Abstract
Although the validity of adult ADHD is well established and research has identified a variety of impairments associated with the condition in adults, study of how ADHD impacts an adult’s ability to parent has been relatively neglected. Parenting is a particularly important domain of functioning given the familial nature of the disorder and emerging evidence that parenting behaviors play a role in the development or maintenance of child ADHD symptoms, comorbid psychopathologies, and other associated difficulties. In this paper, we focus on three broad categories of cognitive dysfunction proposed across models of ADHD — cognitive processes (e.g., working memory, planning, and inhibitory control), self-regulation deficits (e.g., self-monitoring of performance to detect errors or the need for regulation of behavior and/or emotions), and motivational or arousal difficulties (e.g., response to incentives, delay aversion). We consider how these deficits may lead to impairments in the parenting behaviors of effective behavioral control and emotional responsiveness, and review the available evidence regarding parenting in adults with ADHD symptoms. We conclude by noting the limitations in existing studies, and argue for further research that is theoretically grounded in how core deficits of ADHD may be related to dimensions of parenting. The implications of an improved understanding of how ADHD impacts parenting for the development of early intervention or prevention programs are outlined.
Keywords: ADHD, Parenting, Cognitive processing, Parent, child interactions, Maternal psychopathology, Family relationships
1. Introduction
At an accelerating pace over the past two decades, ADHD has been recognized as not restricted to childhood, but a disorder which appears across the lifespan (Kessler et al., 2006). With the increasing recognition of ADHD among adults has come research focused on aspects of the adult disorder such as its correspondence to the childhood form, common comorbidities, and the efficacy of interventions. Central to understanding the nature of ADHD in adults is the extent to which the disorder interferes with or impairs functioning. It is well documented that ADHD symptoms in adults are associated with significant impairment across domains such as academic achievement, occupational history and attainment, and interpersonal relationships (Barkley, Murphy, & Fischer, 2008; Johnston, 2002; Mannuzza et al., 2011). However, only a few studies have examined the impact of ADHD symptoms on parenting. Confirming the importance of this domain of functioning, Barkley (2011b) found that, in a representative sample of adults, meeting diagnostic criteria for ADHD was associated with reports of greater child-rearing impairment. In this paper we argue that parenting is a critical domain of functioning that must be considered in adults with ADHD.
Research on how adult ADHD influences the caregiving environment is essential in order to fully understand the developmental trajectories that lead to ADHD or comorbid disorders, or to the avoidance of such outcomes, among the offspring of adults with ADHD. Given the highly heritable nature of ADHD (Faraone & Biederman, 2005), the co-occurrence of ADHD in child and parent is relatively common. Well over half of adults with ADHD have at least one child with the disorder (Biederman, Faraone, Mick, & Spencer, 1995; Kessler et al., 2006; Minde et al., 2003) and approximately 25–50% of children with ADHD have a parent with the disorder (Biederman et al., 1995; Chronis et al., 2003). Indeed, it is probable that the existing literature describing difficulties in families of children with ADHD reflects, to some extent, the presence of ADHD in the parents as well as in the children (Johnston & Lee-Flynn, 2011a).
To the extent that ADHD symptoms impair parenting, these parenting deficits will have ripple effects that may moderate the genetic risks for children in these families. The parenting difficulties that adults with ADHD face may be amplified by the strong likelihood of difficult child temperament and/or vulnerability to environmental risks in their offspring. Furthermore, the effects of parenting difficulties attributable to ADHD are not circumscribed to child ADHD (Humphreys, Mehta, & Lee, 2010) and may also open developmental pathways to comorbid conditions such as oppositional and conduct problems (Barkley, 2010; Beauchaine, Hinshaw, & Pang, 2010). From a developmental psychopathology perspective, ADHD in the parent contributes critical variance in determining trajectories of child development as the ADHD-linked parenting difficulties are reciprocally related to child vulnerabilities and each drives dynamic changes in the other over time. Although it is likely that parent ADHD and child characteristics often interact in a manner that impedes optimal child development (e.g., parents who lack self-regulation skills are less able to support and scaffold the development of such skills in their young children), there may also be pathways through which parent ADHD serves to attenuate or buffer the development of child problems (e.g., parents with ADHD are more in synchrony with a child’s preference for fast-paced activities). From this standpoint, knowledge of the mechanisms and variations that underlie how parent ADHD and child vulnerabilities interact across development is critical to informing early and lasting interventions for ADHD. Even existing evidence-based treatments for childhood ADHD place heavy responsibilities on the parent for treatment administration (Hoza, Johnston, Pillow, & Ascough, 2006) and parental ADHD impedes the effective delivery of such treatments (Chronis-Tuscano et al., 2011; Sonuga-Barke, Daley, & Thompson, 2002). Parental ADHD may play an even more important role in early interventions which focus on the parenting environment as a modifier of child genetic risk.
Despite the crucial ways in which ADHD symptoms in parents may impact both adult and child functioning, our understanding of parenting in adults with ADHD is underdeveloped. It could be argued that we know more about how ADHD symptoms influence adults’ performance on neuropsychological, personality, or driving tests than we know about how ADHD impacts the ability of adults to appropriately care for and cope with the challenges of parenting their high risk offspring. This lack of research into adult ADHD and parenting is likely the result of several factors, including the relatively recent recognition of the adult diagnosis of ADHD, a heavy emphasis on genetic rather than environmental factors in relation to ADHD, and a desire to avoid blaming parents for child ADHD problems. In this paper, we argue that the slow development of research focused on ADHD and parenting may also be attributed to the lack of a theoretical or conceptual framework to guide such work. Specifically, there is a need to ground studies of parenting impairment in adults with ADHD in what we know about the core dysfunctions of ADHD and how these may impact core aspects of parenting. The goal of this paper is to consider a framework that integrates proposed core deficits of ADHD with key dimensions of parenting. We then review studies of parenting and ADHD symptoms from the lens of this framework. Finally, we summarize directions and challenges for future research in this area.
2. Adults with ADHD
Despite continuing controversy and uncertainty regarding the most appropriate diagnostic criteria for adult ADHD (Barkley et al., 2008), it is recognized that the disorder persists into adulthood in 50 to 80% of individuals with childhood ADHD (Barkley, Fischer, Smallish, & Fletcher, 2006; Faraone, Biederman, & Mick, 2006) and epidemiological studies estimate that approximately 4% of adults have ADHD (Faraone & Biederman, 2005; Kessler et al., 2006). Given the strong possibility that current diagnostic criteria are not entirely appropriate when applied to adults, this may be an underestimate of the true prevalence (Mick, Faraone, Biederman, & Spencer, 2004; Pinkhardt et al., 2009). In contrast to the higher prevalence among male children, in adulthood, prevalence appears similar in males and females (Faraone & Biederman, 2005; Kessler et al., 2006). As in childhood, ADHD in adults is characterized by excessive inattention and hyperactivity/impulsivity, although symptom presentation is believed to differ in developmentally appropriate ways in adults (e.g., hyperactivity may be experienced more as restlessness) (McGough & Barkley, 2004). Although ADHD is subtyped in both children and adults, the fluid and indeterminant nature of these subtype classifications is widely recognized (Nigg, Tannock, & Rohde, 2010). In line with emerging evidence in several areas of psychopathology (Helzer, Kraemer, & Krueger, 2006), adult ADHD symptoms may best be conceptualized in a dimensional fashion (Marcus & Barry, 2010), with a recognition that impairment is associated with elevations in symptom levels whether or not an arbitrary diagnostic threshold is exceeded (Mannuzza et al., 2011). In addition, ADHD is highly comorbid with a range of other adult psychopathologies some of which may reflect disturbances in the same brain systems (Miller, Nigg, & Faraone, 2007). However, consistent with a view of ADHD as a neurodevelopmental disorder, it appears to have an earlier onset than many of its adult comorbidities, and these comorbidities, such as depression or substance use disorders, may be partly due to the effects of ADHD symptoms (Fayyad et al., 2007). Despite evidence of the efficacy of both medications and psychological treatments for adult ADHD (Faraone, Spencer, Aleardi, Pagano, & Beiderman, 2004; Solanto et al., 2010), surveys suggest that a substantial number of adults are untreated for their ADHD and are more likely to enter mental health services because of comorbid problems (Fayyad et al., 2007; Kessler et al., 2006). In sum, ADHD in adults is relatively prevalent, impairing, and often untreated.
3. Core dysfunctions in ADHD and implications for parenting
In considering how ADHD may affect an adult’s ability to function as a caregiver to a child, we conceptualize parenting behavior as composed of two inter-related dimensions — effective behavioral control and emotional responsiveness to the child (Darling & Steinberg, 1993; Rothbaum & Weisz, 1994). The control dimension includes both proactive and reactive parenting behaviors designed to direct or protect the child. Behaviors such as parental monitoring or supervision of the child’s behavior, the use of clear directions and guidance, planning or problemsolving around child-rearing difficulties, and the use of judicious and consistent consequences would all fall within the rubric of parental control behaviors. On the effective control dimension, difficulties would emerge when parenting behaviors are characterized by either insufficient levels of behavior control (e.g., “timid,” lax, permissive or inconsistent parenting), or by the other extreme of harsh, over-reactive, or over-controlling parenting behaviors. Emotional responsiveness focuses on parenting that conveys warmth in interactions with the child, demonstrates sensitivity to the child’s emotional state and needs, and expresses affection, approval, acceptance or other positive behaviors toward the child. On the emotional responsiveness dimension, parenting impairment is most typically seen as low levels of emotional responsiveness, including insensitivity to the child’s needs or a cold, hostile, or rejecting stance toward the child, although difficulties may also emerge when parents are overly involved or enmeshed with their children. Supporting the view that both effective behavioral control and emotional responsiveness are important aspects of parenting, deviations from optimum parenting on each dimension are associated with increased child problems (Collins, Maccoby, Steinberg, Hetherington, & Bornstein, 2003; Kendziora & O’Leary, 1993). For the purpose of this paper, these broad categories allow consideration of parenting across a wide range of child ages. However, it is important to acknowledge that these broad categorizations obscure more fine-tuned variations in parenting that are particularly important at different points in a child’s development (e.g., the parent’s ability to read facial and motor cues in a young infant or parental tolerance of an adolescent’s emerging quest for autonomy). Further, although a full discussion of these factors is beyond the scope of this paper, it must also be remembered that parenting behaviors occur within the broader context of multiple family relationships, as well as social, cultural, and economic influences.
As described above, within a developmental psychopathology framework, reciprocal and transactional relations are proposed between impairments in effective parenting behavioral control or emotional responsiveness and child maladjustment (including not only ADHD symptoms but also closely related conditions such as oppositional defiant and conduct disorder) (Johnston & Mash, 2001; Sonuga-Barke & Halperin, 2010). The links between child characteristics and effective parenting control or emotional responsiveness will reflect not only shared genetic liabilities, but also influences from the environments that both parent and child ADHD symptoms serve to create within the family. Importantly, parent and child characteristics, at both the genetic and phenotypic or behavioral level, also are expected to interact and exert influences that emerge and desist over time. For example, it is possible that during infancy ADHD driven parental insensitivity may serve to influence the child’s developing brain architecture in a manner consistent with delays in the development of circuitry underlying inhibitory control or regulation of arousal that have been identified in recent neuroimaging studies (Shaw et al., 2007). Later in life, the child’s unpredictable or impulsive behaviors may serve to exacerbate the difficulties that a parent with ADHD has in striving to control or monitor the child’s whereabouts or deviant friendships. Thus, as briefly outlined, there are many opportunities for parental ADHD to impact a child’s life. We now turn to the core deficits of ADHD to explore how these may present in parenting behaviors.
Multiple different dysfunctions have been proposed as central to ADHD including deficits in inhibitory control, reinforcement sensitivity, interference control, working memory, motor output regulation, vigilance, sustained attention, and emotional liability to name a few. A comprehensive review of these deficits is beyond the scope of this paper and the reader is referred to excellent reviews by Barkley (2011a), Nigg (2010), or Willcutt and Bidwell (2011). We instead focus on broad categories of dysfunction that have been proposed across numerous models. In outlining these general categories of dysfunction, we recognize the definitional conundrums that have plagued these concepts and the need for more precise distinctions and definitions to describe the processes underlying ADHD. We begin with a brief synopsis of dysfunctions in cognitive processes, motivational/emotional responses, and self-regulation associated with ADHD, and then consider how these may serve as heuristics to organize and guide thinking about how ADHD impacts functioning in the parenting domain. Given the heterogeneity that exists within ADHD and the likelihood that multiple pathways or dysfunctions underlie the disorder across individuals (Miller, Nigg, & Miller, 2009; Nigg, 2010), it is assumed that different dysfunctions may be operational in different individuals and/or may combine in different ways across adults with ADHD to impact parenting.
We consider deficits in what have been labeled as “cool” cognitive or executive processes, including working memory, planning, and inhibitory control (Rubia, 2010); deficits in “hot” cognitive processes or those involved in motivation, response to incentives and emotional regulation (Zelazo, Qu, Kesek, Calkins, & Bell, 2010); and a broader category related to difficulties with self-regulation (Shiels & Hawk, 2010) which seems to bridge the hot and cool categorization and reflects a combination of cognitive and emotional control and regulation. For each category of deficit, we offer a brief description of how the process may serve to guide parenting, and then consider how a deficit in this process may result in impaired parenting control and/or emotional responsiveness.
3.1. Deficits in working memory, planning, and inhibitory control
We first address “cool” cognitive or executive dysfunctions in relation to ADHD and parenting. Across multiple studies, individuals with ADHD have been shown to have difficulties with working memory, particularly verbal memory, and these difficulties are central to several models of ADHD (Castellanos, Sonuga-Barke, Milham, & Tannock, 2006; Rapport et al., 2008). Working memory is defined as the ability to actively hold information in awareness and to manipulate this information in order to guide one’s actions. It would be central to tasks such as following a recipe, remembering a phone number while dialing, or calculating a tip on a restaurant bill. Working memory would also be fundamental to (if not synonymous with) executive functions such as planning, where working memory allows the individual to hold information regarding past performance in mind as needed to adjust future performance. A second cognitive process that has been central to many models of ADHD is effortful control or inhibition, which allows for withholding or interrupting ongoing or prepotent responses in accordance with internal or external stimuli. Inhibitory control includes the ability to control interference from competing responses (Barkley, 1997; Willcutt, Doyle, Nigg, Faraone, & Pennington, 2005). These cognitive processes are seen to underlie the ability to maintain a focus on task goals without interference and to inhibit or change responding as demanded. In daily adaptive functioning, these executive capacities may be involved in time management, self-organization and problem-solving, and self-restraint (Barkley & Murphy, 2011). At a behavioral level, inhibitory control would be required in tasks such as the effortful attending to a lecture, or releasing the gas pedal when an amber light appears.
Cognitive abilities such as working memory, planning, and inhibitory control and their extension into daily adaptive functioning (time management, organization, restraint) seem necessary to support both appropriate parenting control and emotional responsiveness. For example, from an attachment perspective, Barrett and Fleming (2011) argue that parenting appropriately “requires the action of multiple systems in the domains of sensation, perception, affect, reward, executive function, motor output and learning.” (p. 369). They discuss the role of working memory in allowing parents to plan parenting actions, based on input from the child, the context, and previous experiences and cite recent work showing associations between parenting sensitivity (defined as including both appropriate control and emotional responsiveness) and mothers’ performance on cognitive measures such as attentional set-shifting, spatial working memory and sustained attention. With implications for inter-generational transmission of ADHD parenting effects, they also note that early environmental adversities (as may be inherent in the parenting provided by adults with ADHD) impacts the future adult parenting of offspring, mediated through effects on both cognitive processing and the HPA axis. Although studies have shown that appropriate parenting control behaviors and emotional responsiveness skills are diminished among parents of children with ADHD and/or oppositional behaviors (Deault, 2010; Healey, Gopin, Grossman, Campbell, & Halperin, 2010; Seipp & Johnston, 2005), few have specifically examined parents with ADHD symptoms. ADHD-related difficulties with working memory, planning, or inhibition of ongoing behavior may underlie inadequate parenting control behaviors such as inconsistency or over-reactivity in discipline, or problems in prioritizing and organizing parenting tasks, particularly in an ongoing fashion (e.g., switching from playtime with the child to helping the child prepare for bedtime). In another example, a parent who has difficulty holding time limits in mind or in withholding strong, ongoing responses may be a parent who is unable to stop playing an internet game in order to respond to a child’s potentially dangerous play near a stove.
3.2. Deficits in self-regulation
Other models of ADHD have placed an emphasis on self-regulation deficits (Shiels & Hawk, 2010), arguing that problems with self-monitoring of performance and with the processing of errors lead to a lack of adaptive control over behavior. Although such self-regulation deficits would incorporate many of the cognitive processing deficits discussed above, such as inhibitory control, these models take a more over-arching perspective and focus on multiple processes that ultimately culminate in appropriate or insufficient self-regulation. Self-regulation deficits reflect impairments in the “on line” processing of information and are seen to underlie difficulties in the regulation of arousal or emotions, as well as behavior. Translated into the parenting context, self-regulation skills have implications for the parent’s ability to show optimal parenting along both dimensions of parenting control and emotional responsiveness. From monitoring whether parenting control is needed to keep a toddler safe from danger during a walk along a busy street, to the parent recognizing their own mounting annoyance with a child’s repeated interruptions and using this as a cue to engage in emotion modulation, parenting can be framed as an exercise in self-regulation (Sanders, 2008). Such deficits may have an impact beyond the effects evident in observed parent–child interactions. For example, the inattentiveness associated with adult ADHD and the reduced self-monitoring characteristic of ADHD may lead to reduced parental monitoring of child activities. Such poor parental monitoring is a significant predictor of both childhood accidental injuries (Schwebel, Hodgens, & Sterling, 2006) and more generally of externalizing behavior and deviant peer affiliations (Barkley, Fischer, Smallish, & Fletcher, 2004; Jokela, Power, & Kivimäki, 2009; Thapar, van den Bree, Fowler, Langley, & Whittinger, 2006).
Thus, self-regulation deficits that lead to failures to adequately or accurately monitor one’s own behavior in the context of child cues are likely to preclude a parent detecting when their parenting actions fail to meet the child’s needs. Without the detection of such “parenting errors” the parent will be unable to regulate parenting actions in a way that might, for example, increase supportive control in the face of a child’s failure at a task or increase empathy in response to the child’s frustration with the task. In addition, to the extent that a parent is deficient in self-regulation, the likelihood of being able to interact with the developing child in a manner which promotes the child’s acquisition and use of these same critical self-regulation skills is diminished.
Linking working memory and self-regulation to parenting, a recent study by Deater-Deckard, Sewell, Petrill, and Thompson (2010) proposed that working memory is critical in allowing parents to exert cognitive control or self-regulation of emotion, and in promoting optimal responses to challenging child behavior. Working memory allows for continual reappraisal of the effects of parenting actions, for reflection on the ongoing stream of information from the child, and for using this information to guide parenting actions. When working memory is impaired, it was argued that parenting is more likely to be poorly regulated and more reactive to the behavior of the child. This is particularly the case for negative, challenging, or unpredictable child behaviors which elicit emotions that may further hinder rational and purposeful parental cognitive processing. In the Deater–Deckard study, mothers’ working memory skills were used to predict negative parenting. Consistent with the prediction that working memory deficits reduce a mother’s self-regulation of parenting behavior, results indicated that mothers with poor working memory were more reactive to child misbehavior than mothers without such working memory deficits, who were presumably able to exert greater cognitive control and to thereby modulate their responses consistent with parenting goals, rather than having reactions driven by the child’s immediate behavior. The framework proposed by Deater–Deckard is consistent with Barkley’s recent proposal of the centrality of emotional impulsiveness in ADHD and findings that the majority of adults with ADHD report significant problems with emotional self-regulation in daily life activities, as do the majority of children with ADHD in young adulthood (Barkley & Fischer, 2010). The impatience, low tolerance, and hot temper proposed as characteristic of emotional impulsiveness or poor emotional self-regulation would seem to translate readily into harsh emotional reactions to child misbehavior and higher rates of overall parenting stress (Barkley et al., 2008).
3.3. Deficits in motivation and incentive-based responding
A final category of deficit found across several models of ADHD is focused on motivational systems or reinforcement processes that may underlie the symptoms, including aversion to delay in rewards, altered sensitivity to rewards, or deficits in the extinction of reinforced behavior (Sagvolden, Aase, Johansen, & Russell, 2005; Sonuga-Barke, 2003). This set of deficits would be included in those described as “hot” functions (e.g., Zelazo et al., 2010). These models reflect findings that individuals with ADHD benefit from high-intensity reinforcements and their performance consistently suffers under conditions of partial or delayed reinforcement (Luman, Oosterlaan, & Sergeant, 2005). In addition, these motivational impairments may account for poor persistence of effort among individuals with ADHD, particularly in situations of low reinforcement value (e.g., boring, repetitive tasks). It is likely that these deficits in “hot” executive functions translate into difficulties during daily adaptive functioning in the self-regulation of emotion and self-motivation (Barkley & Murphy, 2011).
As with the cognitive processing skills discussed above, motivational functioning also appears as a necessary prerequisite to optimal parenting control and emotional responsiveness. For example, focusing on mothering of infants, Barrett and Fleming (2011) have outlined how infant cues must be attractive and salient in order to allow the mother to attend to the infant within the context of multiple competing stimuli, and they suggest that dopaminergic reward circuitry may play a critical role in this aspect of mothering. The ability to tolerate delays or to maintain effort in the face of sparse reinforcement can easily be linked to parenting skills such as being patient as a developing child masters a task or persisting through failures in toilet training.
Speculating on how deficits in reward sensitivity or intolerance of delay might be evidenced in the parenting domain, parents with such motivational difficulties may experience reduced sensitivity to positive feedback from the child, setting the stage for diminished warmth or emotional responsiveness in interactions with the child. For example, one can imagine how a parent with ADHD may be less likely to engage their young child in age-appropriate play (e.g., peek a boo with infant), because of the repetitive and boring nature of the play. Thus, the rewarding aspects of childrearing that serve to motivate perseverance in the face of the challenges (e.g., just think of the parent who must wait for a child who is learning to manipulate buttons to finish dressing before the parent can proceed with his/her own travel plans), may hold less incentive value in guiding parenting efforts in adults with ADHD. Expanding on the delay aversion aspects of these models, it is proposed that some individuals with ADHD find waiting inordinately aversive, resulting in the selection of smaller, immediate rewards. Considering the behavioral control aspects of parenting, it is easy to imagine that adults who are particularly averse to delays would be prone to inconsistent or permissive parenting given the patience required to effectively monitor child performance and administer consistent consequences. As an interesting caveat to this negative effect on parenting, in situations in which both the parent and child have ADHD symptoms, it remains a possibility that such parents are, in some ways, better “in tune” with children who have the same motivational difficulties and may be better able to pace parenting behaviors so as to avoid delays for the child.
3.4. Conclusion
In concluding this section, we reiterate the incomplete and arbitrary nature of our categorization of the core dysfunctions in ADHD. Numerous distinctions exist among the constructs that we have lumped together, and there are multiple other categories we might have created. One deficit that may be particularly relevant in the context of parenting is the variability in responding that Castellanos et al. (2006) have highlighted as a core characteristic of ADHD. Specifically, increased response variability in the parenting domain may be reflected in inconsistencies in both parenting control and emotional responsiveness (e.g., vacillation between punishing or ignoring misbehavior, sporadic “tuning out” of child directed attempts at interactions). The suggestion of difficulties with variability in a parents’ responding across time highlights the need for more dynamic measures of parenting in studies in this area. Multiple and repeated assessments of parenting will be necessary in order to reveal potential increased variability over time or across parenting situations associated with ADHD.
In another example, personality traits are increasingly explored as a possible pathway to the emergence of ADHD symptoms (Martel, 2009) and may be relevant to functioning in the parenting domain. Weinstein, Apfel, and Weinstein (1998) found that mothers with ADHD reported significantly higher levels of neuroticism and less conscientiousness and agreeableness than mothers without ADHD, with no differences on the dimensions of extroversion and openness. Such personality differences may emerge as difficulties on parenting tasks requiring regulation of anger in response to child misbehavior (e.g., neuroticism), organization (e.g., conscientiousness) or cooperation with the coparent (e.g., agreeableness). By extension, the lack of differences on traits of extroversion and openness may suggest parenting situations that are areas of relative strength for parents with ADHD (e.g., a willingness to try new adventures with the child, spontaneity or strong positive emotions in interactions with the child).
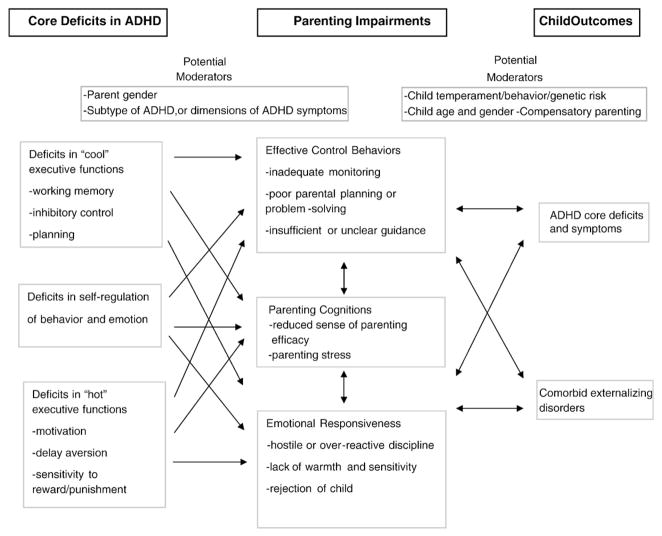
Fig. 1 presents a schematic of how the core deficits of ADHD may affect parenting control and emotional responsiveness, and suggest possible moderators of the links between ADHD deficits and parenting, as well as between parenting and child outcomes. As suggested by authors such as Safren, Sprich, Chulvick, and Otto (2004) and Kessler et al. (2010), the core problems of ADHD (e.g., difficulties with inhibition, working memory, self-regulation and motivation) lead to problem behaviors such as failures to organize, prioritize, or plan; procrastination; or emotional impulsivity. In the parenting domain, these problems manifest in impairments of parenting control such as a lack of planned or organized household routines, failures to monitor or appreciate a child’s needs, or in emotionally impulsive and negative responses to the child. Collectively, these suboptimal approaches to parenting interact with and are linked to negative child outcomes. In addition to direct negative effects on parenting actions, ADHD deficits may also disrupt the adult’s development as a parent and his/her acquisition of adaptive parenting behaviors. It is expected that parenting impairments will be accompanied by negative feedback about parenting and relationship problems both with the child and with others such as the coparent. Ultimately, this persistent negative feedback about parenting promotes the development of dysfunctional cognitions such as a reduced sense of parenting efficacy, demoralization in the parenting role, and culminates in decreased motivation for parenting and perhaps mood disturbances such as depression or anger. This is consistent with findings of higher rates of self-rated parenting stress and lower parenting self-efficacy in parents with ADHD than in clinical control groups or general population samples (Barkley et al., 2008; Sonuga-Barke et al., 2002) In addition, ADHD symptoms may be associated with problems in parenting confidence independent of child problems. For example, Ninowski, Mash, and Benzies (2007) found that even among first-time expectant mothers, ADHD symptoms predicted less positive expectations regarding the infant and the mothering role, and lower parenting self-efficacy. Similarly, among community mothers of 3 to 6 year old children, mothers with more ADHD symptoms reported lower parenting sense of competence, even though their children did not have more ADHD or oppositional behavior (Banks, Ninowski, Mash, & Semple, 2008).
Fig. 1.
Impairments and child outcomes.
In summary, lines can be drawn from core problems such as deficits in working memory, inhibitory control, self-regulation, motivation, and variability in responding to inadequacies in both parental control and emotional responsiveness, as well as to disturbances in parenting cognitions. In the following sections, we consider the evidence regarding impairments in parenting related to adult ADHD and the extent to which these are consistent with expectations based on the core deficits.
4. Parenting in adults with ADHD
Clinical observations in families where both parents and children are diagnosed with ADHD have documented significant parenting struggles (Weiss, Hechtman, & Weiss, 2000). Parents report difficulties sustaining attention during supervision and monitoring of children, procrastination in parenting tasks such as bed or bath time, and problems in planning and carrying out the instrumental and organizational tasks of parenting, such as remembering the child’s activities, play dates, and homework. Certainly such difficulties are consistent with the types of cognitive, regulatory, and motivational deficits proposed as core to ADHD. As outlined next, to a substantial extent clinical observations of links between ADHD and parenting difficulties have been confirmed in empirical studies using a variety of samples, measures, and methodologies. The following review is organized according to the behavioral control and emotional responsiveness dimensions of parenting, with initial consideration of the main effects of parental ADHD symptoms, followed by an examination of how parental ADHD interacts with child vulnerabilities.
4.1. Parental ADHD and effective parenting control
Many studies of ADHD in parents have included measures of how parents respond to child misbehavior, focusing primarily on lax or permissive versus over-reactive parenting control. The majority of these studies have examined parents of preschool or school-aged children and little is known about how ADHD may impact aspects of parental effective control at younger or older child ages. Biederman, Faraone, and Monuteaux (2002) found that clinically diagnosed adults with ADHD reported reduced family cohesion (perhaps indicating reduced parental emotional responsiveness) and increased conflict (presumably including parental control efforts) compared to non-ADHD parents. These associations remained even when controlling for other forms of parent psychopathology, socioeconomic status, and the child’s ADHD status. More recently, Murray and Johnston (2006) compared clinically diagnosed mothers with ADHD to control mothers. All mothers had children with ADHD and other forms of maternal psychopathology and child oppositional behavior were controlled statistically. Compared to mothers without ADHD, mothers with ADHD reported they were less consistent in their parenting, monitored their children less, and had fewer family routines. A comparison of mother and child reports of the mother’s knowledge of the child’s activities confirmed the reduced monitoring. Mothers with ADHD also were observed to offer less effective solutions on a parenting problem-solving task.
Other studies have focused on parents of children with ADHD, assessing ADHD symptoms dimensionally in this group of parents who, because of the high heritability of the disorder, can be considered at risk of having high levels of ADHD symptoms. Chronis-Tuscano et al. (2008) employed both self-reports and observations of parent–child interactions to assess parenting and their findings are consistent with those from clinically diagnosed adults. With child oppositional behavior and maternal depression controlled, maternal ADHD symptoms were related to more inconsistent discipline, more inappropriate repetition of commands, and more negative parenting control (criticism, physical punishment). Among mothers of boys with ADHD, Johnston, Scoular, and Ohan (2004) found that mothers’ reports of their own hyperactive–impulsive, but not inattentive symptoms, were positively correlated with their reports of both over-reactive and lax parenting.
Looking at fathers of children with ADHD, Arnold, O’Leary, and Edwards (1997) found that fathers’ ADHD symptoms moderated the influence of the fathers’ involvement in parenting. Confirming a negative relation between ADHD and parenting control behaviors, for fathers with high levels of ADHD symptoms, greater involvement with their children was associated with more reported over-reactive discipline. In contrast, for fathers with few ADHD symptoms, more involvement was associated with less over-reactivity in discipline. In a second study, Harvey, Danforth, Eberhardt McKee, Ulaszek, and Friedman (2003) found that before parent training, for both mothers and fathers of children with ADHD, symptoms of inattention were associated with reports of lax discipline. Among fathers, impulsivity also was associated with reported over-reactive parenting and with an observed increase in arguments with the child. When depression and alcohol use were controlled, the associations between parenting and parental ADHD were reduced, but most typically remained significant. Interestingly, the relations between parental ADHD and parenting difficulties were often of greater magnitude after the parenting program, suggesting that the treatment was not sufficient to ameliorate the influence of parental ADHD. In a large sample of families with two children diagnosed with ADHD, Pressman et al. (2006) found that, even with other forms of psychopathology in the model, mothers’ ADHD symptoms negatively predicted functional impairment in the younger sibling, and through family disorganization had an indirect effect on impairment in the older sibling. In this study, father ADHD symptoms did not predict child impairment or family functioning beyond the effects associated with mood disorder and substance abuse. Finally, Ellis and Nigg (2009) recently examined parenting and parental ADHD symptoms in mothers and fathers of children with and without ADHD. At the bivariate level, mothers’ ADHD symptoms were correlated with reports of more inconsistent discipline. In analyses testing whether parenting made a contribution above and beyond parental ADHD and child comorbidities, fathers’ inconsistent discipline was a unique predictor of child inattention symptoms. This suggests that, although parent ADHD may contribute directly to child ADHD (i.e., via genes), deficits in parenting control remain important in predicting the child’s level of symptoms.
Moving to community samples of parents, studies indicate similar parenting impairments associated with even sub-clinical elevations in parental ADHD symptoms. Among mothers of preschoolers, Banks et al. (2008) found that those with more ADHD symptoms reported more lax and over-reactive parenting, even though their children did not show more ADHD symptoms or oppositional behavior than mothers with fewer ADHD symptoms. Examining mothers of elementary school aged children, Chen and Johnston (2007) found that at the bivariate level, both maternal inattention and impulsivity were related to reports of parenting over-reactivity and inconsistent discipline. However, in regression analyses only inattention symptoms were uniquely associated with mothers’ use of inconsistent discipline, after controlling for impulsivity, other maternal psychopathologies, family socioeconomic status, and child conduct problems. In an interesting study extending examination of parental organizational skills that may be negatively affected by ADHD, Mokrova, O’Brien, Calkins, and Keane (2010) tested links between community parents’ self-reports of ADHD symptoms and the level of home chaos and inconsistent discipline. For both mothers and fathers, ADHD symptoms were positively related to reports of a more chaotic home environment, even with demographic characteristics and the child’s level of ADHD controlled. For mothers, this home chaos mediated links between maternal ADHD and inconsistent parenting. For fathers, chaos served instead to moderate the association between ADHD symptoms and inconsistent parenting, such that father ADHD symptoms only had a unique relation to inconsistent discipline when home chaos was low. The authors conclude that inhibition and difficulties with attention may compromise parenting organization and planning abilities, leading to inconsistency in discipline.
In summary, the differences demonstrated between parents with elevated levels of ADHD symptoms compared to those with low levels on various measures of parenting control are consistent with what one might expect in adults who struggle with executive dysfunctions in working memory, inhibitory control, self-regulation, or delay aversion, and their daily functioning equivalents of poor time management, self-organization, problem-solving, self-motivation, and emotional self-regulation. difficulties appear in parental planning, problem-solving and organization, as well as in over-reactivity and inconsistent approaches to discipline in parents with ADHD. We speculate that core deficits in working memory and inhibitory control lead to poor parenting organization and planning skills, that inhibition and delay aversion contribute to inconsistent or lax control and poor self-regulation of emotion and motivation, and that self-regulation (and self-monitoring) deficits yield lower rates of detection of and poor modulation of reactions to child misbehavior. However, the existing studies are still few in number and have relied very heavily on parent self-reports on either the Parenting Scale (Arnold, O’Leary, Wolff, & Acker, 1993) or the Alabama Parenting Questionnaire (Shelton, Frick, & Wootton, 1996). Although these are strong and widely used measures, they represent only one method of assessment and a limited range of parenting behaviors. In particular, with the exception of the work on parental organization, the dimension of parenting control has been examined almost exclusively with regards to reactions to child misbehavior. Other important elements of parenting control, such as the ability to proactively structure situations or to provide appropriate instructions and scaffolding for children have seldom been examined. There remains a need for much further work in this area, to expand the aspects of parenting control that are examined and the measurement methods used, to assess parenting across a wider developmental age range, and importantly to relate parenting difficulties more directly to the core deficits of ADHD. Such research would yield important information regarding the specificity or generality of particular cognitive processing–parenting links, both within and across parents.
4.2. Parental ADHD and parenting emotional responsiveness
Emotional responsiveness among parents with ADHD symptoms has been assessed in samples of very young children, and several elements of emotional responsiveness (often labeled positive parenting) such as Sadeh expressing approval or affection or spending time with the child, have been measured in many of the studies reviewed above focused on preschool and elementary-school aged children. The studies of parents of young infants are important as they offer another way to assess how ADHD symptoms may impair parenting, while reducing or controlling for the impact of child difficulties. Auerbach and colleagues assessed parenting in a sample of male infants followed from birth who were designated as high or low risk for ADHD based on the level of ADHD symptomatology in their fathers. Studies of this sample of at risk infants have demonstrated difficulties with sleep regulation, interest in tasks, anger, and activity level (Auerbach, Atzaba-Poria, Berber, & Landau, 2004; Landau, Sadeh et al., 2010). When the infants were 7 months old, Landau, Avital et al. (2010) found no differences in infant behavior as measured in the parent–child interactions (defined as infant negative affect, bids for attention, need for help, and physiological events) between the two groups. But, both fathers and mothers in the high risk group were observed as less responsive in their parenting during face-to-face interactions with the infant, particularly in terms of responding insensitively to infant negative emotions and distress. Results remained even with maternal psychopathology controlled. Interestingly, at the same age, in a block task in which parents were asked to refrain from intervening in the child’s play, no differences were found for fathers’ behavior, but again mothers were less responsive with high risk infants compared to low risk infants (Landau, Amiel-Laviad, Berger, Atzaba-Poria, & Auerbach, 2009). Given that the infant groups were designated on the basis of father ADHD symptoms, these results are puzzling. They may suggest that ADHD in the father serves to reduce the resources the mother can devote to the infant (e.g., time is spent compensating for father deficits). Alternately, fathers’ ADHD symptoms may not impact parenting in all situations, perhaps sparing play interactions, or perhaps the parenting behaviors that are most affected by ADHD vary across parent gender.
Also looking at parenting with infants, Kryski, Mash, Ninowski, and Semple (2010) discovered a significant link between ADHD symptoms (measured dimensionally) and mothers’ decreased utterance length in their interactions with their infants. This is consistent with speculation that an aversion to delays or to boring, repetitive tasks may reduce a mother’s ability to engage in extended pleasant interactions with a young child. This same research group (Semple, Mash, Ninowksi, & Benzies, 2011) also found that levels of inattention symptoms significantly predicted reduced sensitivity and increased intrusiveness and negative regard in mothers’ interactions with their young infants. In this community sample, inattentive symptoms, but not hyperactive–impulsive symptoms, were predictive of these parenting responses, even with maternal anxiety and infant activity level controlled. Arguing that parental ADHD may influence the adult outcome of children with ADHD, Edel, Juckel, and Brune (2010) asked adults with ADHD to retrospectively recall ADHD symptoms in their parents and the parents’ warmth/rejection toward them when they were young children. Recalled parental ADHD was also examined in relation to the adult children’s current levels of functioning. Consistent with previous reports, approximately two-thirds of the adults with ADHD felt that at least one of their parents had had ADHD. They recalled mothers with more ADHD symptoms as being more rejecting and punitive and the fathers in these families as showing more warmth, perhaps reflecting compensation between parents. Arguing for possible long lasting effects, recalled ADHD symptoms in the mother also were associated with attachment difficulties in the adult children with ADHD. There were few effects related to recalled ADHD symptoms in the fathers.
Moving to samples of older children with parenting assessed concurrently, Murray and Johnston (2006) found no difference between mothers with and without ADHD in their levels of positive parenting, either as reported by the mother or by the child. In parents of children with ADHD, Chronis-Tuscano et al. (2008) found maternal ADHD symptoms related to reports of less involvement with the child. In this sample, maternal ADHD symptoms were associated with less positive parenting only when ADHD symptoms were measured solely by mothers’ self-report and only when child oppositional behavior was not controlled. In fact, at the bivariate level, collateral reports of the mothers’ ADHD symptoms were positively associated with the mothers’ positive parenting during play. Using baseline data from the MTA study, Johnston, Murray, Hinshaw, Pelham, and Hoza (2002) found that mothers’ reports of their own childhood ADHD symptoms were not related to their responsiveness in interactions with their ADHD sons. Extending to a sample of both mothers and fathers of children with and without ADHD, Ellis and Nigg (2009) found that fathers’, but not mothers’, ADHD symptoms correlated with reports of less involvement with the child. In community samples with parental ADHD measured dimensionally, Mokrova et al. (2010) found parent-reported positive parenting was not associated with either mothers’ or fathers’ ADHD symptoms, although parental ADHD symptoms were related to less involvement and to unsupportive parenting. Finally, in their community sample, Chen and Johnston (2007) found no relation between mothers’ ADHD symptoms and observations of responsiveness, but did find that both impulsivity and inattention were correlated with mothers’ reports of less involvement and use of less reinforcement.
In summary, results regarding the relation between parental ADHD and measures of parenting emotional responsiveness are somewhat inconsistent across studies. In some studies parent self-reports and observations of emotionally responsive parenting behaviors are not significantly related to parental ADHD, other studies suggest that parental ADHD is associated with reduced emotional responsiveness, and yet other studies find positive associations between parental ADHD and measures of emotional responsiveness, particularly those focused on positive parenting. These divergent findings are likely associated with sample and measurement differences across studies, and the number of investigations remains too small to permit definite conclusions. However, in contrast to the much more consistent negative associations found between parental ADHD and measures of parenting control behaviors, the findings for parental emotional responsiveness open the possibility that the core deficits of ADHD are not equally impairing in all domains of parenting. Perhaps the same failures of inhibition and self-regulation that create difficulties in parenting consistency and task organization play a more positive role in encouraging a parent’s spontaneity or enjoyment of time with the child. As with parenting control behaviors, more studies directly linking parental emotional responsiveness to the core deficits of ADHD, assessing more aspects of emotional responsiveness and across a wider range of child ages, would offer significant advancement in our understanding and would assist in clarifying the existing inconsistencies across studies. For example, studies might address questions such as whether a reduced sensitivity to aversive events in some parents with ADHD allows for greater parental tolerance for child ADHD behaviors and thus more positive parenting experiences with the child, or whether difficulties with inhibitory control allow the parent with higher levels of ADHD to engage, without embarrassment or constraint, in play that is fun- and child-oriented.
5. Summary of parental ADHD in relation to parenting
Across samples of parents diagnosed with ADHD, parents of children with ADHD, and community samples of parents with ADHD symptoms measured dimensionally, evidence indicates that parental ADHD symptoms are associated with deficits in parenting control behaviors, including family disorganization and chaos, less monitoring of child behavior, less effective child-rearing problem-solving, and more inconsistent and over-reactive discipline. In almost all studies, the associations between ADHD and parenting impairments remain even with potential confounds such as comorbid parent psychopathologies, child ADHD or comorbid problems, and family socioeconomic status controlled. In contrast, parental ADHD appears less consistently associated with measures assessing parental emotional responsiveness, including positive parenting, involvement or general responsiveness.
The strength of these broad conclusions is uncertain as the research literature in this area remains underdeveloped. Existing studies have been heavily weighted to samples of mothers and school-aged sons, and a reliance on self-report measures of parenting. Studies that have included fathers have pointed to both similarities and possible differences in the influence of ADHD symptoms across parent genders, but much more research is needed to understand the role of both parent and child gender. Longitudinal studies that trace the relations among parental ADHD deficits, parenting, and child behavior over the span of child development are sorely needed. Existing studies have hinted that parental ADHD may extend its influence to coparents, with possible demands for a compensatory role for these non-ADHD partners. Studies assessing the impact of adult ADHD across multiple family members (e.g., siblings) and subsystems (e.g., the coparenting partnership) would significantly advance our understanding of this broader family perspective. Finally, the majority of existing studies have been conducted from a deficit perspective, focusing on limitations to the parenting abilities of adults with ADHD, and less is known about potential parenting strengths. It is possible that, in some circumstances, parents with ADHD are more energetic, spontaneous, or enthusiastic, or alternately that they are more accepting of ADHD characteristics in their offspring. If they exist, and if evidence links these characteristics to more positive child outcomes, such parenting strengths could be capitalized on in developing treatments for this group of parents.
6. The interactions among parental ADHD, parenting, and child characteristics
We now consider studies where parental ADHD is examined, not as a direct effect on parenting, but as a moderator of the relation between parenting and child ADHD characteristics. Typically framed within a goodness of fit perspective, these studies have assessed both parenting control behaviors (e.g., over-reactive parenting) and emotional responsiveness (e.g., positive parenting). Other studies have examined the interaction of parental and child ADHD in relation to other aspects of parent and child functioning, such as social skills or parental attributions for child behavior. As a preamble to the findings in this section, we note that across studies evidence suggests both that the interaction of parent and child ADHD symptoms may exacerbate parenting difficulties but also that, in some situations, this combination serves to attenuate the effects of parenting deficits on child behavior.
Looking at a community sample of mothers of young infants, Watkins and Mash (2009) found that mothers with higher levels of ADHD symptoms reported more hostile-reactive parenting control, but only in cases where they perceived their young infants to be difficult (these results remained significant with maternal comorbidities controlled). In preschool and school-aged children, studies by Psychogiou and colleagues (Psychogiou, Daley, Thompson, & Sonuga-Barke, 2007; Psychogiou, Daley, Thompson, & Sonuga-Barke, 2008) tested how parent and child ADHD symptoms may interact to affect parenting in both mothers and fathers. In two community samples, maternal ADHD symptoms had main effects of increasing negative expressed emotion, but there also were significant interactions between mother and child ADHD. When maternal ADHD symptoms were low, higher levels of child ADHD were associated with less positive parenting (both parent-reported and observed). However, when mothers had higher levels of ADHD symptoms, child ADHD symptoms were unexpectedly associated with more positive parenting. Psychogiou et al. described this as a “similarity fit” phenomenon, and speculated that mothers with ADHD may be better able to synchronize their parenting with children with ADHD because of shared motivational patterns or cognitive tempos that result in less provocation or conflict, or because mothers with ADHD symptoms are better able to empathize with their child’s difficulties. In contrast to the results for mothers, Psychogiou et al. (2007) found evidence of a “similarity misfit” phenomenon in fathers. Greater child ADHD symptoms were associated with more parent reported control difficulties (poor monitoring, inconsistent discipline, physical punishment), and this association was even stronger for fathers with higher ADHD symptoms.
Studies also have examined how parental ADHD may moderate the relation between parenting and child ADHD in families of individuals diagnosed with ADHD. Although Griggs and Mikami (2011) did not directly assess parenting, they did examine both direct effects of mothers’ ADHD symptoms on mother and child social difficulties, as well as a similarity fit interaction between mother and child ADHD symptoms. Although maternal inattention was associated with observations of reduced prosocial behavior in non-problem children, there was no relation in children with ADHD; and maternal ADHD symptoms were associated with less observed irritability toward children with ADHD with no association found for control children. Finally, also not assessing parenting directly, but consistent with the similarity fit hypothesis, Biederman et al. (2002) found some indication that non-ADHD children of parents with ADHD were academically impaired, while there was no association of parental ADHD and academic problems for children with ADHD. To our knowledge, this is the only study examining the interaction of parent and child ADHD, when both parties met clinical diagnostic criteria.
In summary, these findings suggest the possibility that the parenting difficulties associated with adult ADHD may, in some instances, be offset by an advantage provided by the match of parent and child ADHD. These interactive effects have been noted for measures of both parenting control behaviors and emotional responsiveness, although they have not been extensively tested with regards to either dimension. Psychogiou et al.’s results suggest that different mechanisms might be operating for mothers with ADHD (e.g., greater synchrony, tolerance, or empathy) versus fathers with ADHD (e.g., annoyance or exacerbation of difficulties in the self-regulation of controlling parenting behaviors) with regards to their interactions with children with ADHD. However, complicating the picture, recent data from our lab also found interactions between parental ADHD measured dimensionally and the ADHD status of the child (Johnston & Lee-Flynn, 2011b). But the gender effects in the Johnston and Lee-Flynn study were reversed from those in Psychogiou’s studies. Mothers with high levels of ADHD offered more child-blaming attributions only when their children had ADHD (a similarity misfit), while fathers offered fewer child-blaming attributions when their child had ADHD (similarity fit). Given that the available studies are few in number and vary along numerous dimensions including whether the samples were clinic referred vs. community, the ages and genders of the children, and the measures or aspects of parenting considered, it would be premature to accept any of the findings as conclusive. Obviously, further replications and extensions testing how parental and child ADHD may interact in influencing parenting are needed before confidence can be placed in the findings, or before much speculation is offered regarding possible reasons for the differences across mothers vs. fathers. Linking of possible fit vs. misfit predictions to whether the parent and child with ADHD share similar cognitive or motivational difficulties or patterns of neuropsychological functioning may be useful in clarifying the parameters that limit and potentially moderate these interactive effects.
7. Genetically informed studies of parental ADHD and parenting
In recent years, a growing number of studies have demonstrated that aspects of both parental control and emotional responsiveness interact with the child’s genetic make-up to increase the risk for ADHD or other disruptive disorders in the child, with studies examining genetic variations related to both dopamine and serotonin transmission (Lahey et al., 2011; Martel et al., 2011; Nikolas, Friderici, Waldman, Jernigan, & Nigg, 2010; Sheese, Voelker, Rothbart, & Posner, 2007). For example, Propper et al. (2008) tested infants repeatedly between 3 and 12 months, and found that an interaction between the dopamine receptor gene DRD2 in the infant and maternal sensitivity predicted the development of infants’ regulation of reactivity to stress. Similarly, although they did not measure parenting directly, Auerbach et al. (2010) found that ADHD symptoms in fathers, in conjunction with variations on the DAT1 receptor gene in the young child, predicted child ADHD symptoms. In an intriguing meta-analysis, Bakermans-Kranenburg and Van Ijzendoorn (2011) concluded that, within the general population, dopamine-related genes may provide children not only with an increased vulnerability to the effects of negative child-rearing, but may also create a susceptibility to benefit more from positive parenting effects. Unfortunately, none of these studies have explicitly examined parental ADHD. However, the possibility of differential sensitivity to parenting (Belsky & de Haan, 2011; Obradovic, Bush, Stamperdahl, Adler, & Boyce, 2010) suggests that compensatory behaviors, either within an individual parent with ADHD (e.g., difficulties with control, but strengths in emotional responsiveness), or across parenting couples (e.g., when a partner is able to compensate for the parenting difficulties of the adult with ADHD) may be a particularly important mechanisms for offsetting the genetic risk for ADHD. In the existing genetically informed studies, it is important to remember that, although replications exist, there remains a high potential for false positive findings as studies are often characterized by low power and extensive, exploratory testing of multiple genes and a narrow selection of measures of parenting (Nigg, Nikolas, & Burt, 2010). These risks form part of the impetus for the call, in this paper, for a more theoretically guided selection of parenting variables, rather than post hoc selection of only those genes and parenting measures which demonstrate significant effects.
Following from findings of interactions of parenting and child genetic makeup, researchers also have addressed whether genes exert main or interactive effects on parenting. Based both in child studies linking dopaminergic functioning to ADHD and in animal models confirming the role of this neurotransmitter in parenting behavior, Lee et al. (2010) found that variations in the maternal DAT1 gene predicted difficulties in observed parenting control (i.e., negative parenting and increased commands) in mothers of young children with and without ADHD. In addition, the association between maternal genes and these parenting impairments was particularly strong in the presence of child disruptive behavior. These relations held even accounting for other forms of maternal psychopathology and possible gene–environment associations. Consistent with the suggestion from the behavioral studies that parenting control may be more affected by parental ADHD while emotional responsiveness is relatively spared, in the Lee et al. study maternal genes were not predictive of observed positive parenting, nor did they interact with child characteristics in predicting this aspect of parenting.
Further studies linking parental ADHD at genetic, neurological, neuropsychological, and behavioral levels to parenting difficulties will offer exciting extensions to this beginning knowledge. For example, assessing inhibitory control in adults who have various genetic polymorphisms associated with ADHD across neuropsychological tasks (e.g., continuous performance tasks), measures of neural functioning during such tasks (e.g., fMRI of frontal lobe activation), and measures of parenting where poor inhibitory control is assumed central (e.g., harsh reactions to child misbehavior) would yield fascinating information regarding links between ADHD symptomatology and parenting, as well as the potential mechanisms underlying these associations. Similarly, examining parenting as it occurs in families where both parental ADHD and child ADHD are present and comparing these to families where either only one parent or child with ADHD is present, or where no families members are diagnosed provides opportunities to isolate the contributions of parental and child ADHD to parenting difficulties. Genetically-informed studies may hold special utility in understanding the conditions under which parent and child ADHD interact to exacerbate or buffer parent–child interaction difficulties. Such studies will be particularly useful if they proceed with careful attention to the dimensions of parenting which may or may not suffer from the impact of the core deficits associated with parental ADHD.
8. Issues and future directions
Several issues emerge in assessing the effects of ADHD on parenting behaviors. First, as we have noted throughout this review, there is a need for research to be guided by consideration of how the core deficits of ADHD may impact different dimensions of parenting. Theoretically grounded hypotheses and the inclusion of comprehensive, multi-method assessments of both parenting and ADHD deficits would do much to advance our knowledge of the impact of ADHD on parenting. Acknowledging the heterogeneity of ADHD, it is unlikely that the linkages between ADHD deficits and parenting dimensions are consistent across all parents with ADHD but rather that multiple pathways of influence exist depending on the particular cognitive, self-regulatory, or motivational deficits that characterize the parent’s ADHD. Importantly, research guided by a framework that focuses on ADHD deficits may also elucidate areas of parenting that remain spared, or even enhanced, by parental ADHD.
In considering future genetically informed studies, the overlap and reciprocal relations among parent genetic risk, child genetic risk, and parenting behavior must be addressed. Although not shown in Fig. 1, it is theoretically possible that the entire relationship between parental ADHD and child problems is genetically driven, with little or no role for parenting as an intervening variable (a passive correlation between parent and child ADHD behaviors). Alternately, although not consistent with existing knowledge regarding the heritability of ADHD, the relation could be entirely independent of genetic influence. Instead, it is obvious that the effects of parental ADHD transmit to the child both through genetic channels as well as via mechanisms such as parenting. Here, a number of possible pathways of influence may occur. ADHD may influence parenting which in turn mediates the relation to child ADHD and/or to other conditions such as conduct problems. And, as studies have shown, parenting also functions as a moderator to amplify or dampen the relation between parental and child ADHD and comorbid conditions. Of course, the potentially confounding influence of gene–environment correlations and child effects on parenting must be addressed in studies of such interactions and as noted above comparisons of families in which parental and child ADHD are both, either, or neither present will be particularly informative in this regard.
Beyond the need for further studies integrating genetic and behavioral information, other significant gaps also exist in research on parental ADHD. The vast majority of existing studies are cross-sectional, giving static snapshots of how parental ADHD, parenting, and child problems are associated. It will be crucial that we expand this knowledge with longitudinal studies, following both parents and children across significant developmental stages (e.g., early post-natal care offered by first -time parents, transitions from school-age children to adolescents). Such studies are needed to reveal how the transactional influences among ADHD deficits, parenting impairments (or strengths), and child outcomes may evolve and change over time. Inclusion of the influence of the broader family, cultural, and social context into this research will also be important. Assessing the influence of parental ADHD on early parent–child interactions holds particular promise for opening a window into how the caregiving environment may channel the infant into different pathways of development. For example, understanding how deficits in verbal working memory change the parent’s use of language may lead us to important knowledge regarding how such alterations in parenting behavior impact child’s emerging cognitive structures and processes. Longitudinal perspectives, beginning in early infancy will provide evidence able to address questions of whether different ADHD-linked deficits in parenting may enter into differential relations with child behaviors over time. For example, it is possible that during very early development, disruptions in parental emotional responsiveness caused by motivational or inhibitory deficits are critical in generating a lasting negative influence on the young child’s developing capacity for self-regulation and leading to the emergence of child ADHD symptoms. At the same time, it is also possible that later in child development, parenting deficits in areas such as planning and working memory, lead to greater difficulties on the control dimension of parenting and become more prominent predictors of emerging comorbid externalizing child problems. It also is possible to directly test effects of adult ADHD on parenting and those effects on child behavior through medication studies in which parental ADHD is directly manipulated, much as has been done with child ADHD and parent–child interactions. Finally, reflecting a shift to the integration of important genetic advances into psychosocial research, longitudinal designs will benefit from consideration of epigenetic phenomena (e.g., how poorly regulated parenting control may trigger disruptions in attachment or temperament in the young infant).
As longitudinal research provides a picture of emerging parenting and child problems over time in families of parents with ADHD symptoms, special attention must be paid to the relations between ADHD and related deficits or disorders. Although many existing studies have demonstrated that the relations between parental ADHD and parenting impairments survive statistical control for comorbid conditions, the final answers in this area have not been written. The range of comorbid conditions, in both parent and child, that have been assessed have been somewhat limited, and have seldom included parental antisocial or conduct disordered problems. Given that, at least in children, debate continues regarding how to best characterize the relation between ADHD and conduct problems and the deficits that underlie each (e.g., Beauchaine et al., 2010; Rubia, 2010), the role of such comorbidities must remain prominent in studies of adult ADHD and its impact on functioning.
The measurement of both parental ADHD and parenting in previous studies has left considerable room for improvement. Studies are needed that include measures of the core deficits associated with ADHD, and that select parenting measures consistent with theoretical predictions arising from such dysfunctions. Work linking parenting to core deficits of ADHD will also benefit from more careful consideration of how parenting impairments are related to the two (or three) symptom clusters currently used to define the disorder. Although most studies have not distinguished the symptom types, among those studies which did examine links between parenting and inattention vs. hyperactivity-impulsivity, most suggest that the inattention symptoms are those most strongly linked to parenting impairments (e.g., Chen & Johnston, 2007; Semple et al., 2011). Whether these associations arise because of weaknesses in the description of hyperactive–impulsive symptomatology in adults, or because inattention is most intimately tied to parenting remains to be seen. Proposed changes and expansions to the hyperactive–impulsive symptom cluster in DSM-5 may be important in altering the current pattern of findings (American Psychiatric Association, 2010). What is interesting is the consistency with which links between ADHD and parenting are found across the entire dimension of ADHD severity. In agreement with the suggestion that impairments are likely at even subdiagnostic levels (Mannuzza et al., 2011), associations between parenting difficulties and ADHD symptoms appear generally robust to whether the ADHD symptoms are measured dimensionally in community samples or diagnostically in clinical samples.
A second issue related to the assessment of ADHD in parents concerns self-report of symptoms. The majority of existing studies have relied heavily, if not exclusively, on self-reports of ADHD symptoms typically on very obvious and face-valid measures. Several studies have documented limited agreement between such self-reports and reports of the adult’s ADHD symptoms made by other informants (e.g., parents, friends, spouses) (e.g., Belendiuk, Clarke, Chronis, & Raggi, 2007; Jiang & Johnston, 2011) and have suggested that other reports are more valid predictors of functioning (Barkley, Fischer, Smallish, & Fletcher, 2002). difficulties with self-monitoring and accurate self-assessment, as well as efforts at impression management, are all candidate explanations for the lower utility of self-ratings of ADHD. Thus, as research on parenting in adults with ADHD progresses, more comprehensive assessment standards are needed along with research pointing to the more efficiently and informative methods for integrating the multiple sources of information.
With regard to the measurement of parenting, although some existing studies have used observational measures, this type of objective measurement of parenting is essential and must be more broadly incorporated into this area of research. Given the difficulties with self-awareness and self-assessment that have been shown to characterize individuals with ADHD (Barkley, Knouse, & Murphy, 2011), the predominant reliance on parenting self-report measures represents a significant weakness in existing research. In addition, it would undoubtedly be useful for studies to assess parenting behaviors in more naturalistic contexts. The increasing prominence of easy, accessible recording tools (e.g., cell phone cameras, online posting capabilities) combined with convenient digital prompts or reminders, offers exciting possibilities for obtaining brief samples of ongoing parent–child interactions in naturalistic environments.
The studies reviewed in this paper have seldom, if ever, addressed how the gender of the child may influence relations among parental ADHD, parenting, and child outcomes. The growing literature on gender differences in children with ADHD (Greshon, 2002) and knowledge of parenting differences associated with child gender (Lytton & Romney, 1991) points to the risk of ignoring child gender as a potential influence on parenting. Similarly, gender differences in adult expressions of ADHD symptoms must also be considered as these interact with parenting in mothers and fathers. In addition, the possibility of an interplay between parent and child gender may be particularly important in understanding how parent and child ADHD interact. Although parent gender has been examined in some studies, and there are preliminary suggestions that parent gender may moderate the relations between ADHD symptoms and parenting (e.g., Arnold et al., 1997; Ellis & Nigg, 2009; Landau et al., 2009; Psychogiou et al., 2007), the mother–father differences are difficult to summarize and somewhat inconsistent across studies. Further research is needed, particularly within a framework that is sensitive to the differences in the roles of mothering versus fathering of children (e.g., Cummings, Merrilees, George, & Lamb, 2010). More than mothers, fathers are responsible for involving the child in the world outside the home, teaching skills, and placing demands on the child for autonomy and self-regulation (e.g., Downer, Campos, McWayne, & Gartner, 2008; Lamb & Tamis-LeMonda, 2004). Thus, gender of parent is typically confounded with parenting role and careful attention is needed to sort out which findings are specific to males vs. females, versus effects associated with the different parenting roles commonly assumed by mothers and fathers. In addition, typical measures of parenting may have a mother-centric bias (Adamsons & Buehler, 2007). For example, observations of mother–child interactions typically focus on indoor small toy play and either homework or household chores, such as cleaning up or setting the table. There is a need to expand measurement to include observational situations and parent-report measures that are more inclusive of the distinct role of fathers.
Related to the call for greater study of mothers and fathers with ADHD, more research attention needs to be directed to issues of how parents in these families coordinate their parenting behaviors. Adults with ADHD show elevated rates of marital dissatisfaction and divorce (Eakin et al., 2004; Murphy & Barkley, 1996), and thus, questions arise regarding how these adults coordinate their parenting behavior, either before or after a marital dissolution. Suggesting possible gender differences in how partners react to ADHD in the spouse, Minde et al. (2003) reported that women show greater tolerance for ADHD in their husbands than vice versa. In their survey, 60% of non-ADHD men left their female partners who had ADHD, but only 10% of non-ADHD women left men with ADHD.
In summary, existing studies of ADHD and parenting offer a promising beginning and clearly justify a call for expanded work in this area. However, the future must move beyond correlations between self-report measures of parenting and ADHD symptoms assessed using the available measures from studies not designed to focus on parental ADHD. New work should be theoretically grounded in models of both ADHD deficits and dimensions of parenting, should address the complex transactional patterns that exist between parent and child behavior and genetic risk, and should strive to understand how such patterns evolve over time and development. As always, there are also questions of the generalizability of existing and emerging findings, and replications across a diversity of families are needed. These are tall orders for future research, but the potential for a fuller understanding of parental ADHD to fuel movement toward early intervention, or even prevention, efforts for children at risk more than justifies the needed effort.
9. Implications for interventions for parents and children with ADHD
Both medication and psychosocial treatments have been developed and tested for adults with ADHD, with a focus on outcomes such as symptom reduction and/or functional impairments in work and interpersonal domains (Faraone et al., 2004; Safren et al., 2010; Solanto et al., 2010). In this section, we consider the implications of parenting difficulties and relative strengths in adults with ADHD with regard to how such information might best be incorporated into parent-delivered interventions for children with ADHD. Even pharmacological treatment for child ADHD relies on parents for timely administration of the medication, monitoring of benefits and side effects, and ongoing collaboration with the prescriber. ADHD symptoms may interfere with a parent’s ability to execute these tasks in a manner that maximizes the child’s medication response (e.g., Hoza et al., 2006). Psychosocial interventions for child ADHD rely even more heavily on parent involvement. Sonuga-Barke and Halperin (2010) have recently argued for the need to consider early intervention or even prevention efforts for ADHD. Given the documented familial nature of the disorder, and the parenting deficits outlined above, modifying parenting in adults with ADHD would appear as a high priority target for such early intervention efforts. To the extent that child vulnerabilities interact with risk factors such as inadequate parenting to culminate in developmental pathways that lead to ADHD or other disruptive behavior disorders, efforts are needed to maximize the possible impact of parenting interventions in this population. Unfortunately, current parenting interventions are either untested or less than optimal in affording change in the parenting behavior of adults with ADHD.
Pharmacotherapy with stimulants is the most widely established treatment for adult ADHD. However, the effects of medication on parenting have seldom been tested. Early case studies reported reductions in negative parenting in mothers with ADHD treated with medication (Daly & Fritsch, 1995; Evans, Vallano, & Pelham, 1994). More recently, Chronis-Tuscano et al. (2008, 2010) tested the effects of medication in a small sample of mothers diagnosed with ADHD. During the titration phase, increasing doses of medication were associated with reductions in mother-reported inconsistent discipline and physical punishment, but not with changes in parenting involvement or positive parenting. In a subsequent placebo controlled phase, medication was again associated with medium to large effects for maternal reports regarding involvement, discipline, and punishment, although the effect size for positive parenting was still small. In addition, these parent-reported improvements were not corroborated by collateral reports of parenting or by direct observations. Beyond pharmacotherapy, cognitive behavioral interventions have been shown to be efficacious in treating adult ADHD. Yet the impact of such interventions on functioning in the parenting domain has not been examined.
Focusing on the evidence-based interventions used in the treatment of child ADHD, it is known that children of mothers with high levels of ADHD symptoms are less likely to benefit from either behavioral or medication treatments (Harvey et al., 2003; Jensen et al., 2007; Sonuga-Barke et al., 2002). Looking specifically at behavioral parent training, a recent study by Chronis-Tuscano et al. (2011) provided evidence that changes (or lack thereof) in negative parenting mediate the relation between maternal ADHD and reduced improvements in child behavior. Targeting parental ADHD seems a needed addition to services provided for these families, and research is needed to address how evidence-based treatments for child ADHD may be best modified to be maximally useful to parents with ADHD.
Parenting interventions for adults with ADHD may need several modifications, both in content and in format in order to enhance their effectiveness. The structure of these programs may need to shift from a focus on psycho-education to enhanced skill-based practice, both in session and at home given that repetition may be key to building new parenting habits. Modifications to the typical lecture style group format also may be needed, for example, allowing for more individualized, shorter periods of instruction and reducing the emphasis on dyadic presentations in favor of more interactive or faster-paced learning via media presentations, role-plays, or discussions. Modifications may also be needed to the content of parenting interventions to reflect emerging knowledge regarding the areas of relative strengths and deficiencies in the parenting of adults with ADHD. For example, explicit instruction in organizational and planning skills relevant to parenting may be useful. Programs may need to incorporate teaching of compensatory strategies, such as using friends or partners as parenting coaches, or generating externalized parenting supports such as tutors for the child. Although it seems likely that combining such modified parenting programs with medication treatment of adult ADHD may maximize the benefits, this remains an open question. Recognizing that ADHD may be more of a disorder of performing what one knows than of knowing what to do (Barkley et al., 2008), such parenting interventions may need to focus as well on means of modifying settings in the home and community in which parenting is involved so as to help prompt, cue, and otherwise elicit more appropriate parenting behavior. Similarly, there may be a need for more frequent, external reinforcement for the parenting efforts of adults with ADHD, as child behavior may not change quickly enough to provide reinforcement that is sufficient or immediate enough to sustain changes in parenting behaviors.
Finally, given that ADHD-related deficits may over time, generate additional difficulties related to adults’ sense of competence as parents and this sense of helplessness may interfere with the acquisition of parenting skills, parenting interventions may need to explicitly target dysfunctional cognitions about parenting in order to renew a sense of parenting empowerment. Strategies may be needed to assist the parent in dealing with low motivation (e.g., helping the parent to develop reminders which prompt them to visualize the long term consequences of their parenting choices or the identification of areas of relative strength).
10. Conclusion
In conclusion, we offer this review as a heuristic guide for further, much needed research regarding the impact of adult ADHD on parenting. Viewed from a family systems/developmental psychopathology framework, understanding how ADHD may alter parenting behavior is a critical link in understanding the interplay of genetic and environmental factors that contribute to various child outcomes, including but certainly not limited to ADHD. Research addressing parenting deficits, and possible strengths, as predicted from current theoretical models of the core dysfunctions of ADHD also will provide foundational evidence for the development of prevention and early intervention programs which may ultimately serve to reduce the significant personal and social costs currently associated with ADHD and related conditions.
Footnotes
We thank Russell A. Barkley for his comments on an earlier draft of this paper. Preparation of this article was supported by a grant from the Canadian Institutes of Health Research to the first author, and a University Graduate Fellowship to the third author.
References
- Adamsons K, Buehler C. Mothering versus fathering versus parenting: Measurement equivalence in parenting measures. Parenting: Science and Practice. 2007;7:271–303. [Google Scholar]
- American Psychiatric Association. Attention-deficit/hyperactivity disorder. 2010 Retrieved from. http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=383.
- Arnold EH, O’Leary SG, Edwards GH. Father involvement and self-report parenting of children with attention deficit-hyperactivity disorder. Journal of Consulting and Clinical Psychology. 1997;65:337–342. doi: 10.1037/0022-006X.65.2.337. [DOI] [PubMed] [Google Scholar]
- Arnold DS, O’Leary SG, Wolff LS, Acker MM. The Parenting Scale: A measure of dysfunctional parenting in discipline situations. Psychological Assessment. 1993;5:137–144. [Google Scholar]
- Auerbach JG, Atzaba-Poria N, Berger A, Landau R. Emerging developmental pathways to ADHD: Possible path markers in early infancy. Neural Plasticity. 2004;11:29–43. doi: 10.1155/NP.2004.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach JG, Atzaba-Poria N, Berger A, Landau R, Arbelle S, Raz Y, et al. Dopamine risk and paternal ADHD symptomatology associated with ADHD symptoms in four and a half-year-old boys. Psychiatric Genetics. 2010;20:160–165. doi: 10.1097/YPG.0b013e32833a1f27. [DOI] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, Van Ijzendoorn MH. Differential susceptibility to rearing environment depending on dopamine-related genes: New evidence and a meta-analysis. Development and Psychopathology. 2011;23:39–52. doi: 10.1017/S0954579410000635. [DOI] [PubMed] [Google Scholar]
- Banks T, Ninowski JE, Mash EJ, Semple DL. Parenting behavior and cognitions in a community sample of mothers with and without symptoms of attention-deficit/hyperactivity disorder. Journal of Child and Family Studies. 2008;17:28–43. [Google Scholar]
- Barkley RA. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Defficient emotional self-regulation: A core component of attention-deficit/hyperactivity disorder. Journal of ADHD and Related Disorders. 2010;1:5–37. [Google Scholar]
- Barkley RA. Attention-deficit/hyperactivity disorder, self-regulation, and executive functioning. In: Vohs K, Baumeister RF, editors. Handbook of self-regulation. New York: Guilford; 2011. pp. 551–563. [Google Scholar]
- Barkley RA. Distinguishing sluggish cognitive tempo from attention-deficit/hyperactivity disorder in adults. Journal of Abnormal Psychology. 2011 doi: 10.1037/a0023961. (Electronic publication ahead of print) [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M. The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:503–513. doi: 10.1097/00004583-201005000-00011. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. The persistence of Attention-Deficit/Hyperactivity Disorder into young adulthood as a function of reporting source and definition of disorder. Journal of Abnormal Psychology. 2002;111:279–289. [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: Antisocial activities and drug use. Journal of Child Psychology and Psychiatry. 2004;45:195–211. doi: 10.1111/j.1469-7610.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: Adaptive functioning in major life activities. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Knouse LE, Murphy KR. Correspondence and disparity in the self- and other ratings of current and childhood ADHD symptoms and impairment in adults with ADHD. Psychological Assessment. 2011;23:437–446. doi: 10.1037/a0022172. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR. The nature of executive function (EF) deficits in daily life activities in adults with ADHD and their relationship to performance on EF tests. Journal of Psychopathology and Behavioral Assessment. 2011;33:137–158. [Google Scholar]
- Barkley RA, Murphy KR, Fischer M. ADHD in adults: What the science says. New York: Guilford; 2008. [Google Scholar]
- Barrett J, Fleming AS. Annual research review: All mothers are not created equal: Neural and psychobiological perspectives on mothering and the importance of individual differences. Journal of Child Psychology and Psychiatry. 2011;52:368–397. doi: 10.1111/j.1469-7610.2010.02306.x. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Hinshaw SP, Pang KL. Comorbidity of attention-deficit/hyperactivity disorder and early-onset conduct disorder: Biological, environmental, and developmental mechanisms. Clinical Psychology: Science and Practice. 2010;17:327–336. [Google Scholar]
- Belendiuk KA, Clarke TL, Chronis AM, Raggi VL. Assessing the concordance of measures used to diagnose adult ADHD. Journal of Attention Disorders. 2007;10:276–287. doi: 10.1177/1087054706289941. [DOI] [PubMed] [Google Scholar]
- Belsky J, de Haan M. Parenting and children’s brain development: The end of the beginning. Journal of Child Psychology and Psychiatry. 2011;52:409–428. doi: 10.1111/j.1469-7610.2010.02281.x. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Mick E, Spencer T. High risk for attention deficit hyperactivity disorder among children of parents with childhood onset of the disorder: A pilot study. The American Journal of Psychiatry. 1995;152:431–435. doi: 10.1176/ajp.152.3.431. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Monuteaux MC. Impact of exposure to parental attention-deficit hyperactivity disorder on clinical features and dysfunction in the offspring. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences. 2002;32:817–827. doi: 10.1017/s0033291702005652. [DOI] [PubMed] [Google Scholar]
- Castellanos FX, Sonuga-Barke EJS, Milham MP, Tannock R. Characterizing cognition in ADHD: Beyond executive dysfunction. Trends in Cognitive Sciences. 2006;10:117–123. doi: 10.1016/j.tics.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Chen M, Johnston C. Maternal inattention and impulsivity and parenting behaviors. Journal of Clinical Child and Adolescent Psychology. 2007;36:455–468. doi: 10.1080/15374410701448570. [DOI] [PubMed] [Google Scholar]
- Chronis AM, Lahey BB, Pelham WE, Kipp HL, Baumann BL, Lee SS. Psychopathology and substance abuse in parents of young children with Attention-Deficit/Hyperactivity Disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:1424–1432. doi: 10.1097/00004583-200312000-00009. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, O’Brien KA, Johnston C, Jones HA, Clarke TL, Raggi VL, et al. The relation between maternal ADHD symptoms and improvement in child behavior following brief behavioral parent training is mediated by change in negative parenting. Journal of Abnormal Child Psychology. 2011;39:1047–1057. doi: 10.1007/s10802-011-9518-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Raggi VL, Clarke TL, Rooney ME, Diaz Y, Pian J. Associations between maternal attention-deficit/hyperactivity disorder symptoms and parenting. Journal of Abnormal Child Psychology. 2008;36:1237–1250. doi: 10.1007/s10802-008-9246-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Rooney M, Seymour KE, Lavin HJ, Pian J, Robb A, et al. Effects of maternal stimulant medication on observed parenting in mother–child dyads with attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2010;39:581–587. doi: 10.1080/15374416.2010.486326. [DOI] [PubMed] [Google Scholar]
- Collins WA, Maccoby EE, Steinberg L, Hetherington EM, Bornstein MH. Contemporary research on parenting: The case for nature and nurture. In: Hertzig ME, Farber EA, editors. Annual progress in child psychiatry and child development: 2000–2001. New York: Brunner-Routledge; 2003. pp. 125–153. [Google Scholar]
- Cummings EM, Merrilees CE, George MW, Lamb ME. Fathers, marriages, and families: Revisiting and updating the framework for fathering in family context. In: Lamb ME, editor. The role of the father in child development. 5. Hoboken, NJ: Wiley; 2010. pp. 154–176. [Google Scholar]
- Daly JM, Fritsch SL. Case study: Maternal residual attention deficit disorder associated with failure to thrive in a two-month-old infant. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:55–57. doi: 10.1097/00004583-199501000-00014. [DOI] [PubMed] [Google Scholar]
- Darling N, Steinberg L. Parenting style as context: An integrative model. Psychological Bulletin. 1993;113:487–496. [Google Scholar]
- Deater-Deckard K, Sewell MD, Petrill SA, Thompson LA. Maternal working memory and reactive negativity in parenting. Psychological Science. 2010;21:75–79. doi: 10.1177/0956797609354073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deault LC. A systematic review of parenting in relation to the development of comorbidities and functional impairments in children with attention-deficit/hyperactivity disorder (ADHD) Child Psychiatry and Human Development. 2010;41:168–192. doi: 10.1007/s10578-009-0159-4. [DOI] [PubMed] [Google Scholar]
- Downer J, Campos R, McWayne C, Gartner T. Father involvement and children’s early learning: A critical review of published empirical work from the past 15 years. Marriage and Family Review. 2008;43:67–108. [Google Scholar]
- Eakin L, Minde K, Hechtman L, Ochs E, Krane E, Bouffard R, et al. The marital and family functioning of adults with ADHD and their spouses. Journal of Attention Disorders. 2004;8:1–10. doi: 10.1177/108705470400800101. [DOI] [PubMed] [Google Scholar]
- Edel MA, Juckel G, Brune M. Interaction of recalled parental ADHD symptoms and rearing behavior with current attachment and emotional dysfunction in adult offspring with ADHD. Psychiatry Research. 2010;178:137–141. doi: 10.1016/j.psychres.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Ellis B, Nigg J. Parenting practices and attention-deficit/hyperactivity disorder: New findings suggest partial specificity of effects. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:146–154. doi: 10.1097/CHI.0b013e31819176d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SW, Vallano G, Pelham W. Treatment of parenting behavior with a psychostimulant: A case study of an adult with attention-deficit hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology. 1994;4:63–69. [Google Scholar]
- Faraone SV, Biederman J. What is the prevalence of adult ADHD? Results of a population screen of 966 adults. Journal of Attention Disorders. 2005;9:384–391. doi: 10.1177/1087054705281478. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychological Medicine. 2006;36:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Spencer T, Aleardi M, Pagano C, Beiderman J. Meta-analysis of the efficacy of methylphenidate for treating adult Attention-Deficit/Hyperactivity Disorder. Journal of Clinical Psychopharmacology. 2004;24:24–29. doi: 10.1097/01.jcp.0000108984.11879.95. [DOI] [PubMed] [Google Scholar]
- Fayyad J, de Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, et al. Cross-national prevalence and correlates of adult attention-deficit hyper-activity disorder. The British Journal of Psychiatry. 2007;190:402–409. doi: 10.1192/bjp.bp.106.034389. [DOI] [PubMed] [Google Scholar]
- Greshon J. A meta-analytic review of gender differences in ADHD. Journal of Attention Disorders. 2002;5:143–154. doi: 10.1177/108705470200500302. [DOI] [PubMed] [Google Scholar]
- Griggs MS, Mikami AY. The role of maternal and child ADHD symptoms in shaping interpersonal relationships. Journal of Abnormal Child Psychology. 2011;39:437–449. doi: 10.1007/s10802-010-9464-4. [DOI] [PubMed] [Google Scholar]
- Harvey E, Danforth JS, Eberhardt McKee T, Ulaszek WR, Friedman JL. Parenting of children with Attention-Deficit/Hyperactivity Disorder (ADHD): The role of parental ADHD symptomatology. Journal of Attention Disorders. 2003;7:31–42. doi: 10.1177/108705470300700104. [DOI] [PubMed] [Google Scholar]
- Healey DM, Gopin CB, Grossman BR, Campbell SB, Halperin JM. Mother–child dyadic synchrony is associated with better functioning in hyperactive inattentive preschool children. Journal of Child Psychology and Psychiatry. 2010;51:1058–1066. doi: 10.1111/j.1469-7610.2010.02220.x. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Kraemer HC, Krueger RF. The feasibility and need for dimensional psychiatric diagnoses. Psychological Medicine. 2006;36:1671–1680. doi: 10.1017/S003329170600821X. [DOI] [PubMed] [Google Scholar]
- Hoza B, Johnston C, Pillow DR, Ascough JC. Predicting treatment response for childhood attention-deficit/hyperactivity disorder: Introduction of a heuristic model to guide research. Applied and Preventive Psychology. 2006;11:215–229. [Google Scholar]
- Humphreys KL, Mehta N, Lee SS. Association of parental ADHD and depression With externalizing and internalizing dimensions of child psychopathology. Journal of Attention Disorders. 2010 doi: 10.1177/1087054710387264. (Electronic publication ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen PS, Arnold LE, Swanson JM, Vitiello B, Abikoff HB, Greenhill LL, et al. 3-year follow-up of the NIMH MTA study. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:989–1002. doi: 10.1097/CHI.0b013e3180686d48. [DOI] [PubMed] [Google Scholar]
- Jiang Y, Johnston C. The relations of self- and other reports of ADHD symptoms to competence. Journal of Attention Disorders. 2011 doi: 10.1177/1087054710392541. (Electronic publication ahead of print) [DOI] [PubMed] [Google Scholar]
- Johnston C. The impact of attention deficit hyperactivity disorder on social and vocational functioning in adults. In: Jensen PS, Cooper JR, editors. Attention deficit hyperactivity disorder: State of the science-best practices. Kingston, NJ: Civic Research Institute; 2002. pp. 6-1–6-21. [Google Scholar]
- Johnston C, Lee-Flynn S. Family functioning. In: Hoza B, Evan SW, editors. Treating attention-deficit/hyperactivity disorder. Kingston, NJ: Civic Research Institute; 2011. pp. 17-1–17-19. [Google Scholar]
- Johnston C, Lee-Flynn S. In: Coles EK chairman, editor. Parents’ attributions for child behavior: Relations to parent and child ADHD symptoms; Gender differences in the clinical presentation, treatment and outcome of children with ADHD, Symposium presented at the Association for Behavioral and Cognitive Therapies; Toronto. 2011b. Nov, [Google Scholar]
- Johnston C, Mash EJ. Families of children with Attention-Deficit/Hyperactivity Disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4:183–207. doi: 10.1023/a:1017592030434. [DOI] [PubMed] [Google Scholar]
- Johnston C, Murray C, Hinshaw SP, Pelham WE, Jr, Hoza B. Responsiveness in interactions of mothers and sons with ADHD: Relations to maternal and child characteristics. Journal of Abnormal Child Psychology. 2002;30:77–88. doi: 10.1023/a:1014235200174. [DOI] [PubMed] [Google Scholar]
- Johnston C, Scoular DJ, Ohan JL. Mothers’ reports of parenting in families of children with symptoms of Attention-Deficit/Hyperactivity Disorder: Relations to impression management. Child and Family Behavior Therapy. 2004;26:45–61. [Google Scholar]
- Jokela M, Power C, Kivimäki M. Childhood problem behaviors and injury risk over the life course. Journal of Child Psychology and Psychiatry. 2009;50:1541–1549. doi: 10.1111/j.1469-7610.2009.02122.x. [DOI] [PubMed] [Google Scholar]
- Kendziora KT, O’Leary SG. Dysfunctional parenting as a focus for prevention and treatment of child behavior problems. Advances in Clinical Child Psychology. 1993;15:175–206. [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey replication. The American Journal of Psychiatry. 2006;163:716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Green JG, Adler LA, Barkley RA, Chatterji S, Faraone SV, et al. Structure and diagnosis of adult attention-deficit/hyperactivity disorder: Analysis of expanded symptom criteria from the adult ADHD clinical diagnostic scale. Archives of General Psychiatry. 2010;67:1168–1178. doi: 10.1001/archgenpsychiatry.2010.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kryski KR, Mash EJ, Ninowski JE, Semple DL. Maternal symptoms of attention-deficit/hyperactivity disorder and maternal language: Implications for infant language development. Journal of Child and Family Studies. 2010;19:270–277. [Google Scholar]
- Lahey BB, Rathouz PJ, Lee SS, Chronis-Tuscano A, Pelham WE, Waldman ID, et al. Interactions between early parenting and a polymorphism of the child’s dopamine transporter gene in predicting future child conduct disorder symptoms. Journal of Abnormal Psychology. 2011;120:33–45. doi: 10.1037/a0021133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb ME, Tamis-LeMonda CS. The role of the father: An introduction. In: Lamb ME, editor. The role of the father in child development. 4. Hoboken, NJ: John Wiley & Sons; 2004. pp. 1–31. [Google Scholar]
- Landau R, Amiel-Laviad R, Berger A, Atzaba-Poria N, Auerbach JG. Parenting of 7-month-old infants at familial risk for ADHD during infant’s free play, with restrictions on interaction. Infant Behavior & Development. 2009;32:173–182. doi: 10.1016/j.infbeh.2008.12.007. [DOI] [PubMed] [Google Scholar]
- Landau R, Avital M, Berger A, Atzaba-Poria N, Arbelle S, Faroy M, et al. Parenting of 7-month-old infants at familial risk for attention-deficit/hyperactivity disorder. Infant Mental Health Journal. 2010;31:141–158. doi: 10.1002/imhj.20249. [DOI] [PubMed] [Google Scholar]
- Landau R, Sadeh A, Vassoly P, Berger A, Atzaba-Poria N, Auerbach JG. Sleep patterns of 7-week-old infants at familial risk for attention deficit hyperactivity disorder. Infant Mental Health Journal. 2010;31:630–646. doi: 10.1002/imhj.20275. [DOI] [PubMed] [Google Scholar]
- Lee SS, Chronis-Tuscano A, Keenan K, Pelham WE, Loney J, Van Hulle CA, et al. Association of maternal dopamine transporter genotype with negative parenting: Evidence for gene×environment interaction with child disruptive behavior. Molecular Psychiatry. 2010;15:548–558. doi: 10.1038/mp.2008.102. [DOI] [PubMed] [Google Scholar]
- Luman M, Oosterlaan J, Sergeant JA. The impact of reinforcement contingencies on AD/HD: A review and theoretical appraisal. Clinical Psychology Review. 2005;25:183–213. doi: 10.1016/j.cpr.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Lytton H, Romney DM. Parents’ differential socialization of boys and girls: A meta-analysis. Psychological Bulletin. 1991;109:267–296. [Google Scholar]
- Mannuzza S, Castellanos FX, Roizen ER, Hutchison JA, Lashua EC, Klein RG. Impact of the impairment criterion in the diagnosis of adult ADHD: 33-year follow-up study of boys with ADHD. Journal of Attention Disorders. 2011;15:122–129. doi: 10.1177/1087054709359907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus DK, Barry TD. Does attention-deficit/hyperactivity disorder have a dimensional latent structure? A taxometric analysis. Journal of Abnormal Psychology. 2010;120:427–442. doi: 10.1037/a0021405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM. Research review: A new perspective on attention-deficit hyper-activity disorder: Emotion dysregulation and trait models. Journal of Child Psychology and Psychiatry. 2009;50:1042–1051. doi: 10.1111/j.1469-7610.2009.02105.x. [DOI] [PubMed] [Google Scholar]
- Martel MM, Nikolas M, Jernigan K, Friderici K, Waldman I, Nigg JT. The dopamine receptor D4 gene (DRD4) moderates family environmental effects on ADHD. Journal of Abnormal Child Psychology. 2011;39:1–10. doi: 10.1007/s10802-010-9439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGough JJ, Barkley RA. Diagnostic controversies in adult attention deficit hyperactivity disorder. The American Journal of Psychiatry. 2004;161:1948–1956. doi: 10.1176/appi.ajp.161.11.1948. [DOI] [PubMed] [Google Scholar]
- Mick E, Faraone SV, Biederman J, Spencer TJ. The course and outcome of attention-deficit/hyperactivity disorder. Primary Psychiatry. 2004;11:42–48. [Google Scholar]
- Miller TW, Nigg JT, Faraone SV. Axis I and II comorbidity in adults with ADHD. Journal of Abnormal Psychology. 2007;116:519–528. doi: 10.1037/0021-843X.116.3.519. [DOI] [PubMed] [Google Scholar]
- Miller TW, Nigg JT, Miller RL. Attention-deficit/hyperactivity disorder in African American children: What can be concluded from the past ten years? Clinical Psychology Review. 2009;29:77–86. doi: 10.1016/j.cpr.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minde K, Eakin L, Hechtman L, Ochs E, Bouffard R, Greenfield B, et al. The psychosocial functioning of children and spouses of adults with ADHD. Journal of Child Psychology and Psychiatry. 2003;44:637–646. doi: 10.1111/1469-7610.00150. [DOI] [PubMed] [Google Scholar]
- Mokrova I, O’Brien M, Calkins S, Keane S. Parental ADHD symptomology and ineffective parenting: The connecting link of home chaos. Parenting: Science and Practice. 2010;10:119–135. doi: 10.1080/15295190903212844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy K, Barkley RA. Attention deficit hyperactivity disorder adults: Comorbidities and adaptive impairments. Comprehensive Psychiatry. 1996;37:393–401. doi: 10.1016/s0010-440x(96)90022-x. [DOI] [PubMed] [Google Scholar]
- Murray C, Johnston C. Parenting in mothers with and without attention-deficit/hyperactivity disorder. Journal of Abnormal Psychology. 2006;115:52–61. doi: 10.1037/0021-843X.115.1.52. [DOI] [PubMed] [Google Scholar]
- Nigg JT. Attention-deficit/hyperactivity disorder: Endophenotypes, structure, and etiological pathways. Current Directions in Psychological Science. 2010;19:24–29. [Google Scholar]
- Nigg JT, Nikolas M, Burt SA. Measured gene-by-environment interaction in relation to attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:863–873. doi: 10.1016/j.jaac.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT, Tannock R, Rohde LA. What is to be the fate of ADHD subtypes? An introduction to the special section on research on the ADHD subtypes and implications for the DSM-V. Journal of Clinical Child and Adolescent Psychology. 2010;39:723–725. doi: 10.1080/15374416.2010.517171. [DOI] [PubMed] [Google Scholar]
- Nikolas M, Friderici K, Waldman I, Jernigan K, Nigg JT. Gene×environment interactions for ADHD: Synergistic effect of 5HTTLPR genotype and youth appraisals of inter-parental conflict. Behavioral and Brain Functions. 2010;6:23. doi: 10.1186/1744-9081-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ninowski JE, Mash EJ, Benzies KM. Symptoms of Attention-Deficit/Hyperactivity Disorder in first-time expectant women: Relations with parenting cognitions and behaviors. Infant Mental Health Journal. 2007;28:54–75. doi: 10.1002/imhj.20122. [DOI] [PubMed] [Google Scholar]
- Obradovic J, Bush NR, Stamperdahl J, Adler NE, Boyce WT. Biological sensitivity to context: The interactive effects of stress reactivity and family adversity on socioemotional behavior and school readiness. Child Development. 2010;81:270–289. doi: 10.1111/j.1467-8624.2009.01394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkhardt EH, Kassubek J, Brummer D, Koelch M, Ludolph AC, Fegert JM, et al. Intensified testing for attention-deficit hyperactivity disorder (ADHD) in girls should reduce depression and smoking in adult females and the prevalence of ADHD in the longterm. Medical Hypotheses. 2009;72:409–412. doi: 10.1016/j.mehy.2008.11.025. [DOI] [PubMed] [Google Scholar]
- Pressman LJ, Loo SK, Carpenter EM, Asarnow JR, Lynn D, McCracken JT, et al. Relationship of Family Environment and Parental Psychiatric Diagnosis to Impairment in ADHD. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:346–354. doi: 10.1097/01.chi.0000192248.61271.c8. [DOI] [PubMed] [Google Scholar]
- Propper C, Moore GA, Mills-Koonce WR, Halpern CT, Hill-Soderlund AL, Calkins SD, et al. Gene–environment contributions to the development of infant vagal reactivity: The interaction of dopamine and maternal sensitivity. Child Development. 2008;79:1377–1394. doi: 10.1111/j.1467-8624.2008.01194.x. [DOI] [PubMed] [Google Scholar]
- Psychogiou L, Daley D, Thompson M, Sonuga-Barke E. Testing the interactive effect of parent and child ADHD on parenting in mothers and fathers: A further test of the similarity-fit hypothesis. British Journal of Developmental Psychology. 2007;25:419–433. [Google Scholar]
- Psychogiou L, Daley D, Thompson MJ, Sonuga-Barke EJS. Parenting empathy: Associations with dimensions of parent and child psychopathology. British Journal of Developmental Psychology. 2008;26:221–232. [Google Scholar]
- Rapport MD, Alderson RM, Kofler MJ, Sarver DE, Bolden J, Sims V. Working memory deficits in boys with attention-deficit/hyperactivity disorder (ADHD): The contribution of central executive and subsystem processes. Journal of Abnormal Child Psychology. 2008;36:825–837. doi: 10.1007/s10802-008-9215-y. [DOI] [PubMed] [Google Scholar]
- Rothbaum F, Weisz JR. Parental caregiving and child externalizing behavior in nonclinical samples: A meta-analysis. Psychological Bulletin. 1994;116:55–74. doi: 10.1037/0033-2909.116.1.55. [DOI] [PubMed] [Google Scholar]
- Rubia K. “Cool” inferior frontostriatal dysfunction in attention-deficit/hyperactivity disorder versus “hot” ventromedial orbitofrontal-limbic dysfunction in conduct disorder: A review. Biological Psychiatry. 2010;69:e69–e87. doi: 10.1016/j.biopsych.2010.09.023. [DOI] [PubMed] [Google Scholar]
- Safren SA, Sprich S, Chulvick S, Otto MW. Psychosocial treatments for adults with attention-deficit/hyperactivity disorder. Psychiatric Clinics of North America. 2004;27:349–360. doi: 10.1016/S0193-953X(03)00089-3. [DOI] [PubMed] [Google Scholar]
- Safren SA, Sprich S, Mimiaga MJ, Surman C, Knouse L, Groves M, et al. Cognitive behavioral therapy vs relaxation with educational support for medication-treated adults with ADHD and persistent symptoms: A randomized controlled trial. Journal of the American Medical Association. 2010;304:875–880. doi: 10.1001/jama.2010.1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagvolden T, Aase H, Johansen EB, Russell VA. A dynamic developmental theory of attention-deficit/hyperactivity disorder (ADHD) predominantly hyperactive/impulsive and combined subtypes. The Behavioral and Brain Sciences. 2005;28:397–468. doi: 10.1017/S0140525X05000075. [DOI] [PubMed] [Google Scholar]
- Sanders MR. Triple P-Positive Parenting Program as a public health approach to strengthening parenting. Journal of Family Psychology. 2008;22:506–517. doi: 10.1037/0893-3200.22.3.506. [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Hodgens JB, Sterling S. How mothers parent their children with behavior disorders: Implications for unintentional injury risk. Journal of Safety Research. 2006;37:167–173. doi: 10.1016/j.jsr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Seipp CM, Johnston C. Mother–son interactions in families of boys with Attention-Deficit/Hyperactivity Disorder with and without oppositional behavior. Journal of Abnormal Child Psychology. 2005;33:87–98. doi: 10.1007/s10802-005-0936-x. [DOI] [PubMed] [Google Scholar]
- Semple DL, Mash EJ, Ninowski JE, Benzies KM. The relation between maternal symptoms of attention-deficit/hyperactivity disorder and mother-infant interaction. Journal of Child and Family Studies. 2011;20:460–472. [Google Scholar]
- Shaw P, Eckstrand K, Sharp W, Blumenthal J, Lerch JP, Greenstein D, et al. Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. PNAS Proceedings of the National Academy of Sciences of the United States of America. 2007;104:19649–19654. doi: 10.1073/pnas.0707741104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheese BE, Voelker PM, Rothbart MK, Posner MI. Parenting quality interacts with genetic variation in dopamine receptor D4 to influence temperament in early childhood. Development and Psychopathology. 2007;19:1039–1046. doi: 10.1017/S0954579407000521. [DOI] [PubMed] [Google Scholar]
- Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. Journal of Clinical Child Psychology. 1996;25:317–329. [Google Scholar]
- Shiels K, Hawk LW. Self-regulation in adhd: The role of error processing. Clinical Psychology Review. 2010;30:951–961. doi: 10.1016/j.cpr.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solanto MV, Marks DJ, Wasserstein J, Mitchell K, Abikoff H, Alvir JMJ, et al. Efficacy of meta-cognitive therapy for adult ADHD. The American Journal of Psychiatry. 2010;167:958–968. doi: 10.1176/appi.ajp.2009.09081123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonuga-Barke EJS. The dual pathway model of AD/HD: An elaboration of neuro-developmental characteristics. Neuroscience and Biobehavioral Reviews. 2003;27:593–604. doi: 10.1016/j.neubiorev.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Daley D, Thompson M. Does maternal ADHD reduce the effectiveness of parent training for preschool children’s ADHD? Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:696–702. doi: 10.1097/00004583-200206000-00009. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Halperin JM. Developmental phenotypes and causal pathways in attention deficit hyperactivity disorder: Potential targets for early intervention? Journal of Child Psychology and Psychiatry. 2010;51:368–389. doi: 10.1111/j.1469-7610.2009.02195.x. [DOI] [PubMed] [Google Scholar]
- Thapar A, van den Bree M, Fowler T, Langley K, Whittinger N. Predictors of antisocial behaviour in children with attention deficit hyperactivity disorder. European Child & Adolescent Psychiatry. 2006;15:118–125. doi: 10.1007/s00787-006-0511-1. [DOI] [PubMed] [Google Scholar]
- Watkins SJ, Mash EJ. Sub-clinical levels of symptoms of attention-deficit/hyperactivity disorder and self-reported parental cognitions and behaviours in mothers of young infants. Journal of Reproductive and Infant Psychology. 2009;27:70–88. [Google Scholar]
- Weinstein CS, Apfel RJ, Weinstein SR. Description of mothers with ADHD with children with ADHD. Psychiatry: Interpersonal and Biological Processes. 1998;61:12–19. doi: 10.1080/00332747.1998.11024815. [DOI] [PubMed] [Google Scholar]
- Weiss M, Hechtman L, Weiss G. ADHD in parents. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1059–1061. doi: 10.1097/00004583-200008000-00023. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Bidwell LC. Neuropsychology of Attention-Deficit/Hyperactivity Disorder: Implications for assessment and treatment. In: Evans SW, Hoza B, editors. Treating Attention-Deficit/Hypearctivity Disorder. Kingston, New Jersey: Civic Research Instiute; 2011. pp. 6-2–6-18. [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry. 2005;57:1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- Zelazo PD, Qu L, Kesek AC, Calkins SD, Bell MA. Hot executive function: Emotion and the development of cognitive control. In: Calkins SD, Bell MA, editors. Child development at the intersection of emotion and cognition. Washington, DC: American Psychological Association; 2010. pp. 97–111. [Google Scholar]