Abstract
Background:
The incidence of congenital coronary artery anomalies (CCAAs) is different between ethnic groups, but there is no report about Uyghur CCAAs because of the limitation of inspection methods. This study determined the prevalence of Uyghur CCAAs and analysis the difference of CCAAs between Uyghur and Han ethnic groups by the method of multi-slice computed tomography coronary angiography (MSCTCA).
Methods:
Seven thousand four hundred and sixty-nine MSCTCA were analyzed for the CCAAs retroactively, 1934 were Uyghur patients while 4746 were Han patients. All the coronary artery images dates obtained by MSCTCA were evaluated for the CCAAs by two doctors.
Results:
Nineteen kinds of CCAAs were found: (1) The overall incidence of CCAAs was 2.72% (203/7469) among all patients, 2.34% (111/4746) among Han patients whereas a significant higher 3.93% (76/1934) among Uyghur patients (χ2 = 12.780,P < 0.05); (2) the incidence of CCAAs among male patients was 2.48% (76/3069) in Han while 4.33% (56/1293) in Uyghur (χ2 = 10.663, P < 0.05); (3) the incidence of CCAAs on the left side was 1.07% (51/4746) among Han patients while 2.17% (42/934) among Uyghur patients (χ2 = 12.047, P < 0.05); (4) among these 19 kinds of CCAAs, there were significant differences of the incidence of the following kinds of CCAAs between Uyghur and Han: Left coronary artery (LCA) high location (χ2 = 8.320, P = 0.004), right coronary artery (RCA) originate from left coronary sinus (χ2 = 5.450, P = 0.020), and RCA originate from left Coronary sinus + LCA high location (P = 0.024).
Conclusions:
There exists some difference in CCAAs between Uyghur and Han ethnic groups. The CCAAs incidence of Uyghur is higher than that of Han, especially in male patients and on the left side; among all kinds of CCAAs, the incidence of LCA high location, RCA originate from left coronary sinus, RCA originate from left coronary sinus + LCA high locations of Uyghur is higher than Han.
Keywords: Congenital Coronary Artery Anomalies, Han, Tomography, Uyghur, X-ray Computed
INTRODUCTION
Congenital coronary artery anomalies (CCAAs) are some of incidental, uncommon, asymptomatic, and neglected topics in cardiology. Some may predispose the patient for developing an acute myocardial damage and/or chronic injuries in the area supplied by the anomalous coronary artery,[1,2,3,4] sometimes even fatal. Lots of researchers have been studied the incidence, pathophysiology, and clinical relevance of CCAAs, and the incidence of CCAAs are different between ethnic groups. However, it is hard to obtain Uyghur corpse, so there are no reports about Uyghur CCAAs before. In the past few years, lots of research showed that the multi-slice computed tomography coronary angiography (MSCTCA) should therefore be considered as a prime non-invasive imaging tool for suspecting coronary anomalies,[5,6,7,8,9] which provide us a useful method to evaluate Uyghur CCAAs in vivo. The purpose of this study was to identify the CCAAs of Uyghur and compare the difference of incidence between Uyghur and Han retrospectively by the method of MSCTCA.
METHODS
This was a retrospective study. The study protocol was approved by the Ethics Committee of our institution. All the patients collected after the research begun had clear indications and clinical purpose for MSCTCA and provided written informed consent.
Study population
Between September 2006 and May 2012, 8027 MSCTCA were performed on 7469 patients in our institution. The demographic findings and indications for MSCTCA in these populations are summarized in Tables 1 and 2.
Table 1.
Patients characteristics
| Items | Number of patients (male/female) | Mean age ± SD |
|---|---|---|
| Han | 4746 (3069/1677) | 60.26 ± 12.00 |
| Uyghur | 1934 (1293/641) | 56.33 ± 10.89 |
| Other | 789 (493/296) | 58.12 ± 10.94 |
| Total | 7469 (4855/2614) | 59.07 ± 11.75 |
SD: Standard deviation.
Table 2.
Additional patients’ characteristics of 7469 study patients
| Patients’ characteristics | Number (%) |
|---|---|
| Disease background | |
| Suspicious CHD | 4282 (57.33) |
| Hypertension | 1475 (19.75) |
| Perfect heart function examination before surgery | 761 (10.19) |
| Arrhythmia | 689 (9.22) |
| Type II diabetes | 571 (7.64) |
| Postoperative of PCI | 475 (6.36) |
| Chronic cerebral circulation insufficiency | 262 (3.51) |
| Mental disorder | 119 (1.59) |
| Dyslipidemia | 72 (0.96) |
| Postoperative of CABG | 62 (0.83) |
| Clinical examination purpose | |
| Diagnose/eliminate CHD | 6052 (81.03) |
| Perfect heart function examination before surgery | 761 (10.19) |
| Follow-up of PCI | 475 (6.36) |
| Mental symptoms eliminative diagnosis | 119 (1.59) |
| Follow-up of CABG | 62 (0.83) |
CABG: Coronary artery bypass graft, CHD: Coronary heart disease, PCI: Percutaneous coronary intervention.
Multi-slice computed tomography coronary angiography scanning
With the use of a 64-detector (GE LightSpeed VCT 64 Slice CT, USA) CT unit, MSCTCA was performed from the level of the main pulmonary artery (PA) caudally through the entire heart. Images were acquired with 0.625 mm section collimation, a tube potential of 120 kV, rotation time 0.35 seconds, and tube current range of 300–750 mA (the effective tube current depends on the electrocardiogram-controlled tube current modulation) at 64-detector CT. The 75–90 ml bolus of iohexol (370 mgI/ml) with a 20–25 ml saline solution chaser was administered intravenously at 4–4.5 ml/s depends on different patients.
A region of interest was placed in the ascending aorta at the level of left coronary artery (LCA) root, and image acquisition was artificially initiated once a selected threshold (120 HU) was reached with bolus tracking.
The data set was reconstructed with the reconstruction window starting at the end-diastolic phase (75% of RR interval) or the end-systolic phase (45% of RR interval) of the cardiac cycle. Additional reconstructions were performed if motion artifacts were present.
Image evaluation and data processing
Post-processing techniques contains volume rendering technique (VR), tree VR, curved planar reconstruction, multiple planar reconstruction and maximum intensity projection.
The films were reviewed by two independent investigators. The CT images were analyzed, and those with anomalous coronary arteries were selected for further assessment. In the event of any discrepancy between the two reviewers, a consensus was reached after discussion. Patients with CCAAs occurring as part of a complex congenital heart disease were not included in this study.
The course of the anomalous artery was defined according to the guidelines of Yamanaka and Hobbs.[10]
Statistical analyses
Chi-square test was used to assess for any significant difference of the incidence of CCAAs between Uyghur and Han. P < 0.05 was considered as indicate statistical significance. The statistical analyzes were performed with SPSS software, version 17.0 (SPSS, Chicago, IL, USA).
RESULTS
Data of 7469 patients who underwent MSCTCA were reviewed. 203 patients who had CAAS were entered into final data analysis, and the data of CAAS were summarized in Table 3.
Table 3.
Number of different CCAAs in MSCTCA (total of 7469 patients)
| Items | Number of patients (male/female) | |||
|---|---|---|---|---|
| Uyghur | Han | Other ethnic groups | Total | |
| LCA high location | 21 (18/3) | 22 (17/5) | 4 (1/3) | 47 (36/11) |
| LCA originate from right coronary sinus | 2 (2/0) | 3 (1/2) | 1 (0/1) | 6 (3/3) |
| Absent of LMA | 10 (9/1) | 14 (9/5) | 3 (2/1) | 27 (20/7) |
| Absent of LCX | 5 (4/1) | 4 (2/2) | 1 (1/0) | 10 (7/3) |
| LCX originate from right coronary sinus | 1 (0/1) | 3 (2/1) | 0 (0/0) | 4 (2/2) |
| LCX originate from RCA | 0 (0/0) | 1 (1/0) | 0 (0/0) | 1 (1/0) |
| LCA originate from RPA | 0 (0/0) | 1 (1/0) | 0 (0/0) | 1 (1/0) |
| LAD originate from RCA | 1 (1/0) | 1 (1/0) | 0 (0/0) | 2 (2/0) |
| RCA high location | 11 (7/4) | 26 (19/7) | 0 (0/0) | 37 (26/11) |
| RCA originate from LAD | 0 (0/0) | 1 (0/1) | 0 (0/0) | 1 (0/1) |
| Single coronary artery | 0 (0/0) | 1 (1/0) | 0 (0/0) | 1 (1/0) |
| RCA originate from left coronary sinus | 19 (11/8) | 23 (13/10) | 6 (4/2) | 48 (28/20) |
| RCA originate from left coronary sinus+LCA high location | 3 (2/1) | 0 (0/0) | 0 (0/0) | 3 (2/1) |
| RCA high location+LCA originate from RCA | 0 (0/0) | 1 (1/0) | 0 (0/0) | 1 (1/0) |
| RCA+LCA high location | 1 (1/0) | 7 (6/1) | 1 (1/0) | 9 (8/1) |
| Fistulas from LAD to PA | 1 (1/0) | 0 (0/0) | 0 (0/0) | 1 (1/0) |
| Fistulas from LAD to left ventricle | 0 (0/0) | 1 (1/0) | 0 (0/0) | 1 (1/0) |
| Fistulas from LCA to PA | 1 (0/1) | 1 (0/1) | 0 (0/0) | 2 (0/2) |
| Fistulas from accessory coronary artery to PA | 0 (0/0) | 1 (1/0) | 0 (0/0) | 1 (1/0) |
| Total | 76 (56/20) | 111 (76/35) | 16 (9/7) | 203 (141/62) |
LMA: Left main coronary artery, LCA: Left coronary artery, LAD: Left anterior descending, LCX: Left circumflex coronary artery, RCA: Right coronary artery, PA: Pulmonary artery, RPA: Right pulmonary artery, CCAAs: Congenital coronary artery anomalies, MSCTCA: Multi-slice computed tomography coronary angiography.
Incidence of CCAAs
The overall incidence of CCAAs was 2.72% (203/7469) among all patients, while 2.34% (111/4746) among Han patients and 3.93% (76/1934) among Uyghur patients, which is significant higher than Han (χ2 = 12.780, P = 0.000).
Incidence of CCAAs in different sex
The incidence of CCAAs among male patients was 2.48% (76/3069) in Han while a significant higher 33% (56/1293) in Uyghur (χ2 = 10.663, P = 0.001); the incidence of CCAAs among female patients was 2.09% (35/1677) in Han while 3.12% (20/641) in Uyghur (χ2 = 2.137, P = 0.144).
Incidence of CCAAs on different side
The incidence of CCAAs on the left side was 1.07% (51/4746) among Han patients while a significant higher 2.17% (42/934) among Uyghur patients (χ2 = 12.047, P = 0.001); the incidence of CCAAs on the right side was 1.20% (52/4746) among Han patients while 1.55% (30/1934) among Uyghur patients (χ2 = 2.352, P = 0.125); The incidence of CCAAs on both side was 0.17% (8/4746) among Han patients while 0.21% (4/1934) among Uyghur patients (χ2 = 0.000, P = 0.987).
Incidence of “benign” and “potentially serious” CCAAs
There were 19 different kinds of CCAAs in this research, the “benign” are as follows: LCA high location, absent of left main coronary artery (LMA), absent of left circumflex coronary artery (LCX), LCX originate from right coronary sinus, LCX originate from right coronary artery (RCA), RCA high location, small fistula (fistulas from left anterior descending [LAD] to PA, fistulas from accessory coronary artery to PA, fistulas from LAD to left ventricle, fistulas from LCA to PA), RCA high location + LCA high location (RCA and LCA origin from the ascending aorta above the sinuses of Valsalva separately); the “potentially serious” are as follows: LCA originate from right coronary sinus, LAD originate from RCA, LCA originate from right PA (RPA), RCA originate from LAD, single coronary artery, RCA originate from left coronary sinus, RCA originate from left coronary sinus + LCA high location. RCA high location + LCA originate from RCA, RCA high location + LCA high location (RCA and LCA origin from the ascending aorta above the commissural or the left sinus of Valsalva together) 0.50 in 76 CCAAs of Uyghur are begin while other 26 are potentially serious, and 77 in 111 CCAAs of Han are begin while other 34 are potentially serious, the difference of “benign” and “potentially serious” CCAAs between Uyghur and Han was not statistically significant (χ2 = 0.265, P = 0.606).
Constituent ratio of CCAAs
19 different kinds of CCAAs were found in this research. There were no significant differences of the constituent ratio of CCAAs between Uyghur and Han (χ2 = 17.312, P = 0.358).
Incidence of different kinds of CCAAs
Among these 19 kinds of CCAAs, there were significant differences of the incidence of the following kinds of CCAAs between Uyghur and Han: LCA high location (χ2 = 8.320, P = 0.004), RCA originate from left coronary sinus (χ2 = 5.450, P = 0.020), and RCA originate from left Coronary sinus + LCA high location (P = 0.024); there were no significant differences of the incidence of other CCAAs between Uyghur and Han.
DISCUSSION
Incidence of congenital coronary artery anomalies
Congenital coronary artery anomalies is a very rare disease, this is in agreement with 0.6–1.3% incidence reported previously in different studies.[10,11,12,13,14] In the largest angiographic review reported by Yamanaka and Hobbs, the incidence of coronary artery anomalies in 126,595 American people was reported as 1.3% (1686 out of 126,595 patients).[10] Most of the reported researches used selective CA (SCA) to detect the CCAAs. SCA is a traumatic examination, which is normally used in patients who are suspected of myocardial ischemia or need cardiac surgery. This limits the CCAAs detection rate to a certain extent.
However, autopsy results are lower. Alexander and Griffith found only 54 cases (0.3%) of CCAAs in 18,950 autopsies. Because it is unlikely to use large-scale conventional autopsy to study of CCAAs, so these data only from the sudden death or forensic medicine appraisal results of outside hospital death. Therefore, these two methods can not reflect the incidence of CCAAs among general population.
We found 203 CCAAs in 7469 patients; the incidence (2.72%) was higher than the past reports which used the methods of SCA and autopsy. Coincidentally some other reports which used the methods of MSCTCA also found higher incidence in recent years, like Schmitt R reported the incidence as 2.5% (44 out of 1758 patients),[15] Shi et al. reported the incidence as 6.6% (16 out of 242 patients),[6] and Duran et al. reported the incidence as 5.79% (42 out of 725 patients).[16] The reason causing this difference may be as follows: First, the different methods. The application range of SCA and autopsy are limited, most of the samples are suspected of myocardial ischemia, need cardiac surgery, the sudden death or forensic medicine appraisal results of outside hospital death, however MSCTCA is a non-invasive examination, so it has more widely clinical application and is also used in screening patients with coronary heart disease risk factors, moreover it is better to show the origin, distribution, course of coronary artery which enables clinicians to observe the morphology of coronary artery in a better way, so as to improve the detection rate of CCAAs; Second, we consider of different race. We found the CCAAs incidence was 3.93% among Uyghur patients, which is higher than 2.34% among Han patients.
The clinical significance of congenital coronary artery anomalies
Although there are many different classification methods of CCAAs, most of the researchers agree with Yamanaka and Hobbs,[10] he divided CCAAs into “benign” and “potentially serious” according to whether CCAAs cause myocardial ischemia. In this research, the “benign” are as follows: LCA high location, absent of LMA, absent of LCX, LCX originate from right coronary sinus, LCX originate from RCA, RCA high location; the “potentially serious” are as follows: LCA originate from right coronary sinus, LAD originate from RCA, LCA originate from RPA, RCA originate from LAD, Single coronary artery, RCA originate from left coronary sinus, RCA originate from left coronary sinus + LCA high location, RCA high location + LCA originate from RCA.
We found five cases of fistula, one is fistula from LCA to PA, one is fistula from LAD to left ventricle [Figure 1], two are fistulas from LAD to PA, and one is fistulas from accessory coronary artery to PA. All the fistula were small, and none of them “drained into one of the right cardiac chambers” and cause the “left to right shunts”. As Yamanaka and Hobbs[10] described “Fistulae draining into right heart chambers function as left to right shunts and may result in right ventricular volume overload. Hence, we classified the fistulas into the “benign” group.
Figure 1.
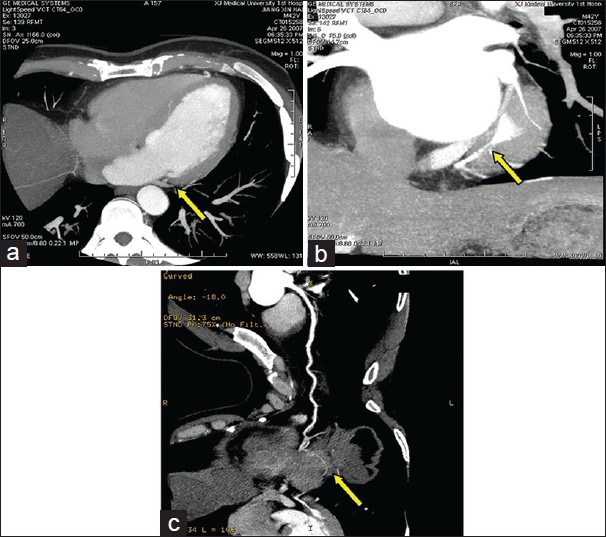
(a-c) The fistula from left anterior descending to left ventricle on axial, coronal maximum intensity projection and multiple planar reconstruction images.
We found nine cases of RCA + LCA high location, and they can divide into two group: One group is RCA and LCA origin from the ascending aorta above the sinuses of Valsalva separately without abnormal distributing [Figure 2], we classified it to “benign” group; another group is RCA and LCA origin from the ascending aorta above the commissural or the left sinus of Valsalva together, RCA passed between the aorta and PA before reaching the right atrioventricular groove [Figure 3], ostial occlusion due to aortic expansion during exercise may result in myocardial ischemia, so we classified it to “potentially serious” group. In this research, one case of RCA + LCA high location in Uyghur and one case of RCA + LCA high locations in other ethnic groups are “potentially serious”, three of seven cases of RCA + LCA high locations in Han are “potentially serious”, and the other 4 cases are “benign”.
Figure 2.
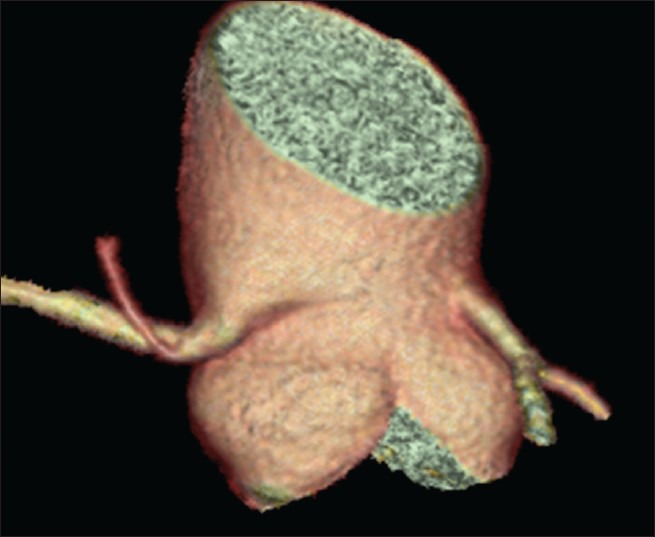
Right coronary artery and left coronary artery origin from the ascending aorta above the sinuses of Valsalva separately without abnormal distributing.
Figure 3.
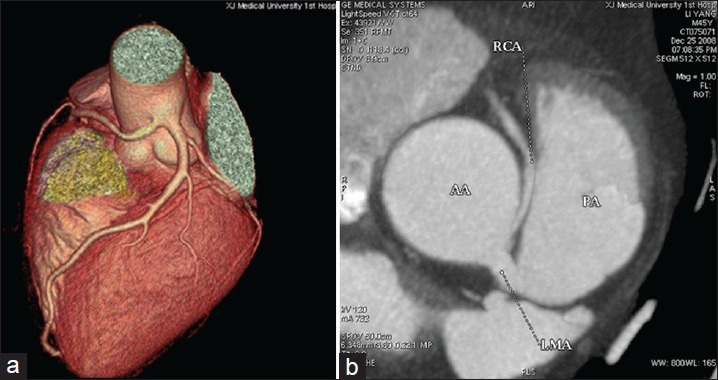
(a) Right coronary artery (RCA) and left coronary artery origin from the ascending aorta above the left sinus of Valsalva together, (b) RCA passed between the aorta and pulmonary artery before reaching the right atrioventricular groove, and ostial occlusion due to aortic expansion.
The incidence of CCAAs in Uyghur is higher than in Han, especially among male patients or on the left side. Among all kinds of CCAAs, the incidence of LCA high location, RCA originate from left coronary sinus, RCA originate from left coronary sinus + LCA high locations in Uyghur is higher than in Han.
Footnotes
Edited by: Jian Gao
Source of Support: Research Award Fund of the first teaching hospital of Xingjiang Medical University (No. 2011YFY09).
Conflict of Interest: None declared.
REFERENCES
- 1.Makaryus AN, Orlando J, Katz S. Anomalous origin of the left coronary artery from the right coronary artery: A rare case of a single coronary artery originating from the right sinus of valsalva in a man with suspected coronary artery disease. J Invasive Cardiol. 2005;17:56–8. [PubMed] [Google Scholar]
- 2.Pelliccia A. Congenital coronary artery anomalies in young patients: New perspectives for timely identification. J Am Coll Cardiol. 2001;37:598–600. doi: 10.1016/s0735-1097(00)01122-0. [DOI] [PubMed] [Google Scholar]
- 3.Angelini P, Walmsley RP, Libreros A, Ott DA. Symptomatic anomalous origination of the left coronary artery from the opposite sinus of valsalva. Clinical presentations, diagnosis, and surgical repair. Tex Heart Inst J. 2006;33:171–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Mavi A, Serçelik A, Ayalp R, Pestemalci T, Batyraliev T, Gümüsburun E. Variants in origin of the left circumflex coronary artery with angiography. Saudi Med J. 2002;23:1390–3. [PubMed] [Google Scholar]
- 5.Datta J, White CS, Gilkeson RC, Meyer CA, Kansal S, Jani ML, et al. Anomalous coronary arteries in adults: Depiction at multi-detector row CT angiography. Radiology. 2005;235:812–8. doi: 10.1148/radiol.2353040314. [DOI] [PubMed] [Google Scholar]
- 6.Shi H, Aschoff AJ, Brambs HJ, Hoffmann MH. Multislice CT imaging of anomalous coronary arteries. Eur Radiol. 2004;14:2172–81. doi: 10.1007/s00330-004-2490-2. [DOI] [PubMed] [Google Scholar]
- 7.Romano S, Morra A, Del Borrello M, Greco P, Daliento L. Multi-slice computed tomography and the detection of anomalies of coronary arteries. J Cardiovasc Med (Hagerstown) 2008;9:187–94. doi: 10.2459/JCM.0b013e32815aa7ef. [DOI] [PubMed] [Google Scholar]
- 8.Sato Y, Inoue F, Matsumoto N, Tani S, Takayama T, Yoda S, et al. Detection of anomalous origins of the coronary artery by means of multislice computed tomography. Circ J. 2005;69:320–4. doi: 10.1253/circj.69.320. [DOI] [PubMed] [Google Scholar]
- 9.Budoff MJ, Ahmed V, Gul KM, Mao SS, Gopal A. Coronary anomalies by cardiac computed tomographic angiography. Clin Cardiol. 2006;29:489–93. doi: 10.1002/clc.4960291104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21:28–40. doi: 10.1002/ccd.1810210110. [DOI] [PubMed] [Google Scholar]
- 11.Chaitman BR, Lespérance J, Saltiel J, Bourassa MG. Clinical, angiographic, and hemodynamic findings in patients with anomalous origin of the coronary arteries. Circulation. 1976;53:122–31. doi: 10.1161/01.cir.53.1.122. [DOI] [PubMed] [Google Scholar]
- 12.Baltaxe HA, Wixson D. The incidence of congenital anomalies of the coronary arteries in the adult population. Radiology. 1977;122:47–52. doi: 10.1148/122.1.47. [DOI] [PubMed] [Google Scholar]
- 13.Donaldson RM, Raphael M, Radley-Smith R, Yacoub MH, Ross DN. Angiographic identification of primary coronary anomalies causing impaired myocardial perfusion. Cathet Cardiovasc Diagn. 1983;9:237–49. doi: 10.1002/ccd.1810090303. [DOI] [PubMed] [Google Scholar]
- 14.Topaz O, DeMarchena EJ, Perin E, Sommer LS, Mallon SM, Chahine RA. Anomalous coronary arteries: Angiographic findings in 80 patients. Int J Cardiol. 1992;34:129–38. doi: 10.1016/0167-5273(92)90148-v. [DOI] [PubMed] [Google Scholar]
- 15.Schmitt R, Froehner S, Brunn J, Wagner M, Brunner H, Cherevatyy O, et al. Congenital anomalies of the coronary arteries: Imaging with contrast-enhanced, multidetector computed tomography. Eur Radiol. 2005;15:1110–21. doi: 10.1007/s00330-005-2707-z. [DOI] [PubMed] [Google Scholar]
- 16.Duran C, Kantarci M, Durur Subasi I, Gulbaran M, Sevimli S, Bayram E, et al. Remarkable anatomic anomalies of coronary arteries and their clinical importance: A multidetector computed tomography angiographic study. J Comput Assist Tomogr. 2006;30:939–48. doi: 10.1097/01.rct.0000230004.38521.8e. [DOI] [PubMed] [Google Scholar]


