Abstract
Aim:
The objective was to compare the use of autologous dermal and temporalis fascia grafts in the treatment of acquired penile curvatures.
Materials and Methods:
It was a prospective observational study of 33 cases, conducted in Sher-i-Kashmir Institute of Medical Sciences, Srinagar from March 2007 to September 2013. All the patients had stable Peyronies disease (PD). Dorsal, dorsolateral and vental curvatures with good preoperative erections were included. PD index with visual analog scales for curvature was used preoperatively. An informed written consent was taken from all the patients with main emphasis on erectile dysfunction.
Results:
After an average follow up of 2 years, complete straightening of penis was observed in all patients with satisfactory sexual intercourse in 30 patients (90%). Three patients (10%) required frequent use of type 5 phosphodiesterase inhibitors for adequate erections. Overall 91% of patients and partners were satisfied with the procedure and cosmetically donor site was better in temporalis fascia graft site. No rejection of any graft was noted and glans hypoesthesia was noticed in 4 patients (12%). None of the patients required penile prosthesis. Total operative time for harvesting and application of the graft was more in dermal grafts (>3 hrs) than for temporalis fascia graft (2 hrs).
Conclusion:
Tunical lengthening procedures by autologous free grafts represents a safe and reproducible technique. A good preoperative erectile function is required for tunical lengthening procedure. Temporalis fascia graft is thin, tough membrane and effective graft for PD with good cosmetic and functional results.
Keywords: Acquired penile, autologous grafts, curvature
INTRODUCTION
Francois Gigotde la Peyronie is credited with a description of peyronie's in 1741.[1] His original description was one of the fibrous cavernositis preventing them from having normal ejaculation of semen. The condition is believed to occur following penile trauma, and is characterized by the formation of a palpable scar that does not stretch in the erect state along with the remaining tunica albuginea. There are two phases-1. Active phase which lasts from 6-18mnths, and, 2. Quiescent phase (stable form). Active phase is characterized by painful erections and changing penile deformity. Quiescent phase by deformity stabilization, fibrosis, plaque and disappearance of painful erections. Peyronie's disease (PD) is associated with dupuytrens contracture, tympanosclerosis, plantar fascial contractures, urethral instrumentation, trauma and medical disease like diabetes, pagets disease and gout.[2] PD can also occur in a familial pattern.[3] and is associated with psychological distress for the patient and her partner as well as sexual relationship strife.[4] PD is a progressive disorder with up to 48% of men experiencing disease progression if left untreated and frequently associated with erectile dysfunction (ED). Despite the numerous medical treatments for PD, none has showed a high success rate. Fortunately, most of the patients require only reassurance and education. Surgical treatment[5,6] is the mainstay of therapy for patients with severe curvature or narrowing that causes difficulty in penetration, affecting both patients and partner's quality of living.
MATERIALS AND METHODS
From March 2005 to September 2013 total 33 patients with stable PD (1-2 years duration) were enrolled into our study. Study was carried out in Sheri Kashmir institute of Medical Sciences Srinagar in the department of Urology. Inclusion criteria were- (1) stable disease with difficulty in engaging coital activity. (2) Stable disease with failure of conservative therapy. (3) Curvatures of more than 60°. Patients with stable disease and poor pre operative erections were excluded from the study. All patients underwent a detailed history and clinical examination of phallus in both flaccid and erect state after vasoactive intracavernosal injection of papaverine. A rigid ruler was used to assess the stretched penile length in the supine position from the pubic bone to meatus dorsally. The size, number of plaque and site of plaque was noted. Clinical examination of hands and feet was done to rule out any duptuyrens contracture. None of our patients had any associated co morbid condition. PD index with visual analog scales for curvature was done. Stretched penile length was recorded pre and postoperatively. Detailed operative consent with honest discussion about the procedure and the possibility of the recurrent curvature, diminished rigidity, ED and penile prosthesis for ED was done
SURGICAL PROCEDURE
Surgery was carried out under general anesthesia by the method of degloving the penis by circumferential incision followed by artificial erection [Figure 1].
Figure 1.
Various plates showing dorsal curvature, artificial erection, outer half of plaque excision, completion of graft with neurovascular bundle kept back, and after 3 months of dermal graft interposition normal penile erection on intracavernosal papaverine
After artificial erection degree of curvature was assessed
Bucks fascia was dissected and neurovascular bundle was separated from the site of plaque
Multiple parallel incisions were given over the dorsal and dorsolateral plaque, and outer half of the plaque was removed meticulously by using no 11 scalpels, so that a very thin covering of the plaque was left in situ to avoid injury to underlying erectile tissue
In ventral curvature urethra was mobilized from corporeal bodies with multiple parallel incisions given over the extensive plaque. Same technique was utilized for plaque removal as that of dorsal/dorsolateral plaque
Autologous free dermal graft was harvested by more than 30% of the defect to compensate for its contracture in post operative period, while as temporalis fascia of the same size was harvested as the size of the defect
Dermal graft was completely defatted and both temporalis fascia and dermal graft soaked in normal saline solution for 10 min
Donor site was closed by subcuticular suture to avoid suture removal in postoperative period
In both dorsal and ventral curvatures defect was filled by free graft by using 5-0 proline suture in a watertight fashion
Artifical intraoperative erection was done to check augmented corporeal anastomosis for any leak and residual curvature
Neurovascular bundle was kept back and bucks fascia sutured back using vicryl suture 3-0.
Length of operative time and harvesting time for dermal graft and defatting the graft was on an average 75 min and for harvesting the temporalis fascia graft was 30 min.
Redivac suction drain was kept in situ for 24 h and the patient was discharged on day 1
Postoperatively patient was put on the tablet Ethinyl estradiol 0.1 mg OD for 2 weeks and patients were instructed to refrain from sexual intercourse for 3 months
Follow up; Typically the patient was seen after 2 weeks of surgery and was advised to stop tablet ethinyl estradiol and do massage therapy, and gently stretch the penis afer shower daily for 5-10 min for 3 months. Nocturnal type 5 phosphodiesterase inhibitors were given twice in a week after 1 month of surgery to enhance postoperative vasodilation to support the graft.
RESULTS
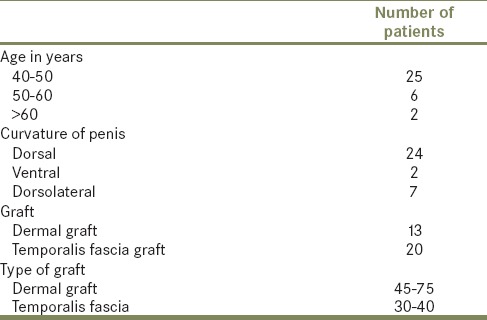
Most of the plaques were on the dorsal side and curvature angle varied between 60° and 90° degrees leading to difficulty in intercourse [Table 1]. Most of the patients were in the age group of 40-50 years and PD was present in a stable form at the time of surgical intervention. In all patients complete straightening of the penis was observed. With a follow up of 2 years, overall 91% of patients and partners were satisfied with the procedure. Cosmetically donor site was better in temporalis fascia graft site as the suture line was camouflaged by normal hair line. No rejection of any graft was noted and glans hypothesia was noticed in 4 patients (12%). Three patients required oral type 5 phosphodiesterase inhibitors for adequate penile rigidity for satisfactorily sexual intercourse. Three patients were unsatisfied with the procedure and reason was early detumescence on penetrative intercourse after erection (2 patients of dorsal and one patient with ventral curvature). None of the patients required penile prosthesis. Total operative time for harvesting and application of the graft was more in dermal grafts (>3 h) than for temporalis fascia graft (2 h). Aim of the procedure was complete straightening of the penis with preserved preoperative erectile function with successful resumption of coitus in all patients with resolution of penile curvature and partner satisfaction was accepted as functional success.
Table 1.
Clinical profile of the patients
DISCUSSION
Peyronie's disease is a sexually debilitating disease causing penile deformity which results in difficulty in penetrative intercourse or even total coital incapacity, as well as psychological distress for the patient and her partner. PD regresses spontaneously in 13% of men, progressing in 40% of untreated ones, and showing no change over time in 47%.[7] Surgical correction is reserved for those patients who fail conservative measures and with stable disease. In the adult patient with PD the curvature causes more psychologial disability than physical disability, where as in the older man with good understanding with his partner is better able to cope with a more severe degree of penile deformity. Of note, ventral curvature causes more difficulty in vaginal penetration than dorsal or dorsolateral one. A 6 month duration of stable disease should surpass before surgery is undertaken, while as less than 6 month duration suffer recurrence postoperatively.[7] Levine proposed an algorithm for the surgical treatment of PD. Simple curvatures < 60° with adequate erectile capacity were candidates for plications, on the other hand tunical lengthening procedures are indicated for complex curvature >60°-90° and short penile length.[8]
Patients with complex curvatures and poor preoperative erections are better treated with penile implantation.[9] penile prosthesis implantation alone results in satisfactory straightening of the penis in patients with mild deformity, but when residual curvature is greater than 20°, additional maneuvers as manual modeling, plication and tunical incision with or without grafting are required to achieve complete straightening.[9,10,11,12,13,14,15,16,17] Historically total plaque excision was designed to remove the diseased tunica, but total plaque excision results in an unacceptably high rate of postoperative ED, probably, as a result, of a compromised veno-occlusive mechanism because of the changes in the relationship between the cavernosum tissue and the overlying graft. Being informed of the advantages and disadvantages of the tunica lengthening procedures, patients and their partners are better able to make an informed decision about the procedure. We operate only those patients with rigid preoperatively erections with complex curvatures. For patients with poor preoperative erections and curvature > 60° we recommend penile prosthesis. In 1974, Horton and Devine devised a procedure using a dermal skin graft after excision of the peyronies plaque to fill the corporal defect.[18] The success of this procedure has been widely reported, while morbidity can be significant and ED follows surgery. Proper patient selection with pre surgery rigid erectile function produces excellent results in most of these patients.[19,20,21] While the ideal graft substitute continues to elude us, we modify the classic H- type incision as multiple parallel incisions over the plaque and keeping a very thin transparent layer till underlying cavernosal tissue is visible. We believe this allows a uniform expansion of plaque area and prevents venoocclusive dysfunction as no cavernosal tissue is exposed in our technique. Most important prerequisite in tunical lengthening procedures is normal rigid presurgery erections. Moreover studies indicate that most critical criterion for any grafting procedure appear to be the quality of their preoperative erections.[22,23,24] kargi et al., lutilized fascia lata grafting with relaxing incision for the surgical correction of PD with one or more years of follow up, and all had statistically significantly penile lengthening.[25] Egydio et al., reported the results of the incomplete circumferential incision of a penile plaque and use of bovine pericardial graft. The authors achieved an 88% rate of penile correction in 33 PD patients, with a mean increase of 2.21 cm in penile length.[15] In our series complete penile straightening was achieved in all patients with either dermal or temporalis fascia graft and successful rigid erection and partner satisfaction was achieve in 30 patients (>90%). With a follow up of 2 years no significant recurrent curvature was observed. Similar results in penile lenghtening with either incision/excision plus grafting were achieved in 63-100%.[26,27,28] However, in the literature, depending on the graft material used, >30° curvature can be seen from 0% to 16% with plaque incision/excision and grafting procedure.[28,29] Ideal graft for PD has been continuously debated. Packaged autologous grafts are readily available, and well tolerated material for PD. However in third world countries due to financial constraints we believe autologous tissue such as temporalis fascia, dermal graft, fascia lata, saphenous vein graft and tunica vaginalis and other autologous materials are the best choice and these do not need any sophisticated techniques for harvesting the graft. We believe harvesting time is less for temporalis fascia graft as a second team of surgeons can be utilized and the incision line gets camouflaged by hair line. In our series three patients had preoperatively received intracorporeal steroid triamcinolone injection with stable disease, subsequently underwent tunical lengthening procedures. Intraoperative dissection was difficult in elevating Bucks fascia and separating neurovascular bundle because of ongoing tunical inflammation with significant glans hypothesia. We believe patient with stable disease and significant penile curvature that interferes intercourse, intracorpeal injection to be avoided as such patients with good rigid preoperatively erections invariably requires tunical lenghtening procedures. In our series no preoperative penile Doppler was used, however the baseline erectile function is necessary for medicolegal purposes. The assessed parameters include peak-systolic velocity (psv), end-diastolic velocity (EDV) and resistive index (RI). Compromised arterial inflow is represented by PSV < 25 cm/S, veno-occlusive dysfunction by EDV > 5 cm/S, and overall ED by RI < 0.8.[30] In our series penile doppler was done postoperatively in five patients and indication was poor penile erection with the rapid detumescence. Three patients had venoocclusive dysfunction on penile Doppler.
CONCLUSION
Tunical lengthening procedures by autologous free grafts represents a safe and reproducible technique. A good and rigid preoperative erectile function is required for tunical lengthening procedure. Temporalis, fascia graft, is thin, tough membrane, easy to harvest and effective graft for PD with good cosmetic and functional results. Based on the results of our study and the literature, we advocate a modified multiple parallel incisions over the calcified plaque, and remove meticulously the outer half of the plaque till a very delicate covering of part of the plaque is visible so that underlying erectile tissue relationship with the tunica albuginea is not disturbed, and it allows a uniform expansion of augmented graft over the excised plaque.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.de la Peyronie FG. “Sur quelques obstacles qui s’opposent ’al´ejaculation naturelle de la semence, ” Memoires de I’Academic Royale des Sciences Montpellier Chir. 1943;1:425–39. [Google Scholar]
- 2.Carrieri MP, Serraino D, Palmiotto F, Nucci G, Sasso F. A case-control study on risk factors for Peyronie's disease. J Clin Epidemiol. 1998;51:511–5. doi: 10.1016/s0895-4356(98)00015-8. [DOI] [PubMed] [Google Scholar]
- 3.Nyberg LM, Jr, Bias WB, Hochberg MC, Walsh PC. Identification of an inherited form of Peyronie's disease with autosomal dominant inheritance and association with Dupuytren's contracture and histocompatibility B7 cross-reacting antigens. J Urol. 1982;128:48–51. doi: 10.1016/s0022-5347(17)52751-2. [DOI] [PubMed] [Google Scholar]
- 4.Nelson CJ, Mulhall JP. Psychological impact of Peyronie's disease: A review. J Sex Med. 2013;10:653–605. doi: 10.1111/j.1743-6109.2012.02999.x. [DOI] [PubMed] [Google Scholar]
- 5.Bella AJ, Perelman MA, Brant WO, Lue TF. Peyronie's disease (CME) J Sex Med. 2007;4:1527–38. doi: 10.1111/j.1743-6109.2007.00614.x. [DOI] [PubMed] [Google Scholar]
- 6.Kendrici M, Hellstrom WJ. Critical analysis of surgery for Peyronie's disease. Curr Opin Urol. 2004;6:382–8. doi: 10.1097/00042307-200411000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Gelbard MK, Dorey F, James K. The natural history of Peyronie's disease. J Urol. 1990;144:1376–9. doi: 10.1016/s0022-5347(17)39746-x. [DOI] [PubMed] [Google Scholar]
- 8.Levine LA, Lenting EL. A surgical algorithm for the treatment of Peyronie's disease. J Urol. 1997;158:2149–52. doi: 10.1016/s0022-5347(01)68184-9. [DOI] [PubMed] [Google Scholar]
- 9.Ralph DJ, Gonzalez-Cadavid N, Mirone V, Perovic S, Sohn M, Usta M, et al. The management of Peyronie's disease: Evidence-based 2010 guidelines. J Sex Med. 2010;7:2359–74. doi: 10.1111/j.1743-6109.2010.01850.x. [DOI] [PubMed] [Google Scholar]
- 10.Kendrici M, Trost L, Sikka SC, Hellstrom GJ. Diabetes mellitus is associated with severe Peyronie's disease. BJU Int. 2007;99:383–6. doi: 10.1111/j.1464-410X.2007.06611.x. [DOI] [PubMed] [Google Scholar]
- 11.Kadioglu A, Tefekli A, Erol B, Oktar T, TuncMet al. A retrospective review of 307 men with Peyronie's disease. J Urol. 2002;68:1075–9. doi: 10.1016/S0022-5347(05)64578-8. [DOI] [PubMed] [Google Scholar]
- 12.Mulhall JP, Schiff J, Guhring P. An analysis of the natural history of Peyronie's disease. J Urol. 2006;175:2115–8. doi: 10.1016/S0022-5347(06)00270-9. [DOI] [PubMed] [Google Scholar]
- 13.Egydio PH, Lucon AM, Arap S. A single relaxing incision to correct different types of penile curvature: Surgical technique based on geometrical principles. BJU Int. 2004;94:1147–57. doi: 10.1111/j.1464-410X.2004.05220.x. [DOI] [PubMed] [Google Scholar]
- 14.Egydio PH. Surgical straightening with tunical incision and grafting technique-single relaxing incision based on geometrical principles. In: Levine LA, editor. Peyronie's Disease Textbook: A Guide to Clinical Management. Totowa: Hymana Press; 2006. pp. 227–3. [Google Scholar]
- 15.Egydio PH, Lucon AM, Arap S. Treatment of Peyronie's disease by incomplete circumferential incision of the tunica albuginea and plaque with bovine pericardium graft. Urology. 2002;59:570–4. doi: 10.1016/s0090-4295(01)01651-x. [DOI] [PubMed] [Google Scholar]
- 16.Wilson SK, Delk 2nd., Jr A new treatment for Peyronie's disease: Modeling the penis over an inflatable penile prosthesis. J Urol. 1994;152:1121–3. doi: 10.1016/s0022-5347(17)32519-3. [DOI] [PubMed] [Google Scholar]
- 17.Dakin BL, Carter MF. Venogenic impotence following dermal graft repair for Peyronie's disease. J Urol. 1991;146:849–51. doi: 10.1016/s0022-5347(17)37941-7. [DOI] [PubMed] [Google Scholar]
- 18.Devine CJ, Jr, Horton CE. Surgical treatment of Peyronie's disease with dermal graft. J Urol. 1974;111:44–6. doi: 10.1016/s0022-5347(17)59886-9. [DOI] [PubMed] [Google Scholar]
- 19.Wild RM, Devine CJ, Horton CE. Dermal graft repair of Peyronie's disease: Survey of 50 patients. J Urol. 1979;121:47. doi: 10.1016/s0022-5347(17)56657-4. [DOI] [PubMed] [Google Scholar]
- 20.Lue TF, El-Sakka AI. Venous patch graft for Peyronie's disease. Part I: Technique. J Urol. 1998;160:2047. doi: 10.1097/00005392-199812010-00029. [DOI] [PubMed] [Google Scholar]
- 21.Gelbard MK, Hayden B. Expanding contractures of the tunica albuginea due to Peyronie's disease with temporalis Fascia free grafts. J Urol. 1991;145:772. doi: 10.1016/s0022-5347(17)38447-1. [DOI] [PubMed] [Google Scholar]
- 22.Taylor F, Abern M, Levine LA. Predicting erectile dysfunction following surgical correction of Peyronie's disease without inflatable penile prosthesis placement: Vascular assessment and preoperative risk factors. J Sex Med. 2012;9:296–301. doi: 10.1111/j.1743-6109.2011.02460.x. [DOI] [PubMed] [Google Scholar]
- 23.Flores S, Choi J, Alex B, Mulhall JP. Erectile dysfunction after plaque incision and grafting: Short-term assessment of incidence and predictors. J Sex Med. 2011;8:2031–7. doi: 10.1111/j.1743-6109.2011.02299.x. [DOI] [PubMed] [Google Scholar]
- 24.Levine LA, Greenfield JM, Estrada CR. Erectile dysfunction following surgical correction of Peyronie's disease and a pilot study of the use of sildenafil citrate rehabilitation for postoperative erectile dysfunction. J Sex Med. 2005;2:241–7. doi: 10.1111/j.1743-6109.2005.20234.x. [DOI] [PubMed] [Google Scholar]
- 25.Kargi E, Yeşilli C, Hoşnuter M, Akduman B, Babuccu O, et al. Relaxation incision and fascia lata grafting in the surgical correction of penile curvature in Peyronie's disease. Plast Reconstr Surg. 2004;113:254–9. doi: 10.1097/01.PRS.0000095951.04305.38. [DOI] [PubMed] [Google Scholar]
- 26.Gur S, Limin M, Hellstrom WJ. Current status and new developments in Peyronie's disease: Medical, minimally invasive and surgical treatment options. Expert Opin Pharmacother. 2011;12:931–44. doi: 10.1517/14656566.2011.544252. [DOI] [PubMed] [Google Scholar]
- 27.Breyer BN, Brant WO, Garcia MM, Bella AJ, Lue TF. Complications of porcine small intestine submucosa graft for Peyronie's disease. J Urol. 2007;177:589–91. doi: 10.1016/j.juro.2006.09.051. [DOI] [PubMed] [Google Scholar]
- 28.Cormio L, Zucchi A, Lorusso F, Selvaggio O, Fioretti F, et al. Surgical treatment of Peyronie's disease by plaque incision and grafting with buccal mucosa. Eur Urol. 2009;55:1469–75. doi: 10.1016/j.eururo.2008.11.041. [DOI] [PubMed] [Google Scholar]
- 29.Usta MF, Bivalacqua TJ, Sanabria J, Koksal IT, Moparty K, et al. Patient and partner satisfaction and long-term results after surgical treatment for Peyronie's disease. Urology. 2003;62:105–9. doi: 10.1016/s0090-4295(03)00244-9. [DOI] [PubMed] [Google Scholar]
- 30.Sikka SC, Hellstrom WJ, Brock G, Morales AM. Standardization of vascular assessment of erectile dysfunction: Standard operating procedures for duplex ultrasound. J Sex Med. 2013;10:120–9. doi: 10.1111/j.1743-6109.2012.02825.x. [DOI] [PubMed] [Google Scholar]



