Abstract
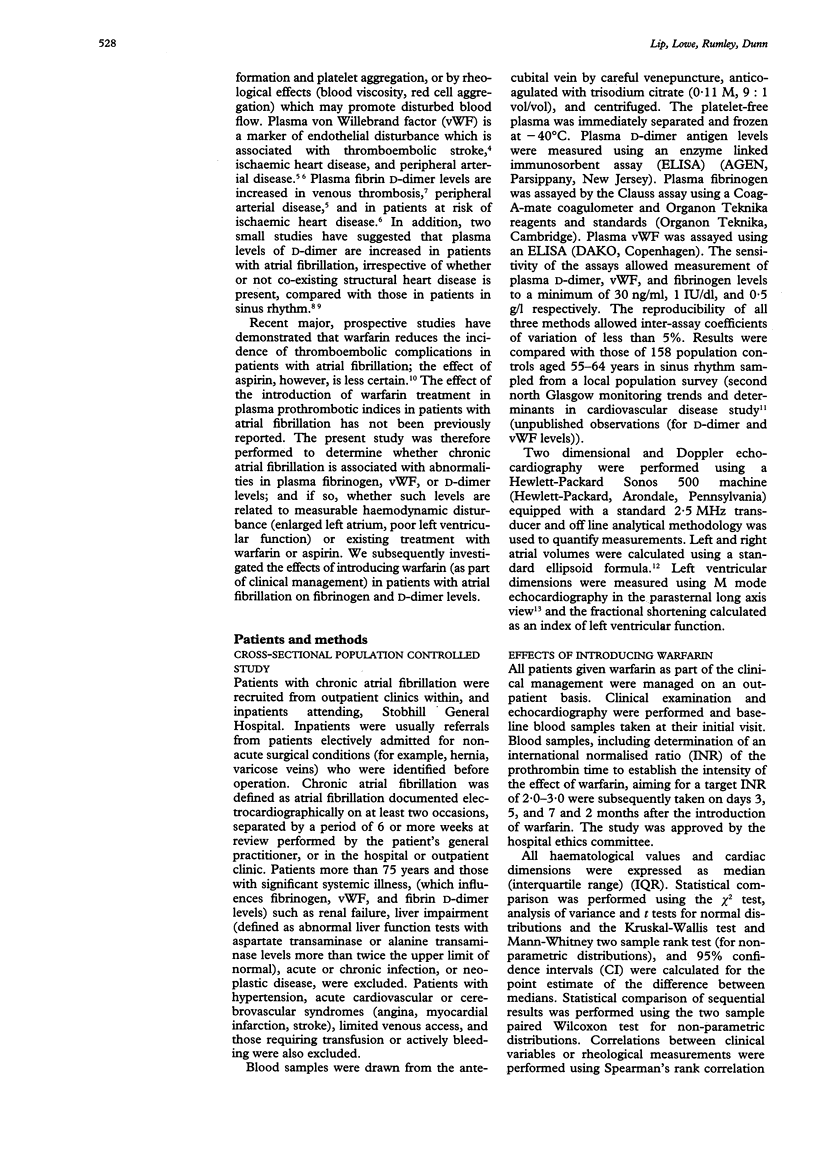
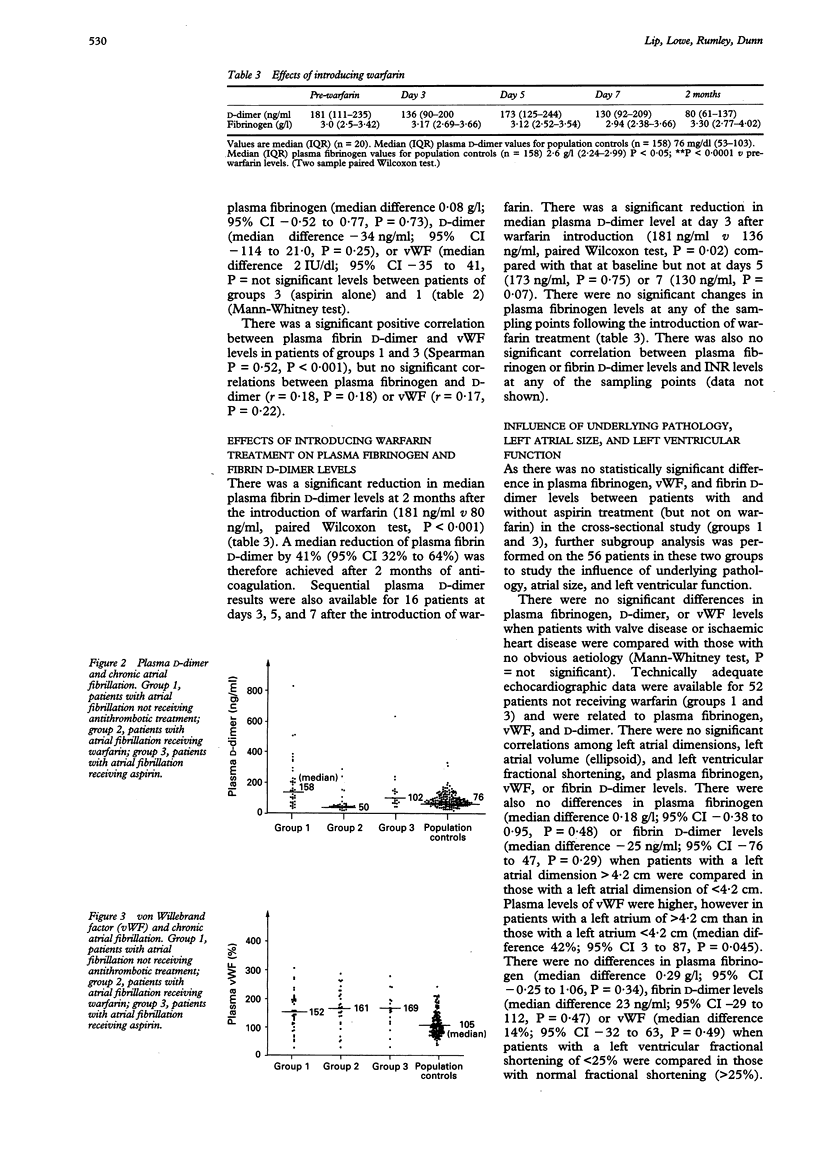
OBJECTIVE--To determine whether chronic atrial fibrillation is associated with abnormalities in plasma fibrinogen, von Willebrand factor (vWF) (a marker of endothelial disturbance), or fibrin D- dimer (a measure of fibrin turnover); and if so, whether such levels are related to haemodynamic disturbance (enlarged left atrium, poor left ventricular function) or existing treatment with warfarin or aspirin. To investigate the effects of introducing warfarin in patients with atrial fibrillation on fibrinogen and D- dimer levels. DESIGN--Cross sectional population sample controlled study and longitudinal study of patients undergoing anticoagulation. SETTING--District general hospital. SUBJECTS--87 patients (44 men and 43 women of mean (SEM) age 63.0 (1.0)) with chronic atrial fibrillation. At the time of the study, 37 were taking no antithrombotic medication (group 1), 31 were taking warfarin (including two on warfarin and aspirin) (group 2) and 19 were taking aspirin alone (group 3). They were compared with 158 population controls from a random population sample (the second Glasgow monitoring trends and determinants in cardiovascular disease study). As part of clinical treatment warfarin was introduced in 20 patients with chronic atrial fibrillation (14 men and six women of mean (SEM) (range) age 63.9 (2.35 (32-74) years). RESULTS--Plasma fibrinogen remained significantly increased in patients of group 1 (no antithrombotic medication) compared with that of the population controls (median difference 1.23 g/l; 95% confidence interval (CI) 0.88 to 1.62, P < 0.0001). There was also a significant increase in plasma D-dimer levels (median difference 77 ng/ml; 95% CI 38 to 122, P < 0.01) and vWF (median difference 63 IU/dl; 95% CI 38 to 89, P < 0.0001). There was no significant difference in plasma fibrinogen (median difference 0.14 g/l; 95% CI -0.44 to 0.77, P = 0.65) or vWF (median difference 3.5 IU/dl; 95% CI - 41 to 41, P = not significant in patients of group 2 (warfarin treatment) compared with that of patients in group 1. Levels of D-dimer were significantly lower in group 2 (median difference 90 ng/ml, 95% CI 39 to 150, P < 0.0001) than in group 1. There were no significant differences in plasma fibrinogen (median difference 0.08 g/l; 95% CI - 0.52 to 0.77, P = 0.73), D-dimer (median difference - 34 ng/ml; 95% CI - 114 to 21.0, P = 0.25), or vWF (median difference 2%; 95% CI - 35 to 41, P = not significant) levels between patients of groups 1 and 3. There were no significant correlations between the coagulation indices and left atrial volume or ventricular function. There was a significant positive correlation between plasma fibrin D-dimer and vWF levels in patients of groups 1 and 3 (r = 0.52, P < 0.001). There was a significant reduction in median plasma fibrin D-dimer levels at 2 months after the introduction of warfarin (181 ng/ml v 80 ng/ml, P < 0.001), but no effect on plasma fibrinogen. CONCLUSIONS--Increased median plasma fibrinogen and vWF levels were found in patients with chronic atrial fibrillation. Plasma D-dimer levels were also increased in patients with chronic atrial fibrillation not receiving warfarin, suggesting increased intravascular thrombogenesis in such patients. Introduction of warfarin normalised circulating fibrin D- dimer levels, suggesting that warfarin treatment was effective in preventing excessive fibrin turnover, consistent with the antithrombotic effects of warfarin. These results suggest three possible thrombotic markers to assess patients with atrial fibrillation who are at high risk of thrombogenesis; D-dimer also merits assessment as a measure of reduction in thrombotic risk in patients receiving warfarin.
Full text
PDF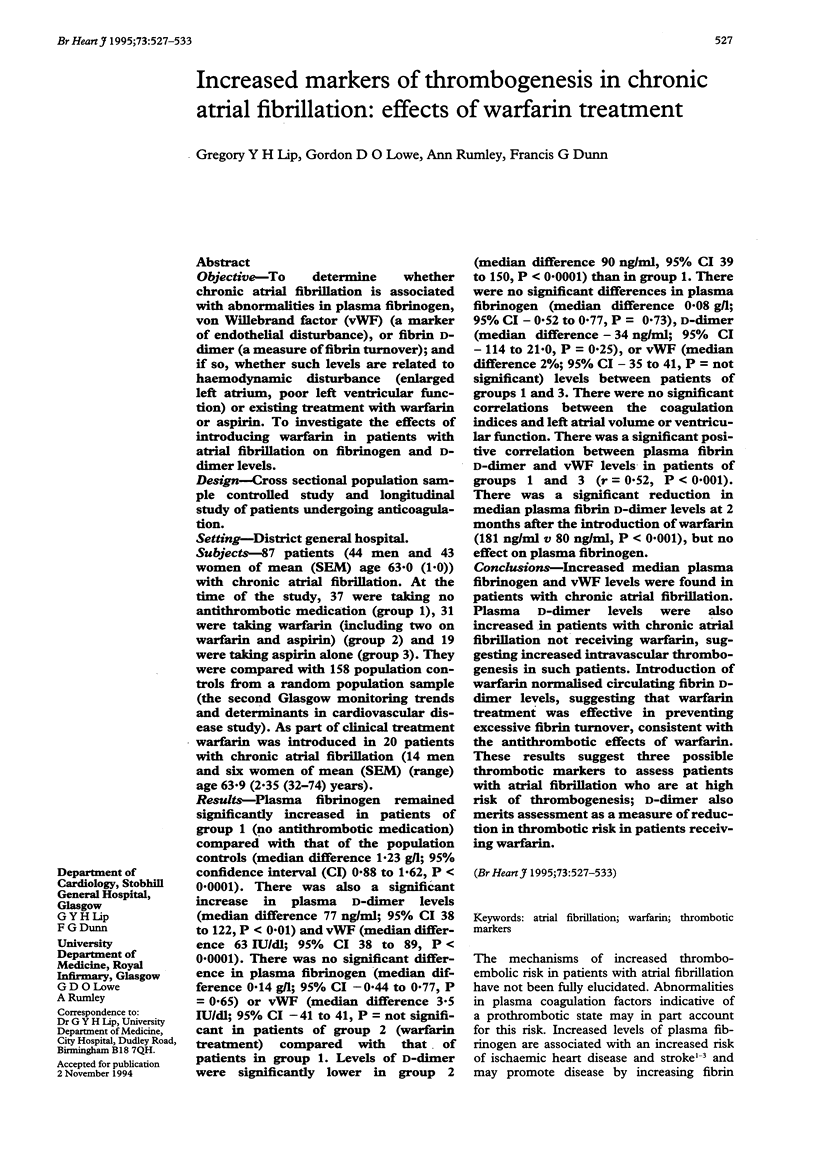

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Banerjee A. K., Pearson J., Gilliland E. L., Goss D., Lewis J. D., Stirling Y., Meade T. W. A six year prospective study of fibrinogen and other risk factors associated with mortality in stable claudicants. Thromb Haemost. 1992 Sep 7;68(3):261–263. [PubMed] [Google Scholar]
- Ernst E., Resch K. L. Fibrinogen as a cardiovascular risk factor: a meta-analysis and review of the literature. Ann Intern Med. 1993 Jun 15;118(12):956–963. doi: 10.7326/0003-4819-118-12-199306150-00008. [DOI] [PubMed] [Google Scholar]
- Fowkes F. G., Lowe G. D., Housley E., Rattray A., Rumley A., Elton R. A., MacGregor I. R., Dawes J. Cross-linked fibrin degradation products, progression of peripheral arterial disease, and risk of coronary heart disease. Lancet. 1993 Jul 10;342(8863):84–86. doi: 10.1016/0140-6736(93)91288-w. [DOI] [PubMed] [Google Scholar]
- Gustafsson C., Blombäck M., Britton M., Hamsten A., Svensson J. Coagulation factors and the increased risk of stroke in nonvalvular atrial fibrillation. Stroke. 1990 Jan;21(1):47–51. doi: 10.1161/01.str.21.1.47. [DOI] [PubMed] [Google Scholar]
- Hunt F. A., Rylatt D. B., Hart R. A., Bundesen P. G. Serum crosslinked fibrin (XDP) and fibrinogen/fibrin degradation products (FDP) in disorders associated with activation of the coagulation or fibrinolytic systems. Br J Haematol. 1985 Aug;60(4):715–722. doi: 10.1111/j.1365-2141.1985.tb07476.x. [DOI] [PubMed] [Google Scholar]
- Jansson J. H., Nilsson T. K., Johnson O. von Willebrand factor in plasma: a novel risk factor for recurrent myocardial infarction and death. Br Heart J. 1991 Nov;66(5):351–355. doi: 10.1136/hrt.66.5.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumagai K., Fukunami M., Ohmori M., Kitabatake A., Kamada T., Hoki N. Increased intracardiovascular clotting in patients with chronic atrial fibrillation. J Am Coll Cardiol. 1990 Aug;16(2):377–380. doi: 10.1016/0735-1097(90)90589-h. [DOI] [PubMed] [Google Scholar]
- Lowe G. D. Antithrombotic treatment and atrial fibrillation. BMJ. 1992 Dec 12;305(6867):1445–1446. doi: 10.1136/bmj.305.6867.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade T. W., North W. R., Chakrabarti R., Stirling Y., Haines A. P., Thompson S. G., Brozovié M. Haemostatic function and cardiovascular death: early results of a prospective study. Lancet. 1980 May 17;1(8177):1050–1054. doi: 10.1016/s0140-6736(80)91498-1. [DOI] [PubMed] [Google Scholar]
- Ramsay L. E. Warfarin in chronic atrial fibrillation. Lancet. 1993 May 29;341(8857):1376–1377. doi: 10.1016/0140-6736(93)90945-d. [DOI] [PubMed] [Google Scholar]
- Ritchie D. G., Levy B. A., Adams M. A., Fuller G. M. Regulation of fibrinogen synthesis by plasmin-derived fragments of fibrinogen and fibrin: an indirect feedback pathway. Proc Natl Acad Sci U S A. 1982 Mar;79(5):1530–1534. doi: 10.1073/pnas.79.5.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahn D. J., DeMaria A., Kisslo J., Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978 Dec;58(6):1072–1083. doi: 10.1161/01.cir.58.6.1072. [DOI] [PubMed] [Google Scholar]
- Sanfilippo A. J., Abascal V. M., Sheehan M., Oertel L. B., Harrigan P., Hughes R. A., Weyman A. E. Atrial enlargement as a consequence of atrial fibrillation. A prospective echocardiographic study. Circulation. 1990 Sep;82(3):792–797. doi: 10.1161/01.cir.82.3.792. [DOI] [PubMed] [Google Scholar]
- Smith F. B., Lowe G. D., Fowkes F. G., Rumley A., Rumley A. G., Donnan P. T., Housley E. Smoking, haemostatic factors and lipid peroxides in a population case control study of peripheral arterial disease. Atherosclerosis. 1993 Sep;102(2):155–162. doi: 10.1016/0021-9150(93)90157-p. [DOI] [PubMed] [Google Scholar]
- Uchiyama S., Takeuchi M., Osawa M., Kobayashi I., Maruyama S., Aosaki M., Hirosawa K. Platelet function tests in thrombotic cerebrovascular disorders. Stroke. 1983 Jul-Aug;14(4):511–517. doi: 10.1161/01.str.14.4.511. [DOI] [PubMed] [Google Scholar]
- Wilhelmsen L., Svärdsudd K., Korsan-Bengtsen K., Larsson B., Welin L., Tibblin G. Fibrinogen as a risk factor for stroke and myocardial infarction. N Engl J Med. 1984 Aug 23;311(8):501–505. doi: 10.1056/NEJM198408233110804. [DOI] [PubMed] [Google Scholar]
- Yamamoto K., Ikeda U., Shimada K. A hypercoagulable state in the left atrium of patients with mitral stenosis. N Engl J Med. 1993 Apr 8;328(14):1043–1044. doi: 10.1056/NEJM199304083281415. [DOI] [PubMed] [Google Scholar]



