Summary
Nasal burns present a challenge for the plastic surgeon in terms of immediate management, choice of primary treatment and secondary reconstruction with the goals of good aesthetic and functional outcome. We present a retrospective analysis of the management of 150 patients with nasal burns treated in our center between July 2005 and July 2011. We rationalized our conservative and all surgical treatments of this subset of burns patients and organized them in a simple and structured way. The reconstructive options for most complex full thickness nasal injury is determined by the integrity of adjacent facial tissues which would always be preferred when available. Microsurgical free tissue transfer is dependent upon the fitness of the patient and the availability of unburned skin at the donor site. Secondary nasal reconstruction is based on an assessment of the residual functional and cosmetic problems. Airways narrowing from scar contracture or loss of support are managed using standard plastic surgical and rhinoplasty principles. Cosmetic refinements range from flap debulking to the importation of new tissue on to the nose. Our experience with this challenging group of patients has led us to develop a simple treatment algorithm for the management of nasal burns.
Keywords: nose, burns, reconstruction, flap, algorithm
Abstract
Les brûlures nasales présentent un défi pour le chirurgien plastique en terme de prise en charge immédiate, de traitement primaire ou de reconstruction avec un objectif de bon résultat esthétique et fonctionnel. Nous présentons une analyse rétrospective de 150 patients souffrant de brûlures nasales traités dans notre centre entre Juillet 2005 et Juillet 2011. Nous avons codifié nos traitements chirurgicaux d’une manière simple et structurée. Les options reconstructives dépendent de l’intégrité des tissus faciaux de voisinage qui seront toujours préférés s’ils sont disponibles. Le transfert microchirurgical libre dépend de la condition physique du patient et de la disponibilité d’une zone donneuse. Les reconstructions nasales secondaires dépendent de l’évaluation des séquelles fonctionnelles et esthétiques. Les sténoses en rapport avec le tissu cicatriciel ou la perte de support sous jacent sont soumises aux principes de la chirurgie plastique et de la rhinoplastie .Les améliorations cosmétiques vont du dégraissage des lambeaux au transfert de tissu. Notre expérience avec ce groupe de patients nous a conduit à développer un algorithme de traitement simple pour la prise en charge des brûlures nasales.
Introduction
The nose is the most central feature of the human face providing the key functions of respiration and olfaction, as well as being an important defining point for appearance and beauty. When injured, the restoration of a nose may pose a challenge to the reconstructive surgeon. Historically, nasal reconstruction can be divided into three techniques: the Indian method using the forehead flap, the French method using cheek tissue and the Italian method using tissue from the arm or forearm. They have provided the foundation for the development of modern nasal reconstruction, which now includes a wide range of local, regional and free flap techniques.1 The concept of aesthetic subunits is also a very useful and where possible it should be applied.2,3
Apart from the early pioneering work on victims of the two World Wars, there are not many publications on the modern approach to nasal reconstruction which deal with large groups of patients. Nasal injury caused by burns poses a particular challenge in that the adjacent facial tissues may also be damaged. This makes it more difficult for many of the established loco-regional flap options to be used. Despite this, many reconstructive surgeons persevere with using damaged and scarred tissue simply because the choices are limited. Some of the techniques and problems encountered are reviewed here.
For small full thickness burns defects on the nasal tip or alar region a nasal turndown flap has been described for coverage.4 Unfortunately the use of scar tissue as flaps is often complicated by further retraction and nasal tip shrinkage. Alar defects may also be reconstructed using tissue from the helical rim as a composite graft, but this is usually unavailable in patients with pan facial burns whose ears are commonly injured. Cheek advancement and nasolabial flaps have also been used for coverage of smaller areas. For reconstruction of extensive nasal defects the forehead flap is usually the preferred option.5 The forehead skin may be pre-expanded and, basing it on the superficial temporal vessels, the flap is tunneled under the cheek skin to reach the nose.6 With the forehead scar hidden along the frontal hairline this is a good way to reduce donor site morbidity but it does make the flap more vulnerable to venous congestion. Despite this, the pre-expanded forehead flap has even been successfully used on patients with scarred or skin grafted forehead in a small case series.7 The Washio technique requires a two-stage reconstruction with significant discomfort for the patient due to the particular design of this flap. In a small series of modified Washio flaps, the authors reported that the risk of venous congestion was high and the dissection was difficult. 8 When confronted with poor quality facial scar tissue, some surgeons occasionally still resort to the use of the tubed pedicle flaps from the neck or forearm.9
Burn injuries add a further complexity to reconstruction of the nose by also injuring the potentially useful adjoining tissues, which may themselves also require reconstruction. In this situation a free flap, such as the radial forearm flap, is frequently used.10 A more unusual option using a dorsalis pedis free flap has also been reported.11 For a total nasal reconstruction, the concept of harvesting two flaps - radial forearm for lining and forehead flap for cover - can give excellent results,12,13 but in the burn patient it is a luxury that is quite often not available. When performing reconstructive rhinoplasty for burn injury, Bernard notes that bright highlights and dark shadows can make defects more pronounced.14 Sometimes a significant improvement in aesthetic outcome can be achieved by applying the simple hump removal or tip elevation technique of traditional rhinoplasty to the burned nose.15
With most publications limited to case reports or small clinical series, it appears that there are no clear guidelines for the management of nasal burns. We therefore reviewed our experience of the management of a large series of burn patients who also suffered concomitant nasal injury and summarized our approach in a simple algorithm.
Materials and methods
We analysed a group of 150 patients (36 children and 114 adults) with burns affecting the nasal area, treated in our unit between July 2005 and July 2011. Data was studied retrospectively using our database, medical records and photo documentation. The study was legitimately approved as a subset analysis of the institutional audit of facial burns, forming a part of service evaluation. The first author reviewed the clinical notes and the following data were gathered: patient’s age, gender, mechanism of injury, percentage of total body surface area burned (TBSA), depth of nasal burns and their management. Surgical procedures were recorded, including the use of autograft, allograft, dermal substitute, loco-regional flap or free flap. Patients who did not complete their treatment and who died during their hospital stay were excluded from the study.
On admission, each patient was stabilized and the mechanism of burns, concomitant injuries, total burn surface, presence or absence of inhalation injury and the patient’s personal data were evaluated and documented. All patients were photographed. The nasal burn depth and extent were estimated clinically and, in cases where it was difficult to distinguish between superficial or deep dermal burn, laser doppler scanning was used. Each patient was then managed in accordance with our Burn Centre protocol. Patients treated in ICU for burns of >40% TBSA usually receive 20 mg/day of Oxandrolone in order to reduce burns catabolism. Patients with inhalation injury usually require prolonged ventilation and present higher rates of delayed nasal healing.
After healing of the burn wounds, all patients are routinely reviewed in our burns clinic by a multidisciplinary team to assess their progress and determine whether any secondary reconstruction is needed.
Results
The study included 150 consecutive patients (36 children and 114 adults) identified as having nasal burns over a 6-year period from July 2005 to July 2011. There were TBSA was 21% ± 25%. The majority – 80/150 (53%) – were non-resuscitation burns involving the head and neck area, consequent to flash/flame burns. Flame injury was the most common cause of nasal burns, affecting 78% of the group. Scald was the second most frequent cause, affecting 16% of these patients, although the child population suffered from scalds in 38% of cases. Chemical and electrical burns are less common causes of nasal burn injury affecting only 4% and 2% of our patients respectively. Less than 1% of patients had full thickness contact burns. The relative frequencies of the different mechanisms of injury are shown in Fig. 1 A. As is shown, flame injuries are the principal mechanism of injury in facial burns in adults and children, but scalds still have a significant place among the child population, being relatively rare in adults where facial burns are concerned.
Fig. 1.
A: percentage of mechanism of burn injury in a group of 150 patients with nasal burns. B: correlation of percentage of burned total body surface area (TBSA) in a group of 150 patients with nasal burns.
Analysis of TBSA has shown that 54% of patients with nasal burns had less than 10% burns in total, 15% sustained 10-20% burns, 9% had 20-30% burns, 3% had 30-40% burns and quite a significant group of 17% of patients was treated for extensive burns of more than 40% (Fig. 1 B).
The mean ± SD of TBSA was 16% ± 21% in the nonsurgically treated group vs. 38 ± 28% in the surgically treated group. Mean age of surgically treated patients (n=20) was 34 ± 19 years and was not much different to mean age of 31 ± 19 years in the non-surgically treated group (n=130).
Our algorithm (Fig. 2) summarizes the steps of treatment taken in this group of 150 patients. We divided the patients into two principal groups: those suffering acute burn injury and those undergoing secondary reconstruction. We separated the patients admitted with extensive burns, requiring primary resuscitation, debridement and coverage of other areas which are more important for patient survival, from the second group of patients with isolated nasal burns or minor burn injury. After life-saving procedures are completed, both groups can be joined in the treatment of nasal burns. At this point burn thickness is a key issue in deciding the type of treatment. If the patient is not suitable for autograft and lacks local tissue, the reconstructive options are similar in primary and a secondary reconstruction.
Fig. 2. Algorithm for the treatment of nasal burns.
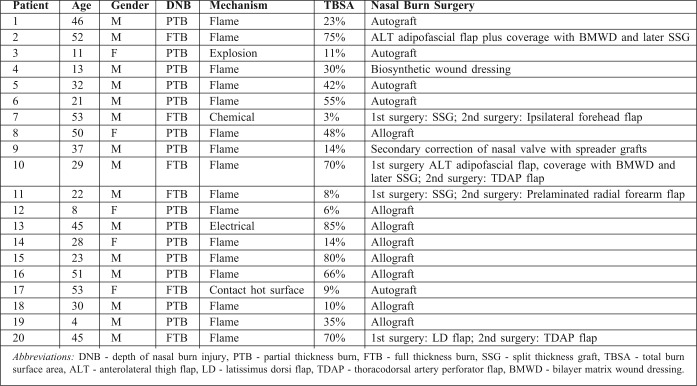
In the surgically treated group there were 15 male vs. 5 female patients. Only four children required surgical treatment of nasal burns, which in three out of four cases was limited to debridement and coverage with Biobrane(R) or allograft. In the group of surgically treated adult patients, in 11 cases nasal burns were debrided and covered with allo or autograft. We performed six free flaps on four adult patients and only one patient was treated with a forehead flap. Five patients required secondary reconstruction. In four cases it was necessary to restore lack of volume of nasal tip after primary skin grafting or resurfacing with a fascia lata plus Integra® in patients with lack of donor sites due extensive burns. In one case we performed secondary reconstruction of a burned and collapsed external nasal valve with spreader grafts in a patient who initially was treated conservatively (Table I).
Table I. Patient details for surgically treated group.
The range of free flaps included two anterolateral thigh adipofascial flaps, one latissimus dorsi flap, two thoracodorsal artery perforator flaps and one prelaminated radial forearm flap. The cases reconstructed with free thoracodorsal artery perforator flaps subsequently required flap thinning. The superior thyroid or facial arteries and veins were usually used as recipient vessels. We had a 100% flap survival.
Discussion
Nasal burns seldom occur in isolation. More commonly they occur as part of a more extensive, even life threatening burn injury involving a significant part of the face as well as the airways. The decision about timing and mode of nasal treatment should only be taken after careful clinical assessment of the patient’s needs based on the total burn size and the depth of injury. In the management of acute extensive burns with limited availability of donor skin, patient survival is the primary goal. Priority is thus given to reducing the wound size starting with coverage of the back and buttocks, followed by the thorax, abdomen and extremities. In the head and neck region, priority is given to the prevention of corneal exposure as well as grafting of any neck burn in order to facilitate the future need for a tracheostomy.
The nose is an end organ whose pattern of blood supply makes it vulnerable to the effects of injury, ischaemia and secondary infection. On the other hand, nasal skin is richly endowed with adnexal structures and sebaceous units, which greatly increases its capacity for re-epithelialization after burn injury. We therefore start with simple measures to optimize the milieu of the burn wound in order to facilitate healing. All patients are nursed with the head elevated in order to reduce oedema, and the wound is checked regularly to ensure that the nose does not become desiccated. Antiseptic dressings are used together with regular microbiological surveillance of the wound to reduce infective complications. The efficacy of this approach is confirmed in our series by the small number of nasal burns requiring surgical debridement and skin cover.
As suggested by Boswick, early nasal debridement is usually not performed, because this may simply denude cartilage and increase subsequent deformity.16 Instead, dermal substitutes such as Biobrane®, allograft, or temporary biological dressings are used to protect burned facial tissue from infection and desiccation as well as to prepare a better base for further reconstruction without the initial use of autografts. In our hands, allograft has been shown to be a good option for intermediate thickness nasal burns. We find that applying it unmeshed provides a good protection of the wound bed and optimizes healing by epithelialization, resulting in a better scar quality and colour match. This reduces the need to perform autograft in acute facial burns. With deep dermal or full thickness nasal burns the surrounding facial skin is usually affected and we perform coverage with a skin graft or a flap as a single procedure. In most of these cases secondary correction is required.
If a nasal burn has extended to the deep dermis but is still graftable, we treat it with a split thickness skin graft (10-12/1000 inch), which provides stable coverage with a good aesthetic outcome in most cases. When treating a deep dermal burn with autograft it is sometimes difficult to find a suitable donor site with optimal colour matching capacity in a patient who may have a shortage of available skin. Blush skin from the scalp or a graft taken from supraclavicular areas can provide a good match for nasal skin. Reconstruction with full thickness skin grafts works well for secondary resurfacing of post-burn nasal scars. The nose is defined by its specific shape and structure rather than by the external skin alone and we usually graft the nose as a single unit. Multiple quilting sutures are a useful technique to ensure a better graft take on the multi- contoured nasal surface.
If more complex reconstruction of residual nasal deformity is required because of poor scar quality or an unacceptable appearance, the availability of local tissue is evaluated. Asuku and McCauley classify post-burn nasal deformity into two groups: those with an isolated soft tissue deformity and those with a composite deformity.17 The forehead flap is usually our first option for reconstruction of non-graftable nasal defects (Figs. 3, 4). Unfortunately, in our group of patients with deep facial burns, local tissue was not available in most cases and reconstruction with free tissue transfer was therefore needed. Our choice of flap depended on availability of unburned donor sites. If the patient had intact skin over areas where fascio-cutaneous flaps can be raised, then the radial forearm flap (RF), anterolateral thigh flap (ALT), or thoracodorsal artery perforator flap (TDAP) were our preferred options for nasal reconstruction.
Fig. 3. Patient 7 (Table I).

A,D: 53-year-old male with chemical full thickness facial burns. B,E- preoperative view. C,F: postoperative view. 1.5 years after nasal reconstruction with forehead flap and cheek reconstruction with submental flap.
Fig. 4. Patient 7 (Table I).

intraoperative view. Left - design of a forehead flap for nasal reconstruction. Middle - insertion of the flap. Right - submental flap for cheek reconstruction.
When performing a free flap reconstruction of a burned nose the surgeon must be prepared to deal with poor quality recipient vessels as well as a more complex dissection due to the surrounding fibrotic tissue. In our experience, suitable recipient vessels can usually be found but in order to allow for greater flexibility one should aim to harvest a longer pedicle length with the flap. Volume and colour mismatch are recognised disadvantages.
If the patient has suffered extensive burns, with exposure of bone, we aim to close the wound first and then perform a secondary reconstruction of the nose if needed. If intact skin donor sites are limited we use adipofascial or muscle flaps covered with a bilayer dermal matrix. Secondary adjustments can be made once the patient has recovered from severe burn trauma.
A second free flap was required in two patients in our study. Both patients had very extensive burns resulting in a shortage of donor tissue. In each of these two patients the first free flap was used to cover extensive defects with exposed frontal bone, frontal sinus, orbital and nasal bones at the early stage, while the second free flap was used to achieve better nasal definition. In our experience, it was difficult to achieve good nasal tip projection in one stage reconstruction and a second fascio-cutaneous flap is usually needed to restore the missing volume and improve cosmesis at a later stage. Unsatisfactory shape of the nasal tip and alar slump can be improved by cartilage grafting harvested from the conchal fossa or costo-chondral regions of the chest.
In cases of reconstruction with pre-laminated radial forearm flap and forehead flap, primary grafting of nasal burn was possible and the restoration of nasal volume and contour with a flap was made at a later stage. Pre-lamination of the radial forearm flap provides good nasal tip projection and good nostril aperture (Figs. 5, 6). The possibility of doing free tissue transfer as a delayed procedure decreases the risk of intra- and postoperative complications.
Fig. 5. Patient 11 (Table I).

A: a 22-year-old male with full thickness burns to face and both hands. B: SSG as a first stage of nasal reconstruction. C,D: prelaminated free radial forearm flap as a second stage to improve nasal volume and contour defect. E: preoperative photo. F: postoperative photo four months after nasal reconstruction with prelaminated radial forearm flap.
Fig. 6. Patient 9 (Table I).

37-year-old male with full thickness nasal burns. A: external nasal valve retracted by post burn scar. B: correction with skin grafts to the nostril and a rhinoplasty with spreader grafts.
If secondary nasal reconstruction is needed, we evaluate if the problem is functional or purely cosmetic. Functional deficiencies of airway narrowing or nasal valving may require the placement of spreader or batten grafts. The nasal aperture may be improved by alar scar release, full thickness skin grafting to the nasal floor and postoperative splintage. Gingivo-mucosal flaps and flaps based on infraorbital vessels were not used in our study but are also possible options to correct nostril stenosis.18,19 If alar retraction is caused by insufficient soft tissue on the lower half of the nose, we evaluate if the defect is small enough to be treated by scar release and resurfacing with a full thickness skin graft or if a composite graft can be used. Patients who had suffered complex naso-facial burns would usually have had a number of life saving procedures. The result of their initial nasal reconstruction often leaves them with an acceptable but less than perfect nose. In our experience, these patients are very unwilling to continue with further multi-staged refinements and generally prefer to just get on with their lives.
As Gaspar Tagliacozzi wrote in De Curtorum Chirurgia per Insitionem (1597):
“We reconstruct and complete parts which nature had given, and we do so, not so much for the enjoyment of an eye, as for psychic comfort for the afflicted .”20
Conclusion
We believe that a systematic evaluation of nasal burn injuries, presented in this algorithm, guides us in the method and timing of treatment. By applying the many tools and surgical techniques available within the plastic surgery repertoire the final appearance and function of the burnt nose may be improved.
Acknowledgments
Conflict of interest. None.
Funding. None.
Acknowledgements. We thank our therapists for all their hard work in treating patients included in this study.
References
- 1.Whitaker IS, Karoo RO, Spyrou G, Fenton OM. The birth of plastic surgery: The story of nasal reconstruction from the Edwin Smith Papyrus to the twenty-first century. Plast Reconstr Surg. 2007;120:327–36. doi: 10.1097/01.prs.0000264445.76315.6d. [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez-Ulloa M, Stevens E. Reconstruction of the nose and forehead by means of regional aesthetic units. Br J Plast Surg. 1961;13:305–9. doi: 10.1016/s0007-1226(60)80060-4. [DOI] [PubMed] [Google Scholar]
- 3.Burget G, Menick F. The subunit principle in nasal reconstruction. Plast Reconstr Surg. 1985;76:239–47. doi: 10.1097/00006534-198508000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Taylor HOB, Carty M, Driscoll D, Lewis M, Donelan MB. Nasal reconstruction after severe facial burns using a local turndown flap. Ann Plast Surg. 2009;62:175–9. doi: 10.1097/SAP.0b013e31817d87ed. [DOI] [PubMed] [Google Scholar]
- 5.Menick F. Nasal reconstruction: Forehead flap. Plast Reconstr Surg. 2004;113:100–11. doi: 10.1097/00006534-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Fan J. A new technique of scarless expanded forehead flap for reconstructive surgery. Plast Reconstr Surg. 2000;106:777–85. doi: 10.1097/00006534-200009040-00004. [DOI] [PubMed] [Google Scholar]
- 7.Jun C, Yunliang Q, Danru W, Yixin Z, Jun Y, Wenxiang G. Expanded scarred or skin grafted forehead flap for nasal reconstruction in severe postburn facial deformity. Ann Plast Surg. 2008;61:447–51. doi: 10.1097/SAP.0b013e31815f12be. [DOI] [PubMed] [Google Scholar]
- 8.Hassanpour SE, Shariati SM. One stage reconstruction of nasal defect by reverse flow retro-auricular island flap-case series and discussion. J Plast Reconstr Aesthet Surg. 2008;61:49–52. doi: 10.1016/j.bjps.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 9.Hassanpour SE, Davami B. Reconstruction of nose and lips with tubed cervical flap in electrical injury: A case report. Burns. 2005;31:510–3. doi: 10.1016/j.burns.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 10.Sinha M, Scott JR, Watson SB. Prelaminated free radial forearm flap for a total nasal reconstruction. J Plast Reconstr Aesthet Surg. 2008;61:953–7. doi: 10.1016/j.bjps.2007.10.068. [DOI] [PubMed] [Google Scholar]
- 11.Benmeir P, Neuman A, Weinberg M, et al. Reconstruction of a completely burned nose by a free dorsalis pedis flap. Br J Plast Surg. 1991;44:570–1. doi: 10.1016/0007-1226(91)90090-7. [DOI] [PubMed] [Google Scholar]
- 12.Menick FJ, Salibian A. Microvascular repair of heminasal, subtotal, and total nasal defects with a folded radial forearm flap and a full-thickness forehead flap. Plast Reconstr Surg. 2011;127:637–51. doi: 10.1097/PRS.0b013e3181fed686. [DOI] [PubMed] [Google Scholar]
- 13.Burget GC, Walton RL. Optimal use of microvascular free flaps, cartilage grafts, and a paramedian forehead flap for aesthetic reconstruction of the nose and adjacent facial units. Plast Reconstr Surg. 2007;120:1171–206. doi: 10.1097/01.prs.0000254362.53706.91. [DOI] [PubMed] [Google Scholar]
- 14.Bernard SL. Reconstruction of the burned nose and ear. Clin Plast Surg. 2000;27:97–112. [PubMed] [Google Scholar]
- 15.Hafezi F, Karimi H, Nouhi A. Aesthetic septorhinoplasty in the burned nose. Burns. 2005;31:223–9. doi: 10.1016/j.burns.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 16.Boswick JA. Burns of the head and neck. Surg Clin North Am. 1973;53:97–104. doi: 10.1016/s0039-6109(16)39935-2. [DOI] [PubMed] [Google Scholar]
- 17.McCauley RL, editor. Functional and aesthetic reconstruction of burned patient. Boca Raton Florida: Taylor and Francis; 2005. Reconstruction of the burned nose; pp. 287–300. [Google Scholar]
- 18.Copcu E. Reconstruction of total and near-total nostril stenosis in the burned nose with gingiva - mucosal flap. Burns. 2005;31:802–3. doi: 10.1016/j.burns.2005.04.025. [DOI] [PubMed] [Google Scholar]
- 19.Hataya Y, Kosaka K, Yamazaki M, et al. Reconstruction of burned nasal alae with vascular island skin flaps pedicled on the infraorbital vessels. Burns. 1995;21:313–15. doi: 10.1016/0305-4179(95)93870-p. [DOI] [PubMed] [Google Scholar]
- 20.Ben-Hur N, Converse JM. The impact of plastic surgery on transplantation from skin graft to microsurgery. Transplant Proc. 1980;12:616–20. [PubMed] [Google Scholar]