Abstract
Background In the lack of consensus, surgeon-based preference determines how acute scaphoid fractures are classified. There is a great variety of classification systems with considerable controversies.
Purposes The purpose of this study was to provide an overview of the different classification systems, clarifying their subgroups and analyzing their popularity by comparing citation indexes. The intention was to improve data comparison between studies using heterogeneous fracture descriptions.
Methods We performed a systematic review of the literature based on a search of medical literature from 1950 to 2015, and a manual search using the reference lists in relevant book chapters. Only original descriptions of classifications of acute scaphoid fractures in adults were included. Popularity was based on citation index as reported in the databases of Web of Science (WoS) and Google Scholar. Articles that were cited <10 times in WoS were excluded.
Results Our literature search resulted in 308 potentially eligible descriptive reports of which 12 reports met the inclusion criteria. We distinguished 13 different (sub) classification systems based on (1) fracture location, (2) fracture plane orientation, and (3) fracture stability/displacement. Based on citations numbers, the Herbert classification was most popular, followed by the Russe and Mayo classifications. All classification systems were based on plain radiography.
Conclusions Most classification systems were based on fracture location, displacement, or stability. Based on the controversy and limited reliability of current classification systems, suggested research areas for an updated classification include three-dimensional fracture pattern etiology and fracture fragment mobility assessed by dynamic imaging.
Keywords: scaphoid, fracture, classification, Herbert, radiograph
Scaphoid fractures were first described in 1905 by Destot following the discovery of radiography.1 These fractures became notorious for their troublesome healing. In 1939, Cravener tried to clarify factors contributing to the establishment of scaphoid nonunion.2 He encouraged classifying scaphoid fractures taking age and location into account. “In discussing carpal scaphoid fractures, we must first arrive on a common ground. Is the fracture through the tuberosity, the waist, or the body? If it is through the tuberosity we can practically neglect it, for it will heal. If it is through the body it will not easily.” More than seven decades later, it seems that we still have not arrived on a common ground considering the numerous different scaphoid fracture classification systems available in the literature, each trying to improve prognosis and treatment selection. In the lack of consensus, surgeon-based preference determines how a fracture pattern is classified. Popular classification systems include the Herbert,3 Mayo,4 and Russe5 classifications, but there are many more and they present considerable controversies.
Scaphoid fractures should be characterized in a reliable and reproducible way that facilitates comparisons among different groups or among similar groups treated differently.6 The use of different classification systems, however, affects comparing outcomes of treatment methods among different clinical trials. An overview of the various classification systems and their subgroups can improve data comparison between studies.
The purpose of this study was to review different concepts and classifications of acute scaphoid fractures and their popularity by comparing citation indexes. As incidence rates of different fracture types may vary in the literature, our second purpose was to study incidence rates based on the original reports.
Materials and Methods
We conducted a two-step systematic search of medical literature from 1950 to 2015: an online search for original (digital or paper) articles and a manual search for original (digital or paper) articles using reference lists in relevant book chapters. The online systematic review and data extraction were performed by two independent reviewers (P. W. L. B. and T. D.). Disagreements were resolved by means of discussion, with arbitration of a third experienced reviewer (G. A. B.) when differences of opinion remained.
Eligibility Criteria Systematic Review
Inclusion criteria for the selection of manuscripts were: (1) original description of a novel classification of the acute scaphoid fracture in an adult population (18 years and older); (2) availability of a (translated) full-text copy of a manuscript online or paper version. We included all types of articles, including clinical, biomechanical, cadaveric, and imaging studies. Exclusion criteria were: (1) (original) description of an already existing classification of acute scaphoid fractures; (2) (original) description of wrist pathologies other than acute scaphoid fractures; (3) languages other than English, French, or German.
Literature Search and Study Selection
The search for articles was performed in Medline (PubMed) in September 2014, and an updated search in October 2015. The search strategy was developed with our academic medical librarian. We used Medical Subject Headings (MeSH) (= scaphoid bone) and MeSH Subheadings (= classification), using free search terms in title and abstract with truncation (=scaphoid fracture*; scaphoid bone fracture*; scaphoid) and using free search terms in all fields with truncation (= class*). This resulted in the following search in Medline: (“Scaphoid Bone”[Mesh] OR scaphoid fracture*[tiab] OR scaphoid bone fracture*[tiab] OR scaphoid[tiab]) AND (“classification” [Subheading] OR class*). We retrieved all titles and abstracts and assessed them for eligibility. If the eligibility criteria were met, full manuscripts were obtained and reviewed. We performed the online search from oldest to most recent article, to identify classifications that were already described.
In addition to online databases, 12 international comprehensive medical books7 8 9 10 11 12 13 14 15 16 17 18 regarding the hand, wrist, or scaphoid were available in our academic medical library and included book chapters concerning acute scaphoid fractures. One author (P. W. L. B) performed a manual search using these book chapters to find additional references. References were further screened in Medline using the same inclusion and exclusion criteria.
Quality Assessment
There are many different clinical, biomechanical, or radiological systems to describe and classify the different acute scaphoid fractures, each with its own characteristics and limitations. To our knowledge, no guidelines have yet been developed to assess the quality of these articles classifying acute scaphoid fractures. Therefore, we did not make a distinction between study design or image modalities used.
Citation Numbers
Classification systems were considered clinically relevant only when applicable to clinical practice. We used a threshold of >10 times cited in the database of Web of Science (WoS) for further inclusion in our systematic review. We used Google Scholar as an additional database to record the number of citations as second measure for popularity of the classifications.
Results
The online search resulted in 308 potentially eligible articles. Eight met our inclusion criteria. Our manual search resulted in four additional relevant articles (Fig. 1). We pooled two articles describing the original Herbert classification3 and a modified Herbert classification.19 In contrast, Bohler et al20 and Cooney et al4 each discussed two different classification systems. In total, 13 different classification systems were divided based on (1) fracture location, (2) fracture plane orientation, and (3) fracture stability/displacement.
Fig. 1.
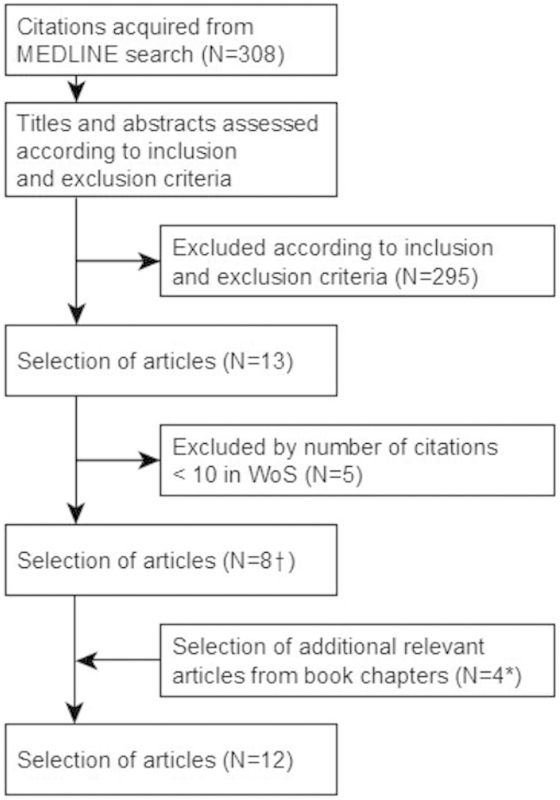
Study flow diagram of the systematic review. †Included eight references3 4 20 21 22 25 26 27; *included four references.5 6 19 28
Classifications based on fracture location (Table 1): Bohler et al20 described 873 conservatively treated fractures between 1925 and 1952. Tuberosity fractures showed 100% healing rate; all other fractures showed 97% rate. Proximal fractures were immobilized for 10 to 12 weeks, and middle and distal fractures for 6 to 8 weeks. Cooney et al4 (Mayo) (Fig. 2) and Schernberg et al21 (Fig. 3) also distinguished fractures by fracture location. Prosser et al22 classified solely distal fractures (Fig. 4). Osteoarthritis might develop in the scaphotrapezial trapezoidal joint due to malunion after compression fractures (type II). The AO foundation introduced a general fracture classification system.23 To standardize research and communication among surgeons, the Orthopaedic Trauma Association (OTA) adopted this latter system, resulting in the AO/OTA system (Fig. 5).6
Table 1. Classification of acute scaphoid fractures based on fracture location.
| Author | Year | No. of citation (World of Science; Google Scholar) | Total cases | Type | Rate (%) | |
|---|---|---|---|---|---|---|
| Bohler et ala | 1954 | 38; 67 | 873 | (1) | Tuberosity | 16 |
| (2)-a | Proximal third | 10 | ||||
| (2)-b | Border, middle/proximal third | 7 | ||||
| (2)-c | Middle third | 55 | ||||
| (2)-d | Middle third: wedge chipped out | 4 | ||||
| (2)-e | Distal third | 9 | ||||
| Cooney et al (Mayo) |
1980 | 110;330 | 45 | 1 | Tuberosity | ↑ |
| 2 | Distal articular surface | 16 | ||||
| 3 | Distal one-third | ↓ | ||||
| 4 | Waist, middle one-third | 67 | ||||
| 5 | Proximal pole | 18 | ||||
| Schernbergb | 1984 | 16;37 | 325 | I | Proximal pole | 4 |
| II, III, IV | Waist | 82 | ||||
| V | Distal Pole | 8 | ||||
| VI- a,b,c | Distal tubercle | 6 | ||||
| Prosser | 1988 | 13;29 | 37 | I | Tuberosity | 54 |
| II (A,B,C) | Distal intra-articular | 41,0,5 | ||||
| III | Osteochondral fracture | 0 | ||||
| AO/OTA | 2007 | N/Ac | x | 72-A1 | Proximal pole, noncomminuted | x |
| 72-A2 | Waist, noncomminuted | x | ||||
| 72-A3 | Distal pole, noncomminuted | x | ||||
| 72-B2 | Waist, comminuted | x | ||||
German article.
French article.
Not applicable, since the article comprised fracture classification systems of the entire musculoskeletal system.
Fig. 2.
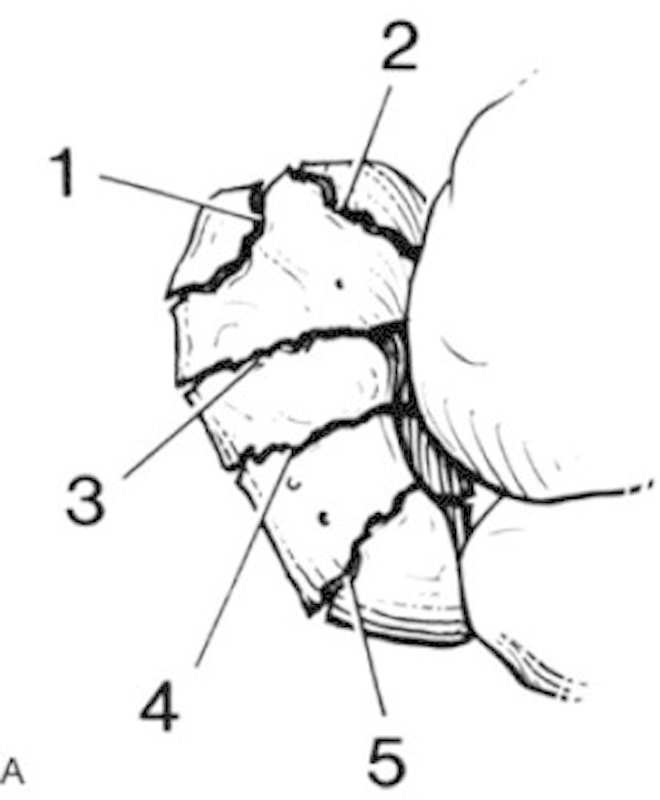
Cooney (Mayo) divided scaphoid fractures into fractures of the distal tubercle (1), distal intra-articular surface (2), distal third (3), waist (4), and proximal pole (5). Fracture location influenced both tendency and time frame for healing. (Reprinted, with permission covered by STM guidelines, from Cooney et al.13)
Fig. 3.
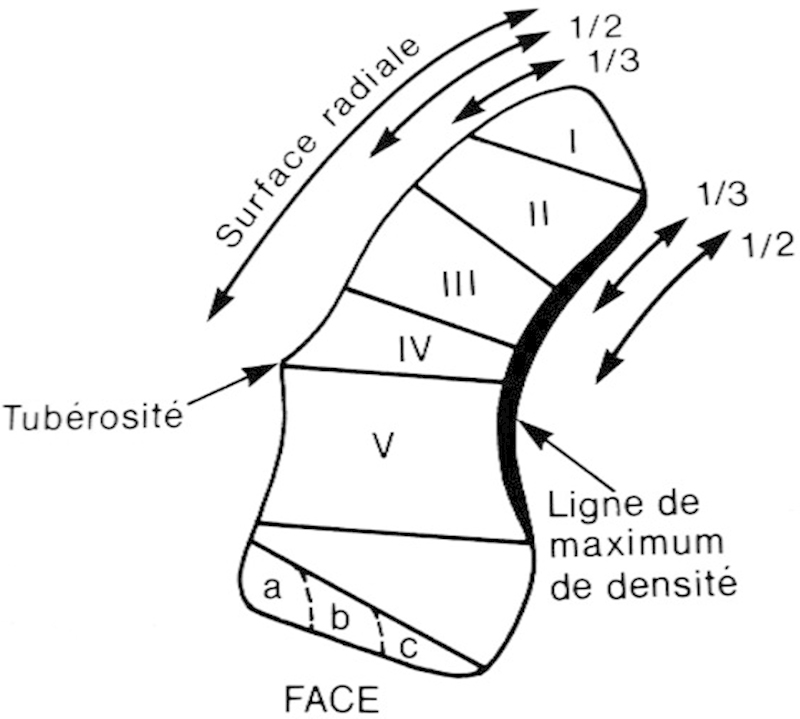
Schernberg distinguished six fracture types (I–VI) ranging from the proximal pole to the distal tubercle using the lateral tuberosity and the radial and medial articular surfaces as references. Distal tubercle fractures were further divided into small (a), intermediate (b), or large (c) fragments, and were considered likely to heal successfully, contrary to proximal fractures. (Reprinted, with permission of authors, from Schernberg et al.21)
Fig. 4.
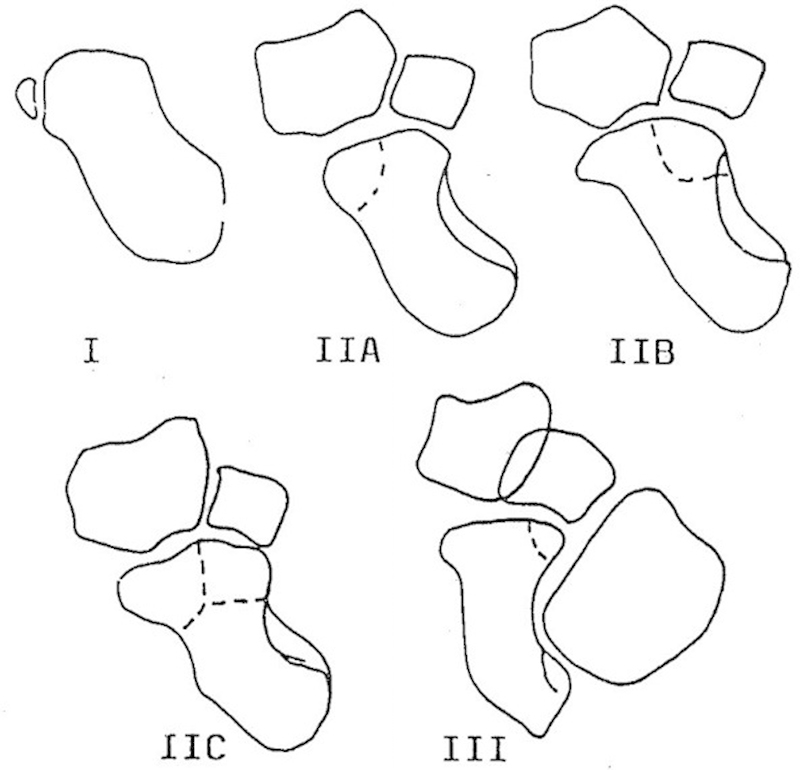
Prosser divided distal fractures into avulsion fractures of the tuberosity (I), intra-articular compression fractures of the scaphotrapezial trapezoidal joint including involvement of the radial half (IIA), ulnar half (IIB), or a combination (IIC), and osteochondral fractures at the capitate border (III). All distal fractures were treated by plaster cast. (Reprinted, with permission from Sage publisher, from Prosser et al.22)
Fig. 5.
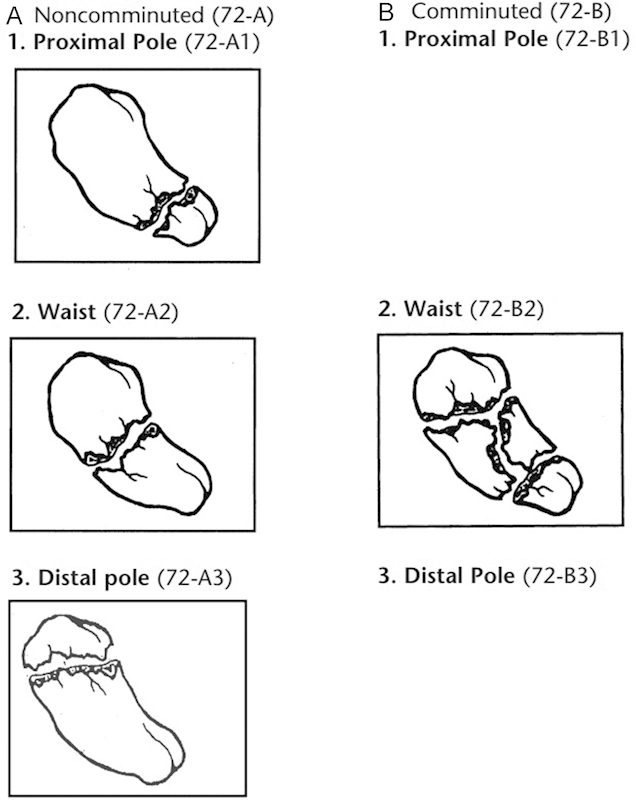
In the AO/OTA classification, scaphoid fractures (registered with number 72) were separated into noncomminuted (A) and comminuted (B; more than three fragments) fractures while taking fracture location into account. (Reprinted , with permission covered by STM guidelines, from Marsh et al.6)
Classifications based on fracture plane orientation (Table 2): Bohler et al20 also distinguished fractures based on fracture planes, resembling Pauwels classification24 of femoral neck fractures. Horizontal oblique fractures might show compressive forces across the fracture site resulting in good tendency to heal. Transverse fractures might have both compressive and shear forces resulting in an average tendency to heal. Vertical oblique fractures were considered to be caused by shearing forces, making it unstable with higher risk of nonunion. Russe5 described a similar system (Fig. 6), which received more attention, probably due to his international publications and presentations. Compson25 distinguished 80 fractures based on dorsal alignment of fracture planes. He reconstructed the fracture outline on transparent solid three-dimensional scaphoid models by looking at multiple standard radiological views. He distinguished transverse fractures through the “surgical waist,” oblique fractures through the dorsal sulcus, and proximal pole fractures.
Table 2. Classification of acute scaphoid fractures based on fracture plane orientation.
| Author | Year | No. of citation (World of Science; Google Scholar) | Total cases | Type | Rate (%) | |
|---|---|---|---|---|---|---|
| Bohler et ala | 1954 | 38; 67 | 734 | HO | Horizontal oblique | 47 |
| T | Transverse | 50 | ||||
| VO | Vertical oblique | 3 | ||||
| Russe | 1960 | 277; 501 | 220 | HO | Horizontal oblique | 35 |
| T | Transverse | 60 | ||||
| VO | Vertical oblique | 5 | ||||
| Compson | 1998 | 41; 69 | 80 | 1 | Transverse waist (surgical waist) | 30 |
| 2 | Oblique waist (dorsal sulcus) | 36 | ||||
| 3 | Proximal pole | 34 | ||||
German article.
Fig. 6.
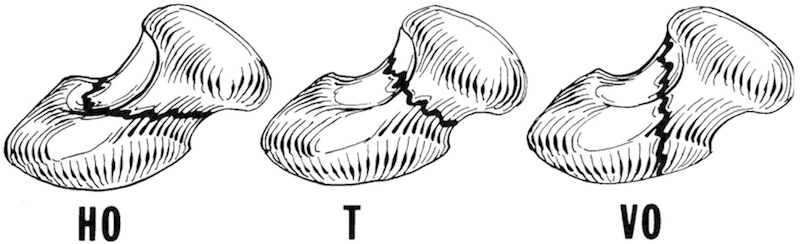
Russe separated fractures based on fracture plane orientation into transverse (T), horizontal oblique (HO), and vertical oblique (VO) fractures. Vertical oblique fractures were most troublesome with healing, requiring longer immobilization time (10–12 weeks). (Reprinted, with permission from Elizabeth Roselius, from Taleisnik.15)
Classifications based on displacement and/or instability (Table 3): McLaughlin and Parkes26 classified fractures by their stability ranging from incomplete fractures with intact shell of cartilage and bone to undisplaced/stable fractures and displaced/unstable fractures. Cooney et al4 (Mayo) also classified fractures by their stability (Table 4). Based on biomechanical experiments, Weber27 described nondisplaced fractures without disruption of ligamentous attachments, angulated fractures with dorsal intercarpal ligamentous disruption due to increasing injury forces, and displaced fractures with complete disruption of ligamentous attachments. Angulation may decrease the amount of surface contact, thus increasing risk of nonunion. Herbert and Fisher3 proposed a classification with the intention to identify fractures most applicable for screw fixation, due to instability (Fig. 7). All complete bicortical fractures (except for tubercle fractures) were considered unstable. According to Garcia-Elias and Lluch,28 proximal scaphoid fractures are stable when running proximal to the scaphoid-lunate ligaments which form the important linkage between the lunate and the distal scaphoid, but are unstable when running distal to them.
Table 3. Classification of acute scaphoid fractures based on displacement/instability.
| Author | Year | No. of citation (World of Science; Google Scholar) | Total cases | Type | Rate (%) | |
|---|---|---|---|---|---|---|
| McLaughlin and Parkes | 1969 | 37; 70 | – | A | Incomplete | – |
| B | Undisplaced and stable | – | ||||
| C | Displaced and unstable | – | ||||
| Cooney et al (Mayo) |
1980 | 110; 330 | 45 | 1 | Nondisplaced/stable | 71 |
| 2 | Displaced/unstable | 29 | ||||
| Weber | 1980 | 35; 127 | 36 | 1 | Nondisplaced | 53 |
| 2 | Angulated | 17 | ||||
| 3 | Displaced | 30 | ||||
| Herbert/Modified Herbert | 1984/1996 | 331; 739 139; 268 |
200/431 | A1 | Stable, tubercle | – |
| A2 | Stable, incomplete waist | – | ||||
| B1 | Unstable, distal oblique | 19a | ||||
| B2 | Unstable, complete waist | 60a | ||||
| B3 | Unstable, proximal pole | 21a | ||||
| B4 | Unstable fracture dislocation | – | ||||
| B5 | Unstable, comminutedb | – | ||||
| Garcia-Elias and Lluch | 2001 | 27; 53 | – | 1 | Stable, proximal to SL-ligament | – |
| 2 | Unstable, distal to SL-ligament | – | ||||
Based on 82 B1, B2, and B3 fractures reported in the article of 1996.
Omitted in the modified Herbert classification.
Table 4. Mayo classification based on instability of acute scaphoid fractures and their characteristics.
| Stable fracture | Unstable fracture |
|---|---|
| Displacement < 1 mm | Displacement > 1 mm |
| Normal intercarpal alignment | DISI alignment |
| Capitate-lunate angle 0 to 15 degrees | Capitate-lunate angle > 15 degrees |
| Scaphoid-lunate angle 30 to 60 degrees | Scaphoid-lunate angle > 60 degrees |
| Lateral intrascaphoid angle < 35 degrees | Lateral intrascaphoid angle > 35 degrees |
| Distal fractures | Comminuted fractures |
| Perilunate fractures |
Abbreviation: DISI, dorsal intercalated segmental instability.
Fig. 7.
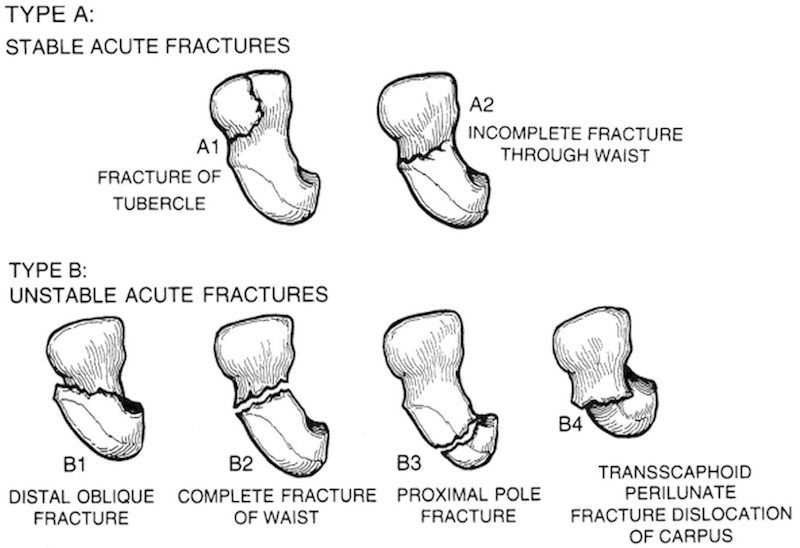
Herbert divided acute scaphoid fractures into acute stable (A) and unstable (B). Stable acute fractures included fractures of the tubercle and incomplete unicortical “crack” fractures. Only this type unites relatively fast and should be treated with a cast. (Reprinted, with permission covered by STM guidelines, from Green DO, ed. Operative Hand Surgery. 3rd ed. New York, NY: Churchill Livingstone; 1993.)
Discussion
In the past few decades, much endeavor has been made to identify the acute scaphoid fracture patterns that are prone to nonunion for purposes of surgical decision making. Based on our search, over a dozen classification systems have been proposed in the literature and were mainly based on fracture location or displacement. Considering the number of citations, the Herbert classification was most popular, followed by the Russe and Mayo classification. Based on original reports describing fracture location,4 20 21 waist fractures occur most often with percentages ranging from 66 to 82%. Considering fracture plane orientation,5 20 25 transverse fractures have the highest incidence ranging from 36 to 60%, followed by horizontal oblique fractures ranging from 30 to 47%. Considering fracture stability,4 27 most fractures are described as stable (53 and 71%).
Based on two recent systematic reviews,29 30 several randomized controlled trials can be identified comparing surgical with conservative treatment for acute scaphoid fractures using various radiographic classification systems, including those described by Herbert,31 32 33 34 the AO/OTA,35 and Russe.34 Inclusion criteria ranged from waist fractures only31 32 33 36 to distal, waist and proximal fractures,34 35 37 or from only nondisplaced31 32 36 to minimally, moderately, and severely displaced fractures.33 34 37 Some trials32 34 35 37 excluded tuberosity and unicortical fractures. One trial35 included vertical and comminuted fractures. In most trials, the exact borders of the waist area and level of displacement/step-off were not defined. In particular, it is often unclear when displacement is considered to be minimal.
Based on interobserver studies, agreement regarding the radiographical assessment of fracture displacement varies between fair,38 moderate,39 and good.40 Displacement close to 1 mm can be easily misclassified as nondisplacement.41 Encouraging results have shown that training can improve interobserver reliability and diagnostic performance for fracture displacement.42 In another interobserver study,39 agreement between observers was only fair regarding the radiographical classification of scaphoid fractures according to Compson, Herbert, and Russe. Observers had difficulty with each classification system and neither did significantly better than the other. None of the systems could predict fracture union. In general, fracture lines as observed on radiographs are difficult to relate to the three-dimensional complex anatomy25 and sometimes difficult to detect due to superimposition over neighboring carpal bones.43 Recently, Luria et al44 used three-dimensional imaging techniques to analyze fracture plane orientation relative to the scaphoid central axis in 124 acute scaphoid fractures. They concluded all fractures were horizontal oblique, and not transverse, unlike previous radiographic observational studies have reported.
It seems that the variation of used radiographic classification systems and their limited reliability confound efforts to compare outcomes of treatment methods among different clinical studies, limiting the level of evidence.45
When distinguishing fractures, the clinical relevance must be clear in relation to either treatment options, or prognosis, or risk of complications.6 At the waist of the scaphoid, displaced fractures are considered unstable, which is the most important factor associated with nonunion, for which open reduction and internal fixation is generally advised.46 47 However, when displacement is not clearly visible on radiographs, as in most patients, potentially unstable scaphoid fractures are difficult to identify. Some surgeons consider all fractures unstable, irrespective of displacement, when the fracture line is readily identified on radiographs48 or show bicortical involvement,49 and suggest operative treatment. First, this may lead to overtreatment as the incidence of unstable fractures being classified as nondisplaced as well as their relative risk of nonunion is currently unknown. Second, in a previous study50 using arthroscopy as reference standard for instability and displacement, only 7 of 22 radiographically nondisplaced (bicortical) fractures were unstable.
We believe that after confirming a scaphoid fracture, management could be further improved if we find a more reliable way to identify substantial interfragmentary motion when displacement is ruled out. Imaging modalities with the wrist in motion using fluoroscopy or dynamic three-dimensional CT may be useful to find predictors for interfragmentary motion (i.e., true instability) in relation to surgical or arthroscopic findings and clinical outcome. To date, one possible predictor of acute fracture instability might be the location relative to the dorsal apex as shown in nonunions.51 However, this factor was not predictive for instability in one previous study52 of acute fractures using arthroscopy as a reference standard. Fracture comminution was the only significant predictor for instability. Considering the fact that the majority of nondisplaced fractures are treated conservatively, predicting instability might improve identification of the small subset of scaphoid fractures unlikely to heal in a cast.
Location
This work was performed at the Department of Plastic, Reconstructive, and Hand Surgery, Academic Medical Center, University of Amsterdam, Amsterdam.
Acknowledgment
The authors thank Faridi van Etten-Jamaludin, librarian at the Academic Medical Center in Amsterdam, for her help with establishing the online search strategy.
Footnotes
Conflict of Interest None. Funding P. W. B. received a PhD grant (2014) from the Academic Medical Center (Amsterdam, the Netherlands) supporting this research.
References
- 1.Peltier L F. The classic. Injuries of the wrist. A radiological study. By Etienne Destot. 1926. Clin Orthop Relat Res. 1986;(202):3–11. [PubMed] [Google Scholar]
- 2.Cravener E K, McElroy D G. Fractures of the carpal (navicular) scaphoid. Am J Surg. 1939;44(1):8. [Google Scholar]
- 3.Herbert T J, Fisher W E. Management of the fractured scaphoid using a new bone screw. J Bone Joint Surg Br. 1984;66(1):114–123. doi: 10.1302/0301-620X.66B1.6693468. [DOI] [PubMed] [Google Scholar]
- 4.Cooney W P, Dobyns J H, Linscheid R L. Fractures of the scaphoid: a rational approach to management. Clin Orthop Relat Res. 1980;(149):90–97. [PubMed] [Google Scholar]
- 5.Russe O. Fracture of the carpal navicular. Diagnosis, non-operative treatment, and operative treatment. J Bone Joint Surg Am. 1960;42-A:759–768. [PubMed] [Google Scholar]
- 6.Marsh J L Slongo T F Agel J et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee J Orthop Trauma 200721(10, Suppl):S1–S133. [DOI] [PubMed] [Google Scholar]
- 7.Green D P, ed. Operative Hand Surgery. 2nd ed New York, NY: Churchill Livingstone; 1988 [Google Scholar]
- 8.Tubiana R, ed. The Hand. 1st ed Philadelphia, PA: W.B. Saunders Company; 1985 [Google Scholar]
- 9.Tubiana R Slade J F III, eds. Hand Clinics: Scaphoid Fractures. 1st ed Philadelphia, PA: W.B. Saunders Company; 2001 [Google Scholar]
- 10.Nakamura R Linscheid R L Miura T, eds. Wrist Disorders. 1st ed.Tokyo: Springer-Verslag; 1992 [Google Scholar]
- 11.Sandzen S C. Littleton, MA: PSG Publishing Company; 1986. Atlas of Wrist and Hand Fractures. 2nd ed. [Google Scholar]
- 12.Barton N J, ed. Hand and Upper Limb: Fractures of the Hand and Wrist. 1st ed New York, NY: Churchill Livingstone; 1988 [Google Scholar]
- 13.Cooney W P Linscheid R L Dobyns J H, eds. The Wrist Diagnosis and Operative Treatment. 1st ed St. Louis, MO: Mosby; 1998 [Google Scholar]
- 14.Lichtman D M Herbert Alexander A, eds. The Wrist and Its Disorders. 2nd ed Philadelphia, PA: W.B. Saunders; 1997 [Google Scholar]
- 15.Taleisnik J. New York, NY: Churchill Livingstone; 1985. The Wrist. 1st ed. [Google Scholar]
- 16.Razemon J P Fisk G R, eds. The Wrist. 1st ed New York, NY: Churchill Livingstone; 1988 [Google Scholar]
- 17.Sennwald G. Berlin: Springer-Verlag; 1987. The Wrist. 1st ed. [Google Scholar]
- 18.Slutsky D J Slade J F, eds. The Scaphoid. 1st ed New York, NY: Thieme Medical; 2010 [Google Scholar]
- 19.Filan S L, Herbert T J. Herbert screw fixation of scaphoid fractures. J Bone Joint Surg Br. 1996;78(4):519–529. [PubMed] [Google Scholar]
- 20.Bohler L, Trojan E, Jahna H. Treatment of 734 cases of fresh fracture of the scaphoid bone of the hand [in German] Wiederherstellungschir Traumatol. 1954;2:86–111. [PubMed] [Google Scholar]
- 21.Schernberg F, Elzein F, Gérard Y. Anatomo-radiological study of fractures of the carpal scaphoid bone. Problems of abnormal callus [in French] Rev Chir Orthop Repar Appar Mot. 1984;70 02:55–63. [PubMed] [Google Scholar]
- 22.Prosser A J, Brenkel I J, Irvine G B. Articular fractures of the distal scaphoid. J Hand Surg [Br] 1988;13(1):87–91. doi: 10.1016/0266-7681_88_90061-7. [DOI] [PubMed] [Google Scholar]
- 23.Müller M E, Allgöwer M, Willenegger H. Berlin: Springer; 1963. Technik der operativen Frakturenbehandlung. 1st ed. [Google Scholar]
- 24.Pauwels F. Stuttgart: Ferdinand Enke Verlag; 1935. Der schenkelhalsbruch ein mechanisches problem: Grundlagen des Haeilungsvorganges Prognose und kausale Therapie. [Google Scholar]
- 25.Compson J P. The anatomy of acute scaphoid fractures: a three-dimensional analysis of patterns. J Bone Joint Surg Br. 1998;80(2):218–224. doi: 10.1302/0301-620x.80b2.6926. [DOI] [PubMed] [Google Scholar]
- 26.McLaughlin H L, Parkes J C II. Fracture of the carpal navicular (scaphoid) bone: gradations in therapy based upon pathology. J Trauma. 1969;9(4):311–319. doi: 10.1097/00005373-196904000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Weber E R. Biomechanical implications of scaphoid waist fractures. Clin Orthop Relat Res. 1980;(149):83–89. [PubMed] [Google Scholar]
- 28.Garcia-Elias M Lluch A Partial excision of scaphoid: is it ever indicated? Hand Clin 2001174687–695., x [PubMed] [Google Scholar]
- 29.Buijze G A, Doornberg J N, Ham J S, Ring D, Bhandari M, Poolman R W. Surgical compared with conservative treatment for acute nondisplaced or minimally displaced scaphoid fractures: a systematic review and meta-analysis of randomized controlled trials. J Bone Joint Surg Am. 2010;92(6):1534–1544. doi: 10.2106/JBJS.I.01214. [DOI] [PubMed] [Google Scholar]
- 30.Symes T H, Stothard J. A systematic review of the treatment of acute fractures of the scaphoid. J Hand Surg Eur Vol. 2011;36(9):802–810. doi: 10.1177/1753193411412151. [DOI] [PubMed] [Google Scholar]
- 31.Adolfsson L, Lindau T, Arner M. Acutrak screw fixation versus cast immobilisation for undisplaced scaphoid waist fractures. J Hand Surg [Br] 2001;26(3):192–195. doi: 10.1054/jhsb.2001.0558. [DOI] [PubMed] [Google Scholar]
- 32.Arora R, Gschwentner M, Krappinger D, Lutz M, Blauth M, Gabl M. Fixation of nondisplaced scaphoid fractures: making treatment cost effective. Prospective controlled trial. Arch Orthop Trauma Surg. 2007;127(1):39–46. doi: 10.1007/s00402-006-0229-z. [DOI] [PubMed] [Google Scholar]
- 33.McQueen M M, Gelbke M K, Wakefield A, Will E M, Gaebler C. Percutaneous screw fixation versus conservative treatment for fractures of the waist of the scaphoid: a prospective randomised study. J Bone Joint Surg Br. 2008;90(1):66–71. doi: 10.1302/0301-620X.90B1.19767. [DOI] [PubMed] [Google Scholar]
- 34.Vinnars B, Pietreanu M, Bodestedt A, Ekenstam Fa, Gerdin B. Nonoperative compared with operative treatment of acute scaphoid fractures. A randomized clinical trial. J Bone Joint Surg Am. 2008;90(6):1176–1185. doi: 10.2106/JBJS.G.00673. [DOI] [PubMed] [Google Scholar]
- 35.Saedén B, Törnkvist H, Ponzer S, Höglund M. Fracture of the carpal scaphoid. A prospective, randomised 12-year follow-up comparing operative and conservative treatment. J Bone Joint Surg Br. 2001;83(2):230–234. doi: 10.1302/0301-620x.83b2.11197. [DOI] [PubMed] [Google Scholar]
- 36.Bond C D, Shin A Y, McBride M T, Dao K D. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001;83-A(4):483–488. doi: 10.2106/00004623-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Dias J J, Wildin C J, Bhowal B, Thompson J R. Should acute scaphoid fractures be fixed? A randomized controlled trial. J Bone Joint Surg Am. 2005;87(10):2160–2168. doi: 10.2106/JBJS.D.02305. [DOI] [PubMed] [Google Scholar]
- 38.Lozano-Calderón S, Blazar P, Zurakowski D, Lee S G, Ring D. Diagnosis of scaphoid fracture displacement with radiography and computed tomography. J Bone Joint Surg Am. 2006;88(12):2695–2703. doi: 10.2106/JBJS.E.01211. [DOI] [PubMed] [Google Scholar]
- 39.Desai V V, Davis T R, Barton N J. The prognostic value and reproducibility of the radiological features of the fractured scaphoid. J Hand Surg [Br] 1999;24(5):586–590. doi: 10.1054/jhsb.1999.0197. [DOI] [PubMed] [Google Scholar]
- 40.Bhat M, McCarthy M, Davis T R, Oni J A, Dawson S. MRI and plain radiography in the assessment of displaced fractures of the waist of the carpal scaphoid. J Bone Joint Surg Br. 2004;86(5):705–713. doi: 10.1302/0301-620x.86b5.14374. [DOI] [PubMed] [Google Scholar]
- 41.Temple C L, Ross D C, Bennett J D, Garvin G J, King G J, Faber K J. Comparison of sagittal computed tomography and plain film radiography in a scaphoid fracture model. J Hand Surg Am. 2005;30(3):534–542. doi: 10.1016/j.jhsa.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 42.Buijze G A Guitton T G van Dijk C N Ring D; Science of Variation Group. Training improves interobserver reliability for the diagnosis of scaphoid fracture displacement Clin Orthop Relat Res 201247072029–2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Moritomo H. Radiographic clues for determining carpal instability and treatment protocol for scaphoid fractures. J Orthop Sci. 2014;19(3):379–383. doi: 10.1007/s00776-014-0546-y. [DOI] [PubMed] [Google Scholar]
- 44.Luria S, Schwarcz Y, Wollstein R, Emelife P, Zinger G, Peleg E. 3-dimensional analysis of scaphoid fracture angle morphology. J Hand Surg Am. 2015;40(3):508–514. doi: 10.1016/j.jhsa.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 45.Bruinsma W E Guitton T G Warner J J Ring D; Science of Variation Group. Interobserver reliability of classification and characterization of proximal humeral fractures: a comparison of two and three-dimensional CT J Bone Joint Surg Am 201395171600–1604. [DOI] [PubMed] [Google Scholar]
- 46.Buijze G A Ochtman L Ring D Management of scaphoid nonunion J Hand Surg Am 20123751095–1100., quiz 1101 [DOI] [PubMed] [Google Scholar]
- 47.Swart E Strauch R J Diagnosis of scaphoid fracture displacement J Hand Surg Am 2013384784–787., quiz 787 [DOI] [PubMed] [Google Scholar]
- 48.Steinmann S P, Adams J E. Scaphoid fractures and nonunions: diagnosis and treatment. J Orthop Sci. 2006;11(4):424–431. doi: 10.1007/s00776-006-1025-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Herbert T J. St. Louis, MO: Quality Medical Publishing; 1990. The Fractured Scaphoid. 1st ed. [Google Scholar]
- 50.Buijze G A, Jørgsholm P, Thomsen N O, Bjorkman A, Besjakov J, Ring D. Diagnostic performance of radiographs and computed tomography for displacement and instability of acute scaphoid waist fractures. J Bone Joint Surg Am. 2012;94(21):1967–1974. doi: 10.2106/JBJS.K.00993. [DOI] [PubMed] [Google Scholar]
- 51.Moritomo H, Murase T, Oka K, Tanaka H, Yoshikawa H, Sugamoto K. Relationship between the fracture location and the kinematic pattern in scaphoid nonunion. J Hand Surg Am. 2008;33(9):1459–1468. doi: 10.1016/j.jhsa.2008.05.035. [DOI] [PubMed] [Google Scholar]
- 52.Buijze G A, Jørgsholm P, Thomsen N O, Björkman A, Besjakov J, Ring D. Factors associated with arthroscopically determined scaphoid fracture displacement and instability. J Hand Surg Am. 2012;37(7):1405–1410. doi: 10.1016/j.jhsa.2012.04.005. [DOI] [PubMed] [Google Scholar]


