Abstract
Background:
Hemoptysis is a significant clinical entity with high morbidity and potential mortality. Both medical management (in terms of resuscitation and bronchoscopic interventions) and surgery have severe limitations in these patients population. Bronchial artery embolization (BAE) represents the first-line treatment for hemoptysis. This article discusses clinical analysis, embolization approach, outcomes and complications of BAE for the treatment of hemoptysis.
Methods:
A retrospective analysis of 344 cases, who underwent bronchial arteriography at Tianjin Haihe Hospital between 2006 and 2013. Several aspects of outcome were analyzed: Demographics, clinical presentation, radiographic studies, results, complications and follow-up of BAE.
Results:
Three hundred and forty-four consecutive patients underwent bronchial arteriography, 336 of 344 patients (97.7%) performed BAE; there were 1530 coils for 920 arteries embolized; the main responsible sources for bleeding were right bronchial artery (29.7%), left bronchial artery (21.6%), combined right and left bronchial trunk (18.4%), right intercostal arteries (13.3%); 61 patients (17.7%) had recurrent hemoptysis within 1 month after undergoing BAE, 74 patients (21.5%) had recurrent hemoptysis over 1 month after undergoing BAE; The common complications of BAE included subintimal dissection, arterial perforation by a guide wire, fever, chest pain, dyspnea, etc. The follow-up was completed in 248 patients, 28 patients had been dead, 21 patients still bleed, 92 patients had lost to follow-up.
Conclusions:
The technique of BAE is a relatively safe and effective method for controlling hemoptysis. The complications of BAE are rare. Although the long-term outcome in some patients is not good, BAE may be the only life-saving treatment option in patients who are poor surgical candidates.
Keywords: Bronchial Artery Embolization, Complications of Bronchial Artery Embolization, Hemoptysis, Recurrent Hemoptysis
INTRODUCTION
Hemoptysis is one of the most common symptoms in patients with respiratory diseases, when massive, has a mortality rate of more than 50%.[1] Therefore, significant or life-threatening hemoptysis calls for quick treatment to stop bleeding. In the past, the control of hemoptysis had been obtained using surgical methods if conservative management failed to be effective. But patients with massive hemoptysis may be associated with high morbidity and mortality using conservative or surgical management. Bronchial artery embolization (BAE) is an established procedure in the emergency management. It is a safe and effective treatment, not only for massive hemoptysis, but also for chronic or recurrent hemoptysis that impairs the patient's quality of life.[2,3] The first procedure for embolization therapy is a complete angiography of the pulmonary vascular tree when bleeding bronchial arteries are seen, embolization therapy is carried out. This retrospective study was undertaken to determine the demographic characteristics, clinical features, results of imaging techniques, complications related to BAE, and follow-up of 344 patients underwent BAE.
METHODS
This study was a retrospective analysis of 344 cases, who underwent bronchial arteriography at Tianjin Haihe Hospital between 2006 and 2013. The patients were hospitalized due to hemoptysis, with the volume of blood ranging 50–2000 ml/24 h. Each patient underwent standard medical management, but the hemoptysis still occurred, so they underwent bronchial arteriography at first and underwent BAE when necessary. There were 186 men and 158 women, with a mean age of 57 years old (ranging 17–83 years old). Two hundred and thirty-four patients had acute and massive hemoptysis, and 110 patients had chronic and recurrent hemoptysis (recurrent rate at least 3 times in 1 year).
The data for outcome analysis were obtained from the clinical records, all of the radiological images were reviewed as possible. We collected such data for analysis: Clinical features; chest computed tomography (CT) scan; bronchial ateriography, BAE, and results; embolization material; complications related to BAE; and follow-up.
This study was approved by the Ethics Committee of Tianjin Haihe Hospital.
RESULTS
The imaging and bronchial arteriography outcomes
A total of 344 patients performed chest CT scanning, which showed all abnormal. About 317 patients (92.2%) were suggestive of causes of hemoptysis, and 27 patients (7.8%) showed focal hemorrhage. Blood lobe could be identified by chest CT scan in 105 cases (30.5%). Bleeding source could be localized in unilateral lung but could not be defined in an exact lobe in 90 cases (36.2%). Both of the lungs had unusual film but not focal hemorrhage in 149 patients (43.3%).
Bronchial arteriography was performed in all patients. All available bronchial arteriograms (which were performed in 344 patients) were reviewed. The findings of angiography suggested that few direct sign found during arteriography, most of the indirect appearances that support a site of bleeding include tortuosity, hypertrophy, hypervascularity, aneurysms, extravasation, and bronchial artery to pulmonary artery or vein shunting. In 131 patients (38.1%), only left-side bronchial arteries were abnormal; in 69 patients, only right-side bronchial arteries were abnormal; in the other 144 patients, bilateral bronchial arteries were abnormal. As the statistics, 944 responsible bronchial arteries involves in according to the angiography: 275 right bronchial arteries; 200 left bronchial arteries; 170 combined right and left bronchial trunk; 123 right intercostal arteries; other 176 arteries [Figure 1]. We analyzed the responsible arteries for tuberculosis, bronchiectasis, bronchogenic carcinomas and undefined reasons as follow [Table 1]. A spinal artery was identified in three patients, one spinal artery originated from the left bronchial artery, one from the right intercostal artery, and one from the right subclavian artery.
Figure 1.
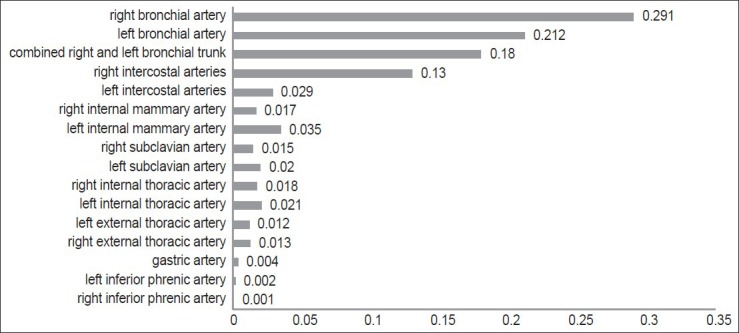
The ratio of responsible bronchial arteries.
Table 1.
The numbers of responsible arteries for different diseases
| Responsible arteries | Tuberculosis | Bronchiectasis | Malignancy | Undifined |
|---|---|---|---|---|
| Right bronchial artery | 153 | 84 | 12 | 15 |
| Left bronchial artery | 111 | 59 | 11 | 11 |
| Combined right and left bronchial trunk | 99 | 47 | 7 | 9 |
| Right intercostal arteries | 66 | 38 | 9 | 5 |
| Left internal mammary artery | 22 | 9 | 2 | 0 |
| Left intercostal arteries | 19 | 7 | 1 | 0 |
| Right internal thoracic artery | 13 | 4 | 0 | 0 |
| Right internal mammary artery | 11 | 4 | 0 | 1 |
| Left subclavian artery | 10 | 9 | 0 | 0 |
| Left internal thoracic artery | 9 | 7 | 4 | 0 |
| Right external thoracic artery | 8 | 3 | 1 | 0 |
| Right subclavian artery | 6 | 6 | 1 | 0 |
| Left external thoracic artery | 5 | 2 | 3 | 0 |
| Right inferior phrenic artery | 1 | 0 | 0 | 0 |
| Gastric artery | 1 | 3 | 0 | 0 |
| Left inferior phrenic artery | 0 | 2 | 0 | 0 |
| Total | 534 | 284 | 51 | 41 |
Despite of which kind of causations, the main responsible arteries were right bronchial artery, left bronchial artery and combined right and left bronchial trunk; more right intercostal arteries were involved than left.
Bronchial artery embolization was performed in 336 of 344 patients (97.7%), artery spasm and closure occurred in six patients, arterial subintimal dissection occurred in one patient, and the responsible vessel couldn’t be super-selective in one patient because of combining with the spinal artery. We used coils and gelatin sponge particles to embolize the arteries. Overall, there were 1530 embolization coils for the 336 patients with a total of 920 arteries embolized (including bronchial and nonbronchial systemic arteries).
The etiologies and outcomes
According to the chest CT scanning and Bronchial arteriography, we concluded the etiologies of the hemoptysis in 344 cases: Tuberculosis in 190 patients (55.2%), bronchiectasis in 99 patients (28.8%), malignancy in 20 patients (5.8%), undefined in 18 patients (5.2%), pneumonia in six patients (1.8%), deformity of bronchial artery in six patients (1.8%), bronchial artery aneurysm in one patients (0.2%), other pulmonary disease in four patients (1.2%).
Bronchial artery embolization was successful in controlling hemoptysis immediately in 330 of 344 patients (96%). 61 patients (17.7%) had recurrent hemoptysis within 1 month after undergoing BAE, only three of them were performed a second BAE, two patients had rebleeding in the previous site, one was found new bleeding area. Three of these patients died of massive hemoptysis in 1 month after undergoing embolization (two patients with bronchogenic carcinoma and one with tuberculosis), one patient with severe chronic obstructive pulmonary disease died of hypercapnia in 3 days after undergoing embolization. The two patients in whom an embolization procedure could not be performed (one because of spinal artery combined with the hemorrhage vessel and one was under subintimal dissection), taken medical treatment for 1 week, the hemoptysis were gradually controlled. Each patient performed BAE had a repeated chest CT scanning after 1 month, which showed that there was no coil dropping or shifting.
Seventy four patients (21.5%) had recurrent hemoptysis over 1 month after undergoing BAE. Hemoptysis in 10 of these patients was resolved spontaneously or controlled by taking medicine. Forty-four patients were performed a repeated embolization, all of the bronchial arteriograms bronchial arteriograms showed there was no dropping of the coil, in 17 patients developed recanalization of the previously embilzed vessels, the remaining 27 patients developed new blood vessels responsible for hemorrhage.
Complications
The complications of BAE included subintimal dissection in one patient. One hundred and seven patients (31.1%) had a fever (<38.5°C) after BAE. Chest pain postprocedure occurred in 65 patients (18.9%), back pain in 51 patients (14.8%), shoulder pain postprocedure in 29 patients (8.4%), and transient dysphagia or lower limb numbness in three patients (0.9%). Five patients (1.5%) developed a groin hematoma at the puncture site.
Follow-up
All of the patients had been followed up over 1 month after BAE except the four patients had been died within 1 month. Two hundred and forty-eight patients had a telephone call follow-up recently (follow-up periods ranging from 6 months to 8 years). It revealed that 28 patients had been dead, six of them died of massive hemorrhage, seven died of deterioration of lung disease but not bleeding, the remainder died of other diseases or accident. Four patients died within 1 year after due to advanced lung cancer (one had a massive bleeding out of controlling), 24 patients died during 2–4 years after BAE. Twenty-one patients have recurrent hemoptysis after repeated BAE, the volume of bleeding is <5 ml/d. Thirteen patients are bleeding due to diffuse bronchiectasis, eight because of pulmonary tuberculosis. One hundred and ninety-nine patients had follow-up periods ranging from 6 months to 8 years without evidence of recurrent hemoptysis. The remaining 92 patients had lost to follow-up.
DISCUSSION
Hemoptysis is a potentially life-threatening occurrence, which requires prompt intervention. Earlier, besides medical treatment, surgery was the fast and best method to control the bleeding. But it required patients many preparations, such as chest CT, pulmonary function, even bronchoscopy to evaluate the patient physical condition and determine the range of surgery.[4,5] Some preparations were impossible for the patients in emergency conditions, the impairment of surgery was so great for a lot of people that gravely lowered the quality of life.[5] BAE is a well-established procedure used to control massive hemoptysis since it first performed in 1974.[1,6,7] Subsequently, BAE was widely used, because non-operable patients could be treated and other patients could be stabilized prior to surgery.[8] In clinical, about 1 hour is needed to prepare before BAE, and the physical requirements of patient are lower than for surgery. The technology is mostly described the outcomes in control of hemoptysis due to varies causations. In some conditions, interventional embolization can be used before surgery.[9]
In our study, bronchial arteriography and embolization were well-tolerated by all patients. Of the 344 cases, an immediate control of bleeding was achieved with embolization in 330 patients (96%), similar to the immediate success rate was reported 75–98% earlier.[10] Recurrent bleeding despite apparently adequate embolotherapy remains a considerable problem, some reported with bleeding occurring in 9–42% of patients after embolization.[11,12,13] In our series, rebleeding occurred within 30 days in 61 of 344 patients (17.7%). A second embolization procedure was performed in three patients, two patients were found rebleeding in the previous points, and one was found new bleeding arteries. Overall the patients, 54 of whom rebleeding over 1 month in the follow-up, 44 of whom were performed a second bronchial arteriography. In 27 patients, an additional bronchial or nonbronchial collateral artery was embolized resulting in the successful control of hemoptysis, 17 patients developed recanalization of the previously embilzed vessels and had been embolizied again. In the recurrent hemoptysis patients, the etiologies were mainly due to cancer, tuberculosis, and severe bronchietasis (at least two lobes were suffered). The disease development contributed to the rebleeding. In our series, a patient with cancer was performed in BAE for three times, and a patient with tuberculosis was performed for five times, both of whom were not suitable for surgery. So it has shown that BAE is an effective procedure with which to definitively treat some patients with hemoptysis and can be repeatedly utilized.
As we know, the source of massive hemoptysis in 90% of cases due to the brochial circulation, as well as the remaining 10% divided equally between the pulmonary circulation (5%) and other systemic arterial supply to the lungs.[6,7,14] It is well-documented that the anatomy of bronchial arteries is variable form person to person, typically origin arises from the descending aorta between the levels of the T5 and T6 vertebrae. Four classic patterns of origin were described:[3,15] Type I (40%): Two on the left and one on the right, presenting as an intercostobronchial trunk (ICBT); type II (21%): One on the left and one ICBT on the right; type III (20%): Two on the left and one on the right (one ICBT and one bronchial artery); type IV (9.7%): One on the left and two on the right (one ICBT and one bronchial artery). According to the statistics, the main responsible vessels for bleeding are right bronchial arteries, left bronchial arteries, combined right and left bronchial trunk, right intercostal arteries. In different etiologies, the rate of abnormal arteries is coincidence with the result. The bronchial arteriography showed that more right intercostal arteries combining with bronchial artery than left. The distribution and frequency of embolization of the arteries were agreed with Kwon et al.[8] Usually, a spinal artery can originate from a bronchial artery in up to 5% of patients, with right side being more common than the left side. As our observation, a spinal artery was identified in three of our patients, with two occurring on the right side and one occurring on the left side.
Significant hemoptysis, chronic and recurrent hemoptysis were the indications for bronchial arteriography. Our result showed that tuberculosis (55.2%), bronchiectasis (28.8%), malignancy (5.8%), undefined (5.2%), pneumonia (1.8%), deformity of bronchial artery (1.8%), bronchial artery aneurysm (0.2%), other pulmonary disease (1.2%). Our patients with bronchogenic carcinomas and tuberculosis were more likely to have recurrent hemoptysis. This finding is similar to that in the series reported by Mal et al.,[13] the etiologies of hemoptysis included tuberculosis (34%), bronchiectasis (26%), aspergilloma (18%), neumoconiosis in coal miners (13%), and bronchogenic carcinoma (3%). Knott-Craig et al. retrospectively studied 120 patients with hemoptysis and found that the right lung was the source in 62% and the left lung in 38%, with the right upper lobe being the area that was most commonly affected.[16] Our results were that the right lung was the source of bleeding in 131 patients (38.1%), the left lung was the source in 69 patients (20.0%), and both lungs were the source in 144 patients (41.8%). The right upper lobe was also more commonly involved in our patients. Our findings are similar with those of several other series.
The common complications of BAE included subintimal dissection, arterial perforation by a guidewire, and reflux of embolic material into the artery without adverse sequelaed during the procedure, and fever, chest pain, dyspnea, Transient dysphagia, groin hematoma, even headache or blindness etc. post-BAE.[17,18] With the technique development, the complications in BAE procedure has been down. Several patients developed transverse myelitis as a result of inadvertent embolization of the spinal arteries. During the procedure of BAE, when a spinal artery was founding, it was usually advised to use superselective BAE to prevent the complication. But in contrast, Mal et al. observed the Brown-Sequard's syndrome,[13,19] following three episodes of spinal cord complications, which regressed after 4 months without sequelae; paraparesis with spontaneous regression after 2 weeks; and complete paraplegia without regression. The complications occurred despite good, selective catheterization of the bronchial artery. If a spinal artery arises from a bronchial artery, we will only embolize the bronchial artery if we can achieve a stable distal position well beyond the spinal artery origin. Our patients showed transistent complications such as fever, chest pain, shoulder pain, groin hematoma, all the symptoms were disappeared in 48 hours, and fewer of our patients experienced any neurologic sequelae.
Anuradha et al.[20] observed the outcome of BAE: The hemoptysis control rate was 93.1% at the end of 2 weeks, 85.7% at the end of 1 month, 79.5% at 90 days, 63.2% at 180 days, 51% at 1 year and 38.7% at the end of 2 years. The follow-up of our patients revealed that 28 patients had died, and six from massive hemorrhage and the remainder as a result of their disease process. Twenty-one patients have recurrent hemoptysis after repeated BAE, the volume of bleeding is <5 ml/d, taking medicine can control the bleeding. One patient suffered recurrent hemoptysis wanted to take a surgical management, but the diffuse disease in lung limited the management. There was no follow-up information available on 92 patients, because they did not return after treatment and the telephone numbers were null. The remaining 199 patients had follow-up periods ranging from 6 months to 8 years without evidence of recurrent hemoptysis.
In summary, hemoptysis represents a significant clinical entity with high morbidity and potential mortality. Medical management (in terms of resuscitation and bronchoscopic interventions) and surgery have severe limitations in these patient populations. BAE procedures represent the first-line treatment for hemoptysis arising from bronchial arterial source. In our study, it was very useful in obtaining immediate bleeding control which was slightly better than that in other report. The technique was a relatively safe and effective method for control the hemoptysis, importantly, it can be used repeatedly. In our study, more than 50% patients had massive hemoptysis, about 70% patients can’t be identified bleeding point by chest CT, 41% patients hemorrhage source from two lungs according the bronchial arteriography. The complications of BAE were rare. Although the long-term outcome in some patients is not good, BAE may be the only life-saving treatment option in patients who are poor surgical candidates.
Footnotes
Edited by: Yuanyuan Ji
Source of Support: This study was supported by a grant of the Science and Technology Foundation of Tianjin Municipal Health Bureau (No. 2011KY14).
Conflict of Interest: None declared.
REFERENCES
- 1.Burke CT, Mauro MA. Bronchial artery embolization. Semin Intervent Radiol. 2004;21:43–8. doi: 10.1055/s-2004-831404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gümüstas S, Akça A, Ciftçi E, Topçu S, Akgül AG. A minimal invasive surgical alternative to aberrant systemic arterial supply: Coil embolization. Interv Med Appl Sci. 2013;5:34–8. doi: 10.1556/IMAS.5.2013.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee S, Chan JW, Chan SC, Chan YH, Kwan TL, Chan MK, et al. Bronchial artery embolisation can be equally safe and effective in the management of chronic recurrent haemoptysis. Hong Kong Med J. 2008;14:14–20. [PubMed] [Google Scholar]
- 4.Al-Refaie RE, Amer S, El-Shabrawy M. Surgical treatment of bronchiectasis: A retrospective observational study of 138 patients. J Thorac Dis. 2013;5:228–33. doi: 10.3978/j.issn.2072-1439.2013.04.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sehitogullari A, Bilici S, Sayir F, Cobanoglu U, Kahraman A. A long-term study assessing the factors influencing survival and morbidity in the surgical management of bronchiectasis. J Cardiothorac Surg. 2011;6:161. doi: 10.1186/1749-8090-6-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lorenz J, Sheth D, Patel J. Bronchial artery embolization. Semin Intervent Radiol. 2012;29:155–60. doi: 10.1055/s-0032-1326923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sidhu M, Wieseler K, Burdick TR, Shaw DW. Bronchial artery embolization for hemoptysis. Semin Intervent Radiol. 2008;25:310–8. doi: 10.1055/s-0028-1085931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kwon W, Kim YJ, Lee YH, Lee WY, Kim MS. The effectiveness of embolotherapy for treatment of hemoptysis in patients with varying severity of tuberculosis by assessment of chest radiography. Yonsei Med J. 2006;47:377–83. doi: 10.3349/ymj.2006.47.3.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cao S, Zhu L, Jin L, Gao J, Chen C. Uterine artery embolization in cesarean scar pregnancy: Safe and effective intervention. Chin Med J (Engl) 2014;127:2322–6. [PubMed] [Google Scholar]
- 10.Barben J, Robertson D, Olinsky A, Ditchfield M. Bronchial artery embolization for hemoptysis in young patients with cystic fibrosis. Radiology. 2002;224:124–30. doi: 10.1148/radiol.2241010654. [DOI] [PubMed] [Google Scholar]
- 11.Zylkowska J, Kurzyna M, Pietura R, Fijalkowska A, Florczyk M, Czajka C, et al. Recurrent hemoptysis: An emerging life-threatening complication in idiopathic pulmonary arterial hypertension. Chest. 2011;139:690–3. doi: 10.1378/chest.10-1134. [DOI] [PubMed] [Google Scholar]
- 12.Swanson KL, Johnson CM, Prakash UB, McKusick MA, Andrews JC, Stanson AW. Bronchial artery embolization: Experience with 54 patients. Chest. 2002;121:789–95. doi: 10.1378/chest.121.3.789. [DOI] [PubMed] [Google Scholar]
- 13.Mal H, Rullon I, Mellot F, Brugière O, Sleiman C, Menu Y, et al. Immediate and long-term results of bronchial artery embolization for life-threatening hemoptysis. Chest. 1999;115:996–1001. doi: 10.1378/chest.115.4.996. [DOI] [PubMed] [Google Scholar]
- 14.Liu FY, Wang MQ, Fan QS, Duan F, Wang ZJ, Song P. Supplementary inferior phrenic artery embolization in the interventional treatment of hemoptysis. Chin Med J. 2009;122:514–20. [PubMed] [Google Scholar]
- 15.Yoon W, Kim JK, Kim YH, Chung TW, Kang HK. Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: A comprehensive review. Radiographics. 2002;22:1395–409. doi: 10.1148/rg.226015180. [DOI] [PubMed] [Google Scholar]
- 16.Knott-Craig CJ, Oostuizen JG, Rossouw G, Joubert JR, Barnard PM. Management and prognosis of massive hemoptysis. Recent experience with 120 patients. J Thorac Cardiovasc Surg. 1993;105:394–7. [PubMed] [Google Scholar]
- 17.Sopko DR, Smith TP. Bronchial artery embolization for hemoptysis. Semin Intervent Radiol. 2011;28:48–62. doi: 10.1055/s-0031-1273940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peng G, Liang H, Ruan L, Luo B. Cortical blindness and ataxia complicating bronchial artery embolization for severe hemoptysis. Intern Med. 2010;49:1445–7. doi: 10.2169/internalmedicine.49.3244. [DOI] [PubMed] [Google Scholar]
- 19.Seon HJ, Song MK, Han JY, Choi IS, Lee SG. Spontaneous cervical epidural hematoma presenting as brown-sequard syndrome following repetitive korean traditional deep bows. Ann Rehabil Med. 2013;37:123–6. doi: 10.5535/arm.2013.37.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anuradha C, Shyamkumar NK, Vinu M, Babu NR, Christopher DJ. Outcomes of bronchial artery embolization for life-threatening hemoptysis due to tuberculosis and post-tuberculosis sequelae. Diagn Interv Radiol. 2012;18:96–101. doi: 10.4261/1305-3825.DIR.3876-11.2. [DOI] [PubMed] [Google Scholar]


