Abstract
We present a case of spontaneous retrograde migration of ureterovesical junction stone to the kidney. A 26-year-old Bahraini male, diagnosed with left lower ureteric stone 7 months before this presentation. On his recent presentation, the stone has migrated down but not passed, confirmed on imaging. Operative removal was planned. X-ray kidney ureter bladder (KUB) in the morning of surgery did not reveal stone in the ureter, but the same shadow was seen in the kidney. An urgent computerized tomography-KUB was done, and this confirms the stone has migrated to the kidney. Surgery was canceled, and the stone was dealt with extracorporeal shockwave lithotripsy and was fragmented in the first session. This retrograde migration of lower ureteric stone to the kidney is not reported in the English literature in human before.
Keywords: Retrograde peristalsis, spontaneous migration, ureteric stone
INTRODUCTION
Urolithiasis is a common diagnosis of patients with acute abdominal pain or flank pain presenting to the emergency room.[1] The lifetime risk of developing urolithiasis is 13% in males and 7% in females.[2] The expected outcome of ureteral stones is spontaneous expulsion in 29.1% while other patients requiring medical or surgical intervention.[3] The stone moves downward with the urine by peristalsis waves in the ureter. A yo-yo mechanism is seen in the upper ureter and lower ureter.[4,5] Our case is unique because of retrograde stone migration in the kidney.
CASE REPORT
A 26-year-old male patient presented to our Department of Emergency Medicine (EMD) on 17th September 2014 with left flank pain and gross hematuria. The pain was radiating to the suprapubic area.
Noncontrast spiral computerized tomography-kidney ureter bladder (CT-KUB) was done next day [Figure 1]. It revealed a single stone, 7.5 mm in the lower third of ureter, with proximal hydro ureter. The stone was radio-opaque on X-ray KUB [Figure 2].
Figure 1.
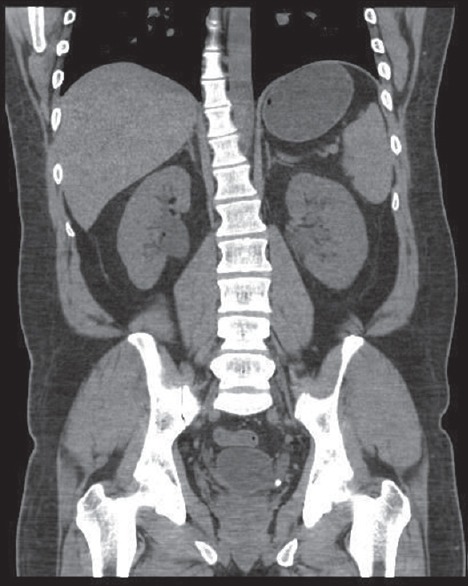
Stone in ureter with hydronephrosis
Figure 2.
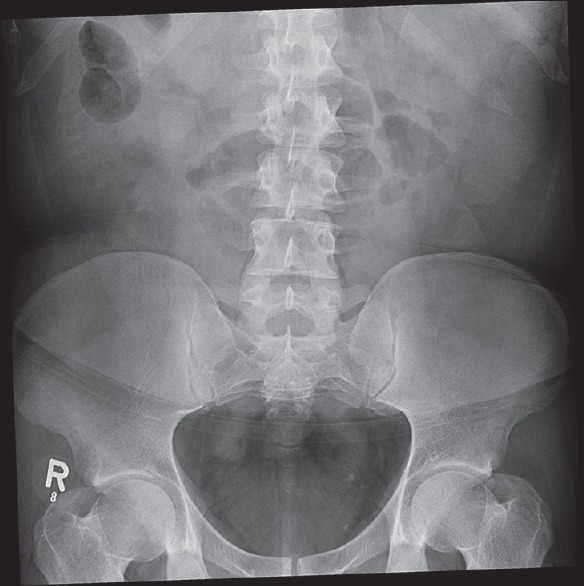
Stone in the left lower ureter
Past medical and surgical history were unremarkable. Clinical examination and laboratory investigations including urine analysis, complete blood count, and renal function test were all fine except for microscopic hematuria.
On September 23, 2014, he was admitted with pain from EMD and was started on medical expulsive therapy, comprising alfuzosin, diclofenac sodium, paracetamol, and omeprazole in appropriate doses. He was discharged home next day with a planned follow-up in 2 weeks’ time. As he was asymptomatic afterward, he neglected the clinic appointment and never reported back to clinic. He presented again with left ureteral colic on April 26, 2015 (after 7 months), repeat CT-KUB shows the same single stone has migrated slightly down, with no formation of other stones. Surgical intervention was planned due to the failure of medical expulsive therapy and noncompliant patient.
X-ray KUB in the morning of surgery revealed a radiopaque shadow in the left kidney, and the previous shadow in the left lower ureter was absent [Figure 3]. No history of stone passage was noted for the past 3 days. Repeat CT confirmed a single 7.5 mm stone in the left lower calyx and no stone in the ureter with the alleviation of the hydroureter. No other stones were picked on CT-KUB [Figure 4]. The planned surgery was canceled, and extracorporeal shockwave lithotripsy was done for the renal stone.
Figure 3.
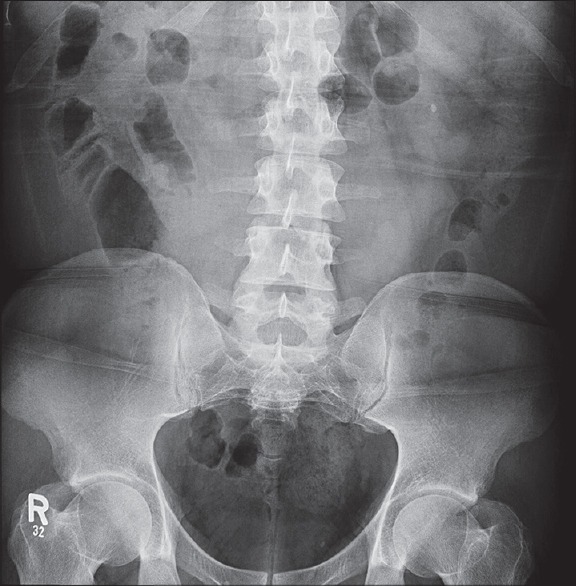
Stone moved to left kidney
Figure 4.
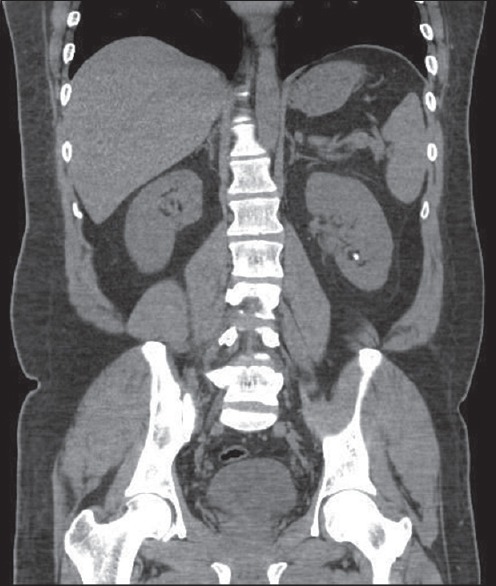
Stone moved to left kidney with resolution of hydronephrosis
On June 17, 2015, the patient presented to EMD with left sided ureteric colic, X-ray KUB showed stone fragment in the left lower ureter at the vesico-ureteric junction. The patient underwent left ureteroscopy and stone fragment was removed with a basket.
DISCUSSION
Urolithiasis is a common disease, with prevalence ranging from 1% to 20%.[6] In a regional middle eastern study, the prevalence of urinary calculi according to ethnic origin in descending order of frequency was Egyptians (29.5%), Pakistani (24.9%), Indian (23.3%), Yemeni (20.5%), Sudanese (17.6%), Bangladeshi (16.2%), Eritrean (15.4%), and Saudi Arabian (7.4%).[7]
Stone formation is the process of crystallization of bio-minerals and biological matrix. It requires supersaturated urine, a status that is, variable depending on many factors such as urine pH, mineral ions concentration and constituent that changes throughout the day from relatively acidic urine in the first morning void to alkaline pH after meals.[1,5]
Urine is passed in downward fashion, from kidneys to bladder, through synchronized peristaltic motion of the ureteric smooth muscles, controlled by a spontaneously firing and progressively propagating pacemaker cells embedded in the renal pelvis and along the ureters. This physiological motion ensures the movement of urine from proximal to distal in a coordinated manner.[8] The backward movement of urine is not observed in normal ureter except for refluxing ureter.
Although the presenting symptoms of the ureteric stone have not changed over years, diagnostic modalities have been refined, become less invasive and more specific. Now CT-KUB is considered to be the gold standard in diagnosing them, it is the most accurate imaging modality in diagnosing a patient with renal and ureteric colic, it clearly demonstrate the site and size of the stone and delineates any associated back pressure changed or anatomical abnormalities.[3] The rate of spontaneous stone passage is 68% for stones of <5 mm, and 47% in stones of size 5–10 mm3. Metabolic workup for recurrent stone formers and dietary advice has gained more support. A multidisciplinary approach including a nephrologist, endocrinologist, and dietician along with the urologist is the order of the day.
About 70% of stone formation remains idiopathic. Dietary, genetic, lack of adequate fluid intake, hot working environment along with congenital anomalies such as pelvi-ureteric junction obstruction, bifid upper ureter, or duplex renal pelvis all are associated with increased incidence of stone formation.[4]
In our patient, our plausible theory is that there is a short period of reverse ureteral peristalsis has taken place, which has moved the stone toward to the kidney. A similar phenomenon has been observed in the canines and reported in the veterinary literature.[9]
Until writing of this case report, there has been no prior reporting of spontaneous retrograde migration of ureteral stone up to the kidneys in humans.
What is the prove that the stone seen in the kidney is the same stone that was in the ureter and not a newly formed stone, and that was in the ureter passed spontaneously?
CT scan that was done in April 26, 2015 showed the left lower ureteric stone, no other stones were detected on CT in the left kidney or right kidney and ureter.
X-ray KUB done after 3 days (April 29, 2015) shows a radio-opaque shadow at the left renal area, and the previously seen left lower ureteric opaque stone was no longer seen.
In conformation that the opaque shadow seen on X-ray was, in fact, a stone, CT-KUB was done on the same day that revealed a stone in the left kidney, of the same size as the one seen in the lower ureter on previous CT, and the previously seen stone at the lower ureter is no longer there.
The patient gave no history of any stone passage during these 3 days.
It is unlikely that a new stone has formed that was not detected in previous CT done just 3 days back.
CONCLUSION
Our case reveals a quite unexpected sequential event for a ureteric stone, which should be kept in mind in dealing with ureteric stone. Stone spontaneously moved retrograde for almost the full length of the ureter. It also highlights an important practice of doing imaging for the ureteric stone in the morning of surgery, to avoid unnecessary anesthesia to the patient.[10]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fwu CW, Eggers PW, Kimmel PL, Kusek JW, Kirkali Z. Emergency department visits, use of imaging, and drugs for urolithiasis have increased in the United States. Kidney Int. 2013;83:479–86. doi: 10.1038/ki.2012.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scales CD, Jr, Smith AC, Hanley JM, Saigal CS. Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur Urol. 2012;62:160–5. doi: 10.1016/j.eururo.2012.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kang HW, Lee SK, Kim WT, Kim YJ, Yun SJ, Lee SC, et al. Natural history of asymptomatic renal stones and prediction of stone related events. J Urol. 2013;189:1740–6. doi: 10.1016/j.juro.2012.11.113. [DOI] [PubMed] [Google Scholar]
- 4.Tüney D, Akpinar IN, Biren T, Aribal ME, Gürmen N. Inverted Y ureter anomaly and associated distal yo-yo phenomenon. Australas Radiol. 1998;42:154–6. doi: 10.1111/j.1440-1673.1998.tb00595.x. [DOI] [PubMed] [Google Scholar]
- 5.Eroglu M, Unsal A, Cimentepe E, Bakirtas H. Giant ureteral stone associated with partial ureteral duplication. Int Urol Nephrol. 2003;35:485–7. doi: 10.1023/b:urol.0000025626.06115.e3. [DOI] [PubMed] [Google Scholar]
- 6.Trinchieri A, Curhan G, Karlsen S, Wu KJ. Epidemiology. In: Segura J, Conort P, Khoury S, Pak C, Preminger GM, Tolley D, editors. Stone Disease; 1st International Consultation on Stone Disease; July 4-5, 2001; Paris, France. Paris: Health Publications; 2003. pp. 13–30. [Google Scholar]
- 7.Ahmad F, Nada MO, Farid AB, Haleem MA, Razack SM. Epidemiology of urolithiasis with emphasis on ultrasound detection: A retrospective analysis of 5371 cases in Saudi Arabia. Saudi J Kidney Dis Transpl. 2015;26:386–91. doi: 10.4103/1319-2442.152557. [DOI] [PubMed] [Google Scholar]
- 8.Feeney MM, Rosenblum ND. Urinary tract pacemaker cells: Current knowledge and insights from nonrenal pacemaker cells provide a basis for future discovery. Pediatr Nephrol. 2014;29:629–35. doi: 10.1007/s00467-013-2631-4. [DOI] [PubMed] [Google Scholar]
- 9.Dalby AM, Adams LG, Salisbury SK, Blevins WE. Spontaneous retrograde movement of ureteroliths in two dogs and five cats. J Am Vet Med Assoc. 2006;229:1118–21. doi: 10.2460/javma.229.7.1118. [DOI] [PubMed] [Google Scholar]
- 10.Youssef FR, Wilkinson BA, Hastie KJ, Hall J. Is pre-operative imaging essential prior to ureteric stone surgery? Ann R Coll Surg Engl. 2012;94:428–31. doi: 10.1308/003588412X13373405385458. [DOI] [PMC free article] [PubMed] [Google Scholar]


