Abstract
Relationships between physicians and hospitals have changed considerably over the past decade as hospitals and physician groups integrate and new public and private payment policies create financial interdependence. The extent to which accountable care organizations (ACOs) involve hospitals in their operations may prove to be vitally important because managing hospital care is a key part of improving quality and lowering cost growth. Using primary data on ACO composition and capabilities paired with hospital characteristics, we found that 20 percent of US hospitals were part of an ACO in 2015, and hospitals that were in urban areas, non-profit, or had a smaller share of Medicare patients were more likely to participate in ACOs compared to other ACOs. Qualitative data identified several advantages of including a hospital in an ACO: the availability of start-up capital, advanced data sharing, and engagement of providers across the care continuum. Although ACOs that include hospitals (63 percent of ACOs) offered more comprehensive services compared to ACOs without hospitals, we found no differences among ACOs in their ability to manage hospital-related aspects of patient care.
Keywords: Health Reform, Hospitals, Medicare, Organization and Delivery of Care, Physicians
Hospitals rely on physicians for patient referrals and physicians depend on hospitals to provide high-quality care for their patients when they are most vulnerable. However, the mechanisms underlying this relationship have changed considerably over time. Historically, physicians owned private practices and admitted their patients to a local non-profit hospital where they rounded on their patients themselves. During the era of managed care (1980s and 1990s), physicians and hospitals joined forces to better manage emerging capitation systems, in which per-patient payments were fixed regardless of the care that was delivered.(1) This trend toward consolidation continued into the 2000s(2), leading researchers, regulators, and policymakers to ponder the trade-offs between consolidation and coordination.(3)
Accountable care organizations (ACOs) are groups of providers that are collectively held responsible for the care of a defined population of patients. Providers participating in ACOs are financially responsible for quality measures and the total cost of care for their patient population, including inpatient acute care. Medicare, Medicaid, and commercial payers are rapidly adopting ACO contracts.(4, 5) Inpatient spending is an essential focus for cost growth reduction throughout Medicare, and for Medicare ACOs in particular (the Pioneer ACO program, the Medicare Shared Savings Program, and Next Generation ACO Model). This is because inpatient hospital spending accounted for 32% of fee-for-service Medicare spending in 2013.(6) Several of the quality measures used in Medicare’s ACO programs are influenced by hospital care, such as patients’ rating of provider communication, all-condition readmission rates, admissions for ambulatory care-sensitive conditions, and medication reconciliation.(7) Additional Medicare ACO quality measures in 2015 included all-cause unplanned admissions for patients with diabetes, heart failure, or multiple chronic conditions. These new measures may be influenced by hospital actions such as alerting physicians about emergency department (ED) admissions or repeat hospitalizations.(8) Generally speaking, ACOs with and without participating hospitals are held accountable for some degree of hospital performance on cost and quality.
The flexibility inherent in ACO programs has allowed for experimentation in the types of organizations forming ACOs and has resulted in diversity of ACO structures.(9, 10) For example, the Medicare ACO programs do not specify the types of providers that must be included in an ACO. A Medicare ACO must only have enough practitioners to allow at least 5,000 beneficiaries to be attributed to the ACO through evaluation and care management. Despite the importance of hospitals to cost and quality, previous research found that about half of the ACOs in the Medicare Shared Savings Program and Pioneer model did not include a hospital.(11) Just over half of all ACOs are physician-led, with another third jointly led by physicians and hospitals.(12) Research on types of ACOs shows a number of different ways that hospitals and provider groups might partner in an ACO: ACOs can be fully or jointly initiated and led by the hospital; the hospital can act as a participant in the accountable care contract without a leadership role; or a physician group can contract with a hospital for inpatient services but not include the hospital in the definition of the ACO.(13)
There are advantages and disadvantages surrounding hospital participation in an ACO. In the dual goals of quality improvement and cost reduction, improved clinical coordination is essential. Management of hospital care is a crucial component of clinical coordination, and one that ACOs are able to impact.(14, 15) Hospital participation in an ACO may improve quality and lower costs by allowing more efficient hospitalizations, better coordination of transitions, both to post-acute care settings and between inpatient and outpatient settings, and improved communication between settings and providers. Hospitals are also key to the referral process, and can help ACOs create savings by referring to lower-cost providers (for imaging, for example) or by limiting the amount of hospital-based ambulatory care they provide. However, hospital participation may make ACOs less nimble if ACOs with a participating hospital must forego revenue from hospital admissions. Finally, large hospital systems may be more centralized, which may negatively impact innovation adoption.(16) From a hospital perspective, the incentives to participate in an ACO are likely to improve coordination of care and to maintain a referral base of primary care physicians.
Analyses of ACO performance are beginning to show that the model is generating improved quality and lower costs,(17, 18) yet the participation of hospitals in ACOs is largely unstudied. Analysis of savings from the first two performance years of the Pioneer model (2012 and 2013) found that inclusion of a hospital had no effect on whether the ACO had savings or losses(19), but ACOs with hospitals performed better on ACO quality measures than ACOs that did not.(20) While theories about the importance of a hospital to the ACO model have been considered (21), this analysis is the first to assess the actual participation of hospitals in ACOs using a mixed-methods approach. In this paper, we analyze the types of hospitals participating in ACOs to determine whether they differ from those not participating, and analyze advantages and disadvantages to hospital inclusion from an ACO perspective.
Study Data And Methods
We collected primary data on hospital participation in ACOs from the National Survey of Accountable Care Organizations and the Leavitt Partners ACO Database. We assessed differences between ACOs with and without participating hospitals and analyzed qualitative interview data on ACO structure, motivations, and clinical priorities to understand advantages and disadvantages of hospital participation in ACOs.
Quantitative Data Sources and Study Sample
In order to analyze the characteristics of hospitals participating in ACOs (versus non participants), we linked the 2012 American Hospital Association Survey and the Leavitt Partners ACO database. We define hospital participation in an ACO as ownership or non-ownership affiliation between the hospital and the ACO. We created a compendium of hospital and area-level attributes from Medicare claims, cost reports, the American Community Survey, the Medicare Provider of Services file, and other publicly available files. In order to determine whether there are differences in characteristics or capabilities of ACOs with and without hospital participation, we collected data on ACO capabilities between October 2012 and March 2014 through the National Survey of Accountable Care Organizations, Waves 1 and 2 (N=269, response rate=66%).(12) A description of the data sets and sources for each of the hospital-level characteristics can be found in online Appendix 1(22)
Quantitative Analyses
First, to assess which types of hospitals are participating in ACOs, we compared characteristics of hospitals that are participating in Medicare and private accountable care contracts to those not participating (Exhibit 1). We used a logistic regression model to examine hospital characteristics associated with participation in an ACO contract and report predicted values to illustrate the relative importance of hospital characteristics in ACO participation, controlling for structural hospital characteristics and characteristics of patients (Exhibit 2). Changing the unit of analysis from hospitals to ACOs, we compared the characteristics and capabilities of ACOs with and without participating hospitals, using information reported by the ACO in the National Survey of Accountable Care Organizations (Exhibit 3). We also report the proportion of ACOs that report their current capability in the top third and bivariate comparison of means tests between the two groups (Exhibit 4).
Exhibit 1. Descriptive Hospital Characteristics by Accountable Care Organization Participation.
The Leavitt Partners ACO Database, Medicare Cost Report data, American Hospital Association Annual Survey Database (2012), The Medicare Provider and Analysis Review (MedPAR) File (2011 and 2012), 2010 American Community Survey, Provider of Services (POS) Extract (2012), The Centers for Medicare and Medicaid Innovation’s 2014 Bundled Payments for Care Improvement Extract, and The Centers for Medicare and Medicaid Services (CMS) Hospital Compare.
| Hospital not part of ACO | Hospital part of ACO | ACO Type | |||
|---|---|---|---|---|---|
| Medicare ACO | Commercial ACO | Medicare & Commercial ACO | |||
| Number of hospitals | 4,068 (79.6%) | 1,042 (20.4%) | 313 (6.1%) | 505 (9.9%) | 224 (4.4%) |
| Ownershipa – Government | 27.1% | 8.2% | 5.8% | 9.3% | 8.9% |
| Ownership – Private Non-Profit | 43.3% | 80.6% | 75.1% | 81.6% | 86.2% |
| Hospital size | |||||
| Small (<16 beds) | 33.4% | 13.5% | 15.7% | 10.3% | 17.9% |
| Medium (16–175 beds) | 47.3% | 41.5% | 41.9% | 41.0% | 42.0% |
| Large (>175 beds) | 19.0% | 44.9% | 42.5% | 48.7% | 39.7% |
| Staffed beds | 105 | 197 | 185 | 209 | 189 |
| Average daily census | 76 | 147 | 138 | 157 | 139 |
| Number of hospital services | 2.9 | 4.1 | 3.9 | 4.1 | 4.3 |
| Hospital typeb- Critical Access | 28.3% | 12.1% | 13.7% | 9.1% | 16.5% |
| Hospital type- Specialty | 19.5% | 2.9% | 2.9% | 3.2% | 2.2% |
| Teaching hospital | 2.7% | 8.5% | 8.0% | 9.3% | 7.6% |
| Percentage of patients, Black | 9.2% | 10.0% | 10.8% | 10.4% | 8.1% |
| Percentage of patients, Hispanic | 1.8% | 2.3% | 2.1% | 2.6% | 2.0% |
| Under poverty line in hospital zip code | 15.7% | 13.1% | 13.2% | 13.2% | 12.8% |
| Case mix index | 1.25 | 1.47 | 1.45 | 1.51 | 1.42 |
| Length of stay | 4.13 | 4.46 | 4.47 | 4.53 | 4.26 |
| Overall rate of serious complications/safety (per 1000 patients) | 0.59 | 0.60 | 0.60 | 0.61 | 0.59 |
| Rate of 30-day readmissions | 16.01% | 15.95% | 16.04% | 15.87% | 15.99% |
| Core Based Statistical Area, Division | 11.5% | 28.0% | 28.1% | 29.3% | 25.0% |
| Core Based Statistical Area, Metro | 44.0% | 51.2% | 50.5% | 51.1% | 52.7% |
| Core Based Statistical Area, Micro | 18.6% | 10.8% | 12.1% | 10.7% | 9.4% |
| Core Based Statistical Area, Rural | 26.0% | 9.9% | 9.3% | 8.9% | 12.9% |
| Patient discount | 54.7% | 62.8% | 63.7% | 63.3% | 60.7% |
| Proportion of patients with Medicare | 48.6% | 39.4% | 42.2% | 36.8% | 41.3% |
| Proportion of patients with Medicaid | 10.6% | 10.6% | 11.0% | 9.6% | 12.3% |
| Proportion of patients with Private/Self-Pay | 40.8% | 50.0% | 46.8% | 53.6% | 46.4% |
| Participates in Bundled Payment Initiative | 17.8% | 31.9% | 34.5% | 33.9% | 23.7% |
| HRR-level hospital HHI index | 1,643 | 1,420 | 1,504 | 1,381 | 1,394 |
Notes
Hospitals that are neither government nor private, non-profit are private, for-profit (not shown).
Hospitals that are neither critical access nor specialty are acute care hospitals (not shown). Bed size categories were determined by calculating the 25th and 75th percentile of the mean. Hospital services include for example: obstetrics services, medical/surgical intensive care, cardiac intensive care. A Core Based Statistical Area division has a population of at least 2.5 million; metro has a population of at least 50,000; micro a population of 10,000 – 49,999; and rural a population less than 10,000. HRR is Hospital Referral Region. HHI is Herfindahl-Hirschman Index Rate of 30-day Readmissions is a composite measure of unplanned readmission rates for heart attack, heart failure, pneumonia, and hip/knee surgery. Except for proportion Medicaid, readmission rate, serious complication rates, and percentage of patients Black and Hispanic, all differences between hospitals participating or not participating in an ACO are significant at p<0.001 as measured by a bivariate t-test for difference in means, or chi-squared test for proportions. Proportion Hispanic and serious complication rates are significant at the p<0.05 level.
Exhibit 2. Predicted Probability of a Hospital Joining an Accountable Care Organization, by Key Characteristics.
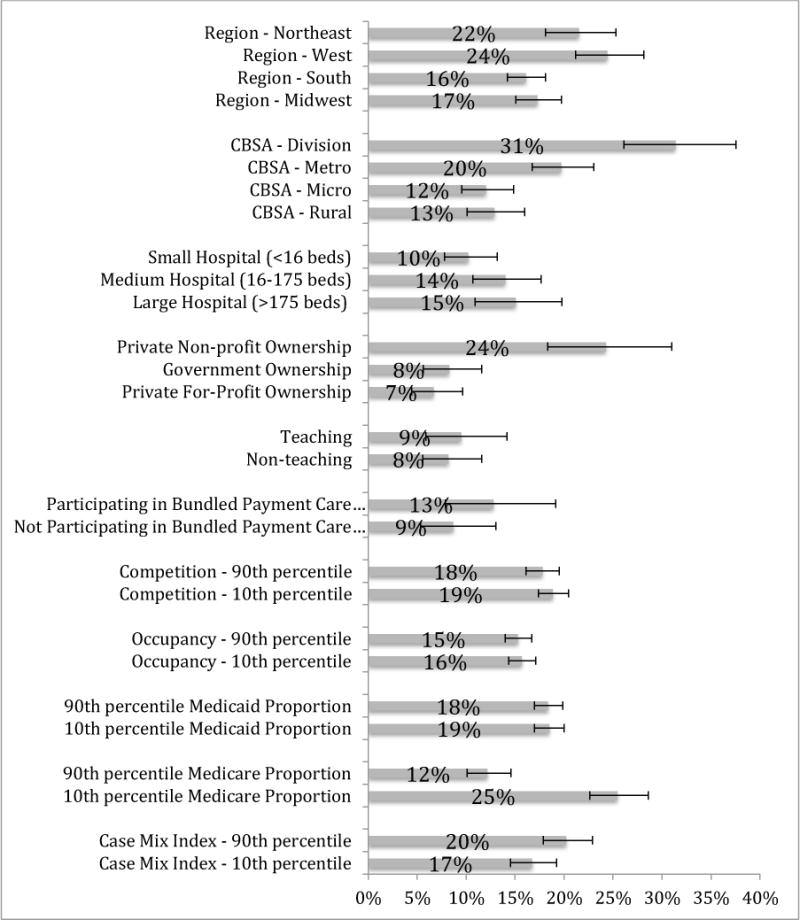
The Leavitt Partners ACO Database, Medicare Cost Report data, American Hospital Association Annual Survey Database (2012), The Medicare Provider and Analysis Review (MedPAR) File (2011 and 2012), 2010 American Community Survey, Provider of Services (POS) Extract (2012), and The Centers for Medicare and Medicaid Innovation’s 2014 Bundled Payments for Care Improvement Extract.
Notes: Predicted probabilities calculated from a multivariate regression where the dependent variable is participation in an ACO contract by the hospital and independent variables are as shown (N=5,110). Covariates in the model were held at their means. The 10th and 90th percentiles were determined across the distribution of hospitals. Error bars represent 95% confidence intervals around the estimates.
Exhibit 3. Accountable Care Organization Characteristics with and without a Participating Hospital.
National Survey of Accountable Care Organizations, Waves 1 and 2.
| Of ACOs with a Hospital N=155 (63%) | Of ACOs without a Hospital N=91 (37%) | |
|---|---|---|
| Medicare ACO contract (Pioneer or MSSP) | 54.84% | 86.81% |
| Private ACO contract | 65.77% | 38.37% |
| Medicaid ACO contract | 38.06% | 15.38% |
| Multipayer | 52.26% | 35.16% |
| Upside risk in year 1 of any ACO contract | 62.07% | 84.27% |
| Upside and downside risk in year 1 of any ACO contract | 37.93% | 15.73% |
| Competition for patients in market | 74.65% | 47.62% |
| FTE primary care clinicians in ACO (mean) | 203 | 100 |
| FTE specialty clinicians in ACO (mean) | 308 | 97 |
| Offer any post-acute care services within ACO | 67.10% | 9.89% |
| Offer behavioral health services within ACO | 52.32% | 20.93% |
| Offer emergency care within the ACO | 79.74% | 9.20% |
| Offer routine specialty care with the ACO | 69.74% | 44.32% |
| Offer palliative/hospice care within the ACO | 59.06% | 10.47% |
| Offer outpatient pharmacy services within the ACO | 36.30% | 10.23% |
Notes: MSSP is Medicare Shared Savings Program. ACO contracts hold the organization financially accountable for quality and total cost of care, and can include only upside risk (bonuses for good performance) or both downside and upside risk (bonuses for good performance, penalties for poor performance). Competition for patients in market is self-reported intensity of competition (competitive or very competitive). Offering of health care services, including post-acute care, behavioral health care, emergency care, specialty care, palliative/hospice care and outpatient pharmacy services, indicates that the ACO includes providers that offer these services. All differences between hospitals participating or not participating in an ACO are significant at p<0.001 except for multipayer and competition for patients in a market, which are p<0.05. Twenty-three organizations did not complete the question on hospital inclusion, and were thus excluded from the analysis, resulting in 246 ACOs available for analyses based on NSACO data.
Exhibit 4. Accountable Care Organization Programs in Place to Improving Hospital Use, by Hospital Inclusion in ACO, National Survey of Accountable Care Organizations, Waves 1 and 2 (N=269).
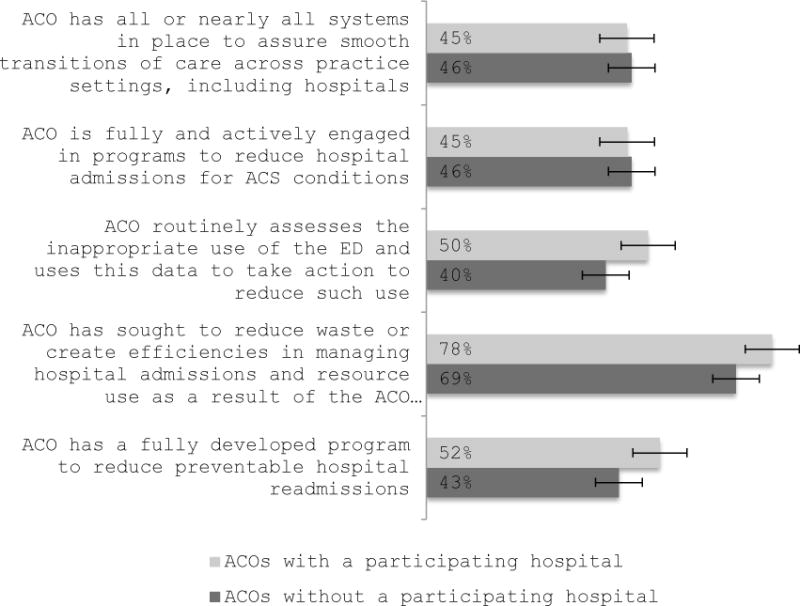
National Survey of Accountable Care Organizations, Waves 1 and 2.
Notes: ED is Emergency department. ACS is Ambulatory care sensitive, or potentially preventable hospitalizations. Twenty-three organizations did not complete the question on hospital inclusion, and were thus excluded from the analysis, resulting in 246 ACOs available for analyses based on NSACO data. Figures reported are unadjusted proportions of ACOs reporting the capability with two-sided bivariate mean comparison tests used to create confidence intervals. Error bars represent 95% confidence intervals around the estimates.
Qualitative Data Sources and Study Sample
Qualitative data come from three sets of semi-structured interviews conducted with key ACO personnel between 2013 and 2014, as well as four site visits between 2014 and 2015. Our sample consists of 58 interviews with 32 ACOs, 24 of which had a hospital participating. Interviewees were predominantly chief medical officers, but also included senior ACO leadership.
Each of the three annual sets of interviews utilized a unique interview guide to facilitate hour-long, semi-structured interviews, while maintaining a common set of questions on ACO structure, motivations and benefits of ACO formation, formation process, challenges to implementation, and future goals. Example questions from the interview guides are included in Appendix 2.(22)
Between September 2014 and March 2015, we also conducted site visits at four ACOs. Each site visit consisted of half-hour and hour-long semi-structured interviews with ACO leaders, clinical leadership, quality improvement staff, care management staff, and community health center leadership. Interviews were guided by a topic list with suggested questions that was developed based on each interviewee’s role in the ACO.
Qualitative Analyses
All interviews were recorded, transcribed, and coded for relevant and important themes. Broadly, we followed the constant comparative method of qualitative analysis,(23) iterating on our themes and results through a process of coding, analysis, re-coding, and updating our analysis. First, we coded globally for all discussion of hospitals. All excerpts related to hospitals were then subcoded for clinical content, or non-clinical discussion of hospitals (organizational structure, financing). A second person coded two interviews using the hospital clinical and hospital non-clinical codes. The two coders then discussed discrepancies and adjusted definitions accordingly. The coders agreed upon subthemes and coded within the non-clinical code, such as historic relationships, ACO and hospital financing, and changes since becoming an ACO. Codes were analyzed for underlying patterns and themes and were stratified by whether or not a hospital was participating in the ACO.
Limitations
Our data have some limitations. Our survey data present a wide spectrum of information about the ACO, but the responses only reflect the perspective of one individual at the organization. We found no evidence of non-response bias among Medicare ACOs using publicly available information,(12) but we cannot assess the presence of non-response bias in commercial ACOs. However, due to the high response rate, it is likely the impact of any non-response bias is small. In addition, our interviews and site visits were conducted on a sample that contains a large number of safety net ACOs, because of the nature of research questions being addressed, including behavioral health and community health center integration. None of the interviews were conducted with the goal of understanding the role of hospitals, yet interviewees frequently talked about hospitals in the context of their organizational structure and the challenges that they faced, and the results were discussed frequently enough to emerge as themes across interviews. Of note, and related to our qualitative findings, is the non-random selection as to whether an ACO includes a hospital.
Study Results
Quantitative Results
Types of Hospitals Participating in ACOs
To assess the types of hospitals participating in ACO contracts, we analyzed 5,110 hospitals; one-fifth of which are part of an ACO (N=1,042, Exhibit 1). Six percent of hospitals participate in a Medicare ACO (either Pioneer or Shared Savings Program), 10% in a commercial ACO, and 4% in both. Large and medium-sized non-profit hospitals make up the vast majority of hospitals participating in ACOs (Exhibit 1). In bivariate analyses, teaching hospitals and those that offer a more comprehensive number of services (such as obstetrics, intensive care, and other specialty services) are more likely to participate in ACOs. The large majority of hospitals participating in ACOs are short-term acute hospitals (85%), rather than critical access (12%) or specialty hospitals (3%). For hospitals participating in ACOs, 13% of the population in the catchment area has income under the federal poverty line compared to 16% for hospitals not participating in an ACO. The mean length of stay is greater in hospitals participating in ACOs and the case mix index is higher, indicating that patients may be more clinically complicated. Quality measures, such as serious complications and readmissions, do not differ significantly between hospitals in ACOs and those not in ACOs.
Controlling for other characteristics, the predicted probability of a non-profit hospital joining an ACO (24%) is markedly greater than a private or government hospital (7% and 8%, respectively, Exhibit 2). Large hospitals are more likely to have an ACO contract compared to small hospitals, with a predicted probability of 15.1% versus 10.2%. Hospitals participating in ACOs are more likely to be in the most heavily populated urban areas, and least likely to be in rural areas. The geographic concentration of hospitals participating in an ACO can be seen in Appendix 3,with more than two-thirds being located in the Eastern or Pacific regions.(22)
Involvement of Hospitals in ACOs – National Survey of ACO Results
Shifting from the population of hospitals to the population of ACOs, three-fifths of ACOs include at least one hospital, based on the National Survey of Accountable Care Organizations (Exhibit 3). ACOs without a hospital are more likely to have a Medicare ACO contract (87%, participating in either the Pioneer or the Shared Savings Program) than ACOs with a hospital (55%). In contrast, 66% of ACOs with a participating hospital have any private ACO contract holding the group financially responsible for quality and total cost of care, as opposed to about one-third of ACOs without a hospital. ACOs with a hospital have twice as many fulltime-equivalent primary care clinicians and more than three times as many specialty physicians compared to those ACOs without hospitals. ACOs that engage hospitals offer more extensive services than those without a hospital. For example, two-thirds of ACOs with a hospital offer any post-acute care, whereas only 10% of ACOs without a hospital provide these services.
Though ACOs that include hospitals offer more comprehensive services, ACOs do not report differences in ability to manage hospital-related aspects of patient care depending on whether or not they are affiliated with a hospital (Exhibit 4). About half of ACOs report having a fully developed program to assess readmissions, while three quarters report actively working on improving the efficiency of hospital use. Only a quarter report all or nearly all processes in place to assure smooth transitions across settings of care, an area where hospital engagement may be especially important.
Qualitative Results
In qualitative analysis we found that ACO formation and participation is largely influenced by previous relationships between primary care practices and hospitals. Three-quarters of ACOs with hospitals expressed having a relationship between primary care and the hospital prior to ACO formation, including a formal contractual relationship, informal connections, or both. There were two types of pre-existing formal contractual relationships. The first was physicians and hospitals previously participating together in risk-based contracts. In one case, a previously unaffiliated hospital and physician practice participated together in a capitated Medicaid contract (with a third party administrator) prior to both participating in the ACO. The second type of formal relationship was ownership relationships. We observed two types of ownership relationships: (1) physician practices owned by hospitals or health systems, and (2) physician practices and hospitals as members of physician hospital organizations. Most frequently among our interviewed ACOs, a set of unaffiliated practices joined with a set of previously affiliated hospitals and practices to pursue an ACO jointly.
ACOs also noted the importance of informal connections as precursors to ACO participation, such as pre-existing referral patterns and professional respect between primary care providers and hospital providers. Few ACOs without hospitals discussed their historic relationships with hospitals. Among those that did, most discussed negative former experiences with hospitals. Experiences such as a lack of success in previous payment reform efforts and mismanagement of outpatient practices by the hospital were noted as motivations to exclude hospitals from ACO formation.
Interviews and site visits provided evidence for three advantages of including a hospital in an ACO: start-up funding or capital for the ACO, more advanced patient data sharing, and engagement of providers across the care continuum. Among ACOs with hospitals, most reported that the hospital was an advantageous source of capital to the ACO (for example, to fund infrastructure work needed for quality reporting). One interviewee believed the hospital’s funds were essential to the ACO’s success because they could hire the necessary additional care management staff; the interviewee speculated that ACOs lacking a hospital partner would be unable to hire those personnel. Leaders of ACOs without hospitals thought a hospital would be a useful source of capital. One ACO without a hospital believed having a hospital could have provided the capital to facilitate participation in the ACO program, but instead the ACO relied on capital from the Advance Payment Model (in which physician-based and rural providers receive upfront and monthly advances on shared savings payments, which they can use to make investments in their care coordination infrastructure). Also, one ACO without a hospital noted that working with a hospital in some capacity was financially essential to taking on downside risk.
A second strategic advantage of hospital participation was patient data sharing between inpatient and outpatient settings, such as discharge summaries or alerts for an ACO patient admission or ED visit. Many of the ACOs including hospitals reported having systems or processes in place to share patient information between the hospital and providers outside of the hospital, though in some cases such exchange remains a challenge. About half of ACOs without hospitals mentioned difficulty getting timely information on ACO patients presenting at the hospital or ED, or details of these visits. None of the ACOs without hospitals mentioned that they have working systems in place to consistently receive patient information from hospitals.
A final strategic advantage to having a hospital in an ACO was the ability to engage care settings across the continuum to improve the capability of the ACO to control both quality and the total cost of care. Multiple ACOs discussed the participation of a hospital as an indication of the alignment of financial incentives across settings to improve coordination.
ACOs also expressed some difficulties about the involvement of hospitals and why the inclusion of a hospital may not be advantageous toward reducing spending. Some interviewees felt that hospitals could not fully commit to reducing spending because it would mean reductions in revenue on the inpatient or ED side. When speaking about the advantages of not having a hospital, one ACO noted that “in a way it’s cleaner, because we’re not part of a hospital, and so if hospital ED visits go down, and avoidable admissions go down, and high-cost imaging goes down, well, that’s just too bad.” This ACO felt that because they did not include a hospital, reductions in revenue due to shifts in utilization were not a problem– the ACO was better able to commit to accountable care because it did not have to worry about decreasing hospital revenue.
Discussion
Our research indicates the composition of ACOs depends in part on historic relationships, but ACOs are thinking strategically about the inclusion of hospitals. More than half of ACOs include a hospital, but the proportion of hospitals participating in an ACO is quite small (20% of all hospitals, with only 10% participating in a Medicare ACO program). Interviews and site visits provided evidence for advantages of including a hospital in an ACO: start-up funding or capital for the ACO, more advanced data sharing, and engagement of providers across the care continuum. Despite the theoretical advantages to hospital inclusion discussed in qualitative interviews, our research indicates that ACOs including hospitals do not report significant differences in their capabilities than their counterparts without hospitals. Large, non-profit, high-acuity hospitals in urban areas are more likely to be participating in ACOs.
Of the triple aim goals inherent to ACOS,(24) ability to control spending may provide the strongest business case for including hospitals in ACOs. ACOs noted the importance of the capital that hospitals can provide, but also considered the difficulties of competing goals. Two approaches regarding hospital care are likely to be taken by ACOs to achieve reductions in hospital spending. The first is to make inpatient care more efficient, using fewer services while the patient is hospitalized. This strategy requires engaging hospitals. A second approach to reducing hospital spending is encouraging patients to receive care in the appropriate location. This approach is likely to involve keeping patients out of the hospital and the ED through improved and increased access to outpatient care. This strategy is likely to dominate as even a minimally intensive hospital stay is still very expensive, and engaging hospitals is not necessary in this approach. In addition, high-occupancy hospitals may be able to use available beds for higher-margin patients. A third approach is to carefully manage the transition out of the hospital in order to minimize use of post-hospital care and reduce readmissions. Engaging hospitals more easily facilitates this strategy.
There may be implications for the large number of hospitals not participating in the ACO model. Hospitals may not be interested in joining ACOs either because they fear potential losses in revenue or do not want to make the necessary upfront investments.(25) In addition, in some cases not all patients or physicians who admit patients to the hospital are part of the ACO, forcing the hospital to straddle different payment schemes and approaches. Hospitals participating in ACOs may forge a new path for their business and may excel on measurable quality through stronger partnerships with outpatient care, impacting the relative performance of non-participating hospitals scores on hospital report cards.(26) Critical access hospitals have previously been shown to be lagging in terms of quality,(27) and participation of large, well-funded hospitals in ACOs as sources of financing may exacerbate differences in quality performance. It could also be that non-participating hospitals are merely biding their time to adapt to these new payment approaches and think they can maximize revenue more effectively by waiting to join ACOs.
We do not know yet whether inclusion of a hospital in an ACO is necessary to achieve successful quality or cost performance. Our qualitative interviews indicate that some ACOs have decided that the costs of hospital inclusion outweigh the benefits. In early results from the Medicare programs, Pioneers (86% of whom have a hospital participating) were able to save money by limiting both inpatient and outpatient care (although spending on outpatient care in office settings differentially increased while spending on hospital outpatient care was differentially lower).(28, 29) These results, in combination with the results showing equal capabilities from the National Survey of Accountable Care Organizations, demonstrate the feasibility for achieving savings regardless of hospital inclusion. Coordination across organizations and settings is notoriously difficult (30–33)and may take more time to be realized. Future research should examine the role of hospital inclusion and the extent of hospital engagement in performance of ACOs on cost and quality metrics, while informing policy solutions to further engage hospitals excluded from the current set of reforms.(34)
Policymakers have the ability to change some of the perceived disadvantages to forming an ACO without a hospital by providing access to capital and support for implementing health information exchange systems so that these groups might more easily obtain such data as Admit-Discharge-Transfer notifications. The Advance Payment Model and the ACO Investment Model (a Medicare program of pre-paid shared savings to use as start-up funding) were created to attract providers that might be otherwise unable to participate in the ACO model due to financial constraints; this may be one reason we observe a greater proportion of ACOs without hospitals with a Medicare contract. If ACOs are able to achieve success across quality and cost goals, it will be important to assure broader and more consistent participation of different types of providers in the model.
Supplementary Material
Acknowledgments
This research was supported by grants from the Commonwealth Fund (Grant No. 20150034), the National Institute on Aging (Grant No. 5R33AG044251), and the Dartmouth Clinical and Translational Science Institute (through Grant No. UL1TR001086 from the National Center for Advancing Translational Sciences). The content of the article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health
Contributor Information
Carrie H. Colla, Email: Carrie.H.Colla@Dartmouth.edu, The Dartmouth Institute for Health Policy & Clinical Practice, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire Phone: (603) 650-3521.
Valerie A. Lewis, The Dartmouth Institute for Health Policy & Clinical Practice, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire.
Emily Tierney, The Dartmouth Institute for Health Policy & Clinical Practice, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire.
David B. Muhlestein, Leavitt Partners, Salt Lake City, Utah
References
- 1.Shortell SM, Gillies RR, Anderson DA. The new world of managed care: creating organized delivery systems. Health Aff (Millwood) 1994;13(5):46–64. doi: 10.1377/hlthaff.13.5.46. [DOI] [PubMed] [Google Scholar]
- 2.Cutler DM, Scott Morton F. Hospitals, market share, and consolidation. JAMA. 2013;310(18):1964–70. doi: 10.1001/jama.2013.281675. [DOI] [PubMed] [Google Scholar]
- 3.Baicker K, Levy H. Coordination versus competition in health care reform. N Engl J Med. 2013;369(9):789–91. doi: 10.1056/NEJMp1306268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lewis VA, Colla CH, Schpero WL, Shortell SM, Fisher ES. ACO contracting with private and public payers: a baseline comparative analysis. Am J Manag Care. 2014;20(12):1008–14. [PubMed] [Google Scholar]
- 5.Muhlestein D. Health Affairs Blog [Internet] 2015 Available from: http://healthaffairs.org/blog/2015/03/31/growth-and-dispersion-of-accountable-care-organizations-in-2015–2/
- 6.Medicare Payment Advisory Commission (MedPAC) Health Care Spending and the Medicare Program. 2015 Jun; http://www.medpac.gov/documents/data-book/june-2015-databook-health-care-spending-and-the-medicare-program.pdf?sfvrsn=0:
- 7.RTI International. Accountable care organization 2014 program analysis quality performance standards narrative measure specifications. 2014 [Google Scholar]
- 8.RTI International. Accountable care organizations 2015 program analysis quality performance standards narrative measure specifications. 2015 [Google Scholar]
- 9.Larson BK, Van Citters AD, Kreindler SA, Carluzzo KL, Gbemudu JN, Wu FM, et al. Insights from transformations under way at four Brookings-Dartmouth accountable care organization pilot sites. Health Aff (Millwood) 2012;31(11):2395–406. doi: 10.1377/hlthaff.2011.1219. [DOI] [PubMed] [Google Scholar]
- 10.Shortell SM, Wu FM, Lewis VA, Colla CH, Fisher ES. A taxonomy of accountable care organizations for policy and practice. Health Serv Res. 2014;49(6):1883–99. doi: 10.1111/1475-6773.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Epstein AM, Jha AK, Orav EJ, Liebman DL, Audet AM, Zezza MA, et al. Analysis of early accountable care organizations defines patient, structural, cost, and quality-of-care characteristics. Health Aff (Millwood) 2014;33(1):95–102. doi: 10.1377/hlthaff.2013.1063. [DOI] [PubMed] [Google Scholar]
- 12.Colla CH, Lewis VA, Shortell SM, Fisher ES. First national survey of ACOs finds that physicians are playing strong leadership and ownership roles. Health Aff (Millwood) 2014;33(6):964–71. doi: 10.1377/hlthaff.2013.1463. [DOI] [PubMed] [Google Scholar]
- 13.Muhlestein D, Gardner P, Merrill T, Petersen M, Tu T. A Taxonomy of Accountable Care Organizations: Different Approaches to Achieve the Triple Aim. 2014 [Google Scholar]
- 14.Colla CH, Lewis VA, Gottlieb DJ, Fisher ES. Cancer spending and accountable care organizations: Evidence from the Physician Group Practice Demonstration. Healthcare: The Journal of Delivery Science and Innovation. 2013;1(3):100–7. doi: 10.1016/j.hjdsi.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colla CH, Wennberg DE, Meara E, Skinner JS, Gottlieb D, Lewis VA, et al. Spending differences associated with the Medicare Physician Group Practice Demonstration. JAMA. 2012;308(10):1015–23. doi: 10.1001/2012.jama.10812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nyweide DJ, Lee W, Cuerdon TT, Pham HH, Cox M, Rajkumar R, et al. Association of Pioneer Accountable Care Organizations vs Traditional Medicare Fee for Service With Spending, Utilization, and Patient Experience. JAMA. 2015 doi: 10.1001/jama.2015.4930. [DOI] [PubMed] [Google Scholar]
- 18.Medicare ACOs Continue to Succeed in Improving Care, Lowering Cost Growth [press release] 2014 Nov 10; [Google Scholar]
- 19.Pham HH, Cohen M, Conway PH. The pioneer accountable care organization model: Improving quality and lowering costs. JAMA. 2014 doi: 10.1001/jama.2014.13109. [DOI] [PubMed] [Google Scholar]
- 20.Muhlestein D, Hall C. Health Affairs Blog [Internet] 2014 Available from: http://healthaffairs.org/blog/2014/12/18/aco-quality-results-good-but-not-great/
- 21.Rittenhouse DR, Shortell SM, Fisher ES. Primary care and accountable care–two essential elements of delivery-system reform. N Engl J Med. 2009;361(24):2301–3. doi: 10.1056/NEJMp0909327. [DOI] [PubMed] [Google Scholar]
- 22.Editor please insert appendix verbiage.
- 23.Glaser BGS, Anselm L. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago: Aldine Publishing Company; 1967. [Google Scholar]
- 24.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood) 2008;27(3):759–69. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 25.Larkin H. ACO or no: how to decide. Hospitals must weigh the benefits and the risks before choosing their paths. Trustee. 2014;67(7):15–6. 21–3, 1. [PubMed] [Google Scholar]
- 26.Centers for Medicare & Medicaid Services. Hospital compare 2014. [cited 2014 October 30]. Available from: http://www.medicare.gov/hospitalcompare/search.html.
- 27.Joynt KE, Harris Y, Orav EJ, Jha AK. Quality of care and patient outcomes in critical access rural hospitals. JAMA. 2011;306(1):45–52. doi: 10.1001/jama.2011.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.L & M Policy Research. (Report No.: Contract HHSM-500-2011-0009i/HHSM-500-T0002).Evaluation of CMMI accountable care organization initiatives. 2013 Nov 3; 2013. [Google Scholar]
- 29.McWilliams JM, Chernew ME, Landon BE, Schwartz AL. Performance Differences in Year 1 of Pioneer Accountable Care Organizations. N Engl J Med. 2015;372(20):1927–36. doi: 10.1056/NEJMsa1414929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gittell JH, Weiss L. Coordination Networks Within and Across Organizations: A Multi-level Framework. Journal of Management Studies. 2004;41(1):127–53. [Google Scholar]
- 31.Bodenheimer T. Coordinating care-a perilous journey through the health care system. N Engl J Med. 2008;358(10):1064. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 32.Boling PA. The value of targeted case management during transitional care. JAMA. 1999;281(7):656–7. doi: 10.1001/jama.281.7.656. [DOI] [PubMed] [Google Scholar]
- 33.Coleman EA. Falling Through the Cracks: Challenges and Opportunities for Improving Transitional Care for Persons with Continuous Complex Care Needs. Journal of the American Geriatrics Society. 2003;51(4):549–55. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 34.Rau J. Many rural hospitals are excluded from government’s push for better quality. Kaiser Health News [Internet] 2014 Available from: http://www.kaiserhealthnews.org/Stories/2014/September/30/Many-Rural-Hospitals-Are-Excluded-From-Governments-Push-For-Better-Quality.aspx.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


