Abstract
Background
Mozambique has one of the world’s highest burdens of human immunodeficiency virus (HIV) infection. Despite the increase in testing services throughout the country, uptake of HIV testing has been low.
Methods
To identify barriers to HIV testing we conducted a study in 6 rural districts in Zambézia Province. We recruited 124 men and women from the community through purposeful sampling to participate in gender-specific focus groups about barriers to HIV testing.
Results
Participants noted three main barriers to HIV testing: (1) poor treatment by clinicians, including intentional disclosure of patient HIV status to other community members; (2) unintentional disclosure of patient’s HIV status through clinical practices; and (3) a widespread fatalistic belief that HIV will result in death among those infected, particularly given poor access to food.
Conclusions
Improving quality and confidentiality within clinical service delivery, coupled with the introduction of food supplement programs should increase people’s willingness to test and remain in care for HIV disease.
Keywords: HIV/AIDS, Mozambique, stigma, testing acceptability, doctor-patient trust, confidentiality, focus groups
Background
Mozambique is a southeast African nation of approximately 21 million people, with one of the world’s highest burdens of human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS). In 2009, a national population based-survey estimated an 11.5% prevalence of HIV infection among Mozambican adults ages 15–49 years [1]. In the same year, low rates of HIV testing were documented. Only 14.5% of women and 8.9% of men received an HIV test and test result in the previous year, and lifetime 33.6% of women and 17.2% of men had ever received an HIV test and test result. High rates of HIV infection in southern Africa have led to calls for universal voluntary testing of all adults [2–4] to reduce the HIV epidemic. HIV infection-related mortality among adults was reported to be 27%, only slightly less than malaria [5]. Government of Mozambique efforts to tackle high rates of HIV infection in the country have increased with the assistance of the President’s Emergency Plan for AIDS Relief (PEPFAR) and the Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund) [6]. Data show that although antiretroviral therapy (ART) is now broadly available, HIV testing rates remain low [1].
Voluntary Counselling and Testing (VCT) and Provider Initiated Counselling and Testing (PICT) are essential to starting the cascade of medical and behavioural interventions designed to improve a patient’s health. Persons who test positive for HIV are counselled to reduce their sexual risk behaviours (“prevention for positives”), often resulting in increased condom use [7]. Those successfully initiated on ART have lower viral loads [8, 9], resulting in lower rates of transmission to their sexual partners [10, 11], and are less likely to pass the virus to their infants [12, 13]. Nonetheless, slow uptake of HIV testing has been documented throughout sub-Saharan Africa [14–16]. Stigma surrounding HIV infection [16–18], the lack of confidentiality at clinical sites [16, 19–21] inconvenience [19, 22, 23], cost of treatment [17, 19, 23, 24], opt-in testing vs. opt-out testing [25], fear of partner reaction [26–28], and low assessment of personal risk [22, 27] have been noted as barriers to testing.
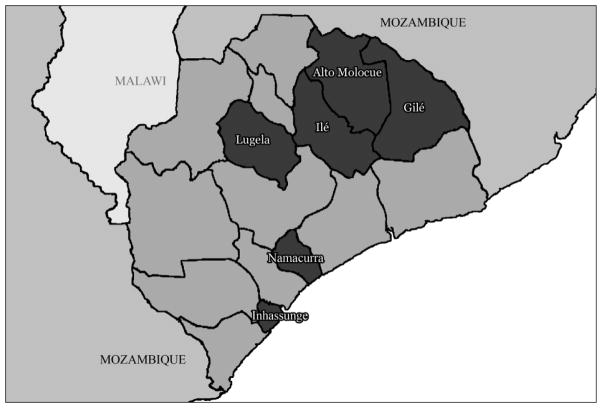
The HIV infection prevalence in Zambézia Province, located in north central Mozambique, was estimated to be 12.6% among adults in 2009 [1]. Friends in Global Health (FGH), affiliated with the Vanderbilt Institute for Global Health, partners with the Mozambican Ministry of Health (MISAU) and the Provincial Health Directorate of Zambézia (DPS) to provide HIV care and treatment to people in rural Zambézia Province through a PEPFAR-supported grant from the Centers for Disease Control and Prevention (CDC) [29]. When this study was conducted in early 2009, testing and treatment was offered at the main hospital in each of the 6 districts (Figure 1). In 2009, only 5733 people were tested for HIV and received their results (from a catchment area of ~1 million), resulting in 1056 patients enrolled in care for HIV services (Friends in Global Health, unpublished data). Patients who enrolled in care and treatment were referred for testing primarily through PICT (32%), VCT (32%) and PMTCT (9%).
Figure 1.
Map of Zambézia Province, Highlighting Study Districts
Intermittent supply shortages of testing kits, anti-retroviral medication, as well as delays in obtaining lab results were common during the initial roll out of services, which began in 2007, negatively impacted the quality of clinical services [29]. Similar problems continue to plague clinical services, and there has been an increase in the number of patients on ART from none in 2007 to 5671 in 2012. Compounding clinical challenges, these districts were characterized by low population densities resulting in long travel times to hospitals for much of the population and high rates of poverty. Despite these challenges, HIV testing was encouraged through radio and billboard advertisements, health care provider initiated testing, and peer educators in clinical and community settings. Our research was designed to identify barriers for testing for HIV infection and thus provide evidence for designing appropriate strategies to increase the number of men and women being tested for HIV infection.
Methods
We conducted the study in 2009 in 6 rural districts (Gilé, Ile, Namacurra, Inhassunge, Alto Molócuè, and Lugela) in Zambézia Province, Mozambique (Figure 1). In each district, two focus groups were conducted; one with male and one with female participants. District administrators and health authorities were approached for local approval. As per the request of these administrators, we asked community leaders to recruit participants; we asked that they obtain a reasonably diverse sample of the community by selecting participants from different families, neighborhoods, ages, and occupations. The community leader created a list of 30 people complete with basic demographic information for our team to review. Our trained focus group leaders chose the final participants (mean n=10 per group, with an equal number of men and women) based on achieving a range of ages and professions. Only a single person from a given family was allowed to participate in an effort to obtain diversity. Receipt of prior VCT was neither a recruitment question nor a consideration. Potential participants from the community were invited for the study and to share their experiences and perceptions related to acceptability of HIV testing and treatment access. All of those who were approached to participate agreed; in fact we had to turn away people who showed up when we had filled the group. All provided written informed consent and demographic information during one-on-one sessions with moderators before the focus groups began. Participants were not paid for their participation but were given a soda and small sandwich to eat during discussions. Verbal assistance with the consent form was provided to persons with low literacy skills. The study was evaluated and approved by Mozambican National Bioethics Committee and the Vanderbilt Institutional Review Board in 2008.
The focus groups were conducted by trained moderators, all of whom had previous experience conducting focus groups in Mozambique. Moderators all spoke both Portuguese and the local language relevant to the districts (Echuabo or Elómwè). All community focus groups were conducted in the local language. While the focus groups were organized by researchers affiliated with the organization FGH, neither the moderators nor researchers conducting data analysis were associated with clinical service delivery, an effort to limit biased responses by community members. Before the focus group began, researchers collected demographic information on each participant. Focus groups were conducted in a community setting to ensure a separation from the clinical site. Each lasted between 1.5 and 2 hours. Several questions were posed to the group, including: 1) For you, what does it mean to be sick? 2) What are the different ways HIV can be transmitted? 3) What is life like for people living with HIV or AIDS? To assess barriers to HIV testing, participants were asked “Why might people chose not to seek HIV testing or treatment?” Focus groups were instructed to discuss testing barriers first, and when this topic was exhausted they discussed barriers to treatment. Only data relating to HIV testing barriers were analysed for this paper. Issues relating to treatment adherence have been published elsewhere[21].
Leaders were asked to probe for differing opinions and agreement after major themes were raised, but were not seeking consensus. Sessions were audio taped and subsequently translated/transcribed into Portuguese, and English. Translations were reviewed by two or more members of the team to ensure accuracy and investigators and moderators discussed and resolved all discrepancies to ensure the data were accurate. Translations and transcriptions were often not verbatim, given complex idioms and local communication styles, but were reviewed by multiple members of the team to ensure that the essence of each response was preserved. Two authors (KG and CA) coded the data by hand separately and compared results. Data were analysed using content analysis techniques[30], although researchers independently created thematic categories as they coded the data. These categories were subsequently compared by the two authors to discuss the importance of identified themes and to compare coding of the transcripts. Any initial disagreement in coding was due to word choice, and after a single meeting there was complete agreement in the coding.
Results
Description of the sample and testing concerns
A total of 60 women and 64 men participated in our 12 focus groups. Community members had a mean age of 35 years, had low levels of education (mean of 4 years), and primarily worked as subsistence farmers (73%). All the men and women lived in the six target communities where clinical sites offered HIV testing and treatment free of charge. Participants spoke both about their own experiences with the health care system and that of their friends and family.
Negative Perceptions and Experiences with the Health Care System
Health care workers were accused of treating patients without respect during consultations by mocking their inability to understand Portuguese and intentionally disclosing patient HIV status to other community members. Negative experiences with health providers, coupled with rumours about clinicians intentionally disclosing patient’s HIV status served as a warning and deterrent to would-be testers.
Participants told of an inability to communicate with clinicians given language barriers, leading many to avoid seeking any type of care, including testing, at a hospital or clinic. Upon completion of training, most clinicians are placed by MISAU in provinces other than their own to complete two years of obligated service and have no knowledge of local languages. The language barrier is compounded with a class difference; most patients have low levels of education, speak local languages, and are poor. In addition to language barriers making it difficult to receive proper health services, some clinicians were reported to mock patients who did not understand Portuguese.
If you ask them to repeat what they said because you didn’t understand, they are insulted. They say, ‘sir you should study at a school.’ And they say this in the presence of many women. The women sit there and laugh
One man summed up the discussion with, “Many people don’t go to the hospital because the nurses treat the patients badly.” This poor treatment extended beyond direct patient-clinician interactions to breaches in patient confidentiality.
Participants offered harsh comments about intentional disclosure and clinicians lying about a patients’ HIV status in their communities. This issue emerged as a strong theme among men’s groups, generating less discussion among women. The concern that just by testing for HIV opened a patient up to the possibility a clinician would spread rumors about their status was a disconcerting belief. A man from the north explained,
It is because there isn’t secrecy at the hospital. You could leave HIV negative or HIV positive and the nurse is going to tell his friend that the person there has AIDS. The friend is going to tell their friend ‘that man has AIDS,’ and like this the information circulates around the entire place.”
Someone in almost all of the men’s groups expressed concerns about intentional disclosure. Regardless of the truth, rumours have the potential to dissuade people from seeking testing. The fear of betrayal by health care workers extended to intentional disclosure of a true positive status, given the small size of these communities and relationships health care workers have with patients outside of the clinic. This exchange explains the value confidentiality plays in the willingness to be tested for HIV:
[Participant 2] Also it’s because the medical technicians don’t keep it secret and confidentiality doesn’t exist. They say, ‘you see that beautiful woman over there? She has AIDS only because he had a relationship with her and she rejected him.
[Participant 8] For us, distance isn’t a problem. The hospital is close.
[Participant 10] The problem is lack of confidentiality and secrecy. Everyone agrees.
Hence, some focus group participants accused health workers of deliberately disclosing or lying about patients’ health status in these small town and rural settings.
Unintentional Disclosure
Clinical practices can also expose an HIV-infected person to unintentional disclosure. A farmer noted,
When the results show that the person has HIV, their pill bottle is wrapped up with paper, and people who are well don’t have their pill bottles wrapped up. This is when the strangeness starts for everyone. This man’s pill bottle is covered up because he has a bug.
Another man added,
This complicates it more. Meanwhile in Nampula [a Provincial capital to the north of Zambézia], it’s easy to discover who has AIDS. Everyone there is taken through 4 different buildings. It’s easy to see that that guy has AIDS, if his papers are in plastic.
Focus group members recognized that this disclosure was not intentional, but indicated that people were unwilling to risk identification as HIV-positive in their home communities when clinical flow (patients being directed from one office to another) functionally revealed the patients’ status. Confidentiality breaches have led to patients traveling to distant clinical sites to receive testing and treatment anonymously. A woman said,
There are people who prefer to spend their money. They make an appointment in another city and get tested there so they won’t be seen because of shame. One time I went to the Quelimane hospital [located about 1 hour away by car] and saw people from here enter the doors where they treat this illness.
While this option to seek HIV care far from home exists for those few with the financial means, others must choose between disclosure and not seeking testing (or follow-up care) at their local clinical sites.
Ironically, focus group participants noted that effective treatment in itself could challenge a patient’s ability to keep their illness a secret. A man explained,
It’s because there are many bad stories about sick people. When you go to the hospital, people think that you have AIDS. You get fat while you used to be thin, and they are going to say, ‘that person there, AIDS has made them fat.’
While some were wary of ART, many others were familiar with ART and the positive effects it had on persons living with HIV. A man in the south said, “I think that ART works. There are many people who were very bad, and when they started ART, they became fat like an elephant. It works.” An exchange between men in the south shows how people’s perspective about the virus has changed in recent years.
[Participant 2] In the past, people thought that when they had AIDS, it was the end of their life. In this moment they think differently and have a perspective of the future.
[Participant 1] People infected with HIV, in our community we are sad for them. Nobody wants to be sick and it’s difficult to be, so we try to help.
[Participant 6] The fact is that it is a complicated situation. We don’t laugh at people in this situation because sometimes we don’t know if we have the same condition.
[Participant 8] We are all worried.
In this exchange it was clear that the widespread prevalence of HIV has somewhat normalized infection. However, people also attributed education and the availability of ART in changing their beliefs about the disease, suggesting that as treatment accessibility and education about HIV improves in this province, stigma surrounding the illness may lesson.
There is no point to getting tested. I will die anyway
Negative perceptions about clinical services were exasperated by a fatalistic view that HIV equals death. A woman in the north said “Here where we are there are many people with AIDS, but nobody wants to take a test to know. How can we manage, when nobody is interested in going to the hospital to see if they have AIDS or not?” Fear of HIV infection was often so strong that many of those who had been offered VCT had declined. A woman summed up her experience:
I had a rash on my skin, went to the hospital, and they said I had to take a paper over there to be tested. I said that I would return to be tested after my rash gets better. When I returned I asked a nurse if I needed to be tested. He said yes. I responded that I would get tested the next time I’m sick. I have fear.
While fear of testing was often associated with symptom expression, even those not experiencing symptoms expressed reservations with testing. A woman described a community based mobile clinic testing service that goes community to community to educate people about HIV and provide testing services. She said, “Last year the nurses came to this neighbourhood to do HIV testing, but many people here didn’t want to do it. They said they don’t want to know if they have AIDS.” The desire to avoid knowing one’s HIV status was interesting to focus group leaders who probed groups with the question of “Why do people not want to know their status?” Participants indicated that having a disease with no cure was pointless, particularly when taking medication necessitated eating well to avoid further side effects [31] A man from the north said “How are you going to do treatment? You take ART for two or three years and if you don’t have good food, you die just the same.” Given high rates of poverty, access to nutritious foods is not common. An exchange about barriers to testing in the north went like this:
[participant 5] I think that those who go over there to get tested and turn out to be positive don’t recuperate. There are many that I have not seen get better, the same as those who go to Nampula [a large city 2 hours north].
[participant 8] Treatment for AIDS requires lots of conditions, like we have to eat well. Instead of getting better, we get worse, unlike the people in the big cities who improve. Here a person takes ART and eats dried fish, xima (boiled mandioca flower), and curry without coconut. People don’t have any interest in living like this.
There was concern that the medication did not cure the patient, even if taken as directed. A man said, “The problem is that ART is for all of their life and people stop thinking about the future because they are upset. If you had an endpoint, it would be good to give hope for life”. Another followed up with, “Thoughts exist but people are sad because even if they do treatment, they know they won’t be cured. You know that you can die whenever.” The expectation that only access to a cure for HIV or assistance out of poverty would promote testing is a public health challenge we have yet to successfully address.
Discussion
Testing is an essential first step in the clinical management of HIV, thus starting a cascade of patient support that results in antiretroviral treatment that reduces viral load. However, data from Mozambique show relatively low rates of testing and the evidence is lacking to why this is the case [1]. This study suggested considerable agreement about the major barriers to uptake of HIV testing services among focus group participants, both men and women, in six diverse districts in Zambézia Province. Negative perceptions and experiences with the health care system, fear of stigma surrounding HIV, as well as the belief that one’s HIV status was not worth knowing were strong themes discussed in all districts. Underlying these themes was anger directed at those tasked with providing health care services. People were frustrated with the perceived expectation that they should seek HIV testing despite poor clinical services that could expose them to social stigma related to HIV diagnosis. They were also frustrated that clinics would distribute medication that required a particularly nutritious diet but not supply the necessary food supplies. The impact of these barriers to scale up of treatment and adherence has been assessed, but less attention has been given to the impact on willingness to test [32, 33]. Given these barriers, many have initially sought care from a traditional healer instead of clinical services, potentially resulting in dangerous delays in testing and treatment [34].
Responses of participants indicate that people are unwilling to be tested for HIV if clinical workers do not treat them appropriately. With the common practice of moving clinicians from urban regions to rural areas, there are issues of clinician competency in local languages (there are over 40 spoken in Mozambique), economic and social class inequality (rural residents tend to be poorer and of lower social status), and a lack of education that inhibits patient empowerment in Zambézia Province [6]. Challenges with patient-physician communication (even when they are actually speaking the same language) are well documented [35–37] and improving communication has been a focus in developed countries [38, 39] although this has been less well-researched in the developing world. In studies looking at the importance of patient-clinician relationships, respectful treatment and treating patients as individuals were found to be extremely important [40, 41]. Patient perception of “good” quality of care may be less related to clinician knowledge and more associated with providing caring treatment[42]. In rural Mozambique, patients spoke of poor experiences with nurses, physicians and pharmacists, limiting their trust and uptake of services. Perceptions about health care quality and fears of disclosure have been documented as barriers in other testing acceptability studies [16, 43, 44]; however, community members felt that not enough was being done to address this issue in Mozambique. Scaling up testing availability is paramount, but not sufficient if people are unwilling to seek testing given their perception of health care services. Compounding the challenge of improving treatment quality is the unachievable expectation many participants had that a cure for their disease was essential to quality care. Improving patient satisfaction with care will require the health system to address both clinical attitudes as well as patient expectations [45].
If a person’s status was exposed, community members believed they would be discriminated against by their neighbours, friends and family. Given the large number of breaches in patient confidentiality, community members were disinclined to accept HIV testing. Stigma surrounding HIV status has been well-documented as a barrier to testing in sub-Saharan Africa [46], including Uganda [16, 47], Kenya [48], Zimbabwe [19, 49], Nigeria [17, 50], South Africa [51–53] as well as in the United States [54], India [55, 56], and China [57, 58]. As treatment programs grow, some have noted VCT to have led a decrease of stigma due to patients’ abilities to resume their traditional roles as breadwinners and effective members of the family and community [59], but this has not been noted in a study in Mozambique [60]. In Zambézia Province, participants suggest that while expanded VCT and ART availability has not eliminated HIV stigma, the disease is less stigmatized than in the past. This decrease may be due in part to increased education as well as with the introduction of ART allowing patients to recover and live healthy productive lives.
Participants may not be motivated to risk the stigma and nutritional challenges associated with an HIV diagnosis unless they believe their health outcomes will improve with treatment; our focus group data suggest this will not occur unless people have sufficient food resources. Concerns about access to nutritious food and the long-term commitment to ART are reasonable and should not be ignored [61, 62]. High rates of poverty in Zambézia Province present challenges to even the best-funded care and treatment programs. The “siloed” vertical approach to providing nutrition and treatment programs separately may need to be reassessed. It is well documented in the literature that appetite increases for undernourished individuals placed on ART, given the immune reconstitution and rebuilding of muscle mass inherent in that process [31, 63]. With the increase of people taking ART in rural Mozambique, what is known to science is now becoming a concern to community members.
It is less clear how to address the fatalism expressed by participants about treating a chronic disease. The health system, originally designed to manage acute conditions, has yet to fully transition into a model where chronic illness is commonly managed successfully [64–66]. With few positive examples to follow, participants had a hard time conceptualizing a “medicine for life” model. While education is of paramount importance, providing more examples of patients successfully living with HIV (or diabetes, asthma, etc.) will likely have a greater impact on community opinions.
A study limitation is that we characterized opinions and perceptions of community participants in only rural districts in Zambézia Province. The opinions of our participants may not be relevant to those living in urban communities or other Provinces in Mozambique and may represent experiences unique to a given health facility, for example. We recommend a quantitative study follow-up in these districts to ensure the views of our participants are representative of the larger population. In addition, we do not know if our participants have been tested for HIV or if they were HIV positive, and thus their views might have been formed by what they had seen first-hand and/or heard from PLHIV. While none of the focus group facilitators provided medical services, participants knew they were affiliated with FGH, an NGO assisting in the scale-up of HIV testing and treatment in the province. While this could be seen as limitation, responses by the participants suggest they did not feel shy to express their displeasure with clinical services or the way HIV service delivery has been handled in Mozambique. Focus groups are known to elicit more views of verbal participants than shy ones. While we attempted to sample for diversity, our participants might not reflect the true representations of local populations’ views and perceptions, as they were chosen by local leaders and not through random sampling. In addition, translation from local languages (Echuabo and Elómwè) to Portuguese and subsequently to English was challenging. While we have made all attempts to maintain the integrity of our data, it is possible that some words or phrases were incorrectly translated, though we believe the substantive viewpoints were correctly inferred. In addition, there are always challenges of cultural understanding, especially in the rural context where only local languages are appropriately understood.
Conclusions
Focus group discussions offered community perceptions of HIV testing barriers in rural Zambézia Province, Mozambique. Despite recent efforts to expand HIV testing services in these six districts, there are still considerable barriers in wider acceptance of VCT particularly in rural setting. The health facility and health personal were both identified as a barrier: structural changes to ensure privacy and stronger regulations to ensure confidentiality among clinical workers are urgent and morally mandated. Stigmatization of HIV infection is still a strong barrier to VCT, but focus group participants suggest that it has lessened in recent years. We believe that additional ART explanation and further visible successes of ART on the physical appearance of people infected by HIV will also contribute in the reduction of stigma and perhaps greater uptake of VCT. However, there are still considerable challenges including poverty, access to effective medical care in rural areas, and the use of traditional healers as primary health care providers. Future programs should focus on facilitating transportation of patients; enabling nutritional supplements and agricultural assistance; and engaging traditional healers in the health care system. However, without improving the quality of clinical site services to improve confidentiality, patients will remain unwilling to test.
Biographies
CMA: carolyn.m.audet@vanderbilt.edu. Carolyn Audet is a medical anthropologist at the Institute for Global Health at Vanderbilt University. She is currently reseraching health seeking behavior and use of traditional medicine in rural Mozambique.
KG: kate.groh@vanderbilt.edu. Kate Groh is a resident in Internal Medicine at Vanderbilt University. She spent a year living in Mozambique as a Medical Scholar during Medical School.
TDM: Troy.Moon@fgh.org.mz. Troy Moon is a pediatrician and currently is the Clinical Director of Friends in Global Health in Mozambique.
SHV: sten.vermund@vanderbilt.edu. Sten Vermund is an Infectious Disease physican and is the Director of the Institute for Global Health at Vanderbilt University
MS: mmsidat@gmail.com. Mohsin Sidat is a Professor at University Eduardo Mondlane in Maputo, Mozambique. His research includes community based interventions to improve health outcomes in sub-Saharan Africa.
Footnotes
All authors read and approved the final manuscript.
References
- 1.Ministério da Saúde and Instituto Nacional de Saude. Inquérito Nacional de Prevalência, Riscos Comportamentais e Informação sobre o HIV e SIDA em Moçambique: Relatório Preliminar sobre a Prevalência da Infecção por HIV. INSIDA; 2009. Available from: http://xa.yimg.com/kq/groups/15255898/801713730/name/INSIDA. [Google Scholar]
- 2.World Health Organization (WHO), The Joint United Nations Programme on HIV/AIDS (UNAIDS), and United Nations Children’s Fund (UNICEF) Towards Universal Access: Scaling up Priority HIV/AIDS Interventions in the Health Sector. Progress Report 2009. 2009. [Google Scholar]
- 3.De Cock KM, Marum E, Mbori-Ngacha DA. A serostatus-based approach to HIV/AIDS prevention and care in Africa. The Lancet Infectious Diseases. 2003;362:1847–1849. doi: 10.1016/S0140-6736(03)14906-9. [DOI] [PubMed] [Google Scholar]
- 4.Granich RM, et al. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 5.National Statistics Institute (INE) National Survey on the Causes of Mortality in Mozambique (INCAM) Maputo: 2010. [Google Scholar]
- 6.Audet CM, et al. Sociocultural and epidemiological aspects of HIV/AIDS in Mozambique. BMC Int Health Hum Rights. 2010;10:15. doi: 10.1186/1472-698X-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bunnell R, et al. Changes in sexual behavior and risk of HIV transmission after antiretroviral therapy and prevention interventions in rural Uganda. AIDS. 2006;20(1):85–92. doi: 10.1097/01.aids.0000196566.40702.28. [DOI] [PubMed] [Google Scholar]
- 8.Vernazza PL, et al. Effect of antiviral treatment on the shedding of HIV-1 in semen. AIDS. 1997;11 (10):1249–54. doi: 10.1097/00002030-199710000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Cu-Uvin S, et al. Effect of highly active antiretroviral therapy on cervicovaginal HIV-1 RNA. AIDS. 2000;14(4):415–21. doi: 10.1097/00002030-200003100-00015. [DOI] [PubMed] [Google Scholar]
- 10.Quinn TC, et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. N Engl J Med. 2000;342(13):921–9. doi: 10.1056/NEJM200003303421303. [DOI] [PubMed] [Google Scholar]
- 11.Anglemyer A, et al. Antiretroviral therapy for prevention of HIV transmission in HIV-discordant couples. Cochrane Database Syst Rev. 2011;5:CD009153. doi: 10.1002/14651858.CD009153. [DOI] [PubMed] [Google Scholar]
- 12.Brocklehurst P, Volmink J. Antiretrovirals for reducing the risk of mother-to-child transmission of HIV infection. Cochrane Database Syst Rev. 2002;(1):CD003510. doi: 10.1002/14651858.CD003510. [DOI] [PubMed] [Google Scholar]
- 13.Volmink J, et al. Antiretrovirals for reducing the risk of mother-to-child transmission of HIV infection. Cochrane Database Syst Rev. 2007;(1):CD003510. doi: 10.1002/14651858.CD003510.pub2. [DOI] [PubMed] [Google Scholar]
- 14.van Dyk AC, van Dyk PJ. “To know or not to know”: service-related barriers to voluntary HIV counseling and testing (VCT) in South Africa. Curationis. 2003;26(1):4–10. doi: 10.4102/curationis.v26i1.1289. [DOI] [PubMed] [Google Scholar]
- 15.Matovu JK, Makumbi FE. Expanding access to voluntary HIV counselling and testing in sub-Saharan Africa: alternative approaches for improving uptake, 2001–2007. Trop Med Int Health. 2007;12(11):1315–22. doi: 10.1111/j.1365-3156.2007.01923.x. [DOI] [PubMed] [Google Scholar]
- 16.Bwambale F, et al. Voluntary HIV counselling and testing among men in rural western Uganda: Implications for HIV prevention. BMC Public Health. 2008;8(1):263. doi: 10.1186/1471-2458-8-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iliyasu Z, et al. Knowledge of HIV/AIDS and attitude towards voluntary counseling and testing among adults. J Natl Med Assoc. 2006;98(12):1917–22. [PMC free article] [PubMed] [Google Scholar]
- 18.Bond V, Chase E, Aggleton P. Stigma, HIV/AIDS and prevention of mother-to-child transmission in Zambia. Evaluation and Program Planning. 2002;25:347–356. [Google Scholar]
- 19.Morin S, et al. Removing barriers to knowing HIV status: same-day mobile HIV testing in Zimbabwe. J Acquir Immune Defic Syndr. 2006;41(2):218–224. doi: 10.1097/01.qai.0000179455.01068.ab. [DOI] [PubMed] [Google Scholar]
- 20.Pool R, Nyanzi S, Whitworth JA. Attitudes to voluntary counselling and testing for HIV among pregnant women in rural south-west Uganda. AIDS Care. 2001;13(5):605–15. doi: 10.1080/09540120120063232. [DOI] [PubMed] [Google Scholar]
- 21.Groh KE, et al. Barriers to antiretroviral therapy adherence in rural Mozambique. BMC Public Health. 2011;11(650) doi: 10.1186/1471-2458-11-650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morin SF, et al. Removing barriers to knowing HIV status: same-day mobile HIV testing in Zimbabwe. J Acquir Immune Defic Syndr. 2006;41(2):218–24. doi: 10.1097/01.qai.0000179455.01068.ab. [DOI] [PubMed] [Google Scholar]
- 23.Muchedzi A, et al. Factors associated with access to HIV care and treatment in a prevention of mother to child transmission programme in urban Zimbabwe. J Int AIDS Soc. 2010;13:38. doi: 10.1186/1758-2652-13-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Balcha TT, Jeppsson A, Bekele A. Barriers to antiretroviral treatment in ethiopia: a qualitative study. J Int Assoc Physicians AIDS Care (Chic) 2011;10(2):119–25. doi: 10.1177/1545109710387674. [DOI] [PubMed] [Google Scholar]
- 25.Chandisarewa W, et al. Routine offer of antenatal HIV testing (“opt-out” approach) to prevent mother-to-child transmission of HIV in urban Zimbabwe. Bull World Health Organ. 2007;85(11):843–50. doi: 10.2471/BLT.06.035188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anglewicz P, Chintsanya J. Disclosure of HIV status between spouses in rural Malawi. AIDS Care. 2011:1–8. doi: 10.1080/09540121.2010.542130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maman S, et al. Women’s barriers to HIV-1 testing and disclosure: challenges for HIV-1 voluntary counselling and testing. AIDS Care. 2001;13(5):595–603. doi: 10.1080/09540120120063223. [DOI] [PubMed] [Google Scholar]
- 28.Maman S, et al. High rates and positive outcomes of HIV-serostatus disclosure to sexual partners: reasons for cautious optimism from a voluntary counseling and testing clinic in Dar es Salaam, Tanzania. AIDS Behav. 2003;7(4):373–82. doi: 10.1023/b:aibe.0000004729.89102.d4. [DOI] [PubMed] [Google Scholar]
- 29.Moon T, et al. Lessons learned while implementing an HIV/AIDS care and treatment program in rural Mozambique. Retrovirology: Research and Treatment. 2010;(3):1–14. doi: 10.4137/RRT.S4613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krippendorff K. Content Analysis: An Introduction to its Methodology. 2. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- 31.Kalofonos IA. All I Eat Is ARV’S: The Paradox of AIDS Treatment Interventions in Central Mozambique. Medical Anthropology Quarterly. 2010;24(3):363–380. doi: 10.1111/j.1548-1387.2010.01109.x. [DOI] [PubMed] [Google Scholar]
- 32.Van Damme W, Kober K, Laga M. The real challenges for scaling up ART in sub-Saharan Africa. AIDS. 2006;20(5):653–6. doi: 10.1097/01.aids.0000216364.44409.b1. [DOI] [PubMed] [Google Scholar]
- 33.Wools-Kaloustian K, et al. Viability and effectiveness of large-scale HIV treatment initiatives in sub-Saharan Africa: experience from western Kenya. AIDS. 2006;20(1):41–8. doi: 10.1097/01.aids.0000196177.65551.ea. [DOI] [PubMed] [Google Scholar]
- 34.Audet C, et al. Traditional healer consultation is associated with a 3 month delay in HIV testing among symptomatic HIV-positive patients in rural Mozambique. XIX International AIDS Conference; 2012; Washington, CD. [Google Scholar]
- 35.Patel V, Rogers R, Haux R. MEDINFO 2001 proceedings of the 10th World Congress on Medical Informatics; London. 2–5 September 2001; London, U.K: IOS Press; 2001. p. 1. computer optical disc. [Google Scholar]
- 36.Teal CR, Street RL. Critical elements of culturally competent communication in the medical encounter: a review and model. Soc Sci Med. 2009;68(3):533–43. doi: 10.1016/j.socscimed.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 37.Street RL, Jr, et al. How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ Couns. 2009;74(3):295–301. doi: 10.1016/j.pec.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 38.Patak L, et al. Improving patient-provider communication: a call to action. J Nurs Adm. 2009;39(9):372–6. doi: 10.1097/NNA.0b013e3181b414ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hudelson P. Improving patient-provider communication: insights from interpreters. Fam Pract. 2005;22(3):311–6. doi: 10.1093/fampra/cmi015. [DOI] [PubMed] [Google Scholar]
- 40.Carr GS. Negotiating trust: a grounded theory study of interpersonal relationships between persons living with HIV/AIDS and their primary health care providers. J Assoc Nurses AIDS Care. 2001;12(2):35–43. doi: 10.1016/S1055-3290(06)60132-5. [DOI] [PubMed] [Google Scholar]
- 41.Fosbinder D. Patient perceptions of nursing care: an emerging theory of interpersonal competence. J Adv Nurs. 1994;20(6):1085–93. doi: 10.1046/j.1365-2648.1994.20061085.x. [DOI] [PubMed] [Google Scholar]
- 42.Attree M. Patients’ and relatives’ experiences and perspectives of ‘Good’ and ‘Not so Good’ quality care. J Adv Nurs. 2001;33(4):456–66. doi: 10.1046/j.1365-2648.2001.01689.x. [DOI] [PubMed] [Google Scholar]
- 43.Fylkesnes K, Siziya S. A randomized trial on acceptability of voluntary HIV counselling and testing. Trop Med Int Health. 2004;9(5):566–72. doi: 10.1111/j.1365-3156.2004.01231.x. [DOI] [PubMed] [Google Scholar]
- 44.Irwin K, Valdiserri R. The acceptability of voluntary HIV antibody testing in the United States: A decade of lessons learned. AIDS. 1996;10:1707–1717. doi: 10.1097/00002030-199612000-00016. [DOI] [PubMed] [Google Scholar]
- 45.Wilkin D, Hallam L, Dogett M. Measures of Need and Outcome for Primary Care. New York: Oxford University Press; 1992. [Google Scholar]
- 46.Matovu J, Makumbi F. Expanding access to voluntary HIV counselling and testing in sub-Saharan Africa: alternative approaches for improving uptake, 2001–2007. Trop Med Int Health. 2007;12(11):1315–1322. doi: 10.1111/j.1365-3156.2007.01923.x. [DOI] [PubMed] [Google Scholar]
- 47.Wolff B, et al. Evaluation of a home-based voluntary counselling and testing intervention in rural Uganda. Health Policy Plan. 2005;20(2):109–116. doi: 10.1093/heapol/czi013. [DOI] [PubMed] [Google Scholar]
- 48.Turan JM, et al. HIV/AIDS Stigma and Refusal of HIV Testing Among Pregnant Women in Rural Kenya: Results from the MAMAS Study. AIDS Behav. 2011;15(6):1111–20. doi: 10.1007/s10461-010-9798-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sherr L, et al. Voluntary counselling and testing: uptake, impact on sexual behaviour, and HIV incidence in a rural Zimbabwean cohort. AIDS. 2007;21(7):851–860. doi: 10.1097/QAD.0b013e32805e8711. [DOI] [PubMed] [Google Scholar]
- 50.Okonkwo KC, et al. An evaluation of awareness: attitudes and beliefs of pregnant Nigerian women toward voluntary counseling and testing for HIV. AIDS Patient Care STDS. 2007;21(4):252–60. doi: 10.1089/apc.2006.0065. [DOI] [PubMed] [Google Scholar]
- 51.Hutchinson P, Mahlalela X. Utilization of voluntary counseling and testing services in the Eastern Cape, South Africa. AIDS Care. 2006;18(5):446–455. doi: 10.1080/09540120500213511. [DOI] [PubMed] [Google Scholar]
- 52.Kalichman S, Simbayi L. HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sex Transm Infect. 2003;79(6):442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Meiberg AE, et al. Fear of stigmatization as barrier to voluntary HIV counselling and testing in South Africa. East Afr J Public Health. 2008;5(2):49–54. [PubMed] [Google Scholar]
- 54.Fortenberry JD, et al. Relationships of stigma and shame to gonorrhea and HIV screening. Am J Public Health. 2002;92(3):378–81. doi: 10.2105/ajph.92.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Solomon S, et al. Challenges of expansion of voluntary counselling and testing in India. Sex Health. 2008;5(4):371–2. doi: 10.1071/sh07090. [DOI] [PubMed] [Google Scholar]
- 56.Meundi AD, et al. Cross-sectional population-based study of knowledge, attitudes, and practices regarding HIV/AIDS in Dakshina Kannada district of Karnataka, India. J Int Assoc Physicians AIDS Care (Chic) 2008;7(1):27–34. doi: 10.1177/1545109707302088. [DOI] [PubMed] [Google Scholar]
- 57.Hong Y, et al. HIV Testing Behaviors Among Female Sex Workers in Southwest China. AIDS Behav. 2011 doi: 10.1007/s10461-011-9960-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Song Y, et al. HIV-testing behavior among young migrant men who have sex with men (MSM) in Beijing, China. AIDS Care. 2011;23(2):179–86. doi: 10.1080/09540121.2010.487088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Castro A, Farmer P. Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. Am J Public Health. 2005;95(1):53–9. doi: 10.2105/AJPH.2003.028563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pearson CR, et al. One year after ART initiation: psychosocial factors associated with stigma among HIV-positive Mozambicans. AIDS Behav. 2009;13(6):1189–96. doi: 10.1007/s10461-009-9596-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anabwani G, Navario P. Nutrition and HIV/AIDS in sub-Saharan Africa: an overview. Nutrition. 2005;21(1):96–9. doi: 10.1016/j.nut.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 62.Weiser SD, et al. Food insecurity as a barrier to sustained antiretroviral therapy adherence in Uganda. PLoS One. 2010;5(4):e10340. doi: 10.1371/journal.pone.0010340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ivers LC, et al. HIV/AIDS, undernutrition, and food insecurity. Clin Infect Dis. 2009;49(7):1096–102. doi: 10.1086/605573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Beran D, Yudkin JS. Diabetes care in sub-Saharan Africa. Lancet. 2006;368(9548):1689–95. doi: 10.1016/S0140-6736(06)69704-3. [DOI] [PubMed] [Google Scholar]
- 65.Idemyor V. Diabetes in sub-Saharan Africa: health care perspectives, challenges, and the economic burden of disease. J Natl Med Assoc. 2010;102(7):650–3. doi: 10.1016/s0027-9684(15)30643-x. [DOI] [PubMed] [Google Scholar]
- 66.Bousquet J, et al. Management of chronic respiratory and allergic diseases in developing countries. Focus on sub-Saharan Africa. Allergy. 2003;58(4):265–83. doi: 10.1034/j.1398-9995.2003.02005.x. [DOI] [PubMed] [Google Scholar]