Abstract
Background:
To investigate the surveillance trend of birth defects, incidence, distribution, occurrence regularity, and their relevant factors in Xi’an City in the last 10 years for proposing control measures.
Methods:
The birth defects monitoring data of infants during perinatal period (28 weeks of gestation to 7 days after birth) were collected from obstetrics departments of all hospitals during 2003–2012. Microsoft Excel 2003 was used for data input, and Statistical Package for the Social Sciences version 16.0 (International Business Machines Corporation, New York, NY, USA) was used for descriptive analysis. χ2 test, Spearman correlation and linear-by-linear association trend test were used for statistical analyses.
Results:
The birth defect rate declined from 9.18% in 2003 to 7.00% in 2012 (χ2 = 45.001, P < 0.01) with a mean value of 7.85%, which is below the Chinese national average level (χ2 = 20.451, P < 0.01). The order of five most common birth defects has changed. The incidence of congenital heart disease (CHD) increased with time, particularly after 2012, it became the most frequent type (rs = 0.808, P < 0.001). Till then, the number of neural tube defects (NTDs) declined significantly (χ2 = 76.254, P < 0.01). The average birth defects rate of 8.11% in rural areas was higher than that in urban areas (7.56%, χ2 = 7.919, P < 0.01) and much higher in males (8.28%) than that in females (7.18%, χ2 = 32.397, P < 0.01). Maternal age older than 35 years (χ2 = 35.298, P < 0.01) is the most dangerous age bracket of birth defects than maternal age younger than 20 years (χ2 = 7.128, P < 0.01).
Conclusions:
A downward trend of birth defects was observed in Xi’an City from 2003 to 2012. NTDs significantly decreased after large-scale supplemental folic acid intervention, while the incidence rate of CHD significantly increased.
Keywords: Congenital Abnormalities, Neural Tube Defects, Perinatal Mortality, Quality Control, Statistics
INTRODUCTION
Birth defects refer to the functional or anatomical abnormalities present in the embryo or fetus during gestation, which may be caused by genetic factors and environmental factors or interactions of both of them.[1,2,3]
It is considered as an important indicator of the quality of newborns in a region or a country. In addition to fertility reduction and the development of biopsychosocial medical model, the burden caused by birth defects is increasingly prominent. Based on the World Health Organization estimates, the birth defects rate of 6.42% in the low-income countries is significantly higher than the birth defect rate of 5.57% in the middle-income countries, 5.6% in China and 4.72% in the developed countries.[4,5,6,7] There are 900,000 new cases with birth defects/year in China, and about 250,000 cases were born with obvious manifestations.[8] Birth defects are the main cause of early abortion, stillbirth, perinatal and infant death and birth disability, which is definitely a public issue of population quality and population health. Improving the quality of birth population and increasingly reducing the birth defects draw the attention of the society and government. At present, the hospital monitoring has been used since 2003 in Xi’an City to get the incidence, distribution, impact factors of birth defects in time and to decrease the occurrence. The analysis of the trend of incidence of birth defects is helpful in finding the clues of teratogenic factors and proposing intervention measures in time for preventing the new occurrence of birth defects.[9,10,11,12,13,14,15,16] From the view of development, population-based surveillance has been adopted by more countries and regions.[17,18] In terms of the time period of other countries’ surveillance period, 21% started from the 28th weeks of pregnancy and 75% ended in 28 days after birth in 1994, but only 9.8% and 43% separately in 2003. In other words, the start time move forward and the end time delayed: The whole monitoring period get prolonged in many countries.[4,5,19] Phenylketonuria (PKU) and hypothyroidism were included in Xi’an monitoring and this paper, but the screening result of the metabolic disease has not been included in Chinese National Birth Defect Monitoring because of the information acquisition process and management mode. In this paper, we address the statistics of the incidence and the order of birth defects that occur each year, the efficacy of intervention for neural tube defects (NTDs), the related factors of congenital heart disease (CHD), the screening and detection of PKU and hypothyroidism and the risk factors of birth defects, for example, rural and urban distribution, low birth weight (LBW), premature birth, postmature delivery, gender, maternal age, harmful exposure during early pregnancy, abnormal reproductive history, and family genetic history.
METHODS
Objects
From 2003 to 2012, regardless of household registration, all the infants during perinatal period (28 weeks of gestation to 7 days after birth) who were born in hospitals of Xi’an City, no matter stillbirth or live birth were included in this study. Infants born with innate defects and older than 28 weeks of gestation were required to fill a case card. However, if the gravida was conducted the therapeutic-induced labor at <28 weeks of gestation, the birth defects should be excluded. Born within 7 days with unconfirmed defects would not be reported until a definite diagnosis is made, and so did the early perinatal disease screening, for example, PKU and hypothyroidism.
Monitoring method
Retrospective description and trend analysis were applied based on the monitoring data of birth defects in Xi’an City from 2003 to 2012. Considering the quality of surveillance and the data scientificity, it was ensured that the monitoring operation should cover the entire medical and health institutions with obstetrics departments. Working staffs were gynecological and pediatric or neonatal doctors. Unified training was carried out before and throughout the surveillance every year. According to the data of every single register card, the summary table has to be filled. Once the data pass the hospital audit, they will be reported quarterly. It costs 20 CNY for filling and reporting one card.
Diagnosis criteria of birth defects
The diagnosis of birth defects was based on the Chinese national criteria of birth defects and tiny deformities given in “maternal and child health monitoring manual in China.” The diagnosis involves professionals in Obstetrics Department, Family Planning Department, Pediatrics Department, Pathology Department, Clinical Laboratory, and Physics Diagnostic Division (such as B-ultrasound room). Experts from each monitoring hospital are in charge of confirmation of birth defects and providing technical support for birth defects. In order to ensure detection quality and avoid misdiagnosis, every child with birth defects must be confirmed by the experts from the above-mentioned departments.
The diagnosis of birth defects should be made by county medical establishments or higher level medical institutions and confirmed by the experts. Because of ban on delivery services in Xi’an City, which includes towns, townships, and subdistricts, the situation where diagnosis of birth defects will be made in county-level hospitals does not exist. The diagnosis of birth defects should be confirmed after birth. For example, diagnosis of CHD that cannot be confirmed only by fetal heart beat using B-ultrasound should be confirmed 3 days after birth and then reported. However, the antenatal diagnosis of fatal or major birth defects and chromosome abnormalities should be recorded as confirmed cases.
There are many types of CHDs, including atrial septal defect, ventricular septal defect, aortic translocation, Fallot with pulmonary stenosis, patent ductus arteriosus, and heterotopic heart. The classification is based on the International Classification of Diseases-10. The diagnosis of CHD should be confirmed 3 days after birth to prevent ongoing short-term changes such as patent foramen ovale at birth.
The main methods of diagnosis are based on clinical observation and physical examination. After the birth of an infant, the clinical observation should focus on spirit, complexion, motor function, breathing function, diet, and excretory functions. System physical examination, especially surface inspection, is needed in newborns. The diagnosis of some internal anomalies needs to be considered in combination with laboratory testing, clinical symptoms, evaluation of case history, and clinical manifestations. Assisted examination includes ultrasonic diagnosis, X-ray test, and postmortem and pathological section aiming at stillbirth, dead-birth, and neonatal death.
Monitoring contents
The essential contents were recorded in detail, for example, the situation of baby birth, birth defects diagnoses, the basic information of mother (such as her residence, economy, and education), the history of her illness and drug use during pregnancy, finding out whether she had childbearing before or family history of any disease, and so on. If the type of birth defect falls into one of the 23 common categories, then one needs to tick the space corresponding to the name, otherwise write in detail in the remarks column.
Quality control
All levels of participants of surveillance must set up opinion of quality first and carry out strict quality control on every segment of operation (filling, collection, entry, and analysis).
Hospital–district–city tertiary quality control system
To avoid cases of under-reporting and redundant reports, double-checking is needed and surveillance hospitals should pay attention to misdiagnosis of congenital fetal abnormalities at birth, the child entering the room, physical examination, and bathing. Maternal and Child Health Care Center of the city examines the reports and cards from all surveillance hospitals. Questionable reports or cards should be returned for correction or supplementation. Periodical quality control inspection and examination of surveillance hospitals were administered twice a year at city level and quarterly at district level.
The content of quality control
The content of quality control includes under-reporting investigation, diagnosis checking, and quality checking of monitoring tables (cards).
Under-reporting investigation
Under-reporting investigation consists of missing reports of perinatal fetus and birth defects. Investigation methods of missing reports: Random examinations should be carried out in the selected surveillance hospitals twice a year. The number of missing reports can be obtained from checking the reported tables and cards against the registration of maternity wards. Records of pediatrics ward should be checked, if necessary, to confirm the diagnosis of birth defects.
Diagnosis checking
The birth defects mentioned in this paper not only include the defects after birth but also the abortion defects (28 + weeks and up). All of the defects, including surface and undersurface deformities, should be further confirmed. Abortion caused by defects (28 + weeks and up) is highly restricted in Xi’an City; the discussion and signatures of the experts and clinical indications are required. Moreover, checking examinations focusing on all of the congenital abnormality abortion cases will be carried out by the obstetric experts in annually obstetrical quality examination.
Quality checking of monitoring tables (cards)
The cards are required to be filled correctly, completely, and verified carefully.
Quality requirements: Integrality rate: Filling integrality rate is 100%. Error rates: Filling error rates in tables are <1%. Under-reporting: Under-reporting of perinatal infants is <1% and under-reporting of 23 birth defects is <1%.
Statistical analysis
Microsoft Excel 2003 (Microsoft Corporation, Redmond, WA, USA) was used for data input. Statistical Package for the Social Sciences (International Business Machines Corporation, New York, NY, USA) version 16.0 was used for descriptive analysis. Chi-square test, Spearman correlation, linear-by-linear association trend test, and hierarchical cluster analysis were used for statistical analyses. If the P < 0.05, the difference would be considered as statistically significant.
RESULTS
Incidence of birth defects
Hospital births were maintained high in Xi’an City from 2003 to 2012 [Table 1]. The rate basically reached 100% since it is free for rural parturient to have hospital delivery in 2009.
Table 1.
The incidence of birth defects of perinatal infants in Xi’an city from 2003 to 2012
| Year | Hospital birth rate (%) | Live birth (n) | Perinatal infants (n) | Birth defects (n) | Birth defect rate (%) | Single deformity | Multiple deformities | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Incidence (%) | Proportion rate (%) | n | Incidence (%) | Proportion rate (%) | ||||||
| 2003 | 92.46 | 35,575 | 42,272 | 388 | 9.18 | 307 | 7.26 | 79.12 | 81 | 1.92 | 20.88 |
| 2004 | 93.65 | 36,894 | 48,489 | 417 | 8.60 | 338 | 6.97 | 81.06 | 79 | 1.63 | 18.94 |
| 2005 | 94.45 | 36,423 | 54,827 | 417 | 7.61 | 338 | 6.16 | 81.06 | 79 | 1.44 | 18.94 |
| 2006 | 96.25 | 35,196 | 58,653 | 461 | 7.86 | 397 | 6.77 | 86.12 | 64 | 1.09 | 13.88 |
| 2007 | 96.46 | 38,122 | 80,530 | 596 | 7.40 | 500 | 6.21 | 83.89 | 96 | 1.19 | 16.11 |
| 2008 | 96.84 | 46,348 | 96,547 | 688 | 7.13 | 592 | 6.13 | 86.05 | 96 | 0.99 | 13.95 |
| 2009 | 98.99 | 49,712 | 98,921 | 824 | 8.33 | 690 | 6.98 | 83.74 | 134 | 1.35 | 16.26 |
| 2010 | 99.57 | 59,251 | 106,822 | 917 | 8.58 | 794 | 7.43 | 86.59 | 123 | 1.15 | 13.41 |
| 2011 | 99.57 | 61,158 | 113,974 | 910 | 7.98 | 788 | 6.91 | 86.59 | 122 | 1.07 | 13.41 |
| 2012 | 99.96 | 69,063 | 131,928 | 923 | 7.00 | 807 | 6.12 | 87.43 | 116 | 0.88 | 12.57 |
| Total | 97.12 | 467,742 | 832,963 | 6541 | 7.85 | 5551 | 6.67 | 84.86 | 990 | 1.19 | 15.14 |
A total of 8,32,963 perinatal infants was monitored from 2003 to 2012, including 6541 babies with birth defects, and the average incidence was 7.85%. A linear downward trend of birth defects was observed in the last 10 years based on linear-by-linear association analysis (χ2 = 6.424, P = 0.011). Spearman rank correlation test proved the same result (rs = −0.467, P = 0.174). It declined by 23.75% in 2012 in contrast to 2003 (χ2 = 20.451, P < 0.01). Among 6541 babies with birth defects, there were 5551 (84.86%) newborns with single deformity, and the incidence was 6.67%; 990 (15.14%) of them were born with multiple deformities, and the rate was 1.19% [Table 1].
The types and the order of birth defects
The order of six most common birth defects has changed a lot since 2003. In 2003, the top one was NTDs, followed by polydactylism, congenital hydrocephalus, cleft lip with cleft palate, simple cleft lip, and CHD. However, the first place was taken by CHD, followed by polydactylism, congenital hydrocephalus, cleft lip with cleft palate, NTDs, and simple cleft lip in 2012.
Neural tube defects
Before 2003, NTDs were the most common birth defects, including rachischisis, anencephalia, and encephalocele. In 2003, the incidence of NTDs was 26.26/10,000 and decreased gradually (χ2 = 76.254, P < 0.01). It declined by 65.78% till 2012 with an average annual rate of 6.58%. Free folic acid was given from preconception until the end of first trimester to prevent NTDs from the fourth quarter in 2009. The difference in the incidence was significant before and after the intervention in this study (χ2 = 39.272, P < 0.001). This is probably due to the benefits obtained from the dual function of the improvement of antenatal sonographic diagnosis and the folic acid supplement. A total of 1135 NTDs was diagnosed in the past decade and 21.06% of them suffered from anencephalia, 57.44% of them got rachischisis, and 21.50% of them were born with encephalocele.
Congenital heart disease
The incidence of CHD increased with time, particularly after 2012, it became the most frequent type (rs = 0.808, P < 0.001). It increased from 3.79/10,000 in 2003 to 11.67/10,000 in 2012 (χ2 = 136.29, P < 0.01). The prevalence of CHD in urban areas each year was proved higher than that in rural areas by Wilcoxon Matched-Pairs Rank Test (Z = 2.805, P = 0.005). However, the difference between urban and rural areas did not make any significant difference on the incidence of CHD except 2005 and 2010. The incidence of CHD in the perinatal period increased year by year, which significantly correlated with LBW in 2004 and 2007–2012 [P < 0.001; Table 2].
Table 2.
The proportions of incidences and relative factors of CHD in Xi’an city from 2003 to 2012
| Year | Urban | Rural | χ2 | P | Contingency coefficient | CHD with LBW | CHD with normal birth weight | χ2 | P | Contingency coefficient | Prenatal diagnosis (n) | Postpartum diagnosis (n) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Incidence (%) | n | Incidence (%) | n | Incidence (%) | n | Incidence (%) | |||||||||
| 2003 | 11 | 0.49 | 5 | 0.28 | 1.50 | 0.220 | 0.0060 | 2 | 1.98 | 14 | 0.34 | 3.35 | 0.067 | 0.0129 | 3 | 13 |
| 2004 | 8 | 0.32 | 5 | 0.25 | 0.39 | 0.534 | 0.0028 | 4 | 3.60 | 9 | 0.19 | 35.11 | <0.001 | 0.0311 | 4 | 9 |
| 2005 | 11 | 0.41 | 3 | 0.12 | 4.52 | 0.033 | 0.0091 | 2 | 1.40 | 12 | 0.22 | 3.62 | 0.057 | 0.0117 | 4 | 10 |
| 2006 | 17 | 0.59 | 13 | 0.48 | 0.66 | 0.415 | 0.0034 | 3 | 1.74 | 27 | 0.47 | 3.06 | 0.080 | 0.0095 | 5 | 25 |
| 2007 | 22 | 0.55 | 16 | 0.43 | 1.03 | 0.310 | 0.0036 | 13 | 6.61 | 25 | 0.32 | 146.84 | <0.001 | 0.0445 | 12 | 26 |
| 2008 | 19 | 0.41 | 17 | 0.37 | 0.28 | 0.594 | 0.0017 | 10 | 4.48 | 26 | 0.28 | 91.95 | <0.001 | 0.0326 | 13 | 23 |
| 2009 | 32 | 0.76 | 28 | 0.51 | 2.74 | 0.098 | 0.0053 | 19 | 8.60 | 41 | 0.42 | 222.80 | <0.001 | 0.0488 | 24 | 36 |
| 2010 | 73 | 1.52 | 51 | 0.88 | 9.76 | 0.002 | 0.0096 | 48 | 19.46 | 76 | 0.73 | 698.88 | <0.001 | 0.0815 | 59 | 65 |
| 2011 | 40 | 0.83 | 47 | 0.73 | 0.45 | 0.503 | 0.0020 | 42 | 18.77 | 45 | 0.40 | 928.32 | <0.001 | 0.0910 | 56 | 31 |
| 2012 | 79 | 1.30 | 75 | 1.05 | 1.75 | 0.185 | 0.0036 | 69 | 29.68 | 85 | 0.66 | 1577.23 | <0.001 | 0.1094 | 76 | 78 |
| Total | 312 | 0.80 | 260 | 0.62 | 13.45 | <0.001 | 0.0040 | 212 | 1133 | 360 | 0.44 | 3122.86 | <0.001 | 0.0611 | 256 | 316 |
CHD: Congenital heart disease; LBW: Low birth weight.
Other types of birth defects
In 2003, the incidence of congenital hydrocephalus was 10.17/10,000 and decreased gradually to 6.90/10,000 in 2012 (χ2 = 76.175, P < 0.001). Cleft lip with cleft palate decreased from 9.94/10,000 in 2003 to 5.23/10,000 in 2012 (χ2 = 32.658, P < 0.05). The occurrences of proctatresia and hypospadias rose up year by year. PKU and hypothyroidism were two metabolic diseases for neonatal screening in Xi’an City from 2003 to 2012. The screening rate of PKU and hypothyroidism increased from 4.89% in 2003 to 77% in 2012. In the last 10 years, 265 PKU patients were diagnosed (the phenylalanine level ≥2 mg/dl) with the average incidence rate of 5.56/10,000. One hundred and fifty six hypothyroidism patients were diagnosed (the thyroid-stimulating hormone level ≥10 uU/ml) with the average incidence rate of 3.39/10,000.
Risk factors of birth defects
Regional and body weight distribution of birth defects and the situation of prenatal diagnosis
In general, the incidence of birth defects was higher in rural areas (average 8.11%) than that in urban areas (average 7.56%; χ2 = 7.919, P < 0.01) and correlated with LBW (P < 0.001) from 2003 to 2012 [Table 3].
Table 3.
The incidences of birth defects in rural and urban areas and the proportions of relative factors in Xi’an city from 2003 To 2012
| Year | Perinatals (n) | Urban | Rural | Birth defects with LBW | Birth defects with normal birth weight | χ2 | P | Contingency coefficient | Prenatal diagnosis (n) | Postpartum diagnosis (n) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Urban | Rural | n | Incidence (%) | n | Incidence (%) | n | Incidence (%) | n | Incidence (%) | ||||||
| 2003 | 22,601 | 19,671 | 183 | 8.10 | 205 | 10.42 | 124 | 12.30 | 264 | 0.64 | 1471.42 | <0.001 | 0.1834 | 127 | 261 |
| 2004 | 25,659 | 22,830 | 200 | 7.79 | 217 | 9.51 | 117 | 10.53 | 299 | 0.63 | 1247.35 | <0.001 | 0.1584 | 115 | 302 |
| 2005 | 27,497 | 27,330 | 170 | 6.18 | 247 | 9.04 | 97 | 6.78 | 310 | 5.99 | 705.61 | <0.001 | 0.1127 | 121 | 296 |
| 2006 | 28,873 | 29,780 | 207 | 7.17 | 254 | 8.53 | 132 | 7.67 | 329 | 0.58 | 1076.73 | <0.001 | 0.1343 | 136 | 325 |
| 2007 | 39,994 | 40,536 | 281 | 7.03 | 315 | 7.77 | 155 | 7.88 | 454 | 0.56 | 1398.32 | <0.001 | 0.1306 | 169 | 427 |
| 2008 | 46,674 | 49,873 | 309 | 6.62 | 379 | 7.60 | 202 | 9.05 | 486 | 0.52 | 2243.70 | <0.001 | 0.1507 | 208 | 480 |
| 2009 | 42,301 | 56,620 | 344 | 8.13 | 480 | 8.48 | 234 | 10.59 | 590 | 0.61 | 2604.21 | <0.001 | 0.1602 | 264 | 560 |
| 2010 | 47,968 | 58,854 | 444 | 9.26 | 473 | 8.04 | 272 | 11.03 | 645 | 0.62 | 3067.23 | <0.001 | 0.1671 | 313 | 604 |
| 2011 | 48,360 | 65,614 | 384 | 7.94 | 526 | 8.02 | 298 | 13.32 | 612 | 0.55 | 4515.66 | <0.001 | 0.1952 | 366 | 544 |
| Total | 39,0583 | 442,380 | 2954 | 7.56 | 3587 | 8.11 | 1944 | 10.39 | 4599 | 0.57 | 22660.94 | <0.001 | 0.1627 | 2200 | 4341 |
LBW: Low birth weight.
Premature or postmature delivery and birth defects
Premature delivery (<37 weeks) was observed to be another significant risk factor of birth defects during 2003–2012 (P < 0.001), and for postmature delivery (longer than 42 weeks), it was only significant during 2005–2006, 2008–2009, and 2011–2012 [Table 4].
Table 4.
Delivery time and birth defects during 2003 - 2012 in Xi’an city
| Year | Premature delivery with birth defects | Postmature delivery with birth defects | Normal delivery with birth defects | Premature delivery andnormal delivery | Postmature delivery andnormal delivery | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Incidence (%) | n | Incidence (%) | n | Incidence (%) | χ2 | P | Contingency coefficient | χ2 | P | Contingency coefficient | |
| 2003 | 119 | 9.57 | 9 | 1.25 | 260 | 0.65 | 1062.62 | <0.001 | 0.1579 | 3.12* | 0.078 | 0.0099 |
| 2004 | 108 | 7.87 | 6 | 0.78 | 303 | 0.65 | 813.01 | <0.001 | 0.1294 | 0.18 | 0.674 | 0.0019 |
| 2005 | 105 | 4.32 | 17 | 1.80 | 295 | 0.57 | 442.06 | <0.001 | 0.0902 | 23.65 | <0.001 | 0.0212 |
| 2006 | 127 | 6.83 | 14 | 1.44 | 320 | 0.57 | 916.39 | <0.001 | 0.1251 | 12.29 | <0.001 | 0.0147 |
| 2007 | 135 | 5.54 | 11 | 0.83 | 450 | 0.59 | 790.49 | <0.001 | 0.0994 | 1.31 | 0.252 | 0.0041 |
| 2008 | 196 | 7.42 | 27 | 2.07 | 465 | 0.50 | 1783.73 | <0.001 | 0.1356 | 60.61 | <0.001 | 0.0254 |
| 2009 | 220 | 7.27 | 20 | 1.46 | 584 | 0.62 | 1586.33 | <0.001 | 0.1265 | 15.41 | <0.001 | 0.0127 |
| 2010 | 281 | 7.88 | 13 | 0.91 | 623 | 0.61 | 2138.73 | <0.001 | 0.1410 | 2.02 | 0.155 | 0.0044 |
| 2011 | 314 | 7.97 | 18 | 1.56 | 578 | 0.53 | 2682.34 | <0.001 | 0.1524 | 22.40 | <0.001 | 0.0143 |
| 2012 | 342 | 6.86 | 16 | 1.93 | 565 | 0.45 | 2867.40 | <0.001 | 0.1463 | 36.52* | <0.001 | 0.0177 |
| Total | 1947 | 7.08 | 151 | 1.40 | 4443 | 0.56 | 14649.84 | <0.001 | 0.1323 | 131.69 | <0.001 | 0.0128 |
*Corrected for expected number <5.
Gender distribution of birth defects
The average incidence of birth defects in males was 8.28% and significantly higher than 7.18% in females (χ2 = 32.397, P < 0.01). The differences between males and females were significant in 2005 (males: 8.4%; females: 6.7%), 2006 (males: 8.72%; females: 6.82%), 2007 (males: 7.98%; females: 6.54%), and 2010 (males: 9.3%; females: 7.48%).
The differences in birth defects among the different age groups of pregnant women
Nonparametric test for paired design reflected that the incidence of birth defects was significantly different in different age groups of puerperae (χ2 = 26.960, P < 0.001). The relatively safest age group was 25–29 years (χ2 = 21.689, P < 0.01), while it was more dangerous if the pregnant women was > 35 years (χ2 = 35.298, P < 0.01) or < 20 years (χ2 = 7.128, P < 0.01).
Risk factors in the first trimester
About 17% of puerperae along with their babies born with defects had been exposed to different harmful factors during early pregnancy. During pregnancy period, 11.71% of puerperae along with their babies born with defects were ill, 2.84% were suffering from viral infection, 9.66% used medication during pregnancy, and 3.41% had contact with harmful substances.
Reproductive history of puerperae
There were 317, namely 4.85% of puerperae had abnormal reproductive history, including 1.30% of stillbirth, 2.77% of spontaneous abortion, and 1.28% of birth defects.
Family history of puerperae
There were 82, namely 1.25% of newborns with birth defects had family history.
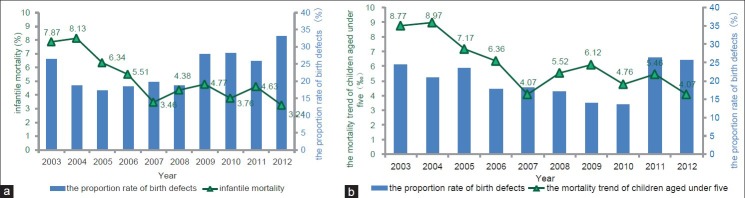
Relationship between birth defects and perinatal deaths
A total of 3650 perinatal deaths was registered during 2003–2012 with a mortality of 4.38%, which significantly declined from 8.63% in 2003 to 4.15% in 2012. With a rank correlation coefficient of –0.952 (P < 0.001), the perinatal mortality went down by time. The perinatal mortality caused by birth defects is 65.77 times the rate due to nonbirth defects, which accounted for 34.35% of perinatal deaths in the same period. The average proportion rate of infantile deaths caused by birth defects was 23.43%, and the average mortality of children aged under 5 years due to birth defects was 20.13% [Figure 1].
Figure 1.
The trend of infantile (a) and children aged under 5 years (b) mortality and the proportion rate of birth defects during 2003–2012. The bars represent the proportion rate of deaths caused by birth defects, and the line represents the mortality trend changing with time.
Hierarchical cluster analysis
Hierarchical cluster analysis is used to cluster common deformities of 13 counties and districts during 2003–2012. Five groups can be clustered subsequently as follows:
Group 1: Beilin District: CHD incidence is the highest one, especially in 2010 and 2012.
Group 2: Lantian County: NTDs incidence is the highest in Lantian County, especially in 2003, 2004, and 2007.
Group 3: Baqiao District, Gaoling County, and Yanliang District: Many kinds of deformity incidence are higher.
Group 4: Consisted of Hu County and Zhouzhi County, and the rest of the districts and counties (Yanta District/Xincheng District/Lianhu District/Weiyang District/Lintong District/Changan District) are classified as Group 5 in which all kinds of deformity incidence are low [Figure 2].
Figure 2.
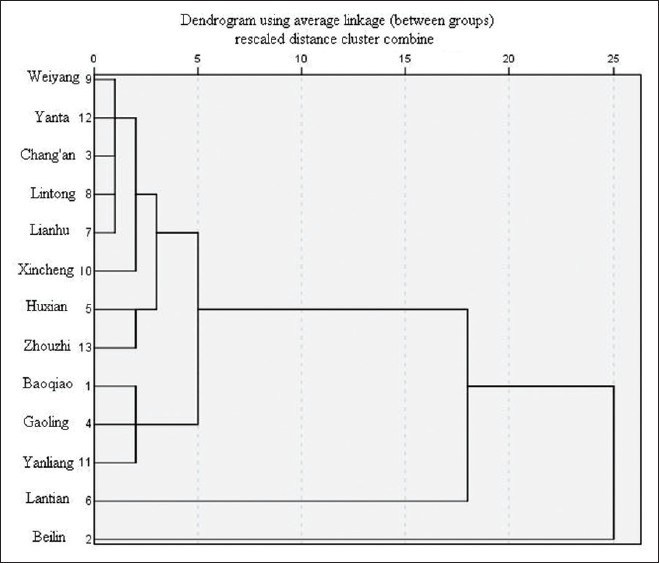
Hierarchical cluster analysis of cumulative incidence of common birth defects in 13 counties and districts during 2003–2012.
DISCUSSION
A total of 8,32,963 perinatal infants was monitored and diagnosed during 2003–2012, including 6541 babies with birth defects, in Xi’an City with an average incidence of 7.85%; a slow downward trend was observed; and the City benefited from the effective measurements performed in the last 10 years. Although single deformity was the most common defect, which constituted 84.86% of all, an imbalance in technology to diagnose syndrome and/or cascading symptoms could still be possible. Birth defects had been known as the first cause of perinatal deaths in Xi’an City. The incidence of birth defects in rural areas was significantly higher than that in urban areas from 2003 to 2009, but this difference changed smaller during 2009–2012 along with the reduction of the gaps such as economy. Birth defects were significantly correlated with premature delivery and LBW always, but only some years had relationship with postmature delivery. The birth defects rate for males was significantly higher than the females. 25–29 years were the safest age group, while puerperae in >35 or <20 age groups tend to have babies born with deformities. The results are consistent with the analysis published in Applied Journal of General Practice in 2009.[20]
Regarding the order of birth defects, NTDs were at the top during 2003–2008, but the CHD had climbed up since 2010 and took the first place in 2012. Meanwhile, the order of birth defects in Xi’an City was consistent with the Chinese national data, namely CHD, polydactylism, cleft lip, NTDs, and hydrocephalus.
The average incidence of NTDs was 1.36%. Fortunately, it decreased from 2.63% in 2003 to 0.90% with a total decline of 65.78%. The nationwide incidence of perinatal NTDs decreased from 2.74% in 1987 to 0.45% in 2011; the trend in Xi’an City was quite consistent with it. The results are in good agreement with the corresponding results in the literature.[21] This defect is one of the preventable deformities. Free folic acid was given from preconception until the end of first trimester to prevent NTDs from the fourth quarter in 2009. The difference in the incidence was significant before and after the intervention in this study (χ2 = 39.272, P < 0.001). Therefore, the drop in NTDs demonstrated the preventive effect of oral folic acid supplement in the early stage of pregnancy. Cluster analysis found that the NTDs cumulative incidence in Lantian County was at a significantly higher level compared with the rest of other districts and counties. The work on supplement of folic acid and nutrition education for pregnant women should be further strengthened in Lantian County.
Congenital heart disease refers to anatomical problems resulting from dyspoiesis or dysplasia of heart and great vessels or cases in which the channels fail to close which is normal for fetus. With a mean value of 0.69%, the incidence of CHD rose from 0.38% in 2003 to 1.17% in 2012. However, CHD was not always relevant to LBW, and the incidence also significantly varied between urban areas and rural areas (χ2 = 13.449, P < 0.001). The studies abroad have suggested that the difference between occurrence of atrial septal defect of fetus or infant between the city and the countryside probably related to the use of chemicals in the countryside.[22] Two possibilities were considered as reasons for increasing incidence of the disease: (1) Prenatal diagnostic level has been enhancing gradually; the percentage of performing this technology climbed from 18.75% in 2003 to 49.35% in 2012, and consequently more diagnoses led to higher positive rate and (2) the monitoring level in the whole city has been increasing with time and the result getting closer and closer to reality. According to the national report, the general incidence of CHD was 0.5–1.25% of the population, and it was approximately 0.8% in America. However, there were no data showing its occurrence during perinatal period. It is more often seen in urban areas than in rural areas, and along with it, the proportion of LBW and prenatal diagnoses increased year by year. Cluster analysis found that the CHD incidence was at a significantly higher level compared with the rest of other districts and counties in Beilin District, and it needs further investigation and analysis to clarify.
The incidence of congenital hydrocephalus and cleft lip with cleft palate decreased significantly from 2003 to 2012. The incidence of proctatresia and hypospadias has been increasing all these years, which deserves further research. Some scholars proposed that it may be related to environmental parahormone pollution in recent years. All of these pollutants were detected with some estrogen-like activity after degrading to a certain extent. If the fetus is impacted by such materials in early pregnancy stage, it could lead to gender differentiation disorders.
Phenylketonuria and hypothyroidism are rarely involved in monitoring schedules. During 2009–2011, the national incidences of PKU were 0.073%, 0.076%, and 0.072%, respectively. Meanwhile, they were 0.701%, 0.43%, and 0.819% in Xi’an City, which marked higher than the former. During the same period, the national incidences of hypothyroidism were 0.49%, 0.463%, and 0.475%, while they were 0.448%, 0.329%, and 0.48% in Xi’an City.[7,23]
Birth defects are mainly caused by genetic and environmental factors.[24] It was found that 4.85% of puerperae mothering babies with birth defects had abnormal reproductive history, 2.77% of them had spontaneous abortion history, and 1.25% of them had family history. Therefore, prenatal care is particularly important as well as health care, guidance and consultation during pregnancy. Early pregnancy stage is critical for development of fetal organs, but it is also the most sensitive and vulnerable phase for fertilized egg to get exposed to teratogenic factors. Unfortunately, 17% of puerperae mothering defective babies were exposed to illness, viral infection, drug use, radiation, pesticides, and other harmful substances in the early pregnancy. Consequently, it is very important to prevent and reduce birth defects by enhancing early pregnancy health guidance, for example, nutrition, medication, disease prevention, and avoiding teratogenic factors.
Among 6541 birth defects, 2073 of them, namely 31.69% have been diagnosed by B ultrasound. Through the surveillance, most defective infants with mainly surface birth defects can be discovered in time, but there are still many shortages for finding the metabolic, functional, and delayed deformities.
Based on the hospital monitoring results, the perinatal mortality was 4.38%. It decreased gradually from 8.63% in 2003 to 4.15% in 2012. The perinatal mortality caused by birth defects is 65.77 times the rate due to nonbirth defects, which accounted for 34.35% of perinatal deaths in the same period, which is consistent with the viewpoint of Li Dai that nearly a quarter of perinatal deaths is due to birth defects.[25] The average proportion rate of infantile deaths caused by birth defects was 23.43%, and the average mortality of children aged under 5 years due to birth defects was 20.13%. In the developed country, it is known that defects are the prime factors of perinatal deaths,[7,26,27] so it was like in the coastal area of China.[28] Besides, birth asphyxia, premature delivery with LBW, and neonatal pneumonia are the main reasons for a large proportion of perinatal deaths in the poor and less developed Northwest China. It indicates that the improvement of medical technology is crucial, especially the diagnoses and treatment levels at obstetrics and neonatal departments in these areas.
The combination of hospital and crowd monitoring is conducive to comprehensively understand the occurrence and outcome of birth defects. It is also important to use new diagnosis technology, strengthen training, and prolong the surveillance time to 1 year after birth in order to fortify the comparability with other countries and regions and reduce the cases failed to report. To sum up, strengthening the preventive care measures from primary preconception and early pregnancy care, comprehensive prenatal screening, and prenatal diagnosis could effectively decrease the occurrence of birth defects and the perinatal mortality rate.
ACKNOWLEDGMENTS
We gratefully acknowledge all the members involved in the work of Xi’an birth defects surveillance. Also, we thank Hui Song, Xingrong Zheng, Yujie Ning, and Guoyan Ma for their help.
Footnotes
Edited by: Yuanyuan Ji
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Wang FL. Beijing: Publishing Company of Peking Union Medical College and Peking University Health Science Center; 1998. Atlas of Congenital Malformations-Birth Defects Monitored in China. [Google Scholar]
- 2.Yang SQ. Cheng Du: Sichuan Science and Technology Press; 1998. Yang SQ. The monitoring method and seasonal analysis of birth defects. [Google Scholar]
- 3.Zheng W, Fang JQ. Case-control study on influencing factors of birth defects. Pract Prev Med. 2009;16:679–82. [Google Scholar]
- 4.ICBDMS. Roma: ICBDMS; 2002. International Clearinghouse for Birth Defects Monitoring Systems – Annual Report 2002. [Google Scholar]
- 5.ICBDMS. Roma: ICBDMS; 2003. International Clearinghouse for Birth Defects Monitoring Systems – Annual Report 2003. [Google Scholar]
- 6.Roma: ICBDMS; 2007. ICBDMS. International Clearinghouse for Birth Defects Monitoring Systems – Annual Report 2007. [Google Scholar]
- 7.Rosano A, Botto LD, Botting B, Mastroiacovo P. Infant mortality and congenital anomalies from 1950 to 1994: An international perspective. J Epidemiol Community Health. 2000;54:660–6. doi: 10.1136/jech.54.9.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dai L, Zhu J, Liang J, Wang YP, Wang H, Mao M. Birth defects surveillance in China. World J Pediatr. 2011;7:302–10. doi: 10.1007/s12519-011-0326-0. [DOI] [PubMed] [Google Scholar]
- 9.Atlanta, GA: National Birth Defects Prevention Network, Inc; 2004. [Accessed June, 2004 at]. National Birth Defects Prevention Network. Guidelines for Conducting Birth Defects Surveillance. http://www.nbdpn.org/docs/NBDPN_Guidelines2008.pdf . [Google Scholar]
- 10.ICBDMS. Roma: ICBDMS; 2008. International Clearinghouse for Birth Defects Monitoring Systems – Annual Report 2008. [Google Scholar]
- 11.Dolk H. EUROCAT: 25 years of European surveillance of congenital anomalies. Arch Dis Child Fetal Neonatal Ed. 2005;90:355–8. doi: 10.1136/adc.2004.062810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lowry RB, Thunem NY, Anderson-Redick S. Alberta Congenital Anomalies Surveillance System. CMAJ. 1989;141:1155–9. [PMC free article] [PubMed] [Google Scholar]
- 13.Edmonds LD, Layde PM, James LM, Flynt JW, Erickson JD, Oakley GP., Jr Congenital malformations surveillance: Two American systems. Int J Epidemiol. 1981;10:247–52. doi: 10.1093/ije/10.3.247. [DOI] [PubMed] [Google Scholar]
- 14.Misra T, Dattani N, Majeed A. Congenital anomaly surveillance in England and Wales. Public Health. 2006;120:256–64. doi: 10.1016/j.puhe.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 15.Zhu J. The discussion on experience of managing national maternal and child health surveillance program (in Chinese) Chin J Med Sci Res Manag. 2002;15:144–6. [Google Scholar]
- 16.Annas GJ, Elias S. Thalidomide and the Titanic: Reconstructing the technology tragedies of the twentieth century. Am J Public Health. 1999;89:98–101. doi: 10.2105/ajph.89.1.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li S, Hong S, Wang T. A population-based surveillance system on birth defects and its application (in Chinese) Chin J Epidemiol. 2001;22:172–5. [PubMed] [Google Scholar]
- 18.Li S, Moore CA, Li Z, Berry RJ, Gindler J, Hong SX. A population-based birth defects surveillance system in the People's Republic of China. Paediatr Perinat Epidemiol. 2003;17:287–93. doi: 10.1046/j.1365-3016.2003.00478.x. [DOI] [PubMed] [Google Scholar]
- 19.Christianson A, Howson CP, Modell B. White Plains, New York: March of Dimes Foundation; 2006. Relationship between birth defect and maternal age, occupation, level of education. March or Dimes Global Report on Birth Defects. [Google Scholar]
- 20.Guan Li, Yun W, Chen XQ, Yang L. Relationship between birth defect and maternal age, occupation, level of education. Appl J Gen Pract. 2009;7:981–2. [Google Scholar]
- 21.Oakley GP., Jr The scientific basis for eliminating folic acid-preventable spina bifida: A modern miracle from epidemiology. Ann Epidemiol. 2009;19:226–30. doi: 10.1016/j.annepidem.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 22.Langlois PH, Scheuerle A, Horel SA, Carozza SE. Urban versus rural residence and occurrence of septal heart defects in Texas. Birth Defects Res A Clin Mol Teratol. 2009;85:764–72. doi: 10.1002/bdra.20586. [DOI] [PubMed] [Google Scholar]
- 23.Ministry of Health of China; 2011. Report on Women and Children's Health Development in China. [Google Scholar]
- 24.ICBDSR. Annual Report 2010. Roma, Italy: ICBDSR; 2010. The Center of the International Clearinghouse for Birth Defects Surveillance and Research. [Google Scholar]
- 25.Dai L, Zhou GX, Zhu J, Miao L, Wang YP, Wu YQ, et al. Impacts of birth defects on perinatal deaths in Chinese population (in Chinese) Chin J Epidemiol. 2004;25:138–41. [PubMed] [Google Scholar]
- 26.Kalter H. Five-decade international trends in the relation of perinatal mortality and congenital malformations: Stillbirth and neonatal death compared. Int J Epidemiol. 1991;20:173–9. doi: 10.1093/ije/20.1.173. [DOI] [PubMed] [Google Scholar]
- 27.Lee K, Khoshnood B, Chen L, Wall SN, Cromie WJ, Mittendorf RL. Infant mortality from congenital malformations in the United States, 1970-1997. Obstet Gynecol. 2001;98:620–7. doi: 10.1016/s0029-7844(01)01507-1. [DOI] [PubMed] [Google Scholar]
- 28.He CH, Wang YP, Zhu J, Liang J, Dai L, Miao L. Mortality from congenital malformations in children under 5 years old in China, 1996-2006 (in Chinese) J Sichuan Univ (Med Sci Ed) 2010;41:324–8. [PubMed] [Google Scholar]