Abstract
Background
While drug use is associated with HIV risk in Southeast Asia, little is known about substance use behaviors among women, including drug injection.
Objectives
To describe patterns of substance use among women using alcohol and drugs in Malaysia and identify correlates of lifetime and active drug injection, a risk factor for HIV transmission.
Methods
A survey of 103 women who used drugs in the last 12 months assessed drug use history and frequency, including drug injection and drug use during pregnancy, self-reported HIV-status, childhood and adulthood physical and sexual abuse, and access to and utilization of harm reduction services, including needle-syringe exchange programs (NSEP) and opioid agonist maintenance therapy (OAT). Principal component analyses (PCA) were conducted to assess drug use grouping.
Results
Amphetamine-type substances (ATS; 82.5%), alcohol (75.7%) and heroin (71.8%) were the most commonly used drugs across the lifetime. Drug injection was reported by 32.0% (n=33) of participants with 21.4% (n=22) having injected in the last 30 days. PCA identified two groups of drug users: opioids/benzodiazepines and club drugs. Lifetime drug injection was significantly associated with lower education, homelessness, prior criminal justice involvement, opioid use, polysubstance use, childhood physical and sexual abuse, and being HIV-infected, but not with prior OAT.
Conclusion
Women who use drugs in Malaysia report high levels of polysubstance use and injection-related risk behaviors, including sharing of injection equipment and being injected by others. Low OAT utilization suggests the need for improved access to OAT services and other harm reduction measures that prioritize women.
1. Introduction
Drug use poses a major public health problem in Southeast Asia. Recent age-adjusted estimates indicate a high prevalence of dependence to opioids (0.15%) and amphetamines (0.42%) in the region (1). East and Southeast Asia account for 20% of the world’s illicit opioid use, due in part to large-scale manufacturing and distribution networks throughout Southeast Asia (2). Likewise, the prevalence of amphetamine-type substance (ATS) use has emerged in this region, with an estimated 34.4 million [13.9–54.8 million] ATS users worldwide in 2012 (2).
While addiction has dire direct health consequences (3, 4), it is also inextricably linked with Human Immunodeficiency Virus (HIV) infection and other health risks and co-morbidities (5, 6). As of 2013, there were an estimated 2.4–4.4 million people who inject drugs (PWID) in the region (2, 7). In Southeast Asia, HIV prevalence among PWID is estimated at 9.6%, yet is over 2-fold greater in Malaysia (4). Malaysia, a religiously and culturally diverse middle-income country of 29.2 million, has one of the fastest growing economies in Southeast Asia. Though PWID still account for the majority of people living with HIV (PLWH) in Malaysia, the epidemic has transitioned towards a generalized HIV epidemic with bridges between PWID and their sexual partners. In 2011, 39% of incident HIV cases were among PWID (8), with increasing evidence of sexual transmission and infection among women (9, 10). Moreover, new infections attributed to sexual transmission remain higher among females than males (87% vs 47%) (11).
Cumulatively, approximately 11,000 (14%) of the 81,000 HIV cases ever reported in Malaysia have been among women and girls (10). While a substantial body of work has examined the relationship between substance use and HIV among men in Malaysia, little attention has been focused on substance use and HIV among women, including drug injection behaviors. Women are likely to experience HIV risk differently than men. In the United States, the impact of drug use (12–14) and interpersonal violence (12, 13, 15–17) on increased HIV risk among women is well-documented. Moreover, women are more likely than men to be introduced to drugs by an intimate partner (18). Interpersonal violence is also a major risk factor for HIV transmission among women, globally (17, 19–21), and high levels of interpersonal violence have been documented in the Asia-Pacific region (22). International research has identified gender-based violence as a significant contributor to gender inequality (23), which in turn impacts access to addiction treatment and HIV prevention and care services (14, 24–26). Likewise, power imbalances in intimate partner relationships often lead to high risk injection practices in which females are injected by male partners using the same equipment used to inject themselves (27, 28), placing females at greater risk for HIV infection. A recent review of data reported to the Joint United Nations Program on HIV and AIDS (UNAIDS) between 2011 and 2013 found that, in Malaysia, women who inject drugs were 1.48 times more likely to be HIV-infected than their male counterparts who inject drugs (29). While women may represent a smaller absolute number of PWID compared to men, these data highlight that women face a greater number of health-related risks, including HIV.
Although drug use remains a serious problem in Malaysia, the increased availability of opioid agonist maintenance treatment (OAT) for opioid dependence has been a major priority for the Malaysian government since 2006 when the Malaysian Ministry of Health introduced government-funded free methadone maintenance treatment for Malaysians at select government clinics (30). For a temporary period, methadone was provided within at least one mosque as an effort to bridge the divide between the government’s advocacy for OAT and skepticism from religious leaders (31). Today, free methadone treatment has been expanded to prisons (32, 33), community health centers, and is also available at select privately operated clinics on a fee-for-service basis. Despite OAT expansion and other harm reduction programs, including needle and syringe exchange programs (NSEP) throughout Malaysia, a recent review confirmed that no data are available for women receiving OAT throughout the country (34) and that these programs are inadequately scaled-to-need (35).
Despite extensive research documenting the syndemic of substance use and HIV among men in Malaysia (36–38), little attention has been directed to the parallel evolving public health crisis of HIV and drug use among women (34). Of the limited information available about women with or at risk for HIV in Malaysia, all has been collected by one NGO and restricted to only 20 drug-using women in Kuala Lumpur (39), which speaks to the hidden epidemic of drug use in women. This absence of data has also been compounded by the criminalization of drug use in Malaysia, which has led to significant stigmatization of drug users, particularly among women who use drugs. Additionally, illicit drug use is considered ‘haram’, a major sin for Muslims, leading to further prejudice and discrimination against people who use drugs. Fear of prosecution by the law and being ostracized by the family and community results in women who use drugs being afraid to come forward for services and treatment (40, 41).
The goal of this study was to explore and better characterize drug use patterns among women who use drugs in Malaysia. The study also sought to describe the prevalence and complexity of lifetime drug use and recent drug injection practices and their relationship to HIV infection and other medical and social co-morbidities. To our knowledge, this paper represents the first empirical study of the substance use patterns and risk behaviors among drug-using women in Malaysia.
2. Methods
2.1 Participants
A cross-sectional survey of 103 women in Kuala Lumpur, Malaysia was conducted from July to August 2011. Participants were recruited using convenience sampling at five sites, including a community drop-in center (n=55), two women’s shelters (n=27), and two voluntary drug treatment centers (n=21). The community drop-in center location provides information and services on HIV testing, sexual and drug use education, outreach and basic health screening services. Information sessions were held at each venue and flyers posted describing the study purpose, potential risks, and benefits to participation were used to assist recruitment efforts. Convenience sampling was chosen over more representative sampling methods like respondent-driven sampling (RDS) due to serious challenges by one of the co-authors with recruiting female PWID in Malaysia using this method, in which only 17 (3.7%) of 460 recruited PWID were women, despite increased incentives offered to recruit women (42). Interested individuals met with trained research assistants who assessed eligibility (> 18 years of age and had used any illicit substance within the past 12 months), obtained written informed consent, and described the anonymous nature of the study and that participation could be terminated at any time without consequence.
2.2 Survey Administration
Participants were administered a 60-minute structured questionnaire that included demographics, criminal justice involvement, substance use history, reproductive history, previous HIV and STI testing and diagnoses, social support, physical and mental health, access to social and medical services, and experience of childhood and adulthood interpersonal violence. The survey content was first developed in English, translated into Bahasa Malaysia and then back-translated to verify accuracy and cultural consistency using previously described techniques (43). Discrepancies in translated content were reviewed together by research and community outreach program staff members. The final version was approved by all research team members. Interviews were conducted in private rooms and all participants were paid 50 Malaysian Ringgit (~$16 USD) for their time.
2.3 Survey Measures
All measures, including health conditions, were self-reported. Validated measures were used to assess certain constructs. Depression screening was measured using the 20-item Center for Epidemiologic Studies Depression (CES-D) scale, using previously validated cut-offs (>20) for major depression (44, 45). Experience of childhood and adulthood physical and sexual violence was measured using the U.S. Centers for Diseases Control’s Behavioral Risk Factor Surveillance System questionnaire for Violence and Victimization (46) and general social support was measured as a continuous variable using the Medical Outcomes Study scale (47).
2.4 Definitions Used for Data Analysis
“Injection drug use” was defined as having ever injected any drug in one’s lifetime and was stratified as “Lifetime” (ever injected) and “Active” (injected in 30 day period prior to the interview). “Any opioid use” was defined as any non-prescription use of methadone, suboxone/subutex, heroin, opium, or ketum. Ketum (Mitragyna speciosa), also known as Kratom, is a psychoactive plant native to Southeast Asia that has opioid agonist properties with high potential for abuse (48–50). Polysubstance use was defined as using three or more different substances in the same day. Club drug use was defined by lifetime use of MDMA (3,4-methylenedioxy-methamphetamine; “ecstasy”), cannabis, ketamine, or ATS. Sharing of drug injection equipment was defined as any use of drug paraphernalia that had previously been used by another person, including needles, syringes, and drawing drugs from a previously used container or cooker. NSEP utilization was defined as ever having exchanged used needles and/or syringes from a NSEP provider. OAT utilization was defined as having ever received methadone or buprenorphine as a medical prescription for the treatment of opioid dependence. Primary source of income, frequency of any unprotected sex, and frequency of transactional sex, defined as exchanging sex for money, drugs, a place to stay, food, or clothes, were assessed over the 6-month period prior to the interview date. Sex work was further stratified by frequency as follows: 1) “Regular” if sex work was their primary income source; 2) “Intermittent” if sex work was not their primary income source but they reported it at least once during the last 6 months; and 3) “No Sex Work” if they did not report it as a source of income. Housing status and drug injection frequency corresponded to the previous 30 days. For women in residential treatment facilities, these variables were assessed for the 30 days before treatment entry. “Criminal justice involvement” included spending at least one night in jail, prison or a compulsory drug detention center (CDDC) in one’s lifetime. Childhood sexual abuse was defined as having answered ‘yes’ to any one of the following: Before the age of 18, have you ever: 1) been touched in a sexual way by an adult or older child when you did not want to be touched that way, 2) been forced to touch an adult or older child in a sexual way, or 3) been forced to have sex by an adult or older child. Adulthood sexual abuse was defined as having ever had any unwanted sexual experiences since the age of 18. Childhood and adulthood physical abuse were defined as having been “hit, slapped, punched, or kicked” by an adult before the age of 18 or since the age of 18, respectively. Poverty was defined using 2010 national estimates as earning ≤800 Malaysian Ringgit (RM) monthly (51, 52). Housing status was defined as: 1) “stable” if living in one’s or a partner’s own home; 2) “unstable” if living temporarily with a friend, family member, or in short-term housing; and 3) “homeless” if living in a temporary shelter, on the streets, or in a detention setting.
2.5 Analytic Approach
Chi-square tests were performed to determine the correlates of the three dependent variables of interest: lifetime injection drug use, active injection drugs use, and self-reported HIV infection. Each dependent variable was evaluated against the covariates presented in Tables 2 and 3. Due to the small sample size, only chi-square p-values are provided for each analysis. Out of an abundance of caution, multicollinearity was examined for the analyses in Tables 2 and 3. Values for variance inflation factor were less than 4. Principal components analysis with Varimax rotation was conducted as a data reduction strategy to better understand the complexity of drug use. All data were analyzed using IBM SPSS version 22 (53).
Table 2.
Principal Components Analysis of Drug Use
| Component 1: Club Drugs |
Component 2: Opioids and benzodiazepines |
|
|---|---|---|
| MDMA (Ecstasy) | 0.828 | −0.247 |
| Cannabis | 0.742 | 0.227 |
| Ketamine | 0.701 | 0.276 |
| Amphetamine-type substances |
0.487 | 0.238 |
| Any Opioid | −0.008 | 0.784 |
| Benzodiazepines | 0.342 | 0.666 |
Table 3.
Characteristics associated with Lifetime (n=33) and Active (n=22) Drug Injection
| Lifetime Drug Injection | Active Drug Injection (Past 30 days) |
||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Total N = 103 |
Yes %(n) |
No %(n) |
P-value | Yes %(n) |
No %(n) |
P- value |
| Ethnicity | |||||||
| Malay | 61.2 (63) | 69.7 (23) | 57.1 (40) | 0.224 | 77.3 (17) | 56.8 (46) | 0.081 |
| Not Malay | 38.8 (40) | 30.3 (10) | 42.9 (30) | 22.7 (5) | 43.2 (35) | ||
| Religion | |||||||
| Muslim | 75.8 (25) | 61.4 (43) | 0.152 | 81.8 (18) | 61.7 (50) | 0.078 | |
| Not Muslim | 24.2 (8) | 38.6 (27) | 18.2 (4) | 38.3 (31) | |||
| Highest level of education completed |
|||||||
| Primary or less | 39.8 (41) | 48.5 (16) | 35.7 (25) | 0.041 | 40.9 (9) | 39.5 (32) | 0.488 |
| Form 3 – Form 4 | 28.2 (29) | 36.4 (12) | 24.3 (17) | 36.4 (8) | 25.9 (21) | ||
| Form 5 – University | 32.0 (33) | 5.2 (5) | 40.0 (28) | 22.7 (5) | 34.6 (28) | ||
| Relationship Status | |||||||
| Single | 69.9 (72) | 87.9 (29) | 61.4 (43) | 0.006 | 86.4 (19) | 65.4 (53) | 0.058 |
| Partnered / married | 30.1 (31) | 12.1 (4) | 38.6 (27) | 13.6 (3) | 34.6 (28) | ||
| Homeless in last 30 days | |||||||
| Yes | 31.1 (32) | 48.5 (16) | 22.9 (16) | 0.009 | 50.0 (11) | 25.9 (21) | 0.039 |
| No | 68.9 (71) | 51.5 (17) | 77.1 (54) | 50.0 (11) | 74.1 (60) | ||
| Criminal Justice Involvement (ever) |
|||||||
| Lock-up or Jail | 93.2 (96) | 100.0 (33) | 90.0 (63) | 0.094 | 100.0 (22) | 91.4 (74) | 0.153 |
| Prison | 70.9 (73) | 100.0 (33) | 57.1 (40) | <0.001 | 100.0 (22) | 63.0 (51) | <0.001 |
| CDDC | 47.6 (49) | 87.9 (29) | 28.6 (20) | <0.001 | 86.4 (19) | 37.0 (30) | <0.001 |
| Unmet Need for Social / Medical Services |
|||||||
| Welfare / Financial Support |
55.3 (57) | 57.6 (19) | 54.3 (38) | 0.750 | 72.7 (16) | 50.6 (41) | 0.064 |
| Educational Training | 43.7 (45) | 33.3 (11) | 48.6 (34) | 0.153 | 36.4 (8) | 45.7 (37) | 0.435 |
| Housing Assistance | 60.2 (62) | 60.6 (20) | 60.0 (42) | 0.951 | 54.5 (12) | 61.7 (50) | 0.542 |
| Medical Services | 18.4 (19) | 9.1 (3) | 22.9 (16) | 0.092 | 9.1 (2) | 21.0 (17) | 0.202 |
| Drop-in Center | 16.5 (17) | 15.2 (5) | 17.1 (12) | 0.784 | 18.2 (4) | 16.0 (13) | 0.811 |
| NSEP | 1.9 (2) | 6.1 (2) | 0 (0) | 0.103 | 4.5 (1) | 1.2 (1) | 0.318 |
| Preferred Drug | |||||||
| ATS | 45.6 (47) | 39.4 (13) | 48.6 (34) | 0.383 | 50.0 (11) | 44.4 (36) | 0.643 |
| Any opioid | 41.7 (43) | 60.6 (20) | 32.9 (23) | <0.001 | 100.0 (22) | 67.9 (55) | 0.002 |
| Club drug | 9.7 (10) | 0 (0.0) | 14.3 (10) | 0.022 | 0.0 (0) | 12.3 (10) | 0.083 |
| Polysubstance use | 53.4 (55) | 72.7 (24) | 44.3 (31) | 0.007 | 81.8 (18) | 45.7 (37) | 0.003 |
| Harm Reduction | |||||||
| NSEP utilization | 13.0 (12.6) | 39.4 (13) | 0.0 (0) | <0.001 | 50.0 (11) | 2.5 (2) | <0.001 |
| OAT utilizationa | 58.3 (60) | 66.7 (22) | 55.1 (38) | 0.266 | 59.1 (13) | 58.8 (47) | 0.977 |
| Sexual Risk Behaviors | |||||||
| Any transactional sex in last 6 months |
44.7 (46) | 36.4 (12) | 48.6 (34) | 0.253 | 45.5 (10) | 44.4 (36) | 0.933 |
| Sex work as primary incomea |
19.6 (20) | 18.8 (6) | 20.0 (14) | 0.882 | 28.6 (6) | 17.3 (14) | 0.246 |
| Any unprotected sex in last 30 days |
47.3 (35/74) | 36.0 (9/25) | 53.1 (26/49) |
0.161 | 42.1 (8) | 49.1 (27) | 0.599 |
| Comorbidities | |||||||
| HIV-infectedb | 20.0 (20) | 39.4 (13) | 10.4 (7) | <0.001 | 4.4 (8) | 15.6 (12) | 0.036 |
| HCV-infectedc | 8.9 (9) | 27.3 (9) | 0 (0) | <0.001 | 2.0 (4) | 7.0 (5) | 0.082 |
| Major Depression | 60.6 (20) | 60.0 (42) | 0.953 | 68.2 (15) | 58.0 (47) | 0.388 | |
| Violence and Victimization | |||||||
| Childhood sexual abuse | 30.7 (31/101) | 48.5 (16) | 22.1 (15/68) |
0.007 | 50.0 (11) | 25.3 (20) | 0.026 |
| Childhood physical abuse |
49.5 (51) | 66.7 (22) | 41.4 (29) | 0.017 | 68.2 (15) | 44.4 (36) | 0.048 |
| Adulthood sexual abuse | 23.8 (24/101) | 33.3 (11) | 19.1 (13) | 0.122 | 40.9 (9) | 19.0 (15) | 0.033 |
| Adulthood physical abuse |
62.0 (62/100) | 75.0 (24) | 55.9 (38) | 0.074 | 86.4 (19) | 55.1 (43) | 0.008 |
| Adulthood physical abuse by an intimate partner |
75.8 (47/62) | 70.8 (17/24) | 78.9 (30/38) |
0.473 | 68.4 (13) | 79.1 (34) | 0.367 |
n=102
n=100
n=101
Legend: ATS: amphetamine-type substance; CDDC: compulsory drug detention center; NSEP: needle/syringe exchange program; OAT: opioid agonist maintenance therapy;
2.6 Ethics and Human Subjects
Participants were assigned a unique code to maintain anonymity. No names or other identifying information was collected. The Institutional Review Boards of Yale University and the University of Malaya reviewed and approved this study.
3. Results
3.1 Sample Characteristics
Sample characteristics are reported in Table 1. Participants were, on average, approximately 40 years old, Muslim (66.0%) and single (69.9%) and had not completed Form 5 education (high school) (68%). Most women reported being either homeless (31.1%) or unstably housed (31.1%). Prior involvement with the criminal justice system was common, including jail detention (93.2%) and prison sentences (70.9%), primarily (91.7%) for drug-related charges. Nearly half (47.6%) had been involuntarily placed in a CDDC, with an average detention time of 22.4 months. Median monthly income was 800 RM, with traditional full-time (31.4%), traditional part-time (22.5%) and transactional sex work (19.6%) constituting the main sources of income.
Table 1.
Sample Characteristics (N=103)
| Ethnicity | %(n) |
|---|---|
| Malay | 61.2 (63) |
| Indian | 16.5 (17) |
| Chinese | 14.6 (15) |
| Other | 7.8 (8) |
| Relationship Status | |
| Single | 69.9 (72) |
| Partnered or married | 30.1 (31) |
| Highest level of education completed | |
| None | 11.7 (12) |
| Primary | 28.2 (29) |
| Form 3 | 28.2 (29) |
| Form 5 | 26.2 (27) |
| Form 6 | 1.9 (2) |
| University | 3.9 (4) |
| Religion | |
| Muslim | 68 (66.0) |
| Buddhist | 11 (10.7) |
| Hindu | 11 (10.7) |
| Christian | 7 (6.8) |
| Other | 4 (3.9) |
| None | 2 (1.9) |
| Age (mean, SD) | 39.4 ±10.7 |
| Age (range) | (19–66) |
| Median income in Malaysian Ringgit (range) | RM 800/ month (0–30,000) |
| Primary Source of Income a | |
| Full-time, traditional | 31.4 (32) |
| Part-time, traditional | 22.5 (23) |
| Sex work | 19.6 (20) |
| Welfare/Public Assistance | 3.9 (4) |
| Friend | 2.9 (3) |
| Other | 19.6 (20) |
| Sex Work | |
| Regular | 19.4 (20) |
| Intermittent | 24.3 (25) |
| None | 56.3 (58) |
| Housing Status | |
| Homeless | 31.1 (32) |
| Unstable | 31.1 (32) |
| Stable | 37.9 (39) |
| Social Support (scale 1–5) (mean, SD) | 3.2 ±1.2 |
| Previous Incarceration or Detention | |
| Jail, ever | 93.2 (96) |
| Prison, ever | 70.9 (73) |
| Any previous incarceration or detention due to drug useb | 91.7 (88/96) |
| Previous incarceration events [jail and prison], medianb | 6 (1–317) |
| Total lifetime months incarcerated [lock-up and prison], mean, SDb | 58.8 ±68.1 |
| Total lifetime months incarcerated [lock-up and prison], median (range) |
46 (2–400) |
| Previous placement in CDDC, evera | 47.6 (49) |
| Total lifetime CDDC events (median)a | 2 (1–14) |
| Total lifetime months in CDDC (mean)a | 22.4 ±16.5 |
| Substance Abuse Risk Behaviors | |
| Injection Drug Use | |
| Never | 68.8 (70/103) |
| Yes, more than 30 days ago (remote) | 10.7 (11/103) |
| Yes, in last 30 days (active) | 21.4 (22/103) |
| Shared injection equipment – Last 30 days | 68.2 (15/22) |
| Injected another person – Last 30 days | 68.2 (15/22) |
| Been injected by another person – Last 30 days | 95.5 (21/22) |
| Sex work | |
| Any sex work (past 6 months) | 44.7 (46) |
| For money | 91.3 (42/46) |
| For drugs | 26.1 (12/46) |
| For a place to stay | 23.9 (11/46) |
| For food | 15.2 (7/46) |
| For clothing | 10.9 (5/46) |
| Comorbidities | |
| Depression | 60.2 (62) |
| Severe | 48.5 (50) |
| Moderate | 11.7 (12) |
| Mild | 11.7 (12) |
| Infectious Diseases (self-reported) | |
| HIV | 20.0 (20/100) |
| Hepatitis C | 8.9 (9/101) |
| Hepatitis B | 4.0 (4/101) |
| Tuberculosis (active) | 3.0 (3/101) |
| Violence and Victimization | |
| Childhood sexual trauma | 30.7 (31/101) |
| Childhood physical abuse | 49.5 (51) |
| Adulthood sexual trauma | 23.8 (24/101) |
| Adulthood physical abuse | 62.0 (62/100) |
| Adulthood physical abuse by an intimate partner | 75.8 (47/62) |
n=102
n=96, or those with any previous incarceration
Self-reported infection status for HIV (20.0%), hepatitis C virus (HCV; 8.9%), hepatitis B virus (HBV; 4.0%), and active tuberculosis (3.0%) was notable and nearly half of participants (48.5%) met screening criteria for severe depression. Concerning were the high self-reported rates of childhood (30.7%) and adulthood (23.8%) sexual abuse, and childhood (49.5%) and adulthood (62%) physical abuse. Importantly, of the 62 women who had experienced physical abuse as adults, 47 (75.8%) had been a victim of interpersonal violence by an intimate partner.
3.2 Substance Use
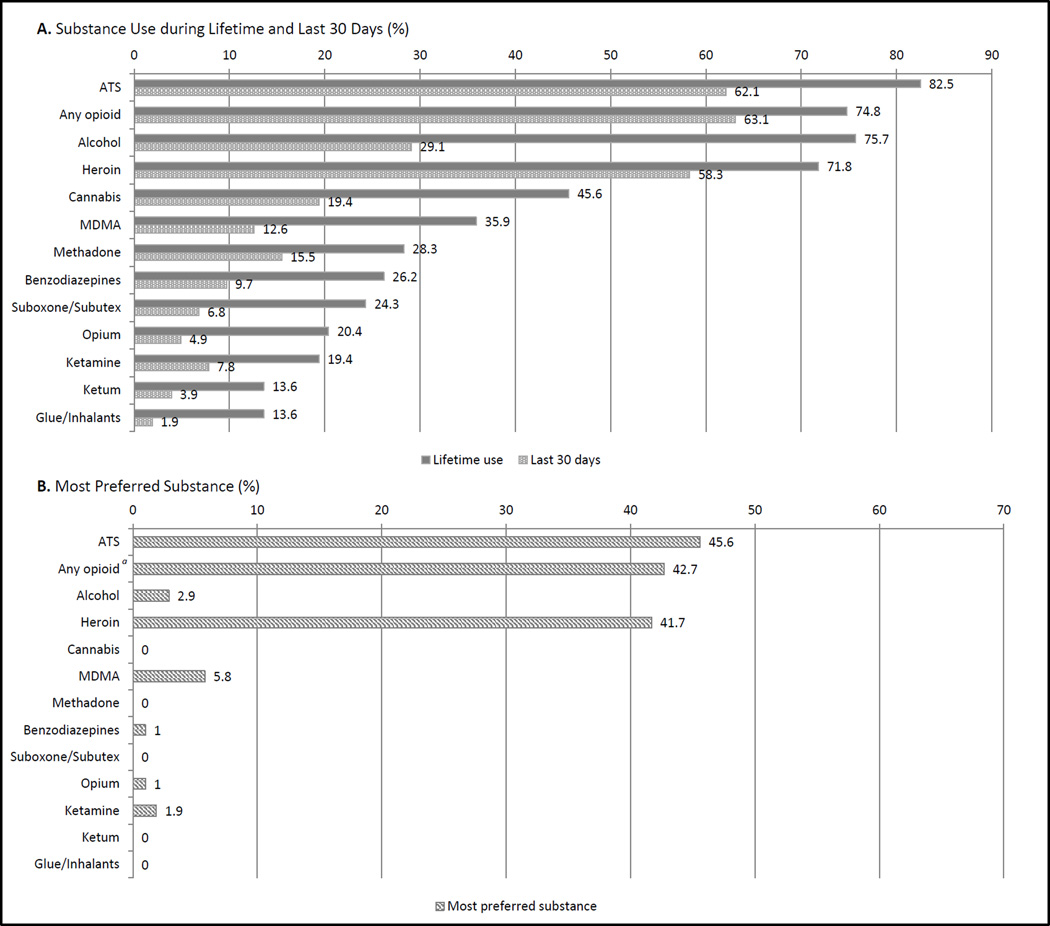
Figure 1 describes participants’ lifetime and active substance use history. ATS (82.5%), opioids (74.8%), alcohol (75.7%) and heroin alone (71.8%) were the most commonly reported substances ever used, while drugs actively being used included opioids (63.1%), ATS (62.1%), heroin alone (41.7%) and alcohol (29.1%). Participants’ primary drugs of choice were ATS (45.6%) and heroin (41.7%).
Figure 1.
Drug use history and most preferred substance
α “Any opioid” is a composite variable representing combined responses to heroin, and any other opioid-based substance. It should not be included in the sum of the percentages of most preferred substances.
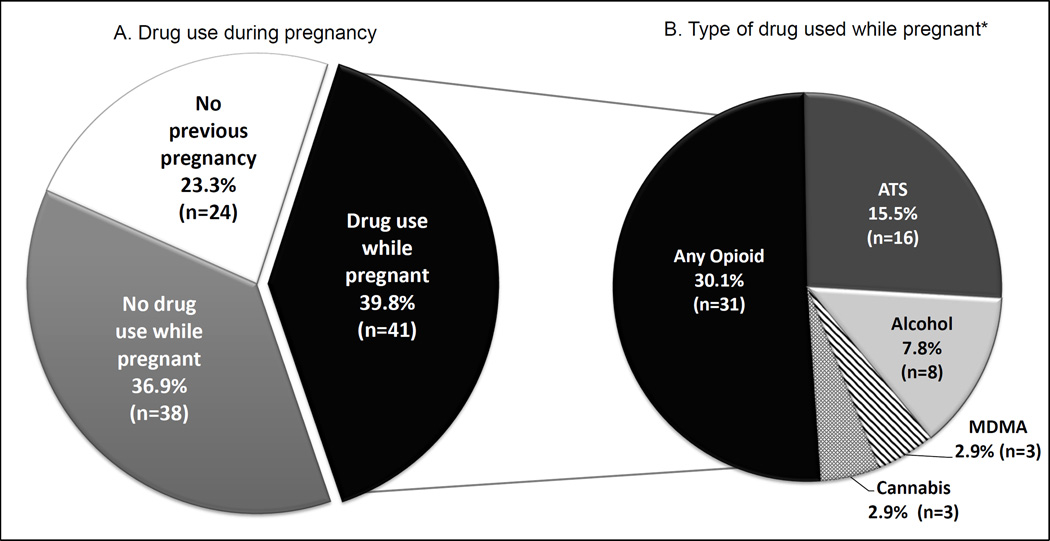
High rates of drug use during pregnancy were reported (Figure 2). Among the 79 (76.7%) participants who had ever been pregnant, 41 (51.9%) had used drugs during pregnancy, including opioids (30.1%), ATS (15.5%) and alcohol (7.8%) most frequently.
Figure 2.
Previous drug use during pregnancy
*Pie chart “B” does not sum to 100% due to participant ability to select more than one drug
3.3 Injection drug use
Overall, (Table 1) nearly one-third (32%) of participants reported having ever injected drugs, with 66.7% (22/33) of them having done so within the last 30 days. Among active injectors, 68.2% reported sharing injection equipment with others and 95.5% had been injected by another person.
Across their lifetime, 32% (33/103) of participants reported having ever injected heroin, followed by ATS (8.7%; 9/103), benzodiazepines (3.9%; 4/103), opium (3.9% 4/103), subutex/suboxone (2.9%; 3/103), methadone (1.9%; 2/103), and ketamine (1.0%; 1/103). Same-day polysubstance injection across the lifetime was 8.7% (9/103). Among the 22 participants who reported having injected drugs in the last 30 days, the most commonly injected substances were heroin (81.0%; 18/22), ATS (31.8%; 7/22), methadone (9.1%; 2/22), and ketamine (4.5%, 1/22). Same-day polysubstance injection in the last 30 days was 27.3% (6/22).
3.4 Principal Components Analysis of Drug Use
Drug use in the last 30 days was explored for patterns using a principal components analysis (PCA). In order to reduce overlap in classes of drugs, only cannabis, MDMA, ketamine, ATS, any opioids, and benzodiazepines were included in the PCA. Table 2 shows the rotated PCA solution, which yielded 2 components that explained 56.2% of the variance in responses. Component 1, comprised of MDMA, cannabis, ketamine, and ATS, was named “club drugs.” Component 2 included any opioids and benzodiazepines, and was named “opioids and benzodiazepines.” Item loadings ranged from strong (0.828) to moderate (0.487) for both components.
3.5 Correlates of lifetime and active drug injection
Table 3 shows the correlates of lifetime and active drug injection. Lifetime drug injection was correlated with lower education, being single, and being HCV-infected. Both lifetime and active drug injection were correlated with reporting opioids as the drug of choice, polysubstance use, NSEP utilization, greater levels of homelessness, criminal justice involvement, being HIV-infected, childhood sexual and physical abuse, and adulthood physical abuse. Active injection was also significantly correlated with sexual abuse as an adult. Neither lifetime nor active drug injection were correlated with having previously received OAT.
3.5 Correlates of self-reported HIV-infection
Table 4 provides the correlates of self-reported HIV infection, including being single, previous criminal justice involvement with prisons or CDDCs, both lifetime and active drug injection, and history of sharing injection equipment. Importantly, engaging in sex work and utilizing harm reduction services (NSEP or OAT) were not associated with HIV.
Table 4.
Characteristics associated with self-reported HIV infection (n=100)a
| Characteristic | Total Pop N = 100 |
HIV-infected (n=20; 20%) |
HIV-uninfected (n=80; 80%) |
P-value |
|---|---|---|---|---|
| Ethnicity | ||||
| Malay | 60.0 (60) | 65.0 (13) | 58.8 (47) | 0.611 |
| Not Malay | 40.0 (40) | 35.0(7) | 41.3 (33) | |
| Religion | ||||
| Muslim | 65.0 (65) | 70.0 (14) | 63.7 (51) | 0.600 |
| Not Muslim | 35.0 (35) | 30.0 (6) | 36.3 (29) | |
| Highest level of education completed | ||||
| None – Primary | 40.0 (40) | 60.0 (12) | 35.0 (28) | 0.103 |
| Form 3 – Form 4 | 29.0 (29) | 25.0 (5) | 30.0 (24) | |
| Form 5 – University | 31.0 (31) | 15.0 (3) | 35.0 (28) | |
| Relationship Status | ||||
| Single | 71.0 (71) | 90.0 (18) | 66.3 (53) | 0.029 |
| Partnered / married | 29.0 (29) | 10.0 (2) | 33.8 (27) | |
| Homeless in last 30 days | ||||
| Yes | 32.0 (32) | 40.0 (8) | 30.0 (24) | 0.394 |
| No | 68.0 (68) | 60.0 (12) | 70.0 (56) | |
| Criminal Justice Involvement (ever) | ||||
| Lock-up or Jail | 93.0 (93) | 95.0 (19) | 92.5 (74) | 0.572 |
| Prison | 73.0 (73) | 90.0 (18) | 68.8 (55) | 0.045 |
| CDDC | 49.0 (49) | 75.0 (15) | 42.5 (34) | 0.009 |
| Preferred drugb | ||||
| ATS | 46.0 (46) | 45.0 (9) | 46.3 (37) | 0.921 |
| Any opioid | 42.7 (44) | 55.0 (11) | 41.3 (33) | 0.268 |
| Club drug | 8.0 (8) | 0.0 (0) | 10.0 (8) | 0.352 |
| Polysubstance use | ||||
| Lifetime drug injection (ever) | 33.0 (33) | 65.0 (13) | 25.0 (20) | <0.001 |
| Active drug injection (last 30 days) | 22.0 (22) | 40.0 (8) | 17.5 (14) | 0.043 |
| NSEP Utilization (ever)c | 12.6 (13) | 25.0 (5) | 10.0 (8) | 0.074 |
| Any sharing of injection equipment (ever) |
15.0 (16) | 35.0 (7) | 11.3 (9) | 0.010 |
| Sexual Risk Behaviors | ||||
| Any transactional sex in last 6 months |
44.0 (44) | 35.0 (7) | 46.3 (37) | 0.363 |
| Sex work as primary incomea | 19.0 (19) | 21.1 (4) | 18.8 (15) | 0.821 |
| Any unprotected sex in last 30 daysd |
48.6 (35/72) | 26.7 (4/15) | 54.4 (31/57) | 0.102 |
| Major Depression | 60.0 (60) | 50.0 (10) | 62.5 (50) | 0.307 |
| Violence and Victimization | ||||
| Childhood sexual abuse | 30.0 (30) | 45.0 (9) | 26.9 (21) | 0.118 |
| Childhood physical abuse | 49.0 (49) | 55.0 (11) | 47.5 (38) | 0.548 |
| Adulthood sexual abuse | 23.0 (23) | 24.4 (19) | 20.0 (4) | 0.682 |
| Adulthood physical abuse | 60.0 (60) | 68.4 (13) | 60.3 (47) | 0.511 |
| Adulthood physical abuse by an intimate partner |
63.0 (63) | 70.0 (14) | 61.3 (49) | 0.468 |
HIV status self-report available for n=100
Drug use based on principle components analysis
N = 99
N =72
Legend: ATS: amphetamine-type substance; CDDC: compulsory drug detention center; NSEP: needle/syringe exchange program
4. Discussion
4.1 Sharing of Injection Equipment
To our knowledge, this study represents the first expanded evaluation of substance use with related drug use patterns and risk behaviors among women who use drugs in Malaysia, and provides important insights into an extraordinarily high-risk population that remains hidden and inadequately assessed. This is particularly relevant as the proportion of women diagnosed with HIV is increasing in a cultural setting where the syndemic nature of substance use, victimization, and HIV are inextricably linked, but are largely absent from the public dialogue on HIV prevention in Malaysia (54).
HIV risk assessments of drug users in Malaysia have almost exclusively focused on men in community (55–60) and criminal justice (33, 37, 38, 61–64) settings. Indeed, even in Malaysia’s largest study of PWID (N=460), which used respondent-driven sampling, only 17 (3.7%) women were successfully recruited despite increased recruitment incentives (42, 65). While women and men were not compared in the present sample, this study provides important insight into women’s substance use and related patterns, which may contribute to improved HIV prevention and treatment strategies in the future. Important from these findings in the PCA is that the interventions that would be effective would differ greatly between those that principally use opioids, where OAT would be most effective (5).
Prevalence of lifetime drug injection behavior was moderate in this sample, however, high rates of sharing behavior among active PWID (n=15/22, 68.2%) combined with almost universal reports of having been recently injected by someone else (n=21/22, 95.5%) point to an environment highly conducive for HIV transmission. High rates of partner injection in opposite-sex relationships often have women on the receiving end of injection equipment previously used by their partner (14). There is also strong evidence that substance use plays a pivotal role in maintaining power imbalances in these relationships, which perpetuates the high risk environment of drug use and HIV (14). In the present sample, this may be evidenced by the correlation of drug injection behavior with sexual and physical abuse during childhood and adulthood as well as recent homelessness, which is consistent with data from other countries showing women’s substance use to be enmeshed with their intimate partner relationships (15, 66–68).
It is possible that high rates of equipment sharing may also be related to sharing of injection equipment among non-partner individuals. In the Malaysian context, so-called “port doctors” – persons in the community who provide injection services and typically operate under bridges or ports near coastal areas, sometimes called “street doctors” in the U.S. – are believed to contribute heavily to onward transmission of HIV in Malaysia (69). Similar evidence has also been found in the United States (70) and Vietnam (71) and demonstrate how such injection activities drive HIV transmission.
Additionally, the present study shows that HIV-infected women were more likely than their HIV-uninfected counterparts to have shared injection equipment across both their lifetime and the past 30 days than their HIV-uninfected counterparts (Table 4), suggesting that this could be driving onward transmission. Because HIV status was self-reported, however, it is also possible that these findings are the result of HIV screening policies targeting PWID; women who use drugs such as club drugs but do not inject may be less likely to be targeted for HIV screening despite being at high risk for sexual transmission.
4.2 Injected Substances
Regarding drug injection, heroin was the drug most likely to have ever been injected, with all women with prior drug injection, primarily of heroin, at least once in their lifetime. This finding underscores the high potential impact of OAT on reducing HIV transmission among women who inject drugs. Likewise, given the high levels of injection equipment sharing among HIV-infected women in the present study, deployment of OAT services, combined with NSEP for polysubstance users, would be one of the single most cost-effective measures for reducing onward transmission of HIV to uninfected women who inject drugs (72, 73).
4.3 Principal Components Analysis and Patterns of Drug Use
Results from the PCA of women’s drug use in the last 30 days revealed a clear pattern of use, with MDMA, cannabis, ketamine, and ATS constituting a component of “club drugs” and any opioids and benzodiazepines constituting the second component. These latent components may shed light on how women in Malaysia use drugs and could inform the design and implementation of interventions that target women’s drug use. Of particular importance, previous research on drug use among men in Malaysia suggests that opioids and benzodiazepines have been used together (58, 74, 75). Although further research is needed, this finding suggests that similar patterns may be occurring among women
4.4 Involvement of Women Drug Injectors with Criminal Justice System
Another strong correlation identified in the data was that of criminal justice involvement among active and lifetime PWID, both of whom were more likely to have been placed in prison and CDDCs than their non-injecting counterparts. Moreover, among those with a history of jail, lock-up or prison, 91.7% (N=88/96) reported having experienced this as a result of drug-related criminal charges. While we cannot conclude that all previous incarcerations were due to drug-related charges, these data suggest incarceration is not being used as an opportunity for deploying evidence-based interventions to identify at-risk persons and provide linkages to treatment and harm reduction services. Furthermore, CDDCs utilize a punitive approach to addressing substance use, fully lacking any evidence-based interventions, even standard healthcare services (63, 76).
4.5 High Use of Amphetamine-Type Substances (ATS)
Unlike most of the studies of male drug users in Malaysia (63, 65, 77), the prevalence of ATS use among women who use drugs is extraordinarily high and in the absence of medication-assisted treatments, remains largely unaddressed (59, 65). This difference in substance use patterns is also observed in Southeast Asia generally, where the estimated age-adjusted prevalence of ATS dependence among women is 0.31% (95% CI: 0.23–0.42), while prevalence of opioid dependence is over three times lower at 0.09% (95% CI: 0.06–0.13)(29). Since medication-assisted therapies are not routinely available for the treatment of ATS-use disorders (5), counseling-based strategies are the mainstay for treating amphetamine addiction. Recently in Malaysia, there has been a transformation from CDDCs to integrated voluntary drug treatment programs, including treatment for ATS (57, 60), that could play a role in engaging women who use drugs, including ATS, especially if that care is sensitive to the unique health needs of women.
4.6 Harm Reduction and Linkage to Opioid Agonist Maintenance Therapy
Not surprising, NSEP utilization was high among participants with a lifetime and active drug injection history. OAT utilization, however, was low and did not differ between injectors and non-injectors. OAT like methadone is one of the most effective evidence-based treatments for opioid dependence, which has been available in Malaysia since 2006 as part of a comprehensive national HIV prevention strategy (30) and has been deployed in several community-based settings and selected prisons (32, 33). While methadone has been introduced in some of the men’s prisons (32), Malaysia has unfortunately not initiated it in women’s prisons. Linkage to OAT and other harm reduction interventions is a critical component of a comprehensive strategy to address the medical needs of affected patients, as well as the larger issue of drug use, generally. Expansion of OAT in community-based settings that target services for at-risk women may improve linkage to medication-assisted treatment for substance use disorders. Likewise, scale-up of OAT in prison settings has been an important priority for Malaysia (32), however, for these treatments to achieve optimal impact, gender parity must be achieved.
One possible interpretation of the non-significant linkage of female PWID into OAT could be due to the lack of outreach services specifically targeting women. Evidence shows clear gender differences in reasons for initiating substance use treatment. For example, previous studies have found initiation of substance use treatment among men is more likely to be facilitated by family members, employment referrals, and the CJS, while women are more likely to be referred through a social worker (78). High rates of substance use during pregnancy further speaks to the need for gender-specific substance use interventions as women may find themselves being denied access to OAT during pregnancy. Moreover, they may avoid seeking drug treatment services out of fear that being identified as a drug user may lead to losing custody of their children.
5. Limitations
This pilot study was limited by convenience sampling, small sample size, and an under-representation of young women. Moreover, HIV status was self-reported without laboratory-based confirmation. Nevertheless, the exploratory nature of this study allowed for characterization of the unique substance use patterns, risk behaviors, and injection drug use correlations specific to women, laying the foundation for further research on women who use drugs.
6. Conclusions
ATS and heroin are the drugs most frequently used among this sample of 103 women in Malaysia. Opioid use during pregnancy in particular is a common and unaddressed problem. Women who inject drugs have high rates of equipment sharing and are more likely to be HIV-infected, which presents a high risk of either contracting HIV or transmitting HIV to others. Drug using women, especially those who inject drugs, also struggle with unstable social circumstances, including homelessness and exposure to physical and sexual violence. While these women have frequently interacted with CDDCs and the criminal justice system for drug-related offenses, they do not appear to be accessing adequate substance use treatment services including medication-assisted therapies. These findings illustrate an urgent need for substance use treatment strategies that target the unique needs of women in order to maximize treatment success and reduce HIV transmission in the general population. While further research is needed to better elucidate the substance use treatment needs of drug-using women, there appears to be a crucial need for access to OAT, social services, and counseling for substance use disorders, including ATS use as well as trauma from physical and sexual violence. Integration of substance use treatment with reproductive healthcare and mental health services should be further explored as a potential strategy for effectively targeting women who use drugs in Malaysia.
Acknowledgments
Funding: This research was supported by grants from the National Institute on Drug Abuse for research (R01 DA025943, Altice, PI) and career development awards (K24 DA017072 for Altice; K01 DA038529 for Wickersham) and University Malaya High Impact Research Grant (AK: E-000001-20001) and the National Institutes of Health Medical Scientist Training Program at Yale University (TG T32GM07205).
References
- 1.Degenhardt L, Whiteford H, Hall WD. The Global Burden of Disease projects: what have we learned about illicit drug use and dependence and their contribution to the global burden of disease? Drug Alcohol Rev. 2014;33(1):4–12. doi: 10.1111/dar.12088. [DOI] [PubMed] [Google Scholar]
- 2.United Nations Office on Drugs and Crime. World Drug Report 2014. New York: 2014. Accessed from: https://www.unodc.org/documents/wdr2014/World_Drug_Report_2014_web.pdf. [Google Scholar]
- 3.Berman S, O'Neill J, Fears S, Bartzokis G, London ED. Abuse of amphetamines and structural abnormalities in the brain. Ann N Y Acad Sci. 2008;1141:195–220. doi: 10.1196/annals.1441.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, Wodak A, Panda S, Tyndall M, Toufik A, Mattick RP. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372(9651):1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- 5.Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376(9738):367–387. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colfax G, Santos GM, Chu P, Vittinghoff E, Pluddemann A, Kumar S, Hart C. Amphetamine-group substances and HIV. Lancet. 2010;376(9739):458–474. doi: 10.1016/S0140-6736(10)60753-2. [DOI] [PubMed] [Google Scholar]
- 7.United Nations Economic and Social Council. Drug demand reduction: World situation with regard to drug abuse. Comission on Narcotic Drugs, 53rd Session. Vienna, Austria: 2009. [Accessed 1 July 2014]. https://www.unodc.org/documents/commissions/CND/CND_Sessions/CND_53/E-CN7-2010-2_V0989480_E.pdf. [Google Scholar]
- 8.UNAIDS. Malaysia 2012 Global AIDS Response Country Progress Report. 2012. [Google Scholar]
- 9.Session UNGAS. 2010 UNGASS Country Progress Report. Kuala Lumpur, Malaysia: UNAIDS; 2010. [Google Scholar]
- 10.United Nations Programme on HIV/AIDS (UNAIDS) Malaysia 2014 Country Progress Report. 2014. The Global AIDS Response Progress Report 2014: Malaysia. [Google Scholar]
- 11.United Nations Programme on HIV/AIDS [UNAIDS] Malaysia 2012 Country Progress Report. 2012 Accessed from: http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_MY_Narrative_Report.pdf 2012.
- 12.Kalichman SC, Williams EA, Cherry C, Belcher L, Nachimson D. Sexual coercion, domestic violence, and negotiating condom use among low-income African American women. Journal of women's health / the official publication of the Society for the Advancement of Women's Health Research. 1998;7(3):371–378. doi: 10.1089/jwh.1998.7.371. [DOI] [PubMed] [Google Scholar]
- 13.Collins RL, Ellickson PL, Orlando M, Klein DJ. Isolating the nexus of substance use, violence and sexual risk for HIV infection among young adults in the United States. AIDS Behav. 2005;9(1):73–87. doi: 10.1007/s10461-005-1683-2. [DOI] [PubMed] [Google Scholar]
- 14.Meyer JP, Springer SA, Altice FL. Substance abuse, violence, and HIV in women: a literature review of the syndemic. Journal of women's health (2002) 2011;20(7):991–1006. doi: 10.1089/jwh.2010.2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clum GA, Andrinopoulos K, Muessig K, Ellen JM. Child abuse in young, HIV-positive women: linkages to risk. Qual Health Res. 2009;19(12):1755–1768. doi: 10.1177/1049732309353418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El-Bassel N, Gilbert L, Wu E, Chang M, Gomes C, Vinocur D, Spevack T. Intimate partner violence prevalence and HIV risks among women receiving care in emergency departments: implications for IPV and HIV screening. Emergency medicine journal : EMJ. 2007;24(4):255–259. doi: 10.1136/emj.2006.041541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stockman JK, Campbell JC, Celentano DD. Sexual violence and HIV risk behaviors among a nationally representative sample of heterosexual American women: the importance of sexual coercion. J Acquir Immune Defic Syndr. 2010;53(1):136–143. doi: 10.1097/QAI.0b013e3181b3a8cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peles E, Adelson M. Gender differences and pregnant women in a methadone maintenance treatment (MMT) clinic. Journal of Addictive Diseases. 2006;25(2):39–45. doi: 10.1300/J069v25n02_06. [DOI] [PubMed] [Google Scholar]
- 19.Ellsberg M, Arango DJ, Morton M, Gennari F, Kiplesund S, Contreras M, Watts C. Prevention of violence against women and girls: what does the evidence say? The Lancet. doi: 10.1016/S0140-6736(14)61703-7. (0) [DOI] [PubMed] [Google Scholar]
- 20.Meyer JP, Wickersham JA, Fu JJ, Brown SE, Sullivan TP, Springer SA, Altice FL. Partner Violence and Health among HIV-Infected Jail Detainees. International journal of prisoner health. 2013;9(3):124–141. doi: 10.1108/IJPH-03-2013-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–48. doi: 10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- 22.Fulu E, Jewkes R, Roselli T, Garcia-Moreno C. Prevalence of and factors associated with male perpetration of intimate partner violence: findings from the UN Multi-country Cross-sectional Study on Men and Violence in Asia and the Pacific. The Lancet Global Health. 2013;1(4):e187–e207. doi: 10.1016/S2214-109X(13)70074-3. [DOI] [PubMed] [Google Scholar]
- 23.Organization WH. WHO Gender Policy. Geneva: World Health Organization; 2002. Available at: http://www.who.int/gender/documents/policy/en/ [Google Scholar]
- 24.Carael M, Marais H, Polsky J, Mendoza A. Is there a gender gap in the HIV response? Evaluating national HIV responses from the United Nations General Assembly Special Session on HIV/AIDS country reports. Journal of Acquired Immune Deficiency Syndromes. 2009;52(Suppl 2):S111–S118. doi: 10.1097/QAI.0b013e3181baeec2. [DOI] [PubMed] [Google Scholar]
- 25.El-Bassel N, Gilbert L, Wu E, Go H, Hill J. HIV and intimate partner violence among methadone-maintained women in New York City. Soc Sci Med. 2005;61(1):171–183. doi: 10.1016/j.socscimed.2004.11.035. [DOI] [PubMed] [Google Scholar]
- 26.Altice FL, Marinovich A, Khoshnood K, Blankenship KM, Springer SA, Selwyn PA. Correlates of HIV infection among incarcerated women: implications for improving detection of HIV infection. J Urban Health. 2005;82(2):312–326. doi: 10.1093/jurban/jti055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wagner KD, Jackson Bloom J, Hathazi SD, Sanders B, Lankenau SE. Control over Drug Acquisition, Preparation, and Injection: Implications for HIV and HCV Risk among Young Female Injection Drug Users. ISRN Addiction. 2013;2013:9. doi: 10.1155/2013/289012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Syvertsen JL, Robertson AM, Rolon ML, Palinkas LA, Martinez G, Rangel MG, Strathdee SA. "Eyes that don't see, heart that doesn't feel": coping with sex work in intimate relationships and its implications for HIV/STI prevention. Soc Sci Med. 2013;87:1–8. doi: 10.1016/j.socscimed.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Larney S, Mathers BM, Poteat T, Kamarulzaman A, Degenhardt L. Global Epidemiology of HIV Among Women and Girls Who Use or Inject Drugs: Current Knowledge and Limitations of Existing Data. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2015;69:S100–S109. doi: 10.1097/QAI.0000000000000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Noordin NM, Merican MI, Rahman HA, Lee SS, Ramly R. Substitution treatment in Malaysia. LANCET. 2008;372(9644):1149–1150. doi: 10.1016/S0140-6736(08)61479-8. [DOI] [PubMed] [Google Scholar]
- 31.Rashid RA, Kamali K, Habil MH, Shaharom MH, Seghatoleslam T, Looyeh MY. A mosque-based methadone maintenance treatment strategy: implementation and pilot results. Int J Drug Policy. 2014;25(6):1071–1075. doi: 10.1016/j.drugpo.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 32.Wickersham JA, Marcus R, Kamarulzaman A, Zahari MM, Altice FL. Implementing methadone maintenance treatment in prisons in Malaysia. Bulletin of the World Health Organization. 2013;91(2):124–129. doi: 10.2471/BLT.12.109132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wickersham JA, Zahari MM, Azar MM, Kamarulzaman A, Altice FL. Methadone dose at the time of release from prison significantly influences retention in treatment: implications from a pilot study of HIV-infected prisoners transitioning to the community in Malaysia. Drug Alcohol Depend. 2013;132(1–2):378–382. doi: 10.1016/j.drugalcdep.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Springer SA, Larney S, Alam-Mehrjerdi Z, Altice FL, Metzger D, Shoptaw S. Drug Treatment as HIV Prevention Among Women and Girls Who Inject Drugs From a Global Perspective: Progress, Gaps, and Future Directions. J Acquir Immune Defic Syndr. 2015;69:S155–S161. doi: 10.1097/QAI.0000000000000637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Degenhardt L, Mathers BM, Wirtz AL, Wolfe D, Kamarulzaman A, Carrieri MP, Strathdee SA, Malinowska-Sempruch K, Kazatchkine M, Beyrer C. What has been achieved in HIV prevention, treatment and care for people who inject drugs, 2010–2012? A review of the six highest burden countries. Int J Drug Policy. 2014;25(1):53–60. doi: 10.1016/j.drugpo.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 36.Bachireddy C, Bazazi AR, Kavasery R, Govindasamy S, Kamarulzaman A, Altice FL. Attitudes toward opioid substitution therapy and pre-incarceration HIV transmission behaviors among HIV-infected prisoners in Malaysia: implications for secondary prevention. Drug Alcohol Depend. 2011;116(1–3):151–157. doi: 10.1016/j.drugalcdep.2010.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Margolis B, Al-Darraji HA, Wickersham JA, Kamarulzaman A, Altice FL. Prevalence of tuberculosis symptoms and latent tuberculous infection among prisoners in northeastern Malaysia. Int J Tuberc Lung Dis. 2013;17(12):1538–1544. doi: 10.5588/ijtld.13.0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zahari MM, Hwan Bae W, Zainal NZ, Habil H, Kamarulzaman A, Altice FL. Psychiatric and substance abuse comorbidity among HIV seropositive and HIV seronegative prisoners in Malaysia. Am J Drug Alcohol Abuse. 2010;36(1):31–38. doi: 10.3109/00952990903544828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Malaysian AIDS Council. Understanding Women Who Use Drugs In Malaysia. Kuala Lumpur, Malaysia: 2014. [Google Scholar]
- 40.Wechsberg WM, Luseno W, Ellerson RM. Reaching women substance abusers in diverse settings: stigma and access to treatment 30 years later. Subst Use Misuse. 2008;43(8–9):1277–1279. doi: 10.1080/10826080802215171. [DOI] [PubMed] [Google Scholar]
- 41.Tucker JS, Wenzel SL, Golinelli D, Zhou A, Green HD. Predictors of Substance Abuse Treatment Need and Receipt Among Homeless Women. Journal of substance abuse treatment. 2011;40(3):287–294. doi: 10.1016/j.jsat.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vijay A, Bazazi AR, Yee I, Kamarulzaman A, Altice FL. Treatment readiness, attitudes toward, and experiences with methadone and buprenorphine maintenance therapy among people who inject drugs in Malaysia. J Subst Abuse Treat. 2015;54:29–36. doi: 10.1016/j.jsat.2015.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brislin RW. Back-Translation for Cross-Cultural Research. J Cross-Cultural Psych. 1970;1:185–216. [Google Scholar]
- 44.Chwastiak L, Ehde DM, Gibbons LE, Sullivan M, Bowen JD, Kraft GH. Depressive symptoms and severity of illness in multiple sclerosis: epidemiologic study of a large community sample. The American journal of psychiatry. 2002;159(11):1862–1868. doi: 10.1176/appi.ajp.159.11.1862. [DOI] [PubMed] [Google Scholar]
- 45.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- 46.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System (BRFSS) Questionnaire. Atlanta, GA: CDC; 2006. [Google Scholar]
- 47.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 48.Singh D, Müller CP, Vicknasingam BK. Kratom (Mitragyna speciosa) dependence, withdrawal symptoms and craving in regular users. Drug and Alcohol Dependence. 2014;139(0):132–137. doi: 10.1016/j.drugalcdep.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 49.Hassan Z, Muzaimi M, Navaratnam V, Yusoff NH, Suhaimi FW, Vadivelu R, Vicknasingam BK, Amato D, von Horsten S, Ismail NI, Jayabalan N, Hazim AI, Mansor SM, Muller CP. From Kratom to mitragynine and its derivatives: physiological and behavioural effects related to use, abuse, and addiction. Neurosci Biobehav Rev. 2013;37(2):138–151. doi: 10.1016/j.neubiorev.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 50.Adkins JE, Boyer EW, McCurdy CR. Mitragyna speciosa, a psychoactive tree from Southeast Asia with opioid activity. Curr Top Med Chem. 2011;11(9):1165–1175. doi: 10.2174/156802611795371305. [DOI] [PubMed] [Google Scholar]
- 51.Hatta ZA, Ali I. Poverty Reduction Policies in Malaysia: Trends, Strategies and Challenges Asian Culture and History. 2013;5(2) [Google Scholar]
- 52.Mat Zin R. Measuring and monitoring poverty and inequality: The Malaysian experience. Singapore: Institute of Southeast Asian Studies; 2011. [Google Scholar]
- 53.IBM Corp. IBM SPSS Statistics for Windows, Version 22. Armonk, NY: IBM Corp.; 2013. [Google Scholar]
- 54.Loeliger KB, Marcus R, Wickersham JA, Pillai V, Kamarulzaman A, Altice FL. The Syndemic of HIV, HIV-related Risk and Multiple Co-morbidities Among Women Who Use Drugs in Malaysia: Important Targets for Intervention Addict Behav. 2015 doi: 10.1016/j.addbeh.2015.09.013. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vicknasingam B, Narayanan S, Navaratnam V. Prevalence rates and risk factors for hepatitis C among drug users not in treatment in Malaysia. Drug and Alcohol Review. 2009;28(4):447–454. doi: 10.1111/j.1465-3362.2009.00087.x. [DOI] [PubMed] [Google Scholar]
- 56.Vicknasingam B, Navaratnam V. The use of rapid assessment methodology to compliment existing national assessment and surveillance data: a study among injecting drug users in Penang, Malaysia. Int J Drug Policy. 2008;19(1):90–93. doi: 10.1016/j.drugpo.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 57.Khan F, Krishnan A, Ghani M, Wickersham JA, Fu J, Lim H, Kamarulzaman A, Altice FL. Assessment of an Innovative Voluntary Substance Abuse Treatment Program Designed to Transition from Compulsory Drug Detention Centers in Malaysia Subst Use Misuse. 2015 doi: 10.1080/10826084.2016.1267217. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vicknasingam B, Mazlan M, Schottenfeld RS, Chawarski MC. Injection of buprenorphine and buprenorphine/naloxone tablets in Malaysia. Drug Alcohol Depend. 2010;111(1–2):44–49. doi: 10.1016/j.drugalcdep.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 59.Al-Darraji HA, Wong KC, Yeow DG, Fu JJ, Loeliger K, Paiji C, Kamarulzaman A, Altice FL. Tuberculosis screening in a novel substance abuse treatment center in Malaysia: Implications for a comprehensive approach for integrated care. J Subst Abuse Treat. 2013 doi: 10.1016/j.jsat.2013.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ghani MA, Brown SE, Khan F, Wickersham JA, Lim SH, Dhaliwal SK, Kamarulzaman A, Altice FL. An exploratory qualitative assessment of self-reported treatment outcomes and satisfaction among patients accessing an innovative voluntary drug treatment centre in Malaysia. Int J Drug Policy. 2015;26(2):175–182. doi: 10.1016/j.drugpo.2014.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Al-Darraji HAA, Wickersham JA, Kamarulzaman A, Altice FL. Prevalence and Correlates of Positive Tuberculin Skin Test Reaction Among HIV-infected Prisoners in Malaysia: Implications for Tuberculosis Prophylaxis and Antiretroviral Therapy. AIDS Patient Care STDS. 2014 In Press. [Google Scholar]
- 62.Al-Darraji HA, Kamarulzaman A, Altice FL. Latent tuberculosis infection in a Malaysian prison: implications for a comprehensive integrated control program in prisons. BMC Public Health. 2014;14(1):22. doi: 10.1186/1471-2458-14-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fu JJ, Bazazi AR, Altice FL, Mohamed MN, Kamarulzaman A. Absence of antiretroviral therapy and other risk factors for morbidity and mortality in Malaysian compulsory drug detention and rehabilitation centers. PLoS One. 2012;7(9):e44249. doi: 10.1371/journal.pone.0044249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Choi P, Kavasery R, Desai MM, Govindasamy S, Kamarulzaman A, Altice FL. Prevalence and correlates of community re-entry challenges faced by HIV-infected male prisoners in Malaysia. Int J STD AIDS. 2010;21(6):416–423. doi: 10.1258/ijsa.2009.009180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bazazi AR, Zelenev A, Fu JJ, Yee I, Kamarulzaman A, Altice FL. High prevalence of non-fatal overdose among people who inject drugs in Malaysia: Correlates of overdose and implications for overdose prevention from a cross-sectional study. Int J Drug Policy. 2015;26(7):675–681. doi: 10.1016/j.drugpo.2014.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Campbell AN, Tross S, Dworkin SL, Hu MC, Manuel J, Pavlicova M, Nunes EV. Relationship power and sexual risk among women in community-based substance abuse treatment. J Urban Health. 2009;86(6):951–964. doi: 10.1007/s11524-009-9405-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.El-Bassel N, Gilbert L, Witte S, Wu E, Chang M. Intimate Partner Violence and HIV Among Drug-Involved Women: Contexts Linking These Two Epidemics--Challenges and Implications for Prevention and Treatment. Substance Use & Misuse. 2011;46(2/3):295–306. doi: 10.3109/10826084.2011.523296. [DOI] [PubMed] [Google Scholar]
- 68.Raj A, Silverman JG, Amaro H. Abused women report greater male partner risk and gender-based risk for HIV: findings from a community-based study with Hispanic women. AIDS Care. 2004;16(4):519–529. doi: 10.1080/09540120410001683448. [DOI] [PubMed] [Google Scholar]
- 69.Kamarulzaman A. Impact of HIV Prevention Programs on Drug Users in Malaysia. Journal of Acquired Immune Deficiency Syndromes. 2009;52:S17–S19. doi: 10.1097/QAI.0b013e3181bbc9af. [DOI] [PubMed] [Google Scholar]
- 70.Battjes RJ, Pickens RW, Haverkos HW, Sloboda Z. HIV risk factors among injecting drug users in five US cities. Aids. 1994;8(5):681–687. doi: 10.1097/00002030-199405000-00016. [DOI] [PubMed] [Google Scholar]
- 71.Hien NT, Giang LT, Binh PN, Deville W, van Ameijden EJ, Wolffers I. Risk factors of HIV infection and needle sharing among injecting drug users in Ho Chi Minh City, Vietnam. J Subst Abuse. 2001;13(1–2):45–58. doi: 10.1016/s0899-3289(01)00059-1. [DOI] [PubMed] [Google Scholar]
- 72.Vickerman P, Platt L, Jolley E, Rhodes T, Kazatchkine MD, Latypov A. Controlling HIV among people who inject drugs in Eastern Europe and Central Asia: Insights from modelling. Int J Drug Policy. 2014;25(6):1163–1173. doi: 10.1016/j.drugpo.2014.09.013. [DOI] [PubMed] [Google Scholar]
- 73.Alistar SS, Owens DK, Brandeau ML. Effectiveness and cost effectiveness of expanding harm reduction and antiretroviral therapy in a mixed HIV epidemic: a modeling analysis for Ukraine. PLoS Med. 2011;8(3):e1000423. doi: 10.1371/journal.pmed.1000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bruce RD, Govindasamy S, Sylla L, Kamarulzaman A, Altice FL. Lack of reduction in buprenorphine injection after introduction of co-formulated buprenorphine/naloxone to the Malaysian market. Am J Drug Alcohol Abuse. 2009;35(2):68–72. doi: 10.1080/00952990802585406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bruce RD, Govindasamy S, Sylla L, Haddad MS, Kamarulzaman A, Altice FL. Case series of buprenorphine injectors in Kuala Lumpur, Malaysia. Am J Drug Alcohol Abuse. 2008;34(4):511–517. doi: 10.1080/00952990802122259. [DOI] [PubMed] [Google Scholar]
- 76.Amon JJ, Pearshouse R, Cohen JE, Schleifer R. Compulsory drug detention in East and Southeast Asia: evolving government, UN and donor responses. Int J Drug Policy. 2014;25(1):13–20. doi: 10.1016/j.drugpo.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 77.Degenhardt L, Charlson F, Mathers B, Hall WD, Flaxman AD, Johns N, Vos T. The global epidemiology and burden of opioid dependence: results from the global burden of disease 2010 study. Addiction. 2014;109(8):1320–1333. doi: 10.1111/add.12551. [DOI] [PubMed] [Google Scholar]
- 78.Grella CE, Joshi V. Gender differences in drug treatment careers among clients in the national Drug Abuse Treatment Outcome Study. Am J Drug Alcohol Abuse. 1999;25(3):385–406. doi: 10.1081/ada-100101868. [DOI] [PubMed] [Google Scholar]