Abstract
Background
There is increasing desire among service commissioners to treat arrhythmia in primary care. Accurate interpretation of the electrocardiogram (ECG) is fundamental to this. ECG interpretation has previously been shown to vary widely but there is little recent data.
Aim
To examine the interpretation of ECGs in primary and secondary care.
Design and setting
A cross-sectional survey of participants’ interpretation of six ECGs and hypothetical management of patients based on those ECGs, at primary care educational events, and a cardiology department in Leeds.
Method
A total of 262 primary care clinicians and 20 cardiology clinicians were surveyed via questionnaire. Answers were compared with expert electrophysiologist opinion.
Results
In primary care, abnormal ECGs were interpreted as normal by 23% of responders. ST elevation and prolonged QT were incorrectly interpreted as normal by 1% and 22%, respectively. In cardiology, abnormal ECGs were interpreted as normal by 3%.
Conclusion
ECG provision and interpretation remains inconsistent in both primary and secondary care. Primary care practitioners are less experienced and less confident with ECG interpretation than cardiologists, and require support in this area.
Keywords: cardiac arrhythmias, cardiology, electrocardiography, general practice, questionnaires
INTRODUCTION
Most patients who experience arrhythmia that does not cause an emergency admission present to primary care. The electrocardiogram (ECG) is fundamental to the assessment of such patients, usually carried out as a first-line investigation after a detailed history and examination; this is an approach recommended in a number of relevant guidelines.1–4 A high-quality ECG accompanied by accurate interpretation is important for the subsequent management of these patients; a normal ECG is an indicator of lower risk, whereas certain ECG features should generally initiate further assessment. Such ECG findings have been defined by the National Institute for Health and Care Excellence, and called ‘red flags’.4 Over- or underreporting of ECG abnormalities in primary care could result in inappropriate patient management.
Previous research has shown that ECG interpretation in primary care can be variable.5,6 The aim of this study was to explore the current levels of GPs’ confidence with regards to ECG interpretation, as well as accuracy and the ability to recognise ‘red flags’, and to assess cardiology clinicians similarly.
METHOD
A survey was conducted at three mandatory training events held over 9 days — one for each clinical commissioning group area in Leeds. A questionnaire was designed that contained two sections. Section 1 collected demographic information, responders’ familiarity with ECG, and their desire for an improved local ECG reporting service (Table 1).
Table 1.
Responses to section 1 of the questionnaire
| Question | Primary care (n= 262), n (%) | Cardiology (n= 20), n (%) |
|---|---|---|
| What is your position? | ||
| GP | 226 (87) | – |
| GP registrar | 13 (5) | – |
| Nurse | 5 (2) | – |
| Other (foundation doctor/nurse practitioner) | 11 (4) | – |
| Consultant cardiologist | – | 10 (50) |
| Cardiology specialty registrar | – | 9 (45) |
| Nurse specialist | – | 1 (5) |
| Unanswered/illegible | 7 (3) | 0 (0) |
|
| ||
| Do you have an ECG machine in your practice? | ||
| Yes | 215 (82) | – |
| No | 15 (6) | – |
| Unanswered/illegible | 32 (12) | – |
|
| ||
| Who performs the ECGs in your practice? | ||
| Nurse | 94 (36) | – |
| Healthcare assistant | 78 (30) | – |
| Both nurse and healthcare assistant | 43 (16) | – |
| Doctor | 5 (2) | – |
| Other | 2 (1) | – |
| Unanswered/illegible | 40 (15) | – |
|
| ||
| How many ECGs do you interpret per week? | ||
| ≤1 | 153 (58) | 2 (10) |
| 2–5 | 82 (31) | 1 (5) |
| 6–10 | 8 (3) | 3 (15) |
| >10 | 2 (1) | 14 (70) |
| Unanswered/illegible | 17 (6) | 0 (0) |
|
| ||
| How comfortable do you feel with ECG interpretation? | ||
| Very comfortable | 6 (2) | 12 (60) |
| Fairly comfortable | 112 (43) | 8 (40) |
| Neither comfortable nor uncomfortable | 42 (16) | 0 |
| Fairly uncomfortable | 67 (26) | 0 |
| Very uncomfortable | 13 (5) | 0 |
| Unanswered/illegible | 22 (8) | 0 |
|
| ||
| Do you feel there is a need for a rapid (same-day) ECG reporting service? | ||
| Yes | 194 (74) | 12 (60) |
| No | 42 (16) | 7 (35) |
| Unanswered/illegible | 26 (10) | 1 (5) |
ECG = electrocardiogram.
For section 2, six ECGs with brief descriptions of the associated patient’s presentation were projected onto a screen in front of delegates for a minute each. The ECGs and accompanying presentations are shown in Figure 1. They were selected by two cardiac electrophysiology consultants who felt that the presenting complaints represented common symptoms that may be associated with arrhythmia, whereas the ECGs contained a range of findings, from normal to ‘red flags’ that would require urgent action. Responders were asked:
Is the ECG abnormal?
If yes, what is the ECG diagnosis?
What would you do based on this ECG? Reassure/treat in primary care/refer to secondary care as an outpatient/refer to secondary care as an emergency/or other.
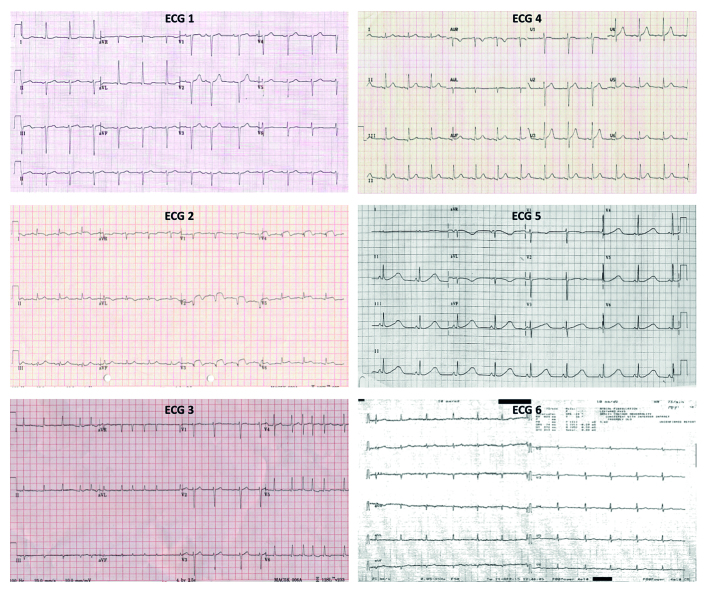
Figure 1.
ECG findings and patient presentations.
ECG 1: Left axis deviation, single atrial ectopic beat. ’40-year-old female with flutters.’
ECG 2: ST elevation. ’55-year-old male, syncope at the gym’ (RED FLAG).
ECG 3: Atrial fibrillation. ’75-year-old female, diabetic, no symptoms.’
ECG 4: Normal ECG. ‘50-year-old female, sudden onset and offset regular palpitations.’
ECG 5: Prolonged QT interval. ’16-year-old female, blackout in school assembly’ (RED FLAG).
ECG 6: Poor-quality ECG, sinus rhythm, erroneous automated report of AF. ’81-year-old female, breathless.’
A similar questionnaire, with section 1 modified for hospital practitioners, was given to staff in cardiology at the Leeds General Infirmary, a large department providing secondary care cardiology services for Leeds and tertiary services for West Yorkshire.
The following rules were followed when recording the responses to the ECG quiz (section 2):
If the responder had not answered A, but had answered B, A was recorded as ‘abnormal’.
If the responder had answered A ‘normal’, but had answered B, A was recorded as ‘abnormal’.
ECG diagnoses in B were answered with free text. Responses were assessed by one of the authors (a cardiology specialty registrar), and recorded as ‘correct’ or ‘incorrect’ based on the predefined diagnosis provided by the two consultant electrophysiologists. Answers that were equivocal were referred to the electrophysiologists, who were blinded to the profession of the responder, for a final decision.
In C, if multiple choices were indicated, the highest response was recorded, for example, if the response was ‘treat in primary care’ and ‘refer to secondary care’, then ‘refer to secondary care’ was recorded.
How this fits in
There is increasing desire to treat arrhythmia in primary care where possible. A number of studies have previously identified inconsistency in reporting ECGs, among diverse groups of clinicians, but no recent study has addressed this in UK primary care. This study has examined the level of accuracy in ECG interpretation in primary care and cardiology in a large city.
Results are presented as simple percentage of responses received for each question, in each group (primary care or cardiology). Missing data (that is, illegible or unanswered responses) are represented as a percentage of the total number of questionnaires returned for the relevant group.
RESULTS
Of 309 primary care attendees, 262 (85%) returned a questionnaire. In cardiology, all 20 attendees returned a questionnaire. Primary care responses were completed by 226 GPs, 13 GP registrars, five nurses, and 11 others, although seven did not identify their role. In cardiology, 10 consultants, nine specialty registrars, and one nurse specialist responded.
Table 1 shows all the responses for section 1 of the questionnaire. In primary care, responses indicated that most ECGs are performed by healthcare assistants and nurses (n = 215; 82%). Most primary care responders (n = 235; 90%) interpreted <5 ECGs a week, whereas 85% of secondary care practitioners (n = 17) interpreted ≥6. A small proportion of responders (n = 15; 6%) indicated that their practice did not have an ECG machine. All cardiology clinicians felt ‘fairly’ or ‘very’ comfortable with ECG interpretation, compared with 45% of those in primary care (n = 118). Both cardiology clinicians (n = 12; 60%) and primary care clinicians (n = 194; 74%) felt that there is a need for an ECG reporting service for primary care.
Table 2 shows all responses to section 2 of the questionnaire. Overall, abnormal ECGs (ECGs 1, 2, 3, and 5) were identified as normal in 23% (238 of 1048 answers) in primary care, with 1% and 22% interpreting as normal the ‘red flags’ of ST elevation and prolonged QT interval, respectively. In cardiology, abnormal ECGs were identified as normal in 3% (2 of 80 answers), with no failure to identify the red flags. In primary care, normal ECGs 4 and 6 were identified as abnormal in 41% (212 of 524 answers). In cardiology this figure was 18% (7 of 40 answers). This was mainly as a result of ECG 6 being a poor-quality recording.
Table 2.
Responses to section 2 of the questionnaire
| ECG number and presentation | Question | PC, %a | C, %a | Unanswered/illegible | |
|---|---|---|---|---|---|
|
| |||||
| PC (% of 262) | C (% of 20) | ||||
| ECG1 = left axis and atrial ectopic | Normal/abnormal answered correctly | 54 | 95 | 7 | 0 |
| Diagnosis answered correctly | 48 | 73 | 59 | 5 | |
| Reassure | 68 | 50 | |||
| ‘40-year-old female with flutters’ | Treat in primary care | 14 | 5 | ||
| Refer as outpatient | 15 | 35 | 19 | 0 | |
| Refer as emergency | 1 | 0 | |||
| Other | 2 | 10 | |||
|
| |||||
| ECG2 = ST elevation | Normal/abnormal answered correctly | 99 | 100 | 4 | 0 |
| RED FLAG | Diagnosis answered correctly | 78 | 100 | 25 | 0 |
| Reassure | 0 | 0 | |||
| ‘55-year-old male, syncope at the gym’ | Treat in primary care | 1 | 0 | ||
| Refer as outpatient | 13 | 0 | 13 | 0 | |
| Refer as emergency | 85 | 100 | |||
| Other | 1 | 0 | |||
|
| |||||
| ECG3 = atrial fibrillation | Normal/abnormal answered correctly | 98 | 100 | 5 | 0 |
| Diagnosis answered correctly | 90 | 95 | 16 | 0 | |
| ‘75-year-old female, diabetic, no symptoms’ | Reassure | 2 | 0 | ||
| Treat in primary care | 19 | 36 | |||
| Refer as outpatient | 75 | 57 | 14 | 0 | |
| Refer as emergency | 3 | 0 | |||
| Other | 1 | 5 | |||
|
| |||||
| ECG4 = normal sinus rhythm | Normal/abnormal answered correctly | 64 | 75 | 12 | 0 |
| Diagnosis answered correctly | NA | NA | NA | NA | |
| Reassure | 36 | 5 | |||
| ‘50-year-old female, sudden onset and offset regular palpitations’ | Treat in primary care | 11 | 10 | ||
| Refer as outpatient | 44 | 75 | 30 | 0 | |
| Refer as emergency | 3 | 5 | |||
| Other | 6 | 5 | |||
|
| |||||
| ECG5 = prolonged | Normal/abnormal answered correctly | 80 | 100 | 7 | 0 |
| QT interval RED FLAG | Diagnosis answered correctly | 37 | 100 | 40 | 0 |
| Reassure | 25 | 0 | 24 | 0 | |
| ‘16-year-old female, blackout in school assembly’ | Treat in primary care | 5 | 0 | ||
| Refer outpatient | 40 | 20 | |||
| Refer as emergency | 25 | 80 | |||
| Other | 6 | 0 | |||
|
| |||||
| ECG6 = sinus rhythm, auto-report states AF | Normal/abnormal answered correctly | 16 | 45 | 13 | 0 |
| Diagnosis answered correctly | NA | NA | NA | NA | |
| Reassure | 10 | 22 | |||
| ‘81-year-old female, breathless’ | Treat in primary care | 18 | 33 | ||
| Refer as outpatient | 45 | 28 | 31 | 10 | |
| Refer as emergency | 20 | 0 | |||
| Other | 7 | 17 | |||
% of attempted answers. Shaded = electrophysiologists’ opinion of best management option. Bold = notable results. AF = atrial fibrillation. C = cardiology. ECG = electrocardiogram. NA = not applicable. PC = primary care.
DISCUSSION
Summary
The results suggest that there is wide variability in both ECG interpretation accuracy and arrhythmia management in primary care. Such variability also exists, to a lesser extent, among cardiology clinicians. Moreover, the questionnaire highlighted specific situations where inaccuracy of interpretation could lead to inappropriate treatment, or, conversely, lack thereof. The potential for inappropriate anticoagulation in sinus rhythm, or inappropriate reassurance in the case of long QT syndrome, are examples.
Strengths and limitations
The authors believe this study is the largest direct survey of ECG interpretation and arrhythmia management in UK primary care. It is a pragmatic assessment of everyday practice incorporating as many responders as possible in a limited time, in a format that minimises the possibility of collusion between responders and the use of external references to assist with answers, albeit not as stringently as formal examination conditions. The six ECGs chosen represent both common problems and uncommon ‘red flag’ diagnoses. Responders were given only a minute to review each ECG to decide on management, reflecting the time pressures that exist in modern clinical care. Although the ECGs were projected, which is not how clinicians would normally view them, little feedback was received about the visibility being poor. The study population was based in one city, and therefore referral and treatment patterns may reflect local policy and health service structure. However, a wider survey was not feasible and the authors believe that these results are likely to reflect UK practice as a whole.
Comparison with existing literature
Recognition of ECG abnormalities was shown to vary greatly according to diagnosis, clinician experience, and frequency of ECG interpretation in a 1990 UK postal questionnaire by Macallan and colleagues.5 In their analysis of the Screening for Atrial Fibrillation in the Elderly (SAFE) trial in 2007, Mant and colleagues6 concluded that automated interpretation, even in conjunction with manual analysis by GPs, was insufficiently accurate to detect atrial fibrillation (AF) in a primary care setting. Problems with automated interpretation with diagnoses beyond AF had also been highlighted in a large prospective Danish analysis in 2005, with GP interpretation sensitivity lower than automatic interpretation.7 GPs exhibited higher specificity, but the danger of reclassifying true positives to false negatives was evident.7 A number of other studies, across a variety of specialties, have shown similar themes.8–10
The current study echoes these findings in a large UK primary care cohort involving a number of arrhythmia diagnoses and confirms that inconsistency in ECG interpretation continues to exist.
Implications for practice
Automated interpretation is widely used in primary care and, although this can be helpful, it does have drawbacks.6,7 ECG 6 included an erroneous automated report identifying AF. The ECG used was a genuine ECG that had accompanied a referral to the AF clinic. It was of poor quality, but did not show AF, which is why it was selected as a ‘real-life’ example. On the basis of this poor-quality trace, 60% of primary care responders believed that the ECG was abnormal and 65% of those who answered the associated management question believed that referral to secondary care was warranted. Conceivably, this may have led to the inappropriate anticoagulation of patients with accompanying risk of bleeding events. Conversely, 22% of primary care responders failed to identify the grossly prolonged QT interval in ECG 5 — a ‘red flag’ — without the aid of an automated report. Although rare, missing such an ECG finding could result in a missed opportunity to prevent sudden cardiac death. Although ECG machines will usually highlight such findings, it is concerning that these results highlight over-reliance on automated reporting, which has led to deterioration in interpretation skills and could increase patients’ exposure to unnecessary treatments and risk.
Salerno et al 10 highlighted in their 2003 review that variability in competency exists not only in primary care but also among diverse cohorts of medical professionals at different stages of training and practice, including cardiologists. They called for improved standardisation of education to help reduce variability. Education is fundamental to the reduction of variability and the current authors received a number of requests for instruction in the free-text responses. However, it is difficult to envisage an education programme capable of delivering the required consistency with the resources currently available. Any education programme for primary care could, perhaps, be focused less on ECG interpretation and instead on the more easily achievable goal of high-quality ECG acquisition, which will both improve automated reporting and facilitate fast, reliable manual interpretation when it is required.
Over half of primary care responders in the current study interpreted <1 ECG per week, with only 4% (n = 10) interpreting >5. It is difficult for GPs to be reasonably expected to make ECG-based management decisions in isolation with such low exposure to ECGs. Indeed, 31% of primary care responders (n = 80) felt ‘fairly’ or ‘very’ uncomfortable with ECG interpretation. A large proportion (74%; n = 194) of primary care responders expressed a desire for an expert ECG reporting service, which may further highlight an understandable lack of confidence with ECG interpretation.
ECG interpretation accuracy is, unsurprisingly, higher and more consistent among cardiologists, but resulting management decisions are variable in both groups. It is therefore unreasonable to expect high levels of consistency among primary care clinicians practising in isolation. Primary care management of arrhythmia may best be carried out in close collaboration with cardiology secondary care services. Such a care model could be based on locally constructed consensus protocols, developed by experts in arrhythmia management and in conjunction with primary care colleagues, in order to minimise variability. A service providing immediate support and advice for primary care could be delivered by dedicated specialist nurses with readily available access to consultant cardiologists. Such an approach would lead to effective, efficient, and, above all, safe care for patients with arrhythmia.
Funding
Funding for printed materials was provided by Leeds Teaching Hospitals NHS Trust.
Ethical approval
Ethical approval was not sought for this survey as no patients or patient data were involved.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
Gordon Begg declares funding from an unrestricted research grant provided by St Jude Medical. All other authors have no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Blomström-Lundqvist C, Scheinman MM, Aliot EM, et al. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias — executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients with Supraventricular Arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003;42(8):1493–1531. doi: 10.1016/j.jacc.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 2.Camm AJ, Lip GY, De Caterina R, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33(21):2719–2747. doi: 10.1093/eurheartj/ehs253. [DOI] [PubMed] [Google Scholar]
- 3.National Institute for Health and Care Excellence . Atrial fibrillation: management. London: NICE; 2014. p. CG180. https://www.nice.org.uk/guidance/cg180 (accessed 25 Feb 2016). [PubMed] [Google Scholar]
- 4.National Institute for Health and Care Excellence . Transient loss of consciousness (‘blackouts’) in over 16s. London: NICE; 2010. p. CG109. https://www.nice.org.uk/guidance/cg109 (accessed 25 Feb 2016). [PubMed] [Google Scholar]
- 5.Macallan DC, Bell JA, Braddick M, et al. The electrocardiogram in general practice: its use and its interpretation. J R Soc Med. 1990;83(9):559–562. doi: 10.1177/014107689008300909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mant J, Fitzmaurice DA, Hobbs FD, et al. Accuracy of diagnosing atrial fibrillation on electrocardiogram by primary care practitioners and interpretative diagnostic software: analysis of data from screening for atrial fibrillation in the elderly (SAFE) trial. BMJ. 2007;335(7616):380. doi: 10.1136/bmj.39227.551713.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jensen MS, Thomsen JL, Jensen SE, et al. Electrocardiogram interpretation in general practice. Fam Pract. 2005;22(1):109–113. doi: 10.1093/fampra/cmh601. [DOI] [PubMed] [Google Scholar]
- 8.Woolley D, Henck M, Luck J. Comparison of electrocardiogram interpretations by family physicians, a computer, and a cardiology service. J Fam Pract. 1992;34(4):428–432. [PubMed] [Google Scholar]
- 9.Jheeta JS, Narayan O, Krasemann T. Accuracy in interpreting the paediatric ECG: a UK-wide study and the need for improvement. Arch Dis Child. 2014;99(7):646–648. doi: 10.1136/archdischild-2013-305788. [DOI] [PubMed] [Google Scholar]
- 10.Salerno SM, Alguire PC, Waxman HS. Competency in interpretation of 12-lead electrocardiograms: a summary and appraisal of published evidence. Ann Intern Med. 2003;138(9):751–760. doi: 10.7326/0003-4819-138-9-200305060-00013. [DOI] [PubMed] [Google Scholar]