Significance
The food system is responsible for more than a quarter of all greenhouse gas emissions while unhealthy diets and high body weight are among the greatest contributors to premature mortality. Our study provides a comparative analysis of the health and climate change benefits of global dietary changes for all major world regions. We project that health and climate change benefits will both be greater the lower the fraction of animal-sourced foods in our diets. Three quarters of all benefits occur in developing countries although the per capita impacts of dietary change would be greatest in developed countries. The monetized value of health improvements could be comparable with, and possibly larger than, the environmental benefits of the avoided damages from climate change.
Keywords: sustainable diets, dietary change, food system, health analysis, greenhouse gas emissions
Abstract
What we eat greatly influences our personal health and the environment we all share. Recent analyses have highlighted the likely dual health and environmental benefits of reducing the fraction of animal-sourced foods in our diets. Here, we couple for the first time, to our knowledge, a region-specific global health model based on dietary and weight-related risk factors with emissions accounting and economic valuation modules to quantify the linked health and environmental consequences of dietary changes. We find that the impacts of dietary changes toward less meat and more plant-based diets vary greatly among regions. The largest absolute environmental and health benefits result from diet shifts in developing countries whereas Western high-income and middle-income countries gain most in per capita terms. Transitioning toward more plant-based diets that are in line with standard dietary guidelines could reduce global mortality by 6–10% and food-related greenhouse gas emissions by 29–70% compared with a reference scenario in 2050. We find that the monetized value of the improvements in health would be comparable with, or exceed, the value of the environmental benefits although the exact valuation method used considerably affects the estimated amounts. Overall, we estimate the economic benefits of improving diets to be 1–31 trillion US dollars, which is equivalent to 0.4–13% of global gross domestic product (GDP) in 2050. However, significant changes in the global food system would be necessary for regional diets to match the dietary patterns studied here.
The choices we make about the food we eat affect our health and have major ramifications for the state of the environment. The food system is responsible for more than a quarter of all greenhouse gas (GHG) emissions (1), of which up to 80% are associated with livestock production (2, 3). The aggregate dietary decisions we make thus have a large influence on climate change. High consumption of red and processed meat and low consumption of fruits and vegetables are important diet-related risk factors contributing to substantial early mortality in most regions while over a billion people are overweight or obese (4). Without targeted dietary changes, the situation is expected to worsen as a growing and more wealthy global population adopts diets resulting in more GHG emissions (5) and that increase the health burden from chronic, noncommunicable diseases (NCDs) associated with high body weight and unhealthy diets (6).
Recent analyses have highlighted the environmental benefits of reducing the fraction of animal-sourced foods in our diets and have also suggested that such dietary changes could lead to improved health (7–14). They have shown that reductions in meat consumption and other dietary changes would ease pressure on land use (11, 12) and reduce GHG emissions (7, 11–14). Changing diets may be more effective than technological mitigation options for avoiding climate change (14) and may be essential to avoid negative environmental impacts such as major agricultural expansion (7) and global warming of more than 2 °C (13) while ensuring access to safe and affordable food for an increasing global population (8, 15).
The diets investigated in these studies include diets with a pro rata reduction in animal products (ruminant meat, total meat, dairy) (11, 13, 14), specific dietary patterns that include reduced or no meat (such as Mediterranean, “pescatarian,” and vegetarian diets) (11, 12), and diets based on recommendations about healthy eating (7, 11). The health consequences of adopting these diets have not been explicitly modeled or quantitatively analyzed, but instead inferences have been drawn from information available in the epidemiological literature (16). In the most comprehensive study to date, Tilman and Clark (12) analyzed the GHG emissions of a series of diets that differed in their animal-sourced food content and presented their results alongside a series of observational studies of the health consequences of adopting the different diets.
Here, we use a region-specific global health model to link the health and environmental consequences of changing diets. We also make a first attempt, to our knowledge, to estimate the economic value of different dietary choices through their effects on health and the environment. For the health analysis, we built a comparative risk assessment model to estimate age and region-specific mortality associated with changes in dietary and weight-related risk factors (4, 17). The specific risk factors influence mortality through dose–response relationships, which allow us to compare different dietary scenarios based on their exposure to those risk factors. Given the availability of consistent epidemiological data, we focused on changes in the consumption of red meat, and of fruits and vegetables, which together accounted for more than half of diet-related deaths in 2010 (4), and also on the fraction of people who are overweight or obese through excess calorie consumption, which too is associated strongly with chronic disease mortality (18, 19). The disease states included were coronary heart disease (CHD), stroke, type 2 diabetes (T2DM), and cancer that is an aggregate of site-specific cancers. These four disease states accounted for about 60% of NCD deaths and for about 40% of deaths globally in 2010 (6). Given that dietary and weight-related risk factors are predominantly associated with chronic disease mortality, we focused on the health implications of changes in those risk factors for adults (aged 20 y and older).
For the environmental analysis, we linked regional and scenario-specific food type consumption levels to GHG emissions using Tilman and Clark’s metaanalysis of life cycle studies (12) although we adjusted for likely future productivity improvements (3). In the economic analysis, we placed a monetary value on changes in GHG emissions by using estimates of the social cost of carbon (20) and explored monetizing the health consequences using the value of statistical life (21, 22) and projections of health-care expenditure by cause of death (23–25). We stress from the outset that we consider the economic valuation to be a first step and that the estimates are not exactly comparable nor do they include all consequences of dietary changes.
We used this coupled modeling framework to analyze the environmental and health impacts of four dietary scenarios in the year 2050 (SI Appendix, Table S1) (7, 9–13). The first (referred to below as REF) is a reference scenario based on projections from the Food and Agriculture Organization of the United Nations (FAO), with adjustments to take into account the fraction of nonedible and wasted food (26, 27). The second scenario [healthy global diets (HGD)] assumes the implementation of global dietary guidelines on healthy eating (16, 28) and that people consume just enough calories to maintain a healthy body weight (29). The last two scenarios also assume a healthy energy intake but based on observed vegetarian diets (30, 31), either including eggs and dairy [lacto-ovo vegetarian (VGT)] or completely plant-based [vegan (VGN)]. The three nonreference scenarios are not intended to be realizable dietary outcomes on a global level but are designed to explore the range of possible environmental and health outcomes of progressively excluding more animal-sourced foods from human diets (7, 9–13).
The different diet scenarios were implemented by adjusting the region-specific diets described in the REF scenario, which maintained the regional character of food consumption (SI Appendix, section SI.1). The HGD diet included (per day) a minimum of five portions of fruits and vegetables (16), fewer than 50 g of sugar (16), a maximum of 43 g of red meat (28), and an energy content of 2,200–2,300 kcal, depending on the age and sex composition of the population (29). The VGT and VGN diets differed from the HGD in including six (VGT) or seven (VGN) portions of fruits and vegetables (30, 31) and one portion of pulses (30, 31), with no red meat, poultry, or fish, and in the VGN diet no dairy or eggs. Energy intake was adjusted to the target levels by varying the proportion of staple foods in the diet, but preserving their region-specific composition.
Results
Less than half of all regions meet, or are projected to meet, dietary recommendations for the consumption of fruit, vegetables, and red meat, and also exceed the optimal total energy intake (SI Appendix, Fig. S1). As a consequence, large changes in the food system would be necessary to achieve the dietary patterns considered here (SI Appendix, Table S7). In the HGD scenario, the changes include increasing global fruit and vegetable consumption by 25% (99 g⋅d−1) and by more in Sub-Saharan Africa (190%, 323 g⋅d−1), South Asia (101%, 248 g⋅d−1), and Latin America (39%, 138 g⋅d−1) and decreasing global red meat consumption by 56% (42 g⋅d−1), and by more in Western high-income and middle-income countries (78%, 113 g⋅d−1 and 69%, 72 g⋅d−1, respectively), East Asia (74%, 93 g⋅d−1), and Latin America (72%, 83 g⋅d−1). The nonmeat diets require greater increases in the consumption of fruits and vegetables (VGT, 39%, 152 g⋅d−1; VEG, 54%, 212 g⋅d−1), and of pulses (324%, 61 g⋅d−1, each). Compared with the reference scenario, the alternative diets require 15% less total energy intake.
Health Impacts.
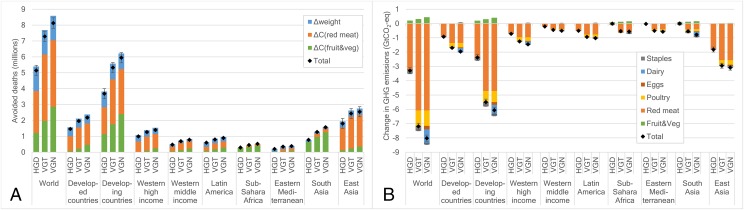
Moving to diets with fewer animal-sourced foods would have major health benefits (Fig. 1A). Compared with the reference scenario, we project that adoption of global dietary guidelines (HGD) would result in 5.1 million avoided deaths per year [95% confidence interval (CI), 4.8–5.5 million] and 79 million years of life saved (CI, 75–83 million) (Fig. 1A and SI Appendix, Fig. S2). The equivalent figures for the vegetarian (VGT) diet are 7.3 million avoided deaths (CI, 7.0–7.6 million) and 114 million life years saved (CI, 111–118 million) and for the vegan (VGN) diet 8.1 million avoided deaths (CI, 7.8–8.5 million) and 129 million life years saved (CI, 125–133 million). Differentiated by risk factor, more than half of avoided deaths (51–57% across the three scenarios) were due to decreased red meat consumption, 24–35% to increased fruit and vegetable consumption, and 19–30% to a lower prevalence of being overweight and obese associated with limiting excessive energy intake. The reduced mortality in the VGT and VGN scenarios compared with the HGD scenario was due to lower red meat consumption (1.7 million additional avoided deaths in each) and higher fruit and vegetable consumption (VGT, 0.8 million; VGN, 1.8 million additional avoided deaths). Across the three nonreference scenarios, about 45–47% of all avoided deaths were from reduced coronary heart disease (CHD), 26% from stroke, 16–18% from cancer, and 10–12% from type 2 diabetes mellitus (T2DM) (SI Appendix, Fig. S3). Adopting the nonreference diets reduced the combined number of deaths per year from CHD, stroke, cancer, and T2DM in 2050 by 12% (HGD), 17% (VGT), and 19% (VEG) and the overall number of deaths from all causes by 6% (HGD), 9% (VGT), and 10% (VEG) (SI Appendix, Table S8).
Fig. 1.
Health and environmental analysis of dietary change for the year 2050. The diet scenarios include a reference scenario based on FAO projections (REF), a scenario based on global guidelines on healthy eating and energy intake (HGD), and scenarios based on vegetarian (VGT) and vegan (VGN) dietary patterns. (A) Number of avoided deaths in the dietary scenarios relative to the reference scenario in 2050 by risk factor and region. Risk factors include changes in the consumption of fruits and vegetables [ΔC(fruit&veg)] and red meat [ΔC(red meat)], combined changes in overweight and obesity (Δweight), and all risk factors combined (Total). The regional aggregation is detailed in SI Appendix, Table S3 and section SI.1). (B) Changes in food-related greenhouse gas (GHG) emissions in the dietary scenarios relative to the reference scenario in 2050 by food group and region.
Our analysis allows a regional breakdown of the health benefits of dietary change. The greatest number of avoided deaths (∼72% across the three nonreference scenarios) occurred in developing countries, in particular in East Asia (31–35%) and South Asia (15–19%) (Fig. 1A). Reducing red meat consumption was the risk factor that had the most positive effect on health in East Asia (78–82%), Western high- and middle-income countries (64–71%; 58–65%), and Latin America (42–48%). Increasing fruit and vegetable consumption was responsible for the majority of avoided deaths in the least developed regions (South Asia, 75–83%; Sub-Saharan Africa, 72–84%). Reduced energy intake and the consequent fewer people overweight and obese were particularly important in the Eastern Mediterranean (41–79%), Latin America (32–48%), and Western high- and middle-income countries (29–40%; 20–33%). The model results can also be expressed as avoided deaths per capita, a measure of personal risk (SI Appendix, Figs S5–S7). By this measure the greatest benefits of dietary change occurred in developed countries due to the relatively larger per capita reductions in red meat consumption and total energy intake that are necessary to meet dietary guidelines (HGD) or a vegetarian diet (VGT, VGN) (SI Appendix, Table S7).
Emissions Impacts.
In line with other studies (7, 12, 13), we find that dietary changes toward less animal-sourced foods can help mitigate an expected growth in food-related GHG emissions. Under our reference scenario, we project GHG emissions associated with food consumption to increase by 51%, from 7.6 ± 0.1 giga tonnes (Gt)⋅y−1 (measured in CO2 equivalents) in 2005/2007 to 11.4 ± 0.2 Gt⋅y−1 in 2050 (SI Appendix, Fig. S8). Food-related GHG emissions in the HGD scenario were 8.1 ± 0.1 Gt⋅y−1, which is 29% less than REF emissions in 2050 and 7% greater than emissions in 2005/2007. The two vegetarian diets resulted in food-related GHG emissions at midcentury (VGT, 4.2 ± 0.1 Gt⋅y−1; VEG, 3.4 ± 0.1 Gt⋅y−1) that were 45–55% lower than the 2005/2007 levels and 63–70% lower than REF emissions. Emissions reductions in the HGD scenario were largely attributable to reduced red meat consumption (3.2 ± 0.1 GtCO2, 97%) whereas reductions in red meat (6.1 ± 0.1 GtCO2, 85%) and poultry (1.08 ± 0.01 GtCO2, 15%) were responsible for lower VGT emissions, and lower consumption of red meat (76%), poultry (13%), and eggs and dairy (1.2 ± 0.03 GtCO2, 15%) for lower VGN emissions (Fig. 1B). In relation to an emissions pathway that is believed to be likely to limit global temperature increase to below 2 °C (32), we project that the ratio of food-related GHG emissions to GHG emissions from all sources increases from 16% in 2005/2007 to 52%, 37%, 19%, and 15% in 2050 in the REF, HGD, VGT, and VGN scenarios, respectively (SI Appendix, Fig. S6 and section SI.3).
We can identify where changes to region-specific diets contribute the most to reduced GHG emissions. About three-quarters of the total reductions (72–76% across the nonreference scenarios) occurred in developing countries, in particular in East Asia (HGD, 55%; VGT, 41%; VEG, 38%) and Latin America (13–15%) (Fig. 1B). In contrast, food-related GHG emissions per capita fell twice as much in developed compared with developing countries across all three nonreference scenarios (SI Appendix, Fig. S10), driven mainly by reductions in red meat consumption (SI Appendix, Table S7). As a result, the difference in food-related per capita GHG emissions between developed and developing countries narrowed (SI Appendix, Fig. S9). The average per capita GHG emissions from someone in a developing country was 53% that of a person from a developed country in the REF scenario but only 26% and 20% in the HGD and VGT scenarios, respectively. In the VGN scenario, food-related GHG emissions per capita were 4% lower in developed countries than in developing ones, which was due to higher fruit and vegetable consumption in some developing countries (exceeding adjusted values in the baseline) (SI Appendix, Table S8). On a country level, 77 out of the 105 regions in the environmental analysis reduced their food-related GHG emissions per capita in the HGD scenario whereas an increase occurred in 28 (SI Appendix, Fig. S11). These increases in emissions were relatively minor (together they made up about 2% of the total changes in food-related GHG emissions) and were primarily due to increasing energy intake in regions with extensive current undernourishment, in particular in Africa. In the VGT and VGN scenarios, the number of regions where per capita food-related GHG emissions increased was reduced from 28 to 1 (the Democratic Republic of the Congo).
Economic Valuation.
We used two complementary approaches to assess the economic value of the health benefits associated with dietary change. First, using “cost-of-illness” techniques (23, 25), we calculated the direct health-care costs and the indirect costs of informal care and lost work days that are associated with deaths from specific diseases. Second, we used region-specific data on the willingness of individuals to pay for incremental mortality reductions, the “value of statistical life” (VSL) (21, 22), to obtain an estimate of the cost of the lives (and life-years) saved under each dietary scenario. The two approaches span the range of potential valuation methods (33, 34); the VSL approach is commonly used in cost-benefit analysis (22) to indicate societal preferences whereas the cost-of-illness approach, in particular its direct cost component, highlights the economic impact on the health-care sector and on patients (23, 25).
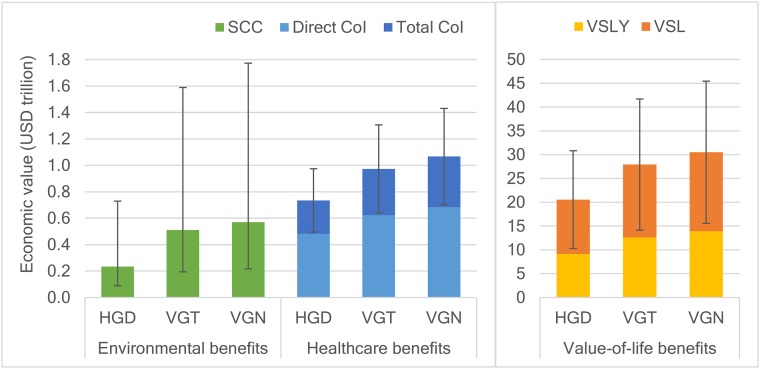
Using the cost-of-illness approach, we estimate that the health-related cost savings of moving to the diets based on dietary guidelines (HGD) from that assumed in the REF scenario will be 735 billion US dollars per year ($735 billion⋅y−1) in 2050 with values in the range [based on uncertainties in the cost transfer method (Methods)] $482–987 billion⋅y−1 (Fig. 2). Greater savings occur with the adoption of vegetarian diets (VGT, $973 billion⋅y−1, range $644–1,303 billion⋅y−1) and vegan diets ($1,067 billion⋅y−1, range $708–1,426 billion⋅y−1). As a percentage of expected world gross domestic product (GDP) in 2050, these savings amount to 2.3% (1.5–3.1%) for HGD diets, 3.0% (2.0–4.0%) for VGT diets, and 3.3% (2.2–4.4%) for VGN diets. About two thirds of the savings (64–66% across the nonreference scenarios) were due to reductions in direct health care-related costs, a third (31–33%) to less need for unpaid informal care (although this figure is an underestimate because we were not able to obtain estimates of the indirect costs of diabetes), and a small fraction (3–4%) to reduced productivity from lost labor time (SI Appendix, Fig. S12). Although more than twice as many deaths were avoided in developing countries than in developed ones, more than half of all cost savings (54–56%) occurred in developed countries due to their higher health expenditure and income (SI Appendix, Fig. S12 and Fig. 1A).
Fig. 2.
Economic valuation of the health and environmental benefits of dietary change compared with a reference scenario for the year 2050. The three nonreference scenarios are as follows: one based on global guidelines on healthy eating and energy intake (HGD) and two based on vegetarian and vegan dietary patterns (VGT and VGN). (Left) The value of environmental benefits derived from estimates of the social cost of carbon (SCC) and the value of healthcare benefits based on estimates of the costs of illness (CoI), including direct healthcare costs and total costs, which also include indirect costs associated with unpaid informal care and productivity losses from lost labor time. (Right) The value of health benefits associated with the willingness to pay for mortality reductions based on the value of statistical life and life-year (VSL and VSLY). The uncertainty intervals for the environmental valuation stem from different SCC values in 2050 [71 US dollars per ton of CO2 (71 USD/tCO2); 27–221 USD/tCO2], and the uncertainty intervals for the health valuation stem from high and low values of the costs of illness (±30%) and the VSL (±50%).
The value-of-statistical-life approach led to much higher estimates of the economic benefits associated with dietary change (Fig. 2). For the HGD scenario, we estimate that the monetized value associated with diet-related changes in mortality amount to 21 trillion (or 1012) US dollars per year ($21 trillion⋅y−1) in 2050 with a range (again reflecting uncertainties in the methodology) of $10–31 trillion⋅y−1. The values we obtain for the VGT diet are $28 trillion⋅y−1 ($14–42 trillion⋅y−1), and for the VGN diet $30 trillion⋅y–1 ($15–46 trillion⋅y−1). In terms of percentage of expected global GDP in 2050, these values amount to 9% (4–14%) for HGD diets, 12% (6–18%) for VGT diets, and 13% (6–20%) for VGN diets (Fig. 2). A criticism of the VSL approach, which treats each avoided death as equally valuable, is that most of the avoided deaths occur late in life (SI Appendix, Fig. S4). Recalculating the estimates by monetizing the years of life saved reduces them by approximately one half (Fig. 2). The regional distribution of the monetized economic benefits broadly corresponds to the distribution of changes in mortality despite regional variation in the value of statistical life (SI Appendix, Fig. S13).
To explore the economic benefits of reduced GHG emissions, we used estimates of the social cost of carbon (20) for the year 2050 and calculated the value of avoided harm due to less CO2 in the atmosphere (Fig. 2). We found that adoption of diets meeting dietary guidelines (HGD) would have monetized environmental benefits of $234 billion⋅y−1, with values in the range $89–729 billion⋅y−1 for different assumptions about discount rates (Methods). The benefits were greater for diets with fewer animal-sourced foods: for VGT, $511 billion⋅y−1 ($194–1,589 billion⋅y−1) and, for VGN, $570 billion⋅y−1 ($217–1,773 billion⋅y−1). As a percentage of expected world GDP in 2050, the benefits amounted to 0.10% (0.04–0.32%) for HGD diets, 0.22% (0.08–0.69%) for VGT diets, and 0.25% (0.09–0.77%) for VGN diets. The regional distribution of the monetized environmental benefits largely reflects the changes in GHG emissions (SI Appendix, Fig. S14 and Fig. 1B).
Discussion
Our analysis indicates that dietary changes toward fewer animal and more plant-based foods are associated with significant benefits due to reductions in diet-related mortality and GHG emissions. Changes in the consumption of red meat, fruits, and vegetables and in total energy intake could result in reductions in total mortality of 6–10%, compared with a reference diet in 2050. This estimate is likely an underestimate of the total impact that the dietary patterns studied here could have on diet-related mortality because we were not able to model the health consequences of changes in the consumption of all food groups. For example, diets with fewer animal-sourced foods typically include more nuts and whole grains (30, 31), which evidence suggests have health benefits and are likely to increase the number of avoided deaths (4). Similarly, it is known that salt and sugar ingested in sugary drinks affect health (4), but comparative international data on their effects is insufficient to include in our models whereas the health impacts of other food groups (for example dairy) is inconclusive (35). Wherever possible, we have placed confidence estimates around our results, but we are aware that other sources of uncertainty exist that we have not been able to treat. Those uncertainties include food demand and mortality projections, possible deviations from the linear dose–response relationships linking risk factors and mortality, and our inability to remove all possible confounding effects when deriving relative risk parameters.
Our health estimates are in line with current epidemiological evidence. Tilman and Clark (12) reported results from a metaanalysis that indicated that adopting vegetarian, pescatarian, and Mediterranean dietary patterns could reduce overall mortality by 0–18%. Orlich et al. (36) reported results from a prospective cohort study, focused on vegetarian dietary patterns, that indicated reductions in mortality from all causes in vegetarians and vegans compared with nonvegetarians of 9% and 15%, respectively; and, in combining those results with two preceding prospective cohort studies, Le and Sabaté (37) reported reductions in mortality in vegetarians compared with nonvegetarians living in the United States of 12–20%. However, a prospective cohort study focused on vegetarians living in the United Kingdom found no statistically significant reduction in mortality compared with nonvegetarians (38), the reasons for which are debated (37). In general, it should be noted that inferring the health impacts of dietary patterns from observational studies is complicated by the potential presence of multiple confounding factors (even if some are controlled for).
The strength of our health analysis is that we used dose–response relationships of dietary and weight-related risk factors, such as changes in red meat consumption and overweight, that are epidemiologically more robust than the association of mortality with complete diets. With this approach, we were able to analyze differences in mortality caused by changes in consumption of specific food groups in individual regions. We found that about half of the global avoided deaths occurred because of the consumption of less red meat and that the other half was due to a combination of increased fruit and vegetable consumption and reductions in total energy intake (and the associated decreases in the fraction of people overweight and obese). However, there were marked regional variations. For example, the two areas with the greatest number of avoided deaths were East Asia and South Asia, in the former primarily driven by reduced red meat consumption and in the latter by increased fruit and vegetable consumption. Regions also differed in whether the net sum of avoided deaths was due to a modest reduction in the risk of mortality of many people or a larger reduction in the risks to a smaller population. The greatest improvement in per capita risk reductions occurred in Western high- and middle-income countries due to reduced red meat consumption and lower energy intakes.
In our environmental analysis, we project reference emissions to increase by 51% between 2005/20007 and 2050 (from 7.6 GtCO2-eq to 11.4 GtCO2-eq) and dietary changes to decrease the reference emissions by 29–70% (3.3–8.0 GtCO2-eq). The latter is likely to be a conservative estimate because we did not account for the beneficial impacts of dietary change on land use through avoided deforestation. Other studies have estimated that the associated emissions reductions could amount to 2.1–2.8 GtCO2-eq per year between 2010 and 2050 (7, 12). We also did not take into account emissions feedbacks from increased life expectancy in the dietary-change scenarios. However, such effects are likely to be small for the health impacts estimated here (SI Appendix, section SI.9).
In aggregate, our results are consistent with previous studies of the environmental consequences of dietary change. Hedenus et al. (13) projected that dietary changes (ranging from the partial replacements of ruminant meats with other meats, and of animal products with pulses and cereals) could reduce food-related GHG emissions in 2050 by 3.4–5.2 GtCO2-eq and that technical mitigation in the agricultural sector and increased productivity could lead to additional reductions of 1.7–2 GtCO2-eq each. Tilman and Clark (12) projected that adopting Mediterranean, pescatarian, and vegetarian diets would reduce food-related GHG emissions in 2050 by 4.2–8.4 GtCO2-eq, and Bajželj et al. (7) projected reductions of 5.8–6.4 GtCO2-eq in 2050 if dietary recommendations were globally adopted. In contrast to our study, Bajželj et al. (7) included land-use emissions, and their dietary scenario is largely based on national health guidelines, which are more stringent than the global ones we used in our HGD scenario. Although we adopted the same baseline GHG emissions factors as Tilman and Clark (12), our reference estimates are slightly lower than theirs (SI Appendix, section SI.10) because we accounted for output-based productivity improvements in agriculture (which lower emissions intensities), and we did not account for the GHG emissions associated with the consumption of fish and seafood. Another difference is that we used food demand projections produced by FAO whereas Tilman and Clark generated their own income-dependent ones.
The strength of our environmental analysis is that we were able to explore regional details. For example, we found that some increases in food consumption-related GHG emissions would be necessary to achieve global dietary recommendations in Sub-Saharan Africa but that, overall, adopting global dietary recommendations would reduce the food-related per capita emissions gap between developing and developed countries (and close the gap completely if purely plant-based diets were adopted). Our analysis also indicated that adopting global dietary guidelines would not be enough to reduce food-related GHG emissions to the same extent that total GHG emissions will need to fall to achieve a climate stabilization pathway that would have a high probability of limiting global temperature increases to below 2 °C (32). For managing food demand (including efficiency improvements in line with current trends) to make its prorated contribution, reductions in animal-based foods of the degree found only in the VGN scenario would be required. Given that such reductions would be hard to achieve, our analysis suggests that, to achieve climate stabilization, a balance will need to be struck between the degree of adoption of plant-based diets, advances in mitigation technologies of the food sector, and disproportionate reductions in non–food-related GHG emissions.
In our economic analysis, we found that the economic value of the health benefits associated with more plant-based diets is comparable with, or exceeds, the value of the environmental benefits (depending on the valuation method used). However, although these valuation techniques are routinely used in cost-benefit analyses (20, 22), they are not strictly comparable. The value of environmental benefits represents the value of avoided damages, the health benefits based on cost-of-illness estimates capture the direct and some of the indirect healthcare costs avoided, and the health benefits based on value-of-statistical-life estimates can be interpreted as the aggregate value that individuals in society would be willing to pay for the reductions in mortality associated with the different dietary patterns. In assessing the worth of public programs aimed to achieve healthier and more environmentally sustainable diets, the use of measures based on avoided costs provides a narrow estimate of cost-effectiveness whereas the use of the value-of-statistical-life approach can be seen as providing a broader estimate of net societal benefits.
We are not aware of other studies that contrasted the value of environmental and health benefits (SI Appendix, section SI.11), and we repeat the caveat that the valuation techniques we used are subject to significant uncertainties. The most important source of uncertainty for the environmental valuation is the discount rate used to calculate the net present value of the future harm caused by climate change. For example, changing the discount rate from five to a measure that assumes higher than expected impacts of temperatures in the upper tails of the modeled distribution (Methods) increases the value of the environmental benefits of the HGD diet scenario from $89 billion to $729 billion. The main source of uncertainty in the health valuation involves the benefit transfer technique (Methods) used to obtain region-specific costs-of-illness (CoI) and value-of-statistical-life (VSL) estimates. Ideally, we would have used values that were specifically estimated for the regions used. However, such data do not exist for all of the regions included in this study, so instead we used a comprehensive and quality-screened database of VSL estimates (21, 22) and a regional set of comparable CoI estimates (23–25). The valuation based on CoI estimates might be further improved by the inclusion of comorbidities that can affect the costs attributable to specific disease, and by breaking down aggregate cancer costs into site-specific costs. Sufficient data already exist in some regions to explore the latter, but not enough for a global analysis (34). Finally, we note that we did not assess the market responses associated with dietary changes: e.g., due price changes, which remain an important area for future research.
There is a general consensus that dietary change across the globe can have multiple health, environmental, and economic benefits (12). Our analysis confirms this view and takes a step forward in providing better estimates of the magnitude of the possible benefits and how they are distributed across different regions. It introduces a framework to analyze multiple costs and benefits across different sectors simultaneously. The size of the projected benefits, even taking into account all of the caveats about the unavoidable sources of uncertainty in our work, should encourage researchers and policy makers to act to improve consumption patterns. But we also show the magnitude of the task. To achieve the HGD diet that embodies a (minimal) global consensus on the consumption of a few major food groups would require a 25% increase in the number of fruits and vegetables eaten globally and a 56% reduction in red meat whereas, overall, the human species would need to consume 15% fewer calories. We hope our work will help identify the targeted, region-specific interventions (8, 39) that will be needed on both the production and consumption sides of the food system to achieve these benefits.
Methods
In the health analysis, we estimated the mortality and disease burden attributable to dietary and weight-related risk factors by calculating “population attributable fractions” (PAFs). PAFs describe the proportions of disease cases that would be avoided were the risk exposure changed from a baseline to a counterfactual (4, 17). We assumed that changes in relative risks follow a dose–response relationship (4) and that PAFs combine multiplicatively (4, 40). Changes in mortality were calculated by multiplying region- and disease-specific PAFs by region, disease, and age-specific death rates and population numbers (SI Appendix, section SI.2). In addition to changes in mortality, we also calculated the years of life lost (YLL) due to a change in dietary and weight-related risk factors. We did this calculation by multiplying each age-specific death by the life expectancy at that age using the Global Burden of Disease standard abridged life table (40).
We used publically available data sources to parameterize the comparative risk analysis. Population and mortality projections for the year 2050 were adapted from the United Nations Population Division and the World Health Organization (WHO), respectively. The diet and weight-related relative risk parameters (SI Appendix, Table S4) were taken from pooled analyses of prospective cohort studies (18, 19) and from metaanalyses of prospective cohort and case-control studies (28, 41–46). The cancer associations have been judged as probable or convincing by the World Cancer Research Fund, and, in each case, a dose–response relationship had been identified and there was consistent evidence suggesting a plausible mechanism (28). For the weight-related risk assessment, we used the scenario estimates of total energy intake to estimate changes in the prevalence of being overweight and obese based on historical relationships between weight categories and caloric availability using data from the WHO and the FAO (SI Appendix, section SI.2).
In the environmental analysis, we calculated the environmental impacts associated with the different dietary scenarios by using commodity-specific GHG emissions factors. The emissions factors are adopted from a recent metaanalysis of life cycle analyses (LCAs) that estimated the “cradle to farm gate” emissions of different food items (12), with adjustments to account for likely productivity improvements that would reduce GHG intensity over time (3) (SI Appendix, section SI.3). The factors exclude emissions from land-use change and post–farm-gate activities, such as processing, packaging, and transportation to households. We did not include GHG emissions related to the consumption of fish and seafood because those food groups are not resolved in the projections of food demand used in this study (26).
To estimate the economic consequences of the health impacts, we used two complementary costing methods (33, 34): the value-of-statistical-life (VSL) approach (22) and the cost-of-illness (CoI) approach (47). We based our VSL valuation on a comprehensive global metaanalysis of stated preference surveys of mortality risk valuation undertaken for the Organization for Economic Co-operation and Development (OECD) (21). Following OECD recommendations, we adopted a VSL base value for the European Union (EU) of 3.5 million US dollars (1.75–5.25 million US dollars) and used the benefit-transfer method to calculate VSLs in other regions (22), taking into account differences in income expressed as GDP per capita adjusted for purchasing power parity (PPP) and projected to 2050 (SI Appendix, section SI.4). We also monetized the health impact in terms of years of life lost (YLL) by using the value of statistical life year (VSLY). We calculated the VSLY for each region by expressing the VSL as the discounted net present value of the VSLY throughout a lifetime, adopting a discount rate of 3% and a maximum age of 86 adapted from the Global Burden of Disease standard life table. We used nonlinear programming (GAMS, NLP solver) to numerically solve for the VSLYs per region (SI Appendix, section SI.4).
To implement the CoI approach, we used a cost transfer method to estimate the costs of illness in different parts of the world. This technique is similar to the benefit transfer method described above, and it has been used in other global assessments (34). We based our cost-of-illness estimates on a comparative assessment of the economic burden of cardiovascular diseases (23, 24) and cancer (25) across the EU. We adopted the total cost estimate associated with CHD, stroke, and cancer for the EU in 2009, which included direct costs (healthcare expenditure, health service utilization, expenditure on medication) and indirect costs (opportunity costs of informal care, productivity costs due to mortality and morbidity), calculated costs per death based on mortality statistics (24), and estimated the costs per death by disease in the EU and other regions in 2050 by scaling the base values by the ratio of health expenditure per capita for direct costs and by the ratio of GDP per capita (adjusted for purchasing power parity) for indirect costs (SI Appendix, section SI.4). Productivity losses due to morbidity and mortality, which are a part of the indirect costs, were included only for deaths occurring among adults of working age (<65 y old). For the CoI analysis related to diabetes (SI Appendix, section SI.4), we adopted country-specific cost estimates (48) and, to avoid double-counting of cardio vascular disease-related complications, adjusted those estimates for the incremental cost component specifically attributable to diabetes (49, 50).
In the economic valuation of the environmental effects of dietary change, we estimated the monetary value of changes in GHG emissions. We used estimates of the social cost of carbon (SCC), which represents the monetized damages associated with an incremental increase in carbon emissions. The values adopted are based on a comprehensive integrated-assessment modeling exercise facilitated by technical experts from several US agencies (20). For the year 2050, the SCC estimates are 27, 71, 98, and 221 US dollars⋅ton−1 of CO2 for discount rates of 5%, 3%, and 2.5%, and the 95th percentile at a 3% discount rate. The last value is designed to represent the possible higher than expected economic impacts from climate change further out in the tails of the SCC distribution (20).
Supplementary Material
Acknowledgments
We thank Aikaterini Kavallari (FAO) for data support and valuable comments and Alastair Gray (HERC, University of Oxford) for useful discussions.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
Data deposition: The region-specific results of the health, environmental, and economic valuation analyses have been deposited in the Oxford University Research Archive (ORA), ora.ox.ac.uk/ (doi: 10.5287/bodleian:XObxm2ebO).
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1523119113/-/DCSupplemental.
References
- 1.Vermeulen SJ, Campbell BM, Ingram JSI. Climate change and food systems. Annu Rev Environ Resour. 2012;37(1):195–222. [Google Scholar]
- 2.Steinfeld H, et al. Livestock’s Long Shadow. FAO; Rome: 2006. [Google Scholar]
- 3.Tubiello FN, et al. Agriculture, Forestry and Other Land Use Emissions by Sources and Removals by Sinks: 1990–2011 Analysis. FAO Statistics Division; Rome: 2014. [Google Scholar]
- 4.Lim SS, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Popkin BM. Global nutrition dynamics: The world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. 2006;84(2):289–298. doi: 10.1093/ajcn/84.1.289. [DOI] [PubMed] [Google Scholar]
- 6.Lozano R, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bajželj B, et al. Importance of food-demand management for climate mitigation. Nat Clim Chang. 2014;4(10):924–929. [Google Scholar]
- 8.Godfray HCJ, et al. Food security: The challenge of feeding 9 billion people. Science. 2010;327(5967):812–818. doi: 10.1126/science.1185383. [DOI] [PubMed] [Google Scholar]
- 9.Hallström E, Carlsson-Kanyama A, Börjesson P. Environmental impact of dietary change: A systematic review. J Clean Prod. 2015;91:1–11. [Google Scholar]
- 10.Ripple WJ, et al. Ruminants, climate change and climate policy. Nat Clim Chang. 2014;4(1):2–5. [Google Scholar]
- 11.Stehfest E, et al. Climate benefits of changing diet. Clim Change. 2009;95(1):83–102. [Google Scholar]
- 12.Tilman D, Clark M. Global diets link environmental sustainability and human health. Nature. 2014;515(7528):518–522. doi: 10.1038/nature13959. [DOI] [PubMed] [Google Scholar]
- 13.Hedenus F, Wirsenius S, Johansson DJA. The importance of reduced meat and dairy consumption for meeting stringent climate change targets. Clim Change. 2014;124(1-2):79–91. [Google Scholar]
- 14.Popp A, Lotze-Campen H, Bodirsky B. Food consumption, diet shifts and associated non-CO2 greenhouse gases from agricultural production. Glob Environ Change. 2010;20(3):451–462. [Google Scholar]
- 15.Ray DK, Mueller ND, West PC, Foley JA. Yield trends are insufficient to double global crop production by 2050. PLoS One. 2013;8(6):e66428. doi: 10.1371/journal.pone.0066428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO . Diet, Nutrition and the Prevention of Chronic Diseases: Report of the Joint WHO/FAO Expert Consultation. WHO; Geneva: 2003. [Google Scholar]
- 17.Murray CJ, Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S. Comparative quantification of health risks conceptual framework and methodological issues. Popul Health Metr. 2003;1(1):1. doi: 10.1186/1478-7954-1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berrington de Gonzalez A, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010;363(23):2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whitlock G, et al. Prospective Studies Collaboration Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Interagency Working Group . Technical Update on the Social Cost of Carbon for Regulatory Impact Analysis-Under Executive Order 12866. Office of Management and Budget; Washington, DC: 2013. [Google Scholar]
- 21.Lindhjem H, Navrud S, Braathen NA, Biausque V. Valuing mortality risk reductions from environmental, transport, and health policies: A global meta-analysis of stated preference studies. Risk Anal. 2011;31(9):1381–1407. doi: 10.1111/j.1539-6924.2011.01694.x. [DOI] [PubMed] [Google Scholar]
- 22.OECD . Mortality Risk Valuation in Environment, Health and Transport Policies. OECD; Paris: 2012. [Google Scholar]
- 23.Leal J, Luengo-Fernández R, Gray A, Petersen S, Rayner M. Economic burden of cardiovascular diseases in the enlarged European Union. Eur Heart J. 2006;27(13):1610–1619. doi: 10.1093/eurheartj/ehi733. [DOI] [PubMed] [Google Scholar]
- 24.Nichols M, Townsend N, Scarborough P, Rayner M. European Cardiovascular Disease Statistics. European Heart Network AISBL; Brussels: 2012. [Google Scholar]
- 25.Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: A population-based cost analysis. Lancet Oncol. 2013;14(12):1165–1174. doi: 10.1016/S1470-2045(13)70442-X. [DOI] [PubMed] [Google Scholar]
- 26.Alexandratos N, Bruinsma J. World Agriculture Towards 2030/2050: The 2012 Revision. FAO; Rome: 2012. [Google Scholar]
- 27.Gustavsson J, Cederberg C, Sonesson U, Van Otterdijk R, Meybeck A. Global Food Losses and Food Waste: Extent, Causes and Prevention. FAO; Rome: 2011. [Google Scholar]
- 28.WCRF/AICR . Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective. AICR; Washington, DC: 2007. [Google Scholar]
- 29.WHO 2004. Human Energy Requirements: Report of a Joint FAO/WHO/UNU Expert Consultation, Rome, Italy, 17–24 October 2001 (WHO, Geneva)
- 30.Haddad EH, Tanzman JS. What do vegetarians in the United States eat? Am J Clin Nutr. 2003;78(3) Suppl:626S–632S. doi: 10.1093/ajcn/78.3.626S. [DOI] [PubMed] [Google Scholar]
- 31.Scarborough P, et al. Dietary greenhouse gas emissions of meat-eaters, fish-eaters, vegetarians and vegans in the UK. Clim Change. 2014;125(2):179–192. doi: 10.1007/s10584-014-1169-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.UNEP . The Emissions Gap Report 2014. United Nations Environment Programme; Nairobi: 2014. [Google Scholar]
- 33.WHO . WHO Guide to Identifying the Economic Consequences of Disease and Injury. WHO; Geneva: 2009. [Google Scholar]
- 34.Bloom DE, et al. The Global Economic Burden of Noncommunicable Diseases. World Economic Forum; Geneva: 2011. [Google Scholar]
- 35.Willett WC, Stampfer MJ. Current evidence on healthy eating. Annu Rev Public Health. 2013;34(1):77–95. doi: 10.1146/annurev-publhealth-031811-124646. [DOI] [PubMed] [Google Scholar]
- 36.Orlich MJ, et al. Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern Med. 2013;173(13):1230–1238. doi: 10.1001/jamainternmed.2013.6473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Le LT, Sabaté J. Beyond meatless, the health effects of vegan diets: Findings from the Adventist cohorts. Nutrients. 2014;6(6):2131–2147. doi: 10.3390/nu6062131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Key TJ, et al. Mortality in British vegetarians: Results from the European Prospective Investigation into Cancer and Nutrition (EPIC-Oxford) Am J Clin Nutr. 2009;89(5):1613S–1619S. doi: 10.3945/ajcn.2009.26736L. [DOI] [PubMed] [Google Scholar]
- 39.Garnett T, Mathewson S, Angelidis P, Borthwick F. Policies and Actions to Shift Eating Patterns: What Works? A Review of the Evidence of the Effectiveness of Interventions Aimed at Shifting Diets in More Sustainable and Healthy Directions. Food Climate Research Network; Oxford: 2015. [Google Scholar]
- 40.Murray CJL, et al. GBD 2010: Design, definitions, and metrics. Lancet. 2012;380(9859):2063–2066. doi: 10.1016/S0140-6736(12)61899-6. [DOI] [PubMed] [Google Scholar]
- 41.Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: A systematic review and meta-analysis. Circulation. 2010;121(21):2271–2283. doi: 10.1161/CIRCULATIONAHA.109.924977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen G-C, Lv D-B, Pang Z, Liu Q-F. Red and processed meat consumption and risk of stroke: A meta-analysis of prospective cohort studies. Eur J Clin Nutr. 2013;67(1):91–95. doi: 10.1038/ejcn.2012.180. [DOI] [PubMed] [Google Scholar]
- 43.Dauchet L, Amouyel P, Dallongeville J. Fruit and vegetable consumption and risk of stroke: A meta-analysis of cohort studies. Neurology. 2005;65(8):1193–1197. doi: 10.1212/01.wnl.0000180600.09719.53. [DOI] [PubMed] [Google Scholar]
- 44.Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: A meta-analysis of cohort studies. J Nutr. 2006;136(10):2588–2593. doi: 10.1093/jn/136.10.2588. [DOI] [PubMed] [Google Scholar]
- 45.Li M, Fan Y, Zhang X, Hou W, Tang Z. Fruit and vegetable intake and risk of type 2 diabetes mellitus: Meta-analysis of prospective cohort studies. BMJ Open. 2014;4(11):e005497. doi: 10.1136/bmjopen-2014-005497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Feskens EJM, Sluik D, van Woudenbergh GJ. Meat consumption, diabetes, and its complications. Curr Diab Rep. 2013;13(2):298–306. doi: 10.1007/s11892-013-0365-0. [DOI] [PubMed] [Google Scholar]
- 47.Akobundu E, Ju J, Blatt L, Mullins CD. Cost-of-illness studies: A review of current methods. Pharmacoeconomics. 2006;24(9):869–890. doi: 10.2165/00019053-200624090-00005. [DOI] [PubMed] [Google Scholar]
- 48.Zhang P, et al. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(3):293–301. doi: 10.1016/j.diabres.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 49.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033–1046. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Köster I, Huppertz E, Hauner H, Schubert I. Direct costs of diabetes mellitus in Germany: CoDiM 2000-2007. Exp Clin Endocrinol Diabetes. 2011;119(6):377–385. doi: 10.1055/s-0030-1269847. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.