INTRODUCTION
Gestational diabetes mellitus (GDM) was earlier defined as “hyperglycemia first recognized during pregnancy” and has more recently been described by American Diabetes Association (ADA) (2012) as diabetes diagnosed during pregnancy that is not clearly overt diabetes.[1] The hyperglycemia and adverse pregnancy outcomes study (HAPO) demonstrated that the risk of adverse maternal, fetal, and neonatal outcomes continuously increase as a function of maternal glycemia at 24−28 weeks, even within ranges previously considered normal for pregnancy.[2] After reviewing the results of the HAPO study, many international diabetes study groups, including the International Association of Diabetes and Pregnancy Study Groups and ADA have adopted the 75 g oral glucose tolerance test (OGTT) at 24−28 weeks as a screening and diagnostic test and defined new cut-off values for GDM diagnosis. The Ministry of Health of China published the criteria for GDM, that is the same as the ADA criteria on July 1, 2011. World Health Organization (WHO) has recommended the 75 g OGTT with different cut-off values as a diagnostic test since 1999, changed its recommendation on 2013. In Hongkong and Yunnan province in China, most hospital adopted the WHO 1999 criteria, nevertheless, there is no evidence of multicenter and large sample to show that the GDM population within the same ethnic group diagnosed by the new WHO criteria matches those diagnosed by the old one and consistency between the two criteria has not been reported. Thus, we conducted this study to analyze the two criteria in Chinese pregnant women.
METHODS
Study population
The World Diabetes Foundation (WDF) Denmark funded a project in 2010 to help establish GDM centers in China (10–517). As part of the project data of 17, 186 pregnant women were systematically collected in 13 hospitals, including Peking University First Hospital (PUFH) where 75 g OGTT between 24 and 28 weeks was carried out on all pregnant women. At the PUFH these records pertained to women registered at the prenatal clinic between January 1, 2010 and December 31, 2012, while at the other 12 participating hospitals records pertained to women registered between July 1, 2011 and February 29, 2012. After an overnight fast venous blood samples were recorded at 0 hour; 1 hour and 2 hours after a 75 g glucose load. Previously known DM patients and DM patients diagnosed by fasting plasma glucose ≥7.00 mmol/L at the first prenatal visit were excluded from the study.
Diagnostic criteria for gestational diabetes mellitus
As described a diagnostic 2-h 75 g OGTT at 24–28th week of gestation was carried out. Two different cut-off values of plasma glucose were used to analyze the data: GDM was diagnosed by WHO 2013 criteria when one of the following plasma glucose value was met or exceeded: 0 hour, 5.10 mmol/L; 1 hour, 10.00 mmol/L; 2 hours, 8.50 mmol/L; GDM was diagnosed by WHO 1999 criteria when 0 hour ≥7.00 mmol/L or 2 hours ≥7.80 mmol/L.
Statistical analysis
Data analysis was performed using the Predictive Analytics Software Statistics (PASW), formerly called SPSS Statistics, which was acquainted by IBM in 2009. The eligible population of pregnant women included in the study was classified into four groups: (1) Normal by both WHO 1999 and 2013 criteria; (2) GDM by both 1999 and 2013 criteria; (3) GDM by WHO 2013 criteria only; (4) GDM by WHO 1999 criteria only. Frequency and mean of each group were analyzed.
RESULTS
As shown in Figure 1 and Table 1, GDM prevalence was similar using both the WHO 1999 and 2013 criteria (17.2% and 17.5%, respectively). The constituent ratio of normal and GDM patients diagnosed by both criteria were 77.0% and 11.6% respectively. The consistency rate of the two criteria was 88.6%. An additional 5.8% of pregnant women were diagnosed GDM by 2013 criteria only and 5.5% only by 1999 criteria.
Figure 1.
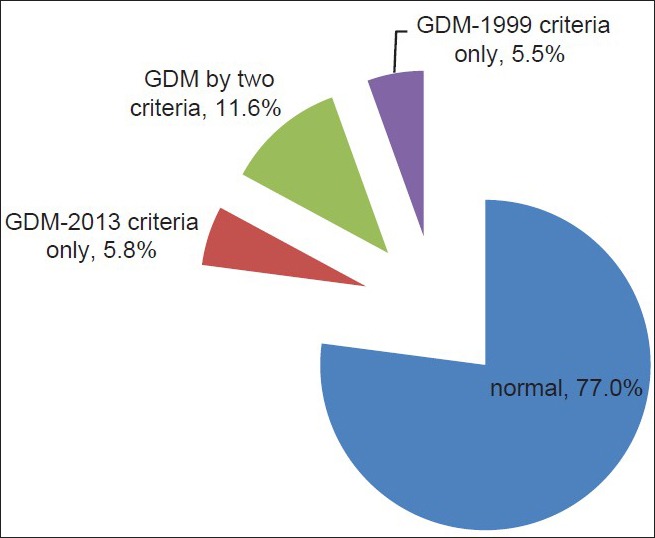
The distribution of gestational diabetes mellitus patients with different criteria in China.
Table 1.
The distribution and mean plasma glucose values of GDM patients with different criteria in China
| Groups | Number (%) | OGTT 0 h (mmol/L) | OGTT 1 h (mmol/L) | OGTT 2H (mmol/L) | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Normal | 13,232 (77.0) | 4.38 | 0.34 | 7.42 | 1.36 | 6.12 | 0.94 |
| GDM by two criteria | 2000 (11.6) | 4.97* | 0.83 | 10.16* | 1.63 | 9.31* | 1.22 |
| GDM-2013 criteria only | 1002 (5.8) | 5.19*,† | 0.47 | 8.98*,† | 1.64 | 6.63*,† | 0.88 |
| GDM-1999 criteria only | 952 (5.5) | 4.45*,†,‡ | 0.35 | 8.57*,†,‡ | 1.04 | 8.09*,†,‡ | 0.19 |
| Total | 17,186 (100.0) | 4.50 | 0.53 | 8.01 | 1.73 | 6.63 | 1.51 |
*,†,‡Show the statistically significant difference when P<0.001. *Compared with group “normal”, †Compared with group “GDM-2013 criteria only”, ‡Compared with group “GDM-1999 criteria only”. GDM: Gestational diabetes mellitus; OGTT: Oral glucose tolerance test; SD: Standard deviation.
As shown in Table 1 and Figure 2, the mean of plasma glucose values at 0 hour, 1 hour and 2 hours show statistically significant differences between any two groups (P < 0.001). Women meeting GDM diagnostic criteria of both 1999 and 2013, had the highest mean plasma glucose value at 1 h (10.16 ± 1.63 mmol/L) and 2 h (9.31 ± 1.22 mmol/L), whereas women meeting the 2013 criteria only displayed the highest mean value at 0 hour (5.19 ± 0.47 mmol/L) and lower mean value at 2 hours (6.63 ± 0.88 mmol/L) compared to women meeting the 1999 criteria, who had higher mean 2 hours (8.09 ± 0.19 mmol/L) value.
Figure 2.
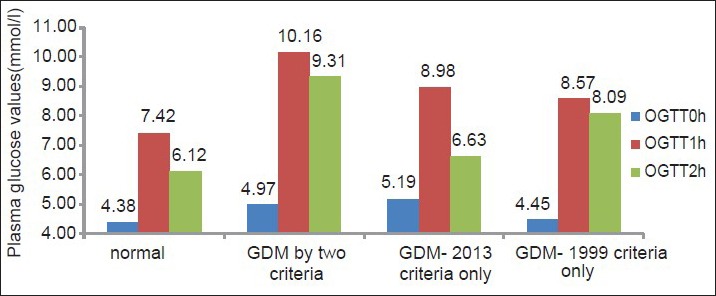
Mean plasma glucose values (mmol/L) of the four groups.
DISCUSSION
Hyperglycemia and adverse pregnancy outcomes study data show that the prevalence increased from 11.3% with the old WHO criteria to 16.1% with the new criteria.[2] Similar results are seen from other countries-in the United Arab Emirates 20.3% to 37.7%;[3] Australia 9.6% to 13.0%.[4] Compared to these other studies where the difference were substantial (3.4–17.4%), the prevalence did not change (0.3%) with the two criteria in China. However, the result shows that GDM patients identified by the two criteria are not exactly same (5.8% were identified only by the WHO 2013 criteria and 5.5% only by the WHO 1999 criteria). When the old WHO criteria changes to the new criteria, from the point of view of reducing complications, the 5.5% pregnant women will not been treated and the outcome in these untreated women needs to be considered.
Furthermore, GDM patients diagnosed only by WHO 1999 criteria displayed higher mean 2 hours postprandial plasma glucose value (8.09 mmol/L) than the ones diagnosed only by WHO 2013 criteria (6.63 mmol/L). de Veciana et al.[5] reported that adjustment of insulin therapy in women with GDM according to the results of postprandial has a better outcome than preprandial. Thus comparing the outcome of the two GDM groups diagnosed only by one single criterion is needed.
Therefore as part of the ongoing WDF project (10–517), we have just started a sampling survey in Beijing and Guangzhou in 2013, which will collect clinical data of over 20 thousand pregnant women to analyze the incidence of GDM and will follow up the postpartum outcomes. We will use the survey data to compare the outcome of different group.
The diagnostic criteria of WHO (2013) and WHO (1999) show disparity and do not exactly identify the same population of pregnant women with GDM in China. For most hospitals in Hongkong and in Yunnan province that use the WHO 1999 criteria, this must be kept in mind when changing to the 2013 criteria for GDM.
Footnotes
Edited by: Limin Chen
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2012;35(Suppl 1):s11–63. doi: 10.2337/dc12-s011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.HAPO Study Cooperative Research Group. Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358:1991–2002. doi: 10.1056/NEJMoa0707943. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal MM, Dhatt GS, Shah SM. Gestational diabetes mellitus: Simplifying the international association of diabetes and pregnancy diagnostic algorithm using fasting plasma glucose. Diabetes Care. 2010;33:2018–20. doi: 10.2337/dc10-0572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi LT, Li GQ. Study on the differences between IADPSG criteria for gestational diabetes mellitus (in Chinese) Chin J Diabetes. 2014;22:385–8. [Google Scholar]
- 5.de Veciana M, Major CA, Morgan MA, Asrat T, Toohey JS, Lien JM, et al. Postprandial versus preprandial blood glucose monitoring in women with gestational diabetes mellitus requiring insulin therapy. N Engl J Med. 1995;333:1237–41. doi: 10.1056/NEJM199511093331901. [DOI] [PubMed] [Google Scholar]


