Abstract
OBJECTIVE
To examine the magnitude and types of hospitalizations among persons with prediabetes, undiagnosed diabetes, and diagnosed diabetes.
RESEARCH DESIGN AND METHODS
This study included 13,522 participants in the Atherosclerosis Risk in Communities (ARIC) study (mean age 57 years, 56% female, 24% black, 18% with prediabetes, 4% with undiagnosed diabetes, 9% with diagnosed diabetes) with follow-up in 1990–2011 for hospitalizations. Participants were categorized by diabetes/HbA1c status: without diagnosed diabetes, HbA1c <5.7% (reference); prediabetes, 5.7 to <6.5%; undiagnosed diabetes, ≥6.5%; and diagnosed diabetes, <7.0 and ≥7.0%.
RESULTS
Demographic adjusted rates per 1,000 person-years of all-cause hospitalizations were higher with increasing diabetes/HbA1c category (Ptrend < 0.001). Persons with diagnosed diabetes and HbA1c ≥7.0% had the highest rates of hospitalization (3.1 times higher than those without a history of diagnosed diabetes, HbA1c <5.7%, and 1.5 times higher than those with diagnosed diabetes, HbA1c <7.0%, P < 0.001 for both comparisons). Persons with undiagnosed diabetes had 1.6 times higher rates of hospitalization and those with prediabetes had 1.3 times higher rates of hospitalization than those without diabetes and HbA1c <5.7% (P < 0.001 for both comparisons). Rates of hospitalization by diabetes/HbA1c category were different by race (Pinteraction = 0.011) and by sex (Pinteraction = 0.020). There were significantly excess rates of hospitalizations due to cardiovascular, endocrine, respiratory, gastrointestinal, iatrogenic/injury, neoplasm, genitourinary, neurologic, and infection causes among those with diagnosed diabetes compared with those without a history of diagnosed diabetes (all P < 0.05).
CONCLUSIONS
Persons with diagnosed diabetes, undiagnosed diabetes, and prediabetes are at a significantly elevated risk of hospitalization compared with those without diabetes. Substantial excess rates of hospitalizations in persons with diagnosed diabetes were for endocrine, infection, and iatrogenic/injury causes, which may be preventable with improved diabetes care.
Introduction
The burden of diabetes and prediabetes in the U.S. is high (1,2). Approximately 21 million adults aged 20 years or older had either diagnosed or undiagnosed diabetes in 2010 (1). Diabetes represents a significant and increasing proportion of U.S. health care costs (3,4). In 2012, the total estimated cost of diagnosed diabetes was 245 billion dollars (compared with 174 billion dollars in 2007) (5,6). Overall, inpatient hospitalizations account for the majority of all medical expenditures (7). Indeed, the largest component of diabetes-related medical expenditures in 2012 was related to inpatient hospital care, which comprised ∼43% of the total estimated cost (5). However, the magnitude of risk of all-cause hospitalization and the different causes of hospitalizations that occur among persons with prediabetes and persons with diabetes are not well characterized.
The objective of this study was to examine the relationships between prediabetes, undiagnosed diabetes, and diagnosed diabetes with all-cause and cause-specific hospitalizations occurring over a median of 20 years of follow-up among middle-aged white and black persons in the community-based Atherosclerosis Risk in Communities (ARIC) study and to evaluate possible interactions by age, race, and sex. We hypothesized that persons with prediabetes, undiagnosed diabetes, and diagnosed diabetes would have higher rates of hospitalization, especially from cardiovascular causes, than those without diabetes and that, in addition to endocrine causes, infectious and iatrogenic/injury (e.g., postoperative complications, fractures, etc.) causes would represent a substantial burden of hospitalizations among persons with diabetes. We further hypothesized that among persons with diagnosed diabetes, higher HbA1c (≥7.0%) would be associated with higher rates of all-cause hospitalization compared with those with lower HbA1c (<7.0%).
Research Design and Methods
Study Population
The ARIC study population is comprised of an ongoing, prospective cohort of 15,792 participants recruited in 1987–1989 (visit 1) from four sites: suburbs of Minneapolis, MN; Washington County, MD; Forsyth County, NC; and Jackson, MS (8). Participants have subsequently attended four additional in-person visits in 1990–1992 (visit 2), 1993–1995 (visit 3), 1996–1998 (visit 4), and 2011–2013 (visit 5). The ARIC study has been approved by the institutional review boards of all participating institutions, and all participants gave written informed consent at each study visit.
HbA1c was first measured at ARIC visit 2; therefore, visit 2 (1990–1992) is the baseline for the current study. Of the 14,348 participants who attended ARIC visit 2, we excluded 283 participants missing HbA1c or fasting glucose data, 90 participants of self-reported nonwhite and nonblack race or of black race from the Minnesota or Maryland sites, 3 participants without follow-up after visit 2, and 450 participants missing data on covariates included in statistical models, leaving a total of 13,522 participants included in the present analyses.
Definition of Diabetes and Measurement of HbA1c and Fasting Glucose
Diagnosed diabetes at visit 2 was defined by self-report of a physician diagnosis or diabetes medication use. Frozen whole-blood samples collected at ARIC visit 2 (1990–1992) were thawed and assayed for the measurement of HbA1c using high-performance liquid chromatography (Tosoh A1c 2.2 Plus Glycohemoglobin Analyzer method in 2003–2004 and Tosoh G7 method in 2007–2008, Tosoh Corporation, Tokyo, Japan) (9). Both instruments were standardized to the Diabetes Control and Complications Trial assay (10). Glucose was measured in 1990–1992 using the hexokinase method. All participants were asked at each visit if they wanted abnormal laboratory results sent to their primary care physician for clinical interpretation. If abnormal (defined as ≥140 mg/dL in 1990–1992), fasting glucose results would be sent to the primary care doctor of participants who opted in for notification. However, since HbA1c was measured >10 years after blood samples were drawn, data on HbA1c were not sent to primary care physicians.
We categorized persons without a history of diagnosed diabetes according to clinical categories of HbA1c: <5.7% (reference), 5.7 to <6.5% (prediabetes), and ≥6.5% (undiagnosed diabetes) (11). In our main analysis, participants with diagnosed diabetes were categorized as having HbA1c <7.0 or ≥7.0% (12,13). We additionally performed a sensitivity analysis using an HbA1c cut point of 8.0% (12,13). In supplementary analyses, we classified participants by diabetes/fasting glucose category. Participants without a history of diagnosed diabetes were classified as follows: <100 mg/dL (reference), 100 to <126 mg/dL (prediabetes), and ≥126 mg/dL (undiagnosed diabetes) (11). Participants with diagnosed diabetes were classified as having fasting glucose <150 or ≥150 mg/dL.
Ascertainment of Hospitalizations and Definition of Hospitalization Categories
We used data that the ARIC study ascertained through hospitalization reports from annual telephone contact with study participants and through active surveillance of hospitalizations occurring in the study community hospitals. For the current study, follow-up was available from baseline through 31 December 2011. The first ICD-9 code listed in the hospital discharge documentation defined the primary cause for hospitalization.
Our main outcome was counts of all-cause hospitalizations. We categorized the primary cause of each hospitalization using the Clinical Classification Software developed by the Agency for Healthcare Research and Quality (https://www.hcupus.ahrq.gov/toolssoftware/ccs/ccs.jsp) (14). The primary cause of each hospitalization was classified into 18 systems-based categories and then subclassified into 285 disease-based categories (14). In sensitivity analyses, we recategorized all infection-related ICD-9 diagnoses to create a more comprehensive infection category, as not all ICD-9 codes that identified infection were classified in the infection category as defined by the Clinical Classification Software (for example, pneumonia was classified under the respiratory system and not the infection category with use of the Clinical Classification Software).
Statistical Analyses
Baseline characteristics of the study population are shown by diabetes/HbA1c category. t tests were used to compare means for continuous variables, and χ2 tests were used to compare proportions for categorical variables. Numbers of all-cause and cause-specific hospitalizations were tabulated by diabetes/HbA1c category. Crude rates of all-cause hospitalization were calculated by diabetes/HbA1c category and by 10-year age categories (<60, 60–69, 70–79, and ≥80 years, with each participant contributing person-time and events to separate 10-year age bins from baseline to death or censoring). Negative binomial regression models were used to calculate adjusted rates of hospitalization per 1,000 person-years (95% CI) when all continuous covariates were set to mean values and all categorical covariates were set to the reference group by diabetes/HbA1c category, with persons with no history of diagnosed diabetes and HbA1c <5.7% serving as the reference group. In the negative binomial regression models, follow-up time (defined as the time from baseline [visit 2] to censoring [31 December 2011] or death) was an offset variable, which serves to account for the competing risk of death. The negative binomial model was preferred over the Poisson model for our data due to overdispersion (likelihood ratio test of α = 0 was significant at P < 0.001). We tested for linear trend across the median of the diabetes/HbA1c categories. In additional sensitivity analyses, we also considered zero-inflated negative binomial models to calculate adjusted rates of hospitalization per 1,000 person-years (95% CI) by diabetes/HbA1c category because 23% of our population was never hospitalized during follow-up. Akaike information criterion and the Vuong test were used to assess goodness of fit for our models. In additional sensitivity analyses, we used negative binomial regression models to calculate adjusted rates of hospitalization per 1,000 person-years (95% CI) when all continuous covariates were set to mean values and all categorical covariates were set to the reference group by diabetes/fasting glucose category. We formally tested for multiplicative interaction by age, race, and sex in our main statistical models.
All covariates used in statistical models were assessed at visit 2 (1990–1992) unless otherwise stated. Covariates in the main statistical model included the following: age (continuous), sex (male, female), race/center (Minnesota whites [reference], Maryland whites, North Carolina whites, North Carolina blacks, Mississippi blacks), and health insurance (yes, no [reference]). We additionally ran a model further adjusted for the Charlson Comorbidity Index (dichotomized as low comorbidity burden [score <2] vs. high comorbidity burden [score ≥2]) (15–17). A supplemental statistical model added the following covariates: education (<high school [reference]; high school or equivalent; college, graduate or professional school; assessed at visit 1), family income (<$35,000/year [reference], ≥$35,000/year, not reported), BMI (continuous [measured as weight in kilograms divided by the square of height in meters]), cigarette smoking (current, former, never [reference]), alcohol consumption (current, former, never [reference]), systolic and diastolic blood pressure (continuous [mmHg]), hypertension medication use (yes, no [reference]), coronary heart disease (yes, no [reference]), total and HDL cholesterol (continuous [mg/dL]), cholesterol medication use (yes, no [reference]), and estimated glomerular filtration rate (continuous; calculated using the Chronic Kidney Disease Epidemiology Collaboration formula [18]).
Since we were unable to perform analyses using time-varying diabetes/HbA1c categories (as HbA1c was only measured at visit 2 in 1990–1992), we performed sensitivity analyses where we limited follow-up time to 5 and 10 years after baseline (when diabetes/HbA1c category was defined) in order to investigate the possible influence of those with prediabetes and undiagnosed diabetes later being diagnosed with diabetes on associations of baseline diabetes/HbA1c category with future hospitalization risk. We additionally performed a sensitivity analysis to assess the impact of diabetes duration. In this analysis, a covariate was added to our model split at diabetes duration of 3 years (<3 years [diagnosed with diabetes between ARIC visits 1 and 2] vs. >3 years [diagnosed with diabetes prior to ARIC visit 1]).
All reported P values were based on two-sided tests, and P < 0.05 was considered statistically significant. Analyses were performed using Stata, version 13 (StataCorp, College Station, TX).
Results
Baseline characteristics (ARIC visit 2, 1990–1992) of the study population are shown by HbA1c/diabetes category in Table 1. Overall, mean age of participants was 57 years, 56% were female, 24% were black, 17.8% had prediabetes, 4.1% had undiagnosed diabetes, and 9.3% had diagnosed diabetes. Compared with those without a history of diagnosed diabetes and HbA1c <5.7%, those with prediabetes (HbA1c 5.7 to <6.5% and no diabetes diagnosis history) were older (58 vs. 57 years, P < 0.001), more likely to be of black race (40 vs. 16%, P < 0.001), and more likely to have higher BMI (29 vs. 27 kg/m2, P < 0.001). Similarly, those with undiagnosed diabetes (HbA1c ≥6.5% and no diabetes diagnosis history) were older (58 vs. 57 years, P < 0.001), more likely to be of black race (51 vs. 16%, P < 0.001), and less likely to have health insurance (83 vs. 94%, P < 0.001) compared with those without a history of diagnosed diabetes and HbA1c <5.7%. Among persons with diagnosed diabetes, those with HbA1c <7.0 vs. ≥7.0% were of similar age (58 years, P = 0.732), but those with diabetes and HbA1c <7.0% were less likely to be of black race (34 vs. 49%, P < 0.001). Cumulative mortality by the end of follow-up was higher with increasing diabetes/HbA1c category (Ptrend < 0.001).
Table 1.
Participant characteristics by baseline diabetes and HbA1c category: the ARIC study, visit 2 (1990–1992)
| No history of diagnosed diabetes |
Diagnosed diabetes |
||||
|---|---|---|---|---|---|
| HbA1c <5.7% | HbA1c 5.7 to <6.5%: prediabetes | HbA1c ≥6.5%: undiagnosed diabetes | HbA1c <7.0% | HbA1c ≥7.0% | |
| n | 9,267 | 2,441 | 553 | 422 | 839 |
| Age (years), mean (SD) | 56.5 (5.7) | 58.0 (5.7) | 57.8 (5.7) | 58.5 (5.7) | 58.4 (5.7) |
| Female, % | 56.1 | 52.5 | 58.2 | 53.6 | 57.7 |
| Race, % | |||||
| White | 84.4 | 60.1 | 49.6 | 66.1 | 51.3 |
| Black | 15.6 | 39.9 | 50.5 | 33.9 | 48.8 |
| Education, % | |||||
| <High school | 16.4 | 30.3 | 34.5 | 35.6 | 37.4 |
| High school, GED, or vocational school | 43.3 | 38.6 | 35.4 | 38.2 | 37.9 |
| College, graduate, or professional school | 40.3 | 31.1 | 30.0 | 27.3 | 24.7 |
| Income ($), % | |||||
| <35,000/year | 44.9 | 60.8 | 65.6 | 66.8 | 70.0 |
| ≥35,000/year | 49.6 | 33.3 | 26.4 | 27.0 | 23.8 |
| Not reported | 5.5 | 6.0 | 8.0 | 6.2 | 6.2 |
| Health insurance, % | 93.7 | 88.5 | 82.5 | 88.2 | 85.3 |
| Charlson Comorbidity Index ≥2, % | 34.7 | 45.5 | 45.9 | 53.1 | 52.1 |
| Smoking status, % | |||||
| Never | 40.7 | 34.3 | 38.9 | 38.9 | 45.7 |
| Former | 38.6 | 36.1 | 37.3 | 37.7 | 37.7 |
| Current | 20.7 | 29.6 | 23.9 | 23.5 | 16.7 |
| Alcohol consumption, % | |||||
| Never | 20.4 | 24.4 | 30.0 | 26.5 | 33.3 |
| Former | 17.2 | 26.1 | 28.9 | 33.4 | 36.8 |
| Current | 62.5 | 49.5 | 41.1 | 40.1 | 29.9 |
| BMI (kg/m2), mean (SD) | 27.0 (4.8) | 29.2 (5.8) | 32.4 (6.1) | 29.9 (5.9) | 31.4 (6.0) |
| Hypertension, % | 28.9 | 44.2 | 57.0 | 54.8 | 63.1 |
| Systolic blood pressure (mmHg), mean (SD) | 119.4 (18.1) | 124.5 (19.1) | 128.1 (17.7) | 127.2 (20.7) | 128.4 (20.3) |
| Diastolic blood pressure (mmHg), mean (SD) | 71.8 (10.2) | 73.3 (10.2) | 74.2 (10.4) | 71.2 (10.2) | 71.0 (10.4) |
| Hypertension medication use, % | 25.8 | 41.7 | 57.0 | 54.8 | 63.1 |
| Coronary heart disease, % | 4.5 | 7.1 | 6.5 | 10.7 | 14.9 |
| Total cholesterol (mg/dL), mean (SD) | 207.6 (38.0) | 213.3 (39.9) | 217.6 (42.1) | 206.3 (40.0) | 217.8 (49.4) |
| HDL cholesterol (mg/dL), mean (SD) | 51.4 (17.2) | 46.9 (14.9) | 42.9 (13.8) | 44.8 (14.6) | 42.4 (14.4) |
| Cholesterol medication use, % | 5.6 | 7.1 | 7.6 | 10.7 | 11.7 |
| Estimated glomerular filtration rate <60 mL/min/1.73 m2, % | 1.4 | 2.4 | 2.9 | 6.9 | 6.8 |
| Mortality by end of follow-up, % | 23.7 | 38.8 | 42.7 | 48.6 | 63.4 |
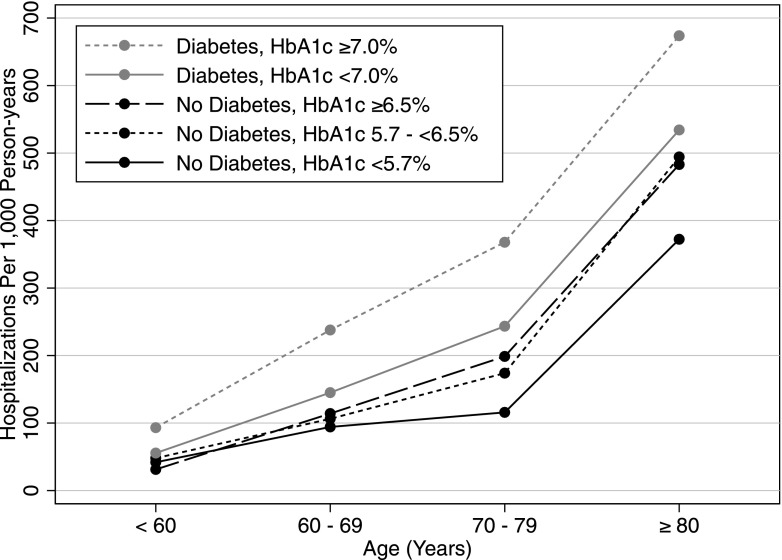
Supplementary Fig. 1 shows the crude number of all-cause hospitalizations by diabetes/HbA1c category over a median of 20 years of follow-up. As HbA1c category increased, the number of hospitalizations per person was higher, with only 3.7% of participants without a history of diagnosed diabetes and HbA1c <5.7% having ≥10 hospitalizations, compared with 13.5% of those with diagnosed diabetes and HbA1c <7.0% and 18.2% of those with diagnosed diabetes and HbA1c ≥7.0%. The crude rates per 1,000 person-years of all cause-hospitalization by 10-year age-group and by baseline diabetes/HbA1c category are shown in Fig. 1. Rates of all-cause hospitalization were higher at older ages and were highest among persons with higher HbA1c at baseline (age <60 years, no history of diagnosed diabetes, and HbA1c <5.7%, 41.9 per 1,000 person-years, vs. diagnosed diabetes and HbA1c ≥7.0%, 93.2 per 1,000 person-years; age ≥80 years, no history of diagnosed diabetes, and HbA1c <5.7%, 372.3 per 1,000 person-years, vs. diagnosed diabetes and HbA1c ≥7.0%, 673.8 per 1,000 person-years).
Figure 1.
Crude rates of all-cause hospitalization per 1,000 person-years by 10-year age-group and by baseline (1990–1992) diabetes and HbA1c category: the ARIC study, 1990–2011.
Table 2 shows the demographic adjusted rates per 1,000 person-years (95% CI) of all-cause hospitalizations by diabetes and HbA1c category from negative binomial regression models. Overall, the demographic adjusted rates per 1,000 person-years of all-cause hospitalizations were higher with increasing diabetes/HbA1c category (Ptrend < 0.001). Persons with diagnosed diabetes and HbA1c ≥7.0% had the highest rates of hospitalization (3.1 times higher than those without a history of diagnosed diabetes and HbA1c <5.7%, P < 0.001). Among those with diagnosed diabetes, those with HbA1c ≥7.0% had significantly higher demographic adjusted rate all-cause hospitalization (504 per 1,000 person-years [95% CI 462–547]) compared with those with HbA1c <7.0% (340 per 1,000 person-years [95% CI 297–384]) (P < 0.001). Among those without a history of diagnosed diabetes, persons with undiagnosed diabetes (HbA1c ≥6.5%) had 1.6 times higher rates of hospitalization and those with prediabetes (HbA1c 5.7 to <6.5%) had 1.3 times higher rates of hospitalization than those with HbA1c <5.7% (P < 0.001 for both comparisons). In tests of multiplicative interaction, rates of all-cause hospitalization across diabetes/HbA1c categories differed by race and sex but not by age. Rates of all-cause hospitalization by diabetes/HbA1c category were higher for blacks compared with whites for all diabetes/HbA1c categories except prediabetes (no history of diagnosed diabetes and HbA1c 5.7 <6.5%) and undiagnosed diabetes (no history of diagnosed diabetes and HbA1c ≥6.5%) (Pinteraction = 0.011). Rates of all-cause hospitalization by diabetes/HbA1c category were higher for men compared with women in all groups except for among those with diagnosed diabetes and HbA1c ≥7.0% (Pinteraction = 0.020). Rates among those who were older at baseline (>55 years) were consistently higher than among those who were younger at baseline (≤55 years) across all diabetes/HbA1c categories (Pinteraction = 0.141). The higher rates of all-cause hospitalization per 1,000 person-years across diabetes/HbA1c categories were slightly attenuated but remained significant with further adjustment for the Charlson Comorbidity Index (Supplementary Table 1) and for social/lifestyle and cardiovascular disease risk factors (Supplementary Table 2). When an HbA1c cut point of 8.0% instead of 7.0% was used to characterize glycemic control among those with diagnosed diabetes, patterns of all-cause hospitalization were similar but with higher rates of all-cause hospitalization in persons with HbA1c ≥8.0% compared with HbA1c ≥7.0% (548 vs. 504 all-cause hospitalizations per 1,000 person-years, respectively) (Supplementary Table 3). The pattern of higher rates of all-cause hospitalization per 1,000 person-years across diabetes/HbA1c categories remained present when using zero-inflated negative binomial regression models (Supplementary Table 4). The pattern of higher rates of all-cause hospitalization per 1,000 person-years with increasing glycemic category remained present when participants were categorized by diabetes/fasting glucose category (Supplementary Table 5). In sensitivity analyses limiting follow-up time to 5 and 10 years after baseline, associations of diabetes/HbA1c category with hospitalization risk remained statistically significant (P < 0.001 for prediabetes [no history of diagnosed diabetes and HbA1c 5.7 to <6.5%], undiagnosed diabetes [no history of diagnosed diabetes and HbA1c ≥6.5%], and diagnosed diabetes with HbA1c <7.0 and ≥7.0% compared with no history of diagnosed diabetes and HbA1c <5.7% for follow-up times of both 5 and 10 years). In sensitivity analyses looking at the impact of diabetes duration, diabetes duration was moderately associated with risk of hospitalization, but this result was not significant at the P = 0.05 level (P = 0.102).
Table 2.
Demographic adjusted* rates of all-cause hospitalization per 1,000 person-years (95% CI) by baseline (1990–1992) diabetes and HbA1c category from negative binomial models: the ARIC study, 1990–2011
| No history of diagnosed diabetes |
Diagnosed diabetes |
Pinteraction§ | ||||
|---|---|---|---|---|---|---|
| HbA1c <5.7% | HbA1c 5.7 to <6.5% | HbA1c ≥6.5% | HbA1c <7.0% | HbA1c ≥7.0% | ||
| n | 9,267 | 2,441 | 553 | 422 | 839 | |
| Total hospitalizations, n | 24,972 | 8,668 | 2,221 | 2,113 | 5,098 | |
| Total person-years | 169,983 | 41,641 | 9,190 | 6,779 | 11,848 | |
| Overall | 163 (158–169) | 217 (206–228)** | 254 (226–281)** | 340 (297–384)** | 504 (462–547)**† | |
| By race | 0.011 | |||||
| White | 161 (156–166) | 223 (209–238)** | 263 (225–302)** | 297 (249–345)** | 473 (423–524)**† | |
| Black | 170 (155–185) | 209 (191–227)** | 251 (211–291)** | 433 (347–519)** | 552 (481–622)**† | |
| By sex | 0.020 | |||||
| Men | 186 (178–195) | 248 (230–266)** | 279 (231–327)** | 397 (316–477)** | 481 (424–537)**† | |
| Women | 146 (140–153) | 195 (180–209)** | 236 (203–269)** | 301 (253–350)** | 518 (459–578)**† | |
| By baseline age | 0.141 | |||||
| ≤55 years | 118 (111–124) | 163 (148–178)** | 181 (145–217)** | 280 (215–346)** | 416 (356–477)**† | |
| >55 years | 209 (201–218) | 270 (254–287)** | 329 (287–372)** | 405 (345–465)** | 599 (539–658)**† | |
*Adjusted for age, sex, race/center, and insurance status.
**P < 0.05, compared with HbA1c <5.7% (reference).
†P < 0.05, HbA1c ≥7.0 vs. <7.0% (reference).
§Multiplicative interaction term.
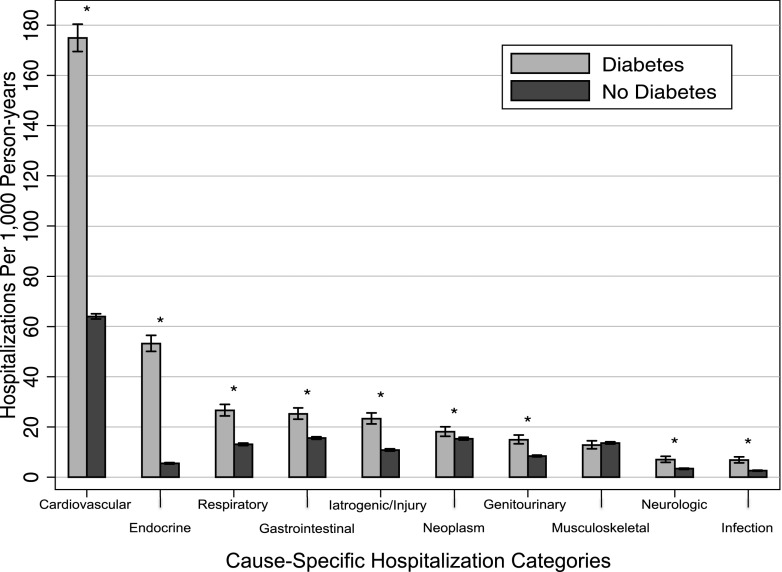
The primary causes for hospitalization are shown according to history of diagnosed diabetes status in Fig. 2. Cardiovascular disease was the most common primary cause for hospitalization among those with and without a history of diagnosed diabetes in (crude rate 174.9 [95% CI 169.5–180.4] and 63.9 [95% CI 62.9–65.0] hospitalizations per 1,000 person-years, respectively, P < 0.001); however, the most common specific cardiovascular diagnosis was coronary atherosclerosis for those without a history of diagnosed diabetes and congestive heart failure for those with diagnosed diabetes (Supplementary Table 5). There were significant excess rates of hospitalizations due to cardiovascular, endocrine, respiratory, gastrointestinal, iatrogenic/injury, neoplasm, genitourinary, neurologic, and infection causes among those with diagnosed diabetes compared with those without a history of diagnosed diabetes (all P < 0.05) (Fig. 2). In sensitivity analyses using a more comprehensive infection category definition, crude rates of hospitalizations with a primary cause of infection were 12.6 (95% CI 12.1–13.1) and 32.4 (95% CI 30.0–35.1) per 1,000 person-years among those without and with a history of diagnosed diabetes, respectively.
Figure 2.
Crude rates of cause-specific hospitalization per 1,000 person-years by baseline (1990–1992) diabetes status: the ARIC study, 1990–2011. *P < 0.05 comparing diabetes vs. no diabetes.
Conclusions
In this community-based population of middle-aged white and black persons, those with prediabetes, undiagnosed diabetes, and diagnosed diabetes had significantly higher rates of all-cause hospitalization over a median of 20 years of follow-up compared with those without a history of diagnosed diabetes and normal HbA1c (<5.7%), even after adjustment for insurance status and comorbidities. Further, among persons with diagnosed diabetes, those with poor glycemic control, as assessed by HbA1c, had higher rates of all-cause hospitalization compared with those with lower HbA1c. Consistent with prior studies (19,20), hospitalization rates across diabetes/HbA1c categories were higher for older versus younger individuals. Even after adjustment, hospitalization rates were higher in blacks versus whites among persons with diagnosed diabetes, suggesting that blacks with diabetes experience a higher burden of morbidity from diabetes compared with their white counterparts. Men had higher rates of hospitalization versus women (in all categories except for diagnosed diabetes with HbA1c ≥7.0%), which contrasts with evidence from epidemiologic studies showing no interaction by sex in the association of HbA1c with overall mortality (21,22). This observed sex difference in hospitalization rates suggests that while risk of mortality by HbA1c category may be similar by sex, men without a diabetes diagnosis or with well-controlled diabetes and women with poorly controlled diabetes are more likely to be hospitalized. We identified major causes of hospitalizations in persons with diabetes and showed substantial risk of hospitalizations for underlying endocrine causes (largely diabetes-related), infection (including pneumonia and urinary tract infections), and iatrogenic/injury causes (including complications of device/implant/graft, surgical complications, and fractures), all of which may be preventable with improved glycemic control.
Our study is consistent with previous studies that showed high rates of hospitalization among those with diabetes compared with those without diabetes (23–32) and studies of common causes for hospitalization among those with diabetes (23–25,33). However, in contrast to prior studies (23–25), we did not identify infectious causes as one of the most common causes of hospitalization (infection was ranked tenth). This may be in part due to the ICD-9 code classification system that we used in our primary analyses. While the Clinical Classification Software developed by the Agency for Healthcare Research and Quality (14) does have an infection category, not all ICD-9 codes that identify infection are classified in that category (for example, pneumonia is classified under the respiratory system and not under the infection category). Indeed, when we reclassified all ICD-9 codes that related to infection, we found that hospitalizations among those with diagnosed diabetes due to infectious causes occurred at a rate of 32 per 1,000 person-years—results that are more similar to prior studies (23–25).
Prior studies of hospitalization rates in persons with diabetes have been limited by cross-sectional designs (23,24), short follow-up (<5 years) (25,27,30–32), and/or by the use of ICD-9 codes to define diabetes status (23,24,26,27). Many prior studies also did not compare hospitalization risk in persons with prediabetes or undiagnosed diabetes (23–32) or evaluate potential differences by age, sex, and race (23–27,30,31). Our study had a median follow-up period of 20 years in a community-based population, and we were able to rigorously characterize and compare hospitalization risk among those with diagnosed diabetes by levels of HbA1c and in those at high risk prior to a formal diagnosis of diabetes (prediabetes and undiagnosed diabetes). Our results extend the literature by showing not only that diagnosed diabetes is associated with a higher risk of hospitalization but also that prediabetes and undiagnosed diabetes were associated with a significant excess rates of hospitalization later in life. Consistent with prior studies establishing that poorer glycemic control in midlife is associated with an increased risk of complications and mortality (21,34–36), we found that higher HbA1c values in persons with diagnosed diabetes were an important indicator of future hospitalization risk later life. Our results suggest that prevention of diabetes and improved management of diabetes could impact later-life hospitalization risk.
Certain limitations should be taken into consideration in the interpretation of this study. First, although we ascertained hospitalization data via both annual telephone contact with study participants and active surveillance of hospitalizations occurring in all study communities, some hospitalizations occurring among ARIC participants (e.g., hospitalizations outside of the surveillance areas that are not reported during follow-up telephone calls) are likely not captured in our data. Therefore, our results likely underestimate the true rates of hospitalization in our population. Second, we only had one measure of HbA1c, and we were thus unable to apply time-varying diabetes/HbA1c categories over follow-up. However, in sensitivity analyses where follow-up time was limited to 5 and 10 years after baseline, rates of all-cause hospitalization remained significantly higher for those with prediabetes and undiagnosed diabetes compared with those with normoglycemia, suggesting that prediabetes and undiagnosed diabetes represent groups at high risk that is not fully explained by a later diagnosis of diabetes. We also did not have detailed data on diabetes duration. However, we were able to look at diabetes duration split at 3 years (<3 years [diagnosed with diabetes between ARIC visits 1 and 2] vs. >3 years [diagnosed with diabetes prior to ARIC visit 1]), which was not significantly associated with hospitalization. Additionally, we observed differential mortality by diabetes/HbA1c category. Therefore, our relative hospitalization rates are likely an underestimation due to competing mortality risk, but we did include follow-up time as an offset variable in our regression models, which served as a means to account for this competing risk of death. The ARIC study was recruited from four U.S. communities and therefore may not be representative of the entire U.S. population. Further, all participants in the ARIC study were given the option to have their primary care doctor notified if lab results were abnormal; therefore, ARIC participants may receive a diagnosis of diabetes at an earlier point than persons in the general community as a result of being in the study. However, an analysis in ARIC study participants showed that diagnosis of diabetes was still delayed on average by 2–7 years after the study visit at which the glucose was elevated (37).
In conclusion, in this community-based longitudinal study, we found that middle-aged persons with prediabetes or diabetes had significantly excess rates of hospitalization during two decades of follow-up. Randomized clinical trials of glucose control have typically enrolled high-risk patients, have had limited follow-up, and have focused on narrowly defined microvascular and/or macrovascular outcomes. Observational cohort studies, such as ours, can provide comprehensive evidence of the long-term risks of hyperglycemia. We found an excess risk of total hospitalizations, and cardiovascular hospitalization in particular, not only among persons with diagnosed diabetes and poorly controlled diabetes but also among those with undiagnosed diabetes and prediabetes. Our results suggest that prevention of prediabetes from progression to overt diabetes and improved glycemic control among those with diagnosed diabetes may reduce the burden of hospitalizations over the life span. The high rate of hospitalization due to endocrine, infection, and iatrogenic/injury causes among those with diagnosed diabetes is concerning and suggests that increased efforts are needed to reduce the burden of preventable hospitalization among persons with diabetes.
Supplementary Material
Article Information
Acknowledgments. The authors thank the staff and participants of the ARIC study for important contributions.
Funding. The ARIC study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). A.L.C.S. was supported by National Institutes of Health/National Heart, Lung, and Blood Institute training grant T32-HL-007024.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. A.L.C.S. was responsible for study conception and design, analysis and interpretation of data, drafting the manuscript, and final approval of the submitted manuscript. R.R.K., S.G., S.C.S., L.W., H.C.Y., and J.C. were responsible for data interpretation, critically revising the manuscript, and final approval of the submitted manuscript. E.S. was responsible for conception and study design, data interpretation, critically revising the manuscript, and final approval of the submitted manuscript. A.L.C.S. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc15-1335/-/DC1.
References
- 1.Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988-1994 and 1999-2010. Ann Intern Med 2014;160:517–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee JW, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997-2008. Diabetes Care 2011;34:353–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dall TM, Yang W, Halder P, et al. . The economic burden of elevated blood glucose levels in 2012: diagnosed and undiagnosed diabetes, gestational diabetes mellitus, and prediabetes. Diabetes Care 2014;37:3172–3179 [DOI] [PubMed] [Google Scholar]
- 4.Dall TM, Zhang Y, Chen YJ, Quick WW, Yang WG, Fogli J. The economic burden of diabetes. Health Aff (Millwood) 2010;29:297–303 [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033–1046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Diabetes Association Economic costs of diabetes in the U.S. In 2007. Diabetes Care 2008;31:596–615 [DOI] [PubMed] [Google Scholar]
- 7.Smith C, Cowan C, Sensenig A, Catlin A, Health Accounts T; Health Accounts Team . Health spending growth slows in 2003. Health Aff (Millwood) 2005;24:185–194 [DOI] [PubMed] [Google Scholar]
- 8.ARIC Study Investigators The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol 1989;129:687–702 [PubMed] [Google Scholar]
- 9.Selvin E, Coresh J, Zhu H, Folsom AR, Steffes MW. Measurement of glycated hemoglobin from stored whole blood samples in the Atherosclerosis Risk in Communities study. J Diabetes 2010;2:118–124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 11.American Diabetes Association 2. Classification and Diagnosis of Diabetes. Diabetes Care 2016;39(Suppl. 1):S13–S22 [DOI] [PubMed] [Google Scholar]
- 12.American Diabetes Association Standards of medical care in diabetes--2014. Diabetes Care 2014;37(Suppl. 1):S14–S80 [DOI] [PubMed] [Google Scholar]
- 13.Huang ES, Davis AM. Glycemic Control in Older Adults With Diabetes Mellitus. JAMA 2015;314:1509–1510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pfuntner A, Wier L, Stocks C. Most frequent conditions in U.S. hospitals, 2011. In Healthcare Cost and Utilization Project (HCUP) Statistical Brief #162. Rockville, MD, Agency for Healthcare Research and Quality, 2013 [PubMed] [Google Scholar]
- 15.Foraker RE, Rose KM, Chang PP, Suchindran CM, McNeill AM, Rosamond WD. Hospital length of stay for incident heart failure: Atherosclerosis Risk in Communities (ARIC) cohort: 1987-2005. J Healthc Qual 2014;36:45–51 [DOI] [PubMed] [Google Scholar]
- 16.Foraker RE, Rose KM, Suchindran CM, Chang PP, McNeill AM, Rosamond WD. Socioeconomic status, Medicaid coverage, clinical comorbidity, and rehospitalization or death after an incident heart failure hospitalization: Atherosclerosis Risk in Communities cohort (1987 to 2004). Circ Heart Fail 2011;4:308–316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992;45:613–619 [DOI] [PubMed] [Google Scholar]
- 18.Levey AS, Stevens LA, Schmid CH, et al.; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) . A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cook CB, Naylor DB, Hentz JG, et al. . Disparities in diabetes-related hospitalizations: relationship of age, sex, and race/ethnicity with hospital discharges, lengths of stay, and direct inpatient charges. Ethn Dis 2006;16:126–131 [PubMed] [Google Scholar]
- 20.Jiang HJ, Stryer D, Friedman B, Andrews R. Multiple hospitalizations for patients with diabetes. Diabetes Care 2003;26:1421–1426 [DOI] [PubMed] [Google Scholar]
- 21.Selvin E, Steffes MW, Zhu H, et al. . Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 2010;362:800–811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sakurai M, Saitoh S, Miura K, et al.; NIPPON DATA90 Research Group . HbA1c and the risks for all-cause and cardiovascular mortality in the general Japanese population: NIPPON DATA90. Diabetes Care 2013;36:3759–3765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cook CB, Tsui C, Ziemer DC, Naylor DB, Miller WJ. Common reasons for hospitalization among adult patients with diabetes. Endocr Pract 2006;12:363–370 [DOI] [PubMed] [Google Scholar]
- 24.Cook CB, Tsui C, Ziemer DC, Naylor DB, Miller WJ, Hentz JG. Common reasons for hospitalization in urban diabetes patients. Ethn Dis 2006;16:391–397 [PubMed] [Google Scholar]
- 25.Rosenthal MJ, Fajardo M, Gilmore S, Morley JE, Naliboff BD. Hospitalization and mortality of diabetes in older adults. A 3-year prospective study. Diabetes Care 1998;21:231–235 [DOI] [PubMed] [Google Scholar]
- 26.Lombardo F, Maggini M, Gruden G, Bruno G. Temporal trend in hospitalizations for acute diabetic complications: a nationwide study, Italy, 2001-2010. PLoS One 2013;8:e63675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Menzin J, Korn JR, Cohen J, et al. . Relationship between glycemic control and diabetes-related hospital costs in patients with type 1 or type 2 diabetes mellitus. J Manag Care Pharm 2010;16:264–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clarke PM, Glasziou P, Patel A, et al.; ADVANCE Collaborative Group . Event rates, hospital utilization, and costs associated with major complications of diabetes: a multicountry comparative analysis. PLoS Med 2010;7:e1000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Berardis G, D’Ettorre A, Graziano G, et al.; DADA (Diabetes Administrative Data Analysis) Study Group . The burden of hospitalization related to diabetes mellitus: a population-based study. Nutr Metab Cardiovasc Dis 2012;22:605–612 [DOI] [PubMed] [Google Scholar]
- 30.Tomlin AM, Dovey SM, Tilyard MW. Risk factors for hospitalization due to diabetes complications. Diabetes Res Clin Pract 2008;80:244–252 [DOI] [PubMed] [Google Scholar]
- 31.Li TC, Kardia SL, Li CI, et al. . Glycemic control paradox: Poor glycemic control associated with higher one-year and eight-year risks of all-cause hospitalization but lower one-year risk of hypoglycemia in patients with type 2 diabetes. Metabolism 2015;64:1013–1021 [DOI] [PubMed] [Google Scholar]
- 32.van der Linden MW, Plat AW, Erkens JA, Emneus M, Herings RM. Large impact of antidiabetic drug treatment and hospitalizations on economic burden of diabetes mellitus in The Netherlands during 2000 to 2004. Value Health 2009;12:909–914 [DOI] [PubMed] [Google Scholar]
- 33.Schneider AL, Williams EK, Brancati FL, Blecker S, Coresh J, Selvin E. Diabetes and risk of fracture-related hospitalization: the Atherosclerosis Risk in Communities Study. Diabetes Care 2013;36:1153–1158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 2008;359:1577–1589 [DOI] [PubMed] [Google Scholar]
- 35.Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008;358:580–591 [DOI] [PubMed] [Google Scholar]
- 36.Hayward RA, Reaven PD, Wiitala WL, et al.; VADT Investigators . Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2015;372:2197–2206 [DOI] [PubMed] [Google Scholar]
- 37.Samuels TA, Cohen D, Brancati FL, Coresh J, Kao WH. Delayed diagnosis of incident type 2 diabetes mellitus in the ARIC study. Am J Manag Care 2006;12:717–724 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.