Abstract
We report a patient with stage IIIB Kienböck disease treated with radial shortening where preoperative and sequential postoperative imaging were done using in vivo high-resolution peripheral quantitative micro–computed tomography (micro-CT) scan. Sequential in vivo micro-CT scan analysis of a target zone of the Kienböck lunate of this patient demonstrated early signs of lunate remodeling (bone trabecular densification) at 5-month follow-up suggesting an ongoing healing process. These early remodeling micro-CT scan signs were confirmed at 5 years' follow-up as well.
Keywords: lunate, Kienböck disease, quantitative micro-CT scan, HR-pQCT
The natural history of Kienböck disease shows a progressive lunate collapse that is currently staged using Lichtman classification on conventional X-rays.1 2 3 However, because very little is known about the etiology and physiopathology of Kienböck disease, the use of sophisticated imaging modalities is critical in the hope that new information can be brought up from new imaging technologies.4 This is especially true if correlations can be made with treatment modalities and clinical status. Magnetic resonance imaging is used for diagnosis at the early stages. Conventional computed tomography (CT) scan is used at any stages to assess lunate morphology, diagnose fragmentation, and follow the results of various lunate-preserving treatments.5 Arthroscopy is used to assess the cartilage status before surgery.6
In vitro micro-CT scan studies have been recently performed on lunates with stage IIIB Kienböck disease that was harvested during proximal row carpectomy. Lunates from embalmed cadavers were used as controls. The use of these micro-CT techniques is currently limited by the conflict between the spatial resolution and the radiation dose. High-resolution peripheral quantitative micro-CT (HR-pQCT) is a new imaging technique that was recently introduced to allow in vivo noninvasive assessment of bony trabecular microstructure in osteoporosis7 and various diseases.7 8 9
In this case report, the HR-pQCT imaging was used to evaluate the bony trabecular microstructure of the lunate in a patient with Kienböck disease before and after radial shortening. The contralateral normal lunate was used as a control.
Case Report
A 27-year-old white-collar woman involved in leisure sports activities (mainly skiing) was referred to our clinic with a history of progressive incapacitating chronic pain in her right dominant wrist for a 6 months' period. She could not recall any traumatic onset or wrist overuse event. At the time of clinical examination, visual analog scale pain was 55/100 at rest and 85/100 with active wrist flexion-extension. Neither wrist rest nor wrist splinting provided any clinical improvement. Clinical examination revealed dorsal-central right wrist swelling as well as severe local tenderness. Active wrist flexion (20 degrees) and extension (20 degrees) were markedly limited. There was no active radial deviation, and active ulnar deviation was only 10 degrees. There was moderate pain and mild stiffness in forearm rotation (pronation 60 degrees, supination 60 degrees). Grip strength (Jamar dynamometer, Lafayette Instrument, Lafayette, IN) was 10 kg (43% of the opposite normal side). The modified Mayo score10 (10 points) and Lyon11 (25 points) right wrist scores were poor.
Standardized posteroanterior (PA) and lateral wrist radiographs revealed a typical Lichtman stage IIIB Kienböck disease (Fig. 1) with negative ulnar variance (−3 mm) on the right side. The radiological aspect of the contralateral asymptomatic lunate was normal. Conventional CT scan confirmed advanced fragmentation of the lunate.
Fig. 1.
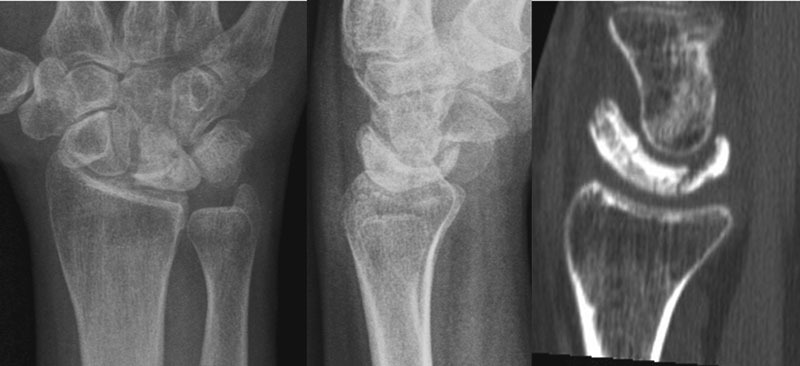
Preoperative PA and lateral standard radiographs and conventional CT scan (sagittal slice) of Kienböck right lunate of our patient.
After informed consent of the patient and of the local ethical committee, in vivo HR-pQCT imaging (XtremeCT; Scanco Medical AG, Brüttisellen, Switzerland) was performed to investigate both the right lunate with Kienböck disease and the contralateral normal lunate as a control. A total of 220 parallel axial, coronal, and sagittal slices with an isotropic voxel size of 82 μm were performed on both wrists. For trabecular microstructure analysis, a cylindrical volume of interest (VOI) perpendicular to the sagittal plane was isolated (length 3 mm, diameter 3 mm) within the dorsal half of both Kienböck and contralateral normal lunates. Morphological and trabecular HR-pQCT microstructural parameters of both Kienböck and control lunates are shown in Table 1. Morphological parameters reflected advanced right lunate's collapse. Trabecular parameters showed that trabecular bone volume fraction and trabeculae number per square millimeter were markedly decreased in Kienböck lunate. Trabecular separation was markedly increased. By contrast, trabecular thickness remained similar.
Table 1. In vivo lunate morphological and trabecular parameters in our patient with right Kienböck disease compared with contralateral left normal lunate. Evolution of parameters after radial shortening.
| In vivo normal contralateral lunate | In vivo Kienböck lunate | In vivo Kienböck lunate 5 months after radial shortening | In vivo Kienböck lunate 5 years after radial shortening | |
|---|---|---|---|---|
| Morphological parameters | ||||
| Sagittal tip to tip distance (mm) | 11.1 | 16.1 | 15.4 | 15.7 |
| Total lunate body height (mm) | 11 | 10.3 | 10.5 | 9.9 |
| Central lunate body height (mm) | 6.8 | 4.5 | 4.1 | 4.1 |
| Trabecular parameters (VOI) | ||||
| BV/TV (%) | 44.2 | 25.9 | 28 | 60 |
| Tb.N per mm2 | 1.91 | 1.16 | 1.56 | 2.55 |
| Tb.Sp (µm) | 438 | 934 | 680 | 295 |
| Tb.Th (µm) | 278 | 266 | 261 | 304 |
Abbreviations: BV/TV, trabecular bone volume fraction; Tb.N, number of trabeculae; Tb.Sp, trabecular separation, i.e., distance between trabeculae; Tb.Th, trabecular thickness; VOI, volume of interest i.e., cylindrical sample of the lunate used for HR-pQCT evaluation.
Because of the negative ulnar variance, surgical treatment with radial shortening was elicited. A 2-mm diaphyseal radial shortening was performed through a classic volar approach by the senior author (G.H.) of this article. The immediate follow-up was uneventful. Postoperatively, a short arm splint was worn for 3 weeks followed by gentle progressive active and passive wrist motion. The patient was prospectively followed with sequential clinical examinations, standard radiographs, conventional CT scans, and micro-CT scan.
At 5 months' follow-up, wrist pain had improved dramatically, allowing pain-free activities of daily living including driving and return to skiing. Standard radiographs showed satisfactory bone healing at the osteotomy site and showed a 2-mm radial shortening compared with the preoperative radiographs. In terms of aspect of the lunate, neither wrist standard radiographs nor conventional CT scan showed any differences compared with the preoperative work-up. HR-pQCT morphological parameters (Table 1) showed similar values, which showed stabilization of Kienböck lunate collapse. Trabecular parameters (Table 1) showed an increase in trabecular bone volume fraction and trabeculae number per square millimeter, suggesting an early bone healing process in the VOI of the dorsal part of the lunate. Trabecular separation had decreased, whereas trabecular thickness remained similar.
At 5 years' follow-up, the patient did not report any residual pain and was fully able to perform sports activities such as skiing. On physical examination, active wrist flexion-extension arc (105 degrees) was markedly improved. Active radial deviation (10 degrees) and ulnar deviation (25 degrees) were improved. The range of active forearm rotation was 160 degrees. Grip strength was 24 kg (83% of the opposite nondominant side). The Mayo (75%, +65 points) and Lyon wrist score (88%, +56 points) were markedly improved (Fig. 2). Standardized PA and lateral wrist radiographs as well as conventional CT scan showed that the lunate was still fragmented (Fig. 3). Compared with the preoperative values, HR-pQCT morphological parameters (Table 1) showed similar values, confirming that the Kienböck lunate did not increase its collapse.
Fig. 2.
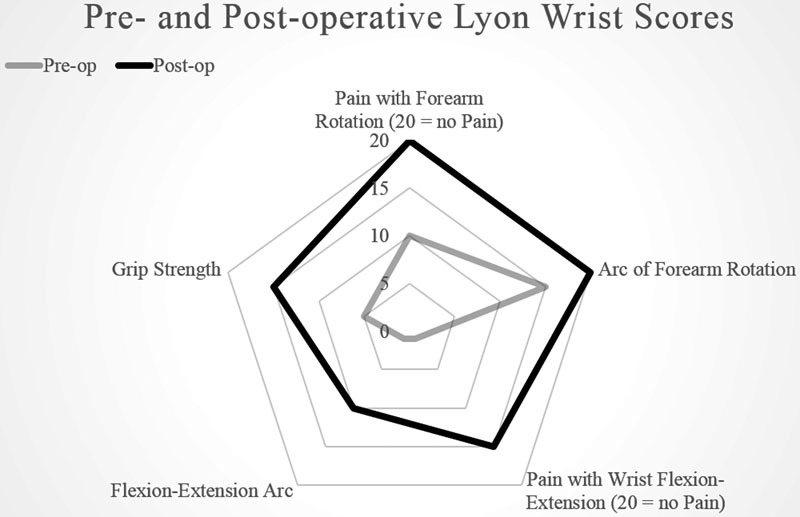
Diagrammatic patterns of Lyon pre- and postoperative (5 years follow up) wrist scores in our patient.
Fig. 3.
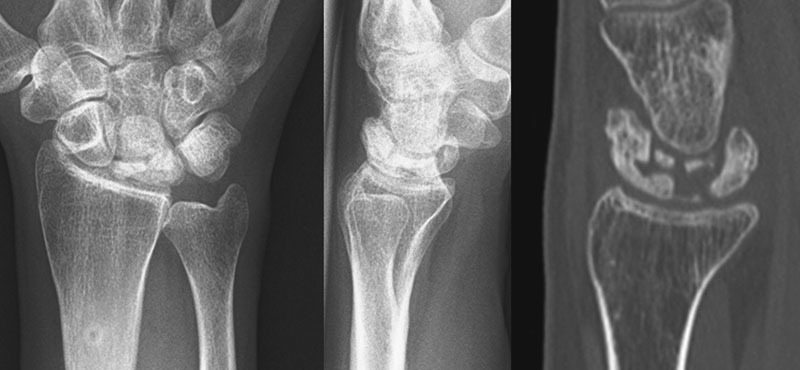
Postoperative 5 years' follow-up PA and lateral standard radiographs and conventional CT scan (sagittal slice) of Kienböck right lunate of our patient. Note the 2-mm radius shortening and the stabilization of the collapse.
Trabecular parameters (Table 1) showed a dramatic progression in terms of trabecular bone volume fraction and trabeculae number per square millimeter, suggesting further bone healing process in the VOI compared with the 5 months' status. Similarly, trabecular separation had further decreased, whereas trabecular thickness remained grossly similar (Fig. 4).
Fig. 4.
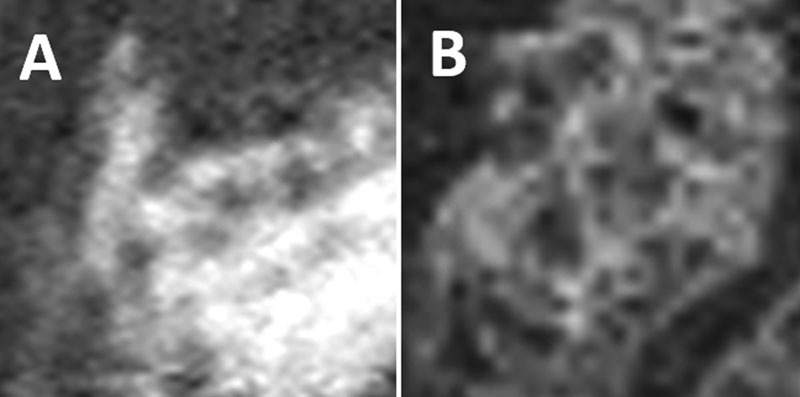
Trabecular microstructure as observed with HR-pQCT within Kienböck lunate VOI from preoperative (A) to 5 years' follow-up (B).
Discussion
Radial shortening osteotomy has been widely performed to successfully treat patients with Kienböck disease associated with negative ulnar variance.12 Radial shortening osteotomy is a unique model of lunate-preserving surgery that may be used to analyze wrist-specific pre- and postoperative changes, since the lunate itself is not involved by the surgical process.
We used a more recent micro-CT scan technology (HR-pQCT) that allowed an in vivo prospective follow-up imaging of the lunate of a patient with stage IIIB Kienböck disease before and after radius shortening. The contralateral asymptomatic normal lunate was used as a control.
The comparison of the in vivo micro-CT scan parameters of our Kienböck lunate with the in vitro findings of the Kienböck lunates excised in Low's previous studies6 13 14 15 revealed similar morphological values (Tables 1 and 2). As for the trabecular microstructure parameters, the trabecular bone volume fraction, trabeculae number, and trabecular thickness showed higher values in our in vivo Kienböck lunate, which may indicate a more severe lunate collapse in our patient. Trabecular separation was almost twice, which was coherent with a more severe Kienböck disease in our study.
Table 2. In vitro lunate morphological and trabecular parameters values found in Low et al's study.
| In vitro normal lunate from embalmed cadavers, average values |
In vitro Kienböck lunate, average values | |
|---|---|---|
| Morphological parameters | ||
| Sagittal tip to tip distance (mm) | 12.9 | 15.7 |
| Total lunate body height (mm) | 14.8 | 11.1 |
| Central lunate body height (mm) | 11.2 | 6.3 |
| Trabecular parameters (VOI) | ||
| BV/TV (%) | 10.4 | 46.2 |
| Tb.N per mm2 | 0.6 | 1.3 |
| Tb.Sp (µm) | 729 | 504 |
| Tb.Th (µm) | 179 | 362 |
Abbreviations: BV/TV, trabecular bone volume fraction; Tb.N, number of trabeculae; Tb.Sp, trabecular separation, i.e., distance between trabeculae; Tb.Th, trabecular thickness; VOI, volume of interest i.e., cylindrical sample of the lunate used for HR- pQCT evaluation.
The evolution of morphological HR-pQCT parameters in our patient's Kienböck lunate from the preoperative status to the 5 months' and 5 years' control showed almost the same values, suggesting that radial shortening had limited the collapse process (Table 1).
The evolution of trabecular HR-pQCT parameters (Table 1) showed a progressive increase in bone volume fraction and trabeculae number, suggesting a healing process with trabecular densification into the Kienböck lunate. At follow-up, there was less empty space as expressed by a much smaller trabecular separation value. Meanwhile, the trabecular thickness increased, which may suggest that remodeling of the lunate occurs after radial shortening, which is in favor of a healing mechanism.
In vivo HR-pQCT imaging technique demonstrated a high potential for analyzing in vivo morphological and trabecular microstructural changes of the lunate before and after surgery. Further studies are needed to confirm our in vivo findings about the fate of the microstructure of the Kienböck lunate after radial shortening.
Footnotes
Conflict of Interest None.
References
- 1.Dias J J, Lunn P. Ten questions on Kienbock's disease of the lunate. J Hand Surg Eur Vol. 2010;35(7):538–543. doi: 10.1177/1753193410373703. [DOI] [PubMed] [Google Scholar]
- 2.Irisarri C. Aetiology of Kienböck's disease. J Hand Surg [Br] 2004;29(3):281–287. doi: 10.1016/j.jhsb.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 3.Owers K L, Scougall P, Dabirrahmani D, Wernecke G, Jhamb A, Walsh W R. Lunate trabecular structure: a radiographic cadaver study of risk factors for Kienbock's disease [corrected] J Hand Surg Eur Vol. 2010;35(2):120–124. doi: 10.1177/1753193409103732. [DOI] [PubMed] [Google Scholar]
- 4.Makabe H, Iwasaki N, Kamishima T, Oizumi N, Tadano S, Minami A. Computed tomography osteoabsorptiometry alterations in stress distribution patterns through the wrist after radial shortening osteotomy for Kienböck disease. J Hand Surg Am. 2011;36(7):1158–1164. doi: 10.1016/j.jhsa.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Herzberg G, Mercier S, Charbonnier J P, Got P. Kienböck's disease in a 14-year-old gymnast: a case report. J Hand Surg Am. 2006;31(2):264–268. doi: 10.1016/j.jhsa.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 6.Bain G I, Durrant A. An articular-based approach to Kienbock avascular necrosis of the lunate. Tech Hand Up Extrem Surg. 2011;15(1):41–47. doi: 10.1097/BTH.0b013e31820e82e8. [DOI] [PubMed] [Google Scholar]
- 7.McCreadie B R, Goulet R W, Feldkamp L A, Goldstein S A. Hierarchical structure of bone and micro-computed tomography. Adv Exp Med Biol. 2001;496:67–83. doi: 10.1007/978-1-4615-0651-5_8. [DOI] [PubMed] [Google Scholar]
- 8.Kocijan R, Englbrecht M, Haschka J. et al. Quantitative and qualitative changes of bone in psoriasis and psoriatic arthritis patients. J Bone Miner Res. 2015;30(10):1775–1783. doi: 10.1002/jbmr.2521. [DOI] [PubMed] [Google Scholar]
- 9.Tsai J N, Uihlein A V, Burnett-Bowie S A. et al. Comparative effects of teriparatide, denosumab, and combination therapy on peripheral compartmental bone density, microarchitecture, and estimated strength: the DATA-HRpQCT Study. J Bone Miner Res. 2015;30(1):39–45. doi: 10.1002/jbmr.2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cooney W P, Linscheid R L, Dobyns J H. Triangular fibrocartilage tears. J Hand Surg Am. 1994;19(1):143–154. doi: 10.1016/0363-5023(94)90238-0. [DOI] [PubMed] [Google Scholar]
- 11.Herzberg G, Burnier M, Marc A, Izem Y. Primary wrist hemiarthroplasty for irreparable distal radius fracture in the independent elderly. J Wrist Surg. 2015;4(3):156–163. doi: 10.1055/s-0035-1558841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matsui Y, Funakoshi T, Motomiya M, Urita A, Minami M, Iwasaki N. Radial shortening osteotomy for Kienböck disease: minimum 10-year follow-up. J Hand Surg Am. 2014;39(4):679–685. doi: 10.1016/j.jhsa.2014.01.020. [DOI] [PubMed] [Google Scholar]
- 13.Aspenberg P, Wang J S, Jonsson K, Hagert C G. Experimental osteonecrosis of the lunate. Revascularization may cause collapse. J Hand Surg [Br] 1994;19(5):565–569. doi: 10.1016/0266-7681(94)90116-3. [DOI] [PubMed] [Google Scholar]
- 14.Low S C, Bain G I, Findlay D M, Eng K, Perilli E. External and internal bone micro-architecture in normal and Kienböck's lunates: a whole-bone micro-computed tomography study. J Orthop Res. 2014;32(6):826–833. doi: 10.1002/jor.22611. [DOI] [PubMed] [Google Scholar]
- 15.Han K J, Kim J Y, Chung N S, Lee H R, Lee Y S. Trabecular microstructure of the human lunate in Kienbock's disease. J Hand Surg Eur Vol. 2012;37(4):336–341. doi: 10.1177/1753193411422337. [DOI] [PubMed] [Google Scholar]


