Abstract
Background:
Residents living in long-term care facilities are a vulnerable population. For many residents, a nursing home is their place of death. Palliative care and end-of-life decisions are important components of their care provision.
Aim:
To study the views of cognitively able residents and relatives on advance care planning, end-of-life care, and decision-making in nursing homes.
Design:
A qualitative study with in-depth interviews with nursing home residents and focus group interviews with relatives of nursing home residents. Analysis is based on interpretive description.
Setting/participants:
In total, 43 informants from nine nursing homes participated in the study (25 nursing home residents and 18 relatives). All included residents had capacity to provide informed consent and lived in long-term care.
Results:
The main findings of this study were the differing views about decision-making and advance care planning of residents and relatives. Residents do trust relatives and staff to make important decisions for them. The relatives are in contrast insecure about the residents’ wishes and experience decision-making as a burden. The majority of the residents had not participated in advance care planning. None of the residents stated challenges connected to end-of-life care or mentioned the wish for euthanasia.
Conclusion:
Although most residents seem to be satisfied with decision-making and end-of life care, there is a need for systematic advance care planning. Advance care planning could help to explore future wishes for care and ease decision-making for the relatives, physicians, and staff and should be offered to all cognitively able nursing homes residents.
Keywords: Nursing homes, long-term care, residential facilities, end-of-life care, decision-making, palliative care, advance care planning, family
What is already known about the topic?
Many people die in nursing homes.
Nursing homes provide palliative care at the end of life.
Systems for advance care planning (ACP) and inclusion of residents and relatives in end-of-life decision-making are unsatisfactorily implemented in many nursing homes.
What this paper adds?
Residents trust their relatives, physicians, and nurses to make decisions for them, but in contrast many relatives do not know for sure what their next of kin really wants.
Talking about death and dying in general and especially about the residents’ preferences for treatment and decision-making in end-of-life care are paramount and should be addressed by the staff in order to maintain autonomy and dignity.
Although some nursing home residents stated a wish to die, none expressed the wish for euthanasia or physician-assisted suicide.
Implications for practice, theory, or policy
Physicians and nursing home staff should engage in ACP and offer the opportunity to discuss death, dying, and wishes for care and treatment at the end of life with nursing home residents and when the resident agrees with their next of kin.
Although most residents and relatives are willing to talk about ACP, they are reluctant to start a conversation on that topic.
Most nursing home residents are unaware that ACP is an option; thus, staff should ensure to offer residents opportunities for these discussions.
Introduction
Older people often need nursing home or home-based care due to multimorbidity and frailty.1 Across different countries, similar issues need to be addressed. For example, about 70%−80% of nursing home residents in the United Kingdom and Norway suffer from cognitive impairment or dementia.2,3 For many people, a nursing home is their place of death. In the United Kingdom, 35% of the people died in care homes or at home in 2006.4 In the United Kingdom, between 2001 and 2010 55% of people suffering from dementia died in care homes.5 In Norway, 48% of all deaths occurred in long-term care facilities and 15% at home in 2012.6 There are numerous ethical challenges in nursing homes.7–9 Nursing homes are places where end-of-life care is provided. Providing end-of-life care involves overcoming various challenges. One such challenge is advance care planning (ACP). ACP is a process with discussion between an individual and a carer (relative, nurse, and physician) to ensure that the individuals’ wishes and preferences are known.10–13 Definitions of ACP are provided in Box 1. The practice and legal framework of ACP differs between countries and may include repeated discussions with relatives, nurses and physicians; appointment of a substitute decision maker; and use of written advance directives. The use of ACP has a positive influence on the quality of end-of-life care.11 Unfortunately, ACP is not yet widely used in nursing homes, and decision-making in end-of-life care may therefore lead to conflicts between the staff and relatives.8,14 Norwegian legislation allows relatives to consent to medical treatment if a patient is unable to make decisions.14 Residents with capacity can decide whether their relatives shall be included in ACP and decision-making.15,16 Although some elderly Norwegians do have their wishes for future care and participation of relatives in decision-making, ACP is not standard.15
Box 1. Advance care planning—definitions.
“Advance care planning (ACP) aims to help patients establish decisions about future care that take effect when they lose capacity.” (Mullick et al.)12
“ACP is a process of discussion between an individual and their care provider, and this may also include family and friends.” (Thomas and Lobo)10
“ACP is a voluntary process of discussion and review to help an individual who has capacity to anticipate how their condition may affect them in the future. If they wish, they can set on record choices or decisions about their care and treatment so that these can then be referred to by those responsible for their care or treatment (whether professional staff or family carers) in the event that they lose capacity to decide once their illness progresses. ACP has three possible outcomes: a verbal or written advance statement of wishes and feelings, beliefs and values—a verbal or written advance decision to refuse treatment (ADRT) (must be written with specific requirements if refusing life-sustaining treatment- see below)—a lasting power of attorney.” (NHS England)13
“ACP is defined as a process of discussion between an individual and their care provider, irrespective of discipline. If the individual wishes, their family and friends may be included.” (Holman and Hockley)16
Aim
The aim of this study was to explore the views of cognitively able residents and relatives from Norwegian nursing homes on ACP, decision-making, and end-of-life care. We were particularly interested in the views on participation in decision-making and in end-of-life care.
Methods
Ethics approval and ethical considerations
This study was approved by the Regional Ethics Committee (REK Sør-Øst A, Norway, reference 2009/1339a). All participants gave their written informed consent after receiving both oral and written information about the study. All participants were informed about their right to end the interview at any time without the need to explain the reasons for doing so and without consequences.
Design
A qualitative study design based on interpretive description described by Thorne17 was used. An interview setting with semi-structured in-depth interviews18,19 with Norwegian nursing home residents and focus group interviews with relatives of nursing home residents were conducted by the first researcher (G.B.). The focus group interviews with relatives were undertaken after primary analysis of the first 11 resident interviews. Box 2 provides an overview over the opening questions used. Reflexivity was sought through repeated comparison of the researchers’ presuppositions with the results, using critical reflection and metapositions19 as well as repeated discussions with the co-authors about alternative interpretations of the results. We followed the consolidated criteria for reporting qualitative studies (COREQ) guidelines for reporting qualitative research (details in Table 1).
Box 2. Opening questions for the interviews.
Opening questions for resident semi-structured interview
Have you thought about death and dying?
Have you talked about critical illness, death, and preferences for care at the end of life with your relatives?
Have you talked about critical illness, death, and preferences for care at the end of life with the nursing home staff (nurses or nurse aids) or your family doctor?
Have you been involved in planning for care in critical medical situations or the end of life (advance care planning (ACP))?
- If you were not able to decide for yourself anymore due to disease or loss of consciousness …
- Who shall make decisions for you?
- Are your relatives/next of kin able to decide for you?
- Do your relatives know what you would want?
Opening questions for relatives focus group interview
Have you talked critical illness, death, and preferences for care at the end of life (ACP) with your relative who lives in the nursing home?
Do you know what your relative would want if he or she would become critically ill?
Do you know which type of care or treatment your relative would want at the end of life?
Are you able to explain/define your relatives’ wishes if they will not be able to do it themselves anymore?
Table 1.
Report on accordance with the COREQ guidelines—checklist for reporting qualitative research.
| No item | Description |
|---|---|
| Domain 1: research team and reflexivity | |
| Personal characteristics | |
| 1. Interviewer/facilitator | G.B. conducted all interviews and focus groups. |
| 2. Credentials | The first author and researcher G.B. was a PhD student, medical doctor (MD), and Master of Advanced Studies (MAS) in Palliative Care specialized in Palliative Medicine and Nursing home medicine; E.G. and J.H.R. hold both a PhD and work as professors at the University of Bergen, Norway. |
| 3. Occupation | G.B. was working both as nursing home physician and consultant in Palliative Medicine at Bergen Red Cross Nursing Home in Bergen, Norway, and as PhD student at the University of Bergen, Norway. |
| 4. Gender | G.B. and J.H.R. are male and E.G. is female. |
| 5. Experience and training | The main investigator G.B. was a MD specialized in Anesthesiology, Palliative Medicine, and Nursing Home Medicine and had experience in research from different areas including quantitative and qualitative research. He received a German doctoral degree (Dr. med.) from the University of Cologne, Germany, in 2000. In addition, he underwent additional formal PhD education in Norway in qualitative research and medical ethics. |
| Relationship with participants | |
| 6. Relationship established | There was no relationship between the researcher/interviewer and the participants. No participants were recruited from the nursing home where G.B. was working as nursing home physician in order to avoid ethical problems and bias grounded on dependence issues. |
| 7. Participant knowledge of the interviewer | The participants did get information that the interviewer was researcher from the University of Bergen and that the goals of the research were to investigate residents and relatives views on living in nursing homes including ethical challenges and their opinion on ACP, end-of-life care, and decision-making in nursing homes. When the residents asked, G.B. told more about his background being both researcher and nursing home physician. |
| 8. Interviewer characteristics | The article includes information about the professional background of the interviewer. The main interest of G.B. in the topic was grounded in his daily work in Nursing Home Care and Palliative Care with experience of challenges related to ethical problems and end-of-life care in the nursing home. |
| Domain 2: study design | |
| Theoretical framework | |
| 9. Methodological orientation | The framework of the study was Palliative Care and Hospice philosophy. The basis for the qualitative methods used was interpretive description as described by Thorne. |
| Participant selection | |
| 10. Sampling | Purposive sampling aiming for geographical spread and different sizes and locations of the included nursing homes was used in this study. All approached nursing homes agreed to participate. |
| 11. Method of approach | The participants were selected and approached face-to-face by nursing home staff (e.g. nurses, nursing home physicians) from nine different nursing homes. They did receive written information about the study and had the opportunity to ask clarifying questions before the interview started. Capacity to decide was based on clinical observation and communication with the resident. Nursing home staff who chose residents to participate did know the informants through their daily work. The residents were not formally tested to assess their cognitive function. |
| 12. Sample size | In total, 43 informants participated in the study: 25 nursing home residents from nine nursing homes and 18 relatives from three of the nine nursing homes. Purposive sampling was used. No resident or relative withdrew from the study. |
| 13. Non-participation | Only one resident who was included in the study had to be excluded due to cognitive impairment detected by the researcher G.B. |
| Setting | |
| 14. Setting of data collection | The data were collected in nine different Norwegian nursing homes. All interviews were conducted in private without participation of staff from the actual nursing home in order to open up for possible negative comments. Data collection was terminated due to data saturation in the collected material. |
| 15. Presence of non-participants | No one else was present beside the participants and the researcher. |
| 16. Description of sample | The sample is described in the ‘Methods’ section. The participants’ characteristics are described in Table 2. |
| Data collection | |
| 17. Interview guide | Opening questions used in the interviews are shown in Box 2. |
| 18. Repeat interviews | Due to the age and often present multimorbidity of the participants as well as long distances between the researcher and the informants, no repeated interviews were carried out. |
| 19. Audio/visual recordings | All interviews were digitally recorded and stored on a computer according to the rules, regulations, and recommendations of the Regional ethics committee. |
| 20. Field notes | The researcher G.B. made field notes during and after the interviews. These included personal impressions and other observations that were not recorded. Field notes were used in the analysis to question and prove the findings. |
| 21. Duration | The duration of the interviews with nursing home residents varied from 10 to 71 min. The shortest interview was of a resident who was excluded due to cognitive impairment which became apparent during the interview. |
| 22. Data saturation | Data saturation was reached for the resident interviews and the focus group discussions. Due to space restriction, this has not been discussed in this article. |
| 23. Transcripts returned | Due to practical reasons (old age of the participants, no possibility to use Internet communication, and long distance between the researcher and the participants), the transcripts were not returned to the participants for comments. |
| Domain 3: analysis and findings | |
| Data analysis | |
| 24. Number of data coders | All three authors participated in coding of the data. |
| 25. Description of the coding tree | We did not use a coding tree. Themes derived from the data. |
| 26. Derivation of themes | Themes derived from the data and were discussed and agreed on by all the authors. |
| 27. Software | Verbatim transcription of the digital interview recordings was supported by the transcription software f4 from audiotranskription. Analysis and coding of the transcripts were aided by the software QSR NVivo 9. |
| 28. Participant checking | There was no feedback from the participants on the findings (due to practical reasons as explained above). At the end of the interviews, the interviewer gave a short summary of the interview content and asked clarifying questions. This made it possible to enable the informant to check whether the researcher did understand the main content right. |
| Reporting | |
| 29. Quotations presented | Themes are presented and illustrated by participant quotations that are identified by a participant number. The participant number does not correspond with the number from Table 2 in order to protect the participants and to ensure confidentiality. |
| 30. Data and findings consistent | The presented data and findings are consistent from our point of view. |
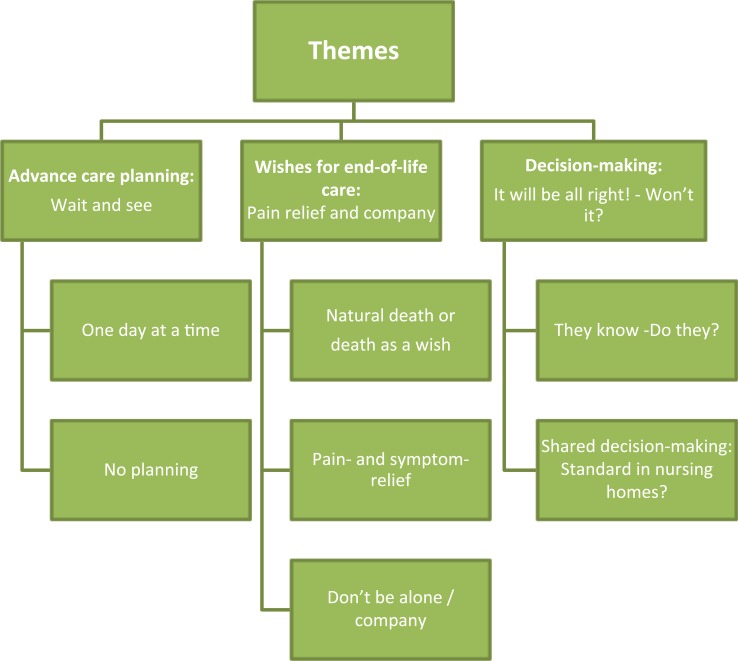
| 31. Clarity of major themes | The major themes are presented in the results/findings and illustrated in Figure 1. |
| 32. Clarity of minor themes | Minor themes are described in the result chapter. |
Setting, participants, and sample selection
In order to ensure that the greatest possible variation of data was obtained, a purposive sampling technique was utilized. This aimed to recruit participants from a wide geographical spread and location. The participants were the same as in a previous study.9 Tables 2 and 3 provide an overview of the participants.
Table 2.
Participants—nursing home residents.
| Nr. | Age (years) | Gender | Main medical diagnoses | Number of nursing home residents in the nursing home |
|---|---|---|---|---|
| 1 | 66 | Male | Multimorbidity | 50–100 |
| Chronic pain | ||||
| Heart disease | ||||
| Depression | ||||
| Stroke | ||||
| 2 | 70 | Male | Multimorbidity | 100–150 |
| Parkinson’s disease | ||||
| Angina pectoris | ||||
| Depression | ||||
| 3 | 74 | Female | Multimorbidity | 100–150 |
| Rheumatoid disease | ||||
| Diabetes | ||||
| Cold | ||||
| Basalioma | ||||
| Arteriosclerosis | ||||
| 4 | 75 | Male | Stroke (several times) | 100–150 |
| 5 | 77 | Female | Multimorbidity | 100–150 |
| Heart disease | ||||
| Atrial fibrillation | ||||
| Chronic pain | ||||
| Osteomyelitis | ||||
| 6 | 79 | Male | Multimorbidity | < 50 |
| Rheumatoid disease | ||||
| Prostate cancer | ||||
| Intestinal diverticulum | ||||
| Ileocolostomy | ||||
| 7 | 81 | Male | Osteoporosis | 100–150 |
| Rheumatoid arthritis | ||||
| 8 | 81 | Female | Multimorbidity | 100–150 |
| Diabetes type II | ||||
| Hypertension | ||||
| Depression | ||||
| Renal insufficiency | ||||
| 9 | 83 | Male | Multimorbidity | < 50 |
| Parkinson’s disease | ||||
| Hypertension | ||||
| Hyperlipoproteinemia | ||||
| Depression | ||||
| 10 | 87 | Female | Multimorbidity | < 50 |
| Stroke | ||||
| Cold | ||||
| Atrial fibrillation | ||||
| 11 | 88 | Female | Rheumatoid disease | 50–100 |
| 12 | 89 | Female | Multimorbidity | 100–150 |
| Hypertension | ||||
| Depression | ||||
| Biological aortic valve | ||||
| Bypass operation | ||||
| 13 | 89 | Female | Multimorbidity | 50–100 |
| Heart disease | ||||
| Atrial fibrillation | ||||
| Chronic muscle pain | ||||
| 14 | 89 | Female | No information provided | 150–200 |
| 15 | 91 | Female | Multimorbidity | 100–150 |
| Intestinal diverticulum | ||||
| Intestinal cancer | ||||
| Ileocolostomy | ||||
| Coxarthrosis | ||||
| Angina pectoris | ||||
| Intervertebral disc disease | ||||
| 16 | 92 | Female | Multimorbidity | 100–150 |
| Heart failure | ||||
| Hypertension | ||||
| Osteoporosis | ||||
| Pulmonary embolism | ||||
| Thrombosis | ||||
| 17 | 92 | Male | Multimorbidity | 100–150 |
| Prostate cancer | ||||
| Macular degeneration | ||||
| Intestinal cancer | ||||
| Paroxysmal tachycardia | ||||
| 18 | 93 | Male | Multimorbidity | 100–150 |
| Stroke | ||||
| Hypercholesterolemia | ||||
| Vertebral canal stenosis | ||||
| Cataract | ||||
| Deafness | ||||
| 19 | 94 | Female | Multimorbidity | 50–100 |
| Stroke | ||||
| Diabetes | ||||
| 20 | 94 | Female | Multimorbidity | 100–150 |
| Atrial fibrillation | ||||
| Stroke | ||||
| Heart disease | ||||
| Intestinal diverticulum | ||||
| Ileocolostomy | ||||
| 21 | 95 | Female | Basalioma | 100–150 |
| Arthrosis | ||||
| 22 | 96 | Female | Multimorbidity | 100–150 |
| Hypertension | ||||
| Depression | ||||
| Stroke | ||||
| 23 | 97 | Male | Multimorbidity | 50–100 |
| Depression | ||||
| Chronic muscle pain | ||||
| Deafness | ||||
| 24 | 99 | Female | Multimorbidity | 50–100 |
| Hypertension | ||||
| Stroke | ||||
| Angina pectoris | ||||
| Atrial fibrillation | ||||
| Esophageal reflux | ||||
| 25 | 100 | Female | Multimorbidity | 100–150 |
| Deafness | ||||
| Aortic stenosis | ||||
| Chronic pain | ||||
| Compression fracture of lumbar vertebrae | ||||
| Glaucoma | ||||
| Esophagitis | ||||
| Coxarthrosis |
In order to protect the residents’ privacy and to ensure that they can stay anonymous, the resident numbers in the table do not correspond with the numbers of the citations. One informant was excluded during the interview because of cognitive impairment.
Table 3.
Participants—relatives of nursing home residents.
| No. | Age (years) | Gender | Number of nursing home residents in the nursing home |
|---|---|---|---|
| 1 | 41 | Female | <50 |
| 2 | 45 | Male | 100–150 |
| 3 | 53 | Female | <50 |
| 4 | 58 | Female | <50 |
| 5 | 59 | Female | 100–150 |
| 6 | 60 | Female | 100–150 |
| 7 | 66 | Female | <50 |
| 8 | 67 | Female | 100–150 |
| 9 | 67 | Female | 100–150 |
| 10 | 71 | Female | 100–150 |
| 11 | 72 | Female | 100–150 |
| 12 | 73 | Female | 100–150 |
| 13 | 74 | Female | 100–150 |
| 14 | 77 | Male | 100–150 |
| 15 | 77 | Female | 100–150 |
| 16 | 80 | Male | 100–150 |
| 17 | 86 | Male | 100–150 |
| 18 | 91 | Male | 100–150 |
In order to protect the relatives’ privacy and to ensure that they can stay anonymous, the relative numbers in the table do not correspond with the numbers of the citations. All participating relatives had a relative (e.g. parent or spouse) living in long-term care in a nursing home.
Inclusion criteria for residents were as follows:
Capacity to provide informed consent;
Living in long-term care.
Residents with cognitive impairment were excluded. Inclusion criterion for relatives was to have a relative living in long-term care.
Nursing home staff (e.g. nurses or physicians) chose and recruited relatives and residents who were able to give written informed consent as study participants. The staff assessed cognitive function clinically without formal cognitive testing. G.B. (a specialized nursing home physician) made a secondary assessment of the resident’s capacity to give informed consent. One patient was excluded because of cognitive impairment.
The interview technique was open-ended with follow-up questions related to the participant’s answers and responses. Key themes in the interview guide were ACP, decision-making, and ethical challenges in end-of-life care in the nursing home. Data were collected from April 2010 to November 2011.
Transcription and analysis
Verbatim transcription of the digital interview recordings was supported by the transcription software f4 from audiotranskription and undertaken by G.B. and two trained assistants. Analysis and coding of the transcripts were conducted systematically, in different phases, aided by the software QSR NVivo 9. A detailed description of the analysis process is provided in Table 4. Analysis of the themes found in the data material and the coded text was repeatedly performed. As a measure to validate the findings, repeated reading of the interview transcripts, in order to question the findings in the interview transcripts, and repeated discussions with the co-authors were undertaken.
Table 4.
Details of the analysis process.
| 1. G.B., E.G., and J.H.R. read the transcripts and familiarized themselves with the data |
| 2. G.B. and E.G. independently identified preliminary codes and themes |
| 3. G.B., E.G., and J.H.R. compared and discussed the preliminary codes and themes |
| 4. G.B. coded all the material according to the preliminary codes and themes |
| 5. G.B. revised the preliminary codes and themes and compared them to his field notes |
| 6. G.B., E.G., and J.H.R. discussed the revised codes and themes and agreed on the final codes and themes |
| 7. G.B., E.G., and J.H.R. checked the transcripts in order to question the findings |
| 8. G.B., E.G., and J.H.R. discussed the findings and themes and agreed about the interpretation of the data |
Results
Participant characteristics
In all, 43 informants from nine Norwegian public and privately owned nursing homes representing different regions and communities of different sizes participated in the study. In total, 25 nursing home residents participated in in-depth interviews. A total of 18 relatives from three different institutions participated in focus groups. After completing three focus group interviews, data saturation was achieved. Source triangulation was used to compare views from residents and relatives. Mean age of the residents and relatives was 87 (66–100) and 68 (41–91) years, respectively. Participants’ characteristics are shown in Tables 2 and 3. The residents’ relation to the relatives was wife (2), husband (4), mother (9), mother-in-law (1), father (2) and no information (1). One relative had both parents in the nursing home. The residents’ and relatives’ views can be summarized in three main themes within a palliative care framework (Figure 1):
Figure 1.
Themes from the interviews of nursing home residents and relatives.
ACP: wait and see
One day at a time
A substantial number of the interviewed residents stated that they had no concern about their coming death, and one of the residents expressed what could be representative for most residents:
I take one day at a time. (Resident 7)
Many residents stated that they had not thought about planning their future at all:
It may sound easy to say but I haven’t thought so much about death. I mean, I live now. (Resident 13)
Some residents talked about their thoughts about accepting death as normal part of life:
There are two things you know for sure: it is to be born and to die. (Resident 18)
In addition, they also talked about their ambivalent attitude to death and the ambivalence of wanting to live and wanting to die at the same time:
My wish has been: Let me die. But this can change. One day you think that you want to die but on another day (you want to live) … When you are back in a somehow normal situation where you receive care and food and (pause) you are able to read a bit and such things, then you are there in that moment at least … But it is obvious, that there are times in-between where I think that I would like … that it ended (life) … I am almost wondering, how long shall I sit here? (Resident 15)
No planning for the future means no ACP
Most residents have not been engaged in ACP. When asked whether they have talked about ACP to relatives or the staff, most answered,
No, we have not talked about that. (Resident 25)
One reason for the lack of ACP may be the lack of time to talk:
No, there is little talk about that (ACP) because they (the staff) are so busy. (Resident 18)
It is not possible to talk with them (physicians and staff) about it. (Resident 3)
Or just in part,
I have talked a bit about it (ACP) with a nurse, and I appreciate to talk about death. I don’t have a problem to talk about it (death). Some people put these things aside and do not even want to think about it. (Resident 15)
A few informants talked about ACP, decision-making, and death with their relatives:
Why shouldn’t I talk about it (death and ACP)? …One is afraid … one is afraid of old prejudices, childhood believes … One is afraid to talk about such fundamental things. You don’t need to be afraid of talking about it. (Resident 24)
ACP does not seem to be important at all, although many do have concrete wishes for end-of-life care that they had not told anybody:
I haven’t thought so far … but it is pretty obvious … I would, in this case, like “a smooth passage”* between life and death. But I am not hysterical about it. (Resident 5)
*“a smooth passage” was explained to be dying without pain and suffering.
Although many residents mentioned the absence of regular physician visits, some had discussed their wishes for end-of-life care with both their family and a physician:
Yes, I have talked about it (death and ACP) with my family. And I have told them very early and told the doctor too … that I would say no if they tried to keep me alive! (Resident 24)
Functional status in daily life seems to be more important than choosing between different treatment options. Some residents expressed the view that they want to participate in life and that living without consciousness and the ability to communicate is not worth living:
I don’t want to become a vegetable. (Resident 17)
Many relatives are reluctant to talk about end-of-life care and treatment decisions with the residents. It seems that many fear this topic:
I do not dare. We are too afraid to take this up (ACP). (Relgr 1/2)
This (ACP and dying) is a subject that you do not talk about. (Relgr 3/4)
Therefore, many relatives do not know the residents’ wishes when decisions have to be made. One reason could be that the residents frequently use denial as a coping strategy:
I wish we had talked about it (ACP) before, but we have not. (Relgr 2/6)
In contrast, it can be experienced as a release if the relatives have talked about wishes and preferences in advance. This can positively lead to certainty about the resident’s wishes and preferences:
It was a difficult process. It really was. But I am very happy that we could talk about it (ACP), he (my husband) and me. (Relgr 2/1)
Wishes for end-of-life care: pain relief and company
Although many informants seemed to feel slightly uncomfortable talking about death and dying in the beginning, most of them were not frightened and talked openly about death as a normal part of life. Many residents had wishes for end-of-life care, but most had not communicated their wishes to the staff or their relatives.
Natural death or death as a wish
Many informants stated that, even when moving in, it was clear to them that they would die in the nursing home:
It is obvious for most people when they come in here, that this is their last stop. (Resident 15)
Some of them even expressed the wish to die:
I have said before that I would like to die. I have lived my life. I am done with life … I am not afraid to die. (Resident 20)
Some informants stated that they want to die as natural as possible:
Yes, I would appreciate a calm and natural death. (Resident 16)
Some stated that a natural death means that physicians should not prolong life without meaning:
I wish that I do not have to lie there suffering … If the physicians see that it (treatment) will not help any longer, they should not continue. (Resident 7)
In addition, many residents do not want artificial nutrition or life-prolonging medical treatment:
If it became the norm to withhold life with every technical means possible, it would just postpone that time (death) for many years. And then it is not sure that there will be quality of life … It won’t be there, I doubt it … It is just, I want to die with dignity. (Resident 24)
A feeling of control and the certainty of not being kept alive against ones wishes can enhance quality of life:
If you ask about quality of life, it may sound weird, but to know that you can end your life with dignity has something to do with quality of life. (Resident 24)
The use of life-prolonging treatment is in contrast to the wishes for a natural death of many informants. Resuscitation efforts or life-prolonging treatment, commonly, are not wanted:
I don’t want to receive life-prolonging means. I want to follow the course of nature… No life-prolonging treatment because what would it lead to? A life without living. You are more than just half-dead. Does that make sense? It does not work, it is unreasonable, its’ inhuman … to lie there … probably paralyzed and just able to stare at the ceiling … Does it make sense? No there is no sense with it… When life is fading away, you should not extend life with force. This is unnatural and uncomfortable if it will just make you live two days longer. (Resident 24)
Some of the informants seemed to be relaxed and stated that they were waiting to die:
I do know that I will die soon. That is the only thing I know … I do not know if it will be in 14 days or two years (laughs) … It cannot last much longer, I think. (Resident 14)
Some wished to die because life is troublesome, filled with waiting and suffering, and perhaps, boredom. Waiting was also part of the researcher’s own observations. The researcher observed that residents had to wait to get help from the staff on some occasions during the fieldwork:
Death can be a release, and for me it will be. (Resident 24)
None of the informants expressed the wish for euthanasia or physician-assisted suicide although several residents stated that they waited for death.
Some relatives do know that the residents’ wish would be to die and that life-prolonging treatment is definitely not intended:
I am sure that my mother often wishes to pass away. (Relgr 1/2)
Natural death can also mean to die in the nursing home instead of being sent to a hospital. In Norway, many relatives do have to decide whether the residents shall receive end-of-life care in the nursing home or whether they shall be transferred to a hospital:
This is a decision we as relatives have to make … Shall they be sent to hospital or not? … I am struggling with that decision. (Relgr 3/4)
Some relatives believe that holistic care is better in nursing homes compared to hospitals because death is more accepted. In hospitals, the intention is to save lives, and as a result, sometimes the needs of dying people are neglected:
I think it (dying) is calmer in the nursing home than in a hospital. (Relgr 3/3)
Pain- and symptom-relief
Many informants were afraid of pain and expressed their expectations to receive adequate pain relief when needed:
I have no other wishes than just to be able to die in a peaceful and quiet way without pain or other terrible things. (Resident 22)
Pain medication, as treatment in end-of-life care, is wanted by most informants and does not seem to interfere with the residents’ concept of a natural death:
There is something I am afraid of, which I don’t like to think about. That is to experience pain. I don’t want to be in pain. I don’t like it … And therefore they have told me that they will start to give me morphine injections. So that I won’t feel pain. (Resident 20)
Relatives agree with the residents that relief from pain and suffering is most important in end-of-life care:
If they only are not in pain … Yes, no pain … This is most important. (Relgr 2/5, 6)
She (the resident) has made it clear that she does not want life-prolonging treatment but that we shall take care that she won’t die in pain. (Relgr 2/5)
Don’t be alone/company
Not to be alone when facing death is a frequently mentioned wish by many residents:
You need a hand to hold on to. (Resident 12)
Many would appreciate their relatives to be there:
Of course I want them (the relatives) to be there when I die. Because this is something unknown … It is not easy for us to be alone then. (Resident 25)
In addition, residents want to be able to contact relatives:
I would like to be able to talk to my relatives as long as possible. (Resident 5)
Decision-making: it will be all right!—won’t it?
Most residents trust their relatives when coming to a decision concerning treatment options, whereas the relatives feel insecure about the resident’s wishes.
They know—do they?
Asked whether the relatives knew the residents’ preferences about their wishes for end-of-life care and decision-making, most residents stated that their relatives did know their wishes:
Yes, they know how I feel. I don’t think that this will be a problem. (Resident 8)
Many relatives are afraid of making important decisions for the residents and are concerned that they do not know what to choose if being asked to decide:
I have never talked about that with my husband because he had not accepted that he was ill. So we have not talked about his wishes. And now he is not able to talk anymore … I have not been asked (to decide something for him yet), but I do see … No, this is so complicated … Sometimes I think that this is undignified as he sits there not being able to do anything. I have not accepted the situation myself (sniffles). We (relatives) become so egoistic. We want to retain them. But how can I say what is the best for him? (Relgr 1/5)
Many relatives experience it as a burden to make decisions without knowing the wishes and opinions of the residents:
I do hope that I will not have to make a decision … I do not want to decide. I cannot decide. (Relgr 1/6)
Shared decision-making: standard in nursing homes?
All residents were asked who should decide if they were incapable to decide themselves. Most of them stated that their relatives should decide:
My relatives shall decide for me. (Resident 12)
Some believed that shared decision-making is standard and that this means that relatives and physicians talk together in order to make decisions:
I suppose that the doctor and my children talk together (in order to make decisions). (Resident 14)
Many residents trust in the physicians’ ability to make decisions about their medical treatment and feel comfortable when just being informed:
You know. They (the physicians) decide. I cannot decide anything myself. But they do provide me with information first. (Resident 19)
Many residents think that the withdrawing of life-prolonging treatment is exclusively a medical decision that should be made by the doctor:
That I do not have to suffer … When the doctors see that it (life-prolonging treatment) does not help anymore, they should not carry on doing it. (Resident 7)
Treatment decisions were often seen as “purely medical decisions” by residents, and although many want their relatives to participate in the decision-making, they want the doctor to decide on issues that the residents regard to be solely medical matters:
The family cannot decide everything, can they? If it is something that has to do with disease, it shall be decided by the physician. (Resident 8)
Most of the residents trust in the ability of physicians and staff to make decisions for them, but some primarily trust the nurses who know them best:
I do not think that I can decide such things. I think this has to be done by the staff … I have no contact with the doctors who work here … They are so seldom around that I hardly know them. (Resident 3)
As many residents do not have regular contact with their physician, they prefer shared decision-making by nurses and physicians:
I just trust in the ones who care for me. What they think is best. (Resident 25)
Many of the relatives seemed to be used to take over decision-making and organization of most things for the residents:
It is almost as if they hand it (decision-making) over to us. We have already taken over most things … Probably they change when they get old. Maybe they cannot bear to make decisions anymore … Uff? … They just want others to do it. They are tired of it … Maybe she (the nursing home resident) thinks that I know best (laughing). (Relgr 3/2)
Although many relatives do not want to decide alone, they want to participate in decision-making and to be heard. They prefer shared decision-making undertaken together with nurses and doctors:
But I think that it is important that one of course will be heard and that one can participate in decision-making when the situation turns up … this should be done in cooperation with the nurses and the doctor. (Relgr 1/6)
ACP has been described as an ongoing process with repeated meetings and communication. Some would appreciate regular meetings with the nursing home staff:
There should be regular meetings between the relatives and the staff at least once a month. (Relgr 1/7)
Discussion
The main findings of the study are that residents trust their relatives, physicians, and nurses to make decisions for them and that most residents believe that the relatives would know their wishes. In contrast, however, many relatives do not know what the resident wants. ACP is lacking in nursing homes.
Relatively, few people have written ACP documents: 8% in England and 10%−20% in the United States, Canada, Australia, Germany, and Japan.20 There are guidelines on ACP and decision-making in end-of-life care in the United Kingdom13,20,21 and Norway.22 Nevertheless, in Norway, limitation of life-prolonging treatment on the family’s request might be more frequent than the law permits.23 Few older adults have expressed their wishes for end-of-life care and many do not talk openly about death.24 Even if preferences had been discussed, documentation and a systematic approach are lacking.25,26 Our data show that there is a striking difference between the views of the residents and the relatives concerning the knowledge of the residents wishes for end-of-life care. The absence of ACP seems not to be problematic for the residents but may lead to psychological stress for the relatives. When decisions in end-of-life care have to be made without knowing what the resident would want, problematic situations occur.27–29 This may cause moral distress for the relatives,28 nurses, and physicians. Challenges in decision-making, communication, or even conflicts between staff and relatives are described in the literature.8,14,27,30–32 Many relatives in our study felt that it was problematic to decide for the residents and that they tried to avoid making important health-related and end-of-life care decisions.
A systematic approach to ACP with repeated conversations is needed as many residents and relatives seem to need a third person with knowledge of the residents medical history to initiate a discussion on ACP.33,34 Both systems to involve residents and relatives in end-of-life care in nursing homes14,27,35 and training of the staff to enable them to discuss ACP are needed.36–38 Our findings suggest that residents do not oppose ACP, but that the opportunity is lacking. This is in accordance with findings from other researchers.39,40 As many residents in nursing homes have cognitive impairment, ACP discussions should be offered much earlier in their disease trajectory.41,42
The resident’s wishes for end-of-life care in our data were as follows: not to be alone, pain relief, and no life-prolonging treatment. These findings are in accordance with previous findings.43
Although some residents talked about death as a wish or relief, none of them mentioned a wish for euthanasia or physician-assisted suicide. One possible reason for a wish to die could be the lack of subjectively felt quality of life perhaps due to lack of activities and contact. Dignity is threatened by illness and the perception of insufficient care.44 Residents’ dignity can be supported and enhanced in many ways including dignity therapy and even by participating in research.45,46 Interestingly, most informants in our study were grateful to take part in our research and to be able to contribute.
In summary, providing residents with opportunities for ACP and talking about death and preferences for end-of-life care are paramount. Besides planning for end of life, ACP helps the residents to prepare for death47 and can reduce moral distress for the relatives. ACP has a positive impact on quality of end-of-life care.48,49
Strengths and weaknesses of the study
G.B.’s experience as a nursing home physician and consultant in palliative medicine and thus talking regularly about death may be considered both as a strength and as a weakness of this study. It is a strength that the interviewer was comfortable talking openly about death and dying in an empathic manner. Nevertheless, it might be a risk for “going blind” to unknown aspects of the nursing home world. The researcher used metapositions and repeated reflection of his presuppositions during the interviews and analysis. The fact that many participants thanked the interviewer for talking about these matters indicates that there was an open atmosphere that enabled the informants to share their views and concerns. One possible weakness could be the selection of informants by nursing home staff to provide a positive picture of their nursing home. Most informants reported, however, both positive and negative aspects. Nevertheless, it should be noted that they represent only a small part of the nursing home residents. A limitation is the exclusion of residents with cognitive impairment due to ethical considerations.
Implications for clinical practice and future research
ACP should be initiated by healthcare workers (nursing home staff and/or medical doctors) and should be an integral part of nursing home care. It seems that most people do need a third person from outside the family to start conversations about ACP. Future research should focus on methods and communication arenas that can enable residents, relatives, and staff to talk openly about end-of-life care and to solve emerging ethical dilemmas.
Conclusion
Communication about the end of life with the residents and relatives including ACP should be routine in all long-term care facilities. In nursing homes, there is a need to talk about ACP and preferences for end-of-life care in order to enable decision-making.
Acknowledgments
We are grateful for all help and support by residents, relatives, and staff from the participating nursing homes and all the other people who supported the research study by different means.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This research project has been financially supported by the Norwegian Extra Foundation for Health and Rehabilitation through EXTRA funds (grant no. 2008/2/0208).
References
- 1. Robinson KM, Reinhard SC. Looking ahead in long-term care: the next 50 years. Nurs Clin North Am 2009; 44(2): 253–262. [DOI] [PubMed] [Google Scholar]
- 2. Alzheimer’s Foundation. Dementia UK: update 2014, https://www.alzheimers.org.uk/site/scripts/download_info.php?fileID=2323 (2014, accessed 4 April 2015).
- 3. Selbæk G, Kirkevold Ø, Engedal K. The prevalence of psychiatric symptoms and behavioural disturbances and the use of psychotropic drugs in Norwegian nursing homes. Int J Geriatr Psychiatry 2007; 22: 843–849. [DOI] [PubMed] [Google Scholar]
- 4. National Audit Office. End of life care, https://www.nao.org.uk/wp-content/uploads/2008/11/07081043.pdf (2008, accessed 4 April 2015).
- 5. Sleeman KE, Ho YK, Verne J, et al. Reversal of English trend towards hospital death in dementia: a population-based study of place of death and associated individual and regional factors, 2001–2010. BMC Neurol 2014; 14: 59 DOI: 10.1186/1471-2377-14-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Statistisk sentralbyrå [Statistics Norway]. Dødsfall etter dødssted 2012 [Deaths and place of death 2012], https://www.ssb.no/statistikkbanken/selectout/ShowTable.asp?FileformatId=2&Queryfile=20151512594894079903Dodssted&PLanguage=0&MainTable=Dodssted&potsize=6 (2012, accessed 27 January 2015).
- 7. Weston CM, O’Brien LA, Goldfarb NI, et al. The NJ SEED project: evaluation of an innovative initiative for ethics training in nursing homes. J Am Med Dir Assoc 2005; 6: 68–75. [DOI] [PubMed] [Google Scholar]
- 8. Gjerberg E, Førde R, Pedersen R, et al. Ethical challenges in the provision of end of life care in Norwegian nursing homes. Soc Sci Med 2010; 71(4): 677–684. [DOI] [PubMed] [Google Scholar]
- 9. Bollig G, Gjengedal E, Rosland JH. Nothing to complain about? Residents’ and relatives’ views on a “good life” and ethical challenges in nursing homes. Nurs Ethics. Epub ahead of print 8 December 2014. DOI: 10.1177/0969733014557719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thomas K, Lobo B. (eds). Advance care planning in end of life care. New York: Oxford University Press, 2011. [Google Scholar]
- 11. Brinkman-Stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med 2014; 28(8): 1000–1025. [DOI] [PubMed] [Google Scholar]
- 12. Mullick A, Martin J, Sallnow L. An introduction to advance care planning in practice. BMJ 2013; 347: f6064 DOI: 10.1136/bmj.f6064. [DOI] [PubMed] [Google Scholar]
- 13. NHS England. Your life—your choice, https://www.nescn.nhs.uk/wp-content/uploads/2014/05/Deciding-Right-Strategy-doc-0414.pdf (2014, accessed 5 May 2015).
- 14. Dreyer A, Førde R, Nortvedt P. Life-prolonging treatment in nursing homes: how do physicians and nurses describe and justify their own practice? J Med Ethics 2010; 36: 396–400. [DOI] [PubMed] [Google Scholar]
- 15. Friis P, Førde R. Forhåndssamtaler med geriatriske pasienter [Advance care planning discussions with geriatric patients]. Tidsskr Nor Laegeforen 2015; 135(3): 233–235. [DOI] [PubMed] [Google Scholar]
- 16. Holman D, Hockley J. Advance care planning—the “what,” the “why,” the “how and when”: a UK perspective. Singapore Nurs J 2010; 37: 10–15. [Google Scholar]
- 17. Thorne S. Interpretive description. 1st ed Walnut Creek, CA: Left Coast Press, 2008, pp. 11–262. [Google Scholar]
- 18. Kvale S. Interviews—an introduction to qualitative research interviewing. 1st ed Thousand Oaks, CA: SAGE, 1996, pp. 124–209. [Google Scholar]
- 19. Malterud K. Kvalitative metoder i medisinsk forskning [Qualitative methods in medical research]. 3rd ed. Oslo: Universitetsforlaget, 2011, pp. 15–136. [Google Scholar]
- 20. Royal College of Physicians. Advance care planning—national guidelines, https://www.rcplondon.ac.uk/resources/concise-guidelines-advance-care-planning (2009, accessed 6 May 2015).
- 21. Hutchinson C, Foster J. Best interests at the end of life. East Lancashire NHS, https://www.scie.org.uk/publications/mca/files/lancspct.pdf?res=true (2009, accessed 6 May 2015). [Google Scholar]
- 22. Helsedirektoratet [Norwegian Directorate of Health]. Beslutningsprosesser ved begrensning av livsforlengende behandling [Decision-making process in limiting life-prolonging treatment], https://helsedirektoratet.no/Lists/Publikasjoner/Attachments/67/IS-2091-Beslutningsprosesser-ved-begrensning-av-livsforlengende-behandling.pdf (2009, accessed 6 May 2015).
- 23. Førde R, Aasland OG. Are end-of-life practices in Norway in line with ethics and law? Acta Anaesthesiol Scand 2014; 58: 1146–1150. [DOI] [PubMed] [Google Scholar]
- 24. Lloyd-Williams M, Kennedy V, Sixsmith A, et al. The end of life: a qualitative study of the perceptions of people over the age of 80 on issues surrounding death and dying. J Pain Symptom Manage 2007; 34: 60–66. [DOI] [PubMed] [Google Scholar]
- 25. Cox K, Moghaddam N, Almack K, et al. Is it recorded in the notes? Documentation of end-of-life care and preferred place to die discussions in the final weeks of life. BMC Palliat Care 2011; 10: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Robinson L, Dickinson C, Bamford C, et al. A qualitative study: professionals experiences of advance care planning in dementia and palliative care, “a good idea in theory but …” Palliat Med 2012; 27(5): 401–408. [DOI] [PubMed] [Google Scholar]
- 27. Dreyer A, Førde R, Nortvedt P. Autonomy at the end of life: life-prolonging treatment in nursing homes-relatives role in the decision-making process. J Med Ethics 2009; 35: 672–677. [DOI] [PubMed] [Google Scholar]
- 28. Givens JL, Lopez RP, Mazor KM, et al. Sources of stress for family members of nursing home residents with advanced dementia. Alzheimer Dis Assoc Disord 2012; 26(3): 254–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hansen L, Archbold PG, Stewart B, et al. Family caregivers making life-sustaining treatment decisions: factors associated with role strain and ease. J Gerontol Nurs 2005; 31(11): 28–35. [DOI] [PubMed] [Google Scholar]
- 30. Kayser-Jones J. The experience of dying: an ethnographic nursing home study. Gerontologist 2002; 42: 11–19. [DOI] [PubMed] [Google Scholar]
- 31. Gorlen TF, Gorlen T, Neergaard MA. Death in nursing homes: a Danish qualitative study. Int J Palliat Nurs 2013; 19(5): 236–242. [DOI] [PubMed] [Google Scholar]
- 32. Schaffer MA. Ethical problems in end-of-life decisions for elderly Norwegians. Nurs Ethics 2007; 14: 242–257. [DOI] [PubMed] [Google Scholar]
- 33. Chan HYL, Pang SMC. Let me talk—an advance care planning programme for frail nursing home residents. J Clin Nurs 2010; 19: 3073–3084. [DOI] [PubMed] [Google Scholar]
- 34. Mathie E, Goodman C, Crang C, et al. An uncertain future: the unchanging views of care home residents about living and dying. Palliat Med 2011; 26(5): 734–743. [DOI] [PubMed] [Google Scholar]
- 35. Gjerberg E, Førde R, Bjørndal A. Staff and family relationships in end-of-life nursing home care. Nurs Ethics 2011; 18(1): 42–53. [DOI] [PubMed] [Google Scholar]
- 36. Silvester W, Fullam RS, Parslow RA, et al. Quality of advance care planning policy and practice in residential aged care facilities in Australia. BMJ Support Palliat Care 2013; 3: 349–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Stone L, Kinley J, Hockley J. Advance care planning in care homes: the experience of staff, residents, and family members. Int J Palliat Nurs 2013; 19: 550–557. [DOI] [PubMed] [Google Scholar]
- 38. Fosse A, Schaufel MA, Ruths S, et al. End-of-life expectations and experiences among nursing home patients and their relatives—a synthesis of qualitative studies. Patient Educ Couns 2014; 97(1): 3–9. [DOI] [PubMed] [Google Scholar]
- 39. Lovell A, Yates P. Advance care planning in palliative care: a systematic literature review of the contextual factors influencing its uptake 2008–2012. Palliat Med 2014; 28(8): 1026–1035. [DOI] [PubMed] [Google Scholar]
- 40. Sharp T, Moran E, Kuhn I, et al. Do the elderly have a voice? Advance care planning discussions with frail and older individuals: a systematic literature review and narrative synthesis. Br J Gen Pract 2013; 63(615): e657–e668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dening KH, Jones L, Sampson EL. Preferences for end-of-life care: a nominal group study of people with dementia and their family carers. Palliat Med 2012; 27(5): 409–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Robinson L, Dickinson C, Rousseau N, et al. A systematic review of the effectiveness of advance care planning interventions for people with cognitive impairment and dementia. Age Ageing 2012; 41: 263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients’ perspectives. JAMA 1999; 281(2): 163–168. [DOI] [PubMed] [Google Scholar]
- 44. Pleschberger S. Dignity and the challenge of dying in nursing homes: the residents view. Age Ageing 2007; 36: 197–202. [DOI] [PubMed] [Google Scholar]
- 45. Chochinov HM. Dignity-conserving care—a new model for palliative care. JAMA 2002; 287(17): 2253–2260. [DOI] [PubMed] [Google Scholar]
- 46. Hall S, Goddard C, Speck P, et al. It makes me feel that I’m still relevant: a qualitative study of the views of nursing home residents on dignity therapy and taking part in a phase II randomized controlled trial of a palliative care psychotherapy. Palliat Med 2012; 27(4): 358–366. [DOI] [PubMed] [Google Scholar]
- 47. Martin DK, Emanuel LL, Singer PA. Planning for the end of life. Lancet 2000; 356: 1672–1676. [DOI] [PubMed] [Google Scholar]
- 48. Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010; 340: c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Teno JM, Gruneir A, Schwartz Z, et al. Association between advance directives and quality of end-of-life care: a national study. J Am Geriatr Soc 2007; 55: 189–194. [DOI] [PubMed] [Google Scholar]