Abstract
Background
Differences in blood pressure between arms are associated with increased cardiovascular mortality in cohorts with established vascular disease or substantially elevated cardiovascular risk.
Aim
To explore the association of inter-arm difference (IAD) with mortality in a community-dwelling cohort that is free of cardiovascular disease.
Design and setting
Cohort analysis of a randomised controlled trial in central Scotland, from April 1998 to October 2008.
Method
Volunteers from Lanarkshire, Glasgow, and Edinburgh, free of pre-existing vascular disease and with an ankle-brachial index ≤0.95, had systolic blood pressure measured in both arms at recruitment. Inter-arm blood pressure differences were calculated and examined for cross-sectional associations and differences in prospective survival. Outcome measures were cardiovascular events and all-cause mortality during mean follow-up of 8.2 years.
Results
Based on a single pair of measurements, 60% of 3350 participants had a systolic IAD ≥5 mmHg and 38% ≥10 mmHg. An IAD ≥5 mmHg was associated with increased cardiovascular mortality (adjusted hazard ratio [HR] 1.91, 95% confidence interval [CI] = 1.19 to 3.07) and all-cause mortality (adjusted HR 1.44, 95% CI = 1.15 to 1.79). Within the subgroup of 764 participants who had hypertension, IADs of ≥5 mmHg or ≥10 mmHg were associated with both cardiovascular mortality (adjusted HR 2.63, 95% CI = 0.97 to 7.02, and adjusted HR 2.96, 95% CI = 1.27 to 6.88, respectively) and all-cause mortality (adjusted HR 1.67, 95% CI = 1.05 to 2.66, and adjusted HR 1.63, 95% CI = 1.06 to 2.50, respectively). IADs ≥15 mmHg were not associated with survival differences in this population.
Conclusion
Systolic IADs in blood pressure are associated with increased risk of cardiovascular events, including mortality, in a large cohort of people free of pre-existing vascular disease.
Keywords: blood pressure, cardiovascular diseases, cohort studies, inter-arm difference, primary care, subclavian artery stenosis
INTRODUCTION
A difference in blood pressure between arms is associated with peripheral arterial disease, and with increased cardiovascular or all-cause mortality.1 Previous studies have demonstrated associations between systolic inter-arm differences (IADs) ≥10 mmHg or ≥15 mmHg and reduced survival in cohorts with established vascular disease or high cardiovascular risk.2–7 The need to explore this association in cohorts more representative of a general population has been identified.6
IAD in previous survival studies has been assessed using two7–9 or three pairs2,6 of blood pressure readings. Multiple readings avoid over-estimation of IADs,10,11 but a single pair of readings can screen out individuals without an IAD.12 It was therefore hypothesised that an IAD assessed from a single pair of readings, although overestimating the true prevalence of any difference in the chosen population, would still predict reduced survival for the cohort of subjects with an apparent IAD, because that cohort will include the majority of subjects with a true difference.
Measurement of both arms is advised in initial assessment of patients with hypertension, but this advice is infrequently followed.13,14 The optimum strategy for assessment of IAD in primary care is unknown, but it should be a simple procedure in order for it to become accepted practice, so it is likely to be based on an initial single measurement of both arms.15
The aspirin for asymptomatic atherosclerosis (AAA) trial, a randomised controlled trial conducted from April 1998 to October 2008, recruited 3350 males and females aged 50–75 years living in central Scotland and free of pre-existing clinical cardiovascular disease, from a community health registry. Participants were selected as having an elevated cardiovascular event risk, defined by an ankle-brachial index ≤0.95, and allocated to receive low-dose aspirin (100 mg) or placebo daily to study the risks and benefits of long-term aspirin use in primary prevention. The recruitment protocol included a bilateral brachial blood pressure measurement. Participants were prospectively followed up for 10 years.16
The authors undertook a cohort study of participants in the AAA trial using the bilateral brachial systolic blood pressures recorded at recruitment to examine the implications of a single assessment of systolic inter-arm blood pressure difference for survival in a large community-based cohort free of confirmed pre-existing vascular disease, but at moderately increased risk based on a low ankle-brachial index.
How this fits in
A difference in blood pressure between arms is associated with peripheral arterial disease, and with increased cardiovascular mortality. Evidence for this association in populations representative of a British primary care population is limited. This study examines the survival implications of a systolic inter-arm blood pressure difference in a representative population, obtained with a single pair of sequential blood pressure measurements. Increased cardiovascular and all-cause mortality is demonstrated for an inter-arm difference (IAD) ≥5 mmHg and ≥10 mmHg. The findings support current guidance to measure both arms in assessing patients for high blood pressure. IADs can predict presence of peripheral arterial disease, and can refine estimation of future cardiovascular risk.
METHOD
Study design
A cohort study of all AAA trial participants. Although conducted following completion of the AAA trial, the authors set up the study hypothesis and pre-defined the evaluation protocol prior to undertaking data analysis.
Study participants
Recruitment and screening methods have been fully described elsewhere.16,17 In summary, volunteers were recruited from Lanarkshire, Glasgow, and Edinburgh in central Scotland via community health indexes and local advertising, and invited for ankle-brachial index screening administered by specially trained nurses. Those with an ankle-brachial index of ≤0.95 entered the study cohort unless they had a history of myocardial infarction, stroke, angina, or peripheral artery disease, currently used aspirin, other antiplatelet or anticoagulant agents, or had contraindications to aspirin use.
Blood pressure assessment
Measurements were taken by specially trained nurses who had regular quality control sessions throughout the trial. Subjects were rested supine for at least 5 minutes, and systolic blood pressures were measured with Doppler probes (Huntleigh Healthcare, Cardiff, UK) and aneroid desk sphygmomanometers (Accoson; A.C. Cossor Ltd, London, UK) in a fixed sequence (right arm — left arm — left leg — right leg). The ankle-brachial index was calculated as the ratio of lowest ankle pressure (lower of posterior tibial and dorsalis pedis and of left and right) to higher arm pressure.18 A further brachial systolic and diastolic blood pressure was then measured in the right arm by auscultation. There was no formal mechanism for deciding on cuff size: this was left to the nurses’ discretion. Originally, only the higher-reading Doppler systolic arm pressure was entered into the study database. For this analysis, both arm systolic pressures were transcribed to the study database from original recruitment screening records. The systolic IAD was calculated as the right minus left brachial pressures. Pulse pressure was calculated from the right-arm brachial auscultation pressures.
Follow-up and outcomes
Participants were followed up 3 months, 1 year, and 5 years post-randomisation to aspirin or placebo at special clinics, and annually by telephone. They received a mid-year letter enquiring generally about problems and an end-of-year newsletter. They were followed up until the end of the trial, irrespective of experiencing any endpoint or adverse event. The trial ran from April 1998 to October 2008. Ascertainment of events was sought annually by participant follow-up, by study reply card attached to GP notes, by flagging for death notifications at the NHS central registry, and also by linkage to databases of deaths and hospital discharges at NHS National Services Scotland. Confirmation of events (Appendix 1) was sought by review of hospital and GP records independently by two members of the outcome events committee, with adjudication by the full committee in cases of disagreement.
Data analysis
Baseline characteristics of participants according to systolic IAD cut-offs ≥5 mmHg, ≥10 mmHg, and ≥15 mmHg were compared using t-tests or χ2 tests as appropriate. Kaplan–Meier analyses were used to compare cardiovascular and total mortality, and Cox proportional univariable regression models were used to derive unadjusted hazard ratios (HRs). Multivariable step-wise Cox regression models were also run to adjust for known potential confounding baseline variables: age, sex, smoking status, presence of diabetes, cholesterol levels, systolic blood pressure, pulse pressure, ankle-brachial index, deprivation index, and aspirin or placebo allocation. The authors chose a priori to undertake analyses for IADs ≥5 mmHg, ≥10 mmHg, and ≥15 mmHg to maintain consistency with previous publications, and also explored fitting of IAD as a continuous variable in multivariable analysis. To assess the specific contribution of IAD, the likelihood ratio test was used to assess the reduction in goodness of fit arising on omission of the IAD term from each adjusted model in stepwise analyses. The prognostic performance of models that included the IAD was assessed by calculating the C-statistic. The C-statistic is a measure of concordance and quantifies how well a model predicts outcome, where a C-statistic of 0.5 indicates a predictive value no better than chance.19 The authors assessed proportionality of hazards over time by plotting −ln(−ln[survival]) versus ln(analysis time) and tested using Schoenfeld residuals.20,21 No major violations of the proportional hazards assumption were found.
As participants in the AAA trial were randomised to aspirin or placebo, the authors also fitted a Cox regression model with an IAD and intervention allocation interaction term. This interaction term allowed the exploration of whether there was a differing survival impact of IAD according to trial treatment allocation.
Results were expressed as HRs and 95% confidence intervals (CIs). Analysis was carried out using SPSS 20 and STATA (Release 12).
RESULTS
Characteristics of participants by IAD
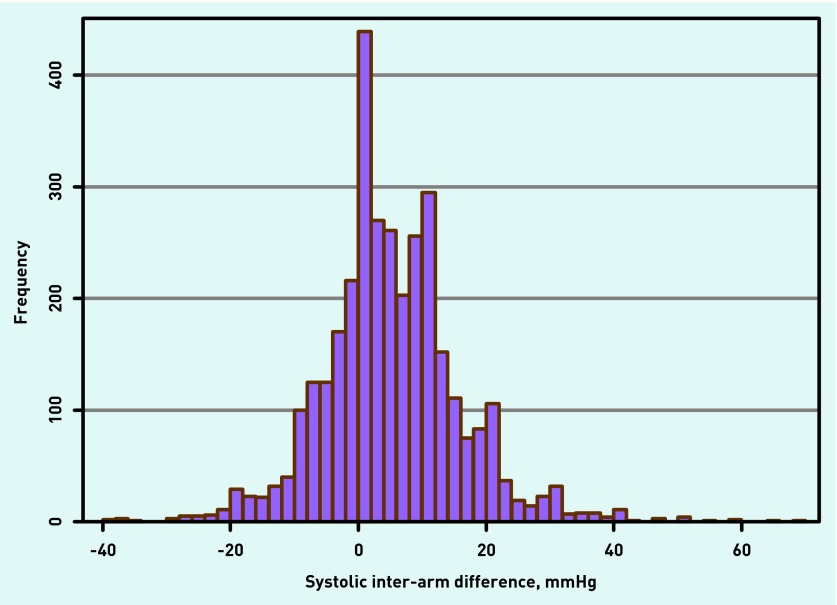
The study enrolled 3350 subjects, mean (SD) age was 61.9 years (6.6), and 2396 (71.5%) were female. Only three (0.1%) subjects had atrial fibrillation. Full baseline characteristics have been previously reported.16 A total of 2013 (60%) had systolic IADs ≥5 mmHg, 1280 (38%) ≥10 mmHg, and 553 (17%) ≥15 mmHg. Subjects with any IAD (≥5, ≥10, or ≥15 mmHg) had higher baseline blood pressures than those without an IAD. Ankle-brachial index was lower with IADs ≥10 or ≥15 mmHg than for those without (Table 1). Mean systolic blood pressure was 4.3 mmHg higher on the right (interquartile range −2 to 10 mmHg, Figure 1).
Table 1.
Baseline characteristics of 3350 subjects in cohort
| All cases (n= 3350) | IAD <5 mmHg (n= 1337) | IAD ≥5 mmHg (n= 2013) | P-value | IAD <10 mmHg (n= 2070) | IAD ≥10 mmHg (n= 1280) | P-value | IAD <15 mmHg (n= 2797) | IAD ≥15 mmHg (n= 553) | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | |||||||||||||
| Sex (% female) | 2396 (71.5) | 966 (72.3) | 1430 (71.0) | 0.47 | 1493 (72.1) | 903 (70.5) | 0.33 | 2013 (72.0) | 383 (69.3) | 0.20 | |||
| Age, years | 61.9 ± 6.6 | 62.3 ± 6.6 | 61.7 ± 6.7 | 0.021 | 62.1 ± 6.7 | 61.8 ± 6.6 | 0.18 | 62.0 ± 6.7 | 61.7 ± 6.6 | 0.39 | |||
| Systolic BP, mmHg | 147.9 ± 21.6 | 146.2 ± 20.9 | 149.0 ± 21.9 | <0.001 | 146.0 ± 20.5 | 150.9 ± 23.0 | <0.001 | 146.6 ± 20.9 | 154.4 ± 23.5 | <0.001 | |||
| Diastolic BP, mmHg | 83.7 ± 10.7 | 83.1 ± 10.4 | 84.1 ± 10.9 | 0.006 | 82.9 ± 10.2 | 84.9 ± 11.4 | <0.001 | 83.1 ± 10.4 | 86.6 ± 11.8 | <0.001 | |||
| ABI | 0.86 ± 0.09 | 0.86 ± 0.09 | 0.85 ± 0.09 | 0.15 | 0.86 ± 0.09 | 0.85 ± 0.09 | <0.001 | 0.86 ±0.09 | 0.84 ± 0.09 | <0.001 | |||
| IAD, mmHg | 4.3 ± 10.8 | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | |||
| Absolute IAD, mmHg | 8.5 ± 8.0 | ||||||||||||
| SIMD | 23.8 ± 17.7 | 24.1 ± 18.1 | 23.6 ± 17.3 | 0.47 | 23.7 ± 17.9 | 24.0 ± 17.3 | 0.68 | 23.8 ± 17.8 | 24.0 ± 16.7 | 0.84 | |||
| Total cholesterol, mmol/L | 6.2 ± 1.1 | 6.2 ± 1.1 | 6.2 ± 1.1 | 0.17 | 6.2 ± 1.1 | 6.2 ± 1.1 | 0.57 | 6.2 ± 1.1 | 6.1 ± 1.1 | 0.10 | |||
| Hypertension | 764 (22.8) | 316 (23.6) | 448 (22.3) | 0.35 | 465 (22.5) | 299 (23.4) | 0.55 | 620 (22.2) | 144 (26.0) | 0.05 | |||
| Diabetes | 88 (2.6) | 35 (2.6) | 53 (2.6) | 0.98 | 57 (2.8) | 31 (2.4) | 0.56 | 74 (2.6) | 14 (2.5) | 0.88 | |||
| Current smoker | 1085 (32.4) | 456 (34.1) | 629 (31.2) | } | 0.22 | 694 (33.5) | 391 (30.5) | } | 0.18 | 927 (33.1) | 158 (28.6) | } | 0.01 |
| Previous smoker | 1106 (33.0) | 429 (32.1) | 677 (33.6) | 678 (32.8) | 428 (33.4) | 931 (33.3) | 175 (31.6) | ||||||
| Never smoked | 1159 (34.6) | 452 (33.8) | 707 (35.1) | 698 (33.7) | 461 (36.0) | 939 (33.6) | 220 (39.8) | ||||||
Data shown as n (%), or mean ± standard deviation. P-values presented for t-tests (continuous variables) or Pearson χ2 tests (categorical variables). ABI = ankle-brachial pressure index. BP = blood pressure. IAD = inter-arm difference. N/A = not applicable. SIMD = Scottish index of multiple deprivation score.
Figure 1.
Distribution of brachial inter-arm pressures (right minus left).
Cross-sectional
All systolic IADs were associated with higher prevalences of peripheral arterial disease, whether defined as an ankle-brachial index <0.9 or ≤0.85 (Table 2), and IAD and ankle-brachial index were weakly negatively correlated as continuous variables (Pearson’s correlation coefficient (r) 0.08, P<0.001). IAD was positively correlated with pulse pressure with an incremental rise of 1.2 mmHg (95% CI = 0.9 to 1.5, r = 0.12, P <0.001) for each 20 mmHg increase in pulse pressure.
Table 2.
Prevalence of reduced ankle-brachial index with and without inter-arm difference
| IAD <5 mmHg (n= 1337) | IAD ≥5 mmHg (n= 2013) | P-value | IAD <10 mmHg (n= 2070) | IAD ≥10 mmHg (n= 1280) | P-value | IAD <15 mmHg (n= 2797) | IAD ≥15 mmHg (n= 553) | P-value | |
|---|---|---|---|---|---|---|---|---|---|
| ABI <0.9 n (%) | 822 (61.5) | 1359 (67.5) | <0.001 | 1275 (61.6) | 906 (70.8) | <0.001 | 1781 (63.7) | 400 (72.3) | <0.001 |
| ABI ≤0.85 n (%) | 408 (30.5) | 698 (34.7) | 0.012 | 633 (30.6) | 473 (37.0) | <0.001 | 881 (31.5) | 225 (40.7) | <0.001 |
P-values presented for Pearson χ2 tests. ABI =ankle-brachial pressure index. IAD =inter-arm difference.
Univariable survival analysis
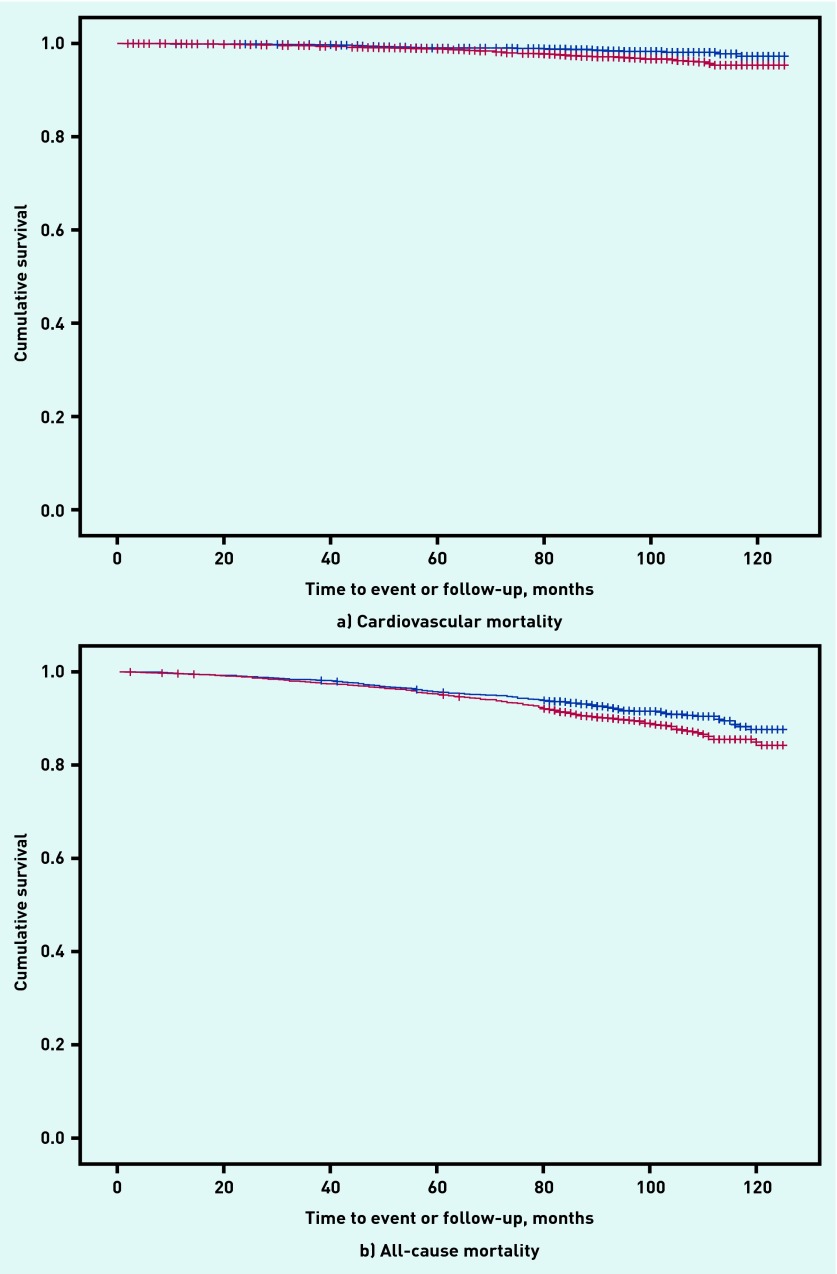
Mean follow-up was 8.2 years (1.6) and 10 (0.3%) subjects were lost to follow-up. There were 362 (10.8%) deaths from any cause, including 94 (2.8%) cardiovascular deaths. Compared with those without IADs, cardiovascular mortality was higher for IADs ≥5 mmHg (unadjusted HR 1.92, 95% CI = 1.21 to 3.05) and ≥10 mmHg (HR 1.62, 95% CI = 1.08 to 2.43), and all-cause mortality was higher with differences ≥5 mmHg (unadjusted HR 1.33, 95% CI = 1.07 to 1.66, Figure 2). No survival differences were seen with IADs ≥15 mmHg (Table 3).
Figure 2.
Kaplan–Meier survival curve for all cases with and without inter-arm difference ≥5 mmHg. Red lines = ≥5mmHg IAD, blue = <5mmHg IAD.
Table 3.
Cox proportional hazard ratios for inter-arm differences
| IAD (mmHg) | Number of events | Unadjusted HR (95% CI) | P-value | Adjusted HRa (95% CI) | P-value | P-value for change in goodness of fit if IAD term removed (LR) |
|---|---|---|---|---|---|---|
| All cases | ||||||
|
| ||||||
| All deaths | ||||||
| ≥5 | 120/1337 versus 242/2013 | 1.33 (1.07 to 1.66) | 0.011 | 1.44 (1.15 to 1.79) | 0.001 | 0.001 |
| ≥10 | 209/2070 versus 153/1280 | 1.14 (0.84 to 1.56) | 0.398 | 1.18 (0.95 to 1.46) | 0.130 | 0.131 |
| ≥15 | 299/2797 versus 63/553 | 1.02 (0.78 to 1.34) | 0.871 | 1.06 (0.80 to 1.40) | 0.675 | 0.676 |
|
| ||||||
| Cardiovascular deaths | ||||||
| ≥5 | 24/1337 versus 70/2013 | 1.92 (1.21 to 3.05) | 0.006 | 1.91 (1.19 to 3.07) | 0.008 | 0.005 |
| ≥10 | 46/2070 versus 48/1280 | 1.62 (1.08 to 2.43) | 0.019 | 1.49 (0.98 to 2.27) | 0.060 | 0.061 |
| ≥15 | 78/2797 versus 16/553 | 1.00 (0.58 to 1.71) | 0.987 | 0.87 (0.50 to 1.53) | 0.634 | 0.629 |
|
| ||||||
| Hypertensive cases | ||||||
|
| ||||||
| All deaths | ||||||
| ≥5 | 27/316 versus 59/448 | 1.54 (0.98 to 2.43) | 0.064 | 1.67 (1.05 to 2.66) | 0.031 | 0.026 |
| ≥10 | 42/465 versus 44/299 | 1.59 (1.04 to 2.43) | 0.031 | 1.63 (1.06 to 2.50) | 0.026 | 0.026 |
| ≥15 | 67/620 versus 19/144 | 1.18 (0.71 to 1.97) | 0.517 | 1.18 (0.70 to 1.99) | 0.541 | 0.546 |
|
| ||||||
| Cardiovascular deaths | ||||||
| ≥5 | 6/316 versus 20/448 | 2.34 (0.94 to 5.83) | 0.068 | 2.63 (0.97 to 7.02) | 0.053 | 0.036 |
| ≥10 | 9/465 versus 17/299 | 2.87 (1.28 to 6.44) | 0.011 | 2.96 (1.27 to 6.88) | 0.012 | 0.008 |
| ≥15 | 22/620 versus 4/144 | 0.76 (0.27 to 2.20) | 0.759 | 0.77 (0.26 to 2.26) | 0.633 | 0.623 |
Model adjusted for age, sex, Scottish index of multiple deprivation, smoking status, cholesterol, systolic blood pressure, pulse pressure, ankle-brachial index, presence of diabetes, and allocation to aspirin or placebo. HR = hazard ratio. IAD = inter-arm difference. LR = likelihood ratio.
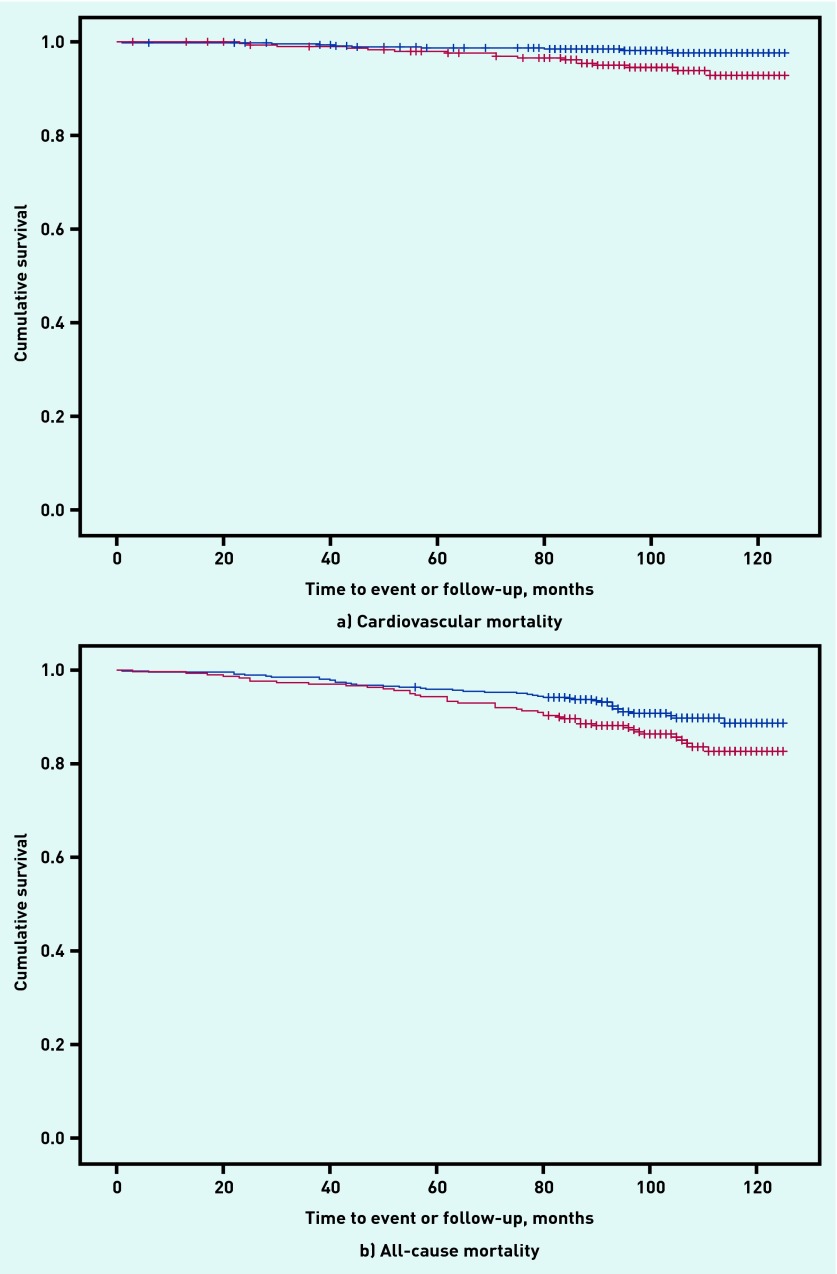
There were 764 (23%) subjects with hypertension. For this subgroup, IADs ≥10 mmHg were associated with increased cardiovascular mortality (unadjusted HR 2.87, 95% CI = 1.28 to 6.44) and increased all-cause mortality (unadjusted HR 1.59, 95% CI = 1.04 to 2.43) (Appendix 2). No survival differences were observed for non-cardiovascular deaths for ≥5 mmHg (HR 1.19, 95% CI = 0.93 to 1.53), for ≥10 mmHg (HR 1.02, 95% CI = 0.80 to 1.31), or for ≥15 mmHg (HR 1.05, 95% CI = 0.77 to 1.44).
Multivariable survival analysis
On regression as a continuous variable, IAD was not significant for mortality. As a discrete variable, an IAD ≥5 mmHg remained a predictor of increased cardiovascular and all-cause mortality (HR 1.91, 95% CI = 1.19 to 3.07, and HR 1.44, 95% CI = 1.15 to 1.79, respectively) in a fully adjusted model, but for an IAD ≥10 mmHg the adjusted HR lost significance for cardiovascular deaths (HR 1.49, 95% CI = 0.98 to 2.27, P = 0.06). Within the hypertensive subgroup after full adjustment, IADs ≥5 mmHg and ≥10 mmHg were associated with both cardiovascular (HR 2.63, 95% CI = 0.97 to 7.02, and HR 2.96, 95% CI = 1.27 to 6.88, respectively) and all-cause mortality (HR 1.67, 95% CI = 1.05 to 2.66, and HR 1.63, 95% CI = 1.06 to 2.50, respectively, Table 3). The regression model included terms for age, sex, smoking status, presence of diabetes, cholesterol levels, systolic blood pressure, pulse pressure, ankle-brachial index, Scottish index of multiple deprivation, and allocation to aspirin or placebo. Examination of likelihood ratios confirmed the significant contribution of IADs ≥5 mmHg and ≥10 mmHg to the multivariable models. There was a consistent loss of goodness of fit with exclusion of the IAD term from models. Cox regression prognostic models performed well, with C-statistic values consistently >0.70. Other significant terms in the models were age, sex, smoking status, pulse pressure, ankle-brachial index, presence of diabetes, and, for all-cause mortality only, deprivation index and systolic blood pressure. There was no evidence of an interaction (P>0.05) between the effect of IAD and death with allocation to trial treatments of aspirin or placebo.
DISCUSSION
Summary
This analysis, with 10 years of followup, has demonstrated that, in a cohort of subjects without clinical evidence of vascular disease at recruitment, an inter-arm systolic difference ≥5 mmHg based on a single pair of measurements, is associated with increased cardiovascular and all-cause mortality. For subjects with hypertension, differences ≥5 mmHg and ≥10 mmHg are associated with increased cardiovascular and all-cause mortality. IADs (≥5, ≥10, or ≥15 mmHg) are associated in cross-sectional analysis with higher prevalences of peripheral arterial disease, and magnitude of IAD is positively associated with pulse pressure.
Strengths and limitations
This study is comparable in size with other recent community-based cohort studies from the US reporting reduced survival with an IAD in blood pressure.8,9 Participants were recruited from primary care age-sex registers and are broadly representative of a general population. The statuses of subjects’ inter-arm blood pressure difference were unknown throughout follow-up, because differences were calculated specifically for this analysis using additional data transcribed from the original recruitment screening records. Consequently the authors are confident that, in IAD terms, any risk of bias in recording of events and deaths was avoided.
Atrial fibrillation was not prevalent in this study, and so does not account for the IADs observed here.3 The prevalence figures reported here for IADs are high in comparison with other large cohort studies,4,8,9 but are based on a single pair of sequential blood pressure measurements. Sequential rather than simultaneous measurements are associated with two- to threefold higher prevalences,11,22 and prevalence is over-estimated when measurements are not repeated,10,11,23 due at least in part to white-coat effects.23,24 Thus simultaneous, automated repeated measurements of IAD should be a reference standard for epidemiological study.10 However, the authors have found that a single sequential pair of measurements can exclude confirmed IAD with a high negative predictive value,11,12 and designed this study to investigate whether IADs detected by this simple method can also predict survival differences.
The method of measurement does not influence the strength of association between peripheral arterial disease and systolic IADs.1 On recent meta-analysis the authors observed a trend towards higher HRs for survival differences when using simultaneous IAD measurement methods compared with sequential methods, thus survival differences reported here may under-estimate the true figures for this cohort.25
This analysis was undertaken following publication of the AAA trial and was not specifically powered to assess a pre-defined difference in survival by IAD. However, the analyses were pre-specified and the large sample size suggests that the risk of a chance finding accounting for the results is small.
In order to identify a cohort free of clinically apparent pre-existing vascular disease but at higher than average community risk of events, an inclusion criterion for this cohort was an ankle-brachial index ≤0.95. Therefore the range of ankle-brachial index values was restricted, leading to a potential underestimate of the strength of correlation of ankle-brachial index with IAD.26,27
Because the AAA trial was not powered to formally assess the effects of aspirin compared with placebo in specific subgroups, the data analysis addressing the question of whether observed reductions in survival associated with IADs are moderated by aspirin treatment should be considered as exploratory.
Comparison with existing literature
Some previous reports have suggested a bias towards higher blood pressure readings on the right,28–35 whereas others have failed to demonstrate this.36–41 Studies looking specifically at left or right handedness have also failed to demonstrate an association with the higher-reading arm.33,42 In the current study, blood pressures were recorded in a fixed sequence for ankle-brachial index assessment,18 which may account for the bias towards higher right-arm blood pressures observed through order effects.
Current guidance suggests that an IAD <10 mmHg can be considered to be normal and that systolic differences ≥20 mmHg warrant specialist referral.14 Previous studies have proposed a ‘normal range’ for systolic or diastolic differences of up to 10 mmHg,39 and it has been argued that the high prevalence of differences above these cut-offs implies that this is a physiological rather than pathological finding.40,43 This study implies that a new threshold as low as ≥5 mmHg for a systolic IAD may be clinically important. Only this and the larger Vietnam experience study8 have shown that an IAD ≥5 mmHg is associated with a survival difference. Whether this new finding can be generalised to populations at higher levels of cardiovascular risk is unknown. However, HRs associated with IAD do increase with rising population cardiovascular risk.25
Peripheral arterial disease is recognised as a risk factor for future cardiovascular events and mortality,44 and the authors have previously proposed that an IAD in blood pressure is due to peripheral arterial disease.45 A systolic IAD ≥15 mmHg is associated with angiographic evidence of carotid or aortic arch disease in selected populations at high risk,46 and upper-limb vascular disease is associated with hypertension.47 Some authors have labelled an IAD ≥15 mmHg ‘subclavian stenosis’,7,48 but there is no direct radiological evidence from general populations, such as the cohort studied here, to confirm that this is the anatomical cause of an IAD.1 Structural changes in large arteries as a result of hypertension begin early in the course of the condition and cardiovascular and peripheral vascular disease are late sequelae of a process of gradual arterial stiffening.49 Recent cross-sectional studies have associated systolic IADs ≥10 mmHg with elevated ankle-brachial pulse wave velocity, an indicator of increasing vascular stiffness.50–52 Increased variability of blood pressure (a potential confounder of sequentially measured IAD) is also associated with increasing arterial stiffness,53,54 and this process also leads to increasing pulse pressures.55 Only non-significant associations of IAD and pulse pressure have previously been reported.50 This study found an association of rising pulse pressure with IAD. This adds to the evidence associating IADs, arterial stiffening, and increased mortality. Further work on these associations may provide a better explanation of the aetiology of IADs.
The survival findings presented here are consistent with those of other recent large community-based cohort studies,4,8 A recent meta-analysis only reported significant survival differences in community-dwelling cohorts for systolic IADs >15 mmHg.56 The current findings show no statistical heterogeneity when pooled with other similar published and unpublished studies4,8,57 and demonstrate survival differences in cardiovascular and all-cause mortality at both ≥5 mmHg and ≥10 mmHg IADs.25 In keeping with other cohorts, HRs for cardiovascular mortality are greater than those for all-cause mortality,25 because the contribution of IAD to all-cause mortality is explained, as shown by this data, by the inclusion of cardiovascular deaths within such analyses.
Associations of reducing ankle-brachial index with increased mortality demonstrate a ‘dose-response’ effect,44 whereas this was not clearly demonstrable for rising IADs in this study. The authors have previously reported failure to fit IAD as a continuous variable in other survival analyses.2 Some previous reports have demonstrated a clear gradient in HRs and magnitude of IADs,4,6,9,12,36 whereas others have not.5,8 There were relatively few events included in analyses at the higher cut-off of ≥15 mmHg difference. However, the full explanation within this cohort is unclear, and potential threshold effects need further study to fully account for the findings.
Implications for research and practice
The prevalence findings in this study support current clinical guidance to measure both arms in the initial assessment of patients for high blood pressure,14 and to confirm any IAD with simultaneous assessment.58 Currently this advice is not routinely followed,13,15,59–61 and therefore patients may be unknowingly under-investigated or under-treated for hypertension if an IAD is not looked for.62
The association of an IAD with peripheral arterial disease confirms the authors’ previous finding that IADs have a high specificity for prediction of reduced ankle-brachial index.1,27 This is not routinely assessed in primary care and requires time, equipment, and expertise.63,64 Diagnosis of peripheral arterial disease can however identify people who can benefit from interventions, and is a domain of the current Quality and Outcomes Framework in the UK. Therefore, identification of an IAD should trigger consideration of symptoms such as claudication, which may require further investigation.
Similarly, the association with reduced cardiovascular survival might suggest that aggressive vascular protection could be considered. This proposition has not been tested in a trial setting. However, these data add to the body of evidence identifying IADs as cross-sectional and prospective risk markers for cardiovascular and peripheral vascular disease.1,65 Blood pressure control is worse in people without established cardiovascular disease (those receiving primary prevention), compared with those with established disease (secondary prevention).66 Therefore, recognition of novel cardiovascular risk markers to refine risk prediction and stratify treatment priorities can be informative,67 and patients will benefit, because communication of excess cardiovascular risk is associated with improved patient adherence to healthy lifestyle changes.68
This study has shown that the association of IADs with reduced survival observed in populations at high cardiovascular risk can be extended to a population free of clinically evident cardiovascular disease. The authors are undertaking further work in cohorts representative of the general population to generalise these findings, determine the minimum clinically important threshold for an IAD, and understand the uncertainty around the presence or absence of a risk gradient with IAD.69 Studies to assess the implications of an IAD for further vascular screening and for therapeutic interventions are also needed, in tandem with work to examine the best pragmatic method for initially detecting an IAD in primary care. Finally, direct vascular imaging and assessment of unselected populations are required to clearly identify the aetiology of an IAD, and to provide evidence to support or refute any future suggested therapeutic intervention.
Acknowledgments
The authors acknowledge the support of The aspirin for asymptomatic atherosclerosis (AAA) trial executive committee. The additional bilateral blood pressure data were transcribed by Mrs C Martin and Mrs E Crooks.
Appendix 1. Definition of events included in the analyses
| Group | Description |
|---|---|
| Fatal coronary events | Definite fatal myocardial infarctiona |
| Definite death due to ischaemic heart diseasea | |
| Probable death due to ischaemic heart diseasea | |
|
| |
| Stroke | Definite fatal stroke due to infarctiona |
| Definite fatal stroke due to haemorrhage | |
| Definite fatal stroke, aetiology not known | |
| Probable fatal stroke | |
|
| |
| Cardiovascular mortality | Items above labelled a, as well as: |
| Cardiovascular death, other | |
|
| |
| All-cause mortality | All events listed above, as well as: |
| Death other causes | |
| Fatal gastrointestinal haemorrhage | |
| Fatal sub-arachnoid haemorrhage/subdural haematoma | |
Appendix 2.
Kaplan–Meier plots for hypertensive subjects with and without inter-arm difference ≥10 mmHg. Red lines = IAD >=10mmHg, blue = IAD <10mmHg.
Funding
Christopher E Clark is supported by a National Institute for Health Research (NIHR) clinical lectureship award. This work was funded jointly, as part of his PhD studies, by the NIHR Collaboration for Leadership in Applied Health Research and Care (CLAHRC) for the South West Peninsula at the Royal Devon and Exeter NHS Foundation Trust, and by a grant from the Scientific Foundation Board of the Royal College of General Practitioners (grant number SFB-2009–06). Rod S Taylor was supported by the NIHR CLAHRC for the South West Peninsula at the Royal Devon and Exeter NHS Foundation Trust. Angela C Shore is supported by the NIHR Exeter clinical research facility. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health in England. Data extraction for this study was funded by the South West General Practice Trust. The AAA trial was supported by the British Heart Foundation and the Chief Scientist’s Office of the Scottish Government.
Ethical approval
Ethical approval was granted by the UK National Health Service research ethics committees in Lanarkshire, Greater Glasgow, and Lothian health boards. All participants gave written informed consent.
Provenance
Freely submitted, externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Clark CE, Taylor RS, Shore AC, et al. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet. 2012;379(9819):905–914. doi: 10.1016/S0140-6736(11)61710-8. [DOI] [PubMed] [Google Scholar]
- 2.Clark CE, Taylor RS, Shore AC, Campbell JL. The difference in blood pressure readings between arms and survival: primary care cohort study. BMJ. 2012;344:e1327. doi: 10.1136/bmj.e1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim J, Song TJ, Song D, et al. Interarm blood pressure difference and mortality in patients with acute ischemic stroke. Neurology. 2013;80(16):1457–1464. doi: 10.1212/WNL.0b013e31828cf87c. [DOI] [PubMed] [Google Scholar]
- 4.Sheng CS, Liu M, Zeng WF, et al. Four-limb blood pressure as predictors of mortality in elderly Chinese. Hypertension. 2013;61(6):1155–1160. doi: 10.1161/HYPERTENSIONAHA.111.00969. [DOI] [PubMed] [Google Scholar]
- 5.Quiroga B, Galán I, García de Vinuesa S, et al. Interarm systolic blood pressure as a predictor of cardiovascular events in patients with chronic kidney disease. Nephrol Dial Transplant. 2015;30(5):801–806. doi: 10.1093/ndt/gfv059. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal R, Bunaye Z, Bekele DM. Prognostic significance of between-arm blood pressure differences. Hypertension. 2008;51(3):657–662. doi: 10.1161/HYPERTENSIONAHA.107.104943. [DOI] [PubMed] [Google Scholar]
- 7.Aboyans V, Criqui MH, McDermott MM, et al. The vital prognosis of subclavian stenosis. J Am Coll Cardiol. 2007;49(14):1540–1545. doi: 10.1016/j.jacc.2006.09.055. [DOI] [PubMed] [Google Scholar]
- 8.White J, Mortensen LH, Kivimaki M, et al. Interarm differences in systolic blood pressure and mortality among US army veterans: aetiological associations and risk prediction in the Vietnam experience study. Eur J Prev Cardiol. 2014;21(11):1394–1400. doi: 10.1177/2047487313496193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weinberg I, Gona P, O’Donnell CJ, et al. The systolic blood pressure difference between arms and cardiovascular disease in the Framingham heart study. Am J Med. 2014;127(3):209–215. doi: 10.1016/j.amjmed.2013.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clark CE, Campbell JL, Evans PH, Millward A. Prevalence and clinical implications of the inter-arm blood pressure difference: a systematic review. J Hum Hypertens. 2006;20(12):923–931. doi: 10.1038/sj.jhh.1002093. [DOI] [PubMed] [Google Scholar]
- 11.Verberk WJ, Kessels AGH, Thien T. Blood pressure measurement method and inter-arm differences, a meta-analysis. Am J Hypertens. 2011;24(11):1201–1208. doi: 10.1038/ajh.2011.125. [DOI] [PubMed] [Google Scholar]
- 12.Clark CE, Steele AM, Taylor RS, et al. Inter-arm blood pressure difference in people with diabetes: measurement and vascular and mortality implications: a cohort study. Diabetes Care. 2014;37(6):1613–1620. doi: 10.2337/dc13-1576. [DOI] [PubMed] [Google Scholar]
- 13.Heneghan C, Perera R, Mant D, Glasziou P. Hypertension guideline recommendations in general practice: awareness, agreement, adoption, and adherence. Br J Gen Pract. 2007 doi: 10.3399/096016407782604965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Institute for Health and Clinical Excellence . Hypertension: the clinical management of primary hypertension in adults. London: NICE; 2011. p. CG127. [Google Scholar]
- 15.Clark CE. Inter-arm blood pressure measurement needs to be practical and accurate. Am J Hypertens. 2011;24(11):1189–1190. doi: 10.1038/ajh.2011.139. [DOI] [PubMed] [Google Scholar]
- 16.Fowkes FG, Price JF, Stewart MCW, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA. 2010;303(9):841–848. doi: 10.1001/jama.2010.221. [DOI] [PubMed] [Google Scholar]
- 17.Price JF, Stewart MC, Deary IJ, et al. Low dose aspirin and cognitive function in middle aged to elderly adults: randomised controlled trial. BMJ. 2008;337:a1198. doi: 10.1136/bmj.a1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aboyans V, Criqui MH, Abraham P, et al. Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation. 2012;126(24):2890–2909. doi: 10.1161/CIR.0b013e318276fbcb. [DOI] [PubMed] [Google Scholar]
- 19.Cook NR, Ridker PM. Advances in measuring the effect of individual predictors of cardiovascular risk: the role of reclassification measures. Ann Intern Med. 2009;150(11):795–802. doi: 10.7326/0003-4819-150-11-200906020-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Collett D. Modelling survival data in medical research. 2nd edn. Boca Raton, FL: Chapman & Hall/CRC; 2003. [Google Scholar]
- 21.Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69(1):239–241. [Google Scholar]
- 22.Clark CE, Taylor RS, Shore AC, Campbell JL. The inter-arm difference in blood pressure: prevalence varies for different populations — a meta-analysis. J Hypertens. 2014;32(e-Suppl 1):e61. [Google Scholar]
- 23.Schwartz C, Koshiaris C, Clark C, et al. Does the right arm know what the left arm is doing? Ethnic variations in clinical inter-arm difference and relationship to white coat effects. J Hypertens. 2015;33(Suppl 1):e7. [Google Scholar]
- 24.Martin U, Holder R, Hodgkinson J, McManus R. Inter-arm blood pressure differences compared with ambulatory monitoring: a manifestation of the white-coat effect? Br J Gen Pract. 2013 doi: 10.3399/bjgp13X663055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clark C, Shore A, Taylor R, Campbell J. The inter-arm difference in blood pressure and mortality: systematic review and meta-analysis. J Hypertens. 2015;33(Suppl 1):e11. [Google Scholar]
- 26.Bland JM, Altman DG. Correlation in restricted ranges of data. BMJ. 2011;342:d556. doi: 10.1136/bmj.d556. [DOI] [PubMed] [Google Scholar]
- 27.Clark CE, Campbell JL, Powell RJ, Thompson JF. The inter-arm blood pressure difference and peripheral vascular disease: cross sectional study. Fam Pract. 2007;24(5):420–426. doi: 10.1093/fampra/cmm035. [DOI] [PubMed] [Google Scholar]
- 28.Amsterdam B, Amsterdam AL. Disparity in blood pressures in both arms in normals and hypertensives and its clinical significance. N Y State J Med. 1943;43:2294–2300. [Google Scholar]
- 29.Cassidy P, Jones K. A study of inter-arm blood pressure differences in primary care. J Hum Hypertens. 2001;15(8):519–522. doi: 10.1038/sj.jhh.1001224. [DOI] [PubMed] [Google Scholar]
- 30.Kay WE, Gardner KD. Comparative blood pressures in the two arms. Cal West Med. 1930;33:578–579. [PMC free article] [PubMed] [Google Scholar]
- 31.Korns HM, Guinand PH. Inequality of blood pressure in the brachial arteries, with especial reference to disease of the arch of the aorta. J Clin Invest. 1933;12(1):143–154. doi: 10.1172/JCI100485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’Shea JC, Murphy MB. Ambulatory blood pressure monitoring: which arm? J Hum Hypertens. 2000;14(4):227–230. doi: 10.1038/sj.jhh.1000998. [DOI] [PubMed] [Google Scholar]
- 33.Lane D, Beevers M, Barnes N, et al. Inter-arm differences in blood pressure: when are they clinically significant? J Hypertens. 2002;20(6):1089–1095. doi: 10.1097/00004872-200206000-00019. [DOI] [PubMed] [Google Scholar]
- 34.Rueger MJ. Blood pressure variations in the two arms. Ann Int Med. 1951;35(5):1023–1027. doi: 10.7326/0003-4819-35-5-1023. [DOI] [PubMed] [Google Scholar]
- 35.Southby R. Some clinical observations on blood pressure and their practical application, with special reference to variation of blood pressure readings in the two arms. Med J Aust. 1935;2(17):569–580. [Google Scholar]
- 36.Clark CE, Powell RJ. The differential blood pressure sign in general practice: prevalence and prognostic value. Fam Pract. 2002;19(5):439–441. doi: 10.1093/fampra/19.5.439. [DOI] [PubMed] [Google Scholar]
- 37.Frank SM, Norris EJ, Christopherson R, Beattie C. Right and left arm blood pressure discrepancies in vascular surgery patients. Anesthesiology. 1991;75(3):457–463. doi: 10.1097/00000542-199109000-00013. [DOI] [PubMed] [Google Scholar]
- 38.Kristensen BO, Kornerup HJ. Which arm to measure the blood pressure? Acta Med Scand. 1982;670(Suppl):69–73. doi: 10.1111/j.0954-6820.1982.tb09877.x. [DOI] [PubMed] [Google Scholar]
- 39.Orme S, Ralph SG, Birchall A, et al. The normal range for inter-arm differences in blood pressure. Age Ageing. 1999;28(6):537–542. doi: 10.1093/ageing/28.6.537. [DOI] [PubMed] [Google Scholar]
- 40.Pesola GR, Pesola HR, Lin M, et al. The normal difference in bilateral indirect blood pressure recordings in hypertensive individuals. Acad Emerg Med. 2002;9(4):342–345. doi: 10.1111/j.1553-2712.2002.tb01333.x. [DOI] [PubMed] [Google Scholar]
- 41.Singer AJ, Hollander JE. Blood pressure. Assessment of interarm differences. Arch Intern Med. 1996;156(17):2005–2008. doi: 10.1001/archinte.156.17.2005. [DOI] [PubMed] [Google Scholar]
- 42.Harrison EG, Roth GM, Hines EA. Bilateral indirect and direct arterial pressures. Circulation. 1960;22:419–436. doi: 10.1161/01.cir.22.3.419. [DOI] [PubMed] [Google Scholar]
- 43.Pesola GR, Pesola HR, Nelson MJ, Westfal RE. The normal difference in bilateral indirect blood pressure recordings in normotensive individuals. Am J Emerg Med. 2001;19(1):43–45. doi: 10.1053/ajem.2001.20021. [DOI] [PubMed] [Google Scholar]
- 44.Ankle Brachial Index Collaboraton Ankle brachial index combined with Framingham risk score to predict cardiovascular events and mortality: a meta-analysis. JAMA. 2008;300(2):197–208. doi: 10.1001/jama.300.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clark CE. Difference in blood pressure between arms might reflect peripheral vascular disease. BMJ. 2001;323(7309):399–400. doi: 10.1136/bmj.323.7309.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baribeau Y, Westbrook B, Charlesworth D, et al. Brachial gradient in cardiac surgical patients. Circulation. 2002;106(Suppl 1):I11–I13. [PubMed] [Google Scholar]
- 47.Sin Lau Y, Yeung J, Krishna Lingam M. Vascular disease of the upper limb. Modern Hypertension Management. 2005;5(1):9–12. [Google Scholar]
- 48.Shadman R, Criqui MH, Bundens WP, et al. Subclavian artery stenosis: prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol. 2004;44(3):618–623. doi: 10.1016/j.jacc.2004.04.044. [DOI] [PubMed] [Google Scholar]
- 49.Williams B. Hypertension in the young: Preventing the evolution of disease versus prevention of clinical events. J Am Coll Cardiol. 2007;50(9):840–842. doi: 10.1016/j.jacc.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 50.Canepa M, Milaneschi Y, Ameri P, et al. Relationship between inter-arm difference in systolic blood pressure and arterial stiffness in community-dwelling older adults. J Clin Hypertens (Greenwich) 2013;15(12):880–887. doi: 10.1111/jch.12178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Su HM, Lin TH, Hsu PC, et al. Association of interarm systolic blood pressure difference with atherosclerosis and left ventricular hypertrophy. PLoS One. 2012;7(8):e41173. doi: 10.1371/journal.pone.0041173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Clark CE, Casanova F, Gooding K, et al. Inter-arm blood pressure difference and arterial stiffness. J Hypertens. 2014;32(e-Suppl 1):e30. [Google Scholar]
- 53.Ichihara A, Kaneshiro Y, Takemitsu T, et al. Ambulatory blood pressure variability and brachial-ankle pulse wave velocity in untreated hypertensive patients. J Hum Hypertens. 2006;20(7):529–536. doi: 10.1038/sj.jhh.1002023. [DOI] [PubMed] [Google Scholar]
- 54.Garcia-Garcia Á, Garcia-Ortiz L, Recio-Rodriguez JI, et al. Relationship of 24-h blood pressure variability with vascular structure and function in hypertensive patients. Blood Press Monit. 2013;18(2):101–106. doi: 10.1097/MBP.0b013e32835ebc58. [DOI] [PubMed] [Google Scholar]
- 55.Safar ME. Systolic blood pressure, pulse pressure and arterial stiffness as cardiovascular risk factors. Curr Opin Nephrol Hypertens. 2001;10(2):257–261. doi: 10.1097/00041552-200103000-00015. [DOI] [PubMed] [Google Scholar]
- 56.Cao K, Xu J, Shangguan Q, et al. Association of an inter-arm systolic blood pressure difference with all-cause and cardiovascular mortality: an updated meta-analysis of cohort studies. Int J Cardiol. 2015;189:211–219. doi: 10.1016/j.ijcard.2015.04.079. [DOI] [PubMed] [Google Scholar]
- 57.Ferrucci L, Bandinelli S, Benvenuti E, et al. Subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the InCHIANTI study. J Am Geriatr Soc. 2000;48(12):1618–1625. doi: 10.1111/j.1532-5415.2000.tb03873.x. [DOI] [PubMed] [Google Scholar]
- 58.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2013;31(7):1281–1357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 59.Gosse P. Blood pressure should be measured in both arms on the first consultation [comment] J Hypertens. 2002;20(6):1045–1046. doi: 10.1097/00004872-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 60.Materson B. Inter-arm blood pressure differences. J Hypertens. 2004;22(12):2267–2268. doi: 10.1097/00004872-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 61.Clark CE, Smith LFP, Harding G, et al. Nurse led hypertension clinics: evolving ahead of the evidence? J Hum Hypertens. 2011;25((S1)(10)):S6. [Google Scholar]
- 62.Giles TD, Egan P. Inter-arm difference in blood pressure may have serious research and clinical implications. J Clin Hypertens. 2012;14(8):491–492. doi: 10.1111/j.1751-7176.2012.00668.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Campbell NC, McNiff C, Sheran J, et al. Targeted screening for peripheral arterial disease in general practice: a pilot study in a high-risk group. Br J Gen Pract. 2007;57(537):311–315. [PMC free article] [PubMed] [Google Scholar]
- 64.Ray SA, Srodon PD, Taylor RS, Dormandy JA. Reliability of ankle:brachial pressure index measurement by junior doctors. Br J Surg. 1994;81(2):188–190. doi: 10.1002/bjs.1800810208. [DOI] [PubMed] [Google Scholar]
- 65.Clark CE, Taylor RS, Shore AC, et al. Interarm blood pressure difference and vascular disease — Authors’ reply. Lancet. 2012;380(9836):24–25. doi: 10.1016/S0140-6736(12)61117-9. [DOI] [PubMed] [Google Scholar]
- 66.Falaschetti E, Mindell J, Knott C, Poulter N. Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet. 2014;383(9932):1912–1919. doi: 10.1016/S0140-6736(14)60688-7. [DOI] [PubMed] [Google Scholar]
- 67.Simon A, Levenson J. May subclinical arterial disease help to better detect and treat high-risk asymptomatic individuals? J Hypertens. 2005;23(11):1939–1945. doi: 10.1097/01.hjh.0000184407.20257.58. [DOI] [PubMed] [Google Scholar]
- 68.Shaw C, Abrams K, Marteau TM. Psychological impact of predicting individuals’ risks of illness: a systematic review. Soc Sci Med. 1999;49(12):1571–1598. doi: 10.1016/s0277-9536(99)00244-0. [DOI] [PubMed] [Google Scholar]
- 69.Clark C, Campbell J, Boddy K, et al. Inter-arm blood pressure difference, cardiovascular events, cerebrovascular disease and mortality: an individual patient data meta-analysis. PROSPERO. 2015. CRD42015031227. http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015031227 (accessed 14 Mar 2016).