Abstract
Background
Although the burden of neurological disorders is highest among populations in developing countries there is a dearth of data on the clinical spectrum of these disorders.
Objective
To profile the frequency of neurologic disorders and basic demographic data in an adult neurology out-patient service commissioned in 2011 in Kumasi, Ghana.
Methods
The study was conducted at the neurology clinic of the Komfo Anokye Teaching Hospital in Kumasi, Ghana. Over a three year period, all medical records of patients enrolled at the out-patient neurology clinic was reviewed by a neurologist and neurological diagnoses classified according to ICD-10.
Results
1812 adults enrolled for care in the neurology out-patient service between 2011 and 2013. This comprised of 882 males and 930 females (male: female ratio of 1.0: 1.1) with an overall median age of 54 (IQR, 39–69) years. The commonest primary neurological disorders seen were strokes, epilepsy and seizure disorders, and movement disorders at frequencies of 57.1%, 19.8%, and 8.2% respectively.
Conclusions
Cerebrovascular diseases, epilepsy and movement disorders were among the commonest neurological disorders and the major contributors to neurologic morbidity among Ghanaians in an urban neurology clinic.
Keywords: Neurologic disorders, Ghana, Demography, Spectrum
Highlights
-
•
An adult neurology clinic has been established in Kumasi, Ghana to provide services to a population of 10 million.
-
•
A 3-year retrospective review of 1,812 patients Stroke, Epilepsy and Parkinson’s disease are the neurological disorders.
-
•
Non-communicable diseases major contributors to the burden of neurological disorders in this urban clinic.
1. Introduction
Neurological disorders account for more than 6% of the global burden of diseases with a greater preponderance of mortality and disability-adjusted life years represented in low-and middle income countries [1]. Available data suggest a dearth of trained neurologists in developing countries. For instance, while the estimated neurologist to population ratio in sub-Saharan countries is 0.03 per 100,000 population, that in the Americas and in Europe are 0.89 and 4.84 respectively [2], [3], [4]. The coupling of lack of skilled human resources with the absence of the needed health infrastructure for neurological services in developing countries means that outcomes of neurological disorders in these settings would be poor unless urgent actions are taken to redress this situation.
Another corollary of the lack of neurologists in resource-limited settings is that the burden of neurological disorders within the community and indeed within hospital settings are not well characterised. Data on the practise of neurology from African settings are required to shed light on the spectrum of neurological disorders and the available level of care for patients with these disorders. In Ghana, a West African country with a population of 25 million, there are 6 neurologists located in 3 referral hospitals in two major cities—Kumasi and Accra. In 2011, an out-patient clinic for neurology services was opened at the Komfo Anokye Teaching Hospital, a tertiary referral centre situated in Kumasi in the central belt of Ghana. The aim of this study is to profile the frequency of neurological disorders and describe basic demographics of patients in our neurology out-patient service over a 3-year period from 2011 to 2013.
2. Methods
This study was approved by the Committee on Human Research Publication and Ethics (CHRPE) of the School of Medical Sciences, Kwame Nkrumah University of Science and Technology, and the Komfo Anokye Teaching Hospital (KATH), Kumasi. This is a retrospective study conducted at the neurology clinic of the Komfo Anokye Teaching Hospital in Kumasi, Ghana. The neurology clinic was established in 2011 by the lead author upon completion of fellowship training. The clinic runs once a week and receives referrals for adults > 16 years with neurologic disorders from 6 out of the 10 administrative regions of Ghana and serves an estimated population of 10 million. A quarter of referrals to the clinic are received from health centres located within the northern and middle belts of Ghana while the remainder are referred from within the teaching hospital particularly after patients have been discharged as in-patients. Occasionally paediatric neurology referrals are received. The clinic has two neurologists (F.S.S. and J.A.) and one nurse (E.B.). A review of neurologic disorders at the clinic from 2011 to 2013 was performed by a review of medical charts of patients by the two neurologists.
Neurologic diseases were classified according to the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) as follows: [1] inflammatory diseases of the central nervous system, [2] systemic atrophies primarily affecting the central nervous system, [3] extrapyramidal and movement disorders, [4] other degenerative diseases of the nervous system, [5] demyelinating diseases of the central nervous system, [6] episodic and paroxysmal disorders, [7] nerve, nerve root and plexus disorders, [8] polyneuropathies and other disorders of the peripheral nervous system, [9] diseases of myoneural junction and muscles, [10] cerebral palsy and other paralytic syndromes, [11] and other disorders of the nervous system. Clinical diagnoses were made by history taking and neurological examination followed by laboratory, radiological and electrophysiological studies as indicated. The range of laboratory testing available included complete blood count, ESR, renal and liver function tests, radiological testing including X-rays, computerised tomography and magnetic resonance imaging and an EEG which became available in late 2013. Among data recorded were age and gender and these were entered into excel spreadsheets by data entry clerks.
2.1. Statistical analysis
Means and medians were compared using either the student's t-test or Mann–Whitney's U-test for paired comparisons or ANOVA or Kruskal Wallis tests for more than 2 group comparisons. Statistical significance was set at a two-tailed p-value < 0.05 with no adjustment for multiple comparisons. Statistical analysis was performed using GraphPad Prism version 7 (GraphPad Software, Inc).
3. Results
3.1. Demography and frequency of classes of neurological disorders
In 2011, 2012 and 2013 a total of 715, 542 and 556 new patients respectively were enrolled for care at the neurology clinic. Thus a total of 1812 patients have been referred to the neurology clinic between January 2011 and December 2013. This comprises 882 males and 930 females (male:female ratio of 1.0:1.1) with an overall median age of 54 (IQR, 39–69) years. The median (IQR) age of females of 55 (38–72) years compared with that of males of 54 (40–66) years, p = 0.04. As shown in Table 1, the commonest primary neurological disorders seen were strokes, epilepsy and seizure disorders, and movement disorders at frequencies of 57.1%, 19.8%, and 8.2% respectively. However a patient could have more than one diagnosis hence a total of 1836 diagnoses were made. The top two most frequently co-existing neurological disorders were post-stroke seizure disorders (n = 12) and vascular dementia (n = 8).
Table 1.
Neurological disorders in Kumasi, Ghana according to ICD-10 classification.
| ICD-10 Classification | Neurological disorders | Frequency, n | Percent (%) |
|---|---|---|---|
| Episodic & paroxysmal disorders | Stroke | 1048 | 57.1 |
| Epilepsy & seizure disorders | 363 | 19.8 | |
| Headaches | 30 | 1.6 | |
| Extrapyramidal & movement disorders | Movement disorders | 151 | 8.2 |
| Nerve, nerve root & plexus disorders | Peripheral nerve disorders | 40 | 2.2 |
| Diseases of myoneuronal junction & muscle | 12 | 0.7 | |
| Inflammatory diseases of the Central Nervous System | Intra-cranial infections | 16 | 0.9 |
| Transverse myelitis | 6 | 0.3 | |
| Demyelinating diseases of the central nervous system | Multiple sclerosis & Neuromyelitis optica | 7 | 0.4 |
| Other neurodegenerative diseases of the nervous system | Dementing illnesses | 42 | 2.3 |
| Friedreich's ataxia | 3 | 0.2 | |
| Cerebral palsy & other paralytic syndromes | Neuro-developmental disorders | 5 | 0.3 |
| Compressive myelopathy | 50 | 2.7 | |
| Non-neurological disorders | Neuro-psychiatric disorders | 18 | 1.0 |
| Brain tumours | 16 | 0.9 | |
| Neuro-cutaneous disorders | 1 | 0.1 | |
| Cranio-trauma | 1 | 0.1 | |
| Unclassified | 27 | 1.5 | |
| Total | 1836 | 100 |
As shown in Table 2, the number of visits to neurology clinic has increased from 1399 visits in 2011 to 2144 in 2013. Similarly, the proportion of visits to the OPD outfit for neurology services increased from 2.0% to 4.1% over the period. Patients after enrolling at the clinic are followed up between one to six monthly appointments.
Table 2.
Neurology clinic attendance in Kumasi, Ghana between 2011 and 2013.
| Year | Total OPD attendance | Number of neurology visits | % of OPD visits to neurology clinic |
|---|---|---|---|
| 2011 | 68,335 | 1399 | 2.0 |
| 2012 | 65,620 | 1900 | 2.9 |
| 2013 | 52,400 | 2144 | 4.1 |
| Total | 186,355 | 5443 | 2.9 |
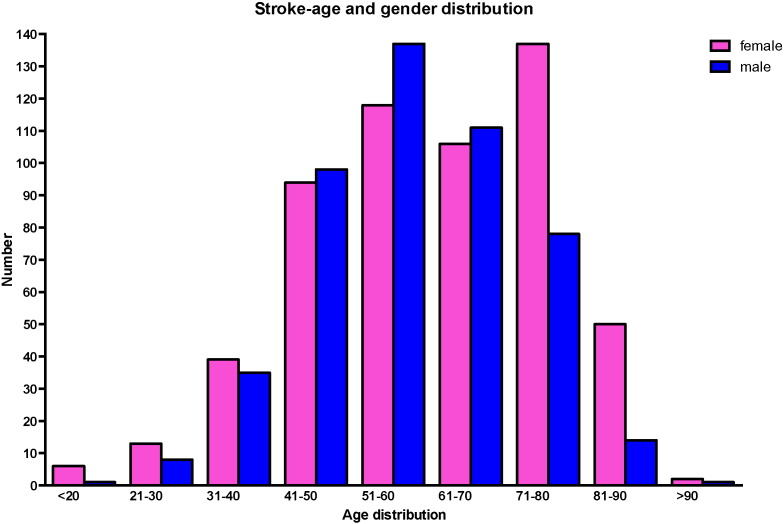
3.2. Strokes and cerebrovascular disorders
Out of 1048 patients with stroke and other cerebrovascular disorders, 483 were males and 565 were females with a male:female ratio of 1.0:1.2. The median (IQR) age of females of 61 (50–74) years was significantly higher than that of males, 57 (49–67) years, p = 0.0003 with an overall median age of 59 (IQR, 49–72) years. The modal age range for males and females were 51–60 years and 71–80 respectively as shown in Fig. 1. 207 out of 1048 (19.8%) had cranial CT scan performed soon after stroke to allow for stroke typing — 115 had ischaemic strokes, 61 had intra-cerebral haemorrhagic strokes and 31 had sub-arachnoid haemorrhages. The median (IQR) age of patients with haemorrhagic, sub-arachnoid and ischaemic strokes were 50 (43–57) years, 52 (43–67) years and 65 (52–72) years respectively with p < 0.0001 (Kruskal Wallis test) and the male/female proportions for the respectively CT-typed strokes were 34/27, 61/54 and 8/9. There were only 6 referrals of transient ischemic attacks for evaluation.
Fig. 1.
Age and gender distribution of stroke patients at a neurology clinic in a tertiary referral centre in Ghana.
Medications available for the control of hypertension among stroke survivors include ACE-Inhibitors, Angiotensin Receptor Blockers, Beta-blockers, Calcium Channel Blockers, Diuretics and methyldopa and hydralazine when needed. A range of oral hypoglycaemic agents including Metformin, first and second generation sulphonylureas, and thiazolidinediones are available on National Insurance for patients as is Insulin. Commonly prescribed statins include Atorvastatin, Rosuvastatin and Simvastatin while antiplatelets such as Aspirin and Clopidogrel are available for secondary stroke prevention. Available rehabilitation services include physiotherapy, however speech and occupational therapy services are not.
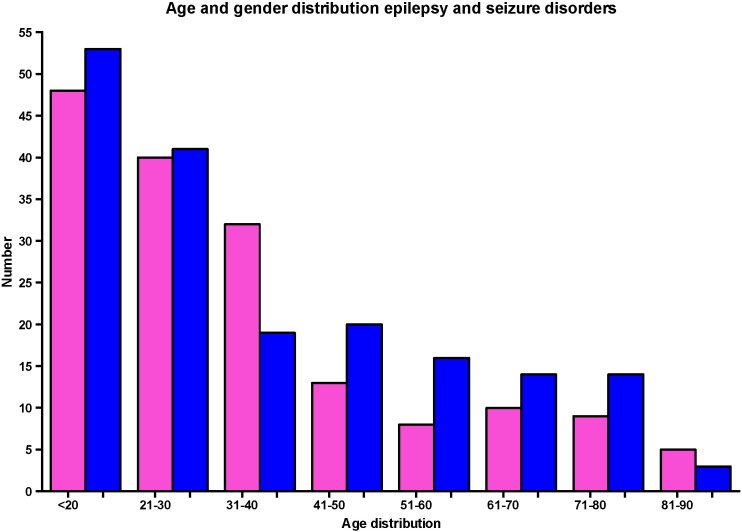
3.3. Epilepsy and seizure disorders
363 patients had epilepsy with active convulsive seizures, 184 were males and 178 were females with a male:female ratio of 1.0:1.0 and median (IQR) ages of 29 (20–52) and 28 (19–42) years respectively, p > 0.05. The modal age of epilepsy and seizure disorders was between 12 and 20 years for both sexes as shown in Fig. 2. The median age of seizure onset was 12 (IQR: 5–54) years. 343 (94%) patients had generalised seizures (336 tonic–clonic, 5 absence and 2 myoclonic types) and 20 (6%) had focal seizures (18 with secondary generalisation and 2 simple partial). Ninety (25%) patients with seizure disorders had cranial CT scans of which 70 (78%) were normal hence were classified as having idiopathic epilepsy, and 20 (12%) were thought to have symptomatic or secondary seizures from previous strokes (n = 14), alcohol-related seizures (n = 3), meningioma (n = 1), neurocysticercosis (n = 1), post-head trauma (n = 1). Inter-ictal electroencephalographic evaluations were performed only to 15 patients with abnormal findings in 6 cases. Four of the 6 with abnormal electroencephalographic evaluations had focal EEG findings and the remaining 2 had generalised epileptiform discharges. Antiepileptic medications and their cost per month of treatment for management of epilepsy include Carbamazepine (≈$20–30 per month), Sodium valproate (≈$30–60 per month), Phenytoin (≈$10–20 per month), Levetiracetam (≈$40–60 per month), Topiramate (≈$25–40 per month), with very limited role for Phenobarbitone.
Fig. 2.
Age and gender distribution of patients with seizure disorders at a neurology clinic in a tertiary referral centre in Ghana.
3.4. Movement disorders
151 patients had movement disorders of which 120 had Parkinsonism and 31 had hyperkinetic movement disorders comprising 16 Essential Tremors, 6 with choreo-athetoid movements disorders, 5 with dystonia, 2 tics and 2 myoclonus. Among patients with Parkinsonism, male-to-female ratio was 2.1:1.0 with a median age (IQR) of 65 years (58–74) overall with no significant differences in age according to gender. 85% with Parkinsonism had idiopathic Parkinson's disease, 10% had vascular Parkinsonism and the remainder had Parkinson plus syndromes (Multiple System Atrophy). Parkinson's disease patients are treated with Levo-dopa with a peripheral decarboxylase inhibitor which are given free of charge to patients as donation by the Parkinson Disease in Africa project. The Parkinson's Disease in Africa project is a collaborative effort between the Parkinson's Institute, Instituti Clinici di Perfezionamento of Milan, Italy and three Ghanaian hospitals, Komfo Anokye Teaching Hospital, Korle-Bu Teaching Hospital and Comboni Hospital and recently with hospitals in Zambia. Furthermore, this partnership is driving research into Parkinson's disease and training clinicians in neuro-degenerative diseases in resource-limited settings.
3.5. Dementias, cranial infections & cephalgias
34 cases of dementing illnesses were diagnosed — 22 vascular dementia, 10 Alzheimer's disease, 1 Binswanger's disease and 1 fronto-temporal dementia. Median (IQR) age for vascular dementia compared Alzheimer's disease was 66 (60–72) years vs 76 (71–89) years, p = 0.001.
There were 14 consultations on account of cranial infective diseases including 7 HIV patients with cerebral toxoplasmosis [5] and progressive multifocal leucoencephalopathy [2]; 5 cases of post-bacterial meningitis follow up and 2 cases of Herpes Simplex encephalitis. Out of 30 consultations for headaches, 19 were due to primary cephalgias and 11 due to secondary causes. Primary headaches were commonly due to migraine (n = 9), tension-type headaches (n = 5), trigeminal neuralgia (n = 4), cluster headaches (n = 1); while secondary headaches were due to sinusitis (n = 6), idiopathic intracranial hypertension (n = 2), hypertension-related cephalgia (n = 2) and post-traumatic cephalgia (n = 1).
3.6. Demyelinating disorders of the CNS
Seven females aged between 18 and 30 met clinical, neuro-radiological criteria as well as demonstrable presence of oligoclonal bands for the diagnosis of demyelinating inflammatory disorders of the CNS. Four out of the seven patients had Neuromyelitis optica on clinical grounds without evidence of Anti-aquaporin-4 autoantibody confirmation due to cost and unavailability of the test in-country.
3.7. Spinal cord disorders & peripheral nerve disorders
Of 56 disorders referable to the spinal cord, 50 were compressive myelopathy due to degenerative disc disorders and 6 were non-compressive were transverse myelitis of presumed infective aetiology. The distributions of 40 peripheral nerve disorders were as follows: 24 symmetrical polyneuropathy, 13 mononeuropathies involving the cranial nerve VII (n = 8), cranial nerve III (n = 1), cranial nerve VIII (n = 1), median nerve (n = 1) and common peroneal nerve (n = 2); 2 sacral plexopathies and one polyradiculopathy due to chronic inflammatory demyelinating polyradiculopathy.
3.8. Neuromuscular junction & muscle disorders
Of the 6 cases of myasthenia gravis, gender distribution was equal and median age was 23 (range: 18 to 39) years. Primary muscle disorders included 5 cases of post-inflammatory myopathy and one case of dermatomyositis.
3.9. Miscellaneous
There were 18 primary neuro-psychiatric diagnoses — 16 with generalised anxiety disorders, 1 each with panic disorder and depression. Of 16 cases of cranial tumours — 9 were astrocytomas, 2 were meningiomas, and 1 each with acoustic neuroma in a patient type 2 neurofibromatosis, pituitary macroadenoma, and metastatic melanoma.
Out of 27 cases with non-conclusive evaluations — 12 presented with cerebellar signs, 6 presented with syncopal attacks with seizures as differential diagnosis, 5 had vertiginous spells, and 4 presented with dysphasia on non-vascular origin. Notably, we had one case of head trauma due to the presence of a vibrant neuro-surgery department at our institution where cases of cranio-trauma are primarily seen.
4. Discussion
In this cohort of 1812 patients referred to an adult neurology specialist clinic in an urban Ghanaian setting, we found that stroke was the commonest presenting neurologic disorder followed by epilepsy and movement disorders. At the global level epilepsy, headaches and cerebrovascular disorders are among the top three prevalent neurological disorders [5], [6], [7], [8], [9] seen at specialist neurology services whilst in primary care setting headaches, epilepsy and vertebral disorders featured most frequently [10], [11], [12], [13], [14]. Thus with the notable exception of headaches which had a lower frequency in the present study, the spectrum of neurologic disorders concur with other similar studies. In Ghana headaches are managed by Primary Physicians while epilepsy traditionally has been seen by Psychiatrists due to unavailability of specialised neurology services.
The major contributor of neurological disorders in the present study was non-infectious diseases such as stroke, epilepsy and Parkinson's disease contrary to previous studies conducted in sub-Saharan Africa where infectious disorders of the nervous system were most commonly observed [15], [16], [17], [18], [19], [20], [21]. There are however important differences in study designs worth noting. Most studies conducted in SSA like the present one are retrospective in design and have either focused on in-patient admissions or combined in-patient and out-patient neurology cases. Some studies have combined paediatric and adult neurology cases and were either conducted in a rural setting or urban settings. Finally, very few studies have been conducted within community settings to characterise the burden of neurological disorders [22], [23] where tremors, headache, stroke, peripheral polyneuropathy and upper limb mononeuropathy were prevalent among the elderly population. The focus for the present study was to provide an in-depth characterisation of the spectrum of neurologic disorders in an out-patient setting where follow-up of cases would allow for full evaluation to establish diagnosis. It is most likely that the array of cases captured in this series was strongly influenced by the high proportions of in-patients referrals received from our teaching hospital. This could for instance explain the high frequencies of strokes observed in this cohort.
The explosion of vascular risk factors such as hypertension, dyslipidaemia and diabetes mellitus in many developing countries has led to escalating rates of cardiovascular diseases mainly stroke and ischemic heart diseases [24], [25]. Hence it is not surprising that stroke is the commonest neurologic disorder in our cohort. Stroke patients were relatively younger compared with those in developed countries. We have recently published data on stroke admissions and mortality between 1983 and 2013 from Kumasi to show that nearly 40% of patients presenting with stroke for admission succumb and that the majority of stroke survivors are discharged with severe functional limitations [26], [27], [28]. It is remarkable that only six cases of transient ischemic attack (TIA) were reflected in this cohort, an observation that may be explained by the low perceived awareness of the relevance of TIAs and health-seeking behaviour patterns for cerebrovascular disorders in resource-limited settings in general. Hence as has been suggested, a comprehensive approach to tackling the menace of stroke in developing countries is urgent since stroke affects the population at the prime of their life [29], [30]. We found vascular dementia the commonest form of dementia within this cohort and this is largely attributable to lack of awareness of and poor control of vascular risk factors.
Over 85% of people living with epilepsy are found in low- and middle-income countries including sub-Saharan Africa [31]. There was no gender predilection among patients with epilepsy as has been previously reported [32] and a median age of seizure onset of 12 years. A recent community-based multicentre study in SSA reported a median age of seizure onset of 5.3 years from a sample of both children and adults [32]. Seizure semiology in this cohort was severely limited by lack of EEG and neuro-imaging hence although 94% had generalised seizures, it is possible that a reasonable proportion may have had focal-onset seizures with secondary generalisation. The recent introduction of EEG services at the clinic is an exciting addition to the diagnostic armamentarium to improve care of patients with epilepsy (kind donation by co-author A.A.).
Neuro-degenerative disorders such Parkinson's disease and Alzheimer's disease were also frequent in this cohort. Although community-based surveys have reported a low prevalence of Parkinson's disease among rural African compared to the Western populations [33], [34], [35], it featured as the third most common neurological disorder in this urban hospital-based study. The median age of patients with Parkinsonism was 65 years and this is comparable to other cohorts from SSA [34], [35], [36]. The management of neurodegenerative diseases such as Parkinson's disease is challenged [37], [38] in our settings by the lack of life-saving medications such as Levodopa which in our centre is provided free of charge to patients by the kind donation by the Parkinson's Disease in Africa Project. Projections by WHO suggest that by 2025, about three-quarters of the estimated 1.2 billion people aged 60 years and older will reside in developing countries with a prediction that dementia rates will rise at an alarming rate in these settings in tandem with an ageing population [39], [40], [41], [42]. In the present cohort, the relative frequency of dementia was low and could be due to several reasons including the perception that such illnesses are perceived as “normal part of ageing” and also the fact that patients with dementia may be referred to see Psychiatrists in our hospital for management. Strategic planning and resource allocation is urgently required to prepare health care services for this impending epidemic of Neuro-degenerative disorders in developing countries.
Patients with primary headaches and infections of the nervous system were often managed by primary care physicians hence the low frequency of these disorders in this study. Although considered a rarity in hot tropical climates, 7 females with central nervous system demyelinating diseases were observed. In particular four of these seven patients had semiology suggestive of Neuromyelitis optica with long segment transverse myelitis and optic neuritis, however testing antibodies against Aquaporin-4 proteins could not be conducted. Further studies are needed to clarify the burden, clinical forms and outcomes of demyelinating disorders in tropical Africa.
Management of neurological disorders has been challenged by lack of diagnostic support for patients. CT and MRI scans are paid for by patients out-of-pocket and EEG services only became available late 2013. The clinic does not have an EMG/NCS services and are sourced from the national capital 240 km away from the clinic in Kumasi. These limitations have impacted on our ability to establish and sub-classify neurological disorders in this cohort. However these patients were evaluated by trained neurologists and were mostly diagnosed on clinical grounds with laboratory confirmation a significant proportion of cases. A further challenge in patient management is the inability to afford medications on a sustainable basis for their clinical conditions. With a median age of 54 years, patients with neurological disorders in our cohort were either retired or unemployed due to disability, hence enlisting neurology care within National Health Insurance would be a major step towards alleviating the health economic burden. With increasing numbers of patients visiting the neurology clinic, the need for training more neurologists has become the more urgent to improve quality and standards of care.
In conclusion, within this adult urban neurology clinic in Kumasi, we found non-communicable diseases such as stroke, epilepsy and Parkinson's disease contributed significantly to the burden of neurological disorders.
Conflict of interest
None to declare.
Acknowledgements
The authors acknowledge the following grant support from the NIH for the published manuscript titled 'Profile of neurological disorders in an adult neurology clinic in Kumasi, Ghana'. 1. Stroke Investigative Research Education Networks (SIREN): U54HG007479 2. Tailored Hospital-based Risk Reduction to Impede Vascular Events after Stroke (THRIVES): U01 NS079179.
References
- 1.Lopez A.D., Mathers C., Ezzati M. The World Bank and Oxford University Press; Washington, DC: 2006. Global Burden of Disease and Risk Factors. [PubMed] [Google Scholar]
- 2.Menken M. The scope of neurologic practice and care in England, Canada, and the United States. Is there a better way? Arch Neurol. 1989;46:210–213. doi: 10.1001/archneur.1989.00520380116024. [DOI] [PubMed] [Google Scholar]
- 3.Birbeck G.L. A neurologist in Zambia. Lancet Neurol. 2002;1:58–61. doi: 10.1016/s1474-4422(02)00007-8. [DOI] [PubMed] [Google Scholar]
- 4.2004. Neurology Atlas 2004. WHO. [Google Scholar]
- 5.Hopkins A., Menken M., DeFriese G. A record of patient encounters in neurological practice in the United Kingdom. J Neurol Neurosurg Psychiatry. 1989;52:436–438. doi: 10.1136/jnnp.52.4.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perkin G.D. An analysis of 7836 successive new outpatient referrals. J Neurol Neurosurg Psychiatry. 1989;52:447–448. doi: 10.1136/jnnp.52.4.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singhal B.S., Gursahani R.D., Menken M. Practice patterns in neurology in India. Neuroepidemiology. 1992;11:158–162. doi: 10.1159/000110926. [DOI] [PubMed] [Google Scholar]
- 8.Holloway R.G. US neurologists in the 1990s: trends in practice characteristics. Neurology. 1999;52:1353–1361. doi: 10.1212/wnl.52.7.1353. [DOI] [PubMed] [Google Scholar]
- 9.Gonzalez Menacho J., Olive Plana J.M. Epidemiology of ambulatory neurological diseases at the Baix Camp. Neurologia. 2001;16:154–162. [PubMed] [Google Scholar]
- 10.Miller J.Q. The neurologic content of family practice. Implications for neurologists. Arch Neurol. 1986;43:286–288. doi: 10.1001/archneur.1986.00520030072021. [DOI] [PubMed] [Google Scholar]
- 11.Papapetropoulos T., Tsibre E., Pelekoudas V. The neurological content of general practice. Journal of Neurology. Neurosurg. Psychiatry. 1989;52:434–435. doi: 10.1136/jnnp.52.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Birbeck G.L. Barriers to care for patients with neurologic disease in rural Zambia. Arch Neurol. 2000;57:414–417. doi: 10.1001/archneur.57.3.414. [DOI] [PubMed] [Google Scholar]
- 13.Lavados P.M., Gomez V., Sawada M. Neurological diagnostics in primary health care in Santiago, Chile. Rev Neurol. 2003;36:518–522. [PubMed] [Google Scholar]
- 14.Lester F.T. Neurological diseases in Addis Ababa, Ethiopia. Afr J Med Med Sci. 1979;8:7–11. [PubMed] [Google Scholar]
- 15.Osuntokun B.O. The pattern of neurological illness in tropical Africa. Experience at Ibadan. J Neurol Sci. 1971;4:417–442. doi: 10.1016/0022-510x(71)90110-9. [DOI] [PubMed] [Google Scholar]
- 16.Matuja W.P., Makene W.J. Neurological disease pattern in adults admitted to the medical wards at Muhimbili Medical Centre, Dar es Salaam. Tanzan Med J. 1989;4:18–21. [Google Scholar]
- 17.TO Kwasa. The pattern of neurological disease at Kenyatta National Hospital. East Afr Med J. 1992;69:236–239. [PubMed] [Google Scholar]
- 18.Birbeck G.L. Neurological disease in a rural Zambian Hospital. Trop Doct. 2001;31:82–85. doi: 10.1177/004947550103100209. [DOI] [PubMed] [Google Scholar]
- 19.Bower J.H., Asmera J., Zebenigus M. The burden of in-patient neurologic disease in two Ethiopian hospitals. Neurology. 2007;68:322–323. doi: 10.1212/01.wnl.0000252801.61190.e8. [DOI] [PubMed] [Google Scholar]
- 20.Winkler A.S., Mosser P., Schmutzhard E. Neurological disorders in rural Africa: a systematic approach. Trop Doct. 2009;102-104 doi: 10.1258/td.2008.080144. [DOI] [PubMed] [Google Scholar]
- 21.Siddiqi O.K., Atadzhanov M., Birbeck G.L. The spectrum of neurological disorders in a Zambian Tertiary care hospital. J Neurol Sci. 2010;290(1–2):1–5. doi: 10.1016/j.jns.2009.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dewhurst F., Dewhurst M.J., Gray W.K. The prevalence of neurological disorders in older people in Tanzania. Acta Neurol Scand. 2013;127(3):198–207. doi: 10.1111/j.1600-0404.2012.01709.x. [DOI] [PubMed] [Google Scholar]
- 23.Dewhurst F., Dewhurst M.J., Gray W.K. Rates of diagnosis and treatment of neurological disorders within a prevalent population of community-dwelling elderly people in sub-Saharan Africa. J Epidemiol Glob Health. 2012;2(4):207–214. doi: 10.1016/j.jegh.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mensah G., Roth G., Sampson U. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990-2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr. 2015;26:S6–S10. doi: 10.5830/CVJA-2015-036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Owolabi M.O., Mensah G.A., Kimmel P.L. Understanding the rise in cardiovascular diseases in Africa: harmonizing H3Africa genomic epidemiological teams and tools. Cardiovasc J Afr. 2014;25(3):134–136. doi: 10.5830/CVJA-2014-030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sarfo F.S., Acheampong J.W., Tetteh L.A. The profile of risk factors and in-patient outcomes of stroke in Kumasi, Ghana. Ghana Med J. 2014;48(3):127–134. doi: 10.4314/gmj.v48i3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sarfo F.S., Akassi J., Awuah D. Trends in stroke admission and mortality rates from 1983 to 2013 in central Ghana. J Neurol Sci. 2015 doi: 10.1016/j.jns.2015.07.043. (pii:S0022-510X(15)0046405) [DOI] [PubMed] [Google Scholar]
- 28.Sarfo F.S., Awuah D.O., Nkyi C. Recent patterns and predictors of neurological mortality among hospitalized patients in Central Ghana. J Neurol Sci. 2016;363:217–224. doi: 10.1016/j.jns.2016.02.041. [DOI] [PubMed] [Google Scholar]
- 29.Owolabi M.O., Akarolo-Anthony S., Akinyemi R. The burden of stroke in Africa: a glance at the present and a glimpse into the future. Cardiovasc J Afr. 2015;26:S27–S38. doi: 10.5830/CVJA-2015-038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Owolabi M.O. Taming the burgeoning stroke epidemic in Africa: stroke quadrangle to the rescue. West Indian Med J. 2011;60(4):412–421. [PubMed] [Google Scholar]
- 31.Ngugi A.K., Bottomley C., Kleinschmidt I. Estimation of the burden of active and life-time epilepsy: a meta-analytic approach. Epilepsia. 2010;51:883–890. doi: 10.1111/j.1528-1167.2009.02481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kariuki S.M., Matuja W., Akpalu A. Clinical features, proximate causes, and consequences of active convulsive epilepsy in Africa. Epilepsia. 2014;55(1):76–85. doi: 10.1111/epi.12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Scheonberg B.S., Osuntokun B.O., Adeuja A.O. Comparison of the prevalence of Parkinson's disease in black populations in the rural United Satates and in rural Nigeria. Neurology. 1988;38:645–646. doi: 10.1212/wnl.38.4.645. [DOI] [PubMed] [Google Scholar]
- 34.Winkler A.S., Tutuncu E., Trendafilova A. Parkinsonism in a population of northern Tanzania: a community-based door-to-door study in combination with a prospective hospital-based evaluation. J Neurol. 2010;257(5):799–805. doi: 10.1007/s00415-009-5420-z. [DOI] [PubMed] [Google Scholar]
- 35.Dotchin C.L., Msuya O., Kissima J. The prevalence of Parkinson's disease in rural Tanzania. Mov Disord. 2008;23(11):1567–1572. doi: 10.1002/mds.21898. [DOI] [PubMed] [Google Scholar]
- 36.Okubadejo N.U., Ojo O.O., Oshinaike O.O. Clinical profile of parkinsonism and Parkinson's disease in Lagos, Southwestern Nigeria. BMC Neurol. 2010;10:1. doi: 10.1186/1471-2377-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cilia R., Akpalu A., Sarfo F.S. The modern pre-levodopa era of Parkinson's disease: insights into motor complications from sub-Saharan Africa. Brain. 2014;137(Pt 10):2731–2742. doi: 10.1093/brain/awu195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dotchin C.L., Msuya O., Walker R.W. The challenge of Parkinson's disease management in Africa. Age Ageing. 2007;36:122–127. doi: 10.1093/ageing/afl172. [DOI] [PubMed] [Google Scholar]
- 39.WHO . World Health Organisation; Geneva: 2002. Active Ageing: a Policy Framework, 2002 Health Report. [Google Scholar]
- 40.Ferri C.P., Prince M., Brayne C. Global prevalence of dementia: a Delphi consensus study. Lancet. 2005;366:2112–2117. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Suh G.H., Shah A. A review of the epidemiological transition in dementia — cross-national comparisons of the indices related to Alzheimer's disease and vascular dementia. Acta Psychiatr Scand. 2001;104:4–11. doi: 10.1034/j.1600-0447.2001.00210.x. [DOI] [PubMed] [Google Scholar]
- 42.Kalaria R.N., Maestre G.E., Arizaga R. Alzheimer's disease and vascular dementia in developing countries: prevalence, management, and risk factors. Lancet Neurol. 2008;7(9):812–826. doi: 10.1016/S1474-4422(08)70169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]