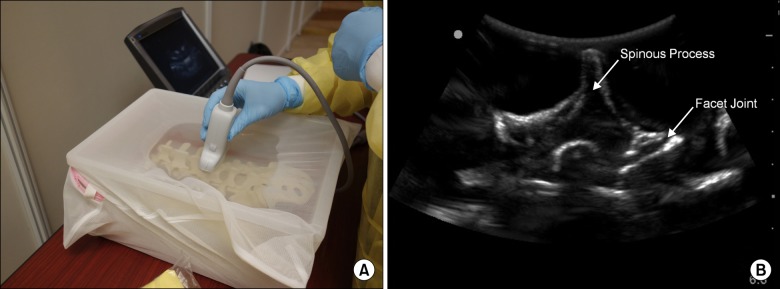
water phantom is a watertight container with a submerged target model. Water makes the background hypoechoic, allowing easy visualization of the target and needle. Water phantoms are readily available, inexpensive, and reusable. However, they provide no tactile feedback, since water cannot hold the needle in place. Therefore, water phantoms are useless for teaching and practicing ultrasound-guided needle performance, except for the identification of sonoanatomy and the development of new needle techniques (Fig. 1) [3,4,5].
Fig. 1. Water phantom. (A) A lumbosacral spine model submerged in water and covered with a mesh to simulate human skin. (B) An ultrasound image of lumbosacral spine model submerged in water. The background echogenicity is close to zero.
2. Agar/Gelatin/Guar Gum-based phantom
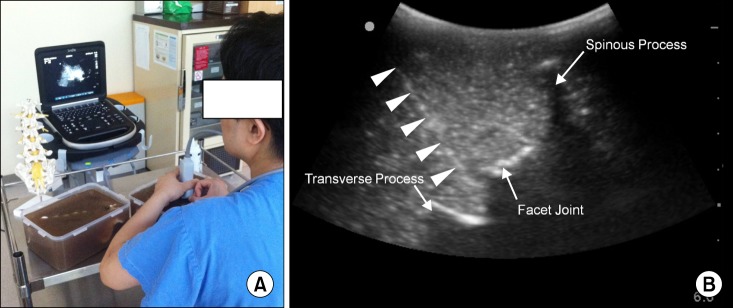
A gelatin-based phantom is produced by placing the target model in a gelatin solution. These designs have been used for ultrasound biopsy and ultrasound-guided vascular access training phantoms [6,7]. Gelatin-based and gelatin/agar-based phantoms of the lumbosacral spine were introduced recently [1,8]. Brascher et al. [9] used a phantom made of guar gum for training in ultrasound-guided intercostal nerve and stellate ganglion blocks. Materials such as flour, cellulose powder, or psyllium husk can be added to the gelatin solution to simulate the appearance of soft tissue in the phantom [3,6,10]. Psyllium husk is a dietary fiber supplement that we usually add to the gelatin solution for spine phantoms to create an opaque, echogenic background. Increasing the psyllium husk content increases the firmness of the phantom and the level of difficulty for novices. Such phantoms are relatively inexpensive and simple to produce. Gelatin phantoms produce sufficient tactile feedback for practicing needle handling (Fig. 2). These phantoms can be stored in a refrigerator for weeks. However, needle-track marks are left in the phantom after practicing injections. The parenchyma of the material can be broken when using a bent or blunt needle. A hyperechogenic needle cannot be used in this phantom, because air pockets instead of fluid remain between the phantom tissue and needle. The gelatin background will deteriorate and decompose over time. A hydrocolloid skin dressing can be used to cover the surface of the phantom to minimize biological breakdown [11] but this can decrease the image resolution.
Fig. 2. A gelatin/psyllium spine phantom. (A) A resident practicing needle handling using a gelatin/psyllium spine phantom. Psyllium husk was added to the gelatin solution to make it opaque. (B) An ultrasound image shows ultrasound-guided medial branch block on gelatin-psyllium lumbosacral spine phantom. Arrowheads indicate needle.
3. Blue phantom
The commercial Blue Phantom (CAE Health Care, Seattle, WA) is made from an elastomeric rubber. Its firm texture gives more tactile feedback than does an agar/gelatin/guar gum model. When a needle is inserted into the elastomeric material, it pushes the material aside and then rebounds to its original location after the needle is withdrawn [3]. Consequently, this phantom has less chance of generating needle-track artifacts. As in a gelatin model, a bent, blunt, or hyperechogenic needle is not used. Although many centers use this phantom, it is expensive compared with homemade phantoms. And its low background echogenicity can lead to false confidence in performance. In addition, it is difficult to incorporate a target model within the structure.
4. Meat phantoms
A meat phantom is moderately cheap compared with the Blue phantom. Since it has anatomic structures, it gives some tactile needle feedback, and the echogenicity of the background mimics human tissue. Practice of needle guidance is possible with less needle-track artifacts, because the tracks fill with tissue fluid after needle removal. Simulation of local anesthetic injection and dissection after injection are available. The pig phantom is popular (Fig. 3). Beef has a thick fat layer, and turkey is too slippery [3].
Fig. 3. A pig carcass used in an ultrasound workshop.

5. Cadavers
Cadaver phantoms are expensive and not readily available without the cooperation of the Anatomy Department. When available, they provide excellent images and tactile feedback that mimic living human tissues. They also permit local anesthetic injection and dissection of the target tissue after injection [3,12]. However, they have no normal vascular anatomy, because the vessels are collapsed. Hocking and McIntyre [12] demonstrated restoration of the normal vascular anatomy following gelatin perfusion.
6. Phantoms made using three-dimensional printing
In three-dimensional (3D) printing, successive layers of material are laid down under computer control. This has the potential to produce objects from multiple materials that either transmit or block ultrasound. West et al. [13] described a method for producing ultrasound phantoms of the spine using 3D printing. Their model had a component representing the ligamentum flavum that transmitted ultrasound. The osseous and ligament components of the model had sonographic appearances similar to those of human patients. The spinal model was secured in a microwave-safe rectangular container, which was filled with gelled agar.
USE OF ULTRASOUND PHANTOMS FOR EDUCATION
Some studies have evaluated the effectiveness of phantoms for improving the proficiency of novices. Mendiratta-Lala et al. [14] reported that the written and practical post-test scores of residents improved significantly after practicing needle penetration into a cyst-like structure secured in a Blue phantom. Moore et al. [2,15] implemented a training system to improve the proficiency of trainees in needle-nerve contact using a gelatin-filled bag containing a simple electric circuit using a copper wire. To train in a specific nerve block, specific models that simulate the real human structures should be embedded in a background material. Michalek et al. [4] simulated an ultrasound-guided infraorbital nerve block using skull models immersed in a water bath and suggested that an ultrasound-guided infraorbital nerve block is feasible using the model. Brascher et al. [9] constructed agarbased phantoms to simulate ultrasound-guided stellate ganglion and intercostal nerve blocks. Kwon et al. [16] showed that training using a gelatin-based spine phantom helped novices to acquire the skills necessary to perform ultrasound-guided lumbar facet joint injections and medial branch blocks.
CONCLUSIONS
Practicing first-time needle placement on a patient is usually not recommended. Many studies have demonstrated the effectiveness of phantoms for improving the proficiency of novices [2,4,9,14,15]. It is helpful to use a phantom to practice ultrasound-guided procedures and educate novices on ultrasound-guided injection. Because a water phantom is not capable of expressing the biological tissue, it is unfit for the beginner's practice of needle placement. Though the meat phantom and cadaver provide excellent images and tactile feedback which resemble living human tissues, they are not always available and relatively expensive. Therefore, a gelatin-like material-based phantom or Blue phantom is appropriate to improve novices' proficiency of ultrasound-guided injections. To practice specific nerve blocks under ultrasound guidance, new ultrasound phantoms need to be developed. In addition, larger studies may be necessary to prove that using new phantoms enhances proficiency of clinical performance.
References
- 1.Bellingham GA, Peng PW. A low-cost ultrasound phantom of the lumbosacral spine. Reg Anesth Pain Med. 2010;35:290–293. doi: 10.1097/AAP.0b013e3181c75a76. [DOI] [PubMed] [Google Scholar]
- 2.Eastwood CB, Moore DL. A simple, inexpensive model for the practice of ultrasound-guided regional anesthesia techniques. Reg Anesth Pain Med. 2010;35:323–324. doi: 10.1097/AAP.0b013e3181d236c8. [DOI] [PubMed] [Google Scholar]
- 3.Hocking G, Hebard S, Mitchell CH. A review of the benefits and pitfalls of phantoms in ultrasound-guided regional anesthesia. Reg Anesth Pain Med. 2011;36:162–170. doi: 10.1097/aap.0b013e31820d4207. [DOI] [PubMed] [Google Scholar]
- 4.Michalek P, Donaldson W, McAleavey F, Johnston P, Kiska R. Ultrasound imaging of the infraorbital foramen and simulation of the ultrasound-guided infraorbital nerve block using a skull model. Surg Radiol Anat. 2013;35:319–322. doi: 10.1007/s00276-012-1039-3. [DOI] [PubMed] [Google Scholar]
- 5.Karmakar MK, Li X, Kwok WH, Ho AM, Ngan Kee WD. Sonoanatomy relevant for ultrasound-guided central neuraxial blocks via the paramedian approach in the lumbar region. Br J Radiol. 2012;85:e262–e269. doi: 10.1259/bjr/93508121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gibson RN, Gibson KI. A home-made phantom for learning ultrasound-guided invasive techniques. Australas Radiol. 1995;39:356–357. doi: 10.1111/j.1440-1673.1995.tb00311.x. [DOI] [PubMed] [Google Scholar]
- 7.Di Domenico S, Santori G, Porcile E, Licausi M, Centanaro M, Valente U. Inexpensive homemade models for ultrasound-guided vein cannulation training. J Clin Anesth. 2007;19:491–496. doi: 10.1016/j.jclinane.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Li JW, Karmakar MK, Li X, Kwok WH, Ngan Kee WD. Gelatin-agar lumbosacral spine phantom: a simple model for learning the basic skills required to perform real-time sonographically guided central neuraxial blocks. J Ultrasound Med. 2011;30:263–272. doi: 10.7863/jum.2011.30.2.263. [DOI] [PubMed] [Google Scholar]
- 9.Brascher AK, Blunk JA, Bauer K, Feldmann R, Jr, Benrath J. Comprehensive curriculum for phantom-based training of ultrasound-guided intercostal nerve and stellate ganglion blocks. Pain Med. 2014;15:1647–1656. doi: 10.1111/pme.12365. [DOI] [PubMed] [Google Scholar]
- 10.Morehouse H, Thaker HP, Persaud C. Addition of Metamucil to gelatin for a realistic breast biopsy phantom. J Ultrasound Med. 2007;26:1123–1126. doi: 10.7863/jum.2007.26.8.1123. [DOI] [PubMed] [Google Scholar]
- 11.Chao SL, Chen KC, Lin LW, Wang TL, Chong CF. Ultrasound phantoms made of gelatin covered with hydrocolloid skin dressing. J Emerg Med. 2013;45:240–243. doi: 10.1016/j.jemermed.2012.11.022. [DOI] [PubMed] [Google Scholar]
- 12.Hocking G, McIntyre O. Achieving change in practice by using unembalmed cadavers to teach ultrasound-guided regional anaesthesia. Ultrasound. 2011;19:31–35. [Google Scholar]
- 13.West SJ, Mari JM, Khan A, Wan JH, Zhu W, Koutsakos IG, et al. Development of an ultrasound phantom for spinal injections with 3-dimensional printing. Reg Anesth Pain Med. 2014;39:429–433. doi: 10.1097/AAP.0000000000000136. [DOI] [PubMed] [Google Scholar]
- 14.Mendiratta-Lala M, Williams T, de Quadros N, Bonnett J, Mendiratta V. The use of a simulation center to improve resident proficiency in performing ultrasound-guided procedures. Acad Radiol. 2010;17:535–540. doi: 10.1016/j.acra.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 15.Moore DL, Ding L, Sadhasivam S. Novel real-time feedback and integrated simulation model for teaching and evaluating ultrasound-guided regional anesthesia skills in pediatric anesthesia trainees. Paediatr Anaesth. 2012;22:847–853. doi: 10.1111/j.1460-9592.2012.03888.x. [DOI] [PubMed] [Google Scholar]
- 16.Kwon SY, Hong SH, Kim ES, Park HJ, You Y, Kim YH. The efficacy of lumbosacral spine phantom to improve resident proficiency in performing ultrasound-guided spinal procedure. Pain Med. 2015;16:2284–2291. doi: 10.1111/pme.12870. [DOI] [PubMed] [Google Scholar]