Abstract
Introduction:
Electronic cigarettes (e-cigs) are becoming increasingly popular, but little is known about their dependence potential. This study aimed to assess ratings of dependence on electronic cigarettes and retrospectively compare them with rated dependence on tobacco cigarettes among a large sample of ex-smokers who switched to e-cigs.
Methods:
A total of 3,609 current users of e-cigs who were ex-cigarette smokers completed a 158-item online survey about their e-cig use, including 10 items designed to assess their previous dependence on cigarettes and 10 almost identical items, worded to assess their current dependence on e-cigs (range 0–20).
Results:
Scores on the 10-item Penn State (PS) Cigarette Dependence Index were significantly higher than on the comparable PS Electronic Cigarette Dependence Index (14.5 vs. 8.1, p < .0001). In multivariate analysis, those who had used e-cigs longer had higher e-cig dependence scores, as did those using more advanced e-cigs that were larger than a cigarette and had a manual button. Those using zero nicotine liquid had significantly lower e-cig dependence scores than those using 1–12mg/ml, who scored significantly lower than those using 13 or greater mg/ml nicotine liquid (p < .003).
Conclusions:
Current e-cigarette users reported being less dependent on e-cigarettes than they retrospectively reported having been dependent on cigarettes prior to switching. E-cig dependence appears to vary by product characteristics and liquid nicotine concentration, and it may increase over time.
Introduction
The popularity of electronic cigarettes (e-cigs) has increased rapidly in many countries over the past 5 years, and in some countries, as many as a third of current or recent ex-cigarette smokers have tried e-cigs.1–3 The most recent data from a large representative sample of US adults found that 4.2% (of all adults) used electronic cigarettes every day, some days, or rarely.4 Assessment of the likely public health risks and benefits of e-cigs will require the systematic collection of data on patterns of use, product characteristics, characteristics of users, effects on toxicant exposure, and effects on health, including dependence. As e-cigs were invented in 2003 and only became popular in recent years, much remains unknown about their safety or dependence potential.
There are a number of brief questionnaires with proven utility in assessing dependence in cigarette users. The Fagerström Test for Nicotine Dependence (FTND) is the most widely used method of assessing cigarette dependence. Many studies have found that two specific items (cigarettes/day and time to first cigarette of the day) are more predictive of difficulty quitting (and other indices of dependence) than the other items and so these two items have come to be widely used and together have come to be known as the Heaviness of Smoking Index (HSI).5–8
With the recent proliferation of nicotine containing products, it has become clear that there is a need for measures capable of assessing nicotine dependence in other products.9,10 However, given that other nicotine delivery products may have different patterns of use, there may be advantages in developing methods of assessing dependence in ways that can facilitate comparison across products, but not be as dominated by heaviness or frequency of use as the FTND or HSI. The Wisconsin Inventory of Smoking Dependence Motives (WISDM) is a longer (68-item) multisubscale assessment, but neither the full score nor most of the subscales are as predictive of cessation outcomes as the much briefer FTND.11 The Hooked On Nicotine Checklist (HONC) was developed specifically to assess the development of dependence in young people.12 It is a 10-item questionnaire that has good psychometric properties, but many adult smokers reach the ceiling score and the average smoker trying nicotine replacement therapy scores 8/10 and so it is less sensitive at the high end of the spectrum.13
The FTND is not designed to help assess DSM-4 or 5 criteria for nicotine dependence,14 and the FTND does not relate well to DSM-based assessments.15 Given the strengths and weaknesses of existing measures of nicotine dependence, we developed a new nicotine dependence index comprising some of the most predictive items from various prior studies, but designed to be easily adapted for different nicotine products. These items were partly selected to cover each of the main components of dependence (consumption, drive, craving, withdrawal, difficulty quitting) and adapted to use a scoring scheme reflective of evidence that dependence can exist at low levels of consumption,12 and to measure aspects of dependence (e.g., cravings and withdrawal symptoms) that have been recommended as being of most practical use in assessing smokers.14 One of our priorities was to create a brief scale, and we acknowledge that for some purposes, it may be worth including more items, including items specifically on withdrawal-related craving or those included in the WISDM.
Recent studies have identified some questionnaire items that appear to assess additional aspects of nicotine dependence very simply. For example, Bover et al. 16 found that 51% of 2,768 cigarette smokers attending a tobacco dependence treatment clinic reported at baseline assessment that they wake at night to smoke, and that a single question about this behavior predicted abstinence at 6-month follow-up in both univariate and multivariate analyses, whereas neither HSI item did. Scharf et al. 17 reported that self-reported night smoking correlated well with electronic diary-measured night smoking and that night smoking quantity predicted lapse risk even when controlling for traditional (less predictive) measures of nicotine dependence. This suggests that quantity of night smoking may capture variance in smoking patterns that is not captured by existing items or scales (FTND or Nicotine Dependence Syndrome Scale items). Fidler et al. 18 found that strength of smoking urges during a recent time period of normal smoking (past 24 hrs or past week) predicted difficulty quitting better than the FTND/HSI scores and may be a useful measure of cigarette addiction.
After completing a review of existing questionnaire assessments of dependence, we developed a Cigarette Dependence Index comprising 10 items. Two of these (accounting for 10 points) were adapted from the FTND/HSI (requiring participants to write the actual numbers, rather than check pre-defined range options), five are from the HONC (covering difficulty quitting, experience of craving, and withdrawal symptoms), two assess waking at night to use (adapted from Bover et al. 16), and one assesses recent strength of urges to use (adapted from Fiddler et al. 18). The items and scoring guide are shown in Box 1.
Box 1. Penn State [Electronic] Cigarette Dependence Index
| [For the Electronic Cigarette Dependence Index, substitute the underlined word with the words in square brackets]1. How many cigarettes [times] per day do you usually smoke [use your electronic cigarette]?a ([assume that one “time” consists of around 15 puffs or lasts around 10 minutes]) (Scoring: 0–4 times/day = 0, 5–9 = 1, 10–14 = 2, 15–19 = 3, 20–29 = 4, 30+ = 5) |
| 2. On days that you can smoke [use your electronic cigarette] freely, how soon after you wake up do you smoke your first cigarette of the day [first use your electronic cigarette]?a
(Scoring: 0–5 mins = 5, 6–15 = 4, 16–30 = 3, 31–60 = 2, 61–120 = 1, 121+ = 0) |
| 3. Do you sometimes awaken at night to have a cigarette [use your electronic cigarette]?b
(Scoring: Yes = 1, No = 0) |
| 4. If yes, how many nights per week do you typically awaken to smoke [use your electronic cigarette]?b
(Scoring: 0–1 nights = 0, 2–3 nights = 1, 4+ nights = 2) |
| 5. Do you smoke [use an electronic cigarette] now because it is really hard to quit?c
(Scoring: Yes = 1, No = 0) |
| 6. Do you ever have strong cravings to smoke [use an electronic cigarette]?c
(Scoring: Yes = 1, No = 0) |
| 7. Over the past week, how strong have the urges to smoke [use an electronic cigarette] been?d
(Scoring: None/Slight = 0, Moderate/Strong= 1, Very Strong/Extremely Strong = 2) |
| 8. Is it hard to keep from smoking [using an electronic cigarette] in places where you are not supposed to?c
(Scoring: Yes = 1, No = 0) |
| When you haven’t used tobacco [an electronic cigarette] for a while or when you tried to stop smoking [using]… 9. Did you feel more irritable because you couldn’t smoke [use an electronic cigarette]?c (Scoring: Yes = 1, No = 0) |
| 10. Did you feel nervous, restless, or anxious because you couldn’t smoke [use an electronic cigarette]?c
(Scoring: Yes = 1, No = 0) |
Total scoring: 0–3= not dependent, 4–8 low dependence, 9–12 medium dependence, 13+ = high dependence.
The original questionnaire asks about cigarette use and electronic cigarette use separately, and the wording for e-cig questions is provided here in brackets merely to facilitate comparisons and save journal space.
aFrom FTND/HSI.
bFrom Bover et al. 16
cFrom Hooked on Nicotine Checklist.
dFrom Fiddler et al. 18
We then piloted the Cigarette Dependence Index in a smoking cessation trial in 225 smokers who received nicotine patches and group support for a month. As expected, the index predicted 1-month intent-to-treat CO-verified abstinence, such that those scoring 0–10 at baseline had a 74% quit rate, those scoring 11–14 had a 52% quit rate, and those scoring 15–20 had a 27% quit rate. This is not surprising as the scale comprises items that have been shown to predict difficulty quitting in numerous prior studies. We piloted similar questions in face-to-face interviews with 108 electronic cigarette users19 and found that the only question needing adaptation/clarification for electronic cigarette users was the item about frequency of use. Some participants mentioned that this was difficult to answer because, unlike a cigarette that is generally smoked as a whole and then discarded, e-cigs can be used more frequently but perhaps with fewer puffs per “session,” because there is no need to “finish the cig” in one sitting. We found that the vast majority of e-cig users are able to estimate their total amount of e-cig use in a way that is comparable with cigarettes, by specifying, “How many times per day do you usually use your electronic cigarette? (assume one ‘time’ consists of around 15 puffs, or lasts around 10min).”
Having developed an index of nicotine dependence that could be easily adapted for use in assessing both cigarette and e-cig dependence, this study aimed to compare ratings of dependence on electronic cigarettes with tobacco cigarettes in a sample of ex-smokers who have switched to e-cigs. This study also aimed to assess the validity of the e-cig dependence index by examining the relationship of the e-cig dependence index with the concentration of nicotine in the liquid being used. It was hypothesized that e-cig dependence would be higher in those using higher concentrations of nicotine and in those who have used e-cigs for a longer period of time.
Methods
Electronic cigarette users were invited to complete an online survey aiming to improve understanding of the use of electronic cigarettes, including the types of e-cigs being used, how frequently they are used and whether or not they are replacing other types of tobacco among e-cig users aged ≥18 years old. Participation in this study was voluntary and respondents could remain anonymous, although individuals who wished to volunteer for additional research on e-cigs were invited to enter their contact details at the end of the survey. The survey was administered and responses were stored on REDCap (Research Electronic Data Capture). REDCap is a secure, web-based application designed to support data capture for research studies. REDCap is maintained by the REDCap Consortium, which is comprised of more than 600 institutional partners including Penn State University. This survey was comprehensive; containing 158 items including demographics, e-cig use history, types of e-cig used, tobacco use history, and various free text responses. Embedded within the survey were the 10 questions that made up the PS Electronic Cigarette Dependence Index and its 10-item cigarette equivalent. The cigarette version was preceded by the following statement: “Think back to a time when you were primarily a traditional cigarette smoker….before you used e-cigs. To the best of your ability, answer the following questions regarding your cigarette smoking at that time.” This survey was first posted on the Internet in December 2012 (https://redcap.ctsi.psu.edu/redcap/surveys/?s=v94cbA). Links to the survey were posted on a variety of websites including www.webMD.com, and sites frequented by e-cig users, including www.e-cigarette-forum.com, one of the largest e-cig user websites. Visitors to these sites were also able to cross-post the survey link to friends and other websites. This study was approved by the Penn State University Institutional Review Board. Data reported here were collected from December 2012 to May 2014.
The dataset was first checked for completeness and likely duplicate completions. Likely duplications were identified as (a) those with the same demographics and e-mail address or (b) those with identical state, city, gender, age, race, and occupation. Where likely duplicates were identified, neither case was included. Cases with incomplete demographics or e-cig history were not included, leaving 6,745 with complete data. Of these, 5,462 were current regular e-cig users (had used e-cigs on at least 30 days, including the past 7 days). A total of 5,363 (98%) had ever been a cigarette smoker of whom 3,859 (72%) had quit smoking for at least 30 days. A total of 193 were excluded as they had recently used another tobacco or smoking cessation product and 57 had incomplete data on their prior cigarette use, leaving a final sample of 3,609 who were exclusive current e-cig users and ex-cigarette smokers.
The data were analyzed using the SAS 9.3 statistical package. Means and percentages were calculated in order to characterize the overall sample. Paired t-tests (two-tailed) were used to compare continuous variables and chi-squared tests were used to compare categorical variables (generally comparing the same individuals’ current e-cig use with their prior cigarette use behavior). When comparing E-Cig Dependence Index scores by response characteristics with more than two options, one-way analysis of variance was used with Tukey adjustment for multiple comparisons. Multivariate regression was used to identify predictors of e-cig dependence using the SAS stepwise procedure (iterative backwards and forwards stepwise).
Results
The main descriptive characteristics of the sample are shown in Table 1. The sample was predominantly White, male, and living in the United States. They reported making multiple attempts to quit smoking and had on average been using e-cigs for over a year. Most reported that they quit smoking cigarettes shortly after they started using e-cigs, but almost 9% had quit smoking cigarettes prior to using e-cigs. However, the majority of these reported that they were still using another traditional tobacco product when they started e-cig use and all reported that they were free of traditional tobacco use at the time of the survey. Only 13% were using first-generation e-cigs that are the same size and shape as a regular cigarette (“a cigalike”), and most were using more advanced e-cigs that included the ability to press a button to activate the heating coil manually prior to puffing and the ability to control the voltage. They had tried an average of five different e-cig models, and almost three quarters had switched to their current brand because it gave them a more satisfying “hit.”
Table 1.
Demographic, Tobacco Use, and Electronic Cigarette Use Characteristics of the Sample
| Characteristic | N = 3,609 |
|---|---|
| Male, % (n) | 72.2 (2,604) |
| Mean age (SD) | 40.5 (12.6) |
| White, % (n) | 92.0 (3,319) |
| With college degree, % (n) | 40.7 (1,467) |
| Live in United States, % (n) | 84.8 (3,062) |
| Mean number of lifetime cigarette quit attempts (SD) | 8.6 (15.5) |
| Mean number of months since quitting smoking (SD) (n = 3,281) | 12.7 (12.2) |
| Mean length of e-cig use in months (SD) | 13.4 (12.9) |
| Mean E-liquid nicotine concentration, mg/ml (SD) | 15.5 (8.6) |
| Mean number of E-cigs used before current model (n = 3,601) | 4.2 (4.1) |
| Use e-cig liquid >12mg/ml, % (n) | 50.8 (1,834) |
| Who started using E-cigs with intention to quit smoking, % (n) | 74.4 (2,684) |
| Who quit smoking cigarettes prior to using E-cig, % (n) | 8.8 (317) |
| Who plan to continue using e-cig for at least another year, % (n) | 78.8 (2,845) |
| E-cig larger than regular cigarette, % (n) | 87.1 (3,145) |
| E-cig cost > $50 (n = 3,583), % (n) | 55.7 (1,994) |
| E-cig purchased at gas (petroleum) station, % (n) | 9.2 (331) |
| Use only Vegetable Glycerin E-liquid, % (n) | 8.8 (234) |
| E-cig with button to press prior to inhalation, % (n) | 84.7 (3,056) |
| E-cig with button to control battery voltage, % (n) | 61.9 (2,234) |
| E-cig uses single 3.7-V battery, % (n) | 72.7 (2,622) |
| E-cig requires more than 1 battery, % (n) | 4.9 (175) |
| E-cig uses proprietary battery, % (n) | 30.3 (1,095) |
| Switched to current brand because it gives a more satisfying “hit,” % (n) | 74.8 (2,699) |
Table 2 shows a comparison of the total Penn State Nicotine Dependence Index and the individual items for current e-cig use and past cigarette use. This table shows that although the e-cig users were having e-cig sessions with a very similar frequency to the number of cigarettes they had previously consumed each day, their overall E-Cig Dependence Index was significantly lower than their Cigarette Dependence Index, as was the individual score on every other item. Over ninety percent reported that they had experienced strong urges to smoke and withdrawal symptoms when a smoker, but only 25 to 35% reported experiencing these symptoms of dependence as an e-cig user.
Table 2.
Penn State Nicotine Dependence Index: Comparison of Total Score and Individual Item Responses for Smoking Cigarettes and Using Electronic Cigarettes
| Penn State Nicotine Dependence Index | Traditional cigarette | Electronic cigarette | p |
|---|---|---|---|
| Mean PSNDI score (SD) | 14.5 (3.7) | 8.1 (3.5) | <.0001 |
| Mean cigarettes (e-cig sessions) per day (SD) | 24.3 (12.4) | 24.0 (25.9) | .4493 |
| Mean time to first smoke (e-cig use) of the day, in mins (SD) | 26.8 (67.3) | 44.5 (72.7) | <.0001 |
| Awakening at night to smoke (use e-cig), % (n) | 41.2 (1,487) | 6.8 (247) | <.0001 |
| Who smoke (use e-cig) because it is really hard to quit, % (n) | 89.4 (3,225) | 28.8 (1,039) | <.0001 |
| Had strong cravings to smoke (use e-cig), % (n) | 92.7 (3,344) | 35.4 (1,277) | .0037 |
| With strong, very strong, or extremely strong urges to smoke (use e-cig), % (n) | 85.7 (3,093) | 11.72 (423) | .0001 |
| Find it hard to keep from using in places where you are not supposed to, % (n) | 64.5 (2,328) | 10. 5 (378) | .0014 |
| More irritable when they cannot smoke (use e-cig), % (n) | 91.7 (3,312) | 25.6 (923) | <.0001 |
| More nervous when they cannot smoke (use e-cig), % (n) | 90.4 (3,263) | 26.4 (953) | <.0001 |
All the variables in Table 1 were entered in a stepwise regression model (ejecting any variables not predictive of E-Cig Dependence Index at p < .15). The final model found that even when adjusting for all other significant predictors, women, Whites, those without a college education, who are older, who have used e-cigs for a longer time, who have previously tried more e-cig models, who currently use an e-cig larger than a cigarette, with a button, with more than one battery, that cost over $50 and who use a higher concentration of nicotine liquid, tend to have a higher e-cig dependence index (all p < .05). When Cigarette Dependence Index was entered in the regression, it too was a highly significant predictor of the E-cig Dependence Index (p < .001) and the two scores had a Pearson correlation of +0.35 (p < .0001).
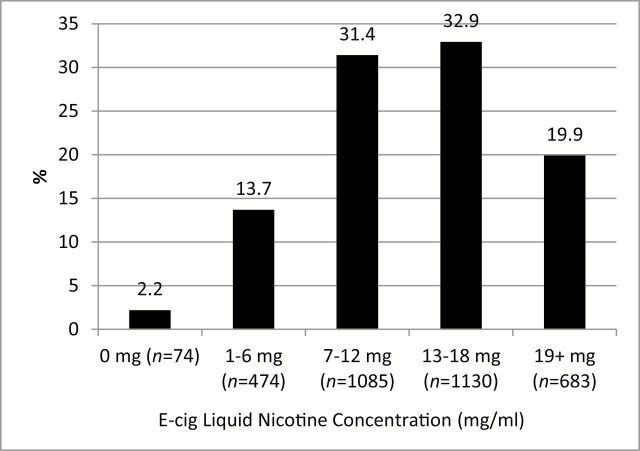
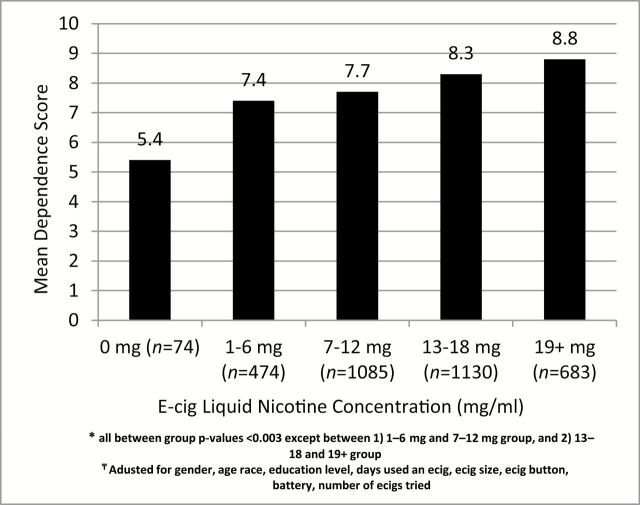
Figure 1 shows the number and proportion of e-cig users using different levels of nicotine concentration in their e-liquid. Figure 2 shows the relationship between the nicotine concentration and the e-cig dependence index, after controlling for all the other significant predictors. Those using zero nicotine liquid had a significantly lower e-cig dependence index than those using 1–12mg/ml (p < .001), who were significantly lower than those using 13 or greater mg/ml nicotine liquid (p < .001).
Figure 1.
E-cig liquid nicotine concentration, % (n = 3,478).
Figure 2.
Adjusteda Penn State Electronic Cigarette Dependence Index by e-cig nicotine concentration* (n = 3,446). aAdjusted for gender, age, race, education level, days used an e-cig, e-cig size, e-cig button, battery, and number of e-cig. *All between group p values <.003 except between (1) 1–6-mg and 7–12-mg group, and (2) 13–18 and 19+ group.
The online survey included questions about whether respondents had advocated for e-cigs or earned income from selling e-cigarette merchandise. It is conceivable that some of the volunteers for this study who were advocates for e-cigarettes may therefore have chosen to underestimate their dependence on e-cigs relative to cigarettes in order to make e-cigs appear more favorable. However, when the question about prior e-cig advocacy was included in the regression model, it did not alter the pattern of results. More importantly, those who had advocated for e-cigs online had higher e-cig dependence scores, which is not consistent with the notion that they may have minimized their e-cig dependence ratings.
The first 2 items of the dependence index comprise a 10-point version comparable with the HSI, whereas the next 8 items comprise a 10-point measure of specific dependence symptoms. On the Cigarette Dependence Index, the two subscores were similar (7.7 vs. 6.8) and moderately correlated (Pearson correlation = +0.51, p < .0001), whereas on the E-cig Dependence Index, there was a lower mean score for the specific symptom subscore (6.1 vs. 2.0) and a lower correlation between the two subscores (Pearson correlation = +0.23, p < .001).
Discussion
This study found that although ex-smoking e-cig users use their e-cigs about as much as they smoked their cigarettes, they appear to be significantly less dependent on their e-cigs than they were on their cigarettes, as assessed on a number of questions that have been shown to be good measures of dependence in cigarette smokers. It is possible that e-cig users could experience less craving and withdrawal because their use of their product is less widely restricted. However, that does not explain the fact that e-cig users are much less likely to waken at night to use an e-cig than they had been to smoke, or that they wait significantly longer before using after waking in the morning than they did as cigarette smokers. Farsalinos et al. 20 also found that e-cig users reported lower dependence on e-cigs than prior cigarette smoking, in a sample of 111 e-cig users with carboxyhemoglobin-validated abstinence from smoking.
Overall, the most parsimonious explanation for these results is that e-cig users are generally less nicotine dependent than they were as cigarette smokers. This is perhaps not surprising given that almost all the studies of nicotine absorption from e-cigs suggest that they deliver markedly lower peak nicotine levels compared with cigarettes, and that they deliver nicotine more slowly than cigarettes, both of which are characteristics likely leading to less addiction.21–25
We also found that users of more advanced e-cigs (in terms of size, battery power, ability to control timing of heat being applied to the coil, cost of e-cig, and so on), score higher on measures of dependence. This is also consistent with existing data, showing that advanced generation models deliver higher blood nicotine levels than current “cigalike” models.25,26
This study found that scores on the PS Electronic Cigarette Index were significantly related to the concentration of nicotine in the e-cig liquid being used, even after controlling for other predictors. This may not be very surprising, but is at least consistent with the idea that the items selected for the index are somewhat sensitive to nicotine consumption after controlling for frequency of use. It should be noted that even when we analyzed only those e-cig users who were using e-cigs that were larger than a regular cigarette, had a button, with a nicotine concentration greater than 12mg/ml, for at least 18 months (n = 405), their E-Cig Dependence Index was still lower than their Cigarette Dependence Index (9.2 vs. 15.4, p < .0001).
The “uncoupling” of the close relationship between heaviness of use (as measured by times per day and time to first use of the day) and the strength of the other dependence symptoms (e.g., strength of urges and withdrawal symptoms) in e-cig users may be due to the wider variation in nicotine absorption from different e-cigs than exists for cigarettes. This underlines the importance of assessing specific dependence symptoms when assessing dependence in e-cig users.
Weaknesses of this study include the nonrepresentative nature of the volunteer sample. Clearly those who found out about the survey on specialist websites and took the time to complete the survey are a particularly experienced and likely “pro-e-cig” sample of e-cig users, and it is possible their answers were designed to make e-cigs look “good” relative to traditional cigarettes. However, we found a similar pattern of results in the 97% of participants who had never sold e-cigarette merchandise and also in the 58% of participants who had never advocated for e-cigs online. Given that the dependence scales were embedded within more than 120 other questions, we also think it doubtful that those completing these items were aware that they would be used to assess dependence and compare products. Another potential weakness is the lack of prior studies of validity and reliability of the PS Electronic Cigarette Dependence Index. However, the fact that these items all have a good track record as indicators of dependence in cigarette users and were positively associated with use of higher nicotine concentration e-liquid in this study are supportive of the validity of the measure. However, with regards to the direct comparison between current dependence on e-cigs and retrospective ratings of dependence on traditional cigarettes, we acknowledge that there is an inherent weakness in this design and a possibility the respondents could attempt to justify their current behavior by making it seem more acceptable (less addiction-based) than their former smoking. Prospective studies that include biomarkers of intake and concurrent ratings of cravings and withdrawal symptoms will be required to more fully compare dependence in those switching from cigarettes to e-cigs. Finally, given that the participants were being asked to retrospectively recall their smoking behavior a year or more earlier, it may have been inaccurate. Hudmon et al. 27 studied the recall of FTND nicotine dependence retrospective assessments 5–12 years later and concluded that these have acceptable reliability.
Strengths of this study lie in the large sample size and the comprehensiveness of the overall survey, enabling analyses that can assess and control for a range of factors that may influence e-cig dependence, including the advocacy involvement of the respondents. Controlling for these variables did not make substantial differences to the pattern of results, suggesting that the findings are fairly robust.
Conclusions
Current e-cigarette users report being less dependent on e-cigarettes than they retrospectively report having been dependent on cigarettes prior to switching. E-cig dependence appears to be related to length of e-cig use, characteristics of the device used that may facilitate nicotine absorption, and is related to the concentration of nicotine used in the e-liquid.
Funding
This work was supported by an internal grant from Penn State Social Science Research Institute and Cancer Institute (PI: SJW). JF, SV, JY, and SH are primarily funded by the National Institute on Drug Abuse of the National Institutes of Health and the Center for Tobacco Products of the US Food and Drug Administration (P50-DA-036107-01 and P50-DA-0361-05). TE is supported by the National Institute on Drug Abuse of the National Institutes of Health (P50-DA-0361-05) and the Center for Tobacco Products of the US Food and Drug Administration.
Declaration of Interests
JF has done paid consulting for pharmaceutical companies involved in producing smoking cessation medications, including GSK, Pfizer, Novartis, J&J, and Cypress Bioscience.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the US Food and Drug Administration.
References
- 1. Brown J, West R, Beard E, Michie S, Shahab L, McNeill A. Prevalence and characteristics of e-cigarette users in Great Britain: findings from a general population survey of smokers. Addic Behav 2014;39(6):1120–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Carroll Chapman SL, Wu L. E-cigarette prevalence and correlates of use among adolescents versus adults: a review and comparison. J Psychiatr Res 2014;54:43–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goniewicz ML, Zielinska-Danch W. Electronic cigarette use among teenagers and young adults in Poland. Pediatrics 2012;130(4):e879–e885. [DOI] [PubMed] [Google Scholar]
- 4. Agaku IT, King BA, Husten CG, et al. Tobacco product use among adults--United States, 2012–2013. MMWR Morb Mortal Wkly Rep 2014;63(25):542–547. [PMC free article] [PubMed] [Google Scholar]
- 5. Fagerström K-O, Russ C, Yu CR, Yunis C, Foulds J. The Fagerström Test for Nicotine Dependence as a predictor of smoking abstinence: a pooled analysis of Varenicline Clinical Trial Data. Nicotine Tob Res 2012. [DOI] [PubMed] [Google Scholar]
- 6. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström K-O. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addic 1991;86(9):1119–1127. [DOI] [PubMed] [Google Scholar]
- 7. Kozlowski LT, Porter CQ, Orleans CT, Pope MA, Heatherton T. Predicting smoking cessation with self-reported measures of nicotine dependence: FTQ, FTND, and HSI. Drug Alcohol Depen 1994;34(3):211–216. [DOI] [PubMed] [Google Scholar]
- 8. Baker TB, Piper ME, McCarthy DE, et al. Time to first cigarette in the morning as an index of ability to quit smoking: implications for nicotine dependence. Nicotine Tob Res 2007;9(suppl 4:S555–S570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. De Leon E, Smith KC, Cohen JE. Dependence measures for non-cigarette tobacco products within the context of the global epidemic: a systematic review. Tob Control 2014;23(3):197–203. [DOI] [PubMed] [Google Scholar]
- 10. Fagerström K-O, Eissenberg T. Dependence on tobacco and nicotine products: a case for product-specific assessment. Nicotine Tob Res 2012;14(11):1382–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Piper ME, McCarthy DE, Bolt DM, et al. Assessing dimensions of nicotine dependence: an evaluation of the Nicotine Dependence Syndrome Scale (NDSS) and the Wisconsin Inventory of Smoking Dependence Motives (WISDM). Nicotine Tob Res 2008;10(6):1009–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. DiFranza JR, Savageau JA, Fletcher K, et al. Measuring the loss of autonomy over nicotine use in adolescents: the DANDY (Development and Assessment of Nicotine Dependence in Youths) study. Arch Pediatr Adolesc Med 2002;156(4):397–403. [DOI] [PubMed] [Google Scholar]
- 13. Wellman RJ, Savageau JA, Godiwala S, et al. A comparison of the Hooked on Nicotine Checklist and the Fagerström Test for Nicotine Dependence in adult smokers. Nicotine Tob Res 2006;8(4):575–580. [DOI] [PubMed] [Google Scholar]
- 14. Baker TB, Breslau N, Covey L, Shiffman S. DSM criteria for tobacco use disorder and tobacco withdrawal: a critique and proposed revisions for DSM-5. Addiction 2012;107(2):263–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moolchan ET, Radzius A, Epstein DH, et al. The Fagerström Test for Nicotine Dependence and the diagnostic interview schedule: do they diagnose the same smokers? Addic Behav 2002;27(1):101–113. [DOI] [PubMed] [Google Scholar]
- 16. Bover MT, Foulds J, Steinberg MB, Richardson D, Marcella SW. Waking at night to smoke as a marker for tobacco dependence: patient characteristics and relationship to treatment outcome. Int J Clin Prac 2008;62(2):182–190. [DOI] [PubMed] [Google Scholar]
- 17. Scharf DM, Dunbar MS, Shiffman S. Smoking during the night: prevalence and smoker characteristics. Nicotine Tob Res 2008;10(1):167–178. [DOI] [PubMed] [Google Scholar]
- 18. Fidler JA, Shahab L, West R. Strength of urges to smoke as a measure of severity of cigarette dependence: comparison with the Fagerström Test for Nicotine Dependence and its components. Addiction 2011;106(3):631–638. [DOI] [PubMed] [Google Scholar]
- 19. Foulds J, Veldheer S, Berg A. Electronic cigarettes (e-cigs): views of aficionados and clinical/public health perspectives. Int J Clin Prac 2011;65(10):1037–1042. [DOI] [PubMed] [Google Scholar]
- 20. Farsalinos KE, Romagna G, Tsiapras D, Kyrzopoulos S, Voudris V. Evaluating nicotine levels selection and patterns of electronic cigarette use in a group of “vapers” who had achieved complete substitution of smoking. Subst Abuse 2013;7:139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bullen C, McRobbie H, Thornley S, Glover M, Lin R, Laugesen M. Effect of an electronic nicotine delivery device (e cigarette) on desire to smoke and withdrawal, user preferences and nicotine delivery: randomised cross-over trial. Tob Control 2010;19(2):98–103. [DOI] [PubMed] [Google Scholar]
- 22. Dawkins L, Corcoran O. Acute electronic cigarette use: nicotine delivery and subjective effects in regular users. Psychopharmacology (Berl) 2014;231(2):401–407. [DOI] [PubMed] [Google Scholar]
- 23. Nides MA, Leischow SJ, Bhatter M, Simmons M. Nicotine blood levels and short-term smoking reduction with an electronic nicotine delivery system. Am J Health Behav 2014;38(2):265–274. [DOI] [PubMed] [Google Scholar]
- 24. Vansickel AR, Cobb CO, Weaver MF, Eissenberg TE. A clinical laboratory model for evaluating the acute effects of electronic “cigarettes”: nicotine delivery profile and cardiovascular and subjective effects. Cancer Epidemiol Biomarkers Prev 2010;19(8):1945–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Vansickel AR, Eissenberg T. Electronic cigarettes: effective nicotine delivery after acute administration. Nicotine Tob Res 2013;15(1):267–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Farsalinos KE, Spyrou A, Tsimopoulou K, Stefopoulos C, Romagna G, Voudris V. Nicotine absorption from electronic cigarette use: comparison between first and new-generation devices. Sci Rep 2014;4:4133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hudmon KS, Pomerleau CS, Brigham J, Javitz H, Swan GE. Validity of retrospective assessments of nicotine dependence: a preliminary report. Addict Behav 2005;30(3):613–617. [DOI] [PubMed] [Google Scholar]