Abstract
Background:
It has rarely been reported about the changes of hemoglobin (Hb) and hematocrit (Hct) in elderly patients receiving total knee arthroplasty (TKA) or total hip arthroplasty (THA). This study aimed to evaluate the changes of Hb and Hct after TKA or THA in elderly patients, and analyze its relationship with sex and type of arthroplasty.
Methods:
This is a prospective cohort study, including 107 patients receiving TKA or THA without allogeneic blood transfusion. There were 54 males and 53 females, with a mean age of 69.42 years. Levels of Hb and Hct were examined preoperatively and during the 6 months follow-up after operation.
Results:
Levels of Hb and Hct decreased postoperatively and reached their minimum points on postoperative day 4. Thereafter, Hb and Hct recovered to their preoperative levels within 6–12 weeks. No significant differences in the levels of Hb and Hct were noticed between different sexes. THA patients showed significantly greater drop in Hb and Hct than TKA patients in the first 4 days postoperatively (P < 0.05).
Conclusions:
Levels of Hb and Hct decreased during the first 4 days after arthroplasty and gradually returned to their normal levels within 6–12 weeks postoperatively. THA may be associated with higher postoperative blood loss than TKA.
Keywords: Arthroplasty, Hemoglobin, Hip, Knee
INTRODUCTION
Lower limb total joint arthroplasty (TJA) consists of total hip arthroplasty (THA) and total knee arthroplasty (TKA), which are the most commonly performed orthopedic procedures for end-stage joint diseases. The techniques of arthroplasty have been perfected. Current research of arthroplasty is focused on tourniquet, the drainage tube, autologous blood doping and application of tranexamic acid or other drugs. However, changes of hemoglobin (Hb) and hematocrit (Hct) in the perioperative period of TJA have rarely been reported.
The trauma of TKA and THA can cause serious stress response and severe loss of Hb. Intraoperative hemorrhage, postoperative concealed hemorrhage, and stress response can decrease Hb levels by 30 g/L,[1,2] which may explain the high rate of allogeneic blood transfusion in TJA.[3] Blood transfusion could lead to longer hospital stay, higher incidence of complication, transfusion reaction and infection. Meanwhile, the majority of patients receiving TJA were the aged people, especially in China.[4]
This study aimed to investigate the perioperative blood variation in aged patients receiving TKA/THA without allogeneic blood transfusion. We attempted to find the changing patterns of Hb and Hct after TKA or THA and assess the influence of sex and type of surgery.
METHODS
Patients
This was a prospective cohort study performed at the Joint Division of our hospital from September 2012 to February 2013. The inclusion criteria were: Age over 60 years; planning to undergo THA or TKA; preoperative Hb >120 g/L in men and >110 g/L in women; preoperative Hct >0.4. Patients with the following conditions were excluded from this study: Receiving allogeneic blood transfusion during surgery; history of rheumatism; iron deficiency; hematinic deficiency; polycythemia; ankylosing spondylitis. This study was approved by the Ethics Committee of our hospital. Informed consent was taken from the patients.
Initially, 120 patients were included in this prospective research. Eight patients were lost to follow-up. One patient was excluded for blood diseases, and four patients were excluded for rheumatoid arthritis. Finally, 107 patients were included in the analysis.
Data collection
Levels of Hb and Hct were examined preoperatively (within 1 week before surgery), immediately after surgery and on postoperative day 1–7. Patients were followed up by clinic visit at 3 weeks, 6 weeks, 3 months and 6 months after surgery. Blood test was performed to examine the levels of Hb and Hct.
Statistical analysis
Data were presented in mean ± standard deviation. The differences between groups were analyzed using Student's t-test Per. All P values were bilateral and was considered as statistically significant when P < 0.05. The statistical analysis was performed with Graphpad Prism 6.0 (Prism, US).
RESULTS
Basic information
A total of 107 patients were finally included in the analysis. There were 54 males and 53 females, with a mean age of 69.42 years. THA was performed in 54 patients and TKA in 53 patients. The baseline data of Hb and Hct did not differ significantly between THA and TKA patients, or between male and female patients [Tables 1 and 2]. No significant complications occurred perioperatively or during the follow-up. None of the patients received other surgeries during the follow-up.
Table 1.
Baseline data of THA and TKA patients (mean ± SD)
| Items | THA (n = 54) | TKA (n = 53) | P |
|---|---|---|---|
| Preoperative Hb | 136.7 ± 12.4 | 136.7 ± 12.4 | 0.986 |
| Preoperative Hct | 42.7 ± 4.2 | 42.9 ± 4.0 | 0.877 |
TKA: Total knee arthroplasty; THA: Total hip arthroplasty; SD: Standard deviation; Hb: Hemoglobin; HCT: Hematocrit.
Table 2.
Baseline data of male and female patients (mean ± SD)
| Items | Male (n = 54) | Female (n = 53) | P |
|---|---|---|---|
| Preoperative Hb | 135.5 ± 11.9 | 137.9 ± 12.8 | 0.326 |
| Preoperative Hct | 42.2 ± 4.1 | 43.4 ± 4.0 | 0.110 |
SD: Standard deviation; Hb: Hemoglobin; Hct: Hematocrit.
Changes in the levels of hemoglobin and hematocrit
To understand the changing pattern of Hb and Hct, ΔHb and ΔHct was calculated by subtracting Hb or Hct levels from the preoperative value [Figure 1]. The mean preoperative Hb level was 136.70 g/L (120–161 g/L). Hb levels dramatically decreased during the first 4 days after surgery, especially on the surgery day (ΔHb 15.98 ± 6.93 g/L) and reached the minimum on postoperative day 4. The Hb level began to increase on postoperative day 5, and rapidly returned to 86.73% of the preoperative level by 3 weeks. By 6 weeks, the Hb level had recovered 93.56% of the preoperative value. Thereafter, Hb steadily reached the preoperative level by 3 months and maintained this level till 6 months after the surgery.
Figure 1.
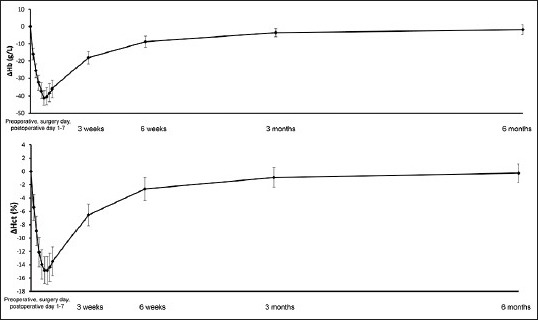
Changes of hemoglobin and hematocrit levels in elderly patients receiving total joint arthroplasty.
The Hct levels showed a similar pattern of changes with Hb levels. The preoperative Hct was 42.78% in our patients. Hct levels reduced most rapidly on the surgery day (ΔHct 5.40%). The minimum point was on the postoperative day 4 (ΔHct 14.83%). Hct showed rapidly recovery during postoperative week 1 to week 3. By the end of week 3, Hct had recovered to 84.76% of the preoperative level and to 93.88% by week 6. Hct reached the preoperative level by 3 months, and remained this level till 6 months after the surgery.
Differences in hemoglobin and hematocrit between sexes
To find out whether sex plays a role in the postoperative levels of Hb and Hct, we compared the Hb and Hct levels between male and female patients [Tables 3 and 4]. No significant differences in Hb and Hct levels were noticed between male and female patients at the various time points, suggesting that sex may not affect the changing pattern of Hb and Hct in elderly patients receiving TJA.
Table 3.
Comparison of ΔHb between male and female patients (g/L, mean ± SD)
| Sex | Preoperative | Surgery day | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Week 3 | Week 6 | Month 3 | Month 6 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (n=54) | 0 | −16.1±7.1 | −25.8±6.7 | −32.3±6.9 | −36.8±6.7 | −40.3±6.9 | −39.4±7.6 | −37.5±8.2 | −35.4±8.3 | −18.1±6.6 | −8.3±6.1 | −2.9±4.5 | 0.1±5.5 |
| Female (n=53) | 0 | −16.2±5.7 | −24.8±6.2 | −30.8±6.0 | −35.4±6.8 | −38.9±7.4 | −38.8±8.4 | −36.6±9.1 | −34.2±8.4 | −17.1±5.6 | −8.4±5.4 | −3.5±4.5 | −1.7±4.1 |
| P | NA | 0.926 | 0.407 | 0.203 | 0.285 | 0.298 | 0.692 | 0.564 | 0.467 | 0.419 | 0.982 | 0.451 | 0.05 |
NA: Not available; SD: Standard deviation; Hb: Hemoglobin.
Table 4.
Comparison of ΔHct between male and female patients (%, mean ± SD)
| Sex | Preoperative | Surgery day | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Week 3 | Week 6 | Month 3 | Month 6 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (n=54) | 0 | −5.2±4.3 | −8.5±3.8 | −11.6±3.9 | −13.5±3.9 | −14.4±3.7 | −14.5±4.0 | −14.0±4.1 | −13.2±4.1 | −6.0±3.2 | −2.3±3.3 | −0.7±2.9 | 0.1±2.8 |
| Female (n=53) | 0 | −5.6±3.5 | −9.3±5.0 | −12.5±5.0 | −14.3±4.8 | −15.1±4.3 | −15.1±4.3 | −14.6±4.4 | −13.6±4.4 | −7.0±3.2 | −2.9±3.6 | −1.1±2.9 | −0.5±2.8 |
| P | NA | 0.599 | 0.353 | 0.301 | 0.346 | 0.369 | 0.456 | 0.467 | 0.627 | 0.323 | 0.523 | 0.421 | 0.365 |
NA: Not available; SD: Standard deviation; Hct: Hematocrit.
Differences in hemoglobin and hematocrit between total knee arthroplasty and total hip arthroplasty
To find out whether surgery types plays a role in the postoperative levels of Hb and Hct, we compared the Hb and Hct levels between patients receiving TKA and those receiving THA [Tables 5 and 6]. On the surgery day, postoperative day 1 and 2, THA patients showed significantly higher ΔHb than TKA patients (all P < 0.05). The two groups of patients did not differ significantly in ΔHb at other time points except at 6 weeks. THA patients only showed significantly higher ΔHct than TKA patients on the surgery day (P = 0.014).
Table 5.
Comparison of ΔHb between patients receiving TKA and those receiving THA (g/L, mean ± SD)
| Items | Preoperative | Surgery day | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Week 3 | Week 6 | Month 3 | Month 6 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TKA (n=53) | 0 | −14.3±6.4 | −23.6±7.2 | −30.2±7.0 | −35.3±7.2 | −38.5±7.5 | −38.4±8.0 | −36.5±8.6 | −34.1±8.5 | −16.8±5.5 | −7.2±5.9 | −2.5±4.9 | −0.7±5.5 |
| THA (n=54) | 0 | −18.0±6.0 | −26.9±5.3 | −32.9±5.6 | −36.9±6.2 | −40.7±6.7 | −39.7±8.0 | −37.6±8.4 | −35.4±8.2 | −18.4±6.7 | −9.5±5.4 | −3.9±3.9 | −0.9±4.3 |
| P | NA | 0.003 | 0.009 | 0.027 | 0.204 | 0.019 | 0.42 | 0.49 | 0.439 | 0.169 | 0.041 | 0.117 | 0.812 |
TKA: Total knee arthroplasty; THA: Total hip arthroplasty; SD: Standard deviation.
Table 6.
Comparison of ΔHct between patients receiving TKA and those receiving THA (%, mean ± SD)
| Items | Preoperative | Surgery day | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Week 3 | Week 6 | Month 3 | Month 6 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TKA (n=53) | 0 | −6.0±4.5 | −8.9±4.1 | −12.0±4.1 | −13.8±4.3 | −14.9±4.1 | −14.9±4.4 | −14.5±4.6 | −13.6±4.6 | −6.5±3.6 | −2.6±3.3 | −0.9±3.0 | −0.1±2.7 |
| THA (n=54) | 0 | −4.9±3.2 | −8.9±4.7 | −12.1±4.8 | −14.0±4.4 | −14.7±4.0 | −14.7±3.9 | −14.1±3.9 | −13.3±4.0 | −6.4±2.8 | −2.6±3.6 | −0.9±2.9 | −0.4±2.9 |
| P | NA | 0.014 | 0.335 | 0.485 | 0.323 | 0.541 | 0.143 | 0.309 | 0.621 | 0.752 | 0.302 | 0.167 | 0.415 |
TKA: Total knee arthroplasty; THA: Total hip arthroplasty; SD: Standard deviation.
DISCUSSION
The perioperative blood management of arthroplasty has been well documented.[5,6,7] However, there have rarely been reports about the changes of Hb and Hct after arthroplasty. Understanding the changing patterns of perioperative blood variation is of clinical importance, especially for aged nontransfusion patients with lower limbs joint arthroplasty. In this study, we summarize the changing patterns of Hb and Hct in arthroplasty and its possible relationship with sex and surgery type.
Concealed hemorrhage has been suggested as an important reason for postoperative blood loss in arthroplasty.[8,9,10] It is mainly caused by hemolysis, blood permeating into the interstitial fluid, blood remaining in the joint cavity and the damage of red blood cell caused by the surgical trauma and other factors. Pattison et al.[11] found that concealed hemorrhage after arthroplasty is mostly associated with hemolysis. Erskine et al.[12] showed that concealed hemorrhage was mainly caused by large amount of blood entering and staying in the intra-articular spaces, with a volume up to 500 ml. It has also been suggested that concealed hemorrhage can be caused by surgical trauma. Markov.[13] found that free radicals can cause damage to red blood cells. Surgical trauma and anesthesia can induce the production of free radicals. Lipid peroxidation induced by free radicals and polyunsaturated fatty acid can be found in the cell membrane, leading to damage to the cell structure and function.[14,15]
In our study, no significant differences in Hb and Hct levels were found between the male and female patients receiving arthroplasty. No consensus has been established regarding the effect of sex on postoperative blood loss and allogeneic blood transfusion. Prasad et al.[16] showed that the postoperative blood loss after TKA in males was significantly higher than that in females. Similarly, another study with 112 patients receiving TKA found that the overall blood loss was greater in men than in women.[17] They considered that it may be related to the larger osteotomy surface and volume in males. Both of these two studies showed that age and body mass index are not significant factors affecting postoperative blood loss in TKA. In the contrary, a retrospective study with 1875 patients receiving arthroplasty found that women presented a higher transfusion rate than men.[18] Another prospective observational study with 5165 patients receiving TKA/THA showed that female sex was a contributing factor for allogeneic blood transfusion. In our study, no significant difference in Hb and Hct levels was noticed between male and female patients. This might be attributed to the exclusion of patients with blood transfusion or preoperative anemia.
The type of joint arthroplasty can also influence the perioperative blood loss. It has been shown that the transfusion rate in THA was 13.5%, significantly higher than that of 9.8% in TKA.[19,20] In our study, greater drop in Hb and Hct was seen in THA patients than TKA patients in the first 4 days postoperatively. The greater blood loss associated with THA can be explained by its anatomy and larger surgical traumas compared with TKA.
The indication for blood transfusion after TJA at our center is Hb <80 g/L. We found that asymptomatic patients with postoperative Hb 75–80 g/L showed similar recovery process of Hb to those with Hb always above 80 g/L. This suggests that the indications for blood transfusion after TJA may be decreased to 75 g/L for patients without typical anemia symptoms. It has been shown that THA patients receiving blood transfusion to maintain Hb over 10 g/dl above did not demonstrate superior outcomes than those with Hb lower than 8 g/dl.[21] This result supports the finding in our study. In addition, transfusion is associated with risks of infection and immune rejection.
This study has limitations. Our study was performed at a single center with a small number of cases. The suggestion of lowering the indications for blood transfusion after joint replacement surgery to 75 g/L needs further validation with larger sample sizes. In addition, our patients were operated by different surgeons and therefore underwent different operation times, which may introduce bias into the results.
In summary, Hb and Hct levels dramatically significantly decrease in the first 4 days after TKA/TJA in elderly patients, and recover to the preoperative levels within 6–12. Sex shows no difference in postoperative Hb and Hct levels. However, the drop in Hb and Hct is greater in THA patients than TKA patients. Blood transfusion may be avoided for asymptomatic patients with Hb over 75 g/L.
Footnotes
Edited by: Yi Cui
Source of Support: Fund Project from China Ministry of Health: Evaluation of Safty and Effect of Arthroplasty (No. 201302007).
Conflict of Interest: None declared.
REFERENCES
- 1.Krebs VE, Higuera C, Barsoum WK, Helfand R. Blood management in joint replacement surgery: What's in and what's out. Orthopedics. 2006;29:801–3. doi: 10.3928/01477447-20060901-02. [DOI] [PubMed] [Google Scholar]
- 2.Bierbaum BE, Meehan JP. Blood conservation in total joint arthroplasty. Orthopedics. 1998;21:989–90. doi: 10.3928/0147-7447-19980901-16. [DOI] [PubMed] [Google Scholar]
- 3.Sehat KR, Evans RL, Newman JH. Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004;86:561–5. [PubMed] [Google Scholar]
- 4.Yang B, Yu JK, Gong X, Chen LX, Wang YJ, Wang J, et al. Sex, age, and annual incidence of primary total knee arthroplasty: A university affiliated hospital survey of 3118 Chinese patients. Chin Med J. 2012;125:3952–5. [PubMed] [Google Scholar]
- 5.Zhang FJ, Xiao Y, Liu YB, Tian X, Gao ZG. Clinical effects of applying a tourniquet in total knee arthroplasty on blood loss. Chin Med J. 2010;123:3030–3. [PubMed] [Google Scholar]
- 6.Zhao X, Lin T, Cai XZ, Yan SG. Comparison of minimally invasive surgery and mini-incision technique for total hip arthroplasty: A sub-group meta-analysis. Chin Med J. 2011;124:4316–23. [PubMed] [Google Scholar]
- 7.Zhang XL, Wang Q, Shen H, Jiang Y, Zeng BF. Minimally invasive two-incision total hip arthroplasty: A short-term retrospective report of 27 cases. Chin Med J. 2007;120:1131–5. [PubMed] [Google Scholar]
- 8.Shen HL, Li Z, Feng ML, Cao GL. Analysis on hidden blood loss of total knee arthroplasty in treating knee osteoarthritis. Chin Med J. 2011;124:1653–6. [PubMed] [Google Scholar]
- 9.Li B, Wen Y, Wu H, Qian Q, Lin X, Zhao H. The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. 2009;33:1263–8. doi: 10.1007/s00264-008-0647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu X, Zhang X, Chen Y, Wang Q, Jiang Y, Zeng B. Hidden blood loss after total hip arthroplasty. J Arthroplasty. 2011;26:1100–5.e1. doi: 10.1016/j.arth.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Pattison E, Protheroe K, Pringle RM, Kennedy AC, Dick WC. Reduction in haemoglobin after knee joint surgery. Ann Rheum Dis. 1973;32:582–4. doi: 10.1136/ard.32.6.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Erskine JG, Fraser C, Simpson R, Protheroe K, Walker ID. Blood loss with knee joint replacement. J R Coll Surg Edinb. 1981;26:295–7. [PubMed] [Google Scholar]
- 13.Markov AK. Hemodynamics and metabolic effects of fructose 1-6 diphosphate in ischemia and shock – experimental and clinical observations. Ann Emerg Med. 1986;15:1470–7. doi: 10.1016/s0196-0644(86)80946-5. [DOI] [PubMed] [Google Scholar]
- 14.Okusaga OO. Accelerated aging in schizophrenia patients: The potential role of oxidative stress. Aging Dis. 2014;5:256–62. doi: 10.14336/AD.2014.0500256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beaulieu E, Ioffe J, Watson SN, Hermann PM, Wildering WC. Oxidative-stress induced increase in circulating fatty acids does not contribute to phospholipase A2-dependent appetitive long-term memory failure in the pond snail Lymnaea stagnalis. BMC Neurosci. 2014;15:56. doi: 10.1186/1471-2202-15-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prasad N, Padmanabhan V, Mullaji A. Blood loss in total knee arthroplasty: An analysis of risk factors. Int Orthop. 2007;31:39–44. doi: 10.1007/s00264-006-0096-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cushner FD, Friedman RJ. Blood loss in total knee arthroplasty. Clin Orthop Relat Res. 1991:98–101. [PubMed] [Google Scholar]
- 18.Rashiq S, Shah M, Chow AK, O’Connor PJ, Finegan BA. Predicting allogeneic blood transfusion use in total joint arthroplasty. Anesth Analg. 2004;99:1239–44. doi: 10.1213/01.ANE.0000132928.45858.92. [DOI] [PubMed] [Google Scholar]
- 19.Evans S, O’Loughlin E, Bruce J. Retrospective audit of blood transfusion and comparison with haemoglobin concentration in patients undergoing elective primary and revision lower limb arthroplasty. Anaesth Intensive Care. 2011;39:480–5. doi: 10.1177/0310057X1103900322. [DOI] [PubMed] [Google Scholar]
- 20.Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81:2–10. doi: 10.2106/00004623-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453–62. doi: 10.1056/NEJMoa1012452. [DOI] [PMC free article] [PubMed] [Google Scholar]


