Abstract
Risk factors for cardiovascular disease (CVD) are well-established in type 2 but not type 1 diabetes (T1DM). We assessed risk factors in the long-term (mean 27 years) follow-up of the Diabetes Control and Complications Trial (DCCT) cohort with T1DM. Cox proportional hazards multivariate models assessed the association of traditional and novel risk factors, including HbA1c, with major atherosclerotic cardiovascular events (MACE) (fatal or nonfatal myocardial infarction [MI] or stroke) and any-CVD (MACE plus confirmed angina, silent MI, revascularization, or congestive heart failure). Age and mean HbA1c were strongly associated with any-CVD and with MACE. For each percentage point increase in mean HbA1c, the risk for any-CVD and for MACE increased by 31 and 42%, respectively. CVD and MACE were associated with seven other conventional factors, such as blood pressure, lipids, and lack of ACE inhibitor use, but not with sex. The areas under the receiver operating characteristics curves for the association of age and HbA1c, taken together with any-CVD and for MACE, were 0.70 and 0.77, respectively, and for the final models, including all significant risk factors, were 0.75 and 0.82. Although many conventional CVD risk factors apply in T1DM, hyperglycemia is an important risk factor second only to age.
Introduction
Type 1 diabetes (T1DM) confers a high risk for cardiovascular disease (CVD) compared with the age-matched population without diabetes (1–3) that historically has also accounted for most of the premature deaths in T1DM and is associated with the development of nephropathy (4–6). The Diabetes Control and Complications Trial (DCCT) previously demonstrated that a mean 6.5 years of intensive diabetes therapy with a mean HbA1c of ∼7% substantially reduced microvascular complications, including nephropathy, compared with conventional therapy with HbA1c of ∼9% (7). After an additional 11 years of observational follow-up in the Epidemiology of Diabetes Interventions and Complications (EDIC) study, the risk of major atherosclerotic cardiovascular events (MACE; fatal or nonfatal myocardial infarction [MI] or stroke) was reduced by 58% and aggregate CVD (MACE plus confirmed angina, silent MI, revascularization, or congestive heart failure) by 42% in the original intensive versus conventional therapy group (8).
In 2013, EDIC reached a prespecified landmark of 100 former DCCT conventionally treated subjects with an adjudicated CVD event that provides adequate power to describe risk factor effects reliably in multivariate Cox proportional hazards regression models. We now present analyses of established and putative risk factors for CVD, including glycemic control, after a mean of 27 years of follow-up of the DCCT/EDIC cohort.
Research Design and Methods
The detailed DCCT/EDIC methods have been described (9,10). In brief, DCCT (1983–1993) was a controlled clinical trial of 1,441 patients with T1DM randomized to conventional diabetes therapy or intensive therapy to assess whether reducing hyperglycemia would decrease the risk of complications of T1DM. Conventional therapy used one or two daily injections of insulin aimed at preventing symptoms of hypo- or hyperglycemia but with no glucose targets. Intensive therapy used multiple (≥3) daily injections or insulin pump therapy, guided by self-monitoring of blood glucose, and aimed to achieve glycemic control as close to the nondiabetic range as safely possible.
Subjects
At DCCT baseline, the 13- to 39-year-old study cohort included a primary prevention cohort with 1–5 years’ diabetes duration, no retinopathy based on 7-field stereoscopic fundus photography, and <40 mg/24 h of albuminuria. The secondary intervention cohort had 1–15 years’ duration, minimal to moderate nonproliferative retinopathy, and <200 mg/24 h of albuminuria (9). Exclusion criteria included neuropathy requiring therapy, hypertension (>140/90 mmHg or medication use), and hyperlipidemia (a fasting serum cholesterol level ≥3 SD above age- and sex-specific means or medication use).
Risk Factors
Risk factors were assessed by standardized methods during DCCT/EDIC (9,10). HbA1c was measured by high-performance liquid chromatography quarterly during DCCT and annually during EDIC (11). Fasting lipoprotein levels and albuminuria were measured annually during DCCT and on alternate years during EDIC. Serum creatinine was measured annually throughout. The DCCT/EDIC central biochemistry laboratory performed all laboratory measurements with standardized methods and long-term controls to guard against assay drift.
Candidate risk factors were grouped into the following 11 blocks (described in detail in Supplementary Table 1):
design (treatment group and cohort);
physical (sex, age, weight, BMI);
behavioral (smoking, alcohol intake, exercise);
family history (hypertension, MI, and T1DM or type 2 diabetes);
blood pressure/pulse (systolic and diastolic blood pressure, pulse pressure, pulse rate);
medication use (ACE inhibitors, angiotensin receptor blockade, β-adrenergic blockers, lipid-lowering agents, calcium channel blockers);
lipid levels (total cholesterol, triglycerides, LDL cholesterol [LDLc], HDL cholesterol [HDLc] levels);
diabetes specific (duration of diabetes, baseline stimulated C-peptide, daily insulin dose, estimated glucose disposal rate [12]);
nephropathy (estimated glomerular filtration rate [GFR], albumin excretion rate [AER], presence of microalbuminuria, presence of macroalbuminuria);
hypoglycemia events (episodes requiring assistance, coma, or seizure); and
glycemia (HbA1c at eligibility and mean HbA1c during DCCT/EDIC).
Some covariates were fixed (e.g., baseline), whereas others were time-dependent covariates representing the current (most recent) measurement or the updated mean of all follow-up values since randomization. For covariates measured at different frequencies during DCCT and EDIC (e.g., HbA1c), the updated time-weighted mean was computed weighting each value by the interval between measurements.
Cardiovascular Outcomes
EDIC embargoed CVD risk factor analyses until 100 conventional group subjects had experienced a CVD event. This led to data lock as of 31 December 2013 for these analyses. CVD events were ascertained based on the patient-reported updated annual CVD histories supported by medical records and annual centrally graded electrocardiograms (ECGs). Events were adjudicated and classified by a committee masked to DCCT treatment assignment and HbA1c levels (13).
The primary CVD outcome (“any-CVD”) was time to the first occurrence of cardiovascular death, nonfatal MI, nonfatal stroke, subclinical MI on ECG, angina confirmed by ischemic changes with exercise tolerance testing or by clinically significant obstruction on coronary angiography, revascularization (with angioplasty or coronary artery bypass), or congestive heart failure (paroxysmal nocturnal dyspnea, orthopnea, or marked limitation of physical activity caused by heart disease). The secondary CVD outcome, major atherosclerotic cardiovascular events (MACE), a subset of any-CVD, included only the time to cardiovascular death, nonfatal MI, or nonfatal stroke, whichever occurred first.
Statistical Analysis
Quartiles describe quantitative variables, and percentages describe discrete variables. A Cox proportional hazards model with 100 CVD cases in the conventional group or ∼150 cases in the combined cohort provided 83% power to detect a 30% risk reduction per SD change in a factor adjusted for 10 other covariates with an R2 = 0.35 with that factor and using a test at the 0.01 level (two-sided) (14).
The analysis was based on the time to the first component event for each outcome (any-CVD or MACE). The Kaplan-Meier method estimated the probability of remaining free of CVD or MACE over time (i.e., the “survival” function). Semiparametric Cox proportional hazards models assessed the influence of fixed and time-dependent covariates on the risk of CVD/MACE (15). Smoothing splines assessed the shape of the empirical log(hazard) functions of any-CVD and MACE over the range of age and time-weighted mean HbA1c (16).
Given the large number of risk factors, variables were entered into the Cox proportional hazards model one block at a time in the order displayed in Supplementary Table 1, starting with design factors, then demographic-physical, etc. Details of the variable selection/deletion process are described in the Supplementary Data. Briefly, after each block was added, a variable was deleted if it was not nominally significant, yielded a poor Akaike information criterion (17), and had a penalized likelihood estimate of zero (18). After the last block was entered, the final model was fit using the selected covariates. Two additional sensitivity analyses started with the complete set of variables, followed by subset selection based on the Akaike information criterion or the penalized likelihood. Interaction terms investigated sex differences in the effect of covariates on the risk of CVD.
There is no standard measure of the proportion of variation explained by a factor in the Cox proportional hazards model. However, the measure of R2 in other models is directly proportional to the test statistic value or inversely proportional to the P value. Accordingly, the Z-test value is used to measure the relative strength of the predictive association with CVD risk.
The area under the receiver operating characteristics curve (AUC = sensitivity vs. 1 – specificity) describes the predictive accuracy of a model, with an AUC = 0.5 meaning chance predictions and an AUC = 1 providing 100% accurate predictions. To allow for time-dependent covariates, a separate model was fit for each year of follow-up and the simple average of the separate AUC estimates was obtained. The AUC value can be interpreted as the probability that a subject who experienced an event has a higher risk score than a subject who is event free.
Results
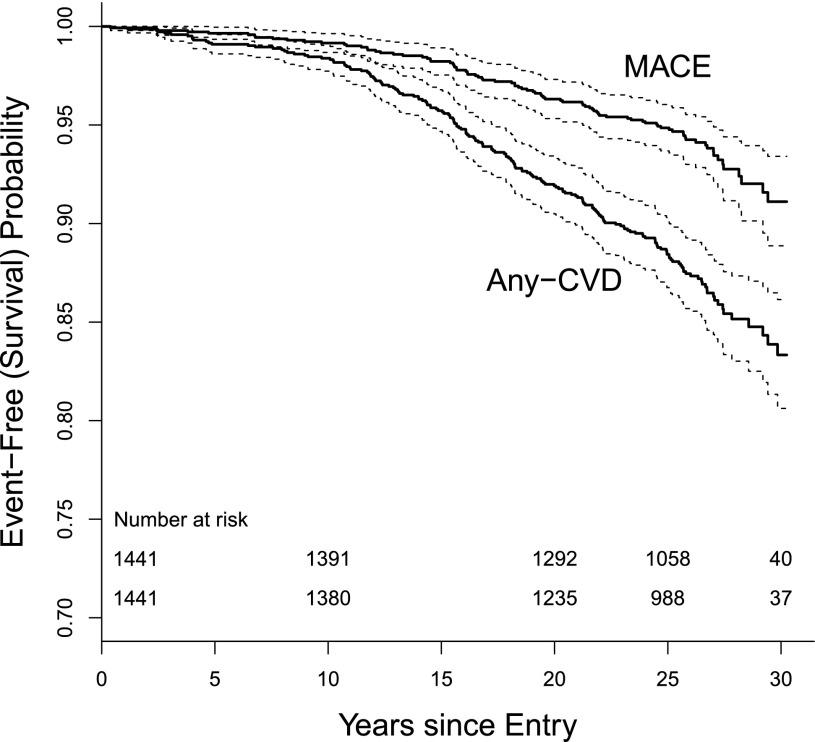
As of 31 December 2013, 85.8% of the original cohort (93.2% of the 1,327 surviving participants) were under active follow-up, with a median follow-up of 27 years. A total of 184 subjects had a CVD event (any-CVD cases) and 88 had MACE, with 82 CVD and 39 MACE cases in the intensive group and 102 CVD and 49 MACE cases in the conventional group. After 27 years of follow-up, ∼85% of the cohort remained free of any-CVD and more than 90% were free of MACE (Fig. 1).
Figure 1.
Kaplan-Meier survival (event-free) curves (solid lines), and 95% CIs (dashed lines) for MACE (top line) and any-CVD (bottom line), with number of subjects at risk for each at 10, 20, and 30 years of follow-up. The number at risk beyond 23 years declines as a function of staggered entry into the study from 1983 to 1989.
Baseline Characteristics
Table 1 reports the baseline characteristics of the DCCT cohort as a whole and among those who did versus did not have any-CVD event as well as the corresponding hazard ratio (HR) without adjustment for other factors. Supplementary Table 2 shows the baseline characteristics for subjects with and without a MACE event. At baseline, 53% of the participants were men, the median age was 27 years, duration of diabetes was 49 months, HbA1c was 8.8% (73 mmol/mol), and 19% were smokers. Nominally significant baseline factors associated with a higher risk of any-CVD included the secondary versus primary cohort, older age, greater weight and BMI in women but not in men, smoking, longer duration of diabetes, family history of MI and type 2 diabetes, higher blood pressure and pulse, and higher total cholesterol, triglyceride, LDLc, and HbA1c levels. These risk factors were also associated with MACE, albeit with lower degrees of significance, presumably owing to fewer events (Supplementary Table 2). Of note, the rate of any-CVD and MACE were not statistically different between men and women (P = 0.98 and P = 0.23 for any-CVD and MACE, respectively) (Table 1 and Supplementary Table 2).
Table 1.
Baseline characteristics of DCCT/EDIC participants according to the presence or absence of any-CVD over the course of DCCT/EDIC
| Any-CVD |
||||||
|---|---|---|---|---|---|---|
| Overall | No | Yes | ||||
| N = 1,441 | n = 1,257 | n = 184 | HR | 95% CI | P value | |
| Design | ||||||
| Treatment group (% conventional) | 51 | 50 | 55 | 1.29 | 0.964, 1.725 | 0.0864 |
| Cohort (% secondary) | 50 | 48 | 62 | 1.592 | 1.18, 2.147 | 0.0023 |
| Demographic | ||||||
| Physical | ||||||
| Sex (% men) | 53 | 53 | 52 | 1.004 | 0.752, 1.341 | 0.9786 |
| Age (years) | 27 (22,32) | 27 (21,32) | 31 (27,35) | 1.091 | 1.066, 1.116 | <0.0001 |
| Adult vs. adolescent (<18 years) | 86 | 85 | 95 | 3.378 | 1.727, 6.611 | 0.0004 |
| Weight men (kg) | 74 (67,82) | 74 (67,82) | 76 (70,84) | 1.011 | 0.993, 1.029 | 0.2422 |
| Weight women (kg) | 62 (56,69) | 61 (55,68) | 65 (57,70) | 1.034 | 1.011, 1.057 | 0.0032 |
| BMI men (kg/m2) | 24 (22,25) | 23 (22,25) | 24 (22,26) | 1.065 | 0.993, 1.142 | 0.0764 |
| BMI women (kg/m2) | 23 (21,25) | 23 (21,25) | 24 (22,26) | 1.096 | 1.022, 1.175 | 0.0098 |
| Behavioral | ||||||
| Smoking (%) | 19 | 17 | 27 | 1.834 | 1.325, 2.538 | 0.0003 |
| Alcohol (% occasional or regular) | 22 | 22 | 20 | 0.888 | 0.617, 1.279 | 0.5246 |
| Exercise (% moderate or strenuous) | 70 | 70 | 71 | 1.067 | 0.775, 1.468 | 0.6901 |
| Family history (%) | ||||||
| Hypertension | 56 | 56 | 59 | 1.123 | 0.838, 1.506 | 0.4377 |
| MI | 49 | 47 | 60 | 1.615 | 1.202, 2.169 | 0.0015 |
| T1DM | 14 | 14 | 17 | 1.294 | 0.884, 1.894 | 0.1856 |
| T2DM | 9 | 9 | 13 | 1.592 | 1.037, 2.446 | 0.0336 |
| Traditional | ||||||
| Blood pressure | ||||||
| Systolic (mmHg) | 114 (106,122) | 114 (106,120) | 116 (110,124) | 1.016 | 1.004, 1.029 | 0.0117 |
| Diastolic (mmHg) | 72 (68,80) | 72 (68,80) | 74 (68,80) | 1.021 | 1.004, 1.038 | 0.0131 |
| Pulse pressure (mmHg) | 40 (34,48) | 40 (34,48) | 42 (34,48) | 1.006 | 0.991, 1.02 | 0.4554 |
| Pulse rate (bpm) | 76 (68,84) | 76 (68,82) | 78 (72,88) | 1.019 | 1.006, 1.031 | 0.0029 |
| Lipids (mg/dL) | ||||||
| Total cholesterol | 174 (153,197) | 172 (152,195) | 185 (162,211) | 1.012 | 1.008, 1.016 | <0.0001 |
| Triglycerides | 73 (55,94) | 72 (55,93) | 80 (59,97) | 1.614 | 1.184, 2.199 | 0.0024 |
| HDLc | 49 (42,57) | 50 (42,58) | 47 (41,55) | 0.992 | 0.98, 1.004 | 0.2001 |
| LDLc | 107 (91,127) | 105 (89,125) | 119 (98,144) | 1.014 | 1.01, 1.019 | <0.0001 |
| Diabetes-related | ||||||
| History | ||||||
| Diabetes duration (months) | 49 (26,108) | 47 (26,104) | 69 (29,130) | 1.004 | 1.001, 1.007 | 0.0032 |
| C-peptide (nmol/L)* | ||||||
| Diabetes duration <5 years | 0.13 (0.04,0.25) | 0.12 (0.04,0.24) | 0.13 (0.03,0.29) | 1.5571 | 0.325, 7.458 | 0.5796 |
| Diabetes duration ≥5 years | 0.03 (0.03,0.04) | 0.03 (0.03,0.04) | 0.03 (0.03,0.03) | 0.079 | 0, 33.708 | 0.4115 |
| Nephropathy | ||||||
| AER (mg/24 h) | 24 (20,29) | 23 (20,28) | 24 (20,30) | 1.17 | 0.978, 1.401 | 0.0861 |
| Glycemia | ||||||
| HbA1c (%) | 8.8 (7.8,10.1) | 8.8 (7.8,10.1) | 9.0 (8.1,10.3) | |||
| HbA1c (mmol/mol) | 73 (62,87) | 73 (62,87) | 75 (65,89) | 1.093 | 1.003, 1.19 | 0.0426 |
Data are presented as median (first quartile,third quartile) or prevalence (%) and as the corresponding HR for any-CVD per unit change in the baseline covariate. An identical table for MACE is presented in the Supplementary Data. T2DM, type 2 diabetes mellitus.
*C-peptide is presented separately within diabetes duration strata because the eligibility range differed among those with ≤5 years’ duration (0–0.5 nmol/L) and those with >5 years’ duration (0–0.2 nmol/L).
Time-Dependent Characteristics
Table 2 presents the HRs for any-CVD and MACE based on the current value or the updated mean value of each time-dependent covariate, without adjustment for other factors. Supplementary Table 3 presents the values of each covariate among those still at risk for any-CVD at 10, 20, and 25 years. During the study, weight and BMI increased among men and women, smoking decreased, alcohol consumption increased, and exercise declined, and there were age-related increases in blood pressure and lipids and in the use of respective medications and increases in the prevalence of nephropathy (Supplementary Table 3). All of these, except for weight, alcohol consumption, and exercise, were significantly associated with the risk of any-CVD, much more so than the baseline value. Similar associations were observed for MACE (Supplementary Table 4).
Table 2.
HR for any-CVD and for MACE per unit change in each time-dependent covariate with no other adjustments, and an indication of the type of covariate used in the analysis
| Any-CVD |
MACE |
||||||
|---|---|---|---|---|---|---|---|
| Type* | HR | 95% CI | P value | HR | 95% CI | P value | |
| Demographic | |||||||
| Physical | |||||||
| Age (years) | C | 1.091 | 1.066, 1.116 | <0.0001 | 1.112 | 1.074, 1.151 | <0.0001 |
| Weight men (kg) | C | 1 | 0.987, 1.014 | 0.954 | 0.984 | 0.964, 1.004 | 0.1092 |
| Weight women (kg) | C | 1.009 | 0.995, 1.022 | 0.1956 | 1.008 | 0.988, 1.028 | 0.4519 |
| Mean BMI (kg/m2) | M | 1.04 | 1, 1.081 | 0.0486 | 1.009 | 0.952, 1.069 | 0.758 |
| BMI men (kg/m2) | C | 1.01 | 0.967, 1.055 | 0.6557 | 0.966 | 0.903, 1.034 | 0.3216 |
| BMI women (kg/m2) | C | 1.024 | 0.985, 1.064 | 0.2303 | 1.019 | 0.962, 1.08 | 0.5147 |
| Behavioral | |||||||
| Smoking (yes vs. no) | C | 1.529 | 1.076, 2.173 | 0.0179 | 2.247 | 1.411, 3.579 | 0.0007 |
| Alcohol (% occasional or regular vs. nondrinker) | C | 0.86 | 0.727, 1.018 | 0.0797 | 0.783 | 0.608, 1.007 | 0.0568 |
| Exercise (% moderate or strenuous vs. sedentary) | C | 0.914 | 0.707, 1.181 | 0.4898 | 0.979 | 0.676, 1.416 | 0.909 |
| Traditional | |||||||
| Blood pressure | C | ||||||
| Systolic (mmHg) | C | 1.027 | 1.018, 1.037 | <0.0001 | 1.034 | 1.022, 1.046 | <0.0001 |
| Mean systolic (mmHg) | M | 1.061 | 1.043, 1.078 | <0.0001 | 1.071 | 1.046, 1.096 | <0.0001 |
| Diastolic (mmHg) | C | 1.009 | 0.993, 1.025 | 0.2721 | 1.01 | 0.987, 1.034 | 0.3842 |
| Mean diastolic (mmHg) | M | 1.055 | 1.028, 1.083 | 0.0001 | 1.044 | 1.005, 1.085 | 0.027 |
| Pulse pressure (mmHg) | C | 1.036 | 1.025, 1.047 | <0.0001 | 1.045 | 1.03, 1.059 | <0.0001 |
| Hypertension (yes vs. no) | C | 2.01 | 1.448, 2.79 | <0.0001 | 2.198 | 1.348, 3.586 | 0.0016 |
| Any hypertension (yes vs. no) | A | 2.308 | 1.583, 3.365 | <0.0001 | 2.291 | 1.303, 4.027 | 0.004 |
| Pulse rate (bpm) | C | 1.021 | 1.008, 1.034 | 0.0012 | 1.029 | 1.011, 1.048 | 0.0016 |
| Mean pulse rate (bpm) | M | 1.057 | 1.036, 1.078 | <0.0001 | 1.074 | 1.044, 1.106 | <0.0001 |
| Medications | |||||||
| ACE inhibitor (yes vs. no) | C | 1.092 | 0.782, 1.523 | 0.6062 | 0.945 | 0.583, 1.533 | 0.8191 |
| ARB (yes vs. no) | C | 1.421 | 0.878, 2.3 | 0.1523 | 1.024 | 0.486, 2.158 | 0.9495 |
| β-Blockers (yes vs. no) | C | 1.827 | 1.002, 3.333 | 0.0493 | 2.796 | 1.441, 5.424 | 0.0024 |
| Calcium channel blockers (yes vs. no) | C | 2.84 | 1.801, 4.478 | <0.0001 | 2.385 | 1.216, 4.68 | 0.0115 |
| Lipid lowering (yes vs. no) | C | 1.401 | 0.991, 1.98 | 0.056 | 1.141 | 0.696, 1.872 | 0.6006 |
| Lipids (mg/dL) | |||||||
| Total cholesterol | C | 1.01 | 1.007, 1.014 | <0.0001 | 1.011 | 1.007, 1.016 | <0.0001 |
| Mean total cholesterol | M | 1.018 | 1.013, 1.023 | <0.0001 | 1.018 | 1.011, 1.025 | <0.0001 |
| Triglycerides (log) | C | 2.133 | 1.674, 2.719 | <0.0001 | 2.522 | 1.807, 3.518 | <0.0001 |
| Mean triglycerides (log) | M | 2.458 | 1.786, 3.382 | <0.0001 | 2.923 | 1.87, 4.568 | <0.0001 |
| HDLc | C | 0.995 | 0.986, 1.005 | 0.3191 | 0.984 | 0.97, 0.999 | 0.0323 |
| Mean HDLc | M | 0.989 | 0.977, 1.001 | 0.0847 | 0.983 | 0.965, 1.002 | 0.0754 |
| LDLc | C | 1.011 | 1.006, 1.015 | <0.0001 | 1.014 | 1.008, 1.019 | <0.0001 |
| Mean LDLc | M | 1.019 | 1.014, 1.025 | <0.0001 | 1.02 | 1.012, 1.029 | <0.0001 |
| Hyperlipidemia (yes vs. no) | C | 1.767 | 1.3, 2.401 | 0.0003 | 1.647 | 1.055, 2.571 | 0.0282 |
| Diabetes-related | |||||||
| History | |||||||
| Insulin dose (units/kg/day) | C | 1.595 | 1.095, 2.325 | 0.0151 | 1.363 | 0.694, 2.678 | 0.3691 |
| Mean insulin dose (units/kg/day) | M | 1.674 | 0.797, 3.516 | 0.174 | 1.296 | 0.433, 3.874 | 0.6431 |
| Estimated glucose disposal rate | C | 0.819 | 0.761, 0.882 | <0.0001 | 0.763 | 0.683, 0.853 | <0.0001 |
| Nephropathy | |||||||
| Estimated GFR (mL/min per 1.73 m2) | C | 0.985 | 0.978, 0.991 | <0.0001 | 0.978 | 0.971, 0.986 | <0.0001 |
| Estimated GFR <60 (yes vs. no) | C | 2.479 | 1.332, 4.613 | 0.0042 | 4.356 | 2.21, 8.586 | <0.0001 |
| Any estimated GFR <60 (yes vs. no) | A | 2.529 | 1.472, 4.346 | 0.0008 | 3.949 | 2.099, 7.429 | <0.0001 |
| AER (mg/24 h) (log) | C | 1.229 | 1.133, 1.334 | <0.0001 | 1.283 | 1.151, 1.431 | <0.0001 |
| Sustained AER ≥30 mg/dL (yes vs. no) | C | 1.8 | 1.278, 2.535 | 0.0008 | 1.916 | 1.18, 3.109 | 0.0085 |
| AER ≥40 mg/dL (yes vs. no) | C | 1.891 | 1.346, 2.656 | 0.0002 | 2.171 | 1.355, 3.478 | 0.0013 |
| AER ≥300 mg/dL (yes vs. no) | C | 2.312 | 1.434, 3.728 | 0.0006 | 3.028 | 1.64, 5.593 | 0.0004 |
| Any AER ≥40 mg/dL (yes vs. no) | A | 1.768 | 1.316, 2.374 | 0.0002 | 1.729 | 1.127, 2.654 | 0.0122 |
| Any AER ≥300 mg/dL (yes vs. no) | A | 1.958 | 1.287, 2.978 | 0.0017 | 3.072 | 1.834, 5.148 | <0.0001 |
| Hypoglycemia | |||||||
| Coma/seizure (yes vs. no) | C | 0.972 | 0.812, 1.163 | 0.7542 | 1.021 | 0.835, 1.248 | 0.8379 |
| Requiring assistance (yes vs. no) | C | 1.002 | 0.93, 1.079 | 0.9626 | 1.005 | 0.905, 1.114 | 0.9319 |
| Glycemia | |||||||
| HbA1c (%) | C | 1.241 | 1.129, 1.364 | <0.0001 | 1.297 | 1.139, 1.478 | 0.0001 |
| Mean HbA1c (%) | M | 1.382 | 1.231, 1.551 | <0.0001 | 1.539 | 1.309, 1.808 | <0.0001 |
ARB, angiotensin receptor blockers.
*Categories C (current or most recent), M (updated mean value), and A (cumulative incidence, such as any use) correspond to time-dependent covariates assessed or measured at or most recently before each event time or right censoring time (i.e., at the most recent visit up to the particular time).
Individual Covariate Effects
Age and time-weighted mean HbA1c levels were the most significant univariate risk factors for any-CVD, with respective Z-test values of 8.1 and 6.6 (P < 1.0E-10), each adjusted for the other and also for MACE. Supplementary Fig. 1 shows that the spline-smoothed model-free estimates of the log(hazard) function for any-CVD and for MACE were both strongly linear functions of age and the time-weighted mean HbA1c.
Table 3 presents the covariates that remained significantly associated with any-CVD and MACE, after adjustment for age and time-weighted mean HbA1c. A higher risk of any-CVD was predicted by family history of MI; higher blood pressure and pulse variables; use of calcium channel blockers (but not the other “cardioprotective” medications); higher cholesterol, triglycerides, and LDLc; lower HDLc (which became significant after adjustment); diabetes-related history variables (including higher mean insulin dose); higher AER; and history of micro- and macroalbuminuria but not estimated GFR. Use of ACE inhibitors was not significant alone or when adjusted for age and time-weighted HbA1c but became significant when also adjusted for blood pressure levels.
Table 3.
HRs per unit change in each baseline or time-dependent covariate in separate Cox models for any-CVD and for MACE, minimally adjusted for age and updated mean HbA1c
| Any-CVD |
MACE |
||||
|---|---|---|---|---|---|
| Type* | HR (95% CI) | P value | HR (95% CI) | P value | |
| Design | |||||
| Secondary cohort (yes vs. no) | B | 1.57 (1.17, 2.13) | 0.003 | ||
| Demographic | |||||
| Behavioral | |||||
| Smoking status (yes vs. no) | C | 1.89 (1.18, 3.04) | 0.009 | ||
| Family history | |||||
| MI (yes vs. no) | B | 1.53 (1.14, 2.06) | 0.005 | ||
| Traditional | |||||
| Blood pressure | |||||
| Systolic (mmHg) | C | 1.02 (1.01, 1.03) | <0.001 | 1.02 (1.01, 1.03) | <0.001 |
| Mean systolic (mmHg) | M | 1.04 (1.02, 1.06) | <0.001 | 1.04 (1.02, 1.07) | <0.0014 |
| Mean diastolic (mmHg) | M | 1.04 (1.01, 1.07) | 0.004 | ||
| Pulse pressure (mmHg) | C | 1.02 (1.01, 1.03) | <0.001 | 1.03 (1.01, 1.04) | 0.001 |
| Mean pulse rate (bpm) | M | 1.05 (1.03, 1.07) | <0.001 | 1.07 (1.03, 1.10) | <0.001 |
| Medications | |||||
| Calcium channel blockers (yes vs. no) | C | 2.02 (1.28, 3.20) | 0.003 | ||
| Lipids (mg/dL) | |||||
| Total cholesterol | C | 1.008 (1.004, 1.012) | <0.001 | 1.009 (1.004, 1.0139) | <0.001 |
| Triglycerides (log) | C | 1.98 (1.53, 2.56) | <0.001 | 2.37 (1.65, 3.40) | <0.001 |
| LDLc | C | 1.008 (1.004, 1.013) | <0.001 | 1.011 (1.005, 1.017) | <0.001 |
| HDLc | C | 0.98 (0.966, 0.995) | 0.007 | ||
| Mean total cholesterol | M | 1.012 (1.006, 1.017) | <0.001 | 1.010 (1.002, 1.018) | 0.013 |
| Mean triglycerides (log) | M | 2.23 (1.60, 3.12) | <0.001 | 2.56 (1.60, 4.11) | <0.001 |
| Mean LDLc | M | 1.013 (1.007, 1.020) | <0.001 | 1.013 (1.004, 1.022) | 0.007 |
| Mean HDLc | M | 0.984 (0.971, 0.996) | 0.010 | 0.976 (0.958, 0.994) | 0.010 |
| Diabetes related | |||||
| History | |||||
| Duration (months) | B | 1.005 (1.002, 1.008) | <0.001 | 1.006 (1.002, 1.01) | 0.006 |
| Mean insulin dose (units/kg/day) | M | 3.72 (1.70, 8.14) | 0.001 | ||
| Nephropathy | |||||
| AER (mg/24 h) (log) | C | 1.17 (1.06, 1.28) | 0.001 | 1.21 (1.06, 1.37) | 0.004 |
| Any AER ≥40 (yes vs. no) | A | 1.66 (1.21, 2.26) | 0.002 | ||
| Any AER ≥300 (yes vs. no) | A | 2.41 (1.39, 4.18) | 0.002 | ||
Only covariates that were nominally significant at P ≤ 0.01 are shown for each model.
*Categories C (current or most recent), M (updated mean value), and A (cumulative incidence, such as any use) correspond to time-dependent covariates assessed or measured at or most recently prior to each event time or right censoring time (i.e., at the most recent visit up to the particular time), with B indicating baseline value.
Similarly, a higher risk of MACE was predicted by the same set of factors, with the exceptions that higher insulin dose and microalbuminuria were not significant, but macroalbuminuria (AER ≥300 mg/24 h) was significant.
Final Multivariate Models
Table 4 reports the final multivariate Cox models for any-CVD and for MACE, with the covariates listed in the order of the unsigned covariate Z values (or P values). Because any Z ≥ 3.28 has P < 0.001 and Z values as high as 7 are observed, the Z value better represents the significance of the covariate effect in the model than does the designation “P < 0.001.” In the model for any-CVD (Table 4), older age (HR 1.54 per 5 years; 95% CI 1.36, 1.73; Z = 7.07, P < 0.001) was the most significant risk factor. A higher time-weighted mean HbA1c was the next most significant factor (HR 1.31 per 1%; 95% CI 1.15, 1.50; Z = 4.0, P < 0.001). Other nominally significant variables were higher mean systolic blood pressure (Z = 3.1, P = 0.002), higher current log(triglycerides) (Z = 3.0, P = 0.003), higher mean pulse rate (Z = 2.8, P = 0.005), longer duration of diabetes (Z = 2.5, P = 0.02), use of ACE inhibitor (Z = −2.3, P = 0.03; ACE inhibitor use being protective), family history of MI (Z = 2.15, P = 0.04), and higher updated mean LDLc (Z = 2.07, P = 0.04). Thus, age is by far the most significant factor, followed by HbA1c, that is more significant than any other factor in the model, even after adjusting for age and the other factors.
Table 4.
The final multivariable Cox models for any-CVD and for MACE as a function of fixed (baseline) and time-dependent covariates, the latter either the current value or mean from baseline as stated
| HR (95% CI)* | Z-test value | P value | |
|---|---|---|---|
| Any-CVD model | |||
| covariate | |||
| Baseline age (per 5 years) | 1.5366 (1.3641, 1.731) | 7.0711 | <0.001 |
| Mean HbA1c (per 1%) | 1.3115 (1.1488, 1.4972) | 4.0133 | <0.001 |
| Mean systolic blood pressure (per 10 mmHg) | 1.3186 (1.1096, 1.567) | 3.1419 | 0.002 |
| Current triglycerides (log) | 1.5536 (1.1688, 2.065) | 3.0346 | 0.003 |
| Mean pulse rate (per 10 bpm) | 1.3855 (1.1051, 1.737) | 2.8267 | 0.005 |
| Baseline duration of diabetes (per 5 years) | 1.247 (1.0514, 1.4789) | 2.5364 | 0.02 |
| Current use of ACE inhibitor (yes vs. no) | 0.6732 (0.4777, 0.9486) | −2.2611 | 0.03 |
| Baseline family history of MI (yes vs. no) | 1.3866 (1.0294, 1.8678) | 2.1507 | 0.04 |
| Mean LDLc (per 10 mg/dL) | 1.0721 (1.0037, 1.1451) | 2.0697 | 0.04 |
| MACE model | |||
| covariate | |||
| Baseline age (per 5 years) | 1.7748 (1.4872, 2.1179) | 6.3613 | <0.001 |
| Mean HbA1c (per 1%) | 1.4186 (1.1785, 1.7077) | 3.6965 | <0.001 |
| Mean pulse rate (per 10 bpm) | 1.5975 (1.1576, 2.2046) | 2.8509 | 0.005 |
| Current triglycerides (log) | 1.7844 (1.1909, 2.6737) | 2.8071 | 0.005 |
| Mean systolic blood pressure (per 10 mmHg) | 1.3863 (1.0929, 1.7583) | 2.6931 | 0.007 |
| Current smoking (yes vs. no) | 1.8686 (1.1647, 2.9978) | 2.5924 | 0.01 |
| Baseline duration of diabetes (per 5 years) | 1.3334 (1.0399, 1.7098) | 2.2685 | 0.03 |
| Current use of ACE inhibitor (yes vs. no) | 0.5819 (0.3553, 0.9529) | −2.1515 | 0.04 |
| Current LDLc (per 10 mg/dL) | 1.0692 (1.0035, 1.1392) | 2.0685 | 0.04 |
Covariates are listed in the order of significance as indicated by the unsigned Z-value.
*The HRs in the Cox proportional hazards model can be converted from HR per x-units (e.g., per 5 years of age above) to HR per y-units (e.g., per 1 year) using the equation: HR(y/x). For example, the HR for MACE per 1 year of age is (1.7748)1/5 = 1.1216. The same equation applies to the confidence limits. The Z test and P values are unchanged by a change of scale of the HRs.
The final time-dependent Cox model was fit separately in men and women (Supplementary Tables 5 and 6). Nonsignificant interaction terms between sex and each of the variables in the multivariable model indicated that the coefficients for men and women were not significantly different.
The multivariable Cox model for MACE (Table 4) was very similar to that for any-CVD even though there were fewer cases of MACE. Again, age was by far the most significant factor, followed by time-weighted mean HbA1c and then other factors. The only differences between the sets of variables in the MACE versus any-CVD models were that smoking replaced family history of MI, whereas the current LDLc value replaced the updated mean LDLc. For each factor that appears in both models in the same manner, the coefficient was somewhat higher in the MACE versus the any-CVD model, but the CI was wider owing to fewer MACE events.
These models for any-CVD and MACE were obtained from a joint forward addition and backward elimination of successive blocks of covariates (see research design and methods). Two sensitivity analyses were also conducted using different methods of model selection (see research design and methods). Both analyses selected the same sets of covariates for any-CVD and MACE and are presented in Table 4.
The AUC measure of predictive ability for each outcome (any-CVD and MACE) was assessed for a Cox model with age as the only covariate, another with age and time-weighted mean HbA1c, and another using the full model. The respective AUC values were 0.67, 0.70, and 0.75 for any-CVD and 0.71, 0.77, and 0.82 for MACE.
Discussion
These results establish mean HbA1c over time as a strong risk factor for clinical CVD (events) in T1DM, even when adjusted for age and other traditional risk factors. The causal effect of hyperglycemia on risk of CVD in T1DM was first suggested a decade ago when DCCT/EDIC established the salutary effects of intensive therapy on CVD (8). Although an association of HbA1c levels with CVD outcomes was demonstrated, the limited number of CVD events at that time precluded a thorough investigation of risk factors as included in this report. The long-term, standardized measurement of numerous established and putative risk factors for CVD during DCCT/EDIC provided the opportunity to examine not only cross-sectional, including baseline, risk factors but also the effects of longitudinal exposure to changing (time-dependent) values of risk factors over time. Our extensive collection of risk factors over many years in patients who began the study when they were relatively young and without CVD also enables an understanding of the temporal relationship between risk factors and outcomes. This minimizes the potential for reverse causality between CVD and a risk factor.
After adjusting for the two most statistically significant risk factors, age and mean HbA1c, essentially the same set of covariates, including higher mean systolic blood pressure, mean pulse rate, current log(triglycerides), current or mean LDLc, and diabetes duration were significantly associated with the risk of any-CVD or MACE (Table 4). Current use of an ACE inhibitor was protective in both models. The only difference in risk factors between the two models was that a family history of MI appeared in the any-CVD model, whereas smoking appeared in the MACE model.
There are a number of possible explanations for our ability to demonstrate a strong relationship between glycemia and CVD when older observational cohort studies in T1DM were unable to do so (1,5). The more frequent and consistent measurement of glycemia over time with standardized methods in DCCT/EDIC provided an accurate assessment of long-term glycemia. In addition, the younger age and exclusion from entry into DCCT of participants at high cardiovascular risk and the relatively infrequent history of smoking in our cohort may have limited the influence of traditional risk factors and allowed the effects of glycemia to be manifest. Finally, the relatively lower average HbA1c levels achieved may have also contributed because recent data from the Swedish National Diabetes Register showed a stronger association with CVD events over a lower HbA1c range (19).
As for the other risk factors identified, systolic blood pressure or hypertension has consistently been reported as a major risk factor for CVD. The importance of the blood pressure finding is magnified by a recent temporal analysis that showed hypertension remains the major unaddressed risk factor for major diabetes complications (20).
The strong association of triglycerides with CVD is consistent with prior studies showing that triglyceride concentration is a particularly strong CVD predictor in diabetes (21). Further, this association was observed at very low mean values of triglycerides, even in those with subsequent CVD, supporting a recent call for resetting “normal” values in T1DM (22). These findings suggest that a trial to examine the effects of triglyceride lowering in T1DM should be performed and that the current lack of American Diabetes Association guidelines for treatment of triglycerides (23) should be reconsidered.
Likewise, the strong reduction in risk with ACE inhibition observed in this study, when adjusted for blood pressure, suggests that a trial of the effects of ACE inhibition in a comparable T1DM population may be warranted. The strong effect of increased pulse rate is also noteworthy. This may reflect autonomic neuropathy that has been shown to predict coronary heart disease (24).
The factors that do not emerge as predictors are also of interest. The similar rates of CVD in men and women with T1DM have been seen in other studies (1,2,5,25) and with even higher rates in women than men with type 2 diabetes (26,27). This finding contrasts with the higher risk of CVD among men than women in the general population (28). As we have observed in DCCT/EDIC, loss of the female protection in diabetes may be related to less aggressive care in women than in men resulting in lower achievement of recommended risk factor levels (29,30). Diabetes has also been hypothesized to have a relatively larger deleterious effect on risk factor levels in women than in men, including lipids, blood pressure, markers of coagulation, and fibrinolysis (31,32). One recent study in T1DM also demonstrated that HDLc lost its protective effect above 50 mg/dL in women but not in men (33).
Another risk factor established for CVD in type 2 diabetes (34) that did not emerge in our study was obesity or BMI. BMI has not been a strong risk factor for CVD (1,5) or mortality in other studies in T1DM (35,36). Weight gain was greater in the intensively treated participants during DCCT (37), and its potential adverse effect on CVD risk might have been mitigated by the other benefits of intensive therapy, including lower mean HbA1c. The absence of a deleterious effect of increased BMI is confirmed by a previous report that showed weight gain in the presence of improved glycemic control was not disadvantageous (38).
A major factor that did not emerge as a risk factor for CVD in the final model was renal disease, measured as albuminuria (AER 30–300 mg/24 h or ≥300 mg/24 h), which for many years has been thought to be a major contributor to CVD (39). More recent studies have also supported a relatively greater role for albuminuria than for reduced GFR in CVD (40). Several factors may explain our inability to demonstrate an association between albuminuria and CVD. First, because HbA1c levels are strongly associated with the development of albuminuria in our study (41), adjusting for HbA1c may have reduced the putative adverse effects of albuminuria. Second, the putative adverse effects of albuminuria may be confounded by the common use of ACE inhibitors, which reduce the risk of CVD in the setting of albuminuria. Finally, the null association in the final model may be a function of inadequate power (with a limited number of cases of macroalbuminuria, for example) or overadjustment because blood pressure may be in the causal pathway between AER and CVD.
Measurement error may have also contributed to the failure to observe a significant association with some factors (e.g., behavioral risk factors or those based on self-report such as smoking, exercise, and alcohol use). Measurement errors would bias the estimates of associations toward the null, thus reducing power to detect associations. Conversely, a risk factor measured with high precision, such as HbA1c, will provide much greater power to detect a given association. Further, when a precisely measured covariate and one measured with error represent the same causal pathway to the outcome, that factor measured precisely will show a more significant effect. Accordingly, a study similar to ours, but with highly precise measures of other exposures, such as exercise, might provide substantially different results than those presented here. However, the results presented here would be expected to apply to other populations with a similar precision of measurement of such factors, as is typically the case in observational follow-up.
The obvious strengths of these analyses include the careful and standardized assessments of established and putative risk factors and cardiovascular outcomes prospectively over decades. In addition, follow-up has been complete, with 93% of the surviving cohort continuing to be monitored over an average of more than 27 years. Limitations include the exclusion of patients with hypertension and dyslipidemia and some patients with albuminuria at baseline. However, owing to a baseline mean age of 27 years and diabetes duration of only 6 years, it is unlikely that more than a small number of patients at higher risk may have been excluded because of these established and putative CVD risk factors.
Regarding the modeling, data-dependent model selection has been shown to be susceptible to various types of biases, including bias in the set of covariates selected for inclusion, the coefficient estimates, and the levels of significance. However, we are confident that the resulting models are reliable. The covariates selected for any-CVD and for MACE were highly internally consistent, each model including the same five most significant covariates of age, HbA1c, systolic blood pressure, triglycerides, and pulse rate, all at P < 0.01. Further, although the initial model building was based on a stepwise process adding one block at a time, exactly the same final models were obtained in two sensitivity analyses: a penalized likelihood approach was used in one and the other was based on selection of an optimal subset of covariates using the Akaike information criterion.
Although these models could be used as the basis for a “risk” or prediction score, we hesitate to do so owing to the relatively small numbers of subjects with an outcome event (184 any-CVD, 88 MACE) compared, for example, with the 1,174 CVD cases used to develop, validate, and calibrate the Framingham Risk Score (42). However, it is encouraging that the AUC, a measure of predictive ability, was 0.75 for the any-CVD model and was 0.82 for MACE.
HbA1c is clearly a robust and important risk factor in the DCCT/EDIC cohort over the substantial but still limited period of study. However, the cohort is still young (mean age of 55 as of 2013), the proportion of survivors (1,327 or 92%) is still quite high (43), and the cumulative incidence of any-CVD is still only ∼17% (Fig. 1). Thus, the effect of hyperglycemia or other risk factors may indeed be substantially different in future decades in which the overall incidence of CVD will increase.
In conclusion, in the DCCT/EDIC cohort with T1DM, increasing age is the most significant risk factor for clinical CVD, as in the general population, followed by the updated weighted-mean HbA1c. Other traditional risk factors also appear to be important as risk factors for CVD and for MACE, particularly blood pressure and triglycerides. Thus, in T1DM, control of glycemia as well as other CVD risk factors should be aggressively pursued to reduce major cardiovascular events.
Supplementary Material
Article Information
Funding. DCCT/EDIC has been supported by cooperative agreement grants (1982–1993, 2012–2017) and contracts (1982–2012) with the Division of Diabetes, Endocrinology, and Metabolic Diseases of the National Institute of Diabetes and Digestive and Kidney Diseases (current grant numbers U01-DK-094176 and U01-DK-094157) and through support from the National Eye Institute, the National Institute of Neurological Disorders and Stroke, the General Clinical Research Centers Program (1993–2007), and the Clinical and Translational Science Center Program (2006–present), Bethesda, MD. Industry contributors have had no role in DCCT/EDIC but have provided free or discounted supplies or equipment to support participants’ adherence to the study: Abbott Diabetes Care (Alameda, CA), Animas (Westchester, PA), Bayer Diabetes Care (North America Headquarters, Tarrytown, NY), Becton Dickinson (Franklin Lakes, NJ), Eli Lilly (Indianapolis, IN), Extend Nutrition (St. Louis, MO), Insulet Corporation (Bedford, MA), LifeScan (Milpitas, CA), Medtronic Diabetes (Minneapolis, MN), Nipro Home Diagnostics (Ft. Lauderdale, FL), Nova Diabetes Care (Billerica, MA), Omron (Shelton, CT), Perrigo Diabetes Care (Allegan, MI), Roche Diabetes Care (Indianapolis, IN), and Sanofi (Bridgewater, NJ).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. D.M.N. and J.M.L. wrote the initial draft of the manuscript. I.B. and B.H.B. conducted statistical analyses under the direction of J.M.L. I.B., B.H.B., T.J.O., C.C.C., M.L.-V., and M.S. contributed revisions to the manuscript. All authors approved the final content. J.M.L. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Appendix
Writing Group: David M. Nathan (Massachusetts General Hospital, Harvard Medical School, Boston, MA); Ionut Bebu, Barbara H. Braffett, and John M. Lachin (The Biostatistics Center, George Washington University, Rockville, MD); Trevor J. Orchard (Graduate School of Public Health, University of Pittsburgh, Pittsburgh, PA); Catherine C. Cowie (National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD); Maria Lopes-Virella (Medical University of South Carolina, Charleston, SC); and Mark Schutta (Hospital of the University of Pennsylvania, Philadelphia, PA).
Footnotes
Clinical trial reg. nos. NCT00360893 and NCT00360815, clinicaltrials.gov.
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db15-1517/-/DC1.
A complete list of participants in the DCCT/EDIC Research Group is presented in the Supplementary Data published online for the article in N Engl J Med 2015;372:1722–1733.
Members of the Writing Group are listed in the appendix.
References
- 1.Orchard TJ, Costacou T, Kretowski A, Nesto RW. Type 1 diabetes and coronary artery disease. Diabetes Care 2006;29:2528–2538 [DOI] [PubMed] [Google Scholar]
- 2.Livingstone SJ, Looker HC, Hothersall EJ, et al. Risk of cardiovascular disease and total mortality in adults with type 1 diabetes: Scottish Registry Linkage Study. PLoS Med 2012;9:e1001321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soedamah-Muthu SS, Fuller JH, Mulnier HE, Raleigh VS, Lawrenson RA, Colhoun HM. High risk of cardiovascular disease in patients with type 1 diabetes in the U.K.: a cohort study using the general practice research database. Diabetes Care 2006;29:798–804 [DOI] [PubMed] [Google Scholar]
- 4.Jensen T, Borch-Johnsen K, Kofoed-Enevoldsen A, Deckert T. Coronary heart disease in young type 1 (insulin-dependent) diabetic patients with and without diabetic nephropathy: incidence and risk factors. Diabetologia 1987;30:144–148 [DOI] [PubMed] [Google Scholar]
- 5.Orchard TJ, Olson JC, Erbey JR, et al. Insulin resistance-related factors, but not glycemia, predict coronary artery disease in type 1 diabetes: 10-year follow-up data from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 2003;26:1374–1379 [DOI] [PubMed] [Google Scholar]
- 6.Pambianco G, Costacou T, Ellis D, Becker DJ, Klein R, Orchard TJ. The 30-year natural history of type 1 diabetes complications: the Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes 2006;55:1463–1469 [DOI] [PubMed] [Google Scholar]
- 7.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 8.Nathan DM, Cleary PA, Backlund JY, et al.; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group . Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005;353:2643–2653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The DCCT Research Group The Diabetes Control and Complications Trial (DCCT). Design and methodologic considerations for the feasibility phase. Diabetes 1986;35:530–545 [PubMed] [Google Scholar]
- 10.The DCCT/EDIC Research Group Epidemiology of Diabetes Interventions and Complications (EDIC). Design, implementation, and preliminary results of a long-term follow-up of the Diabetes Control and Complications Trial cohort. Diabetes Care 1999;22:99–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The DCCT Research Group Feasibility of centralized measurements of glycated hemoglobin in the Diabetes Control and Complications Trial: a multicenter study. Clin Chem 1987;33:2267–2271 [PubMed] [Google Scholar]
- 12.Williams KV, Erbey JR, Becker D, Arslanian S, Orchard TJ. Can clinical factors estimate insulin resistance in type 1 diabetes? Diabetes 2000;49:626–632 [DOI] [PubMed] [Google Scholar]
- 13.Lachin JM, Orchard TJ, Nathan DM; DCCT/EDIC Research Group . Update on cardiovascular outcomes at 30 years of the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study. Diabetes Care 2014;37:39–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hsieh FY, Lavori PW. Sample-size calculations for the Cox proportional hazards regression model with nonbinary covariates. Control Clin Trials 2000;21:552–560 [DOI] [PubMed] [Google Scholar]
- 15.Lachin JM. Biostatistical Methods: The Assessment of Relative Risks. 2nd ed. Hoboken, NJ, Wiley, 2011 [Google Scholar]
- 16.Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. New York, Berlin, Springer, 2000 [Google Scholar]
- 17.Claeskens G, Hjort NL. Model selection and Model Averaging. Cambridge, New York, Cambridge University Press, 2008 [Google Scholar]
- 18.Tibshirani R. The lasso method for variable selection in the Cox model. Stat Med 1997;16:385–395 [DOI] [PubMed] [Google Scholar]
- 19.Lind M, Bounias I, Olsson M, Gudbjörnsdottir S, Svensson AM, Rosengren A. Glycaemic control and incidence of heart failure in 20,985 patients with type 1 diabetes: an observational study. Lancet 2011;378:140–146 [DOI] [PubMed] [Google Scholar]
- 20.Miller RG, Secrest AM, Ellis D, Becker DJ, Orchard TJ. Changing impact of modifiable risk factors on the incidence of major outcomes of type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 2013;36:3999–4006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaiswal M, Schinske A, Pop-Busui R. Lipids and lipid management in diabetes. Best Pract Res Clin Endocrinol Metab 2014;28:325–338 [DOI] [PubMed] [Google Scholar]
- 22.Tolonen N, Forsblom C, Mäkinen VP, et al.; FinnDiane Study Group . Different lipid variables predict incident coronary artery disease in patients with type 1 diabetes with or without diabetic nephropathy: the FinnDiane study. Diabetes Care 2014;37:2374–2382 [DOI] [PubMed] [Google Scholar]
- 23.American Diabetes Association Standards of Medical Care in Diabetes—2015 Diabetes Care 2015;38(Suppl.):3S1–S93 [Google Scholar]
- 24.May O, Arildsen H, Damsgaard EM, Mickley H. Cardiovascular autonomic neuropathy in insulin-dependent diabetes mellitus: prevalence and estimated risk of coronary heart disease in the general population. J Intern Med 2000;248:483–491 [DOI] [PubMed] [Google Scholar]
- 25.Laing SP, Swerdlow AJ, Slater SD, et al. Mortality from heart disease in a cohort of 23,000 patients with insulin-treated diabetes. Diabetologia 2003;46:760–765 [DOI] [PubMed] [Google Scholar]
- 26.Peters SA, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775,385 individuals and 12,539 strokes. Lancet 2014;383:1973–1980 [DOI] [PubMed] [Google Scholar]
- 27.Peters SA, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia 2014;57:1542–1551 [DOI] [PubMed] [Google Scholar]
- 28.Mozaffarian D, Benjamin EJ, Go AS, et al.; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation 2015;131:e29–e322 [DOI] [PubMed] [Google Scholar]
- 29.Ferrara A, Mangione CM, Kim C, et al.; Translating Research Into Action for Diabetes Study Group . Sex disparities in control and treatment of modifiable cardiovascular disease risk factors among patients with diabetes: Translating Research Into Action for Diabetes (TRIAD) Study. Diabetes Care 2008;31:69–74 [DOI] [PubMed] [Google Scholar]
- 30.Larkin ME, Backlund JY, Cleary P, et al.; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Research Group . Disparity in management of diabetes and coronary heart disease risk factors by sex in DCCT/EDIC. Diabet Med 2010;27:451–458 [DOI] [PubMed] [Google Scholar]
- 31.Williams K, Tchernof A, Hunt KJ, Wagenknecht LE, Haffner SM, Sniderman AD. Diabetes, abdominal adiposity, and atherogenic dyslipoproteinemia in women compared with men. Diabetes 2008;57:3289–3296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peters SA, Huxley RR, Sattar N, Woodward M. Sex differences in the excess risk of cardiovascular diseases associated with type 2 diabetes: potential explanations and clinical implications. Curr Cardiovasc Risk Rep 2015;9:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Costacou T, Evans RW, Orchard TJ. High-density lipoprotein cholesterol in diabetes: is higher always better? J Clin Lipidol 2011;5:387–394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meigs JB, Wilson PW, Fox CS, et al. Body mass index, metabolic syndrome, and risk of type 2 diabetes or cardiovascular disease. J Clin Endocrinol Metab 2006;91:2906–2912 [DOI] [PubMed] [Google Scholar]
- 35.Conway B, Miller RG, Costacou T, et al. Adiposity and mortality in type 1 diabetes. Int J Obes 2009;33:796–805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Soedamah-Muthu SS, Chaturvedi N, Witte DR, Stevens LK, Porta M, Fuller JH; EURODIAB Prospective Complications Study Group . Relationship between risk factors and mortality in type 1 diabetic patients in Europe: the EURODIAB Prospective Complications Study (PCS). Diabetes Care 2008;31:1360–1366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.The DCCT Research Group Adverse events and their association with treatment regimens in the diabetes control and complications trial. Diabetes Care 1995;18:1415–1427 [DOI] [PubMed] [Google Scholar]
- 38.Williams KV, Erbey JR, Becker D, Orchard TJ; The Epidemiology of Diabetes Complications Study . Improved glycemic control reduces the impact of weight gain on cardiovascular risk factors in type 1 diabetes. Diabetes Care 1999;22:1084–1091 [DOI] [PubMed] [Google Scholar]
- 39.Pedersen MM, Christensen CK, Mogensen CE. Long-term (18 year) prognosis for normo- and microalbuminuric type 1 (insulin-dependent) diabetic patients. Diabetologia 1992;35(Suppl.):A60 [Google Scholar]
- 40.Matsushita K, Coresh J, Sang Y, et al.; CKD Prognosis Consortium . Estimated glomerular filtration rate and albuminuria for prediction of cardiovascular outcomes: a collaborative meta-analysis of individual participant data. Lancet Diabetes Endocrinol 2015;3:514–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.DCCT/EDIC Research Group Effect of intensive diabetes treatment on albuminuria in type 1 diabetes: long-term follow-up of the Diabetes Control and Complications Trial and Epidemiology of Diabetes Interventions and Complications study. Lancet Diabetes Endocrinol 2014;2:793–800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.D’Agostino RB Sr, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008;117:743–753 [DOI] [PubMed] [Google Scholar]
- 43.The Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular outcomes in type 1 diabetes: the DCCT/EDIC Study 30-year follow-up. Diabetes Care 2016;39:790–797
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.