Abstract
Background:
Previous research suggests that females may be more motivated to smoke for negative reinforcement (NR) than males. However, it remains unclear whether gender differences in smoking outcome expectancies for negative smoking reinforcement—an important theoretical and clinical target defined as beliefs that smoking alleviates negative affect—exist above and beyond gender differences in depression and/or other outcome expectancies.
Methods:
Relations between gender and negative smoking reinforcement expectancies were examined in two independent samples. Sample 1 consisted of non-treatment seeking daily smokers (Male n = 188; Female n = 91) recruited from Southern California (49.5% Black, 32.2% Caucasian, and 18.3% other race/ethnicity). Sample 2 consisted of treatment seeking daily smokers (Male n = 257; Female n = 237) in Northern Florida and Vermont (10.7% Black, 82.9% Caucasian, and 6.4% other).
Results:
Females (vs. males) reported stronger NR smoking expectancies with and without statistically controlling for nicotine dependence, other smoking expectancies, and anxiety and depression in both samples (βs = .06 to .14, ps = .06 to < .001).
Conclusions:
Beliefs that smoking alleviates negative affect may reflect a gender-specific etiological process disproportionately prominent in women. Enhancing ability to cope with negative affect without smoking or challenge NR expectancies may be particularly important for cessation treatment in women.
Introduction
Previous work shows that females report greater increases in negative affect resulting from tobacco abstinence,1–3 are more likely to resume smoking to relieve distress from withdrawal,4 and smoke more5 and sooner6 following experimental negative mood induction. Thus, negative reinforcement (NR) through smoking-related negative affect reduction may be a disproportionately salient factor in maintaining smoking behavior in women versus men.
NR smoking outcome expectancies—beliefs that smoking relieves negative affect—are important cognitive manifestations of NR smoking motivation. Strength of NR expectancies are associated with greater nicotine dependence, initiation and escalation of smoking, motivation to quit,7–10 and have been shown to predict relapse.11 Hence, NR expectancies may be important etiologic and clinical targets for smoking research that, given the experimental research reviewed above, may be different in men and women.
Studies investigating gender differences in NR smoking expectancies have generally supported the notion that women express greater NR smoking expectancies.10,12 Although these studies suggest a potential role for gender in smoking expectancies, they did not account for factors that may explain or confound gender differences in smoking. For instance, women (vs. men) may simply have more generalized pro-smoking expectancies. For example, studies suggest that females show greater expectations that smoking contributes to weight control.7,13 Hence, through controlling for other types of (correlated) smoking expectancies (e.g., positive reinforcement, weight control), one can determine whether the effect of gender is specific to NR expectancies. Furthermore, females typically experience higher levels depression and anxiety,14 and smokers with elevated depression and anxiety symptoms tend to endorse stronger NR expectancies;15–17 thus, it is still unclear whether effects of gender on NR expectancies are explained (or confounded) by negative emotional distress. An important question for gender differences research is, regardless of emotional symptomatology, whether women still hold stronger NR expectancies than men. In this secondary analysis report, we examine the association between gender and NR smoking expectancies in two independent samples. We hypothesized that females would report greater NR expectancies and that these relations would remain after controlling for other smoking expectancies, anxiety and depression levels, and nicotine dependence.
Methods
Participants and Procedures
Sample 1
Non-treatment seeking daily smokers (N = 278) were recruited from the Los Angeles, CA area via advertisements for a laboratory study on personality and smoking, which has been published previously.18 Participants included were 18 years of age or older, had breath CO ≥ 10 ppm, regular smoker (≥10 cigarettes/day) for 2+ years, and were excluded for active mood or substance use disorder or the desire to quit in the next 30 days.
Participants attended a baseline session at the laboratory, which included breath alcohol and carbon monoxide and administration of the Structured Clinical Interview for DSM-IV Non-Patient Edition.19 Eligible participants continued with the remainder of the session, which involved completing the paper-and-pencil measures described below, for which they were compensated $15. The University of Southern California Internal Review Board approved the protocol.
Sample 2
Adult daily smokers (N = 494) were recruited from Tallahassee, FL and Burlington, VT (via flyers, newspaper ads, radio announcements) to participate in a randomized controlled trial examining the efficacy of two smoking cessation interventions.20 Participants were between ages 18–65 who reported smoking ≥8 cigarettes/day, with motivation to quit rated as at least 5 or higher on a 10-point scale. Participants were excluded for inability to give informed consent, current use of smoking cessation products or treatment, past-month suicidality, and history of psychotic-spectrum disorders.
Individuals responding to study advertisements were scheduled for an in-person, baseline assessment. After providing written informed consent, participants were interviewed using the Structural Clinical Interview of DSM-IV Disorders21 and completed a computerized battery of baseline (pre-treatment) self-report questionnaires. The study protocol was approved by the Institutional Review Boards at the University of Vermont and Florida State University.
Measures
Demographics and Smoking Characteristics
In addition to questionnaires assessing demographic and smoking characteristics (e.g., cigarettes smoked per day and age started regularly smoking), participants were administered the Fagerström test of nicotine dependence (FTND),22 which is a widely-used six-item self-report measure of nicotine dependence severity.
Smoking Consequences Questionnaire
The smoking consequences questionnaire (SCQ)7,11 is a 50-item self-report measure, which yields four subscales for different domains of smoking expectancies: NR (e.g., “Smoking calms me down when I feel nervous”), negative consequences (e.g., “The more I smoke, the more I risk my health”), appetite-weight control (e.g., “Smoking keeps my weight down”), and positive reinforcement (e.g., “When I smoke, the taste is pleasant”). In Sample 1, participants rated different expected effects of smoking on a scale from 1 (“Not true of me at all”) to 7 (“Very true of me”). In Sample 2, participants rated different expected effects of smoking on how likely or unlikely a consequence was for them on a scale from 0 (“completely unlikely”) to 9 (“completely likely”). The scales used had identical wording of the questions with the only difference being the anchor labels for the ratings. Both of these anchor labels tapped into likelihood of expected outcome, which appear most related to predictive value of the scale.7
Depression and Anxiety Symptoms
In Sample 1, depression and anxiety was assessed using the Mood and Anxiety Sensitivity Questionnaire-Short Form (MASQ-SF).23,24 Participants rate the extent to which they experienced each symptom during the previous week. The anxious arousal (AA) subscale focuses on somatic tension and arousal specific to anxiety (17-items). The anhedonic depression (AD) subscale assesses low interest, pleasure, and positive affect specific to depression (22 items).
In Sample 2, participants completed the Inventory of Depression and Anxiety Symptoms25 by rating the degree to which they experienced symptoms in the past two weeks. This measure yields a global General Depression score (20 items) and a Panic score, which are conceptually similar to the MASQ-AD and MASQ-AA scales (8 items).
Data Analysis
Preliminary analyses involved reporting sample descriptives by gender, correlations of gender and SCQ-NR to demographics, and smoking characteristics. Variables were checked for normality and homoscedastcity and transformations were applied when appropriate. Primary analyses utilized standardized variables and used hierarchical linear regression models. In the first step, we included gender as the sole predictor. In the second step, we added the FTND score as a covariate. In the third step, we added the other SCQ subscales as covariates. The final step, we added anxiety and depression covariates to the SCQ scales and the FTND. Demographic or smoking characteristics were not correlated with gender (Table 1) and were therefore not included as covariates in any analysis. Samples were analyzed separately and results reported as standardized regression coefficients (βs) with 95% confidence intervals (CIs). Significance was set at .05.
Table 1.
Baseline Demographic, Expectancies, and Anxiety and Depression in the Full Samples and by Gender
| Sample 1: non-treatment seeking, Los Angeles, CA, United States | Sample 2: treatment-seeking, Tallahassee, FL and Burlington, VT, United States | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Descriptive statistics, M (SD) or % | Correlationse | Descriptive statistics, M (SD) or % | Correlationse | |||||||
| Full sample (N = 278) | Female (n = 91) | Male (n = 187) | With male gender | With SCQ-NR | Full sample (N = 494) | Female (n = 237) | Male (n = 257) | With male gender | With SCQ-NR | |
| SCQ-NRa | 4.3 (1.7) | 4.8 (1.8) | 4.0 (1.7) | −.22*** | – | 5.7 (1.8) | 6.0 (1.8) | 5.4 (1.8) | −.18*** | – |
| SCQ-PRa | 4.5 (1.2) | 4.6 (1.2) | 4.5 (1.2) | −.01 | .53*** | 5.7 (1.5) | 5.7 (1.5) | 5.6 (1.6) | −.03 | .59*** |
| SCQ-WCa | 2.9 (2.0) | 3.4 (2.3) | 2.7 (1.9) | −.15* | .39*** | 4.2 (2.4) | 4.8 (2.4) | 3.6 (2.2) | −.26*** | .44*** |
| SCQ-NCa | 4.8 (1.2) | 4.9 (1.3) | 4.8 (1.1) | −.07 | .25*** | 6.5 (1.3) | 6.8 (1.3) | 6.3 (1.3) | −.16*** | .39*** |
| Anxietyb | 1.3 (0.38) | 1.3 (.4) | 1.3 (0.4) | −.04 | .28*** | 1.4 (0.5) | 1.4 (0.6) | 1.4 (0.5) | −.06 | .25*** |
| Depressionc | 2.4 (0.6) | 2.4 (.7) | 2.4 (0.6) | −.01 | .14* | 2.1 (0.7) | 2.1 (0.7) | 2.0 (0.6) | −.11* | .39*** |
| Age | 44.1 (10.7) | 43.2 (11.4) | 44.5 (10.4) | .06 | −.07 | 36.7 (13.5) | 37.9 (13.6) | 35.6 (13.4) | −.08 | −.15** |
| Raced | 49.5% | 49.0% | 49.8% | .00 | −.03 | 10.7% | 10.0% | 11.3% | −.03 | .19*** |
| Cigarettes/day | 17.4 (6.7) | 16.7 (6.4) | 18.0 (6.9) | .07 | .12* | 16.7 (10.1) | 15.4 (8.2) | 17.9 (11.4) | .08 | .02 |
| Age regular smoker | 18.9 (5.3) | 18.8 (4.6) | 5.5 (5.6) | .02 | −.08 | 17.4 (3.9) | 17.2 (3.9) | 17.6 (3.9) | .04 | −.15** |
| FTND | 5.5 (1.9) | 5.5 (1.8) | 1.5 (2.0) | .00 | .26*** | 5.2 (2.3) | 5.1 (2.3) | 5.3 (2.3) | .03 | .19*** |
FTND = Fagerström test of nicotine dependence; M = mean; NC = negative consequences; NR = negative reinforcement; PR = positive reinforcement; SCQ = smoking consequences questionnaire; SD = standard deviation; WC = weight control. Gender coded (0 = female, 1 = male).
aScores reflect mean response per item—possible range sample 1: 1 (not true of me at all) to 7 (very true of me); sample 2: 0 (completely unlikely) to 9 (completely likely).
bAnxiety was measured using the anxious arousal subscale of the Mood and Anxiety Symptom Questionnaire for sample 1 and the Panic subscale of the Inventory of Depression and Anxiety Symptoms in sample 2. Scores reflect mean response per item—possible range 1 (not at all) to 5 (extremely).
cDepression was measured using the anhedonic depression subscale of the Mood and Anxiety Symptom Questionnaire for sample 1 and the general depression subscale of the Inventory of Depression and Anxiety Symptoms in sample 2. Scores reflect mean response per item—possible range 1 (not at all) to 5 (extremely).
dBlack race coded as 1, other race coded as 2.
eRelations between two continuous variables reflect Pearson correlation coefficients. Relations between a binary and continuous variable reflect point-bisearial correlation coefficients. Relations between two binary variables reflect Phi coefficients.
*p < .05, **p < .01, ***p < .001.
Results
Preliminary Analyses
Demographics for the full sample and by gender are reported for each sample in Table 1. Gender and SCQ-NR were associated with each other and other SCQ subscales in both samples; there were no gender differences in demographics and smoking characteristics.
Primary Analyses
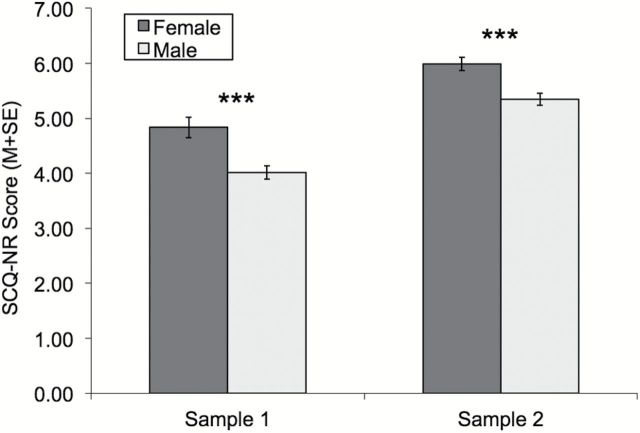
Figure 1 shows mean scores by gender and that female gender associated with stronger NR expectancies without any covariates in both samples (sample 1 β [95% CI] = −.22 [−.33, −.10], p <.001; sample 2 β [95% CI] = −.18 [−.27, −.09]; p < .001). After adding FTND score as a covariate, the predictive influence of gender remained (sample 1 β [95% CI] = −.22 [−.33, −.11], p <.001; sample 2 β [95% CI] = −.18 [−.27, −.10]; p < .001). Adding the other three smoking expectancies as covariates, the predictive effects of gender remained (sample 1 β [95% CI] = −.17 [−.27, −.08], p <.001; sample 2 β [95% CI] = −.08 [−.15, −.01], p = .02). When anxiety and depression were added as covariates in conjunction with SCQ scales and FTND, the effect of gender on NR expectancies was significant in sample 1 (β [95% CI] = −.17 [−.27, −.08], p <.001) and reduced to a non-significant trend in sample 2 (β [95% CI] = −.06 [−.13, .00]; p = .06).
Figure 1.
SCQ-NR score mean and standard error by gender in each sample. SCQ-NR = smoking consequences questionnaire negative reinforcement subscale. *** gender difference significant p < .001.
Discussion
Consistent with our hypothesis, females reported stronger NR expectancies than men in two independent samples. In Sample 2, Gender differences in NR expectancies were reduced to a trend after controlling for anxiety and depression. There is the possibility that sample differences after controlling for anxiety and depression were a result of exclusion of mood disorders in sample 1, but not in sample 2. This might have limited the variability in depression and anxiety covariates for sample 1 and reduced its predictive power. However, visual inspection of the range of scores of psychopathology measures across the samples did not suggest more range restriction for sample 1 versus sample 2, which potentially offsets this concern. Additionally, the consistency of the association between gender and NR expectancies in every other analysis and in sample 1 provides relatively strong evidence of a gender difference effect that is robust to other expectancies and also potentially robust to concomitant anxiety and depression. Furthermore, the 95% CIs surrounding the gender effect sizes (βs) overlapped for every analysis, suggesting that although the βs for the gender difference vacillated across different samples and levels of covariate adjustment, the presence and magnitude of the gender difference was generalizable.
These results are consistent with previous reports showing females express greater NR expectancies,10,12 and extend these findings to show that these relations exist independent of other cigarette expectancies and mood and anxiety symptoms. Furthermore, these findings are consistent with the idea that negative affect and negative affect reduction may be an important motivational factor driving smoking in women,1–3,6 and highlights a potential role for cognitive manifestations of this motivational process.
The results of this study need to be interpreted within the context of its limitations. This study used a cross sectional design, which means that the results do not allow for causal inferences and would benefit from research on longitudinal gender differences in expectancy trajectories. Second, the scales for the SCQ differed between samples. This most likely had limited impact on the findings because (a) the wording of the questions were identical in both measures with the only difference being the anchor labels for rating each item; (b) scales were standardized in the models; and (c) both scales addressed the likelihood of the consequence for the individual; thus they were most likely tapping the same information. Lastly, this paper did not link expectancies to actual smoking behavior. Hence, future work examining whether NR expectancies mediate gender differences in smoking behaviors would be useful to determine clinical and etiologic significance of the results reported here.
Despite these limitations this article may have important clinical applications for improving quit success in women. For one, these results suggest that treatment in women should focus on psychoeducation and behavioral techniques oriented on coping with negative affect without smoking as has been done with other addictive behavior.26 For example, addressing coping-oriented smoking as a “false safety aid” through alternative behavioral practice and psychoeducation may be a useful therapeutic strategy, especially for females.
Funding
This research was supported by funds from Tobacco-Related Disease Research Program of the University of California , Grant Number 22FT-0062 and by NIDA grants R01-DA026831 and R21-DA034768.
Declaration of Interests
None declared.
Acknowledgments
All authors contributed in a significant way to the manuscript and have read and approved the final manuscript.
References
- 1. Leventhal AM, Waters AJ, Boyd S, Moolchan ET, Lerman C, Pickworth WB. Gender differences in acute tobacco withdrawal: effects on subjective, cognitive, and physiological measures. Exp Clin Psychopharmacol. 2007;15:21–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pang RD, Leventhal AM. Sex differences in negative affect and lapse behavior during acute tobacco abstinence: a laboratory study. Exp Clin Psychopharmacol. 2013;21:269–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Xu J, Azizian A, Monterosso J, et al. Gender effects on mood and cigarette craving during early abstinence and resumption of smoking. Nicotine Tob Res. 2008;10:1653–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gunn RC. Reactions to withdrawal symptoms and success in smoking cessation clinics. Addict Behav. 1986;11:49–53. [DOI] [PubMed] [Google Scholar]
- 5. Perkins KA, Karelitz JL, Giedgowd GE, Conklin CA. Negative mood effects on craving to smoke in women versus men. Addictive Behav. 2012;38:1527–1531. S0306-4603(12)00229-8 [pii] 10.1016/j.addbeh.2012.06.002 [] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Weinberger AH, McKee SA. Gender differences in smoking following an implicit mood induction. Nicotine Tob Res. 2012;14:621–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brandon TH, Baker TB. The smoking consequences questionnaire: the subjective expected utility of smoking in college students. Psychol Assess. 1991;3:481–491. [Google Scholar]
- 8. Heinz AJ, Kassel JD, Berbaum M, Mermelstein R. Adolescents’ expectancies for smoking to regulate affect predict smoking behavior and nicotine dependence over time. Drug Alcohol Depend. 2010;111:128–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kristjansson SD, Pergadia ML, Agrawal A, et al. Smoking outcome expectancies in young adult female smokers: individual differences and associations with nicotine dependence in a genetically informative sample. Drug Alcohol Depend. 2011;116:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pulvers KM, Catley D, Okuyemi K, et al. Gender, smoking expectancies, and readiness to quit among urban African American smokers. Addict Behav. 2004;29:1259–1263. [DOI] [PubMed] [Google Scholar]
- 11. Wetter DW, Smith SS, Kenford SL, et al. Smoking outcome expectancies: factor structure, predictive validity, and discriminant validity. J Abnorm Psychol. 1994;103:801–811. [DOI] [PubMed] [Google Scholar]
- 12. Weinberger AH, McKee SA, George TP. Changes in smoking expectancies in abstinent, reducing, and non-abstinent participants during a pharmacological trial for smoking cessation. Nicotine Tob Res. 2010;12:937–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Urbán R, Demetrovics Z. Smoking outcome expectancies: A multiple indicator and multiple cause (MIMIC) model. Addict Behav. 2010;35:632–635. [DOI] [PubMed] [Google Scholar]
- 14. Zender R, Olshansky E. Women’s mental health: depression and anxiety. Nurs Clin North Am. 2009;44:355–364. [DOI] [PubMed] [Google Scholar]
- 15. Johnson KA, Zvolensky MJ, Marshall EC, Gonzalez A, Abrams K, Vujanovic AA. Linkages between cigarette smoking outcome expectancies and negative emotional vulnerability. Addict Behav. 2008;33:1416–1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Leyro TM, Zvolensky MJ, Vujanovic AA, Bernstein A. Anxiety sensitivity and smoking motives and outcome expectancies among adult daily smokers: replication and extension. Nicotine Tob Res. 2008;10:985–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Morrell HE, Cohen LM, McChargue DE. Depression vulnerability predicts cigarette smoking among college students: Gender and negative reinforcement expectancies as contributing factors. Addict Behav. 2010;35:607–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Leventhal AM, Trujillo M, Ameringer KJ, Tidey JW, Sussman S, Kahler CW. Anhedonia and the relative reward value of drug and nondrug reinforcers in cigarette smokers. J Abnorm Psychol. 2014;123:375–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR Axis I disorders, research version, non-patient edition. (SCID-I/NP). New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 20. Zvolensky MJ, Farris SG, Leventhal AM, Schmidt NB. Anxiety sensitivity mediates relations between emotional disorders and smoking. Psychol Addict Behav. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR Axis I disorders, research version, non-patient edition (SCIDI/NP). New York, NY: Biometrics Research, New York State Psychiatric Institute; 2007. [Google Scholar]
- 22. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119–1127. [DOI] [PubMed] [Google Scholar]
- 23. Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. J Abnorm Psychol. 1991;100:316–336. [DOI] [PubMed] [Google Scholar]
- 24. Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, McCormick RA. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. J Abnorm Psychol. 1995;104:3–14. [DOI] [PubMed] [Google Scholar]
- 25. Watson D, O’Hara MW, Simms LJ, et al. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychol Assess. 2007;19:253–268. [DOI] [PubMed] [Google Scholar]
- 26. Buckner JD, Zvolensky MJ, Schmidt NB, Carroll KM, Schatschneider C, Crapanzano K. Integrated cognitive behavioral therapy for cannabis use and anxiety disorders: rationale and development. Addict Behav. 2014;39:495–496. [DOI] [PMC free article] [PubMed] [Google Scholar]