Abstract
Introduction:
Little is known about the pattern of electronic cigarette (e-cigarette) use over time or among smokers with medical comorbidity.
Methods:
We assessed current cigarette smokers’ use of e-cigarettes during the 30 days before admission to 9 hospitals in 5 geographically dispersed US cities: Birmingham, AL; Boston, MA; Kansas City, KS; New York, NY; and Portland, OR. Each hospital was conducting a randomized controlled trial as part of the NIH-sponsored Consortium of Hospitals Advancing Research on Tobacco (CHART). We conducted a pooled analysis using multiple logistic regression to examine changes in e-cigarette use over time and to identify correlates of e-cigarette use.
Results:
Among 4,660 smokers hospitalized between July 2010 and December 2013 (mean age 57 years, 57% male, 71% white, 56% some college, average 14 cigarettes/day), 14% reported using an e-cigarette during the 30 days before admission. The prevalence of e-cigarette use increased from 1.1% in 2010 to 10.3% in 2011, 10.2% in 2012, and 18.4% in 2013; the increase was statistically significant (p < .0001) after adjustment for age, sex, education, and CHART study. Younger, better educated, and heavier smokers were more likely to use e-cigarettes. Smokers who were Hispanic, non-Hispanic black, and who had Medicaid or no insurance were less likely to use e-cigarettes. E-cigarette use also varied by CHART project and by geographic region.
Conclusions:
E-cigarette use increased substantially from 2010 to 2013 among a large sample of hospitalized adult cigarette smokers. E-cigarette use was more common among heavier smokers and among those who were younger, white, and who had higher socioeconomic status.
Introduction
Electronic cigarettes (e-cigarettes) are devices that deliver a nicotine-containing vapor to the user without combusting tobacco.1,2 E-cigarettes are likely to be less hazardous to an individual than continuing to smoke conventional cigarettes, but what impact the availability of e-cigarettes will have on overall public health is unknown and controversial.3 Invented in China in 2003, e-cigarettes are now sold globally. Most adult e-cigarette users are also cigarette smokers.2,4,5 In the United States, the prevalence of e-cigarette use appears to be increasing among both adults and adolescents, although data from population-based surveys are sparse.2,4–9 Most of the estimates of adult use derive from surveys conducted in 2009–2011. E-cigarette sales and marketing increased dramatically after those years, but few US data are available on the prevalence of e-cigarette use after 2011.
There are also few data on the prevalence of e-cigarette use among smokers with medical illnesses, especially those who require a hospital admission. Hospitalized smokers are a vulnerable group who, if they cannot abstain from tobacco completely, might achieve harm reduction by switching from combustible tobacco products to exclusive use of e-cigarettes.3 To our knowledge, only one prior study has examined the use of e-cigarettes by hospitalized smokers.10 In that study, 20% of smokers reported having used an e-cigarette in the 30 days before admission to a large Alabama tertiary-care hospital over a period of 6 months in 2012–2013. E-cigarette use was higher among smokers who were younger, white, and better educated. These data need confirmation in a broader sample that includes a wider range and larger number of US hospitals. Additionally, data collected over a longer time period would permit an analysis of changes in e-cigarette use over time in this group of smokers.
This paper describes the prevalence of current e-cigarette use among adults who were admitted to nine acute-care hospitals in five geographically dispersed US cities (Birmingham, AL; Boston, MA; Kansas City, KS; New York, NY; and Portland, OR) over 3.5 years, from July 2010 to December 2013. The hospitals were participating in the Consortium of Hospitals Advancing Research on Tobacco (CHART), a group of NIH-funded randomized controlled trials that aims to translate efficacious smoking cessation strategies begun during hospitalization and sustained after discharge into effective programs that can be implemented in routine clinical practice.11 As part of the baseline assessment, study patients enrolled at five CHART project sites were asked if they had used an electronic cigarette in the 30 days before hospital admission. We pooled the data to test the hypothesis that the prevalence of e-cigarette use increased over the study period. The analysis also compared the characteristics of smokers who did and did not use e-cigarettes.
Methods
Setting and Subjects
The CHART program is jointly sponsored by the National Heart, Lung, and Blood Institute, National Cancer Institute, National Institute on Drug Abuse, and NIH Office of Behavioral and Social Science Research.11 CHART consists of eight NIH-funded randomized controlled trials that enroll hospitalized cigarette smokers and test a variety of interventions that begin in the hospital and continue after discharge. Each CHART project compares a distinct intervention against a usual care control group. The projects have similar eligibility criteria and collect a core set of common baseline and outcome measures in order to permit cross-project analyses and pooling of results.11 All patients are enrolled during their hospitalization, provide informed consent, and complete a baseline survey at the bedside before being randomly assigned to study condition. All projects enroll hospitalized current smokers, defined as any patient who reports having smoked a cigarette in the 30 days before hospital admission. CHART projects aim to be inclusive, generally excluding only smokers unable to grant informed consent or participate in the intervention due to severe medical illness, cognitive impairment, or communication difficulties.11 CHART projects differ in the population of patients served by the participating hospitals, in some inclusion criteria such as motivation to quit, and in the specific intervention tested.
In addition to the common baseline questions, four of the CHART projects, which enrolled smokers at a total of eight hospitals, asked a question about their use of e-cigarettes in the 30 days before hospital admission.12–15 Another CHART project collected data on e-cigarette use among hospitalized smokers as part of a supplemental grant that enrolled patients separately from the main intervention trial.10 These five projects pooled their data for this analysis.
Participating CHART projects enrolled patients at their hospitals during a 3.5-year observation period (July 2010 to December 2013) (Table 1). One project (New York) continued enrollment after December 31, 2013, but data for this analysis were truncated at that point to permit pooling and analysis. Each project’s Institutional Review Board permitted de-identified data to be shared across the CHART projects and merged into a common data set.
Table 1.
Characteristics of the CHART Study Sites Contributing Patients to the Pooled Analysis
| Study site and e-cigarette questiona | N | Hospital site | N | Period of enrollment | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | ||||||||||||||
| Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||||
| All | 4,660 | All | 4,660 | 21 | 67 | 62 | 48 | 156 | 314 | 519 | 542 | 446 | 393 | 685 | 654 | 557 | 196 |
| Boston, MA | 397 | Massachusetts General Hospital | 397 | X | X | X | X | X | X | X | X | ||||||
| Kansas City, KS | 1,054 | University of Kansas Medical Center | 873 | X | X | X | X | X | X | X | X | ||||||
| Stormont Vail Health Care | 181 | X | X | X | X | X | X | X | X | ||||||||
| New York, NY | 1,330 | Bellevue Hospital Center | 903 | X | X | X | X | X | X | X | X | X | X | ||||
| VA New York Harbor Healthcare System | 427 | X | X | X | X | X | X | X | X | X | |||||||
| Portland, OR | 900 | Kaiser Permanente SMC | 624 | X | X | X | X | X | X | X | X | X | |||||
| Oregon Health Sciences University Hospital | 81 | X | X | X | |||||||||||||
| Legacy Emmanuel Hospital | 195 | X | X | X | X | X | |||||||||||
| Birmingham, AL | 979 | UAB Hospital | 979 | X | X | X | X | ||||||||||
CHART = Consortium of Hospitals Advancing Research on Tobacco.
aQuestion about electronic cigarette used at each site:
New York, Massachusetts: In the past month, have you used the electronic cigarette (also called an e-cigarette?)
Kansas: In the past 30 days, on how many days did you smoke the electronic cigarette?
Alabama: In the past 30 days, have you used an electronic cigarette (also called an e-cigarette)?
Oregon: Did you use any other tobacco product besides cigarettes in the past 30 days (including electronic cigarettes)? What products did you use? (Mark yes or no for each item) Response categories included: Electronic cigarettes.
Measures/Assessments
The dependent variable was self-report of having used one or more electronic cigarettes in the 30 days before the hospital admission. The questions asked by each CHART project were not identical but were sufficiently similar to permit pooling. The exact wording of each question is shown in the footnote of Table 1.
The core measures collected by all projects have previously been described.11 For this analysis, we used the following measures as covariates: enrollment date, age, sex, race/ethnicity, marital status, educational attainment, health insurance, type of admission (emergency room vs. other), number of cigarettes per day before admission, and whether the smoker planned to quit smoking after discharge.
Data Analysis
We pooled data from the five projects and used chi square tests or analysis of variance techniques to compare characteristics of patients across the studies. We calculated the proportion of patients enrolled who reported using an e-cigarette in the 30 days before hospital admission. To identify predictors of e-cigarette use prior to hospital admission, we used chi square tests for the univariate analysis and a multiple logistic regression model for the multivariable analysis. Potential predictors in the multivariate model included age, sex, race/ethnicity, education, health insurance, cigarettes per day, enrollment date, and CHART project. In separate models, we replaced the CHART project variable with a variable indicating the individual hospital site or the geographical region (Northeast, Midwest, South, West). We explored regional differences to see if e-cigarette use rates, such as conventional cigarette smoking rates, vary by geographic region in the United States. A two-sided p value <0.05 was considered statistically significant. All analyses were done using SAS version 9.3 (SAS Institute).
Results
Study Sample
Baseline data on the use of e-cigarettes in the 30 days before hospital admission were collected from 4,660 current cigarette smokers who were admitted to nine participating study hospital sites between July 2010 and December 2013. Several projects had more than one hospital site. Table 1 shows the number of smokers enrolled by each CHART project, at each hospital, and the dates of enrollment at each hospital site.
Baseline Characteristics
Patient characteristics varied across the CHART projects, reflecting the variability in populations served by the hospitals participating in each project (Table 2). Statistically significant differences across projects were observed in age, sex, race, education, marital status, health insurance, type of admission, and intention to quit after discharge (all p < .0001). Most admissions were emergency admissions rather than elective (pre-planned) admissions. The mean number of cigarettes smoked per day ranged from 13 to 17 across projects. The large majority of patients planned to quit or try to quit smoking after discharge, even in the New York project where this commitment was not required for study enrollment.
Table 2.
Characteristics of Study Patients, by Project*
| Characteristic | All | Oregon | New York | Alabama | Kansas | Mass |
|---|---|---|---|---|---|---|
| N = 4,660 | N = 900 | N = 1,330 | N = 979 | N = 1,054 | N = 397 | |
| Age, M (SD) | 49 (13) | 53 (13) | 48 (13) | 45 (13) | 49 (13) | 53 (12) |
| Sex, % male | 57 | 46 | 78 | 54 | 45 | 49 |
| Race/ethnicity, % | ||||||
| Non-Hispanic white | 53 | 71 | 22 | 55 | 65 | 81 |
| Non-Hispanic black | 25 | 9 | 32 | 42 | 24 | 4 |
| Hispanic | 13 | 5 | 34 | 1 | 6 | 6 |
| Other | 9 | 16 | 12 | 2 | 5 | 9 |
| Education, % | ||||||
| Less than high school | 20 | 12 | 25 | 22 | 22 | 12 |
| High school diploma/GED | 34 | 31 | 28 | 38 | 36 | 39 |
| Some college | 34 | 42 | 32 | 32 | 33 | 32 |
| College graduate | 12 | 14 | 15 | 8 | 9 | 16 |
| Married, % | 34 | 46 | 22 | 31 | 37 | 50 |
| Health insurance, % | ||||||
| Commercial | 27 | 52 | 6 | 20 | 29 | 48 |
| Medicare | 22 | 23 | 11 | 25 | 30 | 27 |
| Medicaid | 21 | 9 | 20 | 22 | 34 | 14 |
| Self-pay/none | 13 | 4 | 17 | 29 | 6 | 3 |
| VA/other public | 11 | 0 | 32 | 4 | 1 | 5 |
| Missing | 7 | 12 | 14 | 0 | 0 | 4 |
| Cigarettes/day, mean (SD) | 14 (10) | 13 (9) | 12 (10) | 13 (10) | 16 (11) | 17 (10) |
| Admitted from emergency room, % | 61 | 18 | 76 | 76 | 60 | 74 |
| Post-discharge plan for smoking, %a | ||||||
| Stay quit | 42 | 64 | 28 | — | 44 | 33 |
| Try to quit | 50 | 30 | 54 | 56 | 67 | |
| Do not know | 6 | 5 | 13 | 0 | 0 | |
| Do not plan to quit | 2 | 0 | 5 | 0 | 0 |
GED = General Educational Development certificate; VA = Veterans’ Administration; CHART = Consortium of Hospitals Advancing Research on Tobacco.
aThe New York CHART project enrolled all hospitalized smokers, regardless of intention to quit after discharge. This variable was not available in the Alabama data. The other three sites required smokers to plan to quit after discharge.
* p < .0001 for differences across sites for every variable in the table.
Electronic Cigarette Use Before Hospital Admission
Overall, 14% of all patients admitted between July 2010 and December 2013 reported having used an e-cigarette in the 30 days prior to their hospital admission. The univariate analysis of factors associated with past 30-day e-cigarette use is shown in Table 3. E-cigarette use varied by the patient characteristics of age (p < .0001), race/ethnicity (p < .0001), education (p = .0002), and cigarettes smoked per day (p = .006) (Table 3). E-cigarette use did not vary by sex, marital status, or type of admission (emergency vs. elective). The association with health insurance status had marginal statistical significance (p = .073) (Table 3).
Table 3.
Factors Associated With Electronic Cigarette Use in the 30 Days Before Hospital Admission, Univariate Analysis
| Characteristic | N = 4,660 | Used e-cigarette (%) | p |
|---|---|---|---|
| Year of enrollment | |||
| 2010 | 88 | 1.1 | <.0001 |
| 2011 | 580 | 10.3 | |
| 2012 | 1,900 | 10.2 | |
| 2013 | 2,092 | 18.4 | |
| Age (years), % | |||
| <25 | 3 | 22.2 | <.0001 |
| 25–44 | 216 | 16.9 | |
| 45–64 | 1,323 | 12.1 | |
| 65 or more | 2,598 | 10.0 | |
| Sex, % | |||
| Male | 2,658 | 14.3 | .14 |
| Female | 1,989 | 12.8 | |
| Race/ethnicity, % | |||
| Non-Hispanic white | 2,482 | 15.6 | <.0001 |
| Non-Hispanic black | 1,180 | 9.7 | |
| Hispanic | 600 | 14.0 | |
| Other | 398 | 13.3 | |
| Education, % | |||
| Less than high school | 935 | 10.2 | .0002 |
| High school diploma/GED | 1,565 | 13.2 | |
| Some college or more | 2,148 | 15.6 | |
| Marital status, % | |||
| Married/partner | 1,598 | 13.5 | .45 |
| Other | 2,845 | 14.3 | |
| Health insurance, % | |||
| Commercial | 1,247 | 14.0 | .073 |
| Medicare | 1,005 | 12.6 | |
| Medicaid | 977 | 11.9 | |
| Self-pay/none | 627 | 13.1 | |
| VA/ other public | 492 | 17.1 | |
| Missing | 312 | 17.6 | |
| Cigarettes/day, % | |||
| Less than 10 | 1,635 | 11.8 | .006 |
| 10 or more | 3,020 | 14.7 | |
| Plan about smoking after discharge, % | |||
| Plan to stay quit | 1,589 | 10.6 | .014 |
| Plan to try to quit | 1,953 | 14.2 | |
| Do not know | 260 | 13.5 | |
| Do not plan to quit | 68 | 11.8 | |
| Missing | 790 | ||
| Admitted from emergency room, % | |||
| Yes | 2,846 | 14.1 | .24 |
| No | 1,632 | 12.9 | |
| Geographic region | |||
| South | 979 | 20.9 | <.0001 |
| Northeast | 1,727 | 14.3 | |
| Midwest | 1,054 | 12.3 | |
| West | 900 | 6.2 | |
| CHART project | |||
| Alabama | 979 | 20.9 | <.0001 |
| New York | 1,330 | 16.8 | |
| Kansas | 1,054 | 12.3 | |
| Massachusetts | 397 | 5.8 | |
| Oregon | 900 | 6.2 | |
| Hospital site | |||
| UAB Hospital (AL) | 979 | 20.9 | <.0001 |
| Bellvue Hospital Center (NY) | 903 | 18.1 | |
| VA New York Harbor (NY) | 427 | 14.3 | |
| University of Kansas Med Center (KS) | 873 | 12.7 | |
| Stormont Vail Health Care (KS) | 181 | 10.5 | |
| Kaiser Permanente SMC (OR) | 624 | 7.1 | |
| Massachusetts General Hospital (MA) | 397 | 5.8 | |
| Legacy Emmanuel Hospital (OR) | 81 | 5.1 | |
| Oregon Health Sciences University Hospital (OR) | 195 | 2.5 |
GED = General Educational Development certificate; VA = Veterans’ Administration; CHART = Consortium of Hospitals Advancing Research on Tobacco.
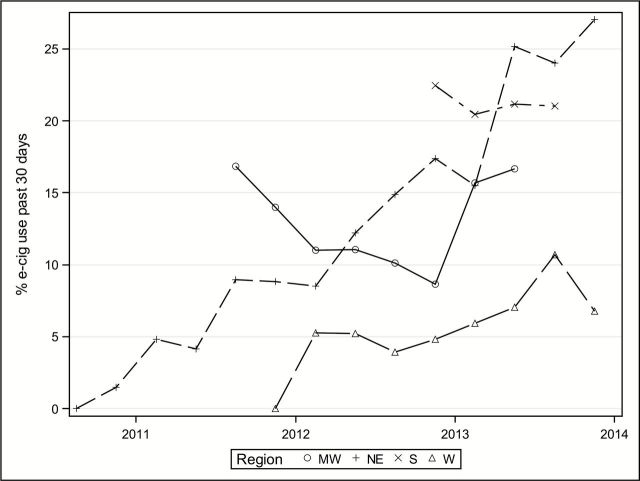
The unadjusted prevalence of e-cigarette use increased over time, from 1.1% in the last half of 2010 to 10.3% in 2011, 10.2% in 2012, and 18.4% in 2013 (p < .0001)(Table 3). E-cigarette use varied widely among the eight hospital sites (3%–21%, p < .0001)(Table 3), among the five CHART projects (6% in Oregon and Massachusetts to 21% in Alabama, p < .0001), and across four geographic regions (Table 3). E-cigarette use over time by region is shown in Figure 1.
Figure 1.
Variation in past 30-day use of electronic cigarettes, by geographic region and time. MW = Midwest (Kansas), NE = Northeast (Boston, New York), S = South (Alabama), W = West (Portland).
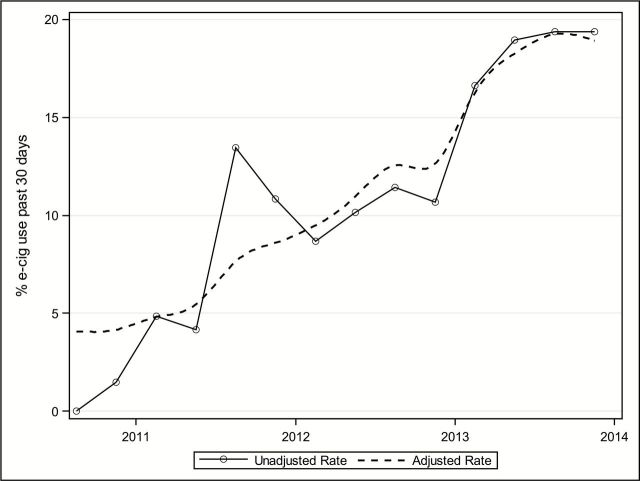
Figure 2 displays the rate of e-cigarette use among patients by their date of enrollment, showing the results of both an unadjusted analysis and a multivariate analysis adjusting for CHART project site, age, race, and education. It demonstrates a steady increase in the prevalence of e-cigarette use among hospitalized smokers enrolled in the CHART projects. The slope of the change in prevalence over time is non-zero in the adjusted analysis (p = .0001).
Figure 2.
Prevalence of electronic cigarette use in the 30 days before hospital admission, 2010–2013. Unadjusted rate plots e-cigarette use by calendar quarters. Adjusted rate plots e-cigarette use over time, adjusted for age, sex, race, education, and study site; p value <.001 for test that slope = 0
Factors independently associated with e-cigarette use in the 30 days before hospital admission were identified in a pooled multiple logistic regression analysis that adjusted for age, sex, race, education, insurance, CHART project site, and year of enrollment (Table 4). Younger smokers (<45 years), heavier smokers (≥10 cigarettes daily), and those with more education (high school diploma or more) were more likely to have used an e-cigarette in the 30 days before hospital admission, controlling for other factors. In contrast, e-cigarette use was lower among Hispanics and non-Hispanic blacks (compared with that among non-Hispanic whites) and among smokers with Medicaid or no insurance (compared with those with commercial insurance). Rates of e-cigarette use did not vary by sex, marital status, or type of admission (emergency vs. elective).
Table 4.
Factors Associated With Electronic Cigarette Use in the 30 Days Before Hospital Admission, Multiple Logistic Regression Analyses
| Characteristic | Multiple logistic regressiona | |
|---|---|---|
| OR | 95% CI | |
| Age (years), % | ||
| <25 | 2.02 | 1.24–3.29 |
| 25–44 | 1.56 | 1.08–2.25 |
| 45–64 | 1.18 | 0.84–1.67 |
| 65 or more | 1.00 | REF |
| Sex, % | ||
| Male | 0.99 | 0.82–1.19 |
| Female | 1.00 | REF |
| Race/ethnicity, % | ||
| Non-Hispanic white | 1.00 | REF |
| Non-Hispanic black | 0.42 | 0.33–0.53 |
| Hispanic | 0.66 | 0.49–0.90 |
| Other | 0.80 | 0.57–1.13 |
| Education, % | ||
| Less than high school diploma | 1.00 | REF |
| High school diploma/GED | 1.41 | 1.08–1.84 |
| Some college or more | 1.69 | 1.31–2.18 |
| Health insurance, % | ||
| Commercial | 1.00 | REF |
| Medicare | 0.92 | 0.69–1.21 |
| Medicaid | 0.70 | 0.53–0.92 |
| Self-pay/none | 0.52 | 0.38–0.71 |
| VA/ other public | 0.94 | 0.66–1.34 |
| Missing | 1.00 | 0.67–1.50 |
| Cigarettes/day, % | ||
| Less than 10 | 1.00 | REF |
| 10 or more | 1.24 | 1.02–1.51 |
| CHART project | ||
| Alabama | 3.68 | 2.06–6.56 |
| New York | 3.87 | 2.19–6.85 |
| Kansas | 2.34 | 1.40–3.93 |
| Oregon | 0.79 | 0.44–1.42 |
| Massachusetts | 1.0 | REF |
| Year of enrollment | ||
| 2010 | 0.10 | 0.01–0.78 |
| 2011 | 0.70 | 0.48–1.02 |
| 2012 | 0.57 | 0.45–0.72 |
| 2013 | 1.0 | REF |
OR = odds raio; CI = confidence interval; GED = General Educational Development certificate; CHART = Consortium of Hospitals Advancing Research on Tobacco. Values in bold are statistically significant at p < .05.
aMultiple logistic regression analysis adjusted for the other factors listed in the table. In separate models that replaced project with individual hospital site or geographic region, the odds ratios changed minimally and statistical significance of variables remained the same (data not shown).
E-cigarette use also varied in the multivariate analysis by CHART project (Table 4). It was higher in Alabama, Kansas, and New York, compared with that in Massachusetts and Oregon. The adjusted odds ratios and 95% confidence limits in the multivariate analysis changed minimally when the CHART project variable was replaced with individual hospital site (data not shown). The results shown in Table 4 were also minimally changed by replacing project with geographic region. In that model, compared to the Northeast, the prevalence of e-cigarette use was lower in the West (adjusted odds ratio [AOR] = 0.27, 95% confidence interval [CI] = 0.19–0.39) and nonsignificantly different in the Midwest (AOR = 0.89, 95% CI = 0.67–1.18) and South (AOR = 1.17, 95% CI = 0.87–1.58).
Discussion
This analysis of data from 4,660 cigarette smokers admitted to nine hospitals in five US cities found a substantial increase in the prevalence of current (past 30-day) e-cigarette use during a 3.5-year period from 2010 to 2013. By 2013, 18% of hospitalized cigarette smokers reported having used an e-cigarette in the month before hospital admission. Younger, better educated, and heavier smokers were more likely to use e-cigarettes, whereas Hispanics, non-Hispanic blacks, and smokers with Medicaid or no insurance were less likely to have used an e-cigarette. These results confirm and extend the results of a previous report of 657 smokers in one Alabama hospital whose results are included in the current analysis.10 That study reported a 20% prevalence of e-cigarette use in 2013 and identified similar patient-level factors that were independently associated with e-cigarette use—younger age, more education, white race, and having commercial health insurance or Medicare.
The trends identified in this subgroup of smokers admitted to a hospital appear to reflect trends in the broader US population. Prior studies of e-cigarette use in national samples of US adults reported a low but increasing rate of current use in the range of 1%–8% between 2009 and 2011.4,5,7–9 Our study population had a comparably low rate of current e-cigarette use in 2010, but the rate increased consistently and dramatically through 2013. To our knowledge, no other estimate of e-cigarette use in the United States during these years has been published. The demographic characteristics of e-cigarette users in our survey resembled those identified from most of the national surveys of adult smokers. In those surveys, e-cigarette users were more likely to be younger, white, better educated, and heavier smokers.5,7–9 Our study, like others, found no gender difference in e-cigarette use. The greater use of e-cigarettes by heavier smokers may reflect their appeal as harm reduction devices to smokers who are more nicotine addicted. In many states, e-cigarettes are more expensive than a pack of conventional cigarettes, which may explain the lower use rates among those with less education and those on Medicaid insurance or having no insurance. Finally, e-cigarette marketing appears to be designed to appeal to youth,2 which may explain why the use rates are higher among young people. Future research should explore the factors that explain the demographic and geographic differences that we and others have observed.
Prior studies have not reported on geographic differences in e-cigarette use. In our study, e-cigarette use varied by CHART project and by geographic region, being less frequent in the West, compared with that in the Northeast, Midwest, or South. This may reflect local differences in the availability or marketing of e-cigarettes or other social or environmental factors. However, the finding of a regional difference should be interpreted with caution. There was only one CHART project in three of the four geographic regions, making it impossible to separate between project and regional differences. Additionally, as explained in detail below, the e-cigarette use question used by the single Western project (Oregon) differed from the question used by other projects in a way that could have contributed to the lower estimate of prevalence at that project.
A major strength of this study is the large number of patients enrolled over a 3.5-year period from diverse geographic areas in the United States. The overall sample was drawn from very different types of hospitals, as illustrated by the differences in the characteristics of populations enrolled across projects (Table 2). Patients were enrolled from large and small private nonprofit hospitals, a Veteran’s Administration hospital, and a safety-net hospital that primarily cares for the poor and uninsured. Most of the hospitals were also university-affiliated teaching hospitals. Collectively, the sample illustrates the diversity in the organization of hospital care in the United States. While the sample does not represent the national population of hospitalized smokers, its geographic and organizational diversity does contribute to the generalizability of our results. The variability in the hospitals had the potential to confound the analysis of change in e-cigarette use over time because the participating hospitals served different populations and the projects enrolled smokers over different time periods. We controlled for these potential confounding factors with a multivariate analysis that adjusted for enrollment date, project site, and individual patient level demographic characteristics. A similar multivariate model that adjusted for individual hospital rather than CHART project had similar results.
This study has several limitations. First, the findings do not represent all smokers admitted to participating hospitals. Patients with very short hospital stays were often discharged before they could be recruited, and it is possible that the prevalence of e-cigarette use may differ in this subset of smokers. Additionally, not all smokers screened were eligible for the study. In three of the five projects, enrollment was limited to smokers who intended to stay quit after hospital discharge. In another project that enrolled all smokers regardless of interest in quitting after discharge and collected data on intention to quit, 82% of the smokers enrolled did plan to quit after discharge. This suggests that a relatively small number of hospitalized smokers were excluded on that basis. Although this analysis cannot determine whether smokers who do not plan to quit are more or less likely to use e-cigarettes, limiting our analysis to those patients who planned to quit did not alter the overall finding of an increase in e-cigarette use over time (data not shown). However, because the majority of smokers sampled wanted to quit, our findings should be interpreted as primarily representing that group of hospitalized smokers.
Second, the wording of the e-cigarette questions asked by each study site was very similar but not identical (Table 1 footnote). The question asked by the Oregon study was the most different. It asked patients if they used “any other tobacco in the last 30 days, including electronic cigarettes”, and documented each type used by the patient. We do not believe the question wording affected the trend in prevalence over time, though it could have underestimated the overall prevalence if some patients did not consider e-cigarettes to be a tobacco product. This might contribute to the lower prevalence observed at the Oregon study compared with the other CHART studies. However, since we included e-cigarettes in the question, we do not expect this had a big effect on our prevalence estimates. Furthermore, e-cigarettes were the most common type of other tobacco reported at the hospitals in the Oregon project.
Third, the data are self-reported and were not confirmed by other means. In a hospital setting, social desirability may lead some individuals to under-report tobacco use. In this study, all subjects were already self-reported cigarette smokers. Whether social desirability bias would lead self-reported cigarette smokers to over- or under-report using e-cigarettes is unknown. Because e-cigarettes are perceived to be harm reduction products,4,8 hospitalized smokers who wish to signal their desire to reduce tobacco-related harm might over-report e-cigarette use. However, we believe that any such bias is likely to be small because the individuals have already admitted to using tobacco products and could more easily achieve their goal by stating that they were interested in quitting smoking after discharge.
Fourth, the analysis cannot provide any further details about e-cigarette use beyond the single question asked about current use. We cannot determine attitudes and beliefs about e-cigarettes, the frequency, intensity, or duration of use or the reasons that smokers used them.
In summary, this study demonstrated a substantial rise in the current e-cigarette use over 3.5 years (2010–2013) among a large sample of cigarette smokers admitted to nine geographically dispersed US hospitals. The 18% prevalence of current e-cigarette use makes it likely that some hospitalized patients are already seeking or will seek to use e-cigarettes in the hospital. Hospitals and clinicians should develop and implement policies regulating e-cigarette use. Because patients in US hospitals are not permitted to smoke cigarettes or to use medications or devices not approved by the Food and Drug Administration, we believe that e-cigarette use by hospital patients should not be allowed. We believe that this is policy is also appropriate given the current uncertainty about the net benefits and harms of e-cigarettes. National hospital regulatory agencies such as the Joint Commission might consider developing regulations to provide guidance to hospitals about e-cigarettes.
Funding
NIH grants RC1HL099668 (NAR), R01HL111821 (NAR, YC, HAT, and TY), U01DA031515 (KFH), U01HL105232 (KR), U01HL105229 (SES and EG), and U01HL105231 (JLF).
Declaration of Interests
NAR has been an unpaid consultant for Pfizer, Inc, and Alere Wellbeing, Inc, and receives royalties from UpToDate. EG has been a paid consultant for the New York City Department of Health and Mental Hygiene.
Acknowledgments
T. Gomperts Jr assisted with the preparation of the manuscript.
References
- 1. Cobb NK, Byron MJ, Abrams DB, Shields PG. Novel nicotine delivery systems and public health: the rise of the “e-cigarette”. Am J Public Health. 2010;100:2340–2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129:1972–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Glynn TJ. E-cigarettes and the future of tobacco control. CA: A Cancer J Clin. 2014;64:164–168. [DOI] [PubMed] [Google Scholar]
- 4. Pepper JK, Brewer NT. Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: a systematic review. Tob Control. In press. 10.1136/tobaccocontrol-2013–051122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. King BA, Alam S, Promoff G, Arrazola R, Dube SR. Awareness and ever-use of electronic cigarettes among US adults, 2010-2011. Nicotine Tob Res. 2013;15:1623–1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention (CDC). Notes from the field: electronic cigarette use among middle and high school students - united states, 2011–2012. MMWR Morb Mort Wkly Rep. 2013;62:729–730. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6235a6.htm [PMC free article] [PubMed] [Google Scholar]
- 7. Adkison SE, O’Connor RJ, Bansal-Travers M, et al. Electronic nicotine delivery systems: international tobacco control four-country survey. Am J Prev Med. 2013;44:207–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pearson JL, Richardson A, Niaura RS, Vallone DM, Abrams DB. E-cigarette awareness, use, and harm perceptions in US adults. Am J Public Health. 2012;102:1758–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Regan AK, Promoff G, Dube SR, Arrazola R. Electronic nicotine delivery systems: adult use and awareness of the ‘e-cigarette’ in the USA. Tob Control. 2013;22:19–23. [DOI] [PubMed] [Google Scholar]
- 10. Harrington KF, Hull NC, Akindoju O, Kim YI, Hendricks PS, Kohler C, Bailey WC. Electronic cigarette awareness, use history, and expected future use among hospitalized cigarette smokers [published online ahead of print May 13, 2014]. Nicotine Tob Res. In press. 10.1093/ntr/ntu054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Riley WT, Stevens VJ, Zhu SH, Morgan G, Grossman D. Overview of the Consortium of Hospitals Advancing Research on Tobacco (CHART). Trials. 2012;13:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rigotti NA, Regan S, Levy DE, et al. Sustained care intervention and post-discharge smoking cessation among hospitalized adults: a randomized clinical trial. JAMA. 2014;312:719–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Richter KP, Faseru B, Mussulman LM, et al. Using “warm handoffs” to link hospitalized smokers with tobacco treatment after discharge: study protocol of a randomized controlled trial. Trials. 2012;13:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fellows JL, Mularski R, Waiwaiole L, et al. Health and economic effects from linking bedside and outpatient tobacco cessation services for hospitalized smokers in two large hospitals: study protocol for a randomized controlled trial. Trials. 2012;13:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Grossman E, Shelley D, Braithwaite RS, et al. Effectiveness of smoking-cessation interventions for urban hospital patients: study protocol for a randomized controlled trial. Trials. 2012;13:126. [DOI] [PMC free article] [PubMed] [Google Scholar]