Abstract
Background:
Cancer patients in lower socioeconomic groups are significantly less likely to die at home and experience more barriers to access to palliative care. It is unclear whether receiving palliative care may mediate the effect of socioeconomic status on place of death.
Aim:
This review examines whether and how use of specialist palliative care may modify the effect of socioeconomic status on place of death.
Design:
A systematic review was conducted. Eligible papers were selected and the quality appraised by two independent reviewers. Data were synthesised using a narrative approach.
Data sources:
MEDLINE, Embase, CINAHL, PsycINFO and Web of Knowledge were searched (1997–2013). Bibliographies were scanned and experts contacted. Papers were included if they reported the effect of both socioeconomic status and use of specialist palliative care on place of death for adult cancer patients.
Results:
Nine studies were included. All study subjects had received specialist palliative care. With regard to place of death, socioeconomic status was found to have (1) no effect in seven studies and (2) an effect in one study. Furthermore, one study found that the effect of socioeconomic status on place of death was only significant when patients received standard specialist palliative care. When patients received more intense care adapted to their needs, the effect of socioeconomic status on place of death was no longer seen.
Conclusion:
There is some evidence to suggest that use of specialist palliative care may modify the effect of socioeconomic status on place of death.
Keywords: Socioeconomic factors, palliative care, place of death, review, neoplasms
What is already known about the topic?
Cancer patients in lower socioeconomic groups are significantly less likely to die at home and experience more barriers to access to palliative care.
Intensity of home care including palliative care is associated with a home death.
It is not clear whether and how use of specialist palliative care may modify the effect of socioeconomic status (SES) on place of death in cancer patients.
What this paper adds?
There is some evidence to suggest that use of specialist palliative care may modify the effect of SES on place of death, thus contributing to the reduction of inequalities in achieving preferred home death.
There is a need for further observational research that fully utilises the existing service patterns and compares the effect of SES on place of death between users and non-users of specialist palliative care.
The common methodological challenges arise from the complexities in providing palliative care to diverse populations. These should be addressed in future research.
Implications for practice, theory or policy
Palliative and supportive care services potentially can help cancer patients to die at their preferred place especially if they adapt level of care to patients’ unique needs.
Introduction
Despite considerable differences in personal, family and cultural meanings associated with dying at home, the overwhelming majority (approximately two-thirds) of cancer patients identify their own home as the preferred place of death;1 and this trend has been found across all socioeconomic groups.2–4 However, the majority of deaths from all diseases/conditions in most Western countries occur in a hospital.1 In the United Kingdom, although the proportion of people with cancer dying at home has been increasing since 2004, hospital remains the most common place of death, and a great discrepancy still exists between the preferred and actual place of death for cancer patients.5,6
Furthermore, the ability to die at home is unequally distributed among cancer patients. Research evidence repeatedly demonstrates that cancer patients with higher socioeconomic status (SES) (e.g. better education, better occupation, higher income, living in more affluent or less deprived areas) are more likely than patients with lower SES to die at home rather than in an institution,1,6–9 and this pattern exists in countries with and without universal health care programmes.10
According to Grande et al.,7 differences in place of death based on SES may be associated with differences in access to palliative care services by different socioeconomic groups. They suggested that cancer patients in higher socioeconomic groups were more likely to die at home possibly because they were more able to access services which improved their chances of dying at home. In contrast, lower socioeconomic groups experience many barriers to access although their health care needs are greater than those of the general health care population.10 Lewis et al.10 identified barriers to access in four dimensions: availability, affordability, acceptability and geographical accessibility. For instance, barriers to access may arise from limited availability of services in deprived/poor areas (availability); inequi-table distribution of services – services far away from and thus hard to reach by those with greatest need (geographical accessibility); limits of informal care arrangements, stigma and mistrust, and communication and health literacy issues in lower socioeconomic groups (acceptability); and financial burdens for the poor accessing services (affordability). As such, lower socioeconomic groups are more likely to rely on acute care services during illness progression and significantly less likely to die at home, both in countries with or without universal health care programmes.10,11
However, it is not clear whether or not SES has the same effect on place of death when cancer patients receive specialist palliative care (see Box 1), having overcome the barriers to access; or how the effect of SES on place of death differs between those who receive specialist palliative care and those who do not. This systematic review of the worldwide literature therefore aims to examine whether or not and how use of specialist palliative care may modify the effect of adult cancer patients’ SES on place of death.
Box 1.
Palliative care is an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.
Source: World Health Organisation 2003
Specialist Palliative Care is the active, total care of patients with progressive, advanced disease and their families. Care is provided by a multi-professional team who have undergone recognised specialist palliative care training. The aim of the care is to provide physical, psychological, social and spiritual support …
Source: Tebbit, National Council for Palliative Care, 1999
Methods
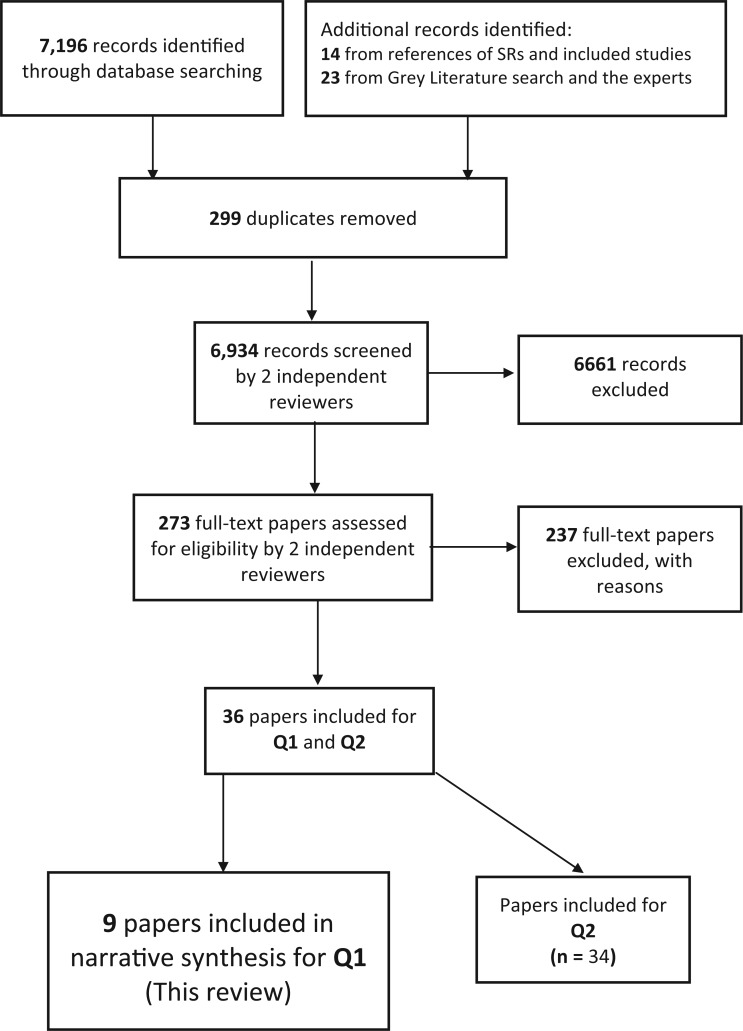
Two reviews (Q1 and Q2) were undertaken simultaneously, guided by the same protocol due to the overlap between their research questions. Q1 (this review) examines how use of specialist palliative care may modify the effect of adult cancer patients’ SES on place of death. Q2 examines how use of specialist palliative care may modify the effect of patients’ age, gender and ethnicity on place of death. Search was conducted separately for Q1 and Q2. However, search results were pooled together for a combined study selection (see Figure 1) because of overlapping data (i.e. some papers reported socio-demographic data which included SES, age, gender and ethnicity). The combined study selection helped to reduce the chance of missing eligible papers for both reviews. Once eligible papers were identified for each review, data extraction, quality appraisal and data synthesis were conducted separately. Q1 has been completed while Q2 is ongoing. This paper reports on Q1 in adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement (http://www.prisma-statement.org/statement.htm), where applicable.
Figure 1.
PRISMA flow chart for Q1 and Q2.
Information sources and searches
MEDLINE, Embase, CINAHL, PsycINFO and Web of Knowledge were searched (January 1997–December 2013). The search terms (MeSH headings and keywords) are summarised in Table 1 and the search strategy for MEDLINE and Embase is presented as an example in Appendix 1. Experts in the field were contacted to identify additional references; and the grey literature was searched using Caresearch (http://www.caresearch.com.au/Caresearch/Default.aspx). The reference lists of relevant reviews8–10,12 and the included studies13–21 were scanned to ensure comprehensiveness of the search. The review was limited to English language papers.
Table 1.
Search terms.
| Cancer | Palliative care | SES | Place of death |
|---|---|---|---|
| Neoplasm Malignancy Tumour Dying Terminal Incurable |
Terminal care End-of-life care Cancer care Home care Community care Nursing care Hospice care Day care Macmillan Marie Curie Inpatient care Outpatient care Supportive care |
Social class Class Inequality Deprivation Poor Poverty Disadvantage Occupation Education Income |
Location of death Home death Hospital death Hospice death Nursing home Aged care home Residential care home |
SES: socioeconomic status.
Study selection (combined for Q1 and Q2)
Two reviewers (D.J.N. and H.C.) screened all titles and abstracts independently. Full-text papers were retrieved for those eligible or indeterminable from titles and abstracts. Two reviewers (D.J.N. and H.C.) independently assessed the full text of all potentially relevant papers. Disagreement at each stage was resolved by consensus and with recourse to a third reviewer (M.J.) and a fourth (U.M.) if necessary.
Eligibility criteria
Papers were included if they reported original, empirical data showing the effect of both SES (e.g. income, education, occupation) and use of specialist palliative care (including hospice care, home care, inpatient or outpatient care) on place of death for adult cancer patients (⩾18 years). Papers were excluded if the diagnosis was unknown or if the paper reported only non-malignant disease; if the study focussed exclusively on children and on preferences or attitudes about place of death rather than actual place of death.
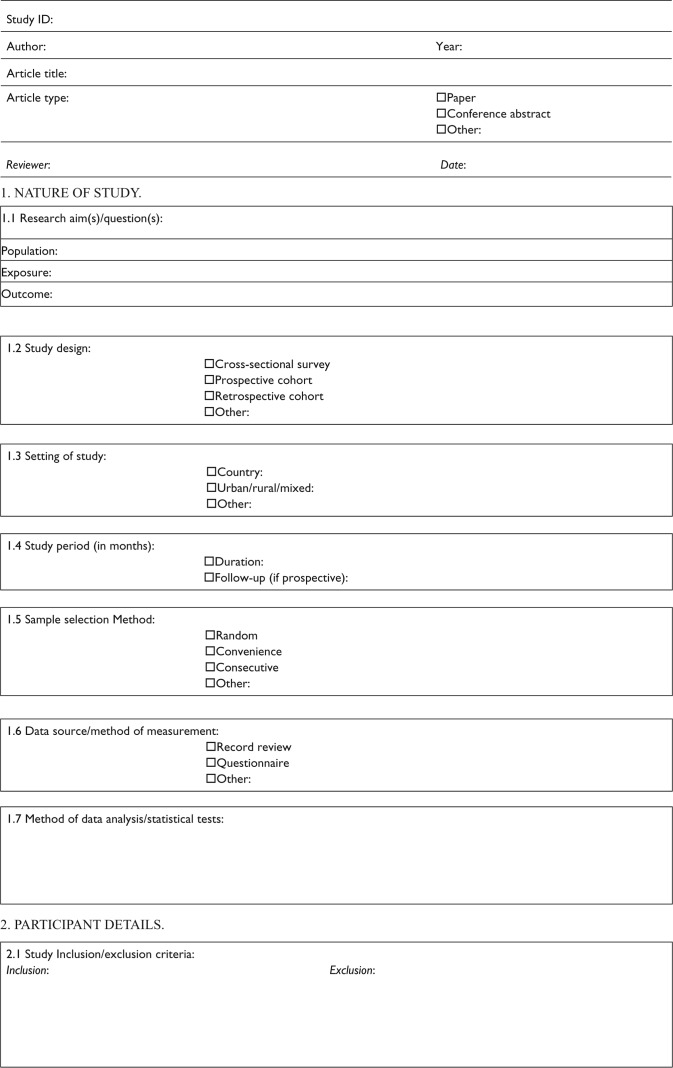
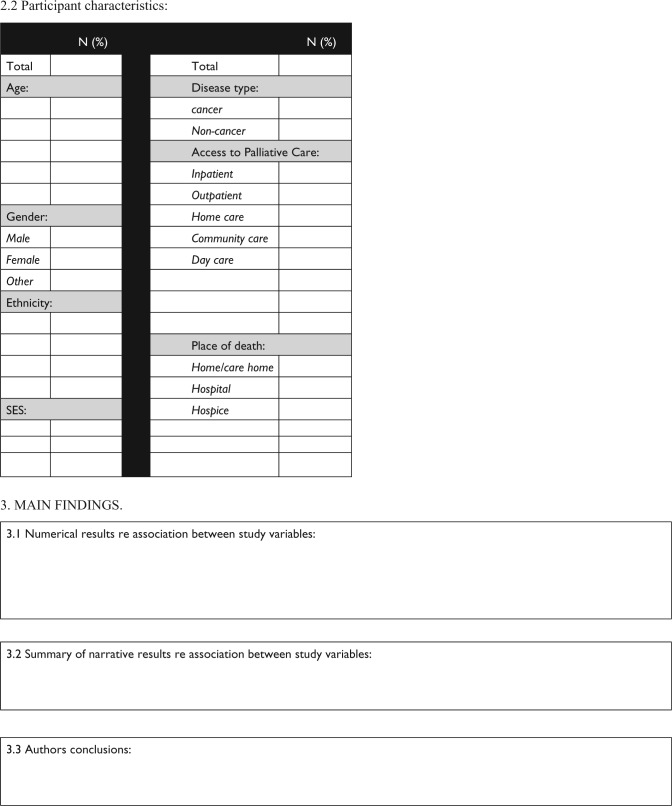
Data extraction
A data extraction form was designed and piloted using three papers and adjustments made following consensus among the research team. Data were independently extracted by two reviewers (D.J.N. and H.C.) for 10% of the papers using the post-pilot form (see Appendix 2). As there was good agreement, the remaining data extraction was completed by D.J.N. Information was extracted from each included study on design and methods, patient characteristics, measure of SES, type of specialist palliative care, place of death outcome, statistical results demonstrating the relationships between SES, specialist palliative care, place of death and so on. Unreported data or clarifications were requested from first authors.
Quality assessment
Quality assessment was conducted independently by two reviewers (D.J.N. and H.C.), using the Item Bank for Assessing Risk of Bias and Confounding for Observational Studies of Interventions or Exposures.22 Disagreement was resolved by team consensus. Main methodological components assessed include inclusion/exclusion criteria, strategy for recruiting participants, selection of the comparison group, variations in intervention/exposures, validity and reliability of measures, length of follow-up, attrition and control for confounding.
Narrative synthesis
All the included studies are non-randomised, observational studies, and there was considerable heterogeneity in methods, participants and outcomes. Under such circumstances, meta-analysis is not sensible and possible, and therefore, a narrative approach to synthesis is necessary and appropriate.23,24 Guidance on the Conduct of Narrative Synthesis in Systematic Reviews23 was followed, particularly with regard to tabulating results; exploring relationships between characteristics of individual studies and their reported findings, and between the findings of different studies; and overall assessment of the robustness of the evidence.
Results
Altogether, 7196 records were identified through database searching for both reviews (Q1 and Q2). Additional 37 records were identified through reference lists, grey literature search and the experts. After adjusting for duplicates, 6934 records remained. Of these, 273 full-text papers were retrieved and assessed in detail for inclusion for Q1 and Q2 (Figure 1). For this review (Q1), nine papers were included which reported nine different empirical studies (see Table 2).
Table 2.
Characteristics of included studies.
| Ref. | Design and methods | Population | SES | Palliative care | Place of death | Results |
|---|---|---|---|---|---|---|
| 13. | Prospective cohort study: patients and carers followed up from patient’s admission to death Patients from single service Logistic regression |
Spain 380 Patients Mean age 66.76 years 60.5% Male 100% Cancer |
Level of education: 9.5% No schooling 50.5% Primary 15.3% Secondary 5.3% High/higher 19.5% Unknown |
100% Home | 64% Home 19% Hospital 16% Hospice 1% Nursing home |
Univariate analysis: after receiving SPC, no differences found in place of death regarding patient’s education level |
| 14. | Retrospective cohort study: review of administrative and clinical database Patients from multiple services in multiple regions Logistic regression |
United States 61,063 Patients 77.7% ⩾65 years 48% Male 70.2% White 64.2% Cancer |
Family income: 1.8% ⩽US$20,000 11.6% >US$20,000–US$30,000 29.3% >US$30,000–US$40,000 24.4% >US$40,000–US$50,000 32.9% >US$50,000 |
Home: 54.9% routine care 45.1% continuous care |
77.4% Home 22.6% Elsewhere |
Multivariate analysis: among those who did not receive continuous care, the odds of non-home death increased as median annual household income decreased. Among those receiving continuous care, no significant difference was found in rates of non-home death across income levels. |
| 15. | Prospective cohort study: patients followed up from admission to death or end of study period Patients from multiple services in single region Cox proportional-hazards regression |
United States 180 Patients Mean age 67 years 49.4% Male 79.4% White 100% Cancer |
Family income (n = 142): 31.7% <US$20,000 39.4% ⩾US$2000 and <US$40,000 28.9% >US$40,000 |
100% Inpatient | 23.7% Home 40.8% Hospice 25% Hospital 10.5% Nursing home |
Bivariate analysis: the inpatient-hospice-death group and the censored group were comparable on family income |
| 16. | Cross-sectional survey of home hospice care agencies Patients from multiple services in multiple regions Logistic regression |
Japan 528 Patients Mean age 75 years 59.5% Male 100% Cancer |
Financial sufficiency: 40.7% yes 59.3% No |
100% Home | 64.8% Home 35.2% Hospital |
Univariate analysis: after receiving SPC, no differences found in place of death regarding patient’s financial situation |
| 17. | Cross-sectional survey of home hospice care agencies Patients from multiple services in multiple regions Logistic regression for multivariate analysis |
Japan 428 Patients Mean age 75 years 57.8% Male 100% Cancer |
Financial sufficiency: Proportion not reported |
100% Home | 64.8% Home 35.2% Hospital |
Univariate analysis: after receiving SPC, no differences found in place of death regarding patient’s financial situation |
| 18. | Cross-sectional survey of home hospice care agencies Patients from multiple services in multiple regions Logistic regression |
Japan 568 Patients Mean age 73 years 59.7% Male 100% Cancer |
Financial sufficiency: 47.4% yes 52.6% No |
100% Home | 54.9% Home 45.1% Hospital |
Univariate analysis: after receiving SPC, no differences found in place of death regarding patient’s financial situation |
| 19. | Prospective cohort study: patients, carers and family physicians followed up from patient’s admission to death Patients from single service Logistic regression |
Canada 73 Patients Mean age 68 years 48% Male 100% Cancer |
Financial resources sufficient (n = 67): 77.6% Yes 22.4% No |
100% Home | 47% home 53% Hospital + Hospice |
Univariate analysis: after receiving SPC, no differences found in place of death regarding patient’s financial situation |
| 20. | Prospective cohort study: primary carers followed up from patient’s admission to death Patients from single service Logistic regression |
Canada 110 Patients 55.5% ⩾70 years 46.4% Male 100% Cancer |
Carstairs Deprivation score: 24.8% ⩽ 0.5 25.7% 0.51–0.64 24.8% 0.65–1.07 24.8% ⩾ 1.08 |
100% Home | 66.4% Home 33.6% Hospital |
Univariate analysis: after receiving SPC, no differences found in place of death regarding patient’s deprivation level |
| 21. | Retrospective cohort study: review of hospice chart Patients from single service Multinomial logistic regression |
New Zealand 1268 Patients 72% > 65 years. 48% Male 82% European 82% Cancer |
Community Services Card: 42% Yes 28% No 30% Missing data |
100% Home+ other | 28% Home 46% hospice 8% hospital 16% care home |
Multivariate analysis: relative to those people without a CSC, people with a CSC were more likely to die at acute hospital than at home (OR = 2.09, 95% CI: 1.096–3.996) |
SES: socioeconomic status; SPC: specialist palliative care; CSC: Community Services Card; OR: odds ratio; CI: confidence interval.
Characteristics of included studies
Of the nine included studies, one was conducted in Spain,13 two in United States,14,15 three in Japan,16–18 two in Canada19,20 and one in New Zealand.21 These studies represent a total of 64,598 patients who received specialist palliative care, ranging from 7319 to 61,06314 patients in an individual study. The majority of the patients had cancer, were White and were aged 65 years and over (see Table 2).
With the exception of one study,14 all aimed to identify factors that are associated with place of death for patients who had received specialist palliative care. Only one study14 specifically examined the relationship between income and intensity of specialist palliative care provision as a predictor of place of death for patients who received home-based specialist palliative care.
All studies are observational, comprising four prospective cohort studies,13,15,19,20 two retrospective cohort studies14,21 and three cross-sectional surveys.16–18 Two studies collected data by extracting them from administrative or clinical database/record;14,21 four studies used a self-developed questionnaire, which was completed by patients, carers and/or health care professionals with or without researcher’s assistance;16–19 and two studies did not describe how data were collected.13,15 Multivariate logistic regression was used to control for confounding variables, except in one study that used Cox proportional-hazards regression.15 The confounding variables taken into account differ and vary greatly across studies.
Patients’ SES was measured in a variety of ways: education in the Spanish study;13 family/household income in the American studies;14,15 financial resources in a Canadian study19 and in the Japanese studies;16–18 Carstairs deprivation Score25 in another Canadian study;20 and a Community Services Card in the New Zealand study.21
All of the patients in the included studies received specialist palliative care. In one study,15 patients received inpatient palliative care provided by freestanding hospices or dedicated units located in hospitals. In another study,21 patients received home palliative care in addition to outpatient and/or inpatient palliative care. In the remaining seven studies, patients received home palliative care.
Categorisation of place of death differs in the studies. All the studies have home as an outcome of place of death, which is compared with ‘hospital, hospice and aged/residential care home’ in three studies,13,15,21 with ‘other than home’ in one study,14 with ‘hospital + hospice’ in one study19 and with ‘hospital’ in four studies.16–18,20
Common methodological limitations included sample unrepresentative, insufficient controlling for confounding factors and imprecise measurement of SES and use of specialist palliative care, all of which exist in the included studies in varying degrees (see ‘Discussion’).
Does use of specialist palliative care modify the effect of SES on place of death?
In seven studies (sample size: 73–568 patients), univariate or bivariate analysis found no statistically significant differences in place of death regarding SES among patients who received home care13,16–20 or inpatient care15 (see Table 2). Two studies14,21 did find statistically significant differences in place of death regarding SES.
Taylor et al.21 found SES to be a predictive factor of place of death for patients receiving specialist palliative care. In this study, retrospective administrative data were obtained from a hospice in New Zealand. Although 1268 patients were included, only 890 patients had information recorded about whether or not they had a Community Services Card (CSC). Having a CSC is a crude indicator of lower SES. Multivariate analysis of these patients (controlling for age, ethnicity, marital status, gender and medical condition) showed that relative to those people without a CSC, people with a CSC were more likely to die at acute hospital than at home (odds ratio (OR) = 2.09, 95% confidence interval (CI): 1.096–3.996). There was no significant difference between those with/without a CSC regarding likelihood of dying in an aged/residential care facility relative to home (OR = 1.50, 95% CI: 0.88–2.565). Likewise, there was no evidence for CSC status to differentiate between likelihood of dying in the hospice inpatient unit relative to home (OR = 1.00, 95% CI: 0.71–1.42).
Barclay et al.’s14 was the largest study, which included 61,063 patients (64.2% with cancer). It was a retrospective administrative dataset obtained from a hospice provider that operated 26 hospice programmes in eight states in the United States. Altogether, 77.4% of 61,063 patients died at home. Two levels of home care (routine versus continuous) were provided to these patients based on their needs; 54.9% of the patients received routine home care only (periodic home visits) and 45.1% received continuous home care, that is, a short-term intense period of care that included the presence of hospice staff providing care for a minimum of 8 h in a 24-h period, with at least half the care provided by a nurse. In the multivariate model, the income × level of care interaction was significant in predicting place of death, after controlling for confounding factors including sex, age, ethnicity, marital status, disease type, payment source, enrolment in a health maintenance organisation, relationship of the primary caregiver to the enrolee, days in hospice care and hospice programme location by region. In the routine-care group, the odds of non-home death increased as median annual household income decreased. Those in the lowest income group compared with those in the highest income group had almost twice the odds of dying elsewhere rather than home (OR = 1.76, 95% CI: 1.48–2.09). In comparison, in the continuous-care group, no significant difference was found in rates of non-home death across income levels; and for all income levels, a smaller proportion of those receiving any continuous care (vs no continuous care) died elsewhere rather than home.
Discussion
Gomes and Higginson8 found strong evidence for the association of SES (i.e. education, social class, income) with place of death for patients with cancer. They found that the evidence that supported the influence of SES was stronger than the evidence that showed no effect, suggesting that higher SES increased the odds of home death. They also found strong and consistent evidence to suggest that intensity of home care (more home care input and more frequent visits) was associated with a home death. However, their review did not examine the link between the two associations, that is, whether or not SES and intensity of home care may interact together to impact on place of death in cancer patients. This review is particularly interested in whether or not and how use of specialist palliative care may modify the effect of SES on place of death. The majority of the included studies (seven) found that SES had no effect on place of death among users of home-based specialist palliative care13,16–20 or inpatient specialist palliative care.15 Only one study found that SES had an effect on place of death among users of specialist palliative care (home, outpatient and/or inpatient).21 However, the biggest study14 (n = 61,063) found that the effect of SES on place of death was only significant when patients received standard home-based specialist palliative care. When patients received more intense home care that was adapted to their needs, SES stopped having an effect on place of death. Moreover, intensity of home care adapted to patients’ needs particularly at the end of life increased the chance of home death across all socioeconomic groups. Particularly, for patients in lower socioeconomic groups, more intense home care meant that they had a higher chance of home death despite the fact that they had been identified as having increased needs. These findings thus suggest that use of specialist palliative care may modify the effect of SES on place of death and thus help to reduce inequalities in achieving preferred home death.
Nonetheless, definite conclusions cannot be reached because not only is there a paucity of empirical studies identified but also considerable heterogeneity exists in the study characteristics. Moreover, all the studies had some methodological weakness, which may have contributed to underestimates or overestimates of the actual effect of SES and use of specialist palliative care on place of death.
Selection bias was common. In four studies,13,19–21 patients were recruited from a single service; even in studies where patients were recruited from multiple services in one region15 or in multiple regions,14,16–18 findings may not be generalisable to other populations or geographical areas, since palliative care services and health and social care environments differ in different areas, regions in the same country and between countries.
Another major methodological problem is controlling for confounding variables because there is a complicated network of factors that affect both use of specialist palliative care services and place of death.8,26 These factors fall into three groups: those related to the illness, the individual and the care and social environment.8 Both studies,14,21 in which SES was entered into the multivariate regression model as a significant predictor of place of death, lacked specific patient, clinician, health system or environmental variables that might represent important sources of residual confounding.27
One of the key variables of this review – SES – is a complex concept that often refers to the position of individuals, families, households or other aggregates on one or more dimensions of stratification.28 These dimensions include income, education, prestige, wealth or other aspects of standing that members of society deem salient. Each of these dimensions is capable of exerting separate effects although they are interrelated. Bollen et al.28 found that although SES was widely referred to in health and health care research, there is a lack of consensus with respect to its conceptual meaning and measurement. The same problem persists in this review. SES was measured differently across studies – by different singular or aggregated dimensions (i.e. education, household income, financial resources and deprivation). As such, outcomes of SES are not comparable across studies. Also, data availability clearly influenced the ways in which SES was measured, leading to imprecise and ambiguous measurement (e.g. Community Services Card).
With regard to use of specialist palliative care, practice variations prevail in and across the studies. First, the composition of multi-disciplinary team differed across the studies that reported such information: in the Spanish study, it consisted of doctor, advanced nurse, assistant nurse and administrative clerk;13 in an American study, it consisted of doctor, nurse, home health aide, chaplain and social worker;14 in a Canadian study, it consisted of nurse, social worker, occupational therapist, physical therapist, respiratory therapist and volunteers;19 in the Japanese studies, it consisted of home care nurse and patient’s family doctor and/or hospital doctor;16–18 in the New Zealand study, it consisted of doctor, nurse, chaplain, social worker, counsellor and music, massage, occupational and physiotherapists.21 Second, the frequency and intensity of periodic home care varied. In some studies, level of care was adapted to the needs of patients and families; for example, in an American study, a short-term intense period of care was provided to patients at the end of life, which included a minimum of 8-h care in a 24-h period, with at least half the care provided by a nurse;14 in a Canadian study, 4–5 h/day or more of services can be provided to patients with advanced disease and 24-h nursing and personal care may be provided for a short period at end of life.19 Third, palliative care services were provided free of charge in Spain, Canada and New Zealand, whereas in United States and Japan, they were mainly covered by medical insurance. Such varying practices were not sufficiently reflected in the measures for the use of specialist palliative care.
In all, this review found some evidence to suggest that use of specialist palliative care may modify the effect of SES on place of death and is the first to synthesise such evidence. The general implication of the findings for practice is that palliative and supportive care services potentially can help cancer patients in all socioeconomic groups to die at their preferred place, especially if they adapt level of care to patients’ unique needs. The review also identified a need for more rigorous empirical evidence in this area and highlighted the methodological issues to be dealt with in future research. Due to the challenges in the use of randomised controlled trial designs, observational data sources and study designs will continue to be strong contributors to building the evidence base for palliative care research and practice.27 As such, future observational research needs to consider how to (1) reduce selection bias; (2) collect data about a myriad of confounding factors, particularly those related to the individual and the care and social environment; (3) better define and measure SES; and (4) more precisely measure use of specialist palliative care to reflect practice variations and complexities in service provision. To further ascertain that use of specialist palliative care can modify the effect of SES on place of death, a better design would be to utilise existing patterns of practice and prospectively or retrospectively compare the effect of SES on place of death between users and non-users of specialist palliative care.
Conclusion
There is some evidence to suggest that use of specialist palliative care may modify the effect of SES on place of death, thus contributing to reducing inequalities in achieving the preferred home death. This also means that palliative and supportive care services potentially can help cancer patients die at their preferred place by adapting level of care to their unique needs. However, more rigorous empirical studies are needed to further confirm this finding. Future observational studies need to fully utilise the existing service patterns and compare the effect of SES on place of death between users and non-users and also pay more attention to selection bias, controlling for confounding factors and measurement of SES and use of specialist palliative care.
Acknowledgments
We thank Ms Helena Sinclair and Mr Peter English for admin support. We thank Jennifer Tieman, Debbie Marriott and David Currow for providing access to Caresearch; Irene Higginson and other experts for providing valuable advice and relevant information.
Appendix 1
Search strategy–MEDLINE and Embase
(MEDLINE and Embase Jan 1997–Dec 2013)
exp Neoplasm/
Neoplasm*.mp.
cancer*.mp. [mp=ti, ab, sh, hw, tn, ot, dm, mf, dv, kw, nm, kf, ps, rs, ui]
or/1-3
exp Social Class/
Social Class*.mp.
Socio-econom*.mp.
socioeconom*.mp.
Inequalit*.mp. [mp=ti, ab, sh, hw, tn, ot, dm, mf, dv, kw, nm, kf, ps, rs, ui]
exp Poverty/
poverty.mp.
or/5-11
exp Hospices/
Hospic*.mp.
exp Terminal care/
Terminal care.mp.
exp Palliative care/
Palliat$.mp.
exp End-of-life/
place of death.adj
location.mp. [mp=ti, ab, sh, hw, tn, ot, dm, mf, dv, kw, nm, kf, ps, rs, ui]
Hospitals/
Hospitals.mp.
Health Services Access*.mp. [mp=ti, ab, sh, hw, tn, ot, dm, mf, dv, kw, nm, kf, ps, rs, ui]
exp Inpatient/
Inpatient.mp.
exp Outpatient/
Outpatient.mp.
or/13-28
4 and 12 and 29
limit 30 to English language
limit 31 to yr=‘1997–Current’
limit 32 to humans
remove duplicates from 33
Appendix 2
Data extraction form
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: This work was supported by a University of Hull Endowment award from Yorkshire Cancer Research (Ref: HEND001).
References
- 1. Tang ST, McCorkle R. Determinants of place of death for terminal cancer patients. Cancer Invest 2001; 19(2): 165–180. [DOI] [PubMed] [Google Scholar]
- 2. Foreman LM, Hunt RW, Luke CG, et al. Factors predictive of preferred place of death in the general population of South Australia. Palliative Med 2006; 20: 447–453. [DOI] [PubMed] [Google Scholar]
- 3. Decker SL, Higginson IJ. A tale of two cities: factors affecting place of cancer death in London and New York. Eur J Public Health 2007; 17: 285–290. [DOI] [PubMed] [Google Scholar]
- 4. Higginson IJ, Costantini M. Dying with cancer, living well with advanced cancer. Eur J Cancer 2008; 44: 1414–1424. [DOI] [PubMed] [Google Scholar]
- 5. Gomes B, Calanzani N, Higginson IJ. Reversal of the British trends in place of death: time series analysis 2004–2010. Palliative Med 2012; 26(2): 102–107. [DOI] [PubMed] [Google Scholar]
- 6. Gao W, Ho YK, Verne J, et al. Changing patterns in place of cancer death in England: a population-based study. PLoS Med 2013; 10(3): e1001410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grande GE, Addington-Hall JM, Todd CJ. Place of death and access to home care services: are certain patient groups at a disadvantage? Soc Sci Med 1998; 47: 565–579. [DOI] [PubMed] [Google Scholar]
- 8. Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ 2006; 332(7540): 515–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gill A, Laporte A, Coyte PC. Predictors of home death in palliative care patients: a critical literature review. J Palliat Care 2013; 29(2): 113–118. [PubMed] [Google Scholar]
- 10. Lewis JM, DiGiacomo M, Currow DC, et al. Dying in the margins: understanding palliative care and socioeconomic deprivation in the developed world. J Pain Symptom Manag 2011; 42(1): 105–118. [DOI] [PubMed] [Google Scholar]
- 11. Higginson IJ, Jarman B, Astin P, et al. Do social factors affect where patients die: an analysis of 10 years of cancer deaths in England. J Public Health Med 1999; 21(1): 22–28. [DOI] [PubMed] [Google Scholar]
- 12. Ahmed N, Bestall JC, Ahmedzai SH, et al. Systematic review of the problems and issues of accessing specialist palliative care by patients, carers and health and social care professionals. Palliative Med 2004; 18(6): 525–542. [DOI] [PubMed] [Google Scholar]
- 13. Alonso-Babarro A, Bruera E, Varela-Cerdeira, et al. Can this patient be discharged home? Factors associated with at-home death among patients with cancer. J Clin Oncol 2011; 29(9): 1159–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Barclay JS, Kuchibhatla M, Tulsky JA, et al. Association of hospice patients’ income and care level with place of death. JAMA Intern Med 2013; 173(6): 450–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tang ST, McCorkle R, Bradley EH. Determinants of death in an inpatient hospice for terminally ill cancer patients. Palliat Support Care 2004; 2(4): 361–370. [DOI] [PubMed] [Google Scholar]
- 16. Fukui S, Kawagoe H, Masako S, et al. Determinants of the place of death among terminally ill cancer patients under home hospice care in Japan. Palliative Med 2003; 17(5): 445–453. [DOI] [PubMed] [Google Scholar]
- 17. Fukui S, Fukui N, Kawagoe H. Predictors of place of death for Japanese patients with advanced-stage malignant disease in home care settings: a nationwide survey. Cancer 2004; 101(2): 421–429. [DOI] [PubMed] [Google Scholar]
- 18. Fukui S, Fujita J, Tsujimura M, et al. Predictors of home death of home palliative cancer care patients: a cross-sectional nationwide survey. Int J Nurs Stud 2011; 48(11): 1393–1400. [DOI] [PubMed] [Google Scholar]
- 19. Cantwell P, Turco S, Brenneis C, et al. Predictors of home death in palliative care cancer patients. J Palliat Care 2000; 16(1): 23–28. [PubMed] [Google Scholar]
- 20. Masucci L, Guerriere DN, Cheng R, et al. Determinants of place of death for recipients of home-based palliative care. J Palliat Care 2010; 26(4): 279–286. [PubMed] [Google Scholar]
- 21. Taylor EJ, Ensor B, Stanley J. Place of death related to demographic factors for hospice patients in Wellington, Aotearoa New Zealand. Palliative Med 2012; 26(4): 342–349. [DOI] [PubMed] [Google Scholar]
- 22. Viswanathan M, Berkman ND, Dryden DM, et al. Assessing risk of bias and confounding in observational studies of interventions or exposures: further development of the RTI item bank (No.13-EHC106-EF). Rockville, MD: Agency for Healthcare Research and Quality, 2013. [PubMed] [Google Scholar]
- 23. Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. Swindon: ESRC Research Methods Programme, 2006. [Google Scholar]
- 24. Centre for Reviews and Dissemination (CRD). Systematic reviews: CRD’s guidance for undertaking reviews in health care. York: CRD, University of York, 2008. [Google Scholar]
- 25. Carstairs V, Morris R. Deprivation and health in Scotland. Aberdeen: Aberdeen University Press, 1991. [Google Scholar]
- 26. Murray MA, Fiset V, Young S, et al. Where the dying live: a systematic review of determinants of place of end-of-life cancer care. Oncol Nurs Forum 2009; 36(1): 69–77. [DOI] [PubMed] [Google Scholar]
- 27. Starks H, Diehr P, Curtis JR. The challenge of selection bias and confounding in palliative care research. J Palliative Med 2009; 12(2): 181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bollen KA, Glanville JL, Stecklov G. Socioeconomic status and class in studies of fertility and health in developing countries. Annu Rev Sociol 2001; 27: 153–185. [Google Scholar]