Abstract
Objectives
Optimal control of type 2 diabetes is challenging in many patient populations including in South Asian patients. We systematically reviewed studies on the effect of diabetes management interventions targeted at South Asian patients with type 2 diabetes on glycaemic control.
Design
Systematic review of MEDLINE, EMBASE and CINAHL databases for randomised controlled trials (RCTs) and pre-post-test studies (January 1990 to February 2014). Studies were stratified by where interventions were conducted (South Asia vs Western countries).
Participants
Patients originating from Pakistan, Bangladesh or India with type 2 diabetes.
Primary outcome
Change in glycated haemoglobin (HbA1c). Secondary end points included change in blood pressure, lipid levels, anthropomorphics and knowledge.
Results
23 studies (15 RCTs) met criteria for analysis with 7 from Western countries (n=2532) and 16 from South Asia (n=1081). Interventions in Western countries included translated diabetes education, additional clinical care, written materials, visual aids, and bilingual community-based peers and/or health professionals. Interventions conducted in South Asia included yoga, meditation or exercise, community-based peers, health professionals and dietary education (cooking exercises). Among RCTs in India (5 trials; n=390), 4 demonstrated significant reductions in HbA1c in the intervention group compared with usual care (yoga and exercise interventions). Among the 4 RCTs conducted in Europe (n=2161), only 1 study, an education intervention of 113 patients, reported a significant reduction in HbA1c with the intervention. Lipids, blood pressure and knowledge improved in both groups with studies from India more often reporting reductions in body mass index and waist circumference.
Conclusions
Overall, there was little improvement in HbA1c level in diabetes management interventions targeted at South Asians living in Europe compared with usual care, although other outcomes did improve. The smaller studies in India demonstrated significant improvements in glycaemic and other end points. Novel strategies are needed to improve glycaemic control in South Asians living outside of India.
Keywords: HEALTH SERVICES ADMINISTRATION & MANAGEMENT
Strengths and limitations of this study.
To the best of our knowledge, this is the first systematic review of the efficacy of diabetes management (multiple components) interventions focused on South Asian patients.
Evidence is stratified by location of study, thereby allowing the examination of chronic diabetes management interventions on South Asians living in India and immigrant South Asian patients living in Western countries.
Included a systematic review of yoga interventions for diabetes management in South Asian patients with diabetes.
Given the significant heterogeneity in interventions and outcome results, a pooled analysis was not possible.
Medication adherence was not addressed in almost all of the trials.
Introduction
South Asian persons originating from Pakistan, Bangladesh or India experience a 50% higher risk of developing type 2 diabetes mellitus compared with other populations, irrespective of whether they live in South Asia or Western countries.1 2 This high global incidence of type 2 diabetes has significant ramifications on this population as type 2 diabetes is associated with a 2–4 times increased risk of myocardial infarction and stroke compared with those without diabetes. In Canada, age-adjusted standardised mortality is also three times higher in South Asian patients with diabetes compared with South Asian patients without diabetes.1 Robust clinical trial evidence demonstrates that reducing glycated haemoglobin (HbA1c), blood pressure and fasting blood lipids, using lifestyle modification and diabetes treatment, reduces total mortality by 46%, cardiovascular death by 57% and non-fatal cardiovascular events by 59%.3 4 As such, multiple national guideline bodies and diabetes programmes recommend diabetes education and behaviour modification to promote diet, exercise and diabetes medication adherence to achieve these critical reductions in HbA1c, blood pressure and lipids.
Despite guidelines and diabetes programmes to improve diabetes management, diabetes control remains suboptimal in many populations including South Asians.5 6 A study in Canada reports that 55% of South Asian patients are above recommended HbA1c targets, 36% above blood pressure targets and 58% are above lipid-level targets for diabetes.5 Further, South Asian patients are 24% less likely to achieve recommended targets for diabetes than the general population and also less likely to exercise or follow a healthy diet.6 7 This large gap in diabetes control in South Asians patients propelled the development of novel and culturally adapted diabetes management strategies in this group. Whether such strategies improve diabetes control in South Asian patients remains unclear. Therefore, we conducted a systematic review of all published randomised controlled trials (RCT) and prospective pre-post-test observational studies evaluating lifestyle or educational interventions compared with usual care or control in South Asian patients with type 2 diabetes on change in HbA1c. We also collected data on change in blood pressure, lipid levels, anthropometric measures and diabetes knowledge. We evaluated potential differences in change in HbA1c by intervention and region of study (South Asia vs Western countries).
Methods
The methods were in accordance with the PRISMA checklist for systematic reviews of intervention trials.
Data sources
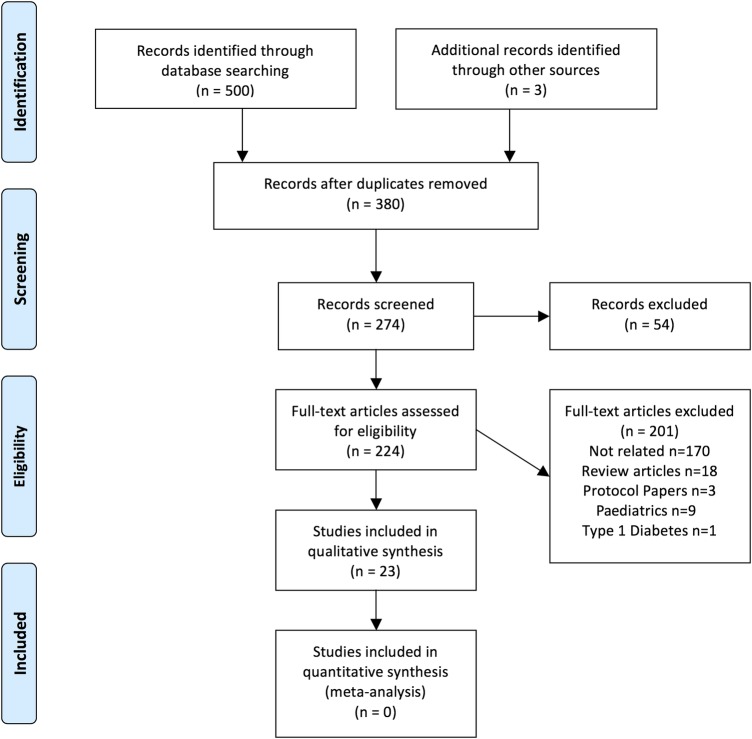
We performed a systematic review of intervention studies for type 2 diabetes management in South Asian patients. With the help of a medical librarian, we reviewed MEDLINE, EMBASE and CINAHL databases for articles published between 1 January 1990 and 1 February 2014. The search terms included India, Pakistan, Bangladesh, South Asian, East Indian, diabetes mellitus (type 2), manage, review, management, intervention, disease management, patient compliance, cultural characteristic, attitudes to health, cultural perception, outcomes, access to care and lifestyle changes (see online supplementary file for the full electronic search strategy). Searches were not limited by language. All articles were combined into a single list, and duplicates were excluded, resulting in 271 abstracts for review (see figure 1).
Figure 1.
Study flow.
bmjopen-2015-008986supp.pdf (96.1KB, pdf)
Study selection
Two authors reviewed all abstracts (NB and JJ; see figure 1). Studies were included if they were: conducted with adult patients identified as South Asian (originating from India, Pakistan or Bangladesh); randomised control trials or pre-post study designs, included any educational or lifestyle intervention for type 2 diabetes management and if they reported on any one of the outcomes of interest: absolute changes in HbA1c (primary outcome of interest), fasting blood glucose, blood pressure, weight, body mass index (BMI), waist circumference (WC), lipid levels and knowledge. We excluded studies where participants were paediatric populations, or had gestational diabetes, prediabetes or type 1 diabetes. We also excluded reviews, cross-sectional, case–control, case series studies as well as drug efficacy studies (including complementary, eg, Ayurvedic medicines). We did not include studies from other South Asian countries as there was a significant paucity of studies in those groups.
Study quality
All full-text studies that met the selection criteria were evaluated for bias, and were appraised on the basis of a component approach from the Cochrane Review Groups and Jadad score for reporting RCTs.8 9 These methodological quality measures are listed in table 3. Given the nature of the interventions, blinding of participants and caregivers was not possible. We evaluated separately the subgroup of higher quality RCTs that specified appropriate methods or type of randomisation, described losses to follow-up and intention-to-treat analysis.
Table 3.
Quality appraisal of trials
| Author, year | Randomised | Randomisation method | Type of randomisation | Allocation concealment | Blinding | Per cent Lost to follow-up | ITT |
|---|---|---|---|---|---|---|---|
| Middelkoop | RCT | Date of birth | NS | NS | None | NS | NS |
| Shenoy, 2009 | RCT | NS | NS | NS | None | 3 | NS |
| Shenoy, 2010 | RCT | NS | NS | NS | None | NS | Yes |
| Shantakumari | Randomised parallel study | NS | NS | NS | None | NS | NS |
| Vaishali | RCT | NS | Block | Sealed opaque envelopes | None | 5.3 | NS |
| Hawthorne | RCT | Random number tables | NS | Sealed envelopes | None | 6.5 | No |
| Adepu | RCT | NS | NS | NS | None | 14.3 | No |
| Baradaran | RCT | NS | Minimisation | NS | None | 37.3 | No |
| Ghosh | RCT | NS | NS | NS | None | Yes | NS |
| Malathy | RCT | NS | NS | NS | None | None | Yes |
| Hameed | RCT | Random number tables | NS | NS | None | Yes | Yes |
| Shetty | RCT | Random number tables | NS | NS | None | NS | No |
| O’Hare | Cluster RCT | None | NS | NS | None | 10.0 | No |
| Bellary | Cluster RCT | Simple | Simple | NS | NS | 10.8 | Yes |
| Vyas | Cluster RCT | NS | By GP practice4 | NS | NS | 44 | No |
| DeSouza, 2003, 2004 | Pretest post-test | Convenience sampling | NA | NA | None | NS | Yes |
| Balagopal, 2008 | Pretest post-test | NA | NA | NA | None | Yes: refusals | Yes |
| Balagopal, 2012 | Pretest post-test | NA | NA | NA | None | Yes: migration and refusals | Yes |
| Mirsa | Pretest post-test | NA | NA | NA | None | NS | Yes |
| Choudhury | Pretest post-test | NA | NA | NA | None | 8.9 | No |
| Pande | Pretest post-test | NA | NA | NA | None | NS | NS |
| Singh | Pretest post-test | NA | NA | NA | NS | NS | NS |
| Madanmohan, 2012 | Pretest post-test | NA | NA | NA | NS | <1 | Yes |
ITT, intention-to-treat; NA, not applicable; NS, not specified; RCT, randomised controlled trial.
Data extraction
Data extraction was completed in duplicate (NB and JJ). Any discrepancies were discussed and consensus achieved (NB, JJ and NAK). Since the outcomes and interventions of the study were clinically heterogeneous, no quantitative data synthesis was performed. Systematic review of the studies was a priori stratified by study location (South Asian countries vs Western countries) as these healthcare delivery systems, and potentially patient populations, were expected to be significantly different. Interventions were also described by type: education, exercise, dietary or mixed studies (defined as a combination of at least two of the aforementioned intervention types). Change in HbA1c from baseline (delta HbA1c) was the primary outcome for this review and was reported, where data were available, as the difference in delta HbA1c between the intervention and control groups. Findings from duplicate publications were only included once.
Results
From a review of 274 articles, 23 studies (n=3613) were included in this final review (figure 1 and table 1). Seven studies were conducted in Western countries (n=2532, all based in Europe)10–17 and 16 studies were conducted in people living in South Asia (n=1081, all based in India (indigenous Indians)).18–35 There were 15 RCTs (n=3279), with 9 (n=789) conducted in India.
Table 1.
Study characteristics by region
| Study | Country | Sample size | Design | Follow-up (months) |
Intervention type /control group |
Intervention |
|---|---|---|---|---|---|---|
| Diabetes management trials in Europe | ||||||
| Mixed trials | ||||||
| O'Hare et al10 | UK (England) | 361 | Cluster RCT | 12 | Mixed/usual care | SA link workers, additional DSME from nurse |
| Bellary et al11 | UK (England) | 1486 | Cluster RCT | 24 | Mixed/usual care | SA link workers, additional DSME from nurse |
| Choudhury et al14 | UK (Wales) | 42 | Pre-post | 1 | Mixed/no control | Culturally adapted X-PERT programme |
| Vyas et al16 | UK (England) | 211 | Cluster RCT | 12 | Mixed/usual care | Diabetes nurse, dietician and chiropodist advice |
| Education trials | ||||||
| Hawthorne and Tomlimson12 | UK (England) | 201 | RCT | 6 | Education/usual care | Picture flashcards and structured education package delivered by link worker |
| Hawthorne13 (duplicate) | UK (England) | 199 | RCT | 6 | Education/usual care | Picture flashcards delivered by link worker (not trained in psychology) |
| Baradaran et al15 | UK (Scotland) | 118 | RCT | 6 | Education/usual care | Cultural-specific education by dietician and podiatrist, didactic and interactive group session, visual aids |
| Middelkoop et al17 | The Netherlands (South Holland) | 113 | RCT | 6 | Education/patients who received educational materials only at the end of the study | Culture-specific education materials: general diabetes information in Surinam-Hindi language and nutrition information specific to South Asian cooking—by specialist diabetes nurse and dietician |
| Diabetes management trials in India | ||||||
| Mixed trials | ||||||
| Balagopal et al18 | India (Tamil Nadu) | 30 | Pre-post | 7 | Mixed/no control | Culturally and linguistically appropriate education on dietary modifications, improving physical activity and reducing stress provided by trained trainers; and education on blood glucose management by a DE |
| Balagopal et al19 | India (Gujarat) | 118 | Pre-post | 6 | Mixed/no control | Culturally and linguistically appropriate health education on dietary modifications, improving physical activity and risk for developing diabetes by CHW; education and counselling by DE. peer based; CHW; group sessions; advice on exercise and diet; Meditation, problem-solving |
| DeSouza and Subrahmanya Nairy,26 DeSouza and Nairy27 | India (Goa) | 60 | Pre-post | 2 | Mixed/usual care | Nurse-directed intervention (education, psychosocial support, visual aids) |
| Exercise-based trials | ||||||
| Hameed et al24 | India (Delhi) | 48 | RCT | 2 | Exercise/group on stationary cycling programme without work load and static stretching exercises | Progressive Resistance Training Program (2–3×/week) |
| Misra et al25 | India (Delhi) | 30 | Pre-post | 3 | Exercise/no control group | Progressive Resistance Training Program (3×/week) |
| Shenoy et al,30 Arora et al31 | India (Punjab) | 30 | RCT | 4 | Exercise/participants underwent no training but continued medications | Progressive resistance training (2 times per weeks) and aerobic exercise (3 times a week) |
| Shenoy et al32 | India (Punjab) | 40 | RCT | 2 | Exercise/participants underwent no training but continued medications | Aerobic walk using a heart rate monitor and pedometer to achieve a target of 150 min per week |
| Yoga-based trials: asanas (body postures) and pranayama (breathing exercises) | ||||||
| Shantakumari et al20 | India (Kerala) | 100 | RCT | 3 | Exercise/patients on OHA without yogic exercises | OHA and yoga exercises (asanas and pranayama meditation techniques) |
| Vaishali et al21 | India (Karnataka) | 57 | RCT | 3 | Exercise/received general healthy lifestyle and exercise information | Yogic exercises (asanas) and specially developed breathing techniques (pranayama) |
| Singh et al34 | India (Delhi) | 24 | Pre-post | 1.3 | Exercise | Yoga asanas |
| Madanmohan et al35 | India (Tamil Nadu) | 15 | Pre-post | 1.5 | Exercise | Yoga (asanas and pranayama) including yogic counselling and lifestyle modification advice |
| Education trials | ||||||
| Adepu et al22 | India (Kerala) | 70 | RCT | 4 | Education/pharmacist counselling at study end | Patient counselling by pharmacist |
| Ghosh et al23 | India (Uttar Pradesh) | 22 | RCT | 1.5 | Education/pharmacist counselling and information leaflets at study end | Counselling by pharmacist, information leaflets |
| Malathy et al29 | India (Tamil Nadu) | 207 | RCT | 3 | Education/patients received counselling and information leaflets at study end | Pharmacist counselling and information leaflets |
| Shetty et al33 | India (Tamil Nadu) | 215 | RCT | 12 | Education/usual care | SMS messaging on cell phones on diabetes management education |
| Diet-based trials | ||||||
| Pande et al28 | India (Maharashtra) | 15 | Pre-post | 1 | Diet/no control | Low and low-medium glycaemic load meals |
Intervention type: education, exercise, dietary or mixed (two or more intervention types).
CBA, controlled before and after experiment; CHW, community health worker; DE, diabetes educator; DSME, diabetes self-management education; OHA, oral hypoglycaemic agent; RCT, randomised controlled trial; SA, South Asian.
Patient characteristics
The average age of patients in the studies ranged from 35 to 66 years with the studies from India more often including younger patients (table 2). While approximately half of the patients enrolled in the European-based studies were women, the majority of participants in the India-based studies were men. Mean HbA1c levels at baseline were ≥61 mmol/mol (7.7%) and were generally similar between study regions.
Table 2.
Patient characteristics in the studies by region
| Study author, year | Study population | Recruitment site | Age Years mean |
Women (%) |
HbA1c mmol/mol (%) |
BMI kg/m2 mean |
SBP mm Hg mean |
DBP mm Hg mean |
|---|---|---|---|---|---|---|---|---|
| Diabetes management trials in Europe | ||||||||
| Mixed trials | ||||||||
| O'Hare, 2004 | Indian, Pakistani and Bangladeshi | GP practices | 58.9 | 49 | 64 (8.0) | 145 | 81 | |
| Bellary and O'Hare, 2008 | Indian, Pakistani and Bangladeshi | Inner city GP practices | 57.0 | 48 | 63 (7.9) | 28.5 | 140 | 83 |
| Choudhury, 2008 | Bangladeshi | Urban community | 67 | |||||
| Vyas, 2003 | Pakistani | GP offices | 46 | |||||
| Education trials | ||||||||
| Hawthorne, 1997 | Pakistani | Manchester Diabetes Centre and 10 GP practices | 53 | 53 | 70 (8.5) | |||
| Hawthorne, 2001 | Pakistani | Manchester Diabetes Centre or diabetes mini clinics | 53.2 | 53 | 68 (8.4) | |||
| Baradaran, 2006 | Indian and Pakistani | Daycare centres and GP offices | 58.4 | 49 | ||||
| Middelkoop, 2001 | South Asian Surinamese | GP practice and outpatient clinics | 53.3 | 50 | 67 (8.3) | |||
| Diabetes management trials in India | ||||||||
| Mixed trials | ||||||||
| Balagopal, 2008 | Indian | Rural community | 35.8 | 59 | 23.3 | 133 | 93 | |
| Balagopal, 2012 | Indian | Rural community | 41.9 | 53 | 24.4 | 151 | 89 | |
| DeSouza, 2003, 2004 | Indian | Outpatient clinic, private hospitals | 41.0–60.0 | 28 | Obese I: 20% C: 6.7% |
<140 I: 93.3% C: 86.7% | ||
| Exercise-based trials | ||||||||
| Hameed, 2012 | Indian | University hospital outpatient clinics | 44.7 | 27 | 68 (8.4) | 27.3 | 130 | 79 |
| Misra, 2008 | Indian | Outpatient and diabetes clinic | 40.8 | 27 | 61 (7.7) | 24.1 | ||
| Shenoy, 2009 | Indian | University health centre | 53.4 | 47 | 62 (7.8) | |||
| Shenoy, 2010 | Indian | Outpatients | 52 | 28 | 57 (7.4) | 27 | 127 | 86 |
| Yoga-based trials | ||||||||
| Shantakumari, 2013 | South Asian | Outpatient department of holistic medicine and university-based diabetes clinic | 45.0 | 49 | 23.1 | |||
| Vaishali, 2012 | South Asian | Diabetes clinic | 65.8 | 37 | 91 (10.5) | 27.6 | ||
| Singh, 2004 | Indian | Not specified | 30–60 | 75 (9.0) | 142 | 86.7 | ||
| Madanmohan, 2012 | Indian | University hospital | 50.4 | 100 | ||||
| Education-based trials | ||||||||
| Adepu, 2007 | South Asian | Urban community pharmacies | 52.6 | 31 | ||||
| Ghosh, 2010 | South Asian | Urban hospital outpatient | >50.0 | 28 | ||||
| Malathy, 2011 | Indian | Urban pharmacies | 52.0 | 59 | 66 (8.2) | Obese I: 22.6% C: 20% | >140 I: 15.3% C: 17.1% |
>90 I: 26.3% C: 25.8% |
| Shetty, 2011 | Indian | Outpatients | 50.2 | 75 (9.0) | 27.4 | >140/90 I: 42.7% C: 41% |
||
| Diet-based interventions | ||||||||
| Pande, 2012 | Indian | Medical College and General Hospital, diabetes outpatient department | 50.0 | 40 | 64 (8.0) | 18.0–26.0 | ||
BMI, body mass index; C, control group; DBP, diastolic blood pressure; GP, general practitioner; HbA1c, glycated haemoglobin; I, intervention group; SBP, systolic blood pressure.
Data quality
Overall, the data quality was modest (table 3). There were five RCTs conducted in India (total n=390) and four RCTs conducted in Europe (total n=2161) that measured HbA1c. Only three of the RCTs reported on either type or method of randomisation and quantified loss to follow-up less than 20%,11 12 21 and only two trials included information on allocation concealment.12 21 Additionally, none of the studies reported on blinding in outcome assessment. Fourteen studies reported loss to follow-up, and two studies had losses greater than 20%.15 16 Only nine studies analysed reported using intention to treat.
Interventions
There were seven studies of mixed interventions (three from India, four from Europe), eight educational interventions (four from India and three from Europe), four exercise intervention studies (all from India), four yoga intervention studies (all from India) and one study with a diet-based intervention (from India; table 1).
Interventions from studies of South Asians living in Europe
Intervention studies with South Asians living in Europe were either mixed interventions or education based. Common features of these interventions included enhanced diabetes education that was culturally specific, the use of bilingual link workers (community members and/or healthcare professionals including nurses or dieticians), as well as the use of written materials and visual aids. Link workers assisted patients with language translation, encouraged patient attendance at clinics, and helped organise educational sessions. One study15 included a dietician and podiatrist to provide education using didactic and interactive sessions with visual aids. The other14 used peer educators trained by a general practitioner with a special interest in diabetes to provide educational sessions giving advice on exercise, diet, attending appointments, cultural behaviours and the development of diabetes.
Interventions from studies of indigenous Indians
Studies with indigenous Indians included mixed interventions, exercise, yoga and educational interventions. Common features of these interventions included resistance exercise, and the use of community-based peers and healthcare professionals (pharmacists, nurses) as well as culture-specific dietary education. Three of the four yoga interventions included both asanas (static yoga positions) and pranayama (breathing exercises) and one only included asanas alone.20 21 34 35 Three exercise studies24 25 30 used resistance training, while one study included aerobic exercise.30 31 The other mixed intervention study from Balagopal et al18 featured education and experiential training on meditation/relaxation techniques, cooking (through demonstrations, recipe competitions and model meals) and exercise (through demonstrations, competitive fun events and dance-based exercise).
Change in HbA1c
Twelve studies reported HbA1c, while six additional studies included other measures of glycaemia (table 4). Among RCTs conducted in India (5 trials; n=390), four studies demonstrated significant reductions in HbA1c in the intervention group compared with usual care (yoga and exercise interventions). The yoga interventions were also significant in Northern and Southern India. All exercise interventions were conducted in Northern India, so regional differences could not be ascertained. Among the four RCTs conducted in Europe (n=2161), only one study of an education intervention in 113 patients reported a significant reduction in HbA1c with the intervention,17 whereas the remainder found no significant change (mixed and education interventions). Overall, the interventions associated with significant reductions in HbA1c tended to be based in India, exercise or yoga focused, while the interventions associated with no significant improvement in HbA1c tended to be among the larger trials, South Asian patients living in Europe and focused on enhanced education.
Table 4.
Outcomes of diabetes intervention studies*
| Study | HbA1c mmol/mol (%) |
BG (mmol/L) | SBP (mmHg) | DBP (mmHg) | Lipids (mmol/L) |
Anthropometrics |
|---|---|---|---|---|---|---|
| Mixed trials in Europe | ||||||
| O'Hare et al10 | −23 (−0.0) (p=0.87) | −4.6 (p=0.035) | −3.4 (p=0.003) | TC: −0.38 (p=0.005) | ||
| Bellary et al11 | −22 (−0.2) (p=0.11) | −0.33 (p=0.76) | −1.91 (p<0.001) | TC: +0.03 (p=0.37) | BMI: +0.40 (p<0.001) WC: −0.2 (p=0.67) |
|
| Mixed trials in India | ||||||
| Balagopal et al18 | FBG: −3.34 (p=0.03) |
−3.2 (p=0.48) | −5.5 (p=0.134) | BMI: +0.2 (p=0.63) WC: −4.8 cm (p=0.04) |
||
| Balagopal et al19 | FBG: I −1.06 (p<0.001) |
I −6.2 (p<0.001) | I −0.17 (p<0.001) | BMI: I −1.02 (p<0.001) WC: I −3.94 cm (p=0.001) |
||
| Exercise-based trials in India | ||||||
| Hameed et al24 | −17 (−0.6) (p<0.001) | −4.79 (p=0.07) | −1.91 (p=0.28) | TC: −0.07 (p=0.53) TG: −0.06 (p=0.56) HDL-C:+0.15 (p=0.004) LDL-C: −0.19 (p=0.10) |
Weight −0.31 (p=0.36) WC (cm): −2.04 (p=0.008) |
|
| Misra et al25 | I −18 (−0.5) (p<0.001) | FBG: I −2.7 (p<0.001) |
I: TC: −0.39 (p=0.003) TG: −0.39 (p<0.001) HDL:+0.02 (p=0.33) LDL: −0.09 (p=0.21) |
I: BMI: +0.1 (p=0.614) WC: −1.6 (p<0.001) |
||
| Shenoy et al30 | PRT: −3 (−1.8) (p=0.002) AE: −9 (−1.3) (p=0.002) C: −21 (−0.21) (p=NS) |
PRT: −3.83 (p=0.021) AE: −1.44 (p=0.021) C: −1.66 (p=NS) |
PRT: −9 (p=0.001) AE: −3 (p=NS) C: +2 (p=NS) |
PRT: −8 (p=0.001) AE: −1 (p=NS) C: +1 (p=NS) |
||
| Shenoy et al32 | I: −15 (−0.8) (p=0.0001) C: −23 (−0.1) (p=0.242) Difference in post-test I and C scores p=0.0023 |
FBG I: −4.24 (p=0.0001) C: −0.12 (p=0.0007) Difference in post-test I and C scores p=0.0001 |
I: +1.5 (p=0.868) C: −3.3 (p=0.133) Difference in post-test I and C scores p=0.019 |
I: −10.8 (p=0.010) C: −3.7 (p=0.0058) Difference in post-test I and C scores p=0.0001 |
BMI: I: −1.1 (p=0.0001) C: +0.6 (p=0.0001) Difference in post-test I and C scores p=0.56 |
|
| Yoga-based interventions in India | ||||||
| Vaishali et al21 | −15 (−0.8) (p<0.001) | FBG: −1.58 (p<0.001) |
TC: −0.48 (p<0.001) TG: −0.25 (p<0.001) HDL:+0.13 (p<0.001) LDL: −0.18 (p<0.05) |
|||
| Singh et al34 | −10 (−1.2) p=0.035 | FBG: −2.7 p<0.001 |
−16 p=0.001 | −8.8 p=0.001 | ||
| Madanmohan et al35 | FBG: −1.1 p=0.004 |
TC: −0.13 p=0.01 LDL −0.28 p=0.001 HDL −0.45 p=0.02 |
||||
| Shantakumari et al20 | TC: I −0.65 (p<0.01) C+0.25 (p=NS) TG: I −0.25 (p<0.05); C +0.28 (p=NS) LDL-C: I −0.63 (p<0.01); C +0.01 (p=NS) HDL-C: I+0.07 (p=NS); C −0.03 (p=NS) |
Weight: I −2.6 (p<0.05) C+0.86 (p<0.05) BMI: I −1.53 (p=NS) C+0.3 (p=NS) |
||||
| Education-based interventions in Europe | ||||||
| Hawthorne and Tomlimson12 | I −20 (−0.3) (p=NS) | I: TC 0.04 | ||||
| Hawthorne13 | −20 (−0.4) (p=NS) | |||||
| Middelkoop et al17 | −19 (−0.4) (p=0.02) | |||||
| Education-based interventions in India | ||||||
| Shetty et al33 | NS difference in mean HbA1c <64 (8%) I:+16.7% C:+24.3% |
FBG: I −1.1 | TC: I: −0.4 p<0.03 C: −0.3 p<0.03 |
|||
| Adepu et al22 | Capillary BG: I: −3.12, (p<0.001) C: −0.14 (p=NS) |
|||||
| Gosh et al23 | FBG: −0.83 (p<0.05) Postprandial G −1.94 (p<0.01) |
|||||
| Malathy et al29 | Postprandial glucose: I −1.81 C −0.99 (p<0.001) |
TC: I −0.53 (p<0.001) C −0.29 (p<0.05) LDL: I −0.52 (p<0.001) C −0.29 (p<0.01) HDL: I+0.04 (p<0.05) C+0.02 (p=NS) TG I −0.12 (p<0.001) C −0.08 (p=NS) |
||||
| Diet-based interventions India | ||||||
| Pande, 2012 | I −14 (−0.9) (p<0.001) |
FBG: I −1.99 (p<0.001) |
I TG −0.90 (p<0.001) TC −1.01 (p<0.001) HDL+0.18 (p=0.003) LDL −0.67 (p=0.009) |
|||
*Note that 4 of the studies (Baradaran, Choudhury, Vyas and DeSouza) only included knowledge outcomes and thus were not included in this table (see (table 5)).
The numbers represent the difference in change in parameters between the intervention and control groups if not otherwise stated.
AE, aerobic exercise; BG, blood glucose; BMI, body mass index; C, control group; DBP, diastolic blood pressure; HbA1c, glycated haemoglobin; HDL-C, high-density lipoprotein cholesterol; I, intervention group; LDL-C, low-density lipoprotein cholesterol; NS, not significant; PRT, progressive resistance training group; SBP, systolic blood pressure; TC, total cholesterol; TG, triglycerides; WC, waist circumference.
Other end points
Eight studies reported blood pressure end points; and in four of the five RCT's reporting blood pressure outcomes, interventions were associated with reduced mean systolic (range −0.33 to −9 mm Hg) or diastolic blood pressure (range −1.91 to −10.8 mm Hg) compared with usual care. Of the two studies conducted in Europe, both reported significant reductions in either systolic or diastolic blood pressure. Of the six studies of indigenous Indians, four reported significant reductions in blood pressure. Mixed and exercise interventions were associated with blood pressure reduction. None of the education or dietary intervention studies evaluated blood pressure (all conducted in India). Eleven studies evaluated lipid levels with 10 intervention studies demonstrating significant reductions in at least one measured lipid level across all the intervention types (table 4) with two of three studies from Europe and the other eight from India reporting significant reductions. Six studies among indigenous Indians included BMI or weight measurement with three studies reporting significant reductions (pretest post-test mixed intervention, one yoga and one exercise-based RCT),19 32 whereas three others reported no significant reduction or weight increases. All four studies conducted in India that measured WC found significant reductions with the intervention. One European mixed trial measured BMI and WC and identified a significant increase in BMI with the intervention.
Ten studies reported the effect of educational and mixed interventions on knowledge of diabetes, its prevention, management and complications and/or on quality of life (table 5). Among indigenous Indians, the majority of studies targeting diabetes knowledge and related practices as well as patients' quality of life through educational interventions reported significant improvement in the targeted outcomes. Among education studies conducted in Europe targeting knowledge of and practices related to diabetes, education intervention was not consistently associated with the improvement of the outcomes. Specifically, while half of the studies reported an improvement in knowledge of and attitudes and behaviours related to diabetes, the other half either found no such improvement14 or the difference in mean change scores between the intervention and control groups did not differ.15 Improvement in knowledge was observed in men and women and across literacy levels in one study.13
Table 5.
Change in knowledge of diabetes, its prevention, management and complications and on quality of life
| Study | Intervention | Knowledge of diabetes, its prevention, management and complications and patients’ quality of life |
|---|---|---|
| Studies based in Europe | ||
| Hawthorne and Tomlimson12 | Education | Change in per cent of patients correctly answering questions about
|
| Hawthorne13 | Education | Change in scores or per cent of patients correctly answering questions related to diabetes in M and W: food knowledge scores (I: M +11%, W +14%; C: M +3%, W +4%), knowledge of eye (I: M +55%, W +63%; C: M −3%, W +4%), heart (I: M +32%, W +54%; C: M −3%, W −3%) and feet diabetes complications (I: M +47%, W +67%; C: M +9%, W +17%), knowledge of chiropody (I: M +42%, W +32%; C: M +10%, W −5%), can manage hyperglycaemia (I: M +68%, W +63%; C: M +9%, W +13%), know why to control glucose (I: M +60%, W +61%; C: M +3%, W 0%), know purpose of annual reviews (I: M +66%, W +33%; C: M +14%, W −7%), check glucose regularly (I: M +27%, W +40%; C: M −29%, W 0%) and keep glucose records (I: M +36%, W +28%; C: M −8%, W −4%)Change in scores or per cent of patients correctly answering questions related to diabetes in LW and IW: food knowledge scores (LW +12%, IW +6%), knowledge of eye (LW +59%, IW +30%), heart (LW +53%, IW +50%), and feet (LW +40%, IW +45%), diabetes complications, knowledge of chiropody (LW +42%, IW +25%), can manage hyperglycaemia (LW +53%, IW +55%), know why to control glucose (LW +71%, IW +42%), know purpose of annual checks (LW +44%, IW +42%), check glucose regularly (LW +20%, IW +17%) |
| Choudhury et al14 | Education | There was no significant change in days study participants adhered to general and specific diet, recommended exercise or foot care (SDSCA Questionnaire); no control group available. |
| Baradaran et al15 | Education | Difference in mean change in scores between I and C groups for knowledge 1.25 (p=0.27); attitude towards seriousness −0.17 (p=0.76); attitude towards complications 0.68 (p=0.38) and practice 0.76 (p=0.23).Per cent improvement in mean scores for knowledge (I intervention, EC, WC) about diabetes (I +12.5% (p=0.04); EC +5% (p=0.53); WC +12.2% (p=0.19), attitudes towards seriousness of diabetes (I +13.5% (p=0.005); EC +16.3% (p=0.001); WC +12.4% (p=0.04)), attitudes towards diabetes complications (I +8.1% (p=0.05); EC +1.5% (p=0.40); WC +6% (p=0.19)), and practice related to diabetes (I +20% (p=0.005); EC +1.7% (p=0.63); WC +25% (p=0.007)) |
| Vyas et al16 | Mixed | Knowledge awareness and self-management questionnaires validated by Hawthorne. I: 0.09 knowledge; −0.15 self-management; C: 0.02 knowledge; 0.29 self-management (differences in prescores and postscores in the I and C groups) NS difference between intervention and control |
| Studies based in India | ||
| Balagopal et al18 | Mixed | Knowledge score: +0.94 (p=0.085) |
| Balagopal et al19 | Mixed | Diabetes knowledge score (American Diabetes Association risk test): +0.47 (p<0.001) |
| Adepu et al22 | Education | Change in per cent of patients correctly answering questions about knowledge of diabetes definition (I +22, C no change), causes of diabetes (I +67, C −2), methods of glucose measurement (I +43, C +4), diabetes complications (kidney (I +43, C no change), eye (I +27, C −3), frequency of eye examinations (I +67, C no change)), relationship between blood pressure and kidney functioning (I +60, C +3), frequency of blood pressure measurement in patients with diabetes (I +46, C +3), role of weight reduction in diabetes (I +47, C no change), hypoglycaemia (I +39, C +2) and its prevention/management (I +44, C −3) |
| DeSouza and Subrahmanya Nairy,26 DeSouza and Nairy27 | Education | 2003; Quality of life scores (difference in prescores and postscores for I and C groups): Total quality of life I +6.50, C +0.99 (p<0.05); health and functioning domain I +7.18, C +0.93 (p<0.05); social-economic domain I +5.81, C +0.61 (p<0.05); psychological-spiritual I +0.81, C +0.15 (p=NS); family domain I +4.17, C +1.45 (p<0.05)2004—Health-promoting behaviours scores (difference between postscores and pretest scores in the I and C groups and p value depicting the difference in post-test scores between the I and C groups): total health-promoting behaviour score: I +33.93, C 2.00 (p<0.001); health and functioning domain I +30.33, C +3.93 (p<0.001); social-economic domain I 3.07, C −0.46 (p<0.001); psychological-spiritual domain I +3.87, C −1.47 (p<0.001); family domain I +2.47, C −0.94 (p<0.001) |
| Malathy et al29 | Education | KAP scores (differences in pre-KAP and post-KAP scores in the I and C groups) Knowledge: I +3.12 (p=0.0001); C −0.06 (p=NS) Attitude: I +0.92 (p=0.0001); C +0.06 (p=NS) Practice: I +0.08 (p=0.06); C no change (p=NS) Overall: I +4 (p=0.0001); C+0.4 (p=NS) |
C, control group; EC, ethnic control; I, intervention group; IW, illiterate women; KAP, knowledge, attitude and practice; LW, literate women; NS, not significant; M, men; W, women; WC, white control.
Higher quality randomised studies
There were three randomised studies with a lower risk of bias11–13 21 (two mixed intervention RCTs conducted in Europe and one yoga-based trial conducted in India). Studies by Bellary et al11 and Hawthorne12 and Hawthorne and Tomlimson,13 conducted in Europe (total n=1687), used bilingual, bicultural enhanced diabetes education, link workers and visual aids, and they found no significant improvement in HbA1c level with these interventions compared with usual control. In contrast, in the exercise intervention study based in India (n=57) and led by Vaishali et al,21 there was a significant reduction in HbA1c levels among patients who underwent the intervention compared with their counterparts who did not undergo the exercise intervention.
Discussion
From the present review, diabetes management interventions targeted at South Asian patients were heterogeneous, yielding variable and limited success in HbA1c reduction. Changes in HbA1c level differed by region and intervention, whereby studies based in India that included exercise or yoga interventions were most successful in reducing HbA1c among individuals with type 2 diabetes. Blood pressure, lipid levels and knowledge were generally improved with various diabetes interventions compared with usual care in European-based and Indian-based studies, whereas BMI did not generally change with the interventions across studies.
The observation that HbA1c reduction was variable and limited across trials in Europe poses a stark contrast to the findings of culturally adapted diabetes management trials targeted at other ethnic groups studied in the Western world.36–38 Meta-analyses of RCTs ascertained that culturally adapted diabetes management programmes are superior to non-culturally adapted programmes with significant improvements (−17 mmol/mol (−0.6%)) in HbA1c at 6 months and knowledge scores.36–38 Cultural adaptation processes aim to adapt interventions or messages using culture to the intended audience. However, these meta-analyses included largely African-American or Hispanic ethnic groups. Interventions that were face to face, incorporated a peer educator and cognitive reframing techniques were found to be associated with reductions in HbA1c compared with usual care in African-American or Hispanic populations.39 In a culturally adapted diabetes programme targeted to a Latin American population, the intervention consisted of use of culturally tailored education, exercise (Latin dance) and dietary change compared with usual care. The cultural adaptations included family involvement, foods common in Latin American countries that could be used in modified Mediterranean diet recipes; and it also incorporated Latin music, language and symbols in meetings and materials.40 The intervention group significantly reduced HbA1c (−19 mmol/mol (−0.4%)) at 6 months compared with the usual care group.
Many of the aforementioned culturally adapted techniques were incorporated in the interventions targeted at South Asian patients with type 2 diabetes described in this review paper; however, reduction in HbA1c levels was not consistent across studies. We can speculate that the success of the trials from the meta-analysis in reducing HbA1c may lie in the depth to which the interventions were culturally adapted. To illustrate this concept, Resnicow et al41 contrasted surface and deep structural cultural adaptations. Surface structure is based on superficial characteristics of a population including people, language, places and food. Conversely, deep structure involves the integration of the sociocultural concepts, historical context and psychological factors unique to a population. Resnicow et al41 states “while adding surface structure to health programming may increase the receptivity of messages, it is deep cultural adaptation that truly fosters salient messaging”. In turn, it is possible that the trials from the meta-analysis achieved a greater depth of cultural adaptation compared with the RCTs conducted in Europe and described in this review.
There are several possible explanations underlying the differences in HbA1c changes reported in trials conducted in India compared with trials of patients living in Europe. While the UK studies were larger and mainly adopted an RCT design, the studies in India were generally smaller and eight of the studies employed a pre-post study design (usually a single group) that limits the ability to ascertain causality with the interventions and are associated with some overinflation of effect estimates.42 In addition, the variance in results may be explained by differences between the patient populations used in the two different regions. Specifically, trials of South Asians living in India included younger patients and more men than women. It is possible that men may have been more able to engage in physical activity programmes or exerted more control over the diet at home than women. Another possible explanation arises from systemic differences between the two regions. While the UK system is publicly funded, the Indian healthcare system has both private and public funding. Considering privatisation and different levels of socioeconomic position between the regions, there may be significantly less baseline knowledge of diabetes among patients living in India allowing for greater gains with interventions. Additional explanations regarding the differences in outcomes may be rooted in the design of the interventions used in trials. Compared with studies from India, the European studies did not include specific exercise programmes. While it is likely that diabetes self-management education featured in the Europe-based studies advised physical exercise, the trials from India formally integrated yoga and resistance training into their interventions. Studies from India also tended to incorporate experiential-based interventions including meditation training, cooking competitions and dancercise. This raises the possibility that strategies that are immersive and experiential rather than didactic/instructional may lead to better health behaviour change in South Asian groups. Moreover, while all studies from both locations delivered education, advice and training in Indian languages, it is not clear if any deeper cultural adaptations were employed; such adaptations may have been more implicit in the Indian-based interventions. For example, the UK studies featured interventions that were linguistically accessible for the patient population (ie, South Asian link workers, picture flashcards); meanwhile, however, many interventions from India ventured beyond language to include culturally rooted traditions such as specific forms of yoga, meditation and dance. Conversely, South Asian trial participants living in Europe may have been more acculturated compared with those living in India so that cultural adaptation of a diabetes education programme was less effective. Several studies identified significant social stigma attached to having diabetes in South Asian populations that might have negatively influenced their taking part in research studies or fully participating in the research interventions within trials in India and the West. Whether this stigma differs between migrant and indigenous Indians is unknown. Indeed, studies of Western trials demonstrate lower participation of South Asians in clinical studies compared with their non-South Asian counterparts.43 Additionally, though all the studies from India reported some statistically significant positive outcomes, it is possible that smaller study effects/publication bias could exist here, and thus small studies from India with negative outcomes may have not been published.
There are several potential reasons underlying the significant intercountry differences in education-based trials, whereby more success in improvement of knowledge of and practices related to diabetes was observed in studies that originated from India. One possible explanation is that the educational interventions from India provided patients with a broader scope of knowledge; that is, information beyond the fundamentals of diabetes self-management. For instance, the intervention conducted by DeSouza and Subrahmanya Nairy26 27 taught patients about relaxation and stress management as well as the role of family support and participation. Similarly, the programme employed by Balagopal et al19 featured education on meditation and relaxation techniques. Meanwhile, on the basis of the descriptions of UK educational studies, the UK interventions did not appear to venture into these domains. Furthermore, it is also unclear as to whether the success of trials from India assessing patient knowledge was due to something more than just education; specifically, there may exist the inherent ability of the interventions from India to encompass more cultural aspects then we realise. Overall, therefore, the strength of the educational trials from India may have been a blend of encompassing a larger breadth of educational domains and embodying a greater depth of cultural adaptation.
There are several limitations of this systematic review. In terms of the studies selected for the review, the overall quality of the studies was in the low-to-moderate range according to the quality components we studied. As such, each study is limited by potential biases. In addition, many of the studies, especially those from India, had smaller sample sizes and interventions between studies varied. Most trials did not report information on blinding of outcome assessment or details of the randomisation, thereby limiting the conclusions of this review. All of the studies conducted in South Asian countries were limited to India, and therefore these findings may not be generalised to other South Asian populations. The lack of studies from other South Asian countries may reflect differences in research support rather than a lower prevalence of diabetes in other South Asian countries. Given the significant heterogeneity in interventions and outcome results, a pooled analysis was not possible. In addition, key components of diabetes management including medication adherence were not addressed in almost all of the trials.
Conclusion
Overall, effectiveness of interventions differed by region. The most successful interventions for reducing HbA1c were more likely to be conducted among South Asians living in India and those interventions included yoga and exercise. While studies from both Western countries and South Asia observed improvements in lipid and blood pressure outcomes, studies from India more often reported reduction in patient BMI, WC and improved diabetes knowledge. Novel interventions are needed to improve glycaemic control of South Asians living in Western countries such as the inclusion of yoga or use of dance to engage participants in improving health behaviours.
Footnotes
Contributors: NB and JJ contributed equally as first authors. NAK, NB, JJ and DG were involved with the study design and concept, acquisition of data, analysis and interpretation of data, and preparation and editing of the manuscript.
Funding: NAK receives funding from a Michael Smith Foundation for Health Research Career Scientist Award.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Khan NA, Wang H, Anand S et al. Ethnicity and sex affect diabetes incidence and outcomes. Diabetes Care 2011;34:96–101. 10.2337/dc10-0865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohan V, Mathur P, Deepa R et al. Urban rural differences in prevalence of self-reported diabetes in India—the WHO-ICMR Indian NCD risk factor surveillance. Diabetes Res Clin Pract 2008;80:159–68. 10.1016/j.diabres.2007.11.018 [DOI] [PubMed] [Google Scholar]
- 3.Gaede P, Vedel P, Parving HH et al. Intensified multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: the steno type 2 randomised study. Lancet 1999;353:617–22. 10.1016/S0140-6736(98)07368-1 [DOI] [PubMed] [Google Scholar]
- 4.Macisaac RJ, Jerums G. Intensive glucose control and cardiovascular outcomes in type 2 diabetes. Heart Lung Circ 2011;20:647–54. 10.1016/j.hlc.2010.07.013 [DOI] [PubMed] [Google Scholar]
- 5.Shah BR, Cauch-Dudek K, Anand SS et al. Absence of disparities in the quality of primary diabetes care for South Asians and Chinese in an urban Canadian setting. Diabetes Care 2012;35:794–6. 10.2337/dc11-1845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gray J, Millett C, Saxena S et al. Ethnicity and quality of diabetes care in a health system with universal coverage: population-based cross-sectional survey in primary care. J Gen Intern Med 2007;22:1317–20. 10.1007/s11606-007-0267-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu R, So L, Mohan S et al. Cardiovascular risk factors in Canadian ethnic populations: results from national surveys. Open Med 2010;4:e143–53. [PMC free article] [PubMed] [Google Scholar]
- 8.Lundh A, Gøtzsche PC. Recommendations by the Cochrane Review Groups for assessment of the risk of bias in studies. BMC Med Res Methodol 2008;8:22 10.1186/1471-2288-8-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moher D, Pham B Jones A et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 1998;352:609–13. 10.1002/9780470988343.app1 [DOI] [PubMed] [Google Scholar]
- 10.O'Hare J, Raymond N, Mughal S et al. Evaluation of delivery of enhanced diabetes care to patients of South Asian ethnicity: the United Kingdom Asian Diabetes Study (UKADS). Diabet Med 2004;21:1357–65. 10.1111/j.1464-5491.2004.01373.x [DOI] [PubMed] [Google Scholar]
- 11.Bellary S, O'Hare JP, Raymond NT et al. Enhanced diabetes care to patients of south Asian ethnic origin (the United Kingdom Asian Diabetes Study): a cluster randomised controlled trial. Lancet 2008;371:1769–76. 10.1016/S0140-6736(08)60764-3 [DOI] [PubMed] [Google Scholar]
- 12.Hawthorne K, Tomlimson S. One-on-one teaching with pictures—flashcard health education for British Asians with diabetes. Br J Gen Pract 1997;47:301–4. [PMC free article] [PubMed] [Google Scholar]
- 13.Hawthorne K. Effect of culturally appropriate health education on glycaemic control and knowledge of diabetes in British Pakistani women with type 2 diabetes mellitus. Health Educ Res Theory Pract 2001;16:373–81. 10.1093/her/16.3.373 [DOI] [PubMed] [Google Scholar]
- 14.Choudhury S, Brophy S, Fareedi MA et al. Intervention, recruitment and evaluation challenges in the Bangladeshi community: experience from a peer lead educational course. BMC Med Res Methodol 2008;8:64 10.1186/1471-2288-8-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baradaran HR, Knill-Jones RP, Wallia S et al. A controlled trial of the effectiveness of a diabetes education programme in a multi-ethnic community in Glasgow [ISRCTN28317455]. BMC Public Health 2006;6:134 10.1186/1471-2458-6-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vyas A, Haidery AZ, Wiles PG et al. A pilot randomized trial in primary care to investigate and improve knowledge, awareness and self-management among South Asians with diabetes in Manchester. Diabet Med 2003;20:1022–6. 10.1046/j.1464-5491.2003.01082.x [DOI] [PubMed] [Google Scholar]
- 17.Middelkoop BJC, Geelhoed-Duijvestijn PHLM, van der Wal G. Effectiveness of culture-specific diabetes care for Surinam South Asian patients in the Hague: a randomized controlled trial/controlled before-and-after study. Diabetes Care 2001;24: 1997–8. 10.2337/diacare.24.11.1997 [DOI] [PubMed] [Google Scholar]
- 18.Balagopal P, Kamalamma N, Patel TG et al. A Community-based diabetes prevention and management education program in a rural village in India. Diabetes Care 2008;31:1097–104. 10.2337/dc07-1680 [DOI] [PubMed] [Google Scholar]
- 19.Balagopal P, Kamalamma N, Patel TG et al. A community-based participatory diabetes prevention and management intervention in rural India using community health workers. Diabetes Educ 2012;38:822–34. 10.1177/0145721712459890 [DOI] [PubMed] [Google Scholar]
- 20.Shantakumari N, Sequeira S, El deeb R. Effects of a yoga intervention on lipid profiles of diabetes patients with dyslipidemia. Indian Heart J 2013;65:127–31. 10.1016/j.ihj.2013.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vaishali K, Kumar KV, Adhikari P et al. Effects of yoga-based program on glycosylated hemoglobin level serum lipid profile in community dwelling elderly subjects with chronic type 2 diabetes mellitus—a randomized controlled trial. Phys Occup Ther Geriatr 2012;30:22–30. 10.3109/02703181.2012.656835 [DOI] [Google Scholar]
- 22.Adepu R, Rasheed A, Nagavi BG. Effect of patient counseling on quality of life in type-2 diabetes mellitus patients in two selected South Indian community pharmacies: a study. Indian J Pharm Sci 2007;69:519–24. 10.4103/0250-474X.36937 [DOI] [Google Scholar]
- 23.Ghosh S, Rajvanshi A, Kushun S. Assessment the influence of patient counseling on quality of life in type-II diabetes mellitus patients. Int J Pharm Bio Sci 2010;1:1–6. [Google Scholar]
- 24.Hameed UA, Manzar D, Raza S et al. Resistance training leads to clinically meaningful improvements in control of glycemia and muscular strength in untrained middle-aged patients with type 2 diabetes mellitus. N Am J Med Sci 2012;4:336–43. 10.4103/1947-2714.99507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Misra A, Alappan NK, Vikram NK et al. Effect of supervised progressive resistance-exercise training protocol on insulin sensitivity, glycemia, lipids and body composition in Asian Indians with type 2 diabetes. Diabetes Care 2008;31:1282–7. 10.2337/dc07-2316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DeSouza M, Subrahmanya Nairy K. Nursing intervention for the quality of life of diabetic adults. Clin Eff Nurs 2003;7:63–72. 10.1016/S1361-9004(03)00044-X [DOI] [Google Scholar]
- 27.DeSouza M, Subrahmanya Nairy K. An interventional study on the health promoting behaviours of adults with diabetes. Clin Eff Nurs 2004;8:68–80. 10.1016/j.cein.2004.11.001 [DOI] [Google Scholar]
- 28.Pande A, Krishnamoorthy G, Moulick ND. Hypoglycaemic and hypolipidaemic effects of low GI and medium GL Indian diets in type 2 diabetics for a period of 4 weeks: a prospective study. Int J Food Sci Nutr 2012;63:649–58. 10.3109/09637486.2011.649247 [DOI] [PubMed] [Google Scholar]
- 29.Malathy R, Narmadha M, Ramesh S et al. Effect of a diabetes counseling programme on knowledge, attitude and practice among diabetic patients in Erode district of South India. J Young Pharm 2011;3:65–72. 10.4103/0975-1483.76422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shenoy S, Arora E, Jaspal S. Effects of progressive resistance training and aerobic exercise on type 2 diabetics in Indian population. Int J Diabetes Metab 2009;17:27–30. [Google Scholar]
- 31.Arora E, Shenoy S, Sandhu JS. Effects of resistance training on metabolic profile of adults with type 2 diabetes. Indian J Med Res 2009;129:515–19. [PubMed] [Google Scholar]
- 32.Shenoy S, Guglani R, Sandhu JS. Effectiveness of an aerobic walking program using heart rate monitor and pedometer on the parameters of diabetes control in Asian Indians with type 2 diabetes. Prim Care Diabetes 2010;4:41–5. 10.1016/j.pcd.2009.10.004 [DOI] [PubMed] [Google Scholar]
- 33.Shetty AS, Chamukuttan S, Nanditha A et al. Reinforcement of adherence to prescription recommendations in Asian Indian diabetes patients using short message service (SMS)—a pilot study. J Assoc Physicians India 2011;59:711–14. [PubMed] [Google Scholar]
- 34.Singh S, Malhotra V, Singh KP et al. Role of yoga in modifying certain cardiovascular functions in type 2 diabetic patients. J Assoc Physicians India 2004;52:203–6. [PubMed] [Google Scholar]
- 35.Madanmohan ABB, Dayanidy G, Sanjay Z et al. Effect of yoga therapy on reaction time, biochemical parameters and wellness score of peri and post-menopausal diabetic patients. Int J Yoga 2012;5:10–15. 10.4103/0973-6131.91696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hawthorne K, Robles Y, Cannings-John R et al. Culturally appropriate health education for Type 2 diabetes in ethnic minority groups: a systematic and narrative review of randomized controlled trials. Diabet Med 2010;27:613–23. 10.1111/j.1464-5491.2010.02954.x [DOI] [PubMed] [Google Scholar]
- 37.Hawthorne K, Robles Y, Cannings-John R et al. Culturally appropriate health education for type 2 diabetes mellitus in ethnic minority groups. Cochrane Database Syst Rev 2008;16:3. [DOI] [PubMed] [Google Scholar]
- 38.Liu JJ, Davidson E, Bhopal RS et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technology Assessment 2012;16:1–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ricci-Cabello I, Ruiz-Pérez I, Rojas-García A et al. Characteristics and effectiveness of diabetes self-management educational programs targeted to racial/ethnic minority groups: a systematic review, meta-analysis and meta-regression. BMC Endocr Disord 2014;14:60 10.1186/1472-6823-14-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lorig KR, Ritter PL, González VM. Hispanic chronic disease self-management: a randomized community-based outcome trial. Nurs Res 2003;52:361–9. 10.1097/00006199-200311000-00003 [DOI] [PubMed] [Google Scholar]
- 41.Resnicow K, Baranowski T, Ahluwalia JS et al. Cultural sensitivity in public health: defined and demystified. Ethn Dis 1999;9:10–21. [PubMed] [Google Scholar]
- 42.Carlson KD, Schmidt F. Impact of experimental design on effect size: findings from the research literature on training. J Appl Psychol 1999;84:851–62. 10.1037/0021-9010.84.6.851 [DOI] [Google Scholar]
- 43.Hussain-Gambles M, Leese B, Atkin K et al. Involving South Asian patients in clinical trials. Health Technol Assess 2004;8:iii, 1–109 10.3310/hta8420 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2015-008986supp.pdf (96.1KB, pdf)